Abstract
Hyperglycemia is an indication of poor outcome for heart attack patients, even for nondiabetic patients with stress-induced hyperglycemia. Previous studies showed that inhibition of aldose reductase, the first and rate-limiting enzyme of the polyol pathway, attenuated contractile dysfunction in diabetic animals, but the mechanism is unclear. We therefore wanted to find out whether the polyol pathway also contributes to acute hyperglycemia-induced cardiac contractile dysfunction, and determine the mechanism involved. Rat hearts were isolated and retrogradely perfused with Krebs buffer containing either normal or high concentrations of glucose for 2 h. Short exposure to high-glucose medium led to contractile dysfunction as indicated by decreased −dP/dtmax, as well as elevation in left ventricular end-diastolic pressure. Cardiomyocytes incubated in high-glucose medium showed abnormal Ca2+ signaling, most likely because of decreased activity of sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA) inactivated by oxidative stress. Inhibition of aldose reductase or sorbitol dehydrogenase, the second enzyme in the polyol pathway, ameliorated contractile dysfunction, attenuated oxidative stress, and normalized Ca2+ signaling and SERCA activity caused by high glucose, indicating that the polyol pathway is the major contributor to acute hyperglycemia-induced oxidative stress leading to the inactivation of SERCA and contractile dysfunction.
Keywords: sarco(endo)plasmic reticulum Ca2+-ATPase, sorbitol dehydrogenase, aldose reductase
it is well recognized that diabetic cardiomyopathy, characterized by myocardial contractile dysfunction independent of coronary artery diseases (48), is a major cause of mortality and morbidity in diabetic patients. Not as well understood is the effect of acute hyperglycemia on hearts. Up to half of the nondiabetic patients with acute myocardial infarction were shown to have high blood glucose levels when admitted to the hospital (41), presumably a consequence of stress. This is associated with increased risk of in-hospital mortality (34).
Acute increase in glucose level in nondiabetic subjects causes biochemical and electrophysiological changes (37). It has been shown that hearts perfused in high-glucose medium (33.3 mmol/l) for 2 h have prolonged repolarization time (QT) interval and increased perfusion pressure, compared with those perfused with normal glucose medium (11.1 mmol/l) (7). Moreover, high glucose-perfused hearts showed increased apoptosis and increased superoxide and nitrotyrosine, indicating that oxidative stress is elevated within a short period of hyperglycemia (7). Acute increases in glucose level, rather than mean glucose level, are strongly correlated with oxidative stress in diabetic patients and animals (7, 39). It has been shown that acute glucose swings and not the mean daily glucose concentration are highly correlated with plasma nitrotyrosine and urinary F2 isoprostane 8-iso prostaglandin F2α, both well-established oxidative stress markers, indicating that sudden increases in glucose level contribute to oxidant formation. It was found that even in healthy subjects, oxidative stress is increased during a 2-h hyperglycemic clamp (36). These hyperglycemic swings are likely to have deleterious effects on the heart.
It has been shown that cardiomyocytes isolated from short-term diabetic animals (4–6 days of hyperglycemia) exhibited prolonged action potential, slower cytosolic Ca2+ clearance, and mechanical relaxations (45, 50), which were similar to the effects of a long-term diabetic model (21, 27, 33, 45). Furthermore, studies showed that culturing normal ventricular myocytes for 1 day or 6 h in high-glucose (25.5 mM) medium prolonged relengthening time compared with those cultured in normal glucose (5.5 mM) medium (24, 46, 47). These studies further support the previous finding which showed that elevating the extracellular glucose from 5.5 mM to 25 mM increased intracellular Ca2+ concentration nearly twofold in cardiomyocytes (16).
The polyol pathway has been shown to be a major contributor to hyperglycemia-induced oxidative stress in various tissues susceptible to diabetes-induced lesions (9). Under normal glycemic conditions, this metabolic pathway is not very active because aldose reductase (AR; EC 1.1.1.21), the first and rate-limiting enzyme of the pathway, has very high Km for glucose. However, during hyperglycemia, AR reduces glucose to sorbitol while its cofactor NADPH is oxidized to form NADP. Sorbitol is then converted to fructose by sorbitol dehydrogenase (SDH: EC 1.1.1.14) with the concomitant reduction of NAD+ to NADH (51). Decrease in the level of NADPH would lead to decreased level of reduced glutathione (GSH) because NADPH is also the cofactor for glutathione reductase that regenerates GSH from oxidized glutathione (GSSG) (28). On the other hand, increased levels of NADH, a substrate for NADH oxidase, would increase the level of superoxide. Thus, during hyperglycemia the polyol pathway activity leads to reduced antioxidation defense and increased levels of reactive oxygen species (ROS), resulting in elevated oxidative stress. Previous findings showed that the activity of AR was elevated in the diabetic mouse heart (20), and treatment with AR inhibitors improved the contractility of cardiac papillary muscle in diabetic rats (6), but the mechanism is not clear. Another study showed that inhibition of AR restored the level of Sir2 and reduced the level of phosphorylated IκB in the cardiac myocytes of diabetic mice (12), but the link between these two proteins and contractile function was not understood. Here we show that the polyol pathway contributes to the acute high glucose-induced cardiac contractile dysfunction by impairing the activity of sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA2), a key protein responsible for the removal of Ca2+ from the sarcoplasmic reticulum (SR).
MATERIALS AND METHODS
Experimental animals.
The animal experimental protocols employed in this study were approved by the Committee on the Use of Animals for Teaching and Research of the University of Hong Kong. These protocols also conform with the Guide for the Care and Use of Laboratory Animals, published by the National Institutes of Health (NIH Publication No. 85-23, revised 1996). Male Sprague-Dawley rats weighing 280 ± 30 g were provided by the Laboratory Animal Unit of the University of Hong Kong.
Isolated perfused heart preparation.
Hearts were isolated and perfused as described previously (55, 57). Rats were anesthetized with pentobarbital sodium (60 mg/kg ip) and given heparin (200 IU iv) before decapitation. Hearts were excised immediately and placed in ice-cold Krebs-Henseleit perfusion buffer before mounting on the Langendorff apparatus for perfusion. Isolated hearts were perfused retrogradely with Krebs-Henseleit buffer [in mmol/l: 118 NaCl (Sigma), 5 KCl, 1.2 MgSO4, 1.2 K2PO4, 1.25 CaCl2, 25 NaHCO3, and 11.1 glucose] equilibrated with 95% O2 + 5% CO2 at a constant pressure of 80 cmH2O and a temperature of 37°C. All rat hearts were paced at 300 beats/min with the use of pacing electrodes placed on the right atrium. Hearts exhibiting arrhythmias during stabilization were discarded. A latex balloon was inserted into the left ventricle, and the end-diastolic pressure (LVEDP) was adjusted to 4–8 mmHg. The cardiac parameters, such as heart rate and left ventricular developed pressure, were monitored continuously by a PowerLab/4SD system (AD Instruments, Castle Hill, Australia). After a 15-min stabilization period, hearts were perfused with 33.3 mmol/l glucose for 2 h, and we perfused 11.1 mM glucose plus 22.2 mM mannitol as osmotic control. We found no significant change in the osmotic control compared with hearts perfused with 11.1 mM glucose, indicating that the alteration of cardiac function found in the hyperglycemic group was not due to osmotic effect. The cardiac parameters were measured continuously, but only the parameters from 105 to 120 min of high-glucose perfusion were used for analysis. This concentration of glucose has been previously determined to induce ventricular instability, oxidative stress, and apoptosis in perfused hearts (7). To investigate the role of the polyol pathway, hearts were perfused with high glucose Krebs plus the AR inhibitor fidarestat (10 μmol/l) or the SDH inhibitor CP-470,711 (1 μmmol/l), niacin (10 μmmol/l), or GSH (0.3 mmol/l) as indicated in the text. The dosages of inhibitors and drugs used in the present study have been demonstrated to be effective in previous studies (7, 12, 18).
Measurement of intracellular calcium concentration transients in cardiomyocytes.
Ventricular myocytes were isolated from the rat hearts by the collagenase method described previously (59). After isolation, they were allowed to stabilize for 30 min before experiments. The yield of myocytes was determined microscopically using a hemocytometer. Preparations were considered satisfactory only if rod-shaped cells accounted for >80% of the counted cells at the beginning of each experiment. The isolated cardiomyocytes were divided into five different groups including normal concentration of glucose (11.1 mmol/l), high concentration of glucose (33.3 mmol/l), high glucose with fidarestat (10 μmol/l), high glucose with CP-470,711 (1 μmol/l), and high glucose with NAD+ (2 mmol/l) for 2 h incubation in Krebs medium containing 1.25 mM Ca2+ at 37°C. NAD+ was used instead of niacin because in cell culture studies it is preferred over niacin (5). All the inhibitors were added at the time when cells were transferred to high-glucose medium.
Intracellular calcium concentration ([Ca2+]i) transients were measured using a spectrofluorometric method with fura-2 AM as the Ca2+ indicator as described previously (32). Ventricular myocytes were incubated with 5 μmol/l fura-2 AM for 30 min. Fluorescent signals obtained at 340-nm and 380-nm excitation wavelengths were recorded and stored in computer for data processing and analysis. Myocytes were electrically stimulated at 0.2 Hz. The amplitude of electrically induced [Ca2+]i transient (E[Ca2+]i) was determined as the difference between the resting and the peak [Ca2+]i levels; the time for 50% decay of the transient (t50) was used to quantitate the decay of transients. [Ca2+]i transients were measured in cardiomyocytes after 2 h of incubation with high-glucose medium.
Isolation of SR vesicles and measurement of 45Ca2+ uptake.
SR vesicles were obtained by a method described previously with some modifications (53, 64), and the ATP-dependent transport of Ca2+ to SR was measured at room temperature (22°C) with a method described previously (26). Tissue homogenates were harvested for isolation of SR protein after 2 h of high-glucose perfusion. SR protein (50–100 μg) was then added to 1 ml of a medium containing 40 mmol/l imidazole-HCl (pH 7.0), 100 mmol/l KCl, 20 mmol/l NaCl, 5 mmol/l MgCl2, 4 mmol/l ATP-Na2, 1.3 μCi 45CaCl2, 5 μmol/l Ru-360, an inhibitor of Ca2+ uptake in mitochondria (63), and 5 μmol/l calmidazolium, an inhibitor of sarcolemmal Ca2+-ATPase (40). The concentration of free Ca2+ in this solution (5 μmol/l) was determined by a Ca2+-EGTA buffer and calculated according to Fabiato and Fabiato (14). To measure the oxalate-supported Ca2+ uptake, 5 mmol/l K-oxalate was added to the aforementioned solution. After 2–20 min, aliquots of 0.9 ml were filtered through Millipore filters (0.45 μm; Bedford, MA). Filters were washed three times with 4 ml of cold (2–4°C) solution containing 40 mmol/l imidazole-HCl (pH 7.0), 100 mmol/l KCl, and 0.1 mmol/l EGTA. After being washed, the Millipore filters were placed into vials containing 10 ml of scintillation cocktail (Universal LSC cocktail for aqueous samples, Sigma) and left for about 40 min. The radioactivity was then counted in scintillation counter (LS 6500, Beckman).
The temperature and conditions for Ca2+ uptake experiments were the same as that described previously (61). The 45Ca2+ uptake by SERCA was defined as the difference between the rate of 45Ca2+ uptake in the K-oxalate-containing solution in the presence and absence of 10 μmol/l cyclopiazonic acid, a specific inhibitor of SERCA (49). The difference between uptake in the presence and absence of 50 μmol/l ryanodine, a specific blocker of ryanodine receptor (RyR), was defined as the 45Ca2+ release via the RyR. The concentration of ryanodine used in this study was based on a previous report (26). Both 45Ca2+ uptake by SERCA and 45Ca2+ release via the RyR were measured in the isolated SR vesicles of hearts after 2 h exposure to high glucose.
Measurement of sorbitol and fructose content.
High-performance liquid chromatography (HPLC) was performed to determine the levels of sorbitol and fructose in rat hearts as previously described (51). Briefly, ∼300 mg of frozen samples were homogenized in 1 ml of ice-cold 5% trichloroacetic acid with 5.5 μl of 10 mmol/l xylitol added as an internal standard. Twenty-five microliters of sample were injected into HPLC MA-1 analytical column (Dionex) by AS-50 autosampler (Dionex), and the components in the sample were separated at a flow rate of 0.4 ml/min. The level of sorbitol and fructose content was determined by integrated amperometry, and the peaks were analyzed by Dionex Peaknet software. The amount of sorbitol and fructose was normalized to the wet weight of the tissue.
Biochemical assay for lactate and pyruvate.
To determine changes in the cytosolic redox state (i.e., NADH/NAD+), parallel experiments were performed with hearts freeze-clamped after 2 h of high-glucose perfusion. Lactate and pyruvate were extracted from the freeze-clamped tissue using perchloric acid and measured using standard biochemical assays as we published previously (51).
Determination of oxidative stress.
The oxidative stress was determined by the method described previously (38). Briefly, about 100 mg of the heart tissue was minced and then incubated in 1 ml of Krebs-Ringer solution (in mmol/l: 115 NaCl, 5.9 KCl, 1.2 MgCl2, 1.2 NaH2PO4, 1.2 Na2SO4, 2.5 CaCl2, 25 NaHCO3, and 10 glucose) containing 0.5 μmol/l lucigenin at pH 7.4. The chemiluminescence elicited by oxidative stress in the presence of lucigenin was measured in a luminometer (Berthold Lumat LB9507). The level of oxidative stress was reported as relative light units after background luminescence subtraction and normalized to milligram wet tissue weight. To validate that the chemiluminescence signals were derived from oxidative stress, the presence of 10 mmol/l Tiron, a superoxide scavenger, was added as a control.
Determination of GSH level.
Approximately 100 mg of the heart tissue was minced and then homogenized in 1 ml of 6% perchloric acid. The homogenate was centrifuged at 13,000 rpm for 10 min at 4°C. The supernatant was collected and added to the solution containing 85.7 μl of 70% perchloric acid, 14.3 μl of double-distilled H2O, and 107 μl of 5 mol/l K2CO3, and then centrifuged at 4,000 rpm for 5 min under 4°C. After centrifugation, 100 μl of supernatant was added to 890 μl of Tris-EDTA (pH 8.1) and 10 μl of O-pathaldialdehyde and the reaction mixture was kept on ice for 15 min. After that, the absorbance of the mixture was measured with a fluorescence spectrometer (425 nm; excitation at 345 nm). The concentration of GSH in the tissue was calculated from the GSH standard curve.
Immunohistochemistry.
Paraffin sections of the hearts were deparaffinized in xylene and rehydrated with a graded series of ethanol. After washing, sections were blocked with 0.3% hydrogen peroxide for 15 min. The sections were then blocked with 1.5% normal goat serum for 1 h (Vector Laboratories). Sections were then incubated with rabbit anti-nitrotyrosine (1:200; Santa Cruz Biotechnology) overnight at 4°C. Immunoreactivity was detected with biotinylated goat anti-rabbit secondary antibodies and the avidin-biotin-peroxidase complex (Vector Laboratories). Immunoreactive signal was developed using diaminobenzidine as a substrate (Zymed Laboratories) for 2 min. Photomicrographs were taken with an Olympus IX71 microscope system. All histological and immunohistochemical samples were coded and examined and graded in a blinded fashion.
Immunohistochemical staining of ROS modification of SERCA was performed using antibodies against SERCAC674-SO3H (62). Briefly, nonspecific binding was blocked with 10% normal goat serum in phosphate-buffered saline (pH 7.4) for 30 min before incubation with individual primary antibodies. Anti-SERCA C674-SO3H antibody was used at 2 μg/ml. The secondary antibody, a biotinylated anti-rabbit IgG secondary antibody, was used at 1:200. Vector Red alkaline phosphatase substrate (Vector) was used to visualize positive immunoreactivity. The quantitative analysis was performed by ImageJ software [Wayne Rasband, National Institutes of Health (NIH), Bethesda, MD].
Immunoblotting assay.
The expression of SERCA and RyR was detected in the isolated SR vesicles as described previously (32). Sample proteins (60 μg/lane) were separated in SDS-polyacrylamide gel (10% for SERCA; 6% for RyR) and transferred electrophoretically. After blocking, the membranes were incubated overnight at 4°C with the goat anti-SERCA2 polyclonal antibody (1:400, Santa Cruz Biotechnology) and mouse anti-RyR2 monoclonal antibody (1:3,330, Affinity BioReagents). The second antibody was either anti-goat or anti-mouse antibody conjugated to horseradish peroxidase (1:2,000, Dako Cytomation) for 1 h at room temperature. The protein bands of SERCA and RyR were detected by the chemiluminescence method (ECL Western blot analysis detection; Amersham Biosciences). The band intensity was analyzed by NIH-developed ImageJ software.
Immunoprecipitation with anti-SERCA2 antibody.
The immunoprecipitation was performed as described previously (1). Briefly, 1 mg protein extract was diluted in 500 μl of lysis buffer. After preclearing with protein G agarose, the supernatant was mixed with 10 μl of anti-SERCA2 and then incubated at 4°C for 4 h. Prewashed protein G (50 μl) was added to the samples and further incubated for 1 h. For detecting the tyrosine nitration of SERCA, the immunocomplex was resuspended in Laemmli buffer containing mercaptoethanol. For detecting the S-glutathiolation of SERCA, the immunocomplex was resuspended in nonreducing loading buffer containing 5 mM N-ethylmaleimide. The samples were separated by SDS-PAGE and transferred electrophoretically as described above. After blocking, the membrane was incubated overnight at 4°C with either anti-nitrotyrosine (1:1,000, Santa Cruz Biotechnology), anti-glutathione (1:1,000, ViroGen), or anti-SERCA (1:400, Santa Cruz Biotechnology) in blocking solution. The second antibody was either anti-rabbit or anti-mouse antibody conjugated to horseradish peroxidase for 1 h at room temperature, followed by detection using the chemiluminescence method. The band intensity was analyzed by NIH-developed ImageJ software.
Drugs and chemicals.
Collagenese (type 1), 2-deoxy-d-glucose, NaN3, sodium dithionite, fura-2 AM, 2,3,5-triphenyltetrazolium chloride, EGTA, leupeptin, and PMSF were purchased from Sigma-Aldrich (St. Louis, MO). Ru-360, calmidazolium, cyclopiazonic acid, and ryanodine were purchased from Calbiochem. 45CaCl2 was purchased from Amersham. Fidarestat and CP-470,711 were gifts from Sanwa Kagaku Kenkyusho and Pfizer Global Research and Development.
Statistical analysis.
Data analysis was performed with a statistical software package (Prism version 5.0; GraphPad Software, San Diego, CA). All data are expressed as means ± SD. Groups comparison were analyzed by one-way analysis of variance and t-test. A difference of P < 0.05 was considered significant.
RESULTS
Polyol pathway activities in acute hyperglycemic hearts.
There is a controversy on the type of perfusate used to study the effect of high glucose in isolated hearts. Since hearts utilize both glucose and fatty acid as sources of fuel, some studies used glucose plus palmitate (15, 58) and some used glucose alone (7, 31, 55). We therefore compared both types of perfusion media in our study. We found that in both types of media, high glucose affected contractile function in a similar manner and that the effects of the AR and SDH inhibitors, GSH, and niacin in hearts perfused with either one of these media were similar (Table 1). Since other reports studying the effect of polyol pathway on isolated rat hearts utilized only glucose in the perfusate (22, 23), we decided to use the same medium to facilitate comparison of results.
Table 1.
Effect of high glucose on ±dP/dtmax, LVSP, and LVEDP in rat hearts perfused with Krebs-Henseleit buffer containing either glucose alone or glucose plus palmitate
| Control | HG | Mannitol | HG + ARI | HG + SDI | HG + GSH | HG + Niacin | HG + Tiron | |
|---|---|---|---|---|---|---|---|---|
| Krebs–Henseleit buffer containing 11.1 mM glucose alone | ||||||||
| n | 9 | 9 | 6 | 8 | 8 | 8 | 8 | 6 |
| +dp/dtmax, mmHg/s | 1,764.3 ± 172.4 | 1,706.7 ± 56.0 | 1,714.4 ± 40.8 | 1,741.4 ± 159.5 | 1,878.5 ± 95.0 | 1,749.4 ± 66.1 | 1,813.7 ± 110.5 | 1,763.2 ± 75.3 |
| −dP/dtmax, mmHg/s | 1,264.3 ± 172.4* | 1,081.9 ± 91.0 | 1,297.9 ± 134.1* | 1,267.3 ± 130.7* | 1,385.3 ± 162.7† | 1,254.7 ± 100.2* | 1,330.6 ± 133.3† | 1,288.7 ± 67.2* |
| LVSP, mmHg | 77.5 ± 12.3 | 77.1 ± 8.8 | 78.6 ± 9.2 | 73.6 ± 18.3 | 82.1 ± 8.3 | 75.3 ± 7.3 | 75.5 ± 18.3 | 77.3 ± 6.1 |
| LVEDP, mmHg | 10.3 ± 0.9† | 13.9 ± 3.0 | 10.5 ± 1.7† | 9.6 ± 1.5† | 9.9 ± 1.6† | 9.0 ± 2.6† | 9.1 ± 1.1† | 9.2 ± 1.9† |
| Krebs-Henseleit buffer containing 11.1 mM glucose plus 0.4 mM palmitate | ||||||||
| n | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| +dp/dtmax , mmHg/s | 2,442.5 ± 38.8 | 2,400.2 ± 15.3 | 2,394.6 ± 7.9 | 2,458.0 ± 28.4 | 2,570.5 ± 84.1 | 2,418.6 ± 43.2 | 2,476.6 ± 88.5 | 2,437.6 ± 56.1 |
| −dP/dtmax, mmHg/s | 1,611.3 ± 45.6 | 1,382.2 ± 34.3 | 1,653.6 ± 47.6 | 1,631.7 ± 22.3 | 1,744.4 ± 79.8 | 1,681.1 ± 70.6 | 1710.4 ± 27.4 | 1,650.5 ± 23.17 |
| LVSP, mmHg | 107.3 ± 3.8 | 112.5 ± 11.9 | 109.5 ± 4.9 | 103.1 ± 5.5 | 100.4 ± 14.7 | 105.8 ± 5.9 | 98.4 ± 4.9 | 103.1 ± 8.2 |
| LVEDP, mmHg | 7.6 ± 0.9 | 11.6 ± 0.6 | 7.7 ± 1.0 | 7.8 ± 0.2 | 8.0 ± 0.1 | 7.0 ± 0.3 | 6.9 ± 0.6 | 7.1 ± 0.7 |
Values are means ± SD. Control, no other addition; mannitol, 22.2 mM mannitol; high-glucose medium (HG), 33.3 mM glucose; HG + ARI, HG plus aldose reductase inhibitor; HG + SDI, HG plus sorbitol dehydrogenase inhibitor; HG + GSH, HG plus glutathione; HG + Niacin, HG plus niacin; HG + Tiron, HG plus Tiron. ±dP/dtmax, maximal first derivative of left ventricular (LV) pressure; LVSP, LV systolic pressure; LVEDP, LV end-diastolic pressure.
P < 0.05,
P < 0.01 vs. HG group.
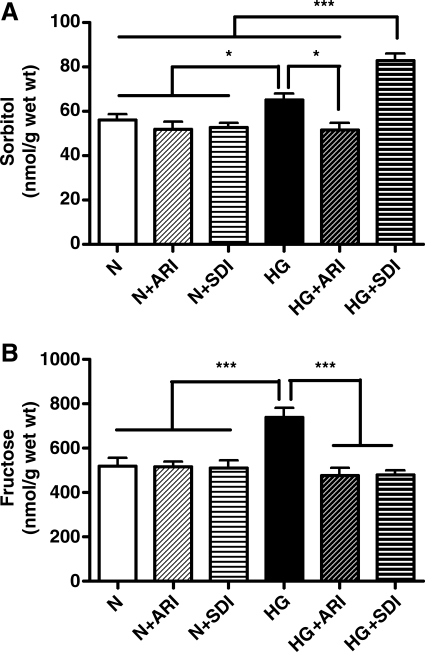
To assess the polyol pathway activities in the rat hearts, the levels of sorbitol and fructose, enzymatic products of AR and SDH, respectively, were determined in hearts perfused in normal or high-glucose medium (Fig. 1). As expected, there was a significant increase in sorbitol and fructose levels in hearts perfused in high-glucose medium. Treatment with AR inhibitor (ARI) or SDH inhibitor (SDI) did not change the levels of sorbitol or fructose in hearts perfused with normal glucose medium, probably because of the modest amount of glucose channeled through the polyol pathway. In hearts perfused with high-glucose medium, ARI reduced sorbitol to basal level while treatment with SDI increased the level of sorbitol and decreased the level of fructose. These results indicate that the polyol pathway is active during hyperglycemia and that ARI and SDI were effective in inhibiting their target enzymes.
Fig. 1.
Changes in levels of sorbitol (A) and fructose (B) in hearts perfused with normal [N; control (Ctrl)] or high glucose (HG) medium. ARI, aldose reductase inhibitor; SDI, sorbitol dehydrogenase (SDH) inhibitor. Data are means ± SD (n = 6). *P < 0.05, ***P < 0.001, vs. corresponding groups.
Inhibition of polyol pathway attenuated contractile dysfunction in high glucose-perfused rat hearts.
As shown in Table 1, hearts perfused with high-glucose medium exhibited significant decrease in −dP/dtmax and marked elevation in LVEDP compared with those in control and mannitol-treated groups, suggesting that high glucose stiffened the myocardium in diastolic state, and the effect was not contributed to by osmotic stress. To determine the role of polyol pathway in high glucose-induced contractile dysfunction, we used AR inhibitor (zopolrestat) and SDH inhibitor (CP-470,711) to block the activity of AR and SDH, respectively. These two inhibitors have been extensively studied in previous reports (17, 19, 30, 44, 52), with no unintended effect on myocardial function. This was also confirmed in our present study (data not shown). Inhibition of AR with 10 μM fidarestat significantly attenuated the high glucose-induced reduction in −dP/dtmax and elevation in LVEDP. A similar effect was also observed in hearts treated with 1 μM SDH inhibitor CP-470,711. These results indicated that the polyol pathway contributed to high glucose-induced diastolic dysfunction. Treatment with niacin, a precursor for NAD+, also normalized −dP/dtmax and LVEDP, suggesting that high glucose-induced increased LVEDP was due to depletion of NAD+ as a consequence of increased SDH activity. Treatment with either GSH, or Tiron, a superoxide scavenger, also normalized −dP/dtmax and LVEDP, indicating that the changes in −dP/dtmax and LVEDP were contributed to by high glucose-induced oxidative stress.
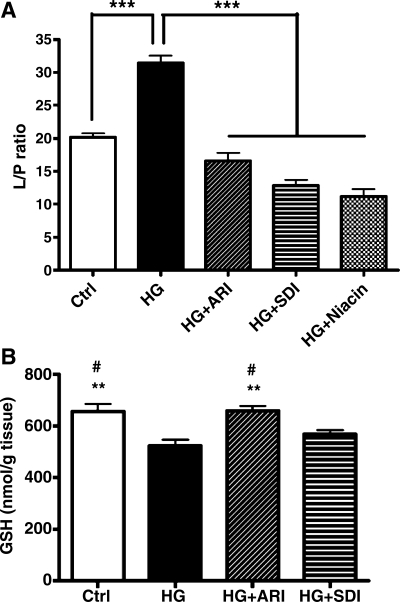
Inhibition of polyol pathway attenuated lactate/pyruvate ratio and GSH level in high glucose-perfused hearts.
The effect of hyperglycemia on the redox state and superoxide production in left ventricular myocardium was examined. Cytosolic lactate/pyruvate ratio was used as surrogate assay for NADH/NAD+ ratio, a redox indicator (44). We found that lactate/pyruvate ratio was increased in high glucose-perfused hearts (Fig. 2A), and attenuated by treatment with AR or SDH inhibitors, suggesting that activation of polyol pathway under hyperglycemia elevated NADH/NAD+ ratio. As expected, treatment with niacin, that replenishes NAD+, lowered the lactate/pyruvate ratio (Fig. 2A). The level of GSH, the major cellular antioxidant, was reduced in high glucose-perfused myocardium (Fig. 2B), and normalized in the presence of ARI. However, SDI had little effect on hyperglycemia-induced decrease in GSH level.
Fig. 2.
A: lactate-to-pyruvate (L/P) ratio indicating NADH-to-NAD+ ratio in hearts perfused with normal (Ctrl), HG medium, HG + ARI, HG + SDI, and HG + niacin. Data are means ± SD (n = 13). ***P < 0.001 vs. Ctrl group. B: effect of acute hyperglycemia on GSH level in normal, ARI-treated, and SDI-treated perfused rat hearts. Data are means ± SD (n = 9). **P < 0.01 vs. HG group; #P < 0.05 vs. SDI group.
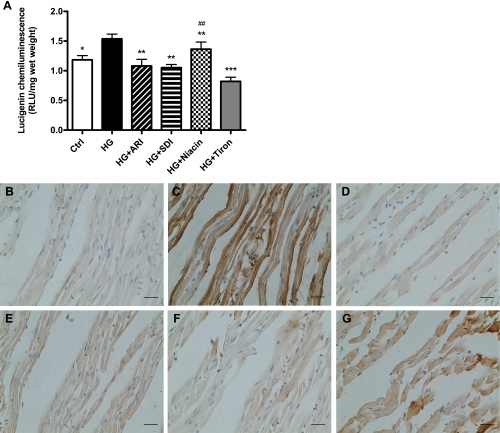
Inhibition of polyol pathway reduced the level of superoxide and peroxynitrite in high glucose-perfused hearts.
Several studies showed that acute hyperglycemia induces oxidative stress in healthy subjects (36), and large increases in superoxide were observed in hearts perfused with high glucose (7). We found that intracellular superoxide content was increased by 32% in high glucose-perfused myocardium (Fig. 3A), and inhibition of AR or SDH attenuated such increase, suggesting that polyol pathway is a major contributor to hyperglycemia-induced elevation of cardiac superoxide production (Fig. 3A). To determine whether increased NADH/NAD+ ratio contributed to oxidative stress, niacin was added to replenish NAD+, but it had no effect on the superoxide level.
Fig. 3.
A: left ventricular superoxide content in hearts perfused with normal (Ctrl), HG medium, HG + ARI, HG + SDI, HG + niacin, and HG + Tiron. RLU, relative light units. Data are means ± SD (n = 5). *P < 0.05, **P < 0.01, ***P < 0.001 vs. Ctrl group; ##P < 0.01 vs. HG + Tiron group. The level of nitrotyrosine was assessed by the immunostaining in left ventricles from isolated perfused rat hearts (n = 4). Representative staining (n = 6) was taken from normal (B), high glucose (C), mannitol (D), ARI-treated (E), SDI-treated (F), and niacin-treated (G) groups. Scale bar, 50 μm.
Formation of nitrotyrosine, reflecting the level of peroxynitrite, is an important oxidative stress marker. Immunohistochemical staining of the heart slices showed that the nitrotyrosine level was much higher in the high glucose-perfused hearts than that of the control group, indicating that acute hyperglycemia led to large increases in peroxynitrite. Inhibition of AR or SDH effectively reduced the level of nitrotyrosine (Fig. 3), demonstrating that the polyol pathway contributed to the increased level of peroxynitrite. This observation further confirmed that the polyol pathway is an important contributor to oxidative stress in the acute hyperglycemic heart. Treatment with niacin did not significantly reduce the level of nitrotyrosine.
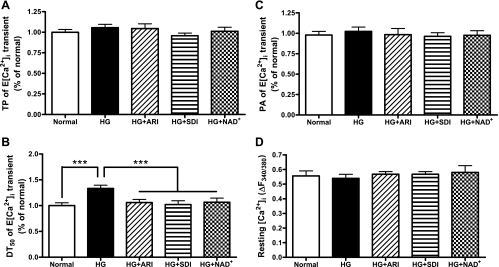
Inhibition of polyol pathway ameliorated high glucose-induced impairment of Ca2+ signaling in cardiomyocytes.
To further understand the role of the polyol pathway in hyperglycemia-induced contractile dysfunction, we investigated the effect of inhibition of AR and SDH activities on electrically stimulated Ca2+ signaling (E[Ca2+]i) in cardiomyocytes. No significant difference was found in the peak amplitude and resting [Ca2+]i level after 2 h incubation in high-glucose medium. Time to peak of E[Ca2+]i (TP) represents the rate of Ca2+ release from the SR, mainly via RyR. Cardiomyocytes, after incubation in high-glucose medium for 2 h, showed no change in TP, suggesting that the activity of RyR was not affected by short exposure to high glucose (Fig. 4A).
Fig. 4.
Effect of acute hyperglycemia on time to peak (TP; A), decay time (DT; B), peak amplitude (PA; C), and resting level (D) of electrically induced [Ca2+]i (E[Ca2+]i) transients of normal, ARI-treated, SDI-treated, and NAD+-treated cardiomyocytes. Data are means ± SD (n = 6 cells from 5 rats in each group). ***P < 0.001 vs. HG group.
The decay of E[Ca2+]i is mainly determined by Ca2+ uptake to SR via SERCA, which is responsible for the removal of ∼90% of Ca2+ from the cytoplasm (4). We therefore measured the time to reduce 50% of the peak E[Ca2+]i (t50) as an indicator of SERCA activity. In control cells after 2 h incubation in high-glucose medium, t50 was increased to 130%. Inhibition of AR or SDH significantly attenuated the prolongation of t50. Treatment with NAD+ also reduced t50 to a similar extent (Fig. 4B).
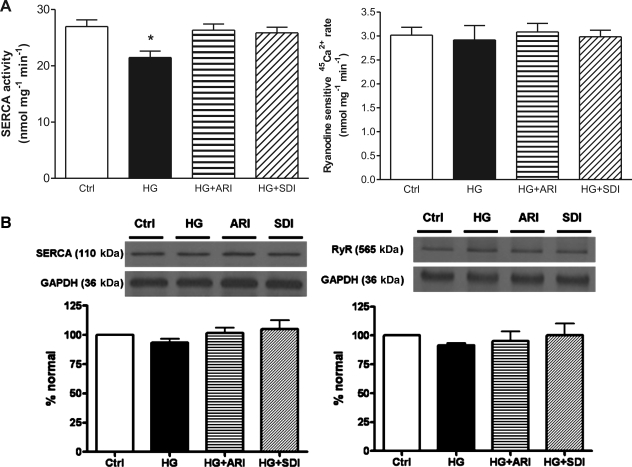
Inhibition of polyol pathway restored the activity of SERCA in high glucose-perfused hearts.
To better understand how the polyol pathway contributes to high glucose-induced contractile abnormalities, we measured 45Ca2+ uptake in SR vesicles isolated from hearts perfused in high-glucose medium for 2 h. We found that 45Ca2+ uptake via SERCA in SR vesicles from high glucose-treated hearts was decreased from 27 nmol·mg−1·min−1 to 20 nmol·mg−1·min−1, even though the level of SERCA protein was not changed. Inhibition of AR or SDH restored Ca2+ uptake to the level of the control (Fig. 5, A and B).
Fig. 5.
A: effect of acute hyperglycemia on the activities of ryanodine (RyR) and sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA) in normal, ARI-treated, and SDI-treated perfused rat hearts. Data are means ± SD (n = 4 vesicles from 5 rats in each group). *P < 0.05 vs. HG group. B: effect of acute hyperglycemia on the protein expression of RyR and SERCA in normal, ARI-treated, and SDI-treated perfused rat hearts. Data are means ± SD (n = 4 vesicles from 5 rats in each group).
Interestingly, ryanodine-sensitive 45Ca2+ release rate, an indication of SR Ca2+ release through the RyR, remained unchanged after 2 h of high-glucose perfusion. Consequently, inhibition of AR or SDH had no effect on ryanodine-sensitive 45Ca2+ release rate (Fig. 5A). Similar to SERCA, the protein level of RyR protein was not altered in high glucose-perfused hearts (Fig. 5B).
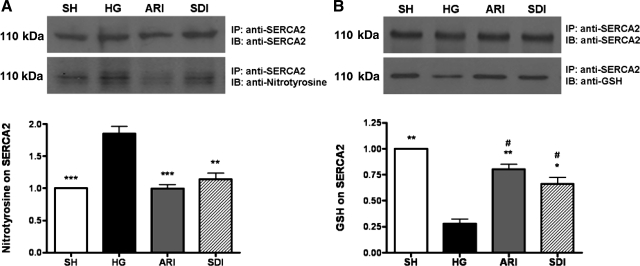
Inhibition of polyol pathway attenuated the tyrosine nitration of SERCA2 and maintained the S-glutathiolation of SERCA2 in high glucose-perfused rat hearts.
Previous studies have shown that SERCA2 is sensitive to oxidative stress, and its activity is inhibited by both ONOO− and nitrotyrosine formation (1, 2, 25, 56). To determine whether SERCA2 had increased nitrotyrosine, SERCA2 protein was immunoprecipitated from heart extracts using anti-SERCA2 antibody and the level of nitrated SERCA2 was assessed by Western blot using anti-nitrotyrosine antibody (Fig. 6A). The level of nitrotyrosine on SERCA2 was significantly increased in high glucose-perfused hearts, and inhibition of either AR or SDH attenuated tyrosine nitration of SERCA2, suggesting that blockade of the polyol pathway restored the activity of SERCA2 by attenuating tyrosine nitration of the protein.
Fig. 6.
A: effect of acute hyperglycemia on the level of tyrosine nitration on SERCA in sham-operated (SH), ARI-treated, and SDI-treated hearts isolated from rats. For detection of nitrotyrosine in SERCA protein, an immunoprecipitate (IP) was obtained using anti-SERCA2 antibody and then immunoblotted (IB) with anti-SERCA2 antibody or anti-nitrotyrosine antibody. Data are means ± SD (n = 3). ***P < 0.001, **P < 0.01 vs. HG group. B: effect of acute hyperglycemia on the level of GSH on SERCA in SH, ARI-treated, and SDI-treated hearts isolated from rats. An IP was obtained using anti-SERCA2 antibody and then immunoblotted with anti-GSH antibody. Data are means ± SD (n = 3). *P < 0.05, **P < 0.01 vs. HG group; #P < 0.01 vs. SH group.
Besides tyrosine nitration of SERCA, S-glutathiolation of SERCA also affects its activity (2). As shown in Fig. 6B, the amount of GSH on the immunoprecipitated SERCA was significantly decreased in high glucose-perfused hearts, indicating that the level of GSS-SERCA was lowered in hearts subjected to acute hyperglycemia. Inhibition of either AR or SDH restored the level of S-glutathiolation, suggesting that restoration of SERCA activity in high glucose-perfused hearts was due to normalizing of S-glutathiolation of the protein.
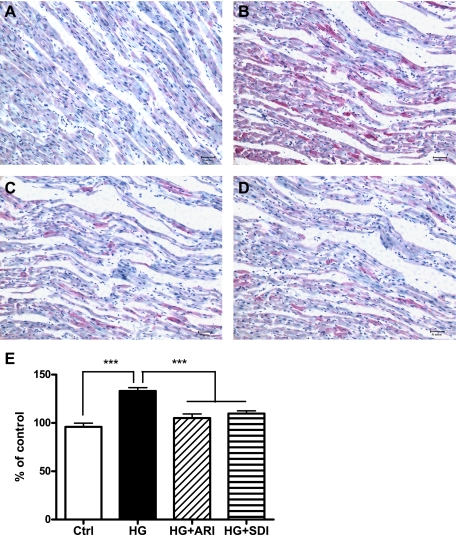
Inhibition of polyol pathway attenuated the oxidation of SERCA-cysteine-674 in high glucose-perfused rat hearts.
Previous studies showed that a high level of peroxynitrite irreversibly oxidized cysteine-674 of SERCA to the sulfonic acid form, contributing to its inactivation (54, 62). Using antibodies specific for SERCAC674-SO3H, we examined the role of the polyol pathway in high glucose-induced oxidative inactivation of SERCA. Compared with control, high glucose-perfused hearts showed a large increase in the staining of SERCAC674-SO3H, and the staining was substantially reduced in tissues treated with ARI or SDI (Fig. 7), indicating that the polyol pathway is a major contributor to oxidative inactivation of SERCA under acute hyperglycemia.
Fig. 7.
Effect of acute hyperglycemia on the level of SERCAC674-SO3H, inactivated SERCA in normal, ARI-treated, and SDI-treated hearts isolated from rats (n = 3). Representative immunohistochemical staining was taken from normal (A), high glucose (B), ARI-treated (C), and SDI-treated (D) groups. Scale bar, 50 μm. E: quantitative analysis of SERCAC674-SO3H staining in normal, ARI-treated, and SDI-treated hearts isolated from rats (n = 3). Data are means ± SD (n = 3). ***P < 0.001 vs. HG group.
DISCUSSION
Rat hearts perfused with high-glucose medium for 2 h exhibited marked decrease in −dP/dtmax as well as elevated LVEDP. Such contractile abnormalities were significantly attenuated by the inhibition of AR or SDH, indicating that the polyol pathway is an important contributor to hyperglycemia-induced diastolic dysfunction. The impairment of contractile function suggested that cardiac Ca2+ homeostasis was altered by short exposure to high glucose. High glucose-induced oxidative stress is likely to be the cause of the altered Ca2+ signaling profile and diastolic dysfunction. As mentioned in the Introduction, the polyol pathway plays a key role in hyperglycemia-induced oxidative stress by contributing to the depletion of GSH and increased production of ROS. This is confirmed here by the observation that ARI restored the level of GSH and reduced the level of ROS, and SDI also attenuated the level of ROS in high glucose-perfused hearts.
To better understand the mechanism, intracellular Ca2+ transients in cardiomyocytes were analyzed. Rat cardiomyocytes incubated in high-glucose medium for 2 h showed significant increase in the decay time of Ca2+ transient, but no change was found in base to peak time, indicating that the rate of Ca2+ reuptake was reduced while the rate of Ca2+ release was normal. Treatment with ARI or SDI significantly attenuated the prolongation of the decay time of Ca2+ transient, suggesting that the polyol pathway contributed to the hyperglycemia-induced impairment of Ca2+ reuptake by SR, leading to diastolic dysfunction.
Since Ca2+ uptake into SR via SERCA is responsible for the removal of ∼90% of Ca2+ from the cytoplasm (4), impairment of SERCA is the most likely cause of contractile dysfunction in hyperglycemic hearts. Indeed, we showed that SERCA activity from hearts with a brief 2-h exposure to high-glucose medium was significantly reduced. Consistent with the finding that the rate of Ca2+ release from SR was not altered in hearts perfused with high-glucose medium, we found that RyR activity was not changed. Previous studies showed that NADH suppresses RyR activity via NADH oxidase tightly linked to RyR in SR (8). Therefore one would expect that, during hyperglycemia, increased NADH due to increased polyol pathway activities would decrease RyR activity. On the other hand, RyR activity has been shown to be inhibited by high GSH/GSSH ratio, which keeps the hyperactive cysteine moieties of RyR in the reduced state (42). During hyperglycemia, polyol pathway activities decrease GSH level and should therefore increase RyR activity. It is likely that increased NADH and decreased GSH from polyol pathway activities counteract each other's effect on RyR activity, leading to no change in RyR activity as we observed in the heart experiencing acute hyperglycemia.
Polyol pathway most likely impaired SERCA activity during acute hyperglycemia by increasing oxidative stress. We showed that the GSH level was reduced and the superoxide level elevated in hyperglycemic hearts, and these changes were significantly attenuated by the administration of ARI and SDI. GSH is required for glutathione peroxidase to remove ROS. Thus low level of GSH would lead to increased level of ROS. Furthermore, one of the major sources of ROS in cardiomyocytes is superoxide produced by the membrane-associated NADH oxidase, an enzyme controlled by cytosolic NADH/NAD+ ratio and oxygen pressure (38). In acute hyperglycemic hearts, the activation of the polyol pathway increases NADH/NAD+ ratio as the consequence of oxidation of sorbitol to fructose by SDH. The increased NADH stimulates NADH oxidase, which is in close proximity to SR, to generate ROS (3, 38). Increased ROS inhibits SERCA by oxidizing the cysteine thiols, interfering with the ATP-binding site, making it unable to hydrolyze the ATP (60). This is supported by the observation that addition of NAD+ attenuated high glucose-induced contractile dysfunction and Ca2+ signaling. Previous studies showed that oxidative stress reduces SERCA activity by nitration of tyrosine (25, 56) and oxidative modification of cysteine-674 leading to reduced level of GSS-SERCA, the activated form of SERCA (1, 2). We found that indeed high-glucose perfusion led to increased nitration of SERCA and increased level of SERCAC674-SO3H, suggesting that reduction of SERCA activity was due to high glucose-induced oxidative stress. Addition of either ARI or SDI to the high-glucose perfusate reduced the levels of nitrated SERCA and SERCAC674-SO3H and normalized SERCA activity, indicating that the polyol pathway is the major contributor to high glucose-induced oxidative stress, and the cause of high glucose-induced inactivation of SERCA. Phospholamban is an important regulator of SERCA activity. However, previous studies showed that, in cardiomyocytes incubated in high-glucose medium, slower rates of Ca2+ transient decay was associated with decreased SERCA activity (11), but not associated with any change in the level of phospholamban expression or phosphorylation (13).
Previous studies using an electrocardiogram showed that, in healthy human and rat models, acute hyperglycemia leads to QTc prolongation, which is probably contributed to by the increased intracellular calcium (10, 35). Moreover, abnormal calcium homeostasis is common in diabetic patients (29). Therefore, it was suggested that hyperglycemia increases production of oxygen free radicals that inhibit Ca2+-ATPase activity (36). This increases cytosolic free calcium, leading to prolongation of myocardial repolarization time, or QT prolongation. However, in these studies, the mechanism of hyperglycemia-mediated free radical generation is not clear. Here we show that the polyol pathway is the major contributor to hyperglycemia-induced oxidative stress and that SERCA activity is impaired by oxidative stress, leading to contractile dysfunction.
Previous studies showed that inhibition of AR normalized Na+ and Ca2+ levels in ischemic-reperfused hearts by normalizing Na+-K+-ATPase activity (43). It was postulated that during ischemic-reperfusion, polyol pathway activity increases NADH/NAD+ ratio, leading to the activation of protein kinase C and inhibition of Na+-K+-ATPase activity. Since NADH/NAD+ ratio is also increased in high glucose-treated hearts because of polyol pathway activity, activation of protein kinase C and reduction of Na+-K+-ATPase activity might also be a potential contributory factor for the abnormal Ca2+ signaling in the acute hyperglycemia hearts.
In conclusion, we demonstrated that polyol pathway activity contributed to the hyperglycemia-induced contractile dysfunction by increasing oxidative stress, leading to increased oxidative modifications of SERCA and its inactivation. Acute hyperglycemia in heart patients is currently being treated by administration of insulin, which needs to be carefully titrated. It would be interesting to see whether ARI treatment might provide a better outcome.
GRANTS
This work was supported by The University of Hong Kong Committee on Research and Conference Grants. X. Y. Tong and X. Y. Hou were supported by National Institutes of Health Grant RO1-HL-31607-25 and American Diabetes Association Grant 7-09-JF-69.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
ACKNOWLEDGMENTS
We thank C. P. Mok and Dr. S. Wu for technical assistance.
REFERENCES
- 1.Adachi T, Matsui R, Xu S, Kirber M, Lazar HL, Sharov VS, Schoneich C, Cohen RA. Antioxidant improves smooth muscle sarco/endoplasmic reticulum Ca(2+)-ATPase function and lowers tyrosine nitration in hypercholesterolemia and improves nitric oxide-induced relaxation. Circ Res 90: 1114–1121, 2002 [DOI] [PubMed] [Google Scholar]
- 2.Adachi T, Weisbrod RM, Pimentel DR, Ying J, Sharov VS, Schoneich C, Cohen RA. S-glutathiolation by peroxynitrite activates SERCA during arterial relaxation by nitric oxide. Nat Med 10: 1200–1207, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Bassenge E, Sommer O, Schwemmer M, Bunger R. Antioxidant pyruvate inhibits cardiac formation of reactive oxygen species through changes in redox state. Am J Physiol Heart Circ Physiol 279: H2431–H2438, 2000 [DOI] [PubMed] [Google Scholar]
- 4.Bers DM. Calcium fluxes involved in control of cardiac myocyte contraction. Circ Res 87: 275–281, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Bowes J, McDonald MC, Piper J, Thiemermann C. Inhibitors of poly (ADP-ribose) synthetase protect rat cardiomyocytes against oxidant stress. Cardiovasc Res 41: 126–134, 1999 [DOI] [PubMed] [Google Scholar]
- 6.Cameron NE, Cotter MA, Robertson S. Contractile properties of cardiac papillary muscle in streptozotocin-diabetic rats and the effects of aldose reductase inhibition. Diabetologia 32: 365–370, 1989 [DOI] [PubMed] [Google Scholar]
- 7.Ceriello A, Quagliaro L, D'Amico M, Di Filippo C, Marfella R, Nappo F, Berrino L, Rossi F, Giugliano D. Acute hyperglycemia induces nitrotyrosine formation and apoptosis in perfused heart from rat. Diabetes 51: 1076–1082, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Cherednichenko G, Zima AV, Feng W, Schaefer S, Blatter LA, Pessah IN. NADH oxidase activity of rat cardiac sarcoplasmic reticulum regulates calcium-induced calcium release. Circ Res 94: 478–486, 2004 [DOI] [PubMed] [Google Scholar]
- 9.Chung SS, Chung SK. Aldose reductase in diabetic microvascular complications. Curr Drug Targets 6: 475–486, 2005 [DOI] [PubMed] [Google Scholar]
- 10.D'Amico M, Marfella R, Nappo F, Di Filippo C, De Angelis L, Berrino L, Rossi F, Giugliano D. High glucose induces ventricular instability and increases vasomotor tone in rats. Diabetologia 44: 464–470, 2001 [DOI] [PubMed] [Google Scholar]
- 11.Davidoff AJ, Ren J. Low insulin and high glucose induce abnormal relaxation in cultured adult rat ventricular myocytes. Am J Physiol Heart Circ Physiol 272: H159–H167, 1997 [DOI] [PubMed] [Google Scholar]
- 12.Dong F, Ren J. Fidarestat improves cardiomyocyte contractile function in db/db diabetic obese mice through a histone deacetylase Sir2-dependent mechanism. J Hypertens 25: 2138–2147, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Dutta K, Carmody MW, Cala SE, Davidoff AJ. Depressed PKA activity contributes to impaired SERCA function and is linked to the pathogenesis of glucose-induced cardiomyopathy. J Mol Cell Cardiol 34: 985–996, 2002 [DOI] [PubMed] [Google Scholar]
- 14.Fabiato A, Fabiato F. Effects of magnesium on contractile activation of skinned cardiac cells. J Physiol 249: 497–517, 1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraser H, Belardinelli L, Wang L, Light PE, McVeigh JJ, Clanachan AS. Ranolazine decreases diastolic calcium accumulation caused by ATX-II or ischemia in rat hearts. J Mol Cell Cardiol 41: 1031–1038, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Gupta RK, Wittenberg BA. 19F nuclear magnetic resonance studies of free calcium in heart cells. Biophys J 65: 2547–2558, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hwang YC, Bakr S, Ellery CA, Oates PJ, Ramasamy R. Sorbitol dehydrogenase: a novel target for adjunctive protection of ischemic myocardium. FASEB J 17: 2331–2333, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Hwang YC, Kaneko M, Bakr S, Liao H, Lu Y, Lewis ER, Yan S, Ii S, Itakura M, Rui L, Skopicki H, Homma S, Schmidt AM, Oates PJ, Szabolcs M, Ramasamy R. Central role for aldose reductase pathway in myocardial ischemic injury. FASEB J 18: 1192–1199, 2004 [DOI] [PubMed] [Google Scholar]
- 19.Iwata K, Matsuno K, Nishinaka T, Persson C, Yabe-Nishimura C. Aldose reductase inhibitors improve myocardial reperfusion injury in mice by a dual mechanism. J Pharm Sci 102: 37–46, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Iwata K, Nishinaka T, Matsuno K, Kakehi T, Katsuyama M, Ibi M, Yabe-Nishimura C. The activity of aldose reductase is elevated in diabetic mouse heart. J Pharm Sci 103: 408–416, 2007 [DOI] [PubMed] [Google Scholar]
- 21.Jourdon P, Feuvray D. Calcium and potassium currents in ventricular myocytes isolated from diabetic rats. J Physiol 470: 411–429, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaiserova K, Srivastava S, Hoetker JD, Awe SO, Tang XL, Cai J, Bhatnagar A. Redox activation of aldose reductase in the ischemic heart. J Biol Chem 281: 15110–15120, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Kaiserova K, Tang XL, Srivastava S, Bhatnagar A. Role of nitric oxide in regulating aldose reductase activation in the ischemic heart. J Biol Chem 283: 9101–9112, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J, Li Q, Fang CX, Ren J. Paradoxical effects of ginkgolide B on cardiomyocyte contractile function in normal and high-glucose environments. Acta Pharmacol Sin 27: 536–542, 2006 [DOI] [PubMed] [Google Scholar]
- 25.Knyushko TV, Sharov VS, Williams TD, Schoneich C, Bigelow DJ. 3-Nitrotyrosine modification of SERCA2a in the aging heart: a distinct signature of the cellular redox environment. Biochemistry 44: 13071–13081, 2005 [DOI] [PubMed] [Google Scholar]
- 26.Kravtsov GM, Pokudin NI, Orlov SN. [Ca2+-accumulating capacity of mitochondria, sarcolemma and sarcoplasmic reticulum of rat heart]. Biokhimiia 44: 2058–2065, 1979 [PubMed] [Google Scholar]
- 27.Lagadic-Gossmann D, Buckler KJ, Le Prigent K, Feuvray D. Altered Ca2+ handling in ventricular myocytes isolated from diabetic rats. Am J Physiol Heart Circ Physiol 270: H1529–H1537, 1996 [DOI] [PubMed] [Google Scholar]
- 28.Lee AY, Chung SS. Contributions of polyol pathway to oxidative stress in diabetic cataract. FASEB J 13: 23–30, 1999 [DOI] [PubMed] [Google Scholar]
- 29.Levy J, Gavin JR, 3rd, Sowers JR. Diabetes mellitus: a disease of abnormal cellular calcium metabolism? Am J Med 96: 260–273, 1994 [DOI] [PubMed] [Google Scholar]
- 30.Li Q, Hwang YC, Ananthakrishnan R, Oates PJ, Guberski D, Ramasamy R. Polyol pathway and modulation of ischemia-reperfusion injury in Type 2 diabetic BBZ rat hearts. Cardiovasc Diabetol 7: 33, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin G, Craig GP, Zhang L, Yuen VG, Allard M, McNeill JH, MacLeod KM. Acute inhibition of Rho-kinase improves cardiac contractile function in streptozotocin-diabetic rats. Cardiovasc Res 75: 51–58, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Liu J, Kam KW, Borchert GH, Kravtsov GM, Ballard HJ, Wong TM. Further study on the role of HSP70 on Ca2+ homeostasis in rat ventricular myocytes subjected to simulated ischemia. Am J Physiol Cell Physiol 290: C583–C591, 2006 [DOI] [PubMed] [Google Scholar]
- 33.Magyar J, Rusznak Z, Szentesi P, Szucs G, Kovacs L. Action potentials and potassium currents in rat ventricular muscle during experimental diabetes. J Mol Cell Cardiol 24: 841–853, 1992 [DOI] [PubMed] [Google Scholar]
- 34.Marfella R, Di Filippo C, Portoghese M, Ferraraccio F, Rizzo MR, Siniscalchi M, Musacchio E, D'Amico M, Rossi F, Paolisso G. Tight glycemic control reduces heart inflammation and remodeling during acute myocardial infarction in hyperglycemic patients. J Am Coll Cardiol 53: 1425–1436, 2009 [DOI] [PubMed] [Google Scholar]
- 35.Marfella R, Nappo F, De Angelis L, Siniscalchi M, Rossi F, Giugliano D. The effect of acute hyperglycaemia on QTc duration in healthy man. Diabetologia 43: 571–575, 2000 [DOI] [PubMed] [Google Scholar]
- 36.Marfella R, Quagliaro L, Nappo F, Ceriello A, Giugliano D. Acute hyperglycemia induces an oxidative stress in healthy subjects. J Clin Invest 108: 635–636, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marfella R, Verrazzo G, Acampora R, La Marca C, Giunta R, Lucarelli C, Paolisso G, Ceriello A, Giugliano D. Glutathione reverses systemic hemodynamic changes induced by acute hyperglycemia in healthy subjects. Am J Physiol Endocrinol Metab 268: E1167–E1173, 1995 [DOI] [PubMed] [Google Scholar]
- 38.Mohazzab HK, Kaminski PM, Wolin MS. Lactate and Po2 modulate superoxide anion production in bovine cardiac myocytes: potential role of NADH oxidase. Circulation 96: 614–620, 1997 [DOI] [PubMed] [Google Scholar]
- 39.Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295: 1681–1687, 2006 [DOI] [PubMed] [Google Scholar]
- 40.Nakazawa K, Higo K, Abe K, Tanaka Y, Saito H, Matsuki N. Blockade by calmodulin inhibitors of Ca2+ channels in smooth muscle from rat vas deferens. Br J Pharmacol 109: 137–141, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oswald GA, Smith CC, Betteridge DJ, Yudkin JS. Determinants and importance of stress hyperglycaemia in non-diabetic patients with myocardial infarction. Br Med J (Clin Res Ed) 293: 917–922, 1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pessah IN, Feng W. Functional role of hyperreactive sulfhydryl moieties within the ryanodine receptor complex. Antioxid Redox Signal 2: 17–25, 2000 [DOI] [PubMed] [Google Scholar]
- 43.Ramasamy R, Liu H, Oates PJ, Schaefer S. Attenuation of ischemia induced increases in sodium and calcium by the aldose reductase inhibitor zopolrestat. Cardiovasc Res 42: 130–139, 1999 [DOI] [PubMed] [Google Scholar]
- 44.Ramasamy R, Oates PJ, Schaefer S. Aldose reductase inhibition protects diabetic and nondiabetic rat hearts from ischemic injury. Diabetes 46: 292–300, 1997 [DOI] [PubMed] [Google Scholar]
- 45.Ren J, Davidoff AJ. Diabetes rapidly induces contractile dysfunctions in isolated ventricular myocytes. Am J Physiol Heart Circ Physiol 272: H148–H158, 1997 [DOI] [PubMed] [Google Scholar]
- 46.Ren J, Dominguez LJ, Sowers JR, Davidoff AJ. Metformin but not glyburide prevents high glucose-induced abnormalities in relaxation and intracellular Ca2+ transients in adult rat ventricular myocytes. Diabetes 48: 2059–2065, 1999 [DOI] [PubMed] [Google Scholar]
- 47.Ren J, Gintant GA, Miller RE, Davidoff AJ. High extracellular glucose impairs cardiac E-C coupling in a glycosylation-dependent manner. Am J Physiol Heart Circ Physiol 273: H2876–H2883, 1997 [DOI] [PubMed] [Google Scholar]
- 48.Rubler S, Dlugash J, Yuceoglu YZ, Kumral T, Branwood AW, Grishman A. New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol 30: 595–602, 1972 [DOI] [PubMed] [Google Scholar]
- 49.Schaefer A, Magocsi M, Stocker U, Kosa F, Marquardt H. Early transient suppression of c-myb mRNA levels and induction of differentiation in Friend erythroleukemia cells by the [Ca2+]i-increasing agents cyclopiazonic acid and thapsigargin. J Biol Chem 269: 8786–8791, 1994 [PubMed] [Google Scholar]
- 50.Schwalbe RA, Wang Z, Wible BA, Brown AM. Potassium channel structure and function as reported by a single glycosylation sequon. J Biol Chem 270: 15336–15340, 1995 [DOI] [PubMed] [Google Scholar]
- 51.Tang WH, Wu S, Wong TM, Chung SK, Chung SS. Polyol pathway mediates iron-induced oxidative injury in ischemic-reperfused rat heart. Free Radic Biol Med 45: 602–610, 2008 [DOI] [PubMed] [Google Scholar]
- 52.Tang WH, Wu S, Wong TM, Chung SK, Chung SS. Polyol pathway mediates iron-induced oxidative injury in ischemic-reperfused rat heart. Free Radic Biol Med 45: 602–610, 2008 [DOI] [PubMed] [Google Scholar]
- 53.Temsah RM, Netticadan T, Chapman D, Takeda S, Mochizuki S, Dhalla NS. Alterations in sarcoplasmic reticulum function and gene expression in ischemic-reperfused rat heart. Am J Physiol Heart Circ Physiol 277: H584–H594, 1999 [DOI] [PubMed] [Google Scholar]
- 54.Tong X, Ying J, Pimentel DR, Trucillo M, Adachi T, Cohen RA. High glucose oxidizes SERCA cysteine-674 and prevents inhibition by nitric oxide of smooth muscle cell migration. J Mol Cell Cardiol 44: 361–369, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsang S, Wu S, Liu J, Wong TM. Testosterone protects rat hearts against ischaemic insults by enhancing the effects of alpha(1)-adrenoceptor stimulation. Br J Pharmacol 153: 693–709, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Viner RI, Ferrington DA, Williams TD, Bigelow DJ, Schoneich C. Protein modification during biological aging: selective tyrosine nitration of the SERCA2a isoform of the sarcoplasmic reticulum Ca2+-ATPase in skeletal muscle. Biochem J 340: 657–669, 1999 [PMC free article] [PubMed] [Google Scholar]
- 57.Waldenstrom AP, Hjalmarson AC, Thornell L. A possible role of noradrenaline in the development of myocardial infarction: an experimental study in the isolated rat heart. Am Heart J 95: 43–51, 1978 [DOI] [PubMed] [Google Scholar]
- 58.Wang L, Lopaschuk GD, Clanachan AS. H(2)O(2)-induced left ventricular dysfunction in isolated working rat hearts is independent of calcium accumulation. J Mol Cell Cardiol 45: 787–795, 2008 [DOI] [PubMed] [Google Scholar]
- 59.Wu S, Li HY, Wong TM. Cardioprotection of preconditioning by metabolic inhibition in the rat ventricular myocyte. Involvement of kappa-opioid receptor. Circ Res 84: 1388–1395, 1999 [DOI] [PubMed] [Google Scholar]
- 60.Xu KY, Zweier JL, Becker LC. Hydroxyl radical inhibits sarcoplasmic reticulum Ca(2+)-ATPase function by direct attack on the ATP binding site. Circ Res 80: 76–81, 1997 [DOI] [PubMed] [Google Scholar]
- 61.Yeung HM, Kravtsov GM, Ng KM, Wong TM, Fung ML. Chronic intermittent hypoxia alters Ca2+ handling in rat cardiomyocytes by augmented Na+/Ca2+ exchange and ryanodine receptor activities in ischemia-reperfusion. Am J Physiol Cell Physiol 292: C2046–C2056, 2007 [DOI] [PubMed] [Google Scholar]
- 62.Ying J, Sharov V, Xu S, Jiang B, Gerrity R, Schoneich C, Cohen RA. Cysteine-674 oxidation and degradation of sarcoplasmic reticulum Ca(2+) ATPase in diabetic pig aorta. Free Radic Biol Med 45: 756–762, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ying WL, Emerson J, Clarke MJ, Sanadi DR. Inhibition of mitochondrial calcium ion transport by an oxo-bridged dinuclear ruthenium ammine complex. Biochemistry 30: 4949–4952, 1991 [DOI] [PubMed] [Google Scholar]
- 64.Zucchi R, Ronca-Testoni S, Yu G, Galbani P, Ronca G, Mariani M. Effect of ischemia and reperfusion on cardiac ryanodine receptors–sarcoplasmic reticulum Ca2+ channels. Circ Res 74: 271–280, 1994 [DOI] [PubMed] [Google Scholar]