Abstract
Previous studies suggest that furanyl-rhodanines might specifically inhibit bacterial RNA polymerase (RNAP). We further explored three compounds from this class. Although they inhibited RNAP, each compound also inhibited malate dehydrogenase and chymotrypsin. Using biosensors responsive to inhibition of macromolecular synthesis and membrane damaging assays, we concluded that in bacteria, one compound inhibited DNA synthesis and another caused membrane damage. The third rhodanine lacked antibacterial activity. We consider furanyl-rhodanines to be unattractive RNAP inhibitor drug candidates.
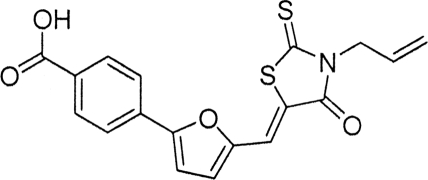
Bacterial RNA polymerase (RNAP) is an attractive drug target (2, 8, 14). However, it is underexploited, since the rifamycins are the only RNAP inhibitors that have been developed for clinical use (2, 8, 14). Recently several furanyl-rhodanines that apparently possess antibacterial activity and inhibit Escherichia coli (RNAP) were described (15). This series had been expanded from a compound considered to be a specific RNAP inhibitor on the basis of cross-screening against unrelated enzymes and failure to inhibit in an in vitro transcription-translation assay using a reticulocyte lysate (15). In view of our interest in RNAP inhibitors (1, 2, 10), we decided to examine in more detail compound 1 (Table 1), the most potent of the recently identified furanyl-rhodanine RNAP inhibitors (15). We also considered whether other furanyl-rhodanines (compounds 2 and 3 in Table 1) reported to possess antibacterial activity (4, 16) might also be inhibitors of RNAP.
TABLE 1.
Inhibition of E. coli RNAP by various compounds
Compound 1 was purchased from Cheshire Sciences Ltd. (United Kingdom). Compounds 2 and 3 were purchased from Chembridge Corporation and the Sigma-Aldrich rare chemical library, respectively. The purity of each sample was >95%, and the published structure for each compound (Table 1) was confirmed by full spectroscopic analysis (see the supplemental material).
We determined the abilities of compounds 1 to 3 to inhibit RNAP in an in vitro assay using the Kool NC-45 universal RNA polymerase template (Epicentre, Madison, WI). Compounds 1 to 3 demonstrated similar 50% inhibitory concentrations (IC50s) for E. coli RNAP (Table 1). However, rifampin, rifamycin SV, and corallopyronin A (obtained from G. Hofle, Helmholtz Centre for Infection Research, Germany), which are all well-documented inhibitors of RNAP (2, 7, 10), were more potent inhibitors of RNAP than the three furanyl-rhodanines examined here (Table 1). Compounds 2 and 3 have also been reported, respectively, to inhibit a class C β-lactamase (4) and penicillin-binding protein 2a from methicillin-resistant Staphylococcus aureus (16). We therefore considered the possibility that compounds 1 to 3 might be nonspecific enzyme inhibitors. The inhibitory activities of compounds 1 to 3 at 100 μM (i.e., approximately 3 to 6 times their IC50s against RNAP) were determined for bovine chymotrypsin and porcine malate dehydrogenase, commonly used specificity screens (12). Assays were run as previously described (12). Compounds 1 to 3 exhibited substantial inhibition of both enzymes (Table 2). In contrast, rifampin, at approximately 4 times its IC50 for RNAP (47.2 nM), exhibited only negligible inhibition (<10%) of chymotrypsin and malate dehydrogenase activities (Table 2).
TABLE 2.
Inhibition of malate dehydrogenase and chymotrypsin by various compounds
| Compound | Concn (μM) | % inhibition ± SD of mean |
|
|---|---|---|---|
| Malate dehydrogenase | Chymotrypsin | ||
| 1 | 100 | 96.3 ± 1.3 | 67.4 ± 16.6 |
| 2 | 100 | 99.7 ± 0.1 | 49.4 ± 0.8 |
| 3 | 100 | 88.1 ± 0.8 | 96.7 ± 1.2 |
| Rifampin | 0.0472 | 8.3 ± 2.2 | 7.8 ± 4.8 |
Compounds 1 to 3 are reported to possess antibacterial activity (4, 15, 16). We therefore sought to examine their modes of action and in particular to elucidate whether inhibition of bacterial growth might be attributed to inhibition of RNAP activity within the whole cell. A variety of bacterial strains were used for these studies (Table 3). Initially we evaluated the antibacterial activities of the three furanyl-rhodanines (compounds 1 to 3 in Table 4) by microdilution in Mueller-Hinton broth according to British Society for Antimicrobial Chemotherapy guidelines (11). In contrast to published data for compound 1 (15), we were unable to detect antibacterial activity against Staphylococcus epidermidis (MIC > 256 μg/ml against S. epidermidis strain ATCC 11047) or E. coli (Table 4), including strains treated with the outer membrane permeabilizing agent polymyxin B nonapeptide (PMBN) (3) or deficient in the AcrAB efflux pump (9). Compound 1 also lacked activity against Staphylococcus aureus and Bacillus subtilis (Table 4). We have no obvious explanation for the discrepancy between our data for compound 1 and the previously published results (15), especially since the structure of compound 1 (Table 1) was confirmed by full spectroscopic analysis (see the supplemental material) to be the same as that previously examined (15). In contrast to the results for compound 1, we confirmed that the other two furanyl-rhodanines (compounds 2 and 3) reported to possess antibacterial activity (4, 16) did indeed prevent the growth of S. aureus, B. subtilis, and E. coli (Table 4). Compounds 2 and 3 displayed moderate activity against E. coli 1411 which was not enhanced in the AcrAB deletion mutant, strain SM1411 (Table 4). Therefore, these compounds appear not to be substrates for the AcrAB efflux pump. However, treatment of E. coli 1411 with the outer membrane permeabilizing agent PMBN enhanced the activities of both compounds (Table 4), suggesting that their uptake across the intact outer membrane is poor.
TABLE 3.
Bacterial strains
| Strain | Relevant description/genotype | Reference/ source |
|---|---|---|
| S. aureus SH1000 | rbsU+ derivative of S. aureus 8325-4 | 6 |
| E. coli 1411 | Parent of SM1411 | 9 |
| E. coli SM1411 | E. coli 1411 DacrAB:Tn903 Kanr | 9 |
| S. epidermidis ATCC 14990 | ATCC type strain | American Type Culture Collection |
| B. subtilis 1S34 | Parental strain of biosensors | 13 |
| B. subtilis 1S34 yorB | Biosensor responsive to inhibition of DNA synthesis | 13 |
| B. subtilis 1S34 yvgS | Biosensor responsive to inhibition of RNA synthesis | 13 |
| B. subtilis 1S34 yheI | Biosensor responsive to inhibition of protein synthesis | 13 |
| B. subtilis 1S34 ypuA | Biosensor responsive to inhibition of cell envelope synthesis | 13 |
| B. subtilis 1S34 fabHB | Biosensor responsive to inhibition of fatty acid synthesis | 13 |
TABLE 4.
Susceptibilities of bacteria to rhodanine compounds 1 to 3 and their effects on B. subtilis antibiotic biosensors and the cytoplasmic membrane of S. aureus
| Compound | MICa (μg/ml) for: |
Induction of B. subtilis antibiotic biosensora,c |
Membrane disruption |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S. aureus SH1000 | S. epidermidis 11047 | E. coli 1411 | E. coli 1411 + PMBNb | E. coli SM1411 | B. subtilis 1S34 | DNA | RNA | Protein | Cell envelope | Fatty acid | % membrane integritya,d | % membrane potentiala,e | |
| 1 | >256 | >256 | >256 | >256 | >256 | >256 | ND | ND | ND | ND | ND | ND | ND |
| 2 | 4 | ND | 16 | 2 | 16 | 1 | 8.0 ± 0.9 | 1.3 ± 0.1 | 1.3 ± 0.3 | 1.0 ± 0.1 | 1.4 ± 0.2 | 82.8 ± 14.9 | 104.8 ± 6.9 |
| 3 | 4 | ND | >128 | 16 | >128 | 1 | 1.1 ± 0.1 | 1.0 ± 0.1 | 1.2 ± 0.1 | 1.0 ± 0.1 | 0.9 ± 0.1 | 27.3 ± 4.2 | 43.1 ± 8.0 |
ND, not determined.
PMBN (4 μg/ml) added together with compound 1, 2, or 3.
Maximum reporter signal induced in the respective biosensor, expressed as a ratio of the signal in noninduced control cultures.
Compared to drug-free control (100%) and measured by the BacLight assay following exposure of S. aureus SH1000 to 4× MIC of compound for 10 min.
Compared to drug-free control (100%) and determined using the fluorescent dye DiSc3(5) following exposure of S. aureus SH1000 to 4× MIC of compound for 10 min.
Biosensors that contain promoter-reporter constructs which are induced by conditions of antibiotic-induced stress can be used for whole-cell-based screening and characterization of inhibitors (13). Based upon a reference compendium of antibiotic-triggered microarray experiments, promoters which are induced in response to treatment of Bacillus subtilis with antibiotics of similar modes of action have been discovered and manipulated to genetically engineer five promoter-luciferase reporter fusion strains (13). These biosensor strains (Table 3) signal the presence of inhibitors of fatty acid (fabHB promoter), DNA (yorB), cell envelope (ypuA), RNA (yvgS), and protein (yheI) biosynthesis and therefore represent an excellent tool for screening of antibacterial agents and potential identification of their mechanisms of action. Induction thresholds for detection of inhibitors by these biosensors have been experimentally defined as 2.5-fold for yorB, 2-fold for yvgS, yheI, and fabHB, and 1.7-fold for ypuA (13). Rifampin, rifamycin SV, and corallopyronin A consistently caused at least a 2-fold induction in the biosensor (yvgS) that signals inhibition of RNA synthesis (data not shown), but compounds 2 and 3 failed to induce the yvgS biosensor, displaying induction ratios of <2.0 (Table 4). The lack of antibacterial activity exhibited by compound 1 (see above) prevented its assessment in this assay.
Further studies were conducted with compounds 2 and 3 to try to establish the basis of their antibacterial activities. Compound 2 triggered the biosensor sensitive to DNA synthesis, whereas compound 3 had no effect on any of the biosensors (Table 4). Compound 3 appears to promote membrane damage, since it caused a loss of membrane integrity and membrane potential in S. aureus as measured by the BacLight and DISC3(5) fluorescence assays (5) (Table 4).
In summary, we propose that due to a broad range of identified targets and whole-cell membrane damaging activity, furanyl-rhodanines should be considered nonspecific inhibitors. Consequently, we do not consider them attractive for development as bacterial RNAP inhibitors. We consider this warning to be timely since the suggestion that furanyl-rhodanines are specific inhibitors of bacterial RNAP is being perpetuated in the review literature (2, 8, 14).
Supplementary Material
Acknowledgments
This work was supported by project grant G0600810, awarded to I.C. by the United Kingdom Medical Research Council, and a CASE Ph.D. studentship awarded to K.R.M. from the United Kingdom Biological and Biosciences Research Council.
We thank Christopher Freiberg, Bayer HealthCare AG, Wuppertal, Germany, for the provision of the B. subtilis biosensors.
Footnotes
Published ahead of print on 26 July 2010.
Supplemental material for this article may be found at http://aac.asm.org/.
REFERENCES
- 1.Agarwal, A. K., A. P. Johnson, and C. W. G. Fishwick. 2008. Synthesis of de novo designed small-molecule inhibitors of bacterial RNA polymerase. Tetrahedron 64:10049-10054. [Google Scholar]
- 2.Chopra, I. 2007. Bacterial RNA polymerase: a promising target for the discovery of new antimicrobial agents. Curr. Opin. Invest. Drugs 8:600-607. [PubMed] [Google Scholar]
- 3.Dixon, R., and I. Chopra. 1986. Leakage of periplasmic proteins from Escherichia coli mediated by the polymyxin analogue, polymyxin B nonapeptide. Antimicrob. Agents Chemother. 29:781-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant, E. B., D. Guiadeen, E. Z. Baum, B. D. Foleno, H. Jin, D. A. Montenegro, E. A. Nelson, K. Bush, and D. J. Hlasta. 2000. The synthesis and SAR of rhodanines as novel class C β-lactamase inhibitors. Bioorg. Med. Chem. Lett. 10:2179-2182. [DOI] [PubMed] [Google Scholar]
- 5.Hobbs, J. K., K. Miller, A. J. O'Neill, and I. Chopra. 2008. Consequences of daptomycin-mediated membrane damage in Staphylococcus aureus. J. Antimicrob. Chemother. 62:1003-1008. [DOI] [PubMed] [Google Scholar]
- 6.Horsburgh, M. J., J. L. Aish, I. J. White, L. Shaw, J. K Lithgow, and S. J. Foster. 2002. σB modulates virulence determinant expression and stress resistance: characterization of a functional rsbU strain derived from Staphylococcus aureus 8325-4. J. Bacteriol. 184:5457-5467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Irschik, H., R. Jansen, G. Hofle, K. Gerth, and H. Reichenbach. 1985. The corallopyronins, new inhibitors of bacterial RNA synthesis from myxobacteria. J. Antibiot. 38:144-152. [DOI] [PubMed] [Google Scholar]
- 8.Mariani, R., and S. J. Maffioli. 2009. Bacterial RNA polymerase inhibitors: an organized overview of their structure, derivatives, biological activity and current clinical development status. Curr. Med. Chem. 16:430-454. [DOI] [PubMed] [Google Scholar]
- 9.O'Neill, A. J., J. Bostock, A. Morais-Moita, and I. Chopra. 2002. Antimicrobial activity and mechanisms of resistance to cephalosporin P1, an antibiotic related to fusidic acid. J. Antimicrob. Chemother. 50:839-848. [DOI] [PubMed] [Google Scholar]
- 10.O'Neill, A., B. Oliva, C. Storey, A. Hoyle, C. Fishwick, and I. Chopra. 2000. RNA polymerase inhibitors with activity against rifampin-resistant mutants of Staphylococcus aureus. Antimicrob. Agents Chemother. 44:3163-3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Report of the Working Party on Antibiotic Sensitivity Testing of the British Society for Antimicrobial Chemotherapy. 1991. A guide to sensitivity testing. J. Antimicrob. Chemother. 27(Suppl. D):1-50. [PubMed] [Google Scholar]
- 12.Seidler, J., S. L. McGovern, T. N. Doman, and B. K. Shoichet. 2003. Identification and prediction of promiscuous aggregating inhibitors among known drugs. J. Med. Chem. 46:4477-4486. [DOI] [PubMed] [Google Scholar]
- 13.Urban, A., S. Eckermann, B. Fast, S. Metzger, M. Gehling, K. Zielgelbauer, H. Rubsamen, and C. Freiberg. 2007. Novel whole-cell antibiotic biosensors for compound discovery. Appl. Environ. Microbiol. 73:6436-6443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villain-Guillot, P., L. Bastide, M. Gualtieri, and J.-P. Leonetti. 2007. Progress in targeting bacterial transcription. Drug Discov. Today 12:200-208. [DOI] [PubMed] [Google Scholar]
- 15.Villain-Guillot, P., M. Gualtieri, L. Bastide, F. J. Roquet, J. Martinez, M. Amblard, M. Pugniere, and J.-P. Leonetti. 2007. Structure-activity relationships of phenyl-furanyl-rhodanines as inhibitors of RNA polymerase with antibacterial activity on biofilms. J. Med. Chem. 50:4195-4204. [DOI] [PubMed] [Google Scholar]
- 16.Zervosen, A., L. Wei-Ping, Z. Chen, R. E. White, T. M. Demuth, and J. M. Frere. 2004. Interactions between penicillin-binding proteins (PBPs) and two novel classes of PBP inhibitors, arylalkylidene rhodanines and arylalkylidene iminothiazolidin-4-ones. Antimicrob. Agents Chemother. 48:961-969. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.