Abstract
Background
Patients with left ventricular dysfunction have an elevated risk of sudden cardiac death. However, the substrate for ventricular arrhythmia in patients with nonischemic cardiomyopathy remains poorly understood. We hypothesized that the distribution of scar identified by MRI is predictive of inducible ventricular tachycardia.
Methods and Results
Short-axis cine steady-state free-precession and postcontrast inversion-recovery gradient-echo MRI sequences were obtained before electrophysiological study in 26 patients with nonischemic cardiomyopathy. Left ventricular ejection fraction was measured from end-diastolic and end-systolic cine images. The transmural extent of scar as a percentage of wall thickness (percent scar transmurality) in each of 12 radial sectors per slice was calculated in all myocardial slices. The percentages of sectors with 1% to 25%, 26% to 50%, 51% to 75%, and 76% to 100% scar transmurality were determined for each patient. Predominance of scar distribution involving 26% to 75% of wall thickness was significantly predictive of inducible ventricular tachycardia and remained independently predictive in the multivariable model after adjustment for left ventricular ejection fraction (odds ratio, 9.125; P=0.020).
Conclusions
MR assessment of scar distribution can identify the substrate for inducible ventricular tachycardia and may identify high-risk patients with nonischemic cardiomyopathy currently missed by ejection fraction criteria.
Keywords: electrophysiology, magnetic resonance imaging, tachyarrhythmias
Detection of scar tissue by stress-rest perfusion imaging has been associated with a higher risk of ventricular arrhythmia and sudden cardiac death in the setting of ischemic cardiomyopathy.1 Recent advances have allowed detailed imaging of nonviable myocardium with high spatial resolution on contrast-enhanced MRI,2–6 and measurements of infarct surface area and mass by cardiac MRI have been correlated with inducible ventricular tachycardia in patients with ischemic cardiomyopathy.7 The presence of myocardial scar has also been described with MRI in patients with nonischemic cardiomyopathy.8 The relation of scar distribution and risk of ventricular arrhythmia, however, has not been studied in patients with nonischemic cardiomyopathy.
Early studies using endocardial recordings suggested that propagation of an excitation wave front around nonconductive ventricular scar (reentry) is the mechanism for ventricular tachycardia.9 Later studies in patients with nonischemic cardiomyopathy revealed that although ventricular tachycardia in this subset of patients also results from reentry associated with scar, the scar is often adjacent to a valve annulus and deep in the myocardium, suggesting the presence of nontransmural scar as a common underlying substrate.10 Although the latter invasive study identified a mechanism for arrhythmia in nonischemic cardiomyopathy patients with clinically manifest ventricular tachycardia, a noninvasive methodology for assessing the substrate may improve prospective identification of patients at high risk for arrhythmia. In this report, we test the hypothesis that the distribution of ventricular scar identified by MRI is predictive of inducible ventricular tachycardia at electrophysiological study in patients with nonischemic cardiomyopathy.
Methods
Patients and Protocol
The protocol was reviewed and approved by the Johns Hopkins Institutional Review Board. All participants gave written informed consent. The patient population included 26 consecutive patients with left ventricular dysfunction (ejection fraction <50%) and lack of flow-limiting coronary artery disease on cardiac catheterization who were referred to the electrophysiology service for electrophysiological study or prophylactic implantable cardioverter-defibrillator (ICD) implantation. Twenty patients (77%) were referred for ICD implantation because of nonischemic cardiomyopathy and ejection fraction criteria.11 The remaining patients were referred for electrophysiological study in the setting of nonischemic cardiomyopathy and syncope (2 patients, 8%), palpitations (1 patient, 4%), family history of sudden cardiac death (1 patient, 4%), nonsustained wide complex tachycardia during exercise testing (1 patient, 4%), and assessment of candidacy for ICD implantation given borderline fulfillment of the Centers for Medicare and Medicaid Services criteria (1 patient, 4%). All patients underwent cardiac MRI, followed by electrophysiological study using standard technique (pacing through percutaneous electrophysiology catheters, 6 patients, 23%) or the ICD (pacing through the right ventricular implanted lead, 20 patients, 77%) with up to 3 extrastimuli. Noninvasive electrophysiological studies were performed immediately after ICD implantation. Patients with sustained monomorphic ventricular tachycardia at electrophysiological study were considered inducible.
MRI Studies
Images were acquired with a 1.5-T (Signa, General Electric Health-care Technologies) scanner and a 4-channel cardiac phased-array coil. After localization of the heart, base-to-apex short-axis cine steady-state free-precession gradient-echo images (repetition time, 3.7 to 4.0 ms; excitation time, 1.7 ms; image matrix, 256×192; field of view, 36 cm; slice thickness, 8 mm; spacing, 4 mm; flip angle, 40°) were obtained with prospective ECG gating. Patients then received 0.2 mmol/kg IV gadodiamide (Omniscan, Amersham Health). Fifteen minutes after the contrast bolus, delayed images were acquired with an inversion-recovery fast-gradient-echo pulse sequence (repetition time, 5.4 ms; excitation time, 1.3 ms; image matrix, 256×256; field of view, 36 cm; slice thickness, 8 mm; spacing, 2 mm; flip angle, 15°; inversion time, 175 to 250 ms). Inversion times were optimized for each patient to maximize conspicuity of delayed areas of myocardial enhancement. The number of image slices acquired depended on the length of the ventricular long axis in each patient. Single vertical and horizontal long-axis delayed enhancement images were also obtained through suspected areas of hyperenhancement to confirm the presence of enhancement in at least 2 planes.
Image Analysis
The CINETOOL (General Electric Healthcare Technologies) software package was used for image analysis. The left ventricular endocardium and epicardium were manually contoured at end diastole and end systole at each short-axis level to calculate left ventricular ejection fraction, end-diastolic volume, and mass. Candidate hyperenhanced regions were contoured, and the intensity of the hyperenhanced region was compared with that of a remote myocardial region without hyperenhancement. Candidate hyperenhanced areas were identified as scar if hyperenhancement was seen in >1 slice and the mean intensity of the hyperenhanced region was >6 SD above the mean intensity of the remote region. Region-of-interest analyses were reviewed and confirmed by 2 independent observers who were blinded to patient identities and electrophysiological study results; discrepancies were resolved by the senior observer with >10 years’ experience in cardiac MRI. The selected region of interest was used to calculate scar volume as a percentage of total myocardial volume.
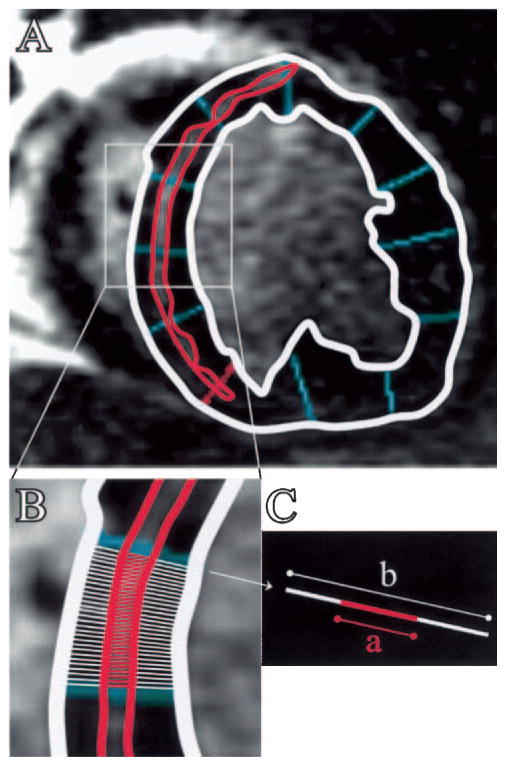
The myocardium was then divided into 12 sectors per slice, starting from the posterior right ventricular insertion point, using a method previously documented.5 To determine the transmural extent of hyperenhancement, 30 radial lines extending from the epicardium to the endocardium were drawn in each sector (Figure 1). The proportion of each line that intersected scar was computed. The transmural extent of scar in each sector was determined by calculating the average scar transmurality of all 30 lines per sector. The percentages of sectors containing 1% to 25%, 26% to 50%, 51% to 75%, and 76% to 100% average scar transmurality were calculated for each patient.
Figure 1.
Analysis of delayed enhancement images. A, The myocardial slice has been divided into 12 radial sectors per slice, and the left ventricular endocardium, epicardium (white contour), and midwall area of scar (red contour) have been contoured. B, Thirty radial lines drawn from the epicardium to the endocardium in 1 sector (inset). C, The proportion of each line that intersected scar was computed by dividing the length of segment a by b for each line. The transmural extent of scar in each sector was then determined by calculating the average scar transmurality of all 30 lines per sector.
Statistical Analysis
Continuous variables are summarized as median and interquartile range (the range between the 25th and 75th percentiles); discrete variables are summarized as absolute numbers and percentages. The Wilcoxon rank-sum and χ2 tests were used to compare medians and proportions of baseline characteristics and MRI parameters among inducible and noninducible groups of patients. The multivariable exact logistic regression model was used to adjust for the effect of left ventricular ejection fraction on scar distribution as a predictor for inducibility. Analyses were performed with SAS statistical software (version 9.1, SAS Institute Inc). All tests were 2 tailed, and values of P<0.05 were considered significant.
Results
Table 1 shows the baseline characteristics of patients before and after stratification by inducibility at electrophysiological study. Median age was 53 years; 46% of patients were female. There were no significant differences in baseline characteristics or β-blocker or amiodarone use (for atrial arrhythmia in all cases) among patient groups stratified by inducibility at electrophysiological study. Figure 2 shows examples of typical delayed enhancement images. The presence of scar was most common in the basal and septal myocardial regions. Scar location (basal versus apical, septal versus free wall) was not predictive of inducible ventricular tachycardia at electrophysiological study.
TABLE 1.
Baseline Characteristics of Subjects and Comparison After Stratification by Inducibility at Electrophysiological Study*
| Electrophysiological Study |
||||
|---|---|---|---|---|
| All Patients (n=26) | Inducible (n=5) | Noninducible (n=21) | P | |
| Age, y | 53 (44–61) | 56 (53–73) | 52 (42–58) | 0.09 |
| Female, n % | 12 (46) | 1 (20) | 11 (52) | 0.33 |
| Sodium, meq/L | 140 (138–141) | 140 (138–140) | 140 (138–141) | 0.92 |
| Creatinine, mg/dL | 1.0 (0.8–1.3) | 1.1 (0.9–1.3) | 1.0 (0.8–1.3) | 0.54 |
| QRS duration, ms | 115 (96–158) | 116 (104–128) | 113 (92–158) | 0.63 |
| β-Blockers, n (%) | 18 (69) | 3 (60) | 15 (71) | 0.63 |
| Amiodarone, n (%) | 4 (15) | 1 (20) | 3 (14) | 1.00 |
Data are expressed as median (interquartile range) or absolute numbers (column percentage).
Figure 2.
Typical contrast-enhanced images obtained by MRI. Scar involvement was most common in the basal myocardial slices. The myocardium has been divided into 12 sectors, starting from the posterior right ventricular insertion point (red line). A, Example of myocardium free of scar. B, Small region of hyperenhancement as an example of predominant scar distribution involving 1% to 25% of wall thickness. Sector numbering is clockwise, starting from the right ventricular insertion point, with sectors 3 to 5 having 4%, 20%, and 17% scar. C, An example of predominance of scar involving 26% to 75% of wall thickness. Sectors 1 to 8 have 50%, 56%, 53%, 61%, 62%, 71%, 40%, and 11% scar; sector 12 has 40% scar. C, The midwall area of hyperenhancement was visualized using a range of inversion times and in multiple planes. D, Example of scar involving 76% to 100% of wall thickness (sectors 11 and 12 with 85% and 78% scar).
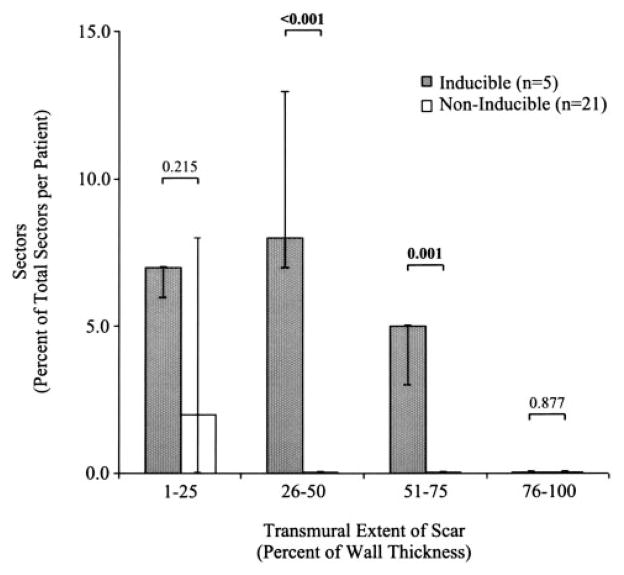
Six different morphologies of sustained monomorphic ventricular tachycardia were inducible in 5 patients (19%) with a median cycle length of 290 ms (interquartile range, 225 to 348 ms). The morphology of ventricular tachycardia was compatible with an exit site near the location of scar on delayed enhancement images in all cases (Figure 3). There was a trend to lower left ventricular ejection fraction and higher scar volume in patients with inducible ventricular tachycardia (Table 2). Scar transmurality distribution stratified by electrophysiological study results is depicted graphically in Figure 4. Patients with inducible ventricular tachycardia at electrophysiological study had significantly fewer sectors without hyperenhancement compared with noninducible patients. Predominance of scar involving 26% to 50% and 51% to 75% of wall thickness was the most significant predictor of inducible ventricular tachycardia at electrophysiological study.
Figure 3.
Example of the relation between scar location on delayed enhancement images and morphology of ventricular tachycardia on 12-lead ECG. A, A 4-chamber image of the heart, with the right atrium and ventricle at the top of the image and left atrium and ventricle at the bottom. B, The left bundle branch–like configuration in lead V1 of the ventricular tachycardia ECG suggests an exit site in the right ventricle or interventricular septum and is compatible with the scar location in A.
TABLE 2.
MRI Parameters and Comparison After Stratification by Inducibility at Electrophysiological Study*
| Electrophysiological Study |
||||
|---|---|---|---|---|
| All Patients (n=26) | Inducible (n=5) | Noninducible (n=21) | P | |
| Left ventricular ejection fraction, % | 27 (17–43) | 16 (13–29) | 29 (19–44) | 0.18 |
| Left ventricular end-diastolic volume, mL | 201 (129–273) | 159 (154–273) | 205 (129–259) | 0.72 |
| Left ventricular mass, g | 153 (113–192) | 184 (160–197) | 144 (113–189) | 0.38 |
| Patients with scar, n (%) | 17 (65) | 5 (100) | 12 (57) | 0.13 |
| Scar volume, % | 4.6 (0.8–7.2) | 6.0 (5.7–7.2) | 1.5 (0.7–6.3) | 0.09 |
| Predominant scar distribution involving 26%–75% of wall thickness, n (%) | 6 (23) | 5 (100) | 1 (5) | <0.001 |
Data are expressed as median (interquartile range) or absolute numbers (column percentage).
Figure 4.
Histogram illustrating median sector involvement in each level of hyperenhancement (scar) transmurality in patients stratified by inducibility at electrophysiological study. Bars represent median±interquartile range. Wilcoxon rank-sum comparisons are reported above the bars. Sectors without hyperenhancement are not shown. The median percent of sectors without hyperenhancement was 98% (interquartile range, 89 to 100) in the noninducible subgroup of patients vs 81% (interquartile range, 75 to 81) in patients with inducible ventricular tachycardia at electrophysiological study (P=0.011).
To adjust for the effect of left ventricular ejection fraction on scar distribution as a predictor for inducible ventricular tachycardia, we created the categorical variable “predominance of scar distribution involving 26% to 75% of wall thickness” (positive if ≥50% of sectors involving scar had average scar transmurality between 26% to 75% of wall thickness). In the exact logistic regression model adjusting for left ventricular ejection fraction, predominance of scar distribution involving 26% to 75% of wall thickness remained significantly associated with inducible ventricular tachycardia (odds ratio, 9.125; P=0.020).
Discussion
The principal finding of this study is that patients with nonischemic cardiomyopathy and predominance of scar distribution involving 26% to 75% of wall thickness are more likely to have inducible ventricular tachycardia. Our findings are consistent with recent reports of the correlation between risk of arrhythmia and the presence and morphology of scar in other patients groups such as those with ischemic cardiomyopathy7 and systemic right ventricles.12 The present study suggests that noninvasive assessment of scar distribution by MRI may predict electrophysiological study results in nonischemic cardiomyopathy.
Substrate for Ventricular Tachycardia in Nonischemic Cardiomyopathy
Catheter mapping studies of patients with nonischemic cardiomyopathy point to reentry around scar deep in the myocardium, near the ventricular base and in the perivalvular region, as the underlying mechanism for ventricular tachycardia.10,13 The present study is unique in assessing myocardial properties across the ventricular wall as a substrate for inducible ventricular tachycardia and expands on findings from endocardial mapping. The rare occurrence of scar involving 76% to 100% of wall thickness in patients with nonischemic cardiomyopathy likely led to the lack of any difference in scar distribution involving this degree of transmurality between patients stratified by inducibility at electrophysiological study. However, McCrohon et al8 reported that contrast-enhanced MRI can identify patchy or longitudinal striae of midwall enhancement in up to 28% of patients with nonischemic cardiomyopathy. The present study suggests that midwall myocardial enhancement involving >25% of wall thickness is the substrate for sustained ventricular tachycardia in nonischemic cardiomyopathy.
Clinical Implications
The absence of inducible ventricular tachycardia in nonischemic dilated cardiomyopathy has not been found to be a reliable negative predictor for subsequent arrhythmia.14 Therefore, the results of this study should not be used as a risk stratification methodology for nonischemic cardiomyopathy patients who meet current ejection fraction criteria for ICD implantation.11,15 Importantly, however, induction of sustained ventricular tachycardia in patients with nonischemic cardiomyopathy is associated with poorer prognosis14 and has strong prognostic value in subgroups of patients with nonischemic cardiomyopathy associated with intramyocardial scar.16–18 There is a high level of concern among treating and referring physicians about the risk of sudden death in patients with mild to moderate nonischemic cardiomyopathy who do not meet ICD implantation criteria by ejection fraction. Our study population included such patients, and the results remained statistically significant after adjustment for left ventricular ejection fraction. Thus, scar distribution may identify a subset of patients with mild to moderate left ventricular dysfunction and high risk of arrhythmia not currently identified for ICD implantation.
Study Limitations
It is possible that with a larger sample size, variables other than scar distribution such as left ventricular ejection fraction and scar volume may also become significant but less powerful predictors for inducibility. There is no consensus on the optimal threshold in intensity difference between areas of delayed enhancement and remote normal myocardium in nonischemic cardiomyopathy. A conservative threshold of 6 SD was used in this study to minimize the chance for identification of artifact as scar. Calculation of scar transmurality yields an average scar distribution for each sector and may misidentify the transmurality of a small scar as a result of averaging. However, review of the minimum and maximum transmurality scores for each sector and qualitative review of images did not identify any significant bias. Two modalities of electrophysiological testing were used to minimize invasive procedures in patients who met criteria for ICD implantation. However, noninvasive testing was done immediately after ICD implantation; ventricular capture by the drive train and extrastimuli was confirmed by 12-lead ECG in all cases; and all patients with inducible ventricular tachycardia were inducible through programmed stimulation from the right ventricular apex. Therefore, differences between the 2 testing modalities were likely unimportant. His-bundle electrograms were not available during noninvasive testing, and the possibility of bundle branch reentry as the mode of ventricular tachycardia induction cannot be ruled out. This possibility, however, is very unlikely because of distinct differences between ventricular tachycardia and sinus rhythm QRS morphology in all cases.19 Endocardial mapping has not yet been performed on any of our patients because none has required ventricular tachycardia ablation. Additional studies to assess the relationship between scar site and reentrant circuit location will refine these results.
Conclusions
Noninvasive assessment of scar distribution by MRI can identify the substrate for inducible ventricular tachycardia and may identify high-risk patients with mild to moderate nonischemic cardiomyopathy currently missed by ejection fraction criteria.
Acknowledgments
This study was funded through National Institutes of Health grants K24-HL04194 and RO1-HL64795 and by a grant from the Donald W. Reynolds Foundation.
Footnotes
Disclosure
Dr Halperin serves as a scientific advisor for Medtronic Inc. Dr Berger serves as a scientific advisor for Guidant Inc.
References
- 1.van der Burg AE, Bax JJ, Boersma E, Pauwels EK, van der Wall EE, Schalij MJ. Impact of viability, ischemia, scar tissue, and revascularization on outcome after aborted sudden death. Circulation. 2003;108:1954–1959. doi: 10.1161/01.CIR.0000091410.19963.9A. [DOI] [PubMed] [Google Scholar]
- 2.Tscholakoff D, Higgins CB, Sechtem U, McNamara MT. Occlusive and reperfused myocardial infarcts: effect of Gd-DTPA on ECG-gated MR imaging. Radiology. 1986;160:515–519. doi: 10.1148/radiology.160.2.3726135. [DOI] [PubMed] [Google Scholar]
- 3.de Roos A, van Rossum AC, van der Wall E, Postema S, Doornbos J, Matheijssen N, van Dijkman PR, Visser FC, van Voorthuisen AE. Reperfused and nonreperfused myocardial infarction: diagnostic potential of Gd-DTPA–enhanced MR imaging. Radiology. 1989;172:717–720. doi: 10.1148/radiology.172.3.2772179. [DOI] [PubMed] [Google Scholar]
- 4.Lima JA, Judd RM, Bazille A, Schulman SP, Atalar E, Zerhouni EA. Regional heterogeneity of human myocardial infarcts demonstrated by contrast-enhanced MRI. Potential mechanisms. Circulation. 1995;92:1117–1125. doi: 10.1161/01.cir.92.5.1117. [DOI] [PubMed] [Google Scholar]
- 5.Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 6.Vignaux O, Dhote R, Duboc D, Blanche P, Devaux JY, Weber S, Legmann P. Detection of myocardial involvement in patients with sarcoidosis applying T2-weighted, contrast-enhanced, and cine magnetic resonance imaging: initial results of a prospective study. J Comput Assist Tomogr. 2002;26:762–767. doi: 10.1097/00004728-200209000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Bello D, Fieno DS, Kim RJ, Pereles FS, Passman R, Song G, Kadish AH, Goldberger JJ. Infarct morphology identifies patients with substrate for sustained ventricular tachycardia. J Am Coll Cardiol. 2005;45:1104–1108. doi: 10.1016/j.jacc.2004.12.057. [DOI] [PubMed] [Google Scholar]
- 8.McCrohon JA, Moon JC, Prasad SK, McKenna WJ, Lorenz CH, Coats AJ, Pennell DJ. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation. 2003;108:54–59. doi: 10.1161/01.CIR.0000078641.19365.4C. [DOI] [PubMed] [Google Scholar]
- 9.Wellens HJ, Duren DR, Lie KI. Observations on mechanisms of ventricular tachycardia in man. Circulation. 1976;54:237–244. doi: 10.1161/01.cir.54.2.237. [DOI] [PubMed] [Google Scholar]
- 10.Soejima K, Stevenson WG, Sapp JL, Selwyn AP, Couper G, Epstein LM. Endocardial and epicardial radiofrequency ablation of ventricular tachycardia associated with dilated cardiomyopathy: the importance of low-voltage scars. J Am Coll Cardiol. 2004;43:1834–1842. doi: 10.1016/j.jacc.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 11.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 12.Babu-Narayan SV, Goktekin O, Moon JC, Broberg CS, Pantely GA, Pennell DJ, Gatzoulis MA, Kilner PJ. Late gadolinium enhancement cardiovascular magnetic resonance of the systemic right ventricle in adults with previous atrial redirection surgery for transposition of the great arteries. Circulation. 2005;111:2091–2098. doi: 10.1161/01.CIR.0000162463.61626.3B. [DOI] [PubMed] [Google Scholar]
- 13.Hsia HH, Callans DJ, Marchlinski FE. Characterization of endocardial electrophysiological substrate in patients with nonischemic cardiomyopathy and monomorphic ventricular tachycardia. Circulation. 2003;108:704–710. doi: 10.1161/01.CIR.0000083725.72693.EA. [DOI] [PubMed] [Google Scholar]
- 14.Brembilla-Perrot B, Donetti J, de la Chaise AT, Sadoul N, Aliot E, Juilliere Y. Diagnostic value of ventricular stimulation in patients with idiopathic dilated cardiomyopathy. Am Heart J. 1991;121(pt 1):1124–1131. doi: 10.1016/0002-8703(91)90672-5. [DOI] [PubMed] [Google Scholar]
- 15.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140–2150. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 16.Fananapazir L, Tracy CM, Leon MB, Winkler JB, Cannon RO, 3rd, Bonow RO, Maron BJ, Epstein SE. Electrophysiologic abnormalities in patients with hypertrophic cardiomyopathy: a consecutive analysis in 155 patients. Circulation. 1989;80:1259–1268. doi: 10.1161/01.cir.80.5.1259. [DOI] [PubMed] [Google Scholar]
- 17.Leite LR, Fenelon G, Simoes A, Jr, Silva GG, Friedman PA, de Paola AA. Clinical usefulness of electrophysiologic testing in patients with ventricular tachycardia and chronic chagasic cardiomyopathy treated with amiodarone or sotalol. J Cardiovasc Electrophysiol. 2003;14:567–573. doi: 10.1046/j.1540-8167.2003.02278.x. [DOI] [PubMed] [Google Scholar]
- 18.Winters SL, Cohen M, Greenberg S, Stein B, Curwin J, Pe E, Gomes JA. Sustained ventricular tachycardia associated with sarcoidosis: assessment of the underlying cardiac anatomy and the prospective utility of programmed ventricular stimulation, drug therapy and an implantable antitachycardia device. J Am Coll Cardiol. 1991;18:937–943. doi: 10.1016/0735-1097(91)90750-4. [DOI] [PubMed] [Google Scholar]
- 19.Lopera G, Stevenson WG, Soejima K, Maisel WH, Koplan B, Sapp JL, Satti SD, Epstein LM. Identification and ablation of three types of ventricular tachycardia involving the His-Purkinje system in patients with heart disease. J Cardiovasc Electrophysiol. 2004;15:52–58. doi: 10.1046/j.1540-8167.2004.03189.x. [DOI] [PubMed] [Google Scholar]