Abstract
A recombinant botulinum vaccine (rBV A/B) is being developed for protection against inhalational intoxication with botulinum neurotoxin (BoNT) complex serotype A, subtype A1 (BoNT/A1), and BoNT serotype B, subtype B1 (BoNT/B1). A critical component for evaluating rBV A/B efficacy will be the use of animal models in which the pathophysiology and dose-response relationships following aerosol exposure to well-characterized BoNT are thoroughly understood and documented. This study was designed to estimate inhaled 50% lethal doses (LD50) and to estimate 50% lethal exposure concentrations relative to time (LCt50) in rhesus macaques exposed to well-characterized BoNT/A1 and BoNT/B1. During the course of this study, clinical observations, body weights, clinical hematology results, clinical chemistry results, circulating neurotoxin levels, and telemetric parameters were documented to aid in the understanding of disease progression. The inhaled LD50 and LCt50 for BoNT/A1 and BoNT/B1 in rhesus macaques were determined using well-characterized challenge material. Clinical observations were consistent with the recognized pattern of botulism disease progression. A dose response was demonstrated with regard to the onset of these clinical signs for both BoNT/A1 and BoNT/B1. Dose-related changes in physiologic parameters measured by telemetry were also observed. In contrast, notable changes in body weight, hematology, and clinical chemistry parameters were not observed. Circulating levels of BoNT/B1 were detected in animals exposed to the highest levels of BoNT/B1; however, BoNT/A1 was not detected in the circulation at any aerosol exposure level. The rhesus macaque aerosol challenge model will be used for future evaluations of rBV A/B efficacy against inhalational BoNT/A1 and BoNT/B1 intoxication.
Botulinum neurotoxins (BoNTs) produced by the bacterium Clostridium botulinum and related clostridial species are the causative agents of the human disease botulism (7). Approximately 145 cases of naturally occurring botulism are reported in the United States each year. Infant botulism accounts for more than 50% of the cases, with food-borne and wound botulism making up the balance (9). The Centers for Disease Control and Prevention (CDC) consider BoNTs to be a serious potential threat and have listed them as a category A threat, a highest-risk threat agent for bioterrorism (8). Use of these BoNTs offensively could potentially result in catastrophic consequences to the nation. Aerosol dissemination represents the most likely method for the use of BoNT as a biological weapon (2).
Treatment of botulism is largely supportive, and any medical care must be initiated quickly to be effective. Current therapies include supportive intensive care (with ventilation) and treatment with antitoxin (2). A licensed vaccine is not currently available to provide protection against botulism. An investigational pentavalent vaccine (pentavalent botulinum toxoid vaccine [PBT]) that induces neutralizing antibodies against BoNT serotypes A, B, C, D, and E has been available for use in “at-risk” laboratory workers for 30 years (21).
A new-generation recombinant botulinum vaccine (rBV A/B) is being developed to prevent fatal botulism following exposure to aerosolized botulinum neurotoxin complex serotype A, subtype A1 (BoNT/A1) and serotype B, subtype B1 (BoNT/B1). The component antigens of rBV A/B, developed by the U.S. Army Medical Research Institute for Infectious Diseases (5), are identified as antigen A and antigen B and were derived from the nontoxic 50-kDa C-terminal domains of BoNT/A1 and BoNT/B1, respectively. The efficacy of rBV A/B cannot be determined directly in humans because the incidence of botulism in the general population is extremely low and direct-challenge studies in humans are unethical. Therefore, rBV A/B efficacy will be evaluated according to the animal rule of U.S. law (9a).
Evaluation of rBV A/B efficacy according to the animal rule requires the development and use of relevant animal models. Draft guidelines describing essential elements of animal models required to address efficacy under the animal rule were made available by the FDA in 2009 (6). Animal studies under the animal rule require a thorough understanding of the pathophysiological mechanism of the pathogenic agent and demonstration of similarities to known aspects of human disease. The challenge agent used for animal studies should be identical to the etiologic agent that causes the human disease, and the purity of the challenge preparation should be documented to the extent possible. Evaluation of efficacy in animal models will use a route of exposure to the etiological agent that is the same as the anticipated human exposure route. Reliable quantification and reproducibility of the challenge dose should be demonstrated. Acceptance of the animal model for evaluation of rBV A/B efficacy involves the performance of well-controlled, well-documented studies which incorporate these requirements.
The rhesus macaque was selected based upon its historic use for evaluation of investigational vaccines and antitoxin therapeutics (4, 13, 14, 18, 20). Available nonclinical data suggest that the pathophysiological response to aerosol exposure in rhesus macaques is relevant to the human disease. Clinical signs in rhesus macaques exposed to aerosolized BoNT/A or BoNT/B include mild muscular weakness, intermittent ptosis, severe weakness of postural muscles of the neck, occasional mouth breathing, serous nasal discharge, salivation, dysphagia, rales, anorexia, severe weakness, and lateral recumbency (4, 13).
The use of well-characterized challenge material is important for maintaining consistency among studies. The diversity of neurotoxin-producing C. botulinum strains has become well recognized, and the quality of BoNT preparations produced by different production facilities varies. Therefore, stocks of well-characterized BoNT/A1 and BoNT/B1 were established for use in the rhesus macaque model development study and all future rBV A/B efficacy studies.
The following study was designed to establish the rhesus macaque BoNT/A1 and BoNT/B1 aerosol challenge models for use in future rBV A/B efficacy studies. The lethality of well-characterized BoNT/A1 and BoNT/B1 challenge material administered by the inhalational route of exposure was evaluated in rhesus macaques. In addition, clinical signs of disease were assessed through clinical observations, body weight measurements, clinical hematology, clinical chemistry, and telemetric monitoring to aid in the understanding of botulism disease progression. The relationships of the estimated total inhaled BoNT/A1 and BoNT/B1 dosages and circulating BoNT/A1 and BoNT/B1 levels to disease progression were also evaluated.
MATERIALS AND METHODS
Animals.
General procedures for animal care and housing were in accordance with the Guide for the Care and Use of Laboratory Animals (17), and studies were conducted under protocols approved by the Battelle Laboratory Animal Care and Use Committee. Forty (20 male and 20 female) rhesus macaques (Macaca mulatta) that were approximately 4.0 to 10.0 kg at randomization were used for this study (three extra monkeys were available for replacement purposes). Only monkeys that were in good health, were free of malformations, and exhibited no signs of clinical disease were placed in the study. Monkeys were prescreened prior to arrival to determine that they were seronegative for simian immunodeficiency virus (SIV), simian T-lymphotrophic virus type 1 (STLV-1), simian retrovirus (SRV), and Cercopithecine herpesvirus 1 (herpes B virus). All monkeys had three consecutive negative tuberculin tests (performed during their quarantine period). Additionally, upon arrival, mouse (toxin) neutralization assays (MNA) were performed to test for the presence of neutralizing antibodies to both BoNT/A1 and BoNT/B1. Undiluted serum samples from each monkey were mixed 1:1 with a solution containing BoNT/A1 or BoNT/B1 and incubated at room temperature for 60 to 120 min. The mixture was then injected intraperitoneally (i.p.) into four mice, and lethality was measured over 96 h (±2 h). Groups of control mice were injected with the BoNT/A1 or BoNT/B1 solution diluted 1:1 with phosphate-buffered saline containing 0.2% gelatin to confirm that the challenge mixture produced full lethality. A sample was considered negative for the presence of BoNT-neutralizing antibodies when at least 75% mortality was demonstrated in the test sample group. All monkeys tested negative for the presence of neutralizing antibodies to both BoNT/A1 and BoNT/B1. Male CD-1 (ICR) mice (Mus musculus), approximately 4 to 5 weeks of age, were used for the study to determine BoNTA/1 and BoNT/B1 concentrations using a mouse potency assay. All mice were supplied by Charles River. Only healthy mice weighing between 18 and 22 g were placed in the study.
Challenge material.
The complex form of BoNT/A1 (lot A071006-01) and BoNT/B1 (lot B071006-01) challenge materials were purchased from Metabiologics (Madison, WI). The BoNT/A1 was produced from the C. botulinum Hall strain. The BoNT/B1 was produced from the C. botulinum Okra strain. The 16S rRNA and neurotoxin progenitor complex gene sequences of DNA extracted from the Metabiologics Hall and Okra strains were analyzed to verify strain identity and BoNT serotype and subtype. Serospecificity was evaluated based on the ability of serotype-specific antitoxin reference standards for BoNTs A, B, C, D, E, F, and G to neutralize the activity of BoNT/A1 and BoNT/B1. Briefly, the BoNT/A1 and BoNT/B1 were diluted to a standard concentration of 100 50% mouse intraperitoneal lethal doses (MIPLD50)/ml and added in 1.5-ml volumes to each of seven appropriately labeled vials that contained 1.5 ml of one of seven (A to G) antitoxin standards at a concentration of 2 U/ml. The mixture (for each vial) was injected i.p. at a volume of 0.5 ml into one group of 4 mice. The serospecificity of the BoNT/A1 and BoNT/B1 was confirmed by demonstrating that 75 to 100% of the mice were protected when the BoNT was mixed with the corresponding antitoxin and that protection was not observed when the BoNT was mixed with noncognate antitoxin. Western blotting was also performed to confirm the identity of the BoNT serotype using the appropriate specific antibodies. Sodium dodecyl sulfate-polyacrylamide gel electrophoresis and size exclusion chromatography were used as qualitative indicators of the purity of the BoNT/A1 and BoNT/B1. Protein concentration and biological activity (in terms of the MIPLD50 units) of both BoNTs were verified using the micro-Bradford protein assay and mouse (toxin) potency assay, respectively. The specific potencies of the BoNT/A1 and BoNT/B1 challenge materials were 3.2 × 107 and 7.5 × 107 MIPLD50 units/mg protein, respectively. Upon completion of these analyses, the BoNT/A1 and BoNT/B1 materials were aliquoted into single-use vials and stored at −70°C ± 10°C.
Aerosol challenge.
A head-only aerosol exposure system was utilized to deliver the target BoNT aerosol doses. The aerosol exposure system contained (i) a Collison nebulizer for generation of aerosols, (ii) glass impinger samplers used to collect aerosol samples for determination of aerosolized BoNT concentrations, (iii) an aerosol particle size analyzer, (iv) temperature and humidity monitors, and (v) mass flow meters (MFM) and mass flow controllers (MFC) to monitor and control the aerosol flows.
Monkeys were anesthetized with Telazol (1 to 6 mg/kg of body weight) and placed into a plethysmograph in a class III hood line. Body plethysmography was performed in real time on each monkey during challenge to measure respiratory parameters, including tidal volume, total accumulated tidal volume, and minute volume. The atmospheric concentration of BoNT in the exposure chamber was controlled by varying the starting BoNT concentration in the nebulizer. Real-time verification of the aerosol concentrations of BoNT in the exposure chamber was not possible. Performance characteristics of the head-only aerosol exposure system were established prior to challenging animals. These characteristics were used to estimate the BoNT concentrations in the exposure chamber and to determine the total volume of air that the animal needed to inspire to achieve a targeted exposure dosage. Exposure duration was based on the time required for each animal to achieve the designated volume of inspired air measured by real-time plethysmography. Actual aerosol concentrations of BoNT achieved were verified postexposure. The estimated inhaled dose was calculated using the actual BoNT aerosol concentration and the total accumulated tidal volume of air inhaled by monkeys during exposure.
A stage-wise or phased approach was used to estimate inhaled 50% lethal doses (LD50) and to estimate 50% lethal exposure concentrations relative to time (LCt50) for BoNT/A1 and BoNT/B1. Four stages were required for this study. Each stage consisted of a prechallenge period (minimum of 7 days) and a postchallenge period, which extended to day 30. Target challenge doses for the first stage were based on previously published estimates of the inhalational LD50 for rhesus macaques (15): inhalational LD50 of 350 MIPLD50/kg and 7,500 MIPLD50/kg for BoNT/A and BoNT/B, respectively. In the first stage for each BoNT, four groups of two animals (one male and one female per group) were challenged with four target challenge doses ranging from 37.5 to 3,750 MIPLD50/kg and 750 to 75,000 MIPLD50/kg for BoNT/A1 and BoNT/B1, respectively. On each challenge day (defined as study day 0), monkeys were challenged in ascending order so that monkeys receiving the lowest target exposure doses were challenged first while the monkeys receiving the highest target exposure doses were challenged last. At the conclusion of each stage, mortality results were analyzed and target exposure doses for the next stage determined.
Determination of BoNT concentrations.
Mouse (toxin) potency assays were performed to determine the BoNT concentrations in the nebulizer and impinger samples. A dilution range encompassing six concentrations at five mice per concentration using an approximately 2-fold to 3-fold dilution factor was utilized, with the dilutions centered around an estimated MIPLD50 value for each sample (based on expected starting concentration and percent recovery). Diluted samples from each impinger or nebulizer were injected into mice intraperitoneally (i.p.). Lethality was recorded for 96 ± 2 h after challenge. Probit analyses were used to calculate the LD50 and corresponding BoNT concentration in MIPLD50 units per ml. The BoNT concentrations (MIPLD50/ml) of impinger samples were used to determine BoNT aerosol concentrations within the exposure chamber.
Clinical observations.
Monkeys were monitored twice daily by trained animal care technicians or a veterinarian during their prechallenge period. Following challenge, clinical observations occurred three times a day (during normal working hours) for 30 days postchallenge or until time of death. Additional clinical observations were initiated every 6 h for six consecutive days (for each phase) based on the onset of illness in the first monkey. Preestablished criteria for euthanasia of animals included decreased body temperature to <93.0°F, >20% loss of body weight from prechallenge weight, respiratory distress/failure, significant reduction in activity (e.g., unable to right itself, complete lack of activity, persistent prostration, or total paralysis), or signs of pneumonia. All monkeys meeting any of the above criteria or judged to be terminally ill by the veterinary staff were euthanized with an overdose of a euthanasia agent containing pentobarbital.
Body weight.
Monkeys were weighed prior to challenge on study day 0 and at least every 3 days until death/euthanasia or until the end of the postchallenge period (day 30).
Hematology and clinical chemistry.
Blood samples were collected from unanesthetized animals from a femoral artery or vein prior to challenge on study day 0 and at 7, 14, 21, and 30 days postchallenge. A terminal blood sample was also collected prior to euthanasia of moribund animals. Blood was collected in EDTA tubes for hematology and in serum separator tubes (SST) for clinical chemistry. Table 1 lists the hematology and clinical chemistry parameters evaluated during the study.
TABLE 1.
Hematology, clinical chemistry, and telemetry parameters
| Hematology parameter | Clinical chemistry parameter | Telemetry parameter |
|---|---|---|
| White blood cell count | Alanine aminotransferase level | Temp |
| Red blood cell count | Aspartate aminotransferase level | Activity |
| Hemoglobin level | Alkaline phosphatase level | Diastolic pressure |
| Hematocrit | Lactate dehydrogenase level | Systolic pressure |
| Mean corpuscular vol | Blood urea nitrogen level | Mean pressure |
| Mean corpuscular hemoglobin level | Creatinine level | Pulse pressure |
| Mean corpuscular hemoglobin concn | Bun/creatinine ratio | Heart rate |
| Red cell distribution width | Albumin/globulin ratio | QA interval |
| Platelet count | Albumin level | Respiratory expiratory time |
| Mean platelet vol | Calcium level | Respiratory inspiratory time |
| Neutrophil count | Chloride level | Respiratory pressure integral |
| Lymphocyte count | Creatinine kinase level | Respiratory pressure peak amplitude |
| Monocyte count | Globulin level | Respiratory rate |
| Eosinophil count | Glucose level | ECG result |
| Basophil count | Phosphorus level | |
| Neutrophil/lymphocyte ratio | Potassium level | |
| Sodium level | ||
| Total protein level | ||
| Amylase level |
Telemetry.
Monkeys were surgically implanted with telemetry units (D70-PCTP transmitters; Data Sciences International) prior to placement in the study. Each D70-PCTP transmitter contained two pressure leads and one bio-potential lead. The transmitter body was inserted into the abdomen and attached to the wall of the abdominal cavity. The cardiac pressure catheter was inserted into the femoral artery and advanced into the iliac artery, where it was fixed into place. The pleura pressure catheter was implanted beneath the serosal layer of the esophagus within the thoracic cavity. The electrocardiogram (ECG) leads were placed against the abdominal muscle along the rib cage below the apex of the heart and against the thoracic wall. The implantation procedure was performed at least 5 weeks prior to aerosol challenge to ensure that the animals had completely recovered from the implantation surgery at the time of challenge. A baseline prechallenge telemetric monitoring period was initiated a minimum of 7 days prior to challenge. After challenge, telemetric monitoring occurred for 30 s every 15 min. Transmitters (surgically implanted in monkeys), receivers (equipped on each cage), consolidation matrices, cabling, and computers utilizing the Dataquest A.R.T. data acquisition and analysis software are all components of the PhysioTel telemetry system. The Dataquest A.R.T. telemetry software was used to collect the telemetry parameters listed in Table 1.
Evaluation of circulating BoNT levels.
To assess circulating BoNT levels, blood samples were collected from unanesthetized animals in SST prior to challenge and at 2 h, 5 h, 7 h, 1 day, 2 days, 7 days, and 14 days postchallenge and in terminal blood samples collected from moribund animals. All blood collection volumes were within IACUC-approved limits based on the size of the animals used in the study. If BoNT was not detected at the day 1 and 2 time points, collection of samples and evaluation of BoNT levels were discontinued. Serum samples prepared from the blood were injected into four naïve CD-1 male mice with 0.5 ml of undiluted serum injected into each mouse. Samples were considered to be positive for BoNT if all four mice died within 96 h of injection. The lower limit of detection using this qualitative approach was 2 MIPLD50/ml of serum.
Necropsy and histopathology.
Gross necropsies were performed on all monkeys that did not survive challenge. The following tissues were collected during necropsy, preserved, and processed for histopathological evaluation: adrenal glands, aorta, bone marrow (sternum), brain, esophagus, eyes, heart, large intestine (cecum, colon, and rectum), kidneys, liver, lungs with main-stem bronchi and mediastinal lymph nodes, lymph nodes (bronchial, mandibular, and mesenteric), mammary glands, optic nerves, ovaries (females), pancreas, pituitary, prostate (males), mandibular salivary glands, sciatic nerve, skeletal muscle, small intestine (duodenum, jejunum, and ileum), spinal cord (cervical, thoracic, and lumbar), spleen, stomach, testes with epididymides (male), trachea, thymus, thyroid and parathyroid, urinary bladder, and uterus with cervix (females). All abnormalities and gross lesions were also sampled. These tissues were processed on ∼5-μm slides and stained with hematoxylin and eosin (H&E) stain for microscopic examination. All microscopic slides were examined by a board-certified veterinary pathologist.
Statistical methods.
All statistical analyses were performed using SAS (version 9.1) procedures. Dose-lethality data from BoNT/A1 and BoNT/B1 were modeled separately using the probit model (12). The inhaled LD50 and inhaled LD90 were expressed per kg of body weight (MIPLD50/kg), and the LCt50 and LCt90 were based on the exposure concentration (MIPLD50·min/liter). The exposure concentration was defined as the aerosol concentration (MIPLD50/liter) multiplied by the time (in minutes) that animals were exposed to the neurotoxin. The LCt50 calculated in this way represents the aerosol exposure concentration that, if breathed by animals for 1 min, would result in approximately 50% lethality.
To evaluate the influence of the challenge dose on the pathophysiological response, animals were grouped into three challenge dose groups: low, middle, and high for each BoNT/A1 and BoNT/B1 group, based on the actual challenge dose and survival data. For BoNT/A1, all animals with challenge doses from 14 to 110 MIPLD50/kg, all of which survived, were assigned to the low-dose group. All animals with challenge doses above 1,200 MIPLD50/kg, all of which died, were assigned to the high-dose group. The remaining animals were assigned to the middle-dose group and included both survivors and dead animals. Similarly, for BoNT/B1, all animals with challenge doses from 676 to 2,014 MIPLD50/kg, all of which survived, were assigned to the low-dose group. All animals with challenge doses above 93,000 MIPLD50/kg, all of which died, were assigned to the high-dose group. The remaining animals were assigned to the middle-dose group and included both survivors and dead animals.
For clinical chemistry and hematology results, an analysis of variance (ANOVA) model was fitted to the baseline data for each parameter and BoNT to determine if there were statistically significant differences among the challenge group levels at baseline. Additional ANOVA models were fitted to the change-from-baseline data to determine whether there were statistically significant differences among the challenge groups at study days 7, 14, 21, and 30. These models were fitted separately for each neurotoxin, for each clinical chemistry or hematology parameter, and for each study day, before and after outliers were excluded.
Statistical analyses of telemetry data were performed on baseline-adjusted hourly postchallenge data. Baseline-adjusted hourly postchallenge values were calculated as follows. First, values averaged hourly for 24 h were calculated (over 7 days) for the prechallenge baseline data for each animal. Then, daily hourly averages (24 h per day for 30 study days or until death) for the postchallenge data were calculated for each animal. Finally, for each animal, the baseline-adjusted hourly postchallenge value at each postchallenge hour was calculated by subtracting the baseline average value from the postchallenge average value at that hour. Preliminary analyses suggested that significant responses occurred in seven parameters: diastolic pressure, systolic pressure, mean pressure, pulse pressure, heart rate, QA interval (the difference between the time of detection of the Q point of the ECG complex and the time of diastole on the blood pressure waveform), body temperature, and heart rate. Baseline data analysis was performed on the values averaged hourly for 24 h for the seven telemetry parameters, separately for BoNT/A1 and BoNT/B1, to assess whether any significant differences existed between the animal groups prior to challenge. The hourly baseline-adjusted postchallenge values for each parameter were then averaged over an 8-h interval, and the 8-hour averages were fitted to ANOVA models using the dose group and survival status (low-dose animals, middle-dose animals that survived, middle-dose animals that died, and high-dose animals) as a single main effect. For the 8-hour models, random animal and repeated-measurement effects were taken into account in the calculation.
RESULTS
Lethality.
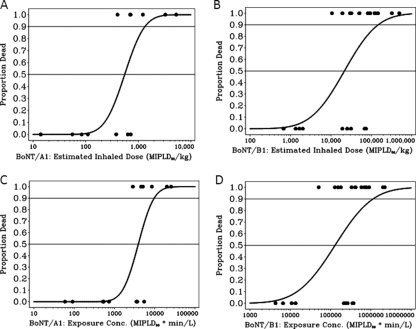
The estimated lethality of BoNT/A1 and BoNT/B1 based on inhaled dosage per kg of body weight and the exposure concentrations are shown in Table 2. The calculated inhaled LD50 for BoNT/A1 was 550 MIPLD50/kg, while the inhaled LD90 was calculated to be 1,330 MIPLD50/kg. The LCt50 for BoNT/A1 was estimated to be 3,910 MIPLD50·min/liter, while the LCt90 was estimated to be 9,680 MIPLD50·min/liter. For BoNT/B1, the calculated inhaled LD50 was 21,600 MIPLD50/kg, while the inhaled LD90 was calculated to be 148,000 MIPLD50/kg. The LCt50 for BoNT/B1 was estimated to be 129,000 MIPLD50·min/liter, while the LCt90 was estimated to be 1,137,000 MIPLD50·min/liter. Figure 1 shows the probit dose lethality curves for both BoNT/A1 and BoNT/B1 based on the estimated inhaled doses and exposure concentrations. Table 3 shows the lethality and times to death for both BoNT/A1 and BoNT/B1 challenge dose groups. Regression models for time to death demonstrated a significant exposure dosage effect (P < 0.001) for both BoNTs. Regression slopes were significantly negative, indicating that as the exposure concentration increased, the time to death decreased. The estimated inhaled doses and mortality results for BoNT/A1 and BoNT/B1 for individual animals used in the study are included in the supplemental materials (Table S1).
TABLE 2.
Estimates of 50th and 90th percentiles for lethality based on estimated inhaled dose and exposure concentration
| Neurotoxin | Estimated inhaled dose |
Exposure concn |
||||||
|---|---|---|---|---|---|---|---|---|
| 50th percentile (MIPLD50/kg) |
90th percentile (MIPLD50/kg) |
50th percentile (MIPLD50·min/liter) |
90th percentile (MIPLD50·min/liter) |
|||||
| LD50 | Confidence intervalsa | LD90 | Confidence intervalsa | LCt50 | Confidence intervalsa | LCt90 | Confidence intervalsa | |
| BoNT/A1 | 550 | (280, 1,080) | 1,330 | (350, 5,060) | 3,910 | 1,980, 7,710 | 9,680 | 2,620, 35,740 |
| BoNT/B1 | 21,600 | (600, 62,700) | 148,000 | (54,000, 6 × 108) | 129,000 | 2,000, 419,000 | 1,137,000 | 368,000, 5 × 1010 |
Delta-type 95% confidence intervals for BoNT/A1; Fieller's 95% confidence intervals for BoNT/B1.
FIG. 1.
Dose lethality curves, with estimated inhaled doses and exposure concentrations. Shown are dose lethality curves for BoNT/A1 and BoNT/B1 based on the estimated inhaled dose in MIPLD50/kg (A and B) and exposure concentration in MIPLD50·min/liter (C and D). Estimated inhaled dose was calculated by multiplying the aerosol concentration (MIPLD50/liter) by the total volume (liter) of air breathed during exposure divided by body weight (kg). Exposure concentration was defined as the aerosol concentration (MIPLD50/liter) multiplied by the exposure time (in minutes) that animals were exposed to the neurotoxin. The LCt50 calculated in this way represents the aerosol exposure concentration that when breathed by animals for 1 min results in approximately 50% lethality. There was a statistically significant dose-response relationship (at the 0.05 level) for an inhaled dose of BoNT/B1 (P = 0.0206), but it was not significant for BoNT/A1 (P = 0.1718). The dose-response relationship (at the 0.05 level of significance) for exposure concentration times time was statistically significant for BoNT/B1 (P = 0.0231) but not for BoNT/A1 (P = 0.1577).
TABLE 3.
Lethality rates and mean times to death for animals that died
| Neurotoxin | Dose group(s) | No. dead/ total no. of animals | % dead | Mean time to death (h)a |
|---|---|---|---|---|
| BoNT/A1 | All | 8/18 | 44 | 125.8 ± 66.7 (58.8-241.5) |
| Low | 0/5 | 0 | ||
| Middle | 3/6 | 50 | 195.4 ± 56.8 (131.9-241.5) | |
| High | 3/3 | 100 | 85.1 ± 12.7 (70.5-93.4) | |
| BoNT/B1 | All | 13/22 | 59 | 58.4 ± 37.7 (19.7-148.1) |
| Low | 0/4 | 0 | ||
| Middle | 7/12 | 58 | 82.0 ± 37.4 (23.7-148.1) | |
| High | 6/6 | 100 | 30.9 ± 7.0 (19.7-40.7) |
Mean ± standard deviation (range).
Body weight.
Monkeys that died following BoNT challenge typically demonstrated a decrease in body weight compared to prechallenge weights. Overall, body weights collected for monkeys surviving BoNT/A1 and BoNT/B1 exposure varied postchallenge, with most of the weights fluctuating approximately ±0.6 kg from the corresponding monkeys prechallenge.
Clinical observations.
The most common clinical observations postchallenge were anorexia, lethargy, ataxia, labored respiration, dysphagia, ptosis, nasal discharge, paresis, coughing, mouth breathing, and lateral recumbency. For monkeys challenged with low doses of either BoNT/A1 or BoNT/B1, the only abnormal clinical observation made postchallenge was anorexia. Monkeys challenged with middle doses of BoNT/A1 and BoNT/B1 that survived were also observed as anorexic, and in this group anorexia was observed more frequently than in low-dose-challenged animals. Abnormal clinical signs, including ataxia, dysphagia, coughing, and lethargy, were also observed more frequently in middle-dose monkeys that survived than in low-dose monkeys. Additional abnormal clinical observations (other than anorexia) were documented in middle-dose animals that died, including labored respiration, lethargy, coughing, and dysphagia. In monkeys challenged with a high dose of BoNT/A1 or BoNT/B1, similar abnormal clinical signs were observed; however, these signs were observed much earlier and did not persist, as the monkeys died rapidly upon onset of these signs. Table S2 in the supplemental material provides a complete listing of the numbers and percentages of animals that showed clinical signs for BoNT/A1 and BoNT/B1.
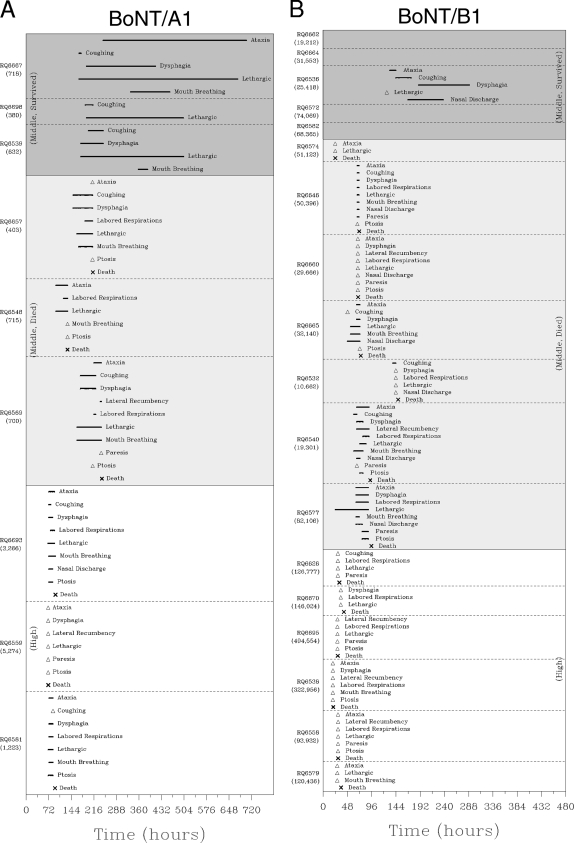
The persistence and times to the onset of each of the clinical signs were recorded until the death, moribund sacrifice, or end of the clinical observation period of the animal. The times to onset of clinical signs were calculated as the difference between the time at which the sign was first observed and the time at which the challenge dose was administered. In the low-dose group, anorexia (the only abnormal sign displayed) was first observed 20 to 40 h after challenge with either BoNT/A1 or BoNT/B1. Anorexia was noted intermittently throughout the postchallenge period and varied from monkey to monkey. For middle-dose-BoNT/A1-challenged monkeys that survived (Fig. 2A), signs other than anorexia (ataxia, dysphagia, coughing, and lethargy) were first observed around 160 h postchallenge. These signs persisted for 8 to 12 days postchallenge. Only one middle-dose-BoNT/B1-challenged monkey that survived showed signs other than anorexia (Fig. 2B). In this monkey, lethargy, ataxia, coughing, nasal discharge, and dysphagia were first observed at approximately 144 h postchallenge. These signs persisted until 5 days postchallenge.
FIG. 2.
Clinical observations. (A and B) Time courses of clinical observations in individual monkeys within the designated dose groups for BoNT/A1 and BoNT/B1, respectively. The upper shaded section of each panel shows clinical observations in middle-dose-group monkeys that survived. The middle, more lightly shaded section of each panel shows clinical observations in middle-dose-group monkeys that died. The bottom, unshaded section of each panel shows clinical observations of monkeys in the high-dose group. All monkeys in the high-dose group died. For BoNT/A1, the challenge dose range for the middle-dose group was 380 to 718 MIPLD50/kg and above 1,200 MIPLD50/kg for the high group. For BoNT/B1, the challenge dose range for the middle-dose group was 10,662 to 82,106 MIPLD50/kg and above 93,000 MIPLD50/kg for the high-dose group. The estimated inhaled dose in MIPLD50/kg for each animal is shown below the animal's identification number at the left of the panels. For other signs, the duration of clinical signs is displayed by a line segment beginning at the time at which the sign was first observed and ending at the time at which the sign was last observed. Anorexia is not shown. Anorexia was a common sign observed in all dose groups and was the only abnormal sign observed in low-dose-group animals. Anorexia was noted intermittently throughout the postchallenge period and varied from monkey to monkey.
For middle-dose-BoNT/A1-challenged monkeys that died, signs other than anorexia were first documented at approximately 96 h postchallenge (Fig. 2A), while these signs were observed much sooner in middle-dose-BoNT/B1 (Fig. 2B)-challenged monkeys, with all seven animals succumbing to disease by approximately 150 h. In monkeys challenged with a high dose of BoNT/A1, abnormal clinical signs were first documented approximately 72 h postchallenge, with all three monkeys in this group succumbing to disease by 96 h (Fig. 2A). In high-dose-BoNT/B1-challenged monkeys, abnormal signs were first observed around 18 h postchallenge (Fig. 2B). The time to death from the appearance of any clinical sign was faster in the high-dose group than in the middle-dose group for both BoNT/A1 and BoNT/B1 (Table 4). In general, BoNT/B1-challenged monkeys died faster upon onset of abnormal clinical signs than BoNT/A1-challenged monkeys.
TABLE 4.
Mean times to death from the onset of any clinical signa after BoNT/A1 and BoNT/B1 exposure for animals that died
| Dose group | Mean time to death from onset of any clinical sign (h) |
|
|---|---|---|
| BoNT/A1 (n = 18) | BoNT/B1 (n = 22) | |
| Middle (animals that died) | 59.4 ± 21.4 (36.5-78.9) | 20.5 ± 25.7 (0.0-71.1) |
| High | 15.1 ± 12.7 (0.6-23.9) | 3.0 ± 3.1 (0.0-7.5) |
Any clinical sign except anorexia. Values are means ± standard deviations (ranges).
Hematology and clinical chemistry.
The biological relevance of any statistically significant changes from baseline in hematological or clinical chemistry parameters was examined with regard to the magnitude and the persistence of the change. Parameters showing a statistically significant change from baseline that did not persist between time points and that had values within the normal range for that parameter were considered not biologically relevant. Based on these criteria, no biologically relevant changes in hematologic and clinical chemistry parameters were observed in monkeys exposed to either BoNT/A1 or BoNT/B1 in the low-, middle-, and high-challenge-dosage groups.
Telemetry.
A preliminary statistical analysis was performed on baseline-adjusted hourly postchallenge data for each of the 13 telemetry parameters (separately for BoNT/A1 and BoNT/B1). Preliminary analysis demonstrated statistically significant dose effects on diastolic pressure, systolic pressure, mean pressure, pulse pressure, heart rate, and QA interval for monkeys challenged with BoNT/B1 and statistically significant dose effects on body temperature and heart rate for monkeys challenged with BoNT/A1. Other telemetry parameters (activity, respiratory expiratory time, respiratory inspiratory time, respiratory pressure integral, respiratory pressure peak amplitude, respiratory rate) did not have a statistically significant dose effect for monkeys challenged with BoNT/A1 or BoNT/B1. Therefore, subsequent statistical analyses were performed only on seven telemetry parameters (mean pressure, diastolic pressure, systolic pressure, pulse pressure, body temperature, heart rate, and QA interval) that showed statistically significant dose effects for monkeys challenged with BoNT/A1 or BoNT/B1.
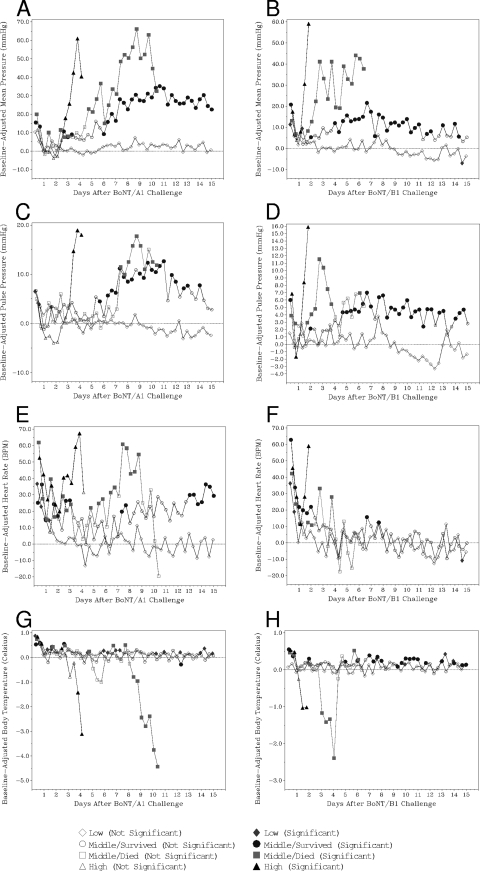
Similar patterns in the changes of mean pressure, diastolic pressure, and systolic pressure following aerosol exposure to BoNT/A1 and BoNT/B1 were observed by telemetry. Figure 3A and B show the baseline-adjusted mean pressure for the different dose groups for BoNT/A1- and BoNT/B1-challenged monkeys, respectively. Monkeys challenged with low doses of BoNT/A1 did not demonstrate any consistently significant change in mean pressure postchallenge. Within the middle-dose group for BoNT/A1, monkeys which eventually died demonstrated a consistently significant increase in mean pressure at approximately 112 h postchallenge, while monkeys that did not die following challenge had a slightly delayed response with a consistently significant increase from baseline at day 6 or 144 h postchallenge. The mean pressure for these middle-dose survivors returned to nonsignificant levels around day 22 postchallenge (data not shown). Monkeys challenged with a high dose of BoNT/A1 showed a significant increase in mean pressure over baseline levels at 64 h postchallenge. Monkeys challenged with a low dose of BoNT/B1 did not demonstrate any consistently significant change in mean pressure postchallenge. Within the middle-dose group for BoNT/B1, monkeys which eventually died demonstrated a consistently significant increase in mean pressure at approximately 40 h postchallenge, while monkeys that did not die following challenge had a delayed response with a consistently significant increase from baseline at day 4 postchallenge. The mean pressure for these middle-dose survivors returned to nonsignificant levels around day 13 postchallenge. Monkeys challenged with a high dose of BoNT/B1 showed a significant increase in mean pressure over baseline levels at 24 h postchallenge.
FIG. 3.
Telemetry. Effects of aerosol challenge with BoNT/A1 and BoNT/B1 on mean pressure (A and B), pulse pressure (C and D), heart rate (E and F), and temperature (G and H). The graphs show averages (for the parameter identified) within a dose group (low-dose monkeys, middle-dose monkeys that survived, middle-dose monkeys that died, and high-dose monkeys) over an 8-h interval. For example, a data point at day 2 (or 48 h) (below the graphs) actually represents the average for the corresponding dose group (low, middle, or high) between 41 and 48 h postchallenge. If the symbol is not filled in, then the value during that 8-h interval was not statistically different from the baseline value of that group. If the symbol is filled in, then the value for that 8-h interval is statistically different from baseline. The graphs depict the telemetry data (for the designated parameter) collected through day 15 postchallenge. In middle-dose animals that survived, parameters that were statistically different from baseline during the 15-day period shown returned to baseline before the end of the 30-day observation period.
Figures 3C and D show the baseline-adjusted pulse pressure for the different dose groups for BoNT/A1- and BoNT/B1-challenged monkeys, respectively. Monkeys challenged with a low dose of BoNT/A1 did not demonstrate any consistently significant change in pulse pressure postchallenge (Fig. 3C). Within the middle-dose-BoNT/A1 group, monkeys that survived challenge showed a consistently significant increase in pulse pressure from baseline early, at 152 h postchallenge. An increased pulse pressure was observed later (176 h postchallenge) in middle-dose monkeys that died; however, the change in pulse pressure appeared to be more rapid and of higher magnitude than in the monkeys that survived. The pulse pressure for these middle-dose survivors returned to nonsignificant levels around day 14 postchallenge. Monkeys challenged with a high dose of BoNT/A1 showed a significant increase in pulse pressure over baseline levels at 80 h postchallenge. Monkeys challenged with a low dose of BoNT/B1 did not demonstrate any consistently significant change in pulse pressure postchallenge. Within the middle-dose group for BoNT/B1, monkeys which eventually died demonstrated a consistently significant increase in pulse pressure at 40 h postchallenge, with the levels decreasing back down to nonsignificant levels around 88 h postchallenge. Monkeys that did not die following challenge with a middle dose of BoNT/B1 demonstrated a consistently significant increase from baseline at 112 h postchallenge. The pulse pressure for these middle-dose survivors returned to nonsignificant levels around day 18 postchallenge (data not shown). Monkeys challenged with a high dose of BoNT/B1 showed a significant increase in pulse pressure over baseline levels at 32 h postchallenge.
Figure 3E and F show the baseline-adjusted heart rate for the different dose groups for BoNT/A1- and BoNT/B1-challenged monkeys, respectively. All BoNT/A1 dose groups demonstrated increased heart rates immediately following challenge. Heart rates for low-dose monkeys returned to baseline levels around day 2, after which they did not show a significant change from baseline postchallenge. Heart rates for the middle-dose-BoNT/A1 group monkeys that died remained elevated until approximately 80 h postchallenge, returned to baseline briefly, increased again around 112 h, and remained elevated until 208 h postchallenge. After this point, heart rate decreased and fell below normal baseline levels. Monkeys in the middle-dose group that survived showed an overall increase in heart rate postchallenge, but this was not consistently significantly different from baseline until day 13 postchallenge. Heart rates for these monkeys returned to nonsignificant levels around day 18. Heart rates for monkeys challenged with a high dose of BoNT/A1 did not return to baseline levels postchallenge and increased dramatically approximately 56 h postchallenge. All BoNT/B1 dose groups demonstrated increased heart rates immediately following challenge. Except with the monkeys in the high-dose group, heart rates returned to baseline levels and were never consistently significantly different from baseline again. Monkeys in the high-dose group for BoNT/B1 showed a decrease in heart rate until 24 h postchallenge, after which heart rates dramatically increased.
Figure 3G and H show the baseline-adjusted temperature for the different dose groups for BoNT/A1- and BoNT/B1-challenged monkeys, respectively. Monkeys challenged with a low dose of BoNT/A1 did not demonstrate any consistently significant change in temperature postchallenge. Within the middle-dose group for BoNT/A1, monkeys that died demonstrated a consistently significant decrease in temperature at approximately 200 h postchallenge, while monkeys which survived in the middle-dose group never demonstrated a consistently significant difference in temperature from baseline to day 21 postchallenge. Monkeys challenged with a high dose of BoNT/A1 showed a significant decrease in temperature over baseline levels at 88 h postchallenge. Monkeys challenged with a low dose of BoNT/B1 did not demonstrate any consistently significant change in temperature postchallenge. Within the middle-dose group for BoNT/B1, monkeys that died demonstrated a significant decrease in temperature at approximately 72 h postchallenge and then returned to near-baseline values around 104 h. Monkeys that survived in the middle-dose group tended to have a significant increase in temperature postchallenge starting around day 7. Monkeys challenged with a high dose of BoNT/B1 showed a significant decrease in temperature over baseline levels at 32 h postchallenge.
The QA interval tended to decrease postchallenge in a dose-dependent manner following exposure to BoNT/A1 and BoNT/B1 (data not shown). However, because of the variability in this parameter, the decrease was not consistently significantly different from baselines. Monkeys in the middle-dose group (that died) and high-dose groups challenged with BoNT/A1 showed statistically significant decreases in expiratory time postchallenge (data not shown). Interestingly, a statistically significant decrease in expiratory time was not observed in monkeys in the middle-dose group (that died) and high-dose groups that were challenged with BoNT/B1. Monkeys in the middle group (that died) and high-dose groups challenged with BoNT/A1 demonstrated a significant increase in inspiratory time postchallenge. Again, this was not observed in BoNT/B1-challenged animals. All animals demonstrated an increase in heart rate within 4 h postchallenge (data not shown). This increase in heart rate, reflecting an increase in the rate of discharge of the sinoatrial node, can be associated with pain, with excitement, with stress, or with a direct effect on ion channels specific for sinoatrial nodal automaticity. The heart rate increase postchallenge appears to be directly related to the dose of BoNT administered. The heart rate remained elevated for extended periods of time within the middle- and high-dose groups of BoNT. The QA interval changes were attributable and inversely proportional to the heart rate changes. When the heart rate increased, the width of the QA interval decreased, demonstrating an increase in the rate of ventricular depolarization. Alternatively, when the heart rate returned to baseline, the QA interval correspondingly increased, demonstrating a decrease in the rate of ventricular depolarization.
Circulating BoNT levels.
Circulating neurotoxin was not observed in monkeys challenged with BoNT/A1. The highest challenge dosage administered for BoNT/A1 was 5,274 MIPLD50/kg. Circulating neurotoxin was not observed in monkeys given BoNT/B1 challenge doses less than 25,000 MIPLD50/kg. At challenge doses between 25,000 and 82,000 MIPLD50/kg that caused death, BoNT/B1 was first detected in the circulation 5 h after challenge. Three monkeys challenged within the 25,000- and 82,000-MIPLD50/kg range survived. These monkeys did not have detectable levels of BoNT/B1 in their circulation at any of the time points evaluated postchallenge. Monkeys challenged with BoNT/B1 at greater than 82,000 MIPLD50/kg had detectable levels of BoNT/B1 in their circulation 2 h after challenge. All monkeys with detectable levels of BoNT/B1 in their circulation died, but some monkeys that did not have detectable BoNT/B1 levels died. Regression analysis of the times to detection of circulating BoNT/B1 demonstrated a strong statistically significant dose effect (P < 0.0001). The regression slope was significantly negative (−1.60), indicating that as the inhaled dose increased, the time to detection of circulating BoNT/B1 decreased.
Necropsy and histopathology.
A pulmonary gross lesion interpreted to be secondary to BoNT/B1 exposure was observed in only one monkey. All other gross findings were considered to be incidental and unrelated to BoNT aerosol exposure. Microscopic pathology findings interpreted to be due to botulinum neurotoxin exposure included suppurative inflammation of the lungs and lymphoid depletion of the spleen. Pulmonary inflammation was characterized microscopically by accumulation of mostly polymorphonuclear leukocytes, with a few mononuclear cells, some fibrin, cellular detritus, and bacteria in alveoli or, less frequently, in bronchi/bronchioles. These microscopic alterations were minimal to mild in severity and interpreted to be compatible in appearance with aspiration pneumonia and to be due to paralysis/paresis of the muscles responsible for swallowing and prevention of food or stomach contents from entering the larynx and from finding their way to the lungs. Also noted in some monkeys with suppurative inflammation of the lungs were hemorrhage and/or infiltration of nearby lymph nodes by polymorphonuclear cells (bronchial, mediastinal, and/or mandibular lymph nodes). This was interpreted to be an extension of suppurative pulmonary inflammation. Pulmonary hemorrhage was also noted in one monkey with pulmonary suppurative inflammation; the hemorrhage was interpreted to be an inflammatory process in this monkey. Suppurative pulmonary inflammation was slightly more frequently found in males than in females (the incidence was 7/10 for males and 4/11 for females). Also noted was a slightly larger incidence of microscopic pulmonary suppurative inflammation in monkeys exposed to BoNT/A1 (6/10) than in monkeys exposed to BoNT/B1 (5/11). Whether these noted sex and serotype differences in the microscopic findings of this study have any larger significance is not clear.
Mild splenic lymphoid hyperplasia characterized by decreased germinal centers was also noted in a number of study monkeys of both sexes and exposed to both serotypes/subtypes and was interpreted to be stress related and therefore secondary to botulinum neurotoxin-induced paralysis/paresis. Other microscopic findings, such as minimal mononuclear cell infiltrations of heart and kidney, mineralization of the renal transitional epithelium, adrenal cortex, and/or ovaries, minimal-to-marked thymic atrophy characteristic of physiological age-related involution, an ovarian cyst, and mild splenic lymphoid hyperplasia, are all findings that frequently are noted incidentally in rhesus macaques. They were interpreted to be unrelated to botulinum neurotoxin exposure, as were those microscopic findings that corresponded to gross findings already discussed above. One monkey had minimal-to-moderate necrotizing vasculitis and/or minimal-to-moderate edema in the submucosa of the stomach and small and large intestines. These findings were interpreted to be due to acute intestinal infection or bacterial toxemia. Their relationship to BoNT exposure was uncertain.
DISCUSSION
A rhesus macaque BoNT aerosol challenge model which addresses essential requirements of the FDA animal rule has been developed to evaluate the efficacy of the rBV A/B vaccine. The inhaled LD50 and LCt50 for BoNT/A1 and BoNT/B1 in rhesus macaques were determined using well-characterized challenge material. Clinical observations were consistent with the recognized clinical pattern of botulism disease progression. A significant dose response was demonstrated with regard to the times to death and onset of clinical signs for both BoNT/A1 and BoNT/B1. Significant dose-related changes in physiologic parameters measured by telemetry were also observed. However, notable changes in body weight, hematology, and clinical chemistry parameters were not observed. Circulating levels of neurotoxin were detected in animals exposed to relatively high levels of BoNT/B1; however, BoNT/A1 was not detectable in the circulation at any aerosol exposure level. No differences in mortality, clinical observations, and telemetric parameters were observed between male and female monkeys exposed to either neurotoxin.
The stage-wise approach used to evaluate the lethality of aerosols containing BoNT/A1 or BoNT/B1 in rhesus macaques began with a small number of monkeys tested over a broad range of doses in the first phase. Doses for subsequent phases were selected based on the cumulative results of earlier phases. The phased approach is a compromise between a traditional “one-shot” study and the “up-down” design (10, 11). The goal of both the phased approach and the up-down design was to reduce the number of animals required for LD50 estimation, while still producing a good LD50 estimate. The phased approach limits the number of stages in comparison to the up-down design. The gains in efficiency (in terms of reducing the number of animals) are the greatest for small numbers of phases. The BoNT/A1 inhalation LD50 determined from this study was 550 MIPLD50/kg and is similar to the previously reported inhalational LD50 for botulinum neurotoxin serotype A of 350 MIPLD50/kg (15). Conversion of the inhaled BoNT/A1 LD50 to mass units based on the specific potency of the BoNT/A1 challenge material (32,000 MIPLD50/μg of protein) yields an inhaled LD50 of approximately 0.017 μg/kg body weight. Estimates of human lethality of serotype A neurotoxin by inhalation are within the range of 0.010 to 0.013 μg/kg body weight (2). The inhaled BoNT/B1 LD50 determined from this study was 21,600 MIPLD50/kg and is approximately three times higher than the 7,500 MIPLD50/kg previously reported (15). The confidence intervals determined from the current study overlap the 7,500-MIPLD50/kg inhaled-LD50 value. The mechanism responsible for the observed difference in the toxicities of BoNT/A1 and BoNT/B1 is unknown. Factors may include different levels of stability of BoNT/A1 and BoNT/B1 in the lung and different means of transport into the circulation. Further studies will be required to address this finding.
There was a statistically significant dose-response relationship for both the inhaled dose and LCt50 for BoNT/B1 but not for BoNT/A1. This is likely the result of the steepness of the slope for BoNT/A1 compared to the slope for BoNT/B1 (Fig. 1). Since the slope of the curve for BoNT/A1 is steep, the inhaled LD90 is only approximately 2.4 times greater than the inhaled LD50. The same is true for the LCt90 for BoNT/A1. However, the slope for BoNT/B1 is less steep, which results in the inhaled LD90 and LCt90 being 7 to 9 times greater than the inhaled LD50 and LCt50, respectively. As a result, a larger number of animals would be required to demonstrate a statistical difference between the inhaled LD50 and inhaled LD90 or the LCt50 and LCt90 for BoNT/A1.
All forms of botulism present with essentially the same clinical syndrome: symmetrical flaccid paralysis of the cranial nerves followed by a symmetrical descending flaccid paralysis of skeletal muscles (voluntary), with death attributed primarily to the paralysis of respiratory musculature. The rate of progression of these signs is proportional to the dose received (22).
At the molecular level, BoNT acts to block the exocytosis of acetylcholine at neuromuscular junctions (19), thus primarily affecting the somatic nervous system and skeletal muscle function. It typically does not cross the blood-brain barrier, so it leaves the preganglionic portion of the autonomic nervous system (ANS) relatively unscathed. There is evidence, however, of ANS dysfunction in some patients resulting in nonskeletal, muscle-related signs, such as heart rate variations, sympathetic skin responses, and hypotension (3). A wide range of effects on a large number of tissues was apparent, with differences being noted across the different neurotoxin serotypes (A to G). Assuming that the parasympathetic system could be more affected due to its use of acetylcholine at both pre- and postganglionic sites, the signs seen would be adrenergic. This would include an increase in heart rate and in contractility and conduction velocity, a relative constriction of arterioles (increasing blood pressure), and a decrease in gastrointestinal motility (16).
Telemetry implants measuring systolic, diastolic, and mean pressures, heart rate, and electrocardiography were employed in this study to assess physiological changes not readily visible, i.e., secondary sequelae of skeletal muscle paralysis or direct blockage of the ANS (primarily parasympathetic system). Typically, flaccid paralysis of cranial nerves (due to the direct effect of BoNT on the somatic nervous system) occurs first, resulting in diplopia (blurred vision), dysarthria (slurred speech), ptosis (drooping eyelids), dysphagia (difficulty swallowing), and muscle weakness. While the first two are not easily assessable in rhesus macaques, the last three are often the first visible signs noted. Early effects on the ANS (parasympathetic system) result in mydriasis (enlargement of the pupil) and dry mouth (lack of saliva secretion). These signs are not easily assessable in rhesus macaques. Later somatic changes include a progression of flaccid, descending paralysis of the muscles of the neck, shoulders, proximal and distal upper extremities, and then proximal and distal lower extremities. Paralysis of the diaphragm and accessory breathing muscles may result in difficulty breathing and death. A later parasympathetic sign seen is constipation.
Of the 13 telemetry parameters collected, seven showed statistically significant dose responses, including diastolic pressure, systolic pressure, mean pressure, pulse pressure, body temperature, heart rate, and QA interval. Generally, initial increases (from baseline) in telemetric parameters occurred earlier (between days 1 and 2) in monkeys challenged with BoNT/B1 than in monkeys challenged with BoNT/A1 (between days 2 and 3). This was presumably due to the larger doses of BoNT/B1 delivered to induce these effects. Consistent with a previous report (1), monkeys in the middle-dose group that survived took longer to resolve the effects of the BoNT (in regard to diastolic, systolic, and mean pressures) and return to nonsignificant baseline levels when challenged with BoNT/A1 than when they were challenged with BoNT/B1. Overall, these results suggest that telemetry is an extremely useful tool in evaluating botulism disease progression. In some animals (generally monkeys challenged with low doses of BoNT/A1 or BoNT/B1), alterations in telemetric parameters were the only abnormal signs that were documented postchallenge (data not shown).
Statistically significant changes in clinical hematology and clinical chemistry parameters were reported. However, generally, these statistically significant changes were inconsistent and fluctuated between postchallenge blood draws and/or between dose groups, suggesting that these differences were not biologically significant. The hematology and clinical chemistry data collected in these analyses represent snapshots in time. When data of this nature are analyzed, consistent statistically significant changes which result in increases or decreases outside the normal range for the given parameter are of interest. These types of changes were not observed in this study. These results suggest that standard hematology and clinical chemistry analyses will be of limited value when the efficacy of medical countermeasures to acute BoNT/A1 and BoNT/B1 exposure in rhesus macaques are evaluated.
Serum BoNT levels following challenge were measured to evaluate the potential relationship between lethality and circulating BoNT concentration. All monkeys with detectable circulating BoNT levels died, but a detectable level was not required for death. The results suggest that the lethal circulating BoNT/A1 and BoNT/B1 concentrations are below the limit of quantitation of 2 MIPLD50/ml of the mouse potency assay.
The only abnormal clinical observation in monkeys challenged with low doses of either BoNT/A1 or BoNT/B1 was anorexia. There was a statistically significant dose response with regard to time to onset of abnormal clinical signs as well as duration of signs for both neurotoxins. Generally, the onset of abnormal clinical signs was documented approximately 18 to 24 h after changes in telemetric parameters were observed. With severe signs, the number and severity of signs increased with exposure dose, with labored respiration and mouth breathing being observed only in animals which died. In animals exposed to middle doses of neurotoxin that survived, the number and severity of abnormal clinical signs correlated with the severity of shifts observed in telemetry parameters.
The abnormal signs observed (dysphagia, ptosis, lethargy, ataxia, etc.) were consistent with previous reports of clinical signs of botulism intoxication, with the most severe signs (mouth breathing, labored respiration, lateral recumbency) being observed later in the disease progression (2). For both the middle-exposure (animals that died) and high-exposure groups, times of death were earlier in BoNT/B1-exposed monkeys than in BoNT/A1-exposed monkeys. There was a significant difference between the exposure levels required for BoNT/B1 to elicit abnormal clinical signs and the exposure levels required for BoNT/A1.
Many of the monkeys that died due to BoNT-induced paralysis had suppurative inflammation of the lungs, with polymorphonuclear cell infiltration of lymph nodes located near the lungs. These microscopic inflammatory changes were interpreted to be aspiration pneumonia secondary to paralysis/paresis of muscles controlling swallowing and responsible for avoidance of pulmonary aspiration. Histopathological changes directly attributable to BoNT were not observed. Given the rapid time to death following BoNT exposure, the absence of extensive histopathological changes was not unexpected.
In summary, rhesus macaque BoNT/A1 and BoNT/B1 aerosol challenge models have been established for use in future rBV A/B vaccine efficacy studies. The alterations in clinical and physiological parameters documented in these models were consistent with the previously reported progression observed in human disease. Relevant endpoints for evaluation of rBV A/B vaccine efficacy studies have also been identified.
Acknowledgments
This study was funded by the Chemical Biological Medical Systems-Joint Vaccine Acquisition Program (CBMS-JVAP), Department of Defense (DoD) contract DAMD 17-98-C-8024, and does not represent official DoD positions, policies, or decisions.
We thank Stephen Miller, Michael Ryan, Nichole Padgett, Joshua Schmidt, and Robert Davenport at Battelle for their expert technical assistance and Mary Kate Hart, Donald Fine, and Doris Snow at DVC for their critical review of the manuscript.
Footnotes
Published ahead of print on 21 July 2010.
Supplemental material for this article may be found at http://cvi.asm.org/.
REFERENCES
- 1.Aoki, K., and B. Guyer. 2001. Botulinum toxin type A and other botulinum toxin serotypes: a comparative review of biochemical and pharmacological actions. Eur. J. Neurol. 8(Suppl. 5):21-29. [DOI] [PubMed] [Google Scholar]
- 2.Arnon, S. S., R. Schechter, T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, J. Hauer, M. Layton, S. Lillibridge, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, D. L. Swerdlow, and K. Tonat. 2001. Botulinum toxin as a biological weapon: medical and public health management. JAMA 285:1059-1070. [DOI] [PubMed] [Google Scholar]
- 3.Böhnel, H., and F. Gessler. 2005. Botulinum toxins—cause of botulism and systemic diseases? Vet. Res. Commun. 29:313-345. [DOI] [PubMed] [Google Scholar]
- 4.Boles, J., M. West, V. Montgomery, R. Tammariello, M. L. Pitt, P. Gibbs, L. A Smith, and R. D. LeClaire. 2006. Recombinant C fragment of botulinum neurotoxin B serotype (rBoNTB (Hc)) immune response and protection in the rhesus monkey. Toxicon 47:877-884. [DOI] [PubMed] [Google Scholar]
- 5.Byrne, M., and L. A. Smith. 2000. Development of vaccines for prevention of botulism. Biochimie 82:955-966. [DOI] [PubMed] [Google Scholar]
- 6.Center for Drug Evaluation and Research. 2009. Guidance for industry. Animal models—essential elements to address efficacy under the animal rule. Food and Drug Administration, Department of Health and Human Services, Rockville, MD. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM078923.pdf.
- 7.Centers for Disease Control and Prevention. 1998. Botulism in the United States, 1899-1996: handbook for epidemiologists, clinicians, and laboratory workers. Public Health Service, U.S. Department of Health and Human Services, Atlanta, GA. http://www.cdc.gov/nczved/dfbmd/diseaselisting/files/botulism.pdf.
- 8.Centers for Disease Control and Prevention. 2010. Emergency Preparedness and Response Bioterrorism. Centers for Disease Control and Prevention, Atlanta, GA. http://www.bt.cdc.gov/agent/agentlist-category.asp.
- 9.Centers for Disease Control and Prevention. 2010. Botulism. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/nczved/dfbmd/disease_listing/botulism_gi.html.
- 9a.Department of Health and Human Services, U.S. Food and Drug Administration. 2009. Code of Federal Regulations, Title 21, vol. 7, subpart H. Approval of biological products when human efficacy studies are not ethical or feasible. 21CFR601. Department of Health and Human Services, U.S. Food and Drug Administration, Washington, DC.
- 10.Feder, P. I., D. W. Hobson, C. T. Olson, R. L. Joiner, and M. C. Matthews. 1992. Statistical design considerations for stagewise, adaptive dose allocation in dose-response studies, p. 37-86. In K. E. Peace (ed.), Biopharmaceutical sequential statistical applications. Marcel Dekker, New York, NY.
- 11.Feder, P. I., C. T. Olson, D. W. Hobson, M. C. Matthews, and R. L. Joiner. 1991. Statistical analysis of dose-response experiments by maximum likelihood analysis and iteratively reweighted nonlinear least squares regression techniques. Drug Inf. J. 25:323-334. [Google Scholar]
- 12.Finney, D. J. 1971. Probit analysis, 3rd ed. Cambridge University Press, Cambridge, England.
- 13.Franz, D. R., L. M. Pitt, M. A. Clayton, M. A. Hanes, and K. J. Rose. 1993. Efficacy of prophylactic and therapeutic administration of antitoxin for inhalation botulism, p. 473-476. In B. R. DasGupta (ed.), Botulism and tetanus neurotoxins: neurotransmission and biomedical aspects. Plenum Press, New York, NY.
- 14.Herrero, B. A., A. E. Ecklung, C. S. Streett, D. F. Ford, and J. K. King. 1967. Experimental botulism in monkeys: a clinical pathology study. Exp. Mol. Pathol. 6:84-95. [DOI] [PubMed] [Google Scholar]
- 15.LeClaire, R. D., and L. M. Pitt. 2005. Agent effect levels, p. 54. In L. E. Lindler, F. J. Lebeda, and G. Korch (ed.), Biological weapons defense: infectious disease and counterbioterrorism. Humana Press, Totowa, NJ.
- 16.McCance, K. L., and S. E. Huether. 2002. Pathophysiology: the biologic basis for disease in adults and children, 4th ed. Elsevier Science, St. Louis, MO.
- 17.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC.
- 18.Scott, A. B., and D. Suzuki. 1988. Systemic toxicity of botulinum toxin by intramuscular injection in the monkey. Mov. Disord. 3:333-335. [DOI] [PubMed] [Google Scholar]
- 19.Simpson, L. L. 2004. Identification of the major steps in botulinum toxin action. Annu. Rev. Pharmacol. Toxicol. 44:167-193. [DOI] [PubMed] [Google Scholar]
- 20.Smith, L. A., and J. M. Rusnak. 2007. Botulinum neurotoxin vaccines: past, present, and future. Crit. Rev. Immunol. 27:303-318. [DOI] [PubMed] [Google Scholar]
- 21.Smith, L. A. 2009. Botulism and vaccines for its prevention. Vaccine 27:D33-D39. [DOI] [PubMed] [Google Scholar]
- 22.Sobel, J. 2005. Botulism. Clin. Infect. Dis. 41:1167-1173. [DOI] [PubMed] [Google Scholar]