Abstract
Aim
We used secondary data from a prospective randomized mammography recruitment trial to examine whether attitudinal and facilitating characteristics mediate the observed relationship between annual household income and mammogram receipt among women in an integrated health plan.
Methods
We compared 1419 women due for a screening mammogram based on the 1995 annual household income poverty definition for a family of four (<$15,000 vs. >$15,000). A telephone survey was used to collect information on household income, demographics, health behavior, attitudinal and facilitating variables. Administrative databases were used to document mammography receipt. We used Cox proportional hazards models to estimate the hazards ratio (HR) and 95% confidence interval (CI) of subsequent mammography use separately for women with and without a prior mammogram.
Results
Several variables, including employment, living alone, believing that mammograms are unnecessary, having friends supportive of mammography, and ease of arranging transportation, completely mediated the effect of income on mammography use. In multivariable models, the direct predictive effect of income on mammography was reduced to nonsignificance (HR 1.13, 95% CI 0.82–1.54 in women with previous mammogram and HR 0.91, 95% CI 0.41–2.00 in women without previous mammogram).
Conclusions
Providing insurance does not ensure low-income populations will seek screening mammography. Efficacious interventions that address attitudes and facilitating conditions may motivate mammography use among low-income women with insurance.
Introduction
Breast cancer is the leading incident cancer and the second leading cause of cancer death in women.1 Recent trends indicate a decline in deaths, attributable to uptake of screening mammograms and treatment advances.1,2 Mortality reduction has not been universally shared, however. Low-income women are at higher risk for breast cancer mortality partially because of lower screening rates.3 Cost is one important barrier4; however, intervention studies show low-income women are less likely to receive a mammogram even with insurance coverage or offers of free mammograms.5–6 Additionally, an analysis of seven integrated health plans showed that 53% of women who had late-stage breast cancers also had not been recently screened, and they were more likely to be from low-income neighborhoods.7 Therefore, addressing insurance access alone may not increase mammography use.
Meta-analyses indicate that access-enhancing interventions are most effective at increasing mammography among low-income populations, but most of these studies have been conducted with populations lacking health insurance.8–10 Thus, less is known about interventions that are effective among low-income women who have insurance. We are unaware of behavioral epidemiological studies in the United states that have examined whether attitudinal and facilitating variables explain the differential patterns of mammography use by income among women with insurance.
We reported previously that low-income women in an integrated health plan, where mammograms are a covered benefit provided free-of-charge, were less likely than higher income women to receive a mammogram within a year following invitation to receive a mammogram.5 We reexamined data from the original trial to evaluate whether attitudinal or facilitating variables mediated the effect of income on mammography use. We are aware of no other longitudinal studies that evaluate mediators along the causal pathway between income and mammography use among women within a managed care organization with access to mammography at no direct cost.
Materials and Methods
Study population
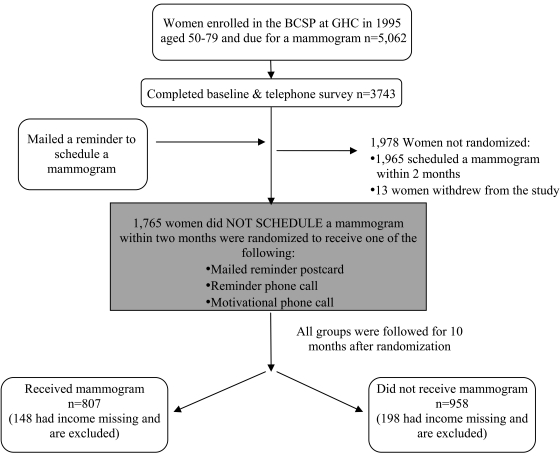
The current report uses data from a randomized trial of screening mammography among 5062 randomly selected women aged 50–79 years who were enrolled in a breast cancer screening program, were due for a screening mammogram in 1995, and did not schedule the examination after a mailed reminder.5 The trial was previously described in detail and is summarized in Figure 1.5 The 1765 women who were nonadherent 2 months after being sent a letter recommending screening were randomized into three intervention groups: a mailed reminder, a telephone reminder, or a motivational telephone call. Group Health's (GH) Institutional Review Board reviewed and approved this analysis. Data were collected from 1996 to 1997.
FIG. 1.
Study design: The 1419 women with income information comprised the study population for the analysis.
Survey
The trial was based on a heuristic conceptual framework that combined aspects of the theory of reasoned action, social learning theory, and the precede/proceed mode.5 In a baseline telephone survey, we collected information on demographic characteristics (age, education, race, employment, marital status, and living situation), health practices (previous mammography or Pap smear, smoking, and health status), attitudinal beliefs about mammography and breast cancer (e.g., perceptions of what others want them to do; anxiety – discomfort, radiation and embarrassment or about waiting for the test; and affect), and conditions that facilitate mammography uptake (e.g., transportation method, parking, scheduling, and courtesy of staff).
Items measuring attitudes and facilitating conditions were assessed on a 5-point Likert scale with varying anchors (e.g., strongly disagree to strongly agree or very easy to very difficult). Don't know was used to describe the midpoint. For highly skewed items, we collapsed responses for strongly to somewhat and excluded Don't know responses if <3 people chose the response.
Participants recruited for the trial were a random sample of 11,570 women due for a mammogram based on administrative records during a 15-month rolling recruitment period in 1995–1996. An introductory letter was sent to women, with the option to exclude themselves from a subsequent telephone contact. At the time of the telephone contact, women were given information about the study, and informed consent was obtained. We approached 5062 women, and 3743 (74%) agreed to participate and completed a 15-minute telephone survey (Fig. 1). There were no financial incentives. After the survey, women were sent a reminder letter saying they were due for a mammogram. This study occurred among the women who did not schedule an examination within 2 months of when the reminder letter was sent (Fig. 1).
Income
We collapsed self-reported annual household income into two categories: low income (at or below the U.S. 1995 poverty level of $15,000/year for a family of four) and high income (above the poverty line).11
Outcome
Our outcome was receipt of a mammogram within 12 months of an invitation to schedule a mammogram and 10 months of being randomized for the parent trial. We ascertained the date of the mammogram from an automated administrative database that has records on all mammograms received at GH as well as those received outside GH if a claim was submitted.
Analysis
The purpose of this analysis was to determine if attitudinal or facilitating variables mediated the effect of income on mammography use. To evaluate mediation, we modified Baron and Kenny's three-step sequential analytic method12 to require that (1) the independent variable is associated with the dependent variable, (2) the independent variable is associated with the mediator, and (3) the mediating variable is associated with the dependent variable when both the independent variable and the mediator are simultaneously regressed on the dependent variable. Complete mediation is indicated if the association between independent and dependent variables is reduced to nonsignificance.
Evidence of the first step, that the independent variable (income) significantly predicted the dependent variable (mammography receipt), was shown in a previous paper.5 Therefore, our analysis began with the second step, determining if the independent variable, income, was significantly associated with the hypothesized mediators. We computed chi-square tests to compare the distributions of all attitudinal and facilitating variables by income level. We also examined the association between attitudinal and facilitating variables and the dependent variable, mammography receipt. Because the parent trial stratified on prior mammography use, we maintained this stratification in this and subsequent analyses.5
To evaluate Baron and Kenny's third stem,12 we used separate Cox proportional hazards models to estimate the hazards ratio (HR) and 95% confidence intervals (CIs) of mammography receipt within 12 months of an invitation to schedule a mammogram, adjusted for randomization group and including one mediator variable at a time (base model). All mediators were modeled as categorical variables using the groups shown in Table 1, with the first category as the referent. We stratified all analyses based on past mammography status, adjusted all analyses for randomization group, and used time since randomization as the time axis. Follow-up time ended at the first of the following events: mammography receipt, death, disenrollment from the health plan, or end of the study period. These Cox models allowed us to assess the individual contribution of each mediator.
Table 1.
Characteristics of Women by Annual Household Incomea and Mammography Experience and by Whether or Not Women Received a Mammogram within 12 Months of an Invitation to Schedule a Mammogram
| |
|
|
Previous mammogram |
No previous mammogram |
||
|---|---|---|---|---|---|---|
| Characteristic | Low incomea(n = 207) Column % | High incomea(n = 1212) Column % | Received mammogram (n = 578) Column % | Did not receive mammogram (n = 448) Column % | Received mammogram (n = 81) Column % | Did not receive mammogram (n = 312) Column % |
| Demographics | ||||||
| Group | ||||||
| Postcard | 27.5 | 35.2 | 26.6 | 43.3 | 17.3 | 38.8 |
| Reminder call | 30.9 | 32.8 | 36.2 | 27.9 | 44.4 | 29.2 |
| Motivational call | 41.6 | 32.1 | 37.2 | 28.8 | 38.3 | 32.1 |
| Annual household incomea | ||||||
| Low income (≤$15,000) | N/A | N/A | 9.7 | 15.8 | 12.3 | 22.4 |
| High income (>$15,000) | N/A | N/A | 90.3 | 84.2 | 87.7 | 77.6 |
| Age, yearsb | ||||||
| 50–59 | 14.5 | 55.5 | 50.2 | 50.4 | 64.2 | 43.3 |
| 60–69 | 30.9 | 26.9 | 28.4 | 25.4 | 23.5 | 29.8 |
| 70–79 | 54.6 | 17.6 | 21.5 | 24.1 | 12.3 | 26.9 |
| Educationb,c | ||||||
| <High school | 65.7 | 31.6 | 34.1 | 37.5 | 35.8 | 39.9 |
| Some college | 25.1 | 35.0 | 30.7 | 33.5 | 43.2 | 36.7 |
| ≥College graduate | 9.2 | 33.4 | 35.2 | 29.0 | 21.0 | 23.5 |
| Raceb | ||||||
| White | 86.5 | 89.8 | 90.5 | 90.2 | 87.7 | 86.2 |
| Native American | 1.9 | 0.7 | 1.0 | 0.9 | 1.2 | 0.3 |
| African American | 6.3 | 3.7 | 3.5 | 4.2 | 4.9 | 4.8 |
| Asian | 1.5 | 4.7 | 4.2 | 3.1 | 4.9 | 5.8 |
| Other | 3.9 | 1.2 | 0.9 | 1.6 | 1.2 | 2.9 |
| Employmentb,d | ||||||
| Employed | 15.0 | 56.9 | 51.8 | 48.9 | 63.2 | 48.3 |
| Unemployed | 17.0 | 10.9 | 10.3 | 13.3 | 11.8 | 12.3 |
| Retired | 65.0 | 30.0 | 34.7 | 35.4 | 25.0 | 38.0 |
| Disabled/other/don't know/refuse | 3.1 | 2.2 | 3.1 | 2.4 | 0.0 | 1.3 |
| Marital statusb,e | ||||||
| Married | 17.0 | 61.4 | 62.2 | 52.3 | 63.6 | 53.0 |
| Unmarried | 83.0 | 38.6 | 37.9 | 47.7 | 36.4 | 47.0 |
| Living situationb,f | ||||||
| Alone | 12.6 | 45.5 | 46.2 | 37.5 | 43.2 | 34.7 |
| Living with relatives | 25.2 | 31.4 | 27.9 | 31.7 | 39.5 | 31.5 |
| Living with nonrelatives | 62.1 | 23.0 | 26.0 | 30.8 | 17.3 | 33.8 |
| Health practices | ||||||
| Prior mammogramb | 61.4 | 74.2 | N/A | N/A | N/A | N/A |
| Pap smear in last 4 yearsb,g | 65.4 | 76.7 | 83.7 | 72.9 | 72.8 | 62.5 |
| Attitudinal beliefs | ||||||
| Mammogram very/somewhat frighteningb,c | 13.0 | 6.9 | 2.8 | 5.8 | 13.6 | 18.3 |
| Mammogram very/somewhat beneficialb | 70.1 | 85.2 | 93.9 | 82.8 | 90.1 | 61.2 |
| Finding breast cancer early is very/somewhat beneficialb | 95.2 | 98.3 | 100.0 | 97.0 | 98.0 | 93.0 |
| Inconvenience of getting a mammogram is very/somewhat acceptableb | 70.1 | 79.6 | 91.1 | 76.1 | 71.7 | 54.5 |
| Mammogram important even without cancer signs (strongly/somewhat agree)b | 64.3 | 76.3 | 86.3 | 75.9 | 81.5 | 49.0 |
| Mammogram might detect cancer clinician can't find during phyiscal examination (strongly/somewhat agree)b | 84.1 | 93.3 | 97.1 | 92.2 | 95.1 | 81.4 |
| Mammogram unnecessary at your age (strongly/somewhat agree)b | 34.3 | 16.0 | 8.1 | 18.8 | 11.1 | 40.1 |
| Regular healthcare provider feels you should have a mammogram (strongly/somewhat agree)b | 70.1 | 84.2 | 90.5 | 82.6 | 84.0 | 65.7 |
| Women friends feel you should have a mammogram (strongly/somewhat agree)b | 38.7 | 58.5 | 65.1 | 52.5 | 60.5 | 39.4 |
| Didn't want mammogram because didn't want to know if had cancer (just/somewhat like you)b,e | 16.4 | 9.0 | 4.3 | 8.1 | 15.2 | 21.7 |
| Didn't want mammogram because too confused with contradictory information (just/somewhat like you)b,e | 22.2 | 14.0 | 5.9 | 13.4 | 18.5 | 34.1 |
| Knowledge of the likelihood women will get breast cancerb | 13.3 | 22.1 | 24.7 | 17.8 | 15.0 | 19.5 |
| 1 in 9 | ||||||
| >1 in 9 | 37.0 | 44.6 | 47.2 | 44.2 | 30.0 | 39.1 |
| <1 in 9 | 23.7 | 22.5 | 19.2 | 23.9 | 38.8 | 23.1 |
| Don't know | 26.1 | 10.8 | 8.9 | 14.0 | 16.3 | 18.2 |
| Facilitating conditions | ||||||
| Very/somewhat easy to arrange transportationb | 68.1 | 90.1 | 92.9 | 85.9 | 83.8 | 77.7 |
| Very/somewhat easy to parkh | 66.9 | 69.4 | 61.1 | 60.5 | 45.7 | 51.6 |
Annual household income collected from self-report in 1995 and classified into low (at or below the U.S. 1995 poverty level of $15,000/year for a family of four) and high income (>$15,000/year).11
<0.05 based on chi-square test for difference between low vs. high income.
Missing 2 responses.
Missing 31 responses.
1 Don't know response excluded.
Missing 1 response.
19 Don't know/refuse responses excluded.
Among those who came to their appointment by car.
N/A, not applicable.
We calculated the percent of the relationship between income and receipt of mammography that could be accounted for by accounting for individual mediator variables (excess risk).13,14 Excess risk was calculated as follows:
(HR income adjusted for randomization group — HR income adjusted for randomization group + explanatory factor)/(1 — HR income adjusted for randomization group)*10013,14
The percent excess risk measures the percent of the HR between income and mammography receipt that can be explained by the mediator variable. The methods used to calculate excess risk for each mediator ignore variables that are collinear (e.g., age, employment). As a result, two factors that are correlated could individually account for a similar percentage of excess risk but, when examined in combination, explain less than their sum.
To examine the combined effect of all significant mediators, we constructed a final multivariable model including all mediators from the bivariate analyses that accounted for ≥10% of the excess risk for income and mammography receipt, adjusting for randomization group.15 For example, a variable could strongly predict mammogram use but not be associated with income; such a variable would not change the beta-estimate for income and, therefore, was not included. The same is true for variables associated with income but not with mammography. This method assures that only variables associated with both the exposure (income) and outcome (mammography) are included in the multivariable model.15
We repeated this process adjusting for age and living situation in the base model to determine if there were any different mediators identified after adjusting for age in all the base models. All analyses were conducted in Stata 9.2 (College Station, TX).
Results
Among the 1765 potentially eligible women, 346 women (19.6%) provided no information about their income and were excluded, leaving a total sample of 1419 women in our study. The proportion of nonresponse to the income item observed in this study was similar to that in national surveys, such as the National Health Interview Survey (NHIS).16 Fifteen percent of the women (n = 207) reported low income. Mammography use was lower among low-income (31.9%) compared with high-income women (48.9%). Lower-income women were older; less educated; more likely to be non-white, unemployed or retired, unmarried, living with non-relatives; and less likely to have had a prior mammogram or a recent Pap smear than high-income women (Table 1). There were many differences between lower-income and higher-income women for variables measuring attitudinal beliefs. Lower-income women were more likely to believe that having a mammogram is frightening, feel the inconvenience of getting a mammogram is unacceptable, believe that having a mammogram is unnecessary at their age, not want to know if they had cancer, and be confused by contradictory information about mammography (Table 1). There were no differences by income in attitudes reflecting anxiety about the mammogram (e.g., physical discomfort, radiation, embarrassment) or about waiting for results (data not shown). The only facilitating condition associated with income was ease in arranging transportation; there were no differences in transportation method, issues related to making an appointment, or perceived courtesy of staff (data not shown).
Twenty-eight percent of the women (n = 393) reported no previous mammogram, and these women were significantly less likely than women who had had a previous mammogram to receive a mammogram during the study period (Table 1). When stratified by past mammography behavior, mammography receipt was associated with being in one of the telephone intervention groups, higher income, younger age, employment status, and having a recent Pap test (Table 1). Women who did not get a mammogram during the study period were more likely to report negative attitudes (Table 1).
Higher-income women were more likely to get a mammogram when it was recommended, regardless of their previous screening behavior (Table 2). For women who had a previous mammogram, employment, living alone, recent Pap test, and four attitudinal or facilitating conditions (believing mammography is unnecessary at her age, whether women friends thought she should have a mammogram, knowledge of the likelihood of getting breast cancer, and ease of arranging transportation) each independently explained part of the relationship between income and mammography, with significant percent excess risks for individual mediators ranging from 13.8% (Pap smear in past 4 years) to 20.7% (employment). After accounting for all seven mediators identified in the base models in the multivariable model, there was no association between income and mammography receipt for women with a prior mammogram (HR 1.13, 95% CI 0.82–1.54), explaining 77.6% of the relationship between income and mammography.
Table 2.
Hazards Ratios (HR) and 95% Confidence Intervals (CI) for Mammography Receipt within 12 Months of Invitation to Schedule a Mammogram among Higher, Income Relative to Lower-Incomea Women: Univariate Analysis, Base Modelb Mediator Analyses, and Overall Multivariable Models Stratified by Prior Mammography Use
| Previous mammogram (n = 1026) | No previous mammogram (n = 393) | |||
|---|---|---|---|---|
| Univariate model | HR (95% CI) for mammography use among higher-income vs. lower-income women adjusting for randomization group | |||
| Risk of receiving a mammogram among higher vs. lower-income women | 1.58 (1.20–2.08) | 2.02 (1.04–3.92) | ||
| Base model: potential mediators | Base model HR (95% CI) for mammography use among higher-income vs. lower-income women adjusted for randomization group and including one potential mediator variableb | |||
| % Excess riskc | % Excess riskc | |||
| Demographics | ||||
| Age | 1.59 (1.19–2.13) | 1.7% | 1.48 (0.74–2.97) | −52.9% |
| Education | 1.55 (1.17–2.05) | −5.2% | 2.04 (1.03–4.04) | 2.0% |
| Race | 1.55 (1.17–2.05) | −5.2% | 2.00 (1.03–3.90) | −2.0% |
| Employment | 1.46 (1.09–1.95) | −20.7% | 1.50 (0.73–3.08) | −51.0% |
| Living alone | 1.49 (1.12–1.99) | −15.5% | 1.57 (0.79–3.12) | −44.1% |
| Past preventive behavior | ||||
| Pap smear in last 4 years | 1.50 (1.14–1.98) | −13.8% | 2.03 (1.04–3.94) | 1.0% |
| Attitudes | ||||
| Mammogram frightening | 1.57 (1.19–2.07) | −1.7% | 1.71 (0.87–3.35) | −30.4% |
| Mammogram beneficial | 1.55 (1.18–2.05) | −5.2% | 1.42 (0.72–2.78) | −58.8% |
| Finding breast cancer early is beneficial | 1.56 (1.19–2.06) | −3.4% | 1.99 (1.02–3.87) | −2.9% |
| Inconvenience of getting a mammogram acceptable | 1.56 (1.18–2.06) | −3.4% | 1.93 (0.99–3.78) | −8.8% |
| Mammogram important even without cancer signs | 1.56 (1.18–2.05) | −3.4% | 1.66 (0.85–3.24) | −35.3% |
| Mammogram might detect cancer clinician can't find during physical examination | 1.54 (1.17–2.03) | −6.9% | 1.75 (0.90–3.43) | −26.5% |
| Mammogram unnecessary at your age | 1.48 (1.12–1.95) | −17.2% | 1.46 (0.75–2.87) | −54.9% |
| Do what people important to you think you should do | 1.58 (1.20–2.09) | 0.0% | 1.98 (1.02–3.85) | −3.9% |
| Regular healthcare provider thinks you should have a mammogram | 1.53 (1.16–2.02) | −8.6% | 1.79 (0.91–3.52) | −22.5% |
| Women friends think you should have a mammogram | 1.49 (1.13–1.96) | −15.5% | 1.79 (0.91–3.51) | −22.5% |
| Didn't want mammogram because didn't want to know if had cancer | 1.57 (1.19–2.06) | −1.7% | 1.93 (0.99–3.75) | −8.8% |
| Didn't want mammogram because too confused with contradictory information | 1.60 (1.21–2.11) | 3.4% | 1.82 (0.93–3.55) | −19.6% |
| Knowledge of the likelihood women will get breast cancer | 1.48 (1.12–1.96) | −17.2% | 2.05 (1.04–4.02) | 2.9% |
| Facilitating conditions | ||||
| Easy/difficult to arrange transportation | 1.43 (1.08–1.89) | −25.9% | 1.90 (0.95–3.80) | −11.8% |
| Easy/difficult to park | 1.57 (1.19–2.08) | −1.7% | 2.08 (1.07–4.06) | 5.9% |
| Multivariable model | Multivariabale HRd,e (95% CI) for mammography use among higher-income vs. lower-income women for income and mammography use | |||
| Multivariable model | 1.13d (0.82–1.54) | 77.6% | 0.91e (0.41–2.00) | >100% |
Annual household income collected from self-report in 1995 and classified into low-income (at or below the U.S. 1995 poverty level of $15,000/year for a family of four) and high-income (>$15,000/year).11
Each base model includes income and randomization group with one potential mediator variable. All mediators were modeled as categorical variables using the groups shown in Table 1, with the first category as the referent. For example, among women with no previous mammogram, high-income women were 2.02 times more likely to receive a mammogram than lower-income women (HR 2.02, 95% CI 1.04–3.92). After including age as a mediator variable, higher-income women were 1.48 times more likely to receive a mammogram compared with lower-income women (HR 1.48, 95% CI 0.74–2.97).
Excess risk is the proportion of the relation between income and receipt of mammogram explained by individual mediators. Excess risk = [(HR income adjusted for randomization group – HR income adjusted for randomization group + mediator)/(1 – HR income adjusted for randomization group)]*100.13,14 The methods used to calculate excess risk for each mediator ignore variables that are collinear. As a result, two factors that are correlated could individually account for a similar percentage of excess risk but, when examined in combination, explain less than their sum.
Mediators included in the multivariable model for women with a previous mammogram. Any mediator that accounted for ≥10% of the relation between income and mammography use was included in the multivariable model: employment; living alone; Pap smear in the last 4 years; belief that a mammogram is unnecessary at your age and women friends think you should have a mammogram; knowledge of the likelihood women will get breast cancer; and easy/difficult to arrange transportation.
Mediators included in the multivariable model for women who never had a previous mammogram. Any mediator that accounted for ≥10% of the relation between income and mammography use was included in the multivariable model: age; employment; living alone; belief that mammograms are frightening, mammogram is beneficial, mammogram is important even without cancer signs, mammogram might detect cancer clinician can't find, mammogram is unnecessary at your age; regular healthcare provider feels you should have a mammogram; women friends feel you should have a mammogram; don't want mammogram because too confused with contradictory information; and easy/difficult to arrange transportation.
For women with no previous mammogram, five of the seven variables described (employment, living alone, mammogram unnecessary at her age, whether women friends thought she should have a mammogram, and ease of arranging transportation) mediated the effect of income on mammography (Table 2). Other mediators included age and several attitudes (believing that mammograms are frightening, beneficial, important even without cancer signs; may detect cancer that a clinician cannot find; provider recommendation; being confused by contradictory information about mammography). Mediators appeared to have a greater impact on explaining the income-mammography receipt relationship among women with no prior mammography, with seven variable individually having excess risk values >30%; age, employment, and believing that mammography is beneficial and necessary at a given age individually accounted for >50% of the relationship. After accounting for individual mediators in our multivariable model in women with no previous mammogram, there was no relationship between income and mammography receipt (HR 0.91, 95% CI 0.41–2.00).
Our results were the same for women who had a previous mammogram with or without age adjustment and living status adjustment in the base model. The relationship between income and mammography was attenuated when age adjustment and living status adjustment were included in the base model, but the mediators identified did not change.
Discussion
We identified several attitudes and facilitating conditions that mediated the effect of income on mammography use in a population of women who have insurance coverage. Regardless of a woman's past behavior, three variables emerged as important targets for future interventions: belief in the necessity of mammograms, recommendations from friends, and ease of arranging transportation to the appointment. Women with no prior mammography experience reported several additional negative beliefs. If interventions are able to change these attitudes and facilitating conditions, mammography use may increase among low-income women whose direct cost barrier has been removed. Interventionists should direct their resources at addressing negative attitudes and transportation issues when designing programs targeted at low-income women with insurance.
This study also demonstrates that there can be disparities in the uptake of mammography, and likely other preventive healthcare, even among individuals with access to medical care. Providing coverage for mammograms cannot be expected to be sufficient to remove all barriers to its use; addressing the importance of early detection and variables related to ease of getting a mammogram must also be addressed to improve screening among low-income populations. Addressing these issues needs some careful thought, however, as the parent trial explicitly addressed attitudes and facilitating conditions in motivational interviews that did not result in higher participation than with simple reminder calls.5,17
There are some limitations to our findings. First, the results may not be generalizable to women seeking care in the general community who do not have health insurance or a usual source of healthcare.18 Low-income women with these types of barriers to accessing healthcare probably have more structural barriers to obtaining a mammogram. A second limitation is our measure of income. We did not ask if these women had additional assets. However, a study among Medicare beneficiaries showed that low-income people tended to have minimal assets; thus, our population is unlikely to have substantial savings that might cause misclassification and invalidation of the study findings.19 Income information was missing for 19.6% of women, although nonresponse was not related to mammography use. Thus, nonresponse bias is not likely to threaten the validity of our findings. Misclassification may result in women living alone or in families both being included in the low-income group, but this potential misclassification would tend to reduce the strength of the relationship between income and mammography use if women had more resources than we attributed to them through our income level classification.
The age of the data might be of concern. Although some variables may have changed since the data were collected, the findings about beliefs, transportation, and provider recommendation are still important barriers to receiving mammography among low-income women, as supported by more recent literature.8,20–23 A study in the U.K.24 found that cognitive variables (benefits, barriers, fears, and fatalism) eliminated differences by socioeconomic status in intention for colorectal cancer screening, which supports our findings in the United States. We know of no prior studies examining mediators that may be manipulated to encourage low-income women with insurance to get screened.
Strengths of the study include a population-based sample because it included a random sample of the entire population of enrollees in a managed care plan as well as individual-level data on women's perceptions, attitudes, and beliefs. Additionally, longitudinal data were used to test associations prospectively, which is important for designing interventions, as prospective data have been shown to serve as a richer set of predictors of future behavior than cross-sectional data.25 Conducting the study in an integrated health plan enabled an examination of barriers beyond cost. The study was conducted in a closed healthcare setting where the outcome could be ascertained through administrative files, eliminating recall bias and overestimation of the outcome commonly found when using self-reported data.26
Conclusions
The results of this study should be used to inform future mammography interventions, especially efforts to reach low-income women in managed care settings. Recent work23 suggests that even today lower income women are under-screened, so increasing mammography use in low-income populations may be an important step to addressing socioeconomic disparities in breast cancer mortality. An efficacious tailored approach to a woman's past behavior that addresses specific beliefs about the importance of mammography and facilitates transportation to the appointment may also increase use among all groups of women.
Footnotes
This research was supported by National Cancer Institute cooperative agreement, grants U01CA63731 and CA63188. D.S.M.B. was supported in part by American Cancer Society grant CRTG-03-024-01-CCE.
Acknowledgments
We extend our appreciation to Sue Curry, Ph.D., Evette Ludman, Ph.D., and William Barlow, Ph.D., who helped develop and conduct the original study.
Disclosure Statement
No competing financial interests exist.
References
- 1.Edwards BK. Brown ML. Wingo PA, et al. Annual report to the nation on the status of cancer, 1975–2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005;97:1407–1427. doi: 10.1093/jnci/dji289. [DOI] [PubMed] [Google Scholar]
- 2.Blanks RG. Moss SM. McGahan CE. Quinn MJ. Babb PJ. Effect of NHS breast screening programme on mortality from breast cancer in England and Wales, 1990–8: Comparison of observed with predicted mortality. BMJ. 2000;321:665–669. doi: 10.1136/bmj.321.7262.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley CJ. Given CW. Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer inst. 2002;94:490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 4.Urban N. Anderson GL. Peacock S. Mammography screening: How important is cost as a barrier to use? Am J Public Health. 1994;84:50–55. doi: 10.2105/ajph.84.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taplin SH. Barlow WE. Ludman E, et al. Testing reminder and motivational telephone calls to increase screening mammography: A randomized study. J Natl Cancer Inst. 2000;92:233–242. doi: 10.1093/jnci/92.3.233. [DOI] [PubMed] [Google Scholar]
- 6.Klassen AC. Smith AL. Meissner HI. Zabora J. Curbow B. Mandelblatt J. If we gave away mammograms, who would get them? A neighborhood evaluation of a no-cost breast cancer screening program. Prev Med. 2002;34:13–21. doi: 10.1006/pmed.2001.0956. [DOI] [PubMed] [Google Scholar]
- 7.Taplin SH. Ichikawa L. Yood MU, et al. Reason for late-stage breast cancer: Absence of screening or detection, or breakdown in follow-up? J Natl Cancer Inst. 2004;96:1518–1527. doi: 10.1093/jnci/djh284. [DOI] [PubMed] [Google Scholar]
- 8.Legler J. Meissner HI. Coyne C. Breen N. Chollette V. Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11:59–71. [PubMed] [Google Scholar]
- 9.Stone EG. Morton SC. Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: A meta-analysis. Ann Intern Med. 2002;136:641–651. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 10.Vernon SW. Tiro JA. Meissner HI. Behavioral research in cancer screening. In: Miller S, editor; Bowen D, editor; Croyle R, editor; Rowland J, editor. Handbook of behavioral science and cancer. American Psychological Association: In press; [Google Scholar]
- 11.U.S. Census Bureau. Poverty thresholds: 1995. U.S. Bureau of the Census. Current population survey. www.census.gov/hhes/www/poverty/threshld/thresh95.html. [Feb 29;2008 ]. www.census.gov/hhes/www/poverty/threshld/thresh95.html
- 12.Baron RM. Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 13.Tarver-Carr ME. Powe NR. Eberhardt MS, et al. Excess risk of chronic kidney disease among African-American versus white subjects in the United States: A population-based study of potential explanatory factors. J Am Soc Nephrol. 2002;13:2363–2370. doi: 10.1097/01.asn.0000026493.18542.6a. [DOI] [PubMed] [Google Scholar]
- 14.Buist DSM. Porter PL. Lehman C. Taplin SH. White E. Factors contributing to mammography failure in women aged 40–49 years. J Natl Cancer Inst. 2004;96:1432–1440. doi: 10.1093/jnci/djh269. [DOI] [PubMed] [Google Scholar]
- 15.Greenland S. Introduction to regression modeling. In: Rothman K, editor; Greenland S, editor. Modern epidemiology. Philadelphia: Lippincott-Raven; 1998. pp. 401–434. [Google Scholar]
- 16.2001 National Health Interview Survey (NHIS) Public use data release. Hyattsville, MD: U.S. Department of Health and Human Services; 2003. [Google Scholar]
- 17.Ludman EJ. Curry SJ. Meyer D. Taplin SH. Implementation of outreach telephone counseling to promote mammography participation. Health Educ Behav. 1999;26:689–702. doi: 10.1177/109019819902600509. [DOI] [PubMed] [Google Scholar]
- 18.Lawson HW. Henson R. Bobo JK. Kaeser MK. Implementing recommendations for the early detection of breast and cervical cancer among low-income women. Oncology. 2000;14:1528–1530. [PubMed] [Google Scholar]
- 19.Moon M. The Henry J. Kaiser Family Foundation; Menlo Park, CA: 2002. Medicare beneficiaries and their assets: Implications for low-income programs. [Google Scholar]
- 20.Zhu K. Hunter S. Bernard LJ. Payne-Wilks K. Roland CL. Levine RS. Mammography screening in single older African-American women: A study of related factors. Ethnicity Dis. 2000;10:395–405. [PubMed] [Google Scholar]
- 21.Andersen MR. Yasui Y. Meischke H. Kuniyuki A. Etzioni R. Urban N. The effectiveness of mammography promotion by volunteers in rural communities. Am J Prev Med. 2000;18:199–207. doi: 10.1016/s0749-3797(99)00161-0. [DOI] [PubMed] [Google Scholar]
- 22.Danigelis NL. Ashley JA. Worden JK. Dorwaldt AL. Roberson NL. Two community outreach strategies to increase breast cancer screening among low-income women. J Cancer Educ. 2001;16:55–58. doi: 10.1080/08858190109528726. [DOI] [PubMed] [Google Scholar]
- 23.Halliday T. Taira DA. Davis J. Chan H. Socioeconomic disparities in breast cancer screening in Hawaii. Prev Chronic Dis. 2007;4:A91. [PMC free article] [PubMed] [Google Scholar]
- 24.Wardle J. McCaffery K. Nadel M. Atkin W. Socioeconomic differences in cancer screening participation: Comparing cognitive and psychosocial explanations. Soc Sci Med. 2004;59:249–261. doi: 10.1016/j.socscimed.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 25.Bastani R. Maxwell AE. Bradford C. Cross-sectional versus prospective predictors of screening mammography. Cancer Epidemiol Biomarkers Prev. 1996;5:845–848. [PubMed] [Google Scholar]
- 26.Vernon SW. Briss PA. Tiro JA. Warnecke RB. Some methodologic lessons learned from cancer screening research. Cancer. 2004;101(Suppl 5):1131–1145. doi: 10.1002/cncr.20513. [DOI] [PubMed] [Google Scholar]