Abstract
The Cancer Risk Education Intervention Tool (CREdIT) is a computer-based (non-interactive) slide presentation designed to educate low-literacy, and ethnically and racially diverse public hospital patients at risk of Hereditary Breast and Ovarian Cancer (HBOC) about genetics. To qualitatively evaluate participants’ experience with and perceptions of a genetic education program as an adjunct to genetic counseling, we conducted direct observations of the intervention, semi-structured in person interviews with 11 women who viewed CREdIT, and post-counseling questionnaires with the two participating genetic counselors. Five themes emerged from the analysis of interviews: (1) genetic counseling and testing for breast/ovarian cancer was a new concept; (2) CREdIT’s story format was particularly appealing; (3) changes in participants’ perceived risk for breast cancer varied; (4) some misunderstandings about individual risk and heredity persisted after CREdIT and counseling; (5) the context for viewing CREdIT shaped responses to the presentation. Observations demonstrated ways to make the information provided in CREdIT and by genetic counselors more consistent. In a post-session counselor questionnaire, counselors’ rating of the patient’s preparedness before the session was significantly higher for patients who viewed CREdIT prior to their appointments than for other patients. This novel educational tool fills a gap in HBOC education by tailoring information to women of lower literacy and diverse ethnic/racial backgrounds. The tool was well received by interview participants and counselors alike. Further study is needed to examine the varied effects of CREdIT on risk perception. In addition, the implementation of CREdIT in diverse clinical settings and the cultural adaptation of CREdIT to specific populations reflect important areas for future work.
Keywords: Hereditary breast and ovarian cancer, Health disparities, Underserved, Genetic Education, Qualitative Research
Introduction
The institutionalization of clinical practices for assessing cancer risk related to BRCA1 and BRCA2 has advanced at a rapid pace in the 15 years since these genes were discovered. New medical technologies can bring new disparities, however, and a key challenge is to ensure that these new technologies and services are accessible to medically underserved populations. We define medically underserved to include people who are low-income, low-literacy, uninsured and/or members of ethnic, racial and linguistic minority groups. While family history is a strong risk factor for breast cancer for all women, and ethnic/racial minority women are as likely as other women to have BRCA mutations, less than 10% of all women who receive BRCA testing across the US are from ethnic minority groups (Frank et al. 2002).
Several recent studies have shown disparities in awareness and uptake of BRCA testing among racial and ethnic minorities in the USA (Armstrong et al. 2005; Halbert et al. 2005; Hall and Olopade 2006; Honda 2003; Peters et al. 2004; Zimmerman et al. 2006). Among these, Armstrong et al. (2005) in a case control study, found that African American women with a family history of breast or ovarian cancer were 78% less likely to undergo genetic counseling and BRCA testing than White women with similar family histories. Ramirez et al. (2006) found that while Hispanic family members of breast cancer survivors “seem to have positive perceptions about genetic testing for breast cancer susceptibility” (p.398), their high interest may be driven by a lack of knowledge about the complexity of genetic testing results and implications. According to Peters et al. (2004) the “awareness of and attitudes about predictive genetic testing for cancer risk differ by race, with lower awareness, less belief in the potential benefits of testing, and more concern about racial discrimination from genetic testing among African-Americans than Caucasians” (p.361). This echoed the findings of Thompson et al. (2003) who identified more concerns about the disadvantages, especially potential abuses of genetic testing for cancer risk among both African Americans and Latinos.
Furthermore, recent immigration to the US and educational background can also play a role in the awareness of cancer genetic testing. The Cancer Control Supplement of the 2000 National Health Interview Survey found that of 32,000 adults, 42% reported having heard of genetic testing for cancer risk, but only 13.8% of foreign-born adults and only 29.3% of adults with high school education or less knew about genetic testing for cancer risk (Schaefer and Dunston 2006). To address these apparent disparities, a recent editorial in the Journal of the American Medical Association recommends that interventions be designed to improve the uptake of genetic testing in underserved populations in order to fulfill its potential as a tool for effective cancer control and prevention (Huo and Olopade 2007).
Gaps in effective communication (where “effective communication” refers to instances when a message directly reaches the intended audience and where the meaning is mutually understood) (US DHHS 2000) have been widely recognized as a major element in health disparities (Thomas et al. 2004). The increasing cultural and linguistic diversity of the US population magnifies the need to address issues of culture, language, and literacy in health communications (Ad Hoc Committee on Health Literacy 1999; Williams et al. 1995). Patients with limited literacy tend to have limited health vocabulary, less basic knowledge of anatomy, and they have trouble reading health education materials, prescription labels, instructions for preoperative procedures, and consent forms required for some screening and treatment procedures (Ad Hoc Committee on Health Literacy 1999; Davis et al. 1998; 1999; Doak et al. 1998; Williams et al. 1995).
Several tools and methods have been developed to educate women with a family history of breast cancer prior to genetic counseling (Meilleur and Littleton-Kearney 2009). Some of these tools are decision aids, and thus serve the dual purpose of educating patients and helping them to make specific decisions with appropriate information and recognition of personal values. For example, these aids address decisions such as whether to have a genetic test (e.g., Green et al. 2004; Lerman et al. 1997) or whether or not to have prophylactic surgery after a BRCA positive test result (Healthwise 2007). Other tools are educational, without an explicit decision-making component, and they primarily aim to increase patient knowledge, improve accuracy of patient risk perception, reduce counselor time, and/or enable the counselor to focus on psychosocial aspects of counseling (Meilleur and Littleton-Kearney 2009). Such tools include CD-roms (Wang et al. 2005), an “information aid” consisting of a self-administered audiotape and booklet (Warner et al. 1999 and Warner et al. 2003), and a video (Cull et al. 1998).
Few education tools have been tailored or adapted for specific populations, such as those of lower literacy, or those belonging to an ethnic or racial minority group. One research team developed educational materials tailored for communication about HBOC within a large African American BRCA1 kindred (Baty et al. 2003); however, to our knowledge the implementation outcomes for these materials have not been published. Some research has shown that tailored communication for genetic risk services—including education—may be effective at increasing awareness of genetic risk (Hughes et al. 2003) and satisfaction with genetic counseling (Charles et al. 2006) among African American women. The need for further understanding of culturally appropriate risk communication and tailored education aids for genetic risk services is underscored by evidence of cultural differences in beliefs about inheritance and kinship (e.g., Chinese Australians’ belief in patrilineal descent) (Barlow-Stewart et al. 2006), and temporal orientation (i.e., the perception of events and actions in relation to past, present and future) (Edwards et al. 2008; Hughes et al. 2003).
The Cancer Risk Education Intervention Tool (CREdIT) is a novel contribution to this field. It is an educational tool tailored specifically for women of lower literacy that depicts a multi-racial Latino family and is available in English and Spanish. In contrast to tools tailored for a specific ethnic/racial group (e.g., Baty), and in contrast to tools made available online, CREdIT aims to reach women who are less well-educated, Spanish speakers, and those without access to the Internet. Only 10% of San Francisco General Hospital (SFGH) breast clinic patients have internet access, and only a handful of those women actually used the internet regularly. (Unpublished research, Bahtia V. 2007). Furthermore, CREdIT is informed not only by educational theory, but also by clinical experience in a unique program that provides free genetic counseling and BRCA testing to medically underserved women in a public hospital (Lee et al. 2005; Lubitz et al. 2007). With funding from the Avon Foundation in 2002, the UCSF Cancer Risk Program pioneered a program to offer free genetic counseling and testing to low income and uninsured families at San Francisco General Hospital (SFGH), a county “safety net” hospital that provides care to all residents of San Francisco County, regardless of ability to pay. Similar to many U.S. “safety-net” hospitals, SFGH is publicly owned and operated and serves a population that is approximately 50% uninsured at the time of presentation for care. Patients at SFGH are more likely to be from racial and ethnic minorities than the San Francisco population, less likely to speak English, and more than half have inadequate or marginal health literacy (Schillinger et al. 2002). The majority of safety-net institutions nationwide do not provide access to cancer genetic counseling and testing; at SFGH not only are these services provided for SF residents, but follow-up services for screening and preventive procedures are covered, as well as testing for SF Bay Area family members of women who test positive. Since 2002, 625 women have participated in genetic counseling at SFGH, and 156 women have been BRCA tested.
Formative research conducted for the design of CREdIT utilized focus groups to assess women’s preferences for “conventional” versus “colloquial” presentation of risk information (Lubitz et al. 2007). The “conventional” version utilized pictures of genes, pedigrees, and quantitative representations of risk while the “colloquial” version used an analogy of the “information book” of genes, family stories and vignettes, and visual representations of risk, without scientific words. Based on the results of the Lubitz study, CREdIT was revised by an interdisciplinary team (genetic counselor, oncologist, primary care physician, epidemiologist and anthropologist) to incorporate Lubitz’s findings that “simplicity, analogies and familiarity support comprehension, while vignettes, family stories and photos of real people provide comfort and hope” (p.276). The resulting educational tool reported herein is structured around a first-person, narrative vignette delivered via a 16-min (non-interactive) computer-based slide presentation. It is designed to provide basic education about: 1) familial cancer and genetic counseling; 2) genes, inheritance, and probabilities for inheriting cancer; and 3) risk management and risk reduction options. These three topics coincide with three parts in the narrative (see Appendix), beginning with “Theresa’s Story,” narrated by Theresa herself, a woman who has a strong family history of early onset breast cancer. It utilizes a family tree with pictures of family members rather than kinship symbols to talk about the family and to show “how cancer can be passed down in families.” Part 2, “Why My Family is Different,” explains genes and genetic mutations using the analogy of an instruction book, and illustrates risk probabilities visually. In Part 3, “How Can I Reduce My Cancer Risk?” Theresa explains in a conversational manner what the genetic counselor told her about how she can reduce her cancer risk, and she provides information on risk management options. The tool aims to appeal to low literacy populations by using jargon-free language, non-scientific images, and the instruction book analogy to discuss genetics.
Purpose of the Study
The purpose of this study was to qualitatively evaluate participants’ experience with and perceptions of a genetic education program provided as an adjunct to genetic counseling. We conducted a pilot test of an intervention to show CREdIT to patients immediately prior to their initial genetic counseling appointment at SFGH. Our evaluation of the pilot intervention included direct observations of a subset of participants viewing CREdIT and their genetic counseling sessions, in-person qualitative semi-structured interviews with a sub-set of observation participants, and a Genetic Counselor post-counseling session questionnaire. Our major research questions were: (1) How do women respond to this genetic education program administered prior to an initial genetic counseling session? (2) How does CREdIT affect genetic counselors’ satisfaction with their sessions, perceptions of patient anxiety and preparedness, and counseling time? (3) What changes and improvements are needed to make CREdIT accessible and culturally appropriate to this public hospital population?
Methods
Population and Setting
Table 1 shows the overall population in the Cancer Risk Program (CRP) as well as the self-reported race/ethnicity of pilot study participants (N = 52), and a subset of these who comprise our interview participants (N = 11). The interview participants are the focus of this report. The anthropologist (first author) observed 17 of the 52 CREdIT sessions in order to recruit 11 women for interviews; 6 participants declined or were unable to participate in an interview. While the interview sample is small (N = 11), as is common in qualitative research, the sample, in terms of immigrant status, ethnicity and education was heterogeneous. Compared to the SFGH Cancer Risk Program population overall, our interview sample were all English speakers (100% versus 77%) and thus a smaller percentage were Latina (9% versus 26%) and Asian (9% versus 13%).
Table 1.
Self-Identified Race and Ethnicity of SFGH Cancer Risk Program Population and Interview Participants
| San Francisco General Hospital Cancer Risk Program Population | Self Reported Race and Ethnicity of Pilot Study Participants | Self-Reported Race and Ethnicity of Interview Participants | |
|---|---|---|---|
| (N = 750) | (N = 52) | (N = 11) | |
| African American | 90 (12%) | 8 (15%) | 2 (18%) |
| Latino | 195 (26%) | 16 (31%) | 1 (9%) |
| Asian/Pacific Islander | 98 (13%) | 5 (10%) | 1 (9%) |
| White | 360 (48%) | 20 (38%) | 5 (45%) |
| Mixed Race | Unknown | 2 (4%) | 2 (18%)a |
aThese participants self-identified as African American/White and Latina/White
Table 2 shows the age, race/ethnicity, education and breast cancer status of the 11 interview participants.
Table 2.
Interview Participant Characteristics
| Participant | Age | Ethnicity/Race (country of origin, if outside US) | Education | Breast cancer |
|---|---|---|---|---|
| 01 | 30 | White (Bosnia-Herzegovina) | Masters degree | No |
| 02 | 34 | White | HSa degree | No |
| 03 | 62 | Latina (El Salvador) | HS degree | No |
| 04 | 42 | Latina/White | <HS | No |
| 05 | 52 | Filipina (Philippines) | HS degree | DCISb |
| 06 | 54 | African American | HS degree | No |
| 07 | 65 | White | HS degree | No |
| 08 | 23 | African American/White | HS degree | No |
| 09 | 41 | White | College Degree | DCISb |
| 10 | 63 | White | College Degree | No |
| 11 | 61 | African American | College Degree | No |
aHigh School
bDuctal carcinoma in situ
All women who were interviewed had one or more first-degree relatives with cancer, and 2 had a personal history of breast cancer [ductal carcinoma in situ (DCIS) in both cases]. The baseline family history risk of participants in this study was comparable to that of SFGH CRP patients overall. Among the 11 interview participants, the mean age was 49 (Range: 23–65). Seven had a high school education or less, and three were foreign born (Philippines, El Salvador and Bosnia-Herzegovina). Self-reported race and ethnicity included: 5 Whites; 2 African Americans; 1 Filipina; 1 Latina; and 2 mixed race (African American/White and Latina/White). All were uninsured or on Medicaid, and 45% were unemployed; thus in terms of socio-economic status, our participants reflected the SFGH population overall and the SFGH CRP program participants.
Recruitment
Approximately half of all the patients seen in the SFGH Cancer Risk Program (CRP) are referred by a clinician in SFGH affiliated practices including breast oncology, GYN oncology, surgery, and primary care. The other half are referred based on a single-page family cancer history questionnaire (available in four languages: English, Spanish, Chinese, Russian) administered to women waiting for screening mammograms at SFGH. A genetic counselor systematically classifies the questionnaires collected each week to identify women who may be at high risk [see Lee et al. (2005) for criteria used], and uses a faxback form to contact primary care physicians of women with high heritable cancer risk for referral to SFGH. These patients are then called by a Genetic Counseling Assistant (GCA), who confirms family history documented in the referral or mammography screening questionnaire, and then invites the patient for a free genetic counseling appointment if counseling is appropriate. Two GCAs (who were involved consecutively in this study) recruited participants in the course of their usual calls to patients to offer appointments.
Data Collection Procedures
We followed well-described data collection procedures for direct observations and semi-structured interviews (Berg 1995; Emerson et al. 1995; Fetterman 1998). The GCA who scheduled the genetic counseling/CREdIT appointment showed CREdIT to the participant on a laptop computer. She scrolled through the slide presentation manually in a private room at the clinic, and was available to answer questions.
The GCA and/or the first author then accompanied the participant to see the genetic counselor in another location on the hospital campus. Thus, each participant received an individual one-on-one appointment with a genetic counselor immediately after viewing CREdIT. The structure and content of the genetic counseling sessions with participants and non-participants was similar to regular non-CREDIT counseling sessions. Specifically, the counselors took a detailed four-generation pedigree, and then discussed individual hereditary risk, the value or lack thereof of BRCA testing given the patient’s individual family history, and appropriate cancer screening for the participant and her family members. Differences in the content of the sessions were primarily associated with counselors’ acknowledgement of and references to content provided in CREdIT; that is they used CREdIT to develop rapport (e.g., by asking “Did you see your family in CREdIT?”), and by referring to it when discussing hereditary risk and screening options—to reinforce what patient’s heard in CREdIT (e.g., referring to a character in the program or to an image illustrating risk visually.)
The first author observed as CREdIT was presented to each participant in a private room at the SFGH mammography center, and then observed the genetic counseling session. Observations were systematically recorded in field notes, and included patient-GCA interactions, patient questions during and after watching CREdIT, and topics covered during counseling.
The first author conducted all of the semi-structured interviews in a conference room at the hospital within 2 weeks of viewing CREdIT/seeing the genetic counselor. The purpose of the interviews was to assess the experience of viewing CREdIT and meanings of this genetic education program in the context of genetic counseling. A standard set of interview questions was utilized in all interviews to cover the following topics: personal and health background; genetic counseling referral process; content and format of CREdIT; observed reactions to CREdIT (e.g., if participant had asked questions or responded in other ways while watching); and the genetic counseling session following CREdIT. Additional questions were added based on participant responses to the standard questions and the observations of the participant viewing CREdIT and in Genetic Counseling. Interviews lasted 30–75 min (Mdn = 51) and were digitally recorded and transcribed by a professional transcriptionist.
Two genetic counselors filled out brief questionnaires regarding their perceptions of the genetic counseling session for 52 sessions in the CREdIT pilot study as well as for 24 sessions that were not part of the CREDIT study. These questionnaires assessed appointment duration, genetic counselor satisfaction, perception of patient’s anxiety, and perception of patient’s preparedness for the session (See Table 3).
Table 3.
Genetic Counselors’ Mean Responses to Post-Counseling Questionnaire
| No CREdIT (n = 24) | CREdIT (n = 24) | p value | |||
|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | ||
| Appointment Duration (minutes) | 42.2 | 17.9 | 35.0 | 8.8 | 0.19 |
| Genetic Counselor’s satisfactiona | 4.6 | 1.3 | 4.9 | 1.5 | 0.40 |
| Patient’s anxietyb | 4.4 | 1.6 | 4.4 | 1.5 | 0.79 |
| Patient’s preparednessc | 3.8 | 1.6 | 5.1 | .9 | < 0.0001 |
aQuestion: Overall, how satisfied were you with the session?
Answer: Very unsatisfied/Somewhat unsatisfied/Mildly satisfied/Somewhat satisfied/Very satisfied
bQuestion: Please rate the patient’s anxiety level at the start of the session:
Very anxious/Somewhat anxious/Mildly anxious/Calm/Somewhat calm/Very calm
cQuestion: Please rate the patient’s preparedness (education/background) at the start of the session:
Very unprepared/Somewhat unprepared/Mildly unprepared/Mildly prepared/Somewhat prepared/Very prepared
Data Analysis
We created a qualitative database using Atlas-ti software to facilitate searching, coding, and analysis of the interview transcripts and observation fieldnotes (Weitzman 1999; Weitzman and Miles 1995). We coded data according to substantive content to identify the key themes presented here (Berg 1995; Strauss 1987). The first author conducted data analysis, including writing memos that highlighted preliminary findings and examples that emerged during the coding process. Other authors commented on these memos, shaping successive iterations of coding and analysis. The genetic counselors’ questionnaire responses were tallied and the session durations were calculated from genetic counselor reports of start and end time of each session. Means, standard deviations, and alpha values were used to describe and compare quantitative data from the genetic counselor questionnaires. Genetic counselors were aware of which patients viewed CREdIT when they filled out each genetic counselor questionnaire.
The University of California San Francisco (UCSF) Committee on Human Research approved the research protocol. We obtained verbal informed consent for observations and written consent for interviews. All 52 pilot study participants were compensated $20 in cash for their participation in the viewing of CREdIT, and interview participants received an additional $25 gift card.
Results
The following themes emerged from analysis of the interviews: (1) Genetic counseling and testing for breast/ovarian cancer was a new concept for most participants. (2) Participants generally reacted positively to CREdIT, especially the story format. (3) Women who viewed CREdIT reported a range of changes in their perceived risk for breast cancer. (4) Some misunderstandings about individual risk and heredity persisted after CREdIT and counseling. (5) The context for viewing CREdIT (clinical setting; personal and family cancer history) shaped responses to the intervention. Analysis of the observations of the pilot intervention and the genetic counseling sessions facilitated identification of gaps between the content of CREdIT and the genetic counseling sessions, and helped to identify elements of the CREdIT program that could be improved. Finally, from the genetic counselors’ perspectives, patient preparedness was significantly higher in patients who viewed CREdIT prior to their genetic counseling session (Table 3).
Analysis of Interviews
Genetic Counseling and Testing for Breast Cancer was a New Idea for Most Participants
Most participants in this study had never heard of genetic counseling and/or genetic testing for breast cancer. For example, two women in our study found the concepts of “genetic” and “counseling” a perplexing combination.
“I’ve never heard of genetic counseling. I mean, what do you get advised on, it’s like such a medical/biological thing, …counseling is something that you associate with mind rather than matter. How can the two, have anything to do with one another?” (01)
“I don’t know what they do. ‘Sorry that you have the gene. Do you want to talk about that’?” (09)
While not familiar with genetic counseling or genetic testing for breast cancer, many participants were familiar with the idea of inherited disease, especially with regard to diseases they believed ran in their own families (e.g., asthma, diabetes, high blood pressure), and conditions their children had (e.g., Down Syndrome and scoliosis). Some associated genetic testing with purposes and contexts such as prenatal screening, paternity identification, and DNA testing in the justice system. Despite never having heard of genetic counseling or genetic testing specifically for breast/ovarian cancer, most participants said they had agreed to attend genetic counseling (after referral from a clinician or the mammography center), and to participate in the CREdIT study in order to learn more about their cancer risk: “I just thought it was a good experience to learn more about my situation or possible situation” (02). Another said she came because she wanted to learn “how come everyone in my family was having breast cancer” (06).
Patients Generally Reacted Positively to CREdIT, Especially the Story Format
Most participants expressed appreciation for the opportunity to learn, and said CREdIT provided new information and even corrected misunderstandings about inheritance of disease. For example, one participant reported that watching it made her realize, “I was wrong about things I thought I knew.” That is, she had misunderstood how cancer can be inherited. In particular, participants found the story format and the focus on a particular family an engaging way to learn, and a few participants were curious about the family’s ethnicity and background.
The CREdIT presentation is structured as a first person narrative in which “Theresa” explains her family’s cancer history, and what she learned from a genetic counselor about her risk and preventive options. Participants assumed that Theresa’s story was true, rather than a didactic tool or hypothetical case, and the story evoked participants’ concern and curiosity about Theresa’s BRCA and cancer status, as well as her treatment choices. “I just felt sorry for the family” (06). In addition, a couple of participants identified with Theresa and her family. When asked by the interviewer or by the genetic counselor in the counseling session following the viewing of CREdIT if Theresa’s family seemed like their own, only two of eleven reported this similarity. One woman said what she remembered most from the presentation was “How she [Theresa] was worried about her risk and how I’m worried about my risk”(08). But even those who did not identify with Theresa and her family seemed to appreciate learning through the story format.
“I thought [the story] was good because it’s easier to relate with a real family, like people are really going through it …I thought that was very good, very helpful.” (02)
“It made me think how many women in my larger family have been affected in the same way, …But … I also thought that it wasn’t really my family, it wasn’t as obvious because of [the] generational span [in my family], that things were happening at different times, and also because we were really like literally geographically so spread out, that it wasn’t really so …in your face.” (01)
“:…[the story is] different than just seeing a piece of paper. It doesn’t necessarily mean that much to you, just numbers on a piece of paper, how many people will get this or that.” (07)
Only two of the women interviewed raised the issue of Theresa’s ethnicity. For example, one African American participant said she thought it would be easier to relate to a family of the same ethnicity.
“Yeah, because I think they relate more with it, you know. They can understand it. For some reason, if I see an Oriental family that have just this particular problem then I say ‘Oh, well that’s terrible,’ but it doesn’t affect me as much as if I’d seen a black family with it. And then I go ‘Oh, my goodness,’ you know. It gets a little bit closer.” (11)
A recent immigrant from Bosnia-Herzegovina said:
“To my way of thinking it [race/ethnicity of CREdIT narrator] doesn’t really matter, it doesn’t make any difference, but a lot of people don’t think the same kind of an opened up way....any kind of an illness, people always automatically connect it with like the way of life and nutrition and everything. And then you think wow, you know, I lead a completely different lifestyle so maybe it wouldn’t apply to me as much as it does to them.” (01)
While these two participants volunteered this information (that is, the interviewer did not pose a specific question about race/ethnicity of family portrayed in CREdIT), we do not have sufficient information to determine how important this factor is in learning from CREdIT.
Participants Reported a Range of Changes in Their Perceived Risk of Breast Cancer
Regarding their personal sense of cancer risk, participants articulated a wide range of reactions to the experience of watching CREdIT and seeing a genetic counselor. Although participants were asked to talk about CREdIT and genetic counseling separately, many had difficulty separating the effects of the two components of study participation. For example, one woman said, “after I saw [CREdIT] and I was talking to all of you…I feel much better. Yes, a lot better” (03). For another participant, who had assumed she would get cancer at some point in her lifetime, talking with the genetic counselor after viewing CREdIT lowered her risk perception.
“…Cancer is always something that I just kind of think about because my mother had it and my grandmother had it...it’s something that I’ve always had a little concern about…just kind of in the back of my head,… but now that I’ve actually gone through the counseling I’m not quite so worried about it.” (02)
In other cases, CREdIT and/or the counseling increased an awareness of risk. For example, one participant said that the presentation increased her awareness of her cancer risk, but also of her preventive options.
“I’m more aware that I might get it, like more chances of getting it, so I’m lucky if I don’t get it...when you watch it, oh, shoot, it’s like this. So you have to be, you know, prepare in a more, do something.” (05)
Another participant revealed that CREdIT and counseling had increased her sense of risk, and had negatively affected her mood. She described how her sister (who was undergoing chemotherapy for breast cancer at the time) had tried to reassure her.
“I was telling her that, you know, that it [CREdIT] made me more concerned that maybe I might have a genetic trait of something, you know. And so…she was just telling me not to worry about it…because I was starting to feel kind of low, feeling kind of sad.” (06)
In particular, reviewing her family history with the genetic counselor, and seeing the counselor draw her pedigree made her aware of how all the cancer in her family was concentrated on her father’s side.
“I didn’t realize that it was all—the majority of the cancer ran on my father’s side. That was something else—I guess it wasn’t new to me but I had never really, you know, sat and really thought about it, and that was kind of nervy....Because it made me feel that I could be at risk for cancer, for breast cancer, more now than I thought before.” (06)
The CREdIT presentation left another participant feeling “frazzled” because “Theresa’s” story seemed extreme, and left her without hope of a successful outcome. In contrast, the meeting with the genetic counselor was reassuring because it put her specific family and personal cancer history in context, and differentiated it from Theresa’s.
“[CREdIT] wasn’t reassuring at first. Being told by [the counselor] that, “Oh, you know what? Actually, I think you’re fine. Let us know if your history changes or whatever.”” (09)
“With something like that because it is very difficult to watch…for me, I was kind of looking at a story: this could be me. It’d be possibly a good idea to have a success story on the other end. So kind of have a comparison of ‘this is Theresa and this is Mary’ and, you know, like there’s kind of a way of containment. Because I was pretty frazzled when I left. Not necessarily frazzled, it was just more of a thing of, ‘Oh, okay. Now what do I do with this?’ Like I didn’t feel, I didn’t feel like a success was given to me.” (09)
For a couple of women, the process of viewing CREdIT and attending genetic counseling did not change their perception of risk level, but did change their understanding or reasoning behind their sense of risk. For example, one woman learned that she probably does not have an inherited risk of cancer, but also that most cancer is not inherited, so her sense of her own risk stayed more or less the same, though for different reasons.
“I would feel like I’m just the same as I thought before...obviously since I don’t have the genetic cancer, I probably don’t have the genetic cancer, that’s better. It’s kind of almost down the middle because that’s better but then again, now that I know that most cancer is not genetic then it kind of just puts me right back in the same spot. So I feel like I’m probably just about the same—with more accurate knowledge and understanding, but probably about where I was anyway.” (02)
Another participant, who had been referred to the genetic counselor by her mother who had also seen the counselor, said that while the program “eased her nerves” somewhat at the time she saw it, the recent diagnosis of her grandmother’s cancer, and her mother’s recent discovery of a breast lump overrode what she learned from CREdIT.
“… the continual reality that cancer is in my family just keeps coming and coming and coming. …[I] don’t even really think about the video. …it keeps hitting closer and closer. It’s just I feel that the women in our family are like predestined to get it...” (08)
The timing and specific circumstances can critically affect the interpretation of the information provided by CREdIT and genetic counseling. The context of this woman’s family history overrode the information about inheritance she obtained by watching CREdIT and the information about her own risk provided by the genetic counselor. She interpreted the genetic counselor’s explanation of her risk as dependent on her mother’s risk:
“She says that my risk isn’t too high, that my mom’s risk is higher than mine, and we would go from what my mom’s risk and what her outcome is to come up with my outcome. So it’s like I’m basically stumped. So if my mom doesn’t have it then I’ll be like oh, okay. But then if she does have it, it’s kind of like well, I do have a risk.” (08)
Thus, depending on the individual’s circumstances, family cancer history, and personal cancer history, CREdIT impacted her sense of her own risk in various ways: increasing or decreasing it, or changing her understanding of the underlying reason for her risk. Given the wide range of effects on risk perception, it is important that CREdIT is used as an adjunct to counseling rather than on its own, so that an individual risk assessment can be integrated with the general information provided by CREdIT and so that the particular story offered by CREdIT can be used as a point of comparison.
Misunderstandings of Individual Risk and Heredity Persist After CREdIT and Counseling
While overall knowledge seemed to improve after viewing CREdIT, a few participants misunderstood or confused the information in CREdIT and/or the genetic counseling session. This confusion seemed to contribute to variations in risk perception, and understanding of how cancer can be inherited. For example, despite being reassured by the counselor about her own status after feeling “frazzled” by CREdIT, this participant’s understanding of her own risk was still somewhat confused.
“Am I convinced that it’s not genetic? I’m not yet. Just because there’s a couple of things missing as far as my mom was an only child. … I learned a lot from watching, that it was a 50/50 shot that one would carry it....if there’s two siblings, you get a 50/50 chance. If you have one sibling, there’s no real detection. There’s no way to detect whether or not the gene is present or whatever. …I think that’s what the overall point was that because both my parents have such small families that it was difficult to determine whether or not genetically that was the reason why I, you know, was diagnosed with DCIS.” (09)
Thus, she combined two pieces of information—the one in two chance of passing on the genetic predisposition discussed in CREdIT, and the genetic counselor’s reasoning for not offering her a BRCA test. She thus misunderstood the reason that the cause of her cancer remains unknown. Another participant also confused the referent for the 50/50 figure in a manner that left her feeling less fearful:
That genetic information really kind of helped me a little bit more not to be so frightened by, you know, a remote person in the family having it....Even that 50/50 chance is still good. [laughs] 50%, 50%. (10)
Another participant commented to the GCA before viewing CREdIT and reiterated after viewing CREdIT, that she thought she had probably inherited cancer from her niece.
These misunderstandings suggest that while the “level” of the content presented in CREdIT and by the genetic counselors was generally appropriate for the lower-literacy population, a few participants had difficulty combining the different pieces of information into a coherent individual story to make sense of their own risk.
The Context for Viewing CREdIT Shaped Responses to It
The CREdIT presentation was intended for use as an adjunct to genetic counseling, and participants indicated that the context of viewing CREdIT, which we define as the clinical setting in which they viewed CREdIT as well as life circumstances, could be important to their comfort level with the material presented. For our study, the setting was personalized and intimate. The GCA who scheduled the genetic counseling/CREdIT appointment showed CREdIT to the participant on a laptop computer. She scrolled through the slide presentation manually in a private room at the clinic, and was available to answer questions. When asked whether they would be equally comfortable watching CREdIT without the GCA present, most participants said that they would not be.
“I think it would have been worse because … I don’t really necessarily need to be tended to and cushioned, but...I think it’s much better to have people around you even if they’re not saying anything, you know, even if you’ve got [the GCA] sitting there and just clicking for you. It gives you a different kind of an impression that people have gathered here for you, even if it’s not true.” (01)
“I guess if I had questions, or like you wanted to clarify something, …That’s the thing, like you need somebody there. It helps a lot.” (05)
Our participants felt it was important to have the GCA there for general support as well as to answer questions.
The research setting in which participants viewed CREdIT was also significant for at least one participant. She clearly articulated that the pre-CREdIT questionnaire raised her level of anxiety about her cancer risk, but that watching CREdIT calmed her:
“When I was filling out the paperwork [questionnaire] I was, everything was high risk and the percentage was so high that, your risk of getting it and it was, the video actually calmed me down a lot.” (08)
In addition to the setting for viewing CREdIT, the life circumstances of the participant also influenced the experience of watching CREdIT. One participant described CREdIT as an “emotional buffer” before the intensity of her first genetic counseling appointment.
“It probably did act as some kind of a little emotional buffer and something that just kind of maybe eases you into what you’re just going to talk about. Because, you know, … the way it’s done is kind of pretty light. There’s nothing gory and there’s no pictures of body parts and open wounds and people in death beds. …it makes you think about things but it doesn’t really upset you, whereas just launching straight into your personal story and talking about people who’ve died, it isn’t easy ever, especially when you’re talking to people that you don’t know and you don’t even know how they’re going to react.” (01)
The CREdIT presentation enabled this participant to prepare for the genetic counseling appointment, which she said, “would have been a lot harder without the slides.” In contrast, another participant who had recently gone through treatment for DCIS, described viewing CREdIT as “an intense meeting,” and she suggested that participants should bring a family member to the appointment to view it with them.
Clearly life circumstances, and the setting in which CREdIT was viewed, affected how different participants experienced CREdIT and the counseling appointment that followed. Providing support appropriate to the circumstances may be critical to the effectiveness of using CREdIT with genetic counseling as an intervention to increase knowledge without increasing anxiety.
Analysis of Observations
The observations of the CREdIT intervention facilitated identification of issues related to the content of CREdIT, and the potential for implementing CREdIT at SFGH and beyond. Analysis of the observations of the pilot intervention and the genetic counseling sessions that followed identified minor discrepancies between the language used in CREdIT and the genetic counseling sessions, and helped to identify elements of the CREdIT program that could be clarified. For example, the term “genetic mutation” was not used in CREdIT in favor of more a colloquial description of a “genetic change.” However, in the counseling sessions, the counselors used the term genetic mutation. It was not clear that participants correlated the terms used in CREdIT with those used in the counseling sessions, or that they gathered the same meaning from both. In addition, observations identified a somewhat different emphasis on individual risk and screening (CREdIT) and family risk and screening (Counselors). The genetic counselors emphasized familial risk and screening, tailoring their recommendations for both the individual patient and her family, taking into account the patient’s particular family history and relationships, while CREdIT provided basic information about screening, chemoprevention, and surgical prevention options that an individual might choose. Further research should explore how these different emphases are understood by participants.
Analysis of Counselors’ Questionnaire
The short post-counseling questionnaire was filled out by each of the two counselors after a total of 52 CREdIT appointments and 24 regular appointments with new patients. Counselor rating of the patient’s preparedness before the session was significantly higher for CREdIT patients (mean = 5.1 on a preparedness scale of 6) versus patients who did not view CREdIT beforehand (mean = 3.8 on a preparedness scale of 6). The alpha value for this difference was p≤.0001. For other ratings on the Genetic Counselor questionnaire, there were no statistically significant differences in the CREdIT patients versus the non-CREdIT patients with respect to session length, counselor satisfaction, or patient anxiety (Table 3.)
Discussion
As clinical genetics becomes more widespread and reaches underserved populations in greater numbers, it is vital that information and education about genetic counseling, testing and hereditary risk is delivered in an appropriate manner. Gaps in the effectiveness of communication have been widely recognized as a major element in health disparities (Thomas et al. 2004), and the lack of appropriate genetic education materials for underserved individuals may contribute to the documented disparities in who uses cancer genetic counseling/testing services (Armstrong et al. 2005; Halbert et al. 2005; Hall and Olopade 2006; Honda 2003; Peters et al. 2004; Singer et al. 2004; Vadaparampil et al. 2006; Zimmerman et al. 2006;) and why (Charles et al. 2006; Hughes et al. 2003; Ramirez et al. 2006).
Understanding the contribution of genetics to cancer risk, the mechanisms of inheritance and the implications of genetic test results can be challenging for anyone; for those who are of lower literacy or education, it can be even more daunting. Given the documented lack of awareness and knowledge about cancer genetics services among medically underserved women (Armstrong et al. 2005; Halbert et al. 2005; Hall and Olopade 2006; Honda 2003; Peters et al. 2004; Zimmerman et al. 2006), the development and evaluation of educational tools such as CREdIT are critical. The CREdIT presentation is a novel program that fills a gap in educational tools for hereditary cancer by tailoring the delivery of pre-counseling genetic education to patients of lower literacy. Furthermore, CREdIT aims to reach this audience by depicting a multi-racial Latino family using the format of a first person narrative vignette, and it is available in English and Spanish. It is informed not only by educational theory, but also by clinical experience in a unique program that provides free genetic counseling and testing to diverse low-income/underserved women in a public hospital.
It must be noted that CREdIT is an educational program, not a decision aid; thus, it differs from other programs not only in its language and style of presentation, but also in its goal. It was designed to orient patients prior to their first genetic counseling appointment, and to provide a platform from which the viewer can engage in discussion with a genetic counselor about individual family history, individual and familial cancer risk, and pros and cons of genetic testing. It provides basic information about familial cancer and genetic counseling: genes, inheritance, probabilities for inheriting cancer, and risk management and risk reduction options. Genetic testing is mentioned, but the benefits and limitations of testing are not discussed and explored. Furthermore, because CREdIT is aimed at an audience that may have little or no prior knowledge of genetics or hereditary cancer, it provides very basic information, with the idea that one on one counseling will provide personalized information for decision-making about genetic testing for HBOC.
Several authors have discussed whether educational tools and decision aids can be used independently or only as an adjunct to counseling (Cull et al. 1998; McGee and Malik 1999; Rubinstein 1999). Given the growth of genetic counseling and testing, educational and decision making tools have been examined for ways to economize the time of counselors and other clinicians. Yet Cull et al. (1998) for example, concluded that “Observations of misunderstandings and distress emphasize the video should be seen as an aid to, not a substitute, for communications at the clinic” (p. 830). Green et al. (2004) in a randomized controlled trial assessed the differential impact of using an educational program independently or as an adjunct to counseling, and found that their computer program “had the potential to stand alone… for low-risk women, but should be used as a supplement to genetic counseling for those at high risk” (p. 442). It should be noted however, that the program evaluated by Green et al. had a decision-making component. In the future, it will be important to determine whether CREdIT could be used as a stand-alone tool or only as an adjunct to genetic counseling as originally conceived.
A related question raised by our pilot study is: what is the best setting for the viewing of an educational program like CREdIT—at home, in a high-risk clinic, in a mammography clinic, in a group, with family, individually? Interview participants were generally satisfied with the setting in which they viewed CREdIT. In particular they liked having a GCA on hand, and it is unknown whether CREdIT would be equally satisfying and effective without the GCA. Clearly, the procedures used in our pilot study (individual viewing in a private room accompanied by a GCA) were labor, time and space intensive, and they are not likely to be replicated in other clinic environments, and non-research routines. In a survey of genetic counselors, Axilbund et al. (2005) found that “Of the 70% who do not use videos, predominant barriers included the perceived lack of an appropriate video, lack of space and/or equipment, and concern that videos are impersonal” (p. 235). While the CREdIT pilot test reflected a “realist approach” for the clinical context where it was developed, with technical upgrades, it could be made appropriate for other clinical settings. For example, CREdIT could be shown without an assistant, and in a group setting (e.g., a waiting room), privately immediately prior to an appointment or on DVD at home prior to an appointment. These alternatives should be explored in future research.
One of the concerns with using educational aids on their own is that they may contribute to inaccurate risk perception. Other studies have found that accurate risk perception is more often achieved with genetic counseling than with a computer program. For example, Green et al. (2004) found that “genetic counseling was more effective than the computer at reducing women’s anxiety and facilitating more accurate risk perceptions” (p.442). Another study found that an information aid “substantially reduced the mean risk estimate of low- and moderate-risk groups to a more appropriate level; however, there were still women who greatly overestimated or underestimated their risk of developing breast cancer” (Warner et al. 2003, p.59). Given the range of responses to CREdIT, in terms of risk perception—increased risk perception, decreased risk perception, or change in understanding of underlying reasons for risk—further study of risk perception in relation to this genetic education tool is needed.
Participants responded enthusiastically and positively to CREdIT in general, but several participants also offered suggestions for improving it, including (1) provision of additional information about the treatments “Theresa” and her family members with cancer underwent and about preventive care options for those who test BRCA positive; (2) specific information about Theresa’s outcome and a more positive or “success” story to compare with Theresa’s extreme family history; and (3) ethnic tailoring to enable closer identification with the characters in the story. Some of these changes are being incorporated into the program, and will be evaluated as further pilot testing is implemented. By depicting a multiracial Latino family, the program aims to appeal to an ethnically and racially diverse audience. Based on our findings and on the literature (e.g., Hughes et al. 2003; Baty et al. 2003) we suspect that further cultural tailoring will improve our ability to provide effective genetic education to subpopulations. For example, Hughes et al. (2003) found that cultural beliefs and values may influence genetic test acceptance by African American women, and that therefore integrating such beliefs and values into genetic counseling and education may be appropriate. In collaboration with two other public hospital cancer risk programs that primarily serve African Americans, we are currently conducting research to inform the cultural adaptation of CREdIT for African Americans. In addition, while CREdIT has been translated to Spanish, no adaptations or enhancements have been made for the Latino cultural context. We are planning to tailor CREdIT for Latinos as well.
Study Limitations and Additional Research Recommendations
Limitations of this study include the inability to generalize from our findings to other genetic tests, larger populations, or other locations, due to the small sample size typical of our qualitative study design. However, certain elements of CREdIT could be adapted for educational materials for other genetic tests, for example, the analogy of genes to an instruction book, the first-person vignette format, and the family pictures in the family tree. Our qualitative research has shown that these elements helped participants to engage with and understand basic genetic concepts.
The study design also did not include gathering baseline data to describe the experiences of women in the Cancer Risk Program Population who do not elect CREdIT. Future research should include a comparison to patients who do not use CREdIT, and the protocol should ensure inclusion of more non-English speakers, and more participants with less education. Due to the fact that participants were interviewed after viewing CREdIT and meeting with the genetic counselor, the qualitative evaluation was not designed to determine the effects of CREdIT alone. This design choice was made to evaluate CREdIT as an adjunct to counseling, and to ascertain how the two procedures work together. While this method precludes isolation of the independent effects of CREdIT and counseling, it does reflect a “realist approach” that evaluates CREdIT as it was intended to be used in practice (Pawson et al. 2005).
Although patients who viewed CREdIT were rated as having significantly higher “preparedness” than patients who did not view CREdIT, there were only 2 genetic counselors, and they were aware of which patients had viewed CREdIT. In practice, it was difficult to blind genetic counselors, as patients often brought up parts of CREdIT in the counseling session. Nevertheless, we feel that the highly significant alpha value for this comparison (p≤.0001) reflects an increase in “preparedness” in patients who view CREdIT before their genetic counseling sessions. Future research should examine patient-rated measurements of “preparedness” and also examine CREdIT compared to other educational tools to determine whether this difference in preparedness can be replicated.
Another limitation is that the pilot test procedures are unlikely to be replicated in other clinical settings, particularly non-research settings. Further research is needed to test alternate implementation scenarios for CREdIT that would be less labor, time, and space intensive. If part of the goal is to save time in a busy practice, how can CREdIT be integrated into usual practice in a streamlined way that does not add a burden to counselors and the clinic overall? Future research should address that question, as well as evaluate whether and how CREdIT can help to address particular problems faced by clinics serving underserved patients. For example, another public hospital high-risk clinic is planning to evaluate whether CREdIT can be employed to reduce the no-show rate for counseling and testing appointments. Other research might evaluate what might be added or removed from the CREdIT program to make it more of a “stand-alone” for use with certain categories of women (e.g., lower risk women referred for counseling; women obtaining a screening mammography, etc.). However, we do not foresee using CREdIT as a decision-making tool, but rather to support the genetic counseling process. Finally, given the diversity of participants within our small sample in terms of race/ethnicity, education and personal/family experiences with cancer, we cannot perform subgroup analyses to compare responses to CREdIT between subgroups.
Conclusions
Our findings suggest that CREdIT was a welcome adjunct to individualized genetic counseling for both patient participants and genetic counselors involved in the pilot study. The CREdIT program has potential to improve patient understanding of HBOC, and to prepare underserved women with no prior knowledge of genetic counseling/testing for their initial genetic counseling appointment. Given the evidence that mastectomy and oophorectomy following a positive BRCA test can reduce cancer risk (Kauff et al. 2002; Meijers-Heijboer et al. 2001; Rebbeck et al. 2002), and that BRCA test outcomes have been shown to influence treatment decisions (Morgan et al. 2009), it is critical that all women at high risk of Hereditary Breast/Ovarian Cancer (HBOC) have access to appropriate genetic counseling and testing services—including education—that enable them to make informed decisions. The public health benefits of predictive genetic testing will not be fully realized unless disparities in knowledge and utilization of genetic risk services are addressed (Ponce et al. 2007).
While elimination of financial and other physical access barriers is essential, this is not sufficient to ensure equitable use of risk services. Similar to free mammography, hereditary cancer education, counseling, and testing services must be delivered in appropriate and acceptable ways. For both public health and ethical reasons, it is imperative that we minimize the expansion of cancer disparities as new forms of medicine and medical technologies are implemented in clinical settings. Genetic education tools are a critical component of clinical practices that will make genetic counseling and testing accessible and appropriately deliverable to underserved populations.
Acknowledgments
This research study was made possible with support from the Avon Foundation. In addition, the authors would like to thank the participants for generously giving their time and sharing their thoughts.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix I. Screen Shots and script from CREdIT
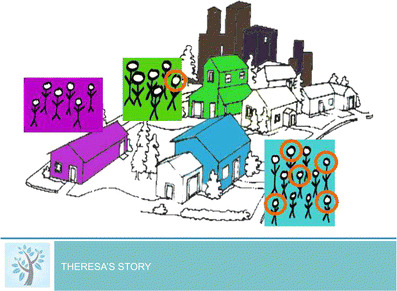
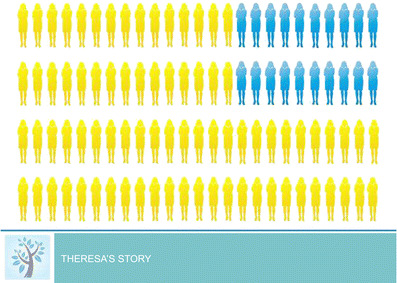
Part 1 Theresa’s Story (Fig. 1)
Theresa introduces her family
“I grew up in this blue house in a neighborhood in a big city, and the same families had been on my street for as long as I can remember. All these women circled in my family had cancer, but I knew many other families in my neighborhood and none of them had as much cancer as ours. Our neighbors in the green house across the street had only one person in their family who had cancer. And our neighbors in the purple house next door had an older cousin who had gotten sick with cancer. But no one in their immediate family at home had ever had cancer. Although other families were touched by cancer, ours seemed very different because so many more of our family members had developed cancer.”
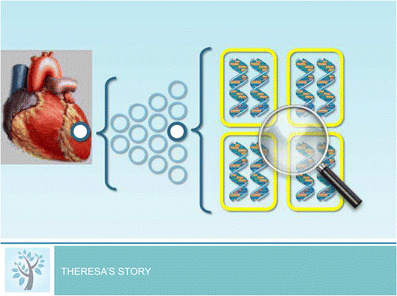
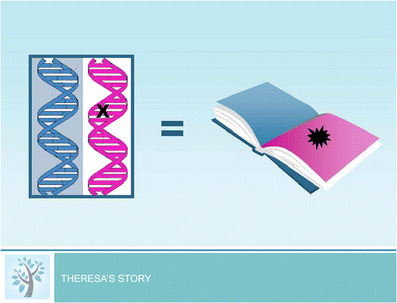
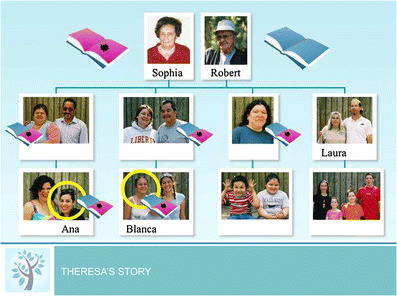
Part 2 “Why My Family is Different” (Figs. 2, 3, and 4)
Theresa explains genes and genetic mutations using the analogy of an instruction book,
“We can find the same set of genes in every cell in our bodies—in the heart, the blood and the breast, as well as everywhere else in the body.”
“You can think of a gene as a page in an instruction book that tells the body how to work. …Sometimes our genes carry mistaken information that make it hard for our bodies to work properly. You can think of this as a page in an instruction book that cannot be read.”
“After the genetic counselor looked at our family tree she explained how the cancer was being passed down in our family. The counselor suspected that my mother Maria, aunt Lucia and uncle Carlos probably inherited a genetic change or mutation…”
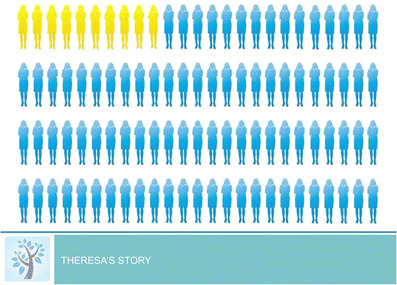
Part 3 “How Can I reduce my cancer risk?” (Figs. 5 and 6)
Theresa explains what the genetic counselor told her about how she can reduce her cancer risk, and provides information on risk management options.
“If women who have inherited the mistaken information have both breasts removed, this would lower their chances of getting breast cancer from this picture (80 out of 100)…”
“…to this picture (10 out of 100), which is the same as the general population.”
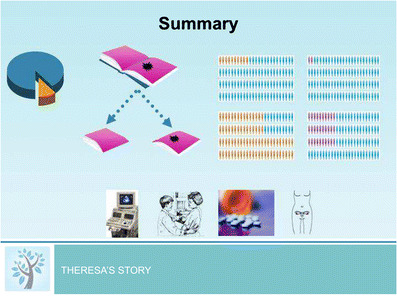
Part 4 Summary (Fig. 7)
“Only a small portion of cancer is hereditary. A person with the mistaken information has a 50% or 1 in 2 chance of passing it down to each child. In the general population, 10 out of 100 women will develop breast cancer. Out of the women who have inherited the mistaken information, 80 out of 100 will develop breast cancer in their lifetime. In the general population only 2 out of 100 women will develop ovarian cancer. Out of the women with the inherited mistaken information 30 out of 100 will develop ovarian cancer. A woman who has inherited the mistaken information may choose to have regular mammograms and ultrasounds, may take medicines, or may choose to have preventative surgery to lower her risk of cancer.”
References
- Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association Health literacy: report of the council on scientific affairs. JAMA. 1999;281:552–557. doi: 10.1001/jama.281.6.552. [DOI] [PubMed] [Google Scholar]
- Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293:1729–36. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- Axilbund JE, Hamby LA, Thompson DB, Olsen SJ, Griffin CA. Assessment of the use and feasibility of video to supplement the genetic counseling process: a cancer genetic counseling perspective. J Genet Couns. 2005;14(3):235–243. doi: 10.1007/s10897-005-4065-z. [DOI] [PubMed] [Google Scholar]
- Barlow-Stewart K, Yeo SS, Meiser B, Goldstein D, Tucker K, Eisenbruch M. Toward cultural competence in cancer genetic counseling and genetics education: lessons learned from Chinese-Australians. Genet Med. 2006;8(1):24–32. doi: 10.1097/01.gim.0000195884.86201.a0. [DOI] [PubMed] [Google Scholar]
- Baty BJ, Kinney AY, Ellis SM. Developing culturally sensitive cancer genetics communication aids for African Americans. Am J Med Genet A. 2003;118:146–55. doi: 10.1002/ajmg.a.10150. [DOI] [PubMed] [Google Scholar]
- Berg B. Qualitative research methods for the social sciences. 2. New York: Allyn and Bacon; 1995. [Google Scholar]
- Charles S, Kessler L, Stopfer JE, Domchek S, Halbert CH. Satisfaction with genetic counseling for BRCA1 and BRCA2 mutations among African American women. Patient Educ Couns. 2006;63(1–2):196–204. doi: 10.1016/j.pec.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Cull A, Miller H, Porterfield T, Mackay J, Anderson ED, Steel CM, et al. The use of videotaped information in cancer genetic counselling: a randomized evaluation study. Br J Cancer. 1998;77(5):830–837. doi: 10.1038/bjc.1998.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TC, Holcombe RF, Berkel HJ, Pramanik S, Divers SG. Informed consent for clinical trials: a comparative study of standard versus simplified forms. J Natl Cancer Inst. 1998;90(9):668–674. doi: 10.1093/jnci/90.9.668. [DOI] [PubMed] [Google Scholar]
- Davis TC, Williams MV, Branch WT, Green KW. In: Explaining illness to patients with limited literacy. Explaining illness: research, theory, and strategies for comprehension. Whaley B, editor. Mahway: Lawrence Erlbaum Associates, Inc; 1999. [Google Scholar]
- Doak CC, Doak LG, Friedell GH, Meade CD. Improving comprehension for cancer patients with low literacy skills: strategies for clinicians. CA Cancer J Clin. 1998;48(3):151–162. doi: 10.3322/canjclin.48.3.151. [DOI] [PubMed] [Google Scholar]
- Edwards TA, Thompson HS, Kwate NO, Brown K, McGovern MM, Forman A, et al. Association between temporal orientation and attitudes about BRCA1/2 testing among women of African descent with family histories of breast cancer. Patient Educ Couns. 2008;72(2):276–282. doi: 10.1016/j.pec.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson RM, Fretz R, Shaw LL. Writing ethnographic fieldnotes. Chicago: University of Chicago Press; 1995. [Google Scholar]
- Fetterman D. Ethnography: step by step. 2. Thousand Oaks: Sage; 1998. [Google Scholar]
- Frank TS, Deffenbaugh AM, Reid JE, Hulick M, Ward BE, Lingenfelter B, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10, 000 individuals. J Clin Oncol. 2002;20(6):1480–1490. doi: 10.1200/JCO.2002.20.6.1480. [DOI] [PubMed] [Google Scholar]
- Green MJ, Peterson SK, Baker MW, Harper GR, Friedman LC, Rubinstein WS, et al. Effect of a computer-based decision aid on knowledge, perceptions, and intentions about genetic testing for breast cancer susceptibility: a randomized controlled trial. JAMA. 2004;292(4):442–452. doi: 10.1001/jama.292.4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, Kessler LJ, Mitchell E. Genetic testing for inherited breast cancer risk in African Americans. Cancer Invest. 2005;23(4):285–295. doi: 10.1081/CNV-58819. [DOI] [PubMed] [Google Scholar]
- Hall MJ, Olopade OI. Disparities in genetic testing: thinking outside the BRCA box. J Clin Oncol. 2006;24(14):2197–2203. doi: 10.1200/JCO.2006.05.5889. [DOI] [PubMed] [Google Scholar]
- Honda K. Who gets the information about genetic testing for cancer risk? the role of race/ethnicity, immigration status, and primary care clinicians. Clin Genet. 2003;64(2):131–136. doi: 10.1034/j.1399-0004.2003.00112.x. [DOI] [PubMed] [Google Scholar]
- Healthwise (2007) Ovarian cancer: Should I have my ovaries removed to prevent ovarian cancer? Accessed January 14, 2010. https://doi.org/www.healthwise.net/cochranedecisionaid/Content/StdDocument.aspx?DOCHWID=zx3060
- Hughes C, Fasaye GA, LaSalle VH, Finch C. Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Educ Couns. 2003;51(2):107–114. doi: 10.1016/S0738-3991(02)00179-9. [DOI] [PubMed] [Google Scholar]
- Huo D, Olopade OI. Genetic testing in diverse populations: are researchers doing enough to get out the correct message? JAMA. 2007;298(24):2910–2911. doi: 10.1001/jama.298.24.2910. [DOI] [PubMed] [Google Scholar]
- Kauff ND, Satagopan JM, Robson ME, Scheuer L, Hensley M, Hudis CA, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002;346(21):1609–1615. doi: 10.1056/NEJMoa020119. [DOI] [PubMed] [Google Scholar]
- Lee R, Beattie M, Crawford B, Mak J, Stewart N, Komaromy M, et al. Recruitment, genetic counseling, and BRCA testing for underserved women at a public hospital. Genet Test. 2005;9(4):306–312. doi: 10.1089/gte.2005.9.306. [DOI] [PubMed] [Google Scholar]
- Lerman C, Biesecker B, Benkendorf JL, Kerner J, Gomez-Caminero A, Hughes C, et al. Controlled trial of pretest education approaches to enhance informed decision-making for BRCA1 gene testing. J Natl Cancer Inst. 1997;89(2):148–157. doi: 10.1093/jnci/89.2.148. [DOI] [PubMed] [Google Scholar]
- Lubitz RJ, Komaromy M, Crawford B, Beattie M, Lee R, Luce J, et al. Development and pilot evaluation of novel genetic educational materials designed for an underserved patient population. Genet Test. 2007;11(3):276–290. doi: 10.1089/gte.2007.0012. [DOI] [PubMed] [Google Scholar]
- McGee G, Malik C. Review of: Green MJ, Fost N. Breast cancer risk and genetic testing. JAMA. 1999;281:1652. doi: 10.1001/jama.281.17.1652. [DOI] [Google Scholar]
- Meijers-Heijboer H, van Geel B, van Putten WL, Henzen-Logmans SC, Seynaeve C, Menke-Pluymers MB, et al. Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2001;345(3):159–164. doi: 10.1056/NEJM200107193450301. [DOI] [PubMed] [Google Scholar]
- Meilleur KG, Littleton-Kearney MT. Interventions to improve patient education regarding multifactorial genetic conditions: a systematic review. Am J Med Genet A. 2009;149A(4):819–830. doi: 10.1002/ajmg.a.32723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D, Sylvester H, Lucas FL, Miesfeldt S. Cancer prevention and screening practices among women at risk for hereditary breast and ovarian cancer after genetic counseling in the community setting. Fam Cancer. 2009;8(4):277–287. doi: 10.1007/s10689-009-9242-z. [DOI] [PubMed] [Google Scholar]
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review—a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(Suppl 1):21–34. doi: 10.1258/1355819054308530. [DOI] [PubMed] [Google Scholar]
- Peters N, Rose A, Armstrong K. The association between race and attitudes about predictive genetic testing. Cancer Epidemiol Biomark Prev. 2004;13(3):361–365. [PubMed] [Google Scholar]
- Ponce NA, Afable-Munsuz A, Nordyke RJ. Conceptualising the impact of genetic testing on cancer disparities in the USA. Int J Healthc Technol Manage. 2007;8(5):536–548. doi: 10.1504/IJHTM.2007.013522. [DOI] [Google Scholar]
- Ramirez AG, Aparicio-Ting FE, de Majors SS, Miller AR. Interest, awareness, and perceptions of genetic testing among Hispanic family members of breast cancer survivors. Ethn Dis. 2006;16(2):398–403. [PubMed] [Google Scholar]
- Rebbeck TR, Lynch HT, Neuhausen SL, Narod SA, Van’t Veer L, Garber JE, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346(21):1616–1622. doi: 10.1056/NEJMoa012158. [DOI] [PubMed] [Google Scholar]
- Rubinstein WS. Computer-based genetic counseling. JAMA. 1999;282(18):1719–1720. doi: 10.1001/jama.282.18.1719. [DOI] [PubMed] [Google Scholar]
- Schaefer GB, Dunston GM. Health-care disparities in medical genetics. In: Satcher D, Paimes RJ, editors. Multicultural medicine and health disparities. New York: McGraw-Hill; 2006. pp. 471–484. [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Singer E, Antonucci T, Van Hoewyk J. Racial and ethnic variations in knowledge and attitudes about genetic testing. Genet Test. 2004;8(1):31–43. doi: 10.1089/109065704323016012. [DOI] [PubMed] [Google Scholar]
- Strauss A. Qualitative Analysis for Social Scientists. New York: Cambridge University Press; 1987. [Google Scholar]
- Thomas SB, Fine MJ, Ibrahim SA. Health disparities: the importance of culture and health communication. Am J Public Health. 2004;94(12):2050. doi: 10.2105/AJPH.94.12.2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W. Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns. 2003;51(3):217–227. doi: 10.1016/S0738-3991(02)00219-7. [DOI] [PubMed] [Google Scholar]
- US DHHS. (2000). Healthy People 2010. 2nd ed. Understanding and Improving Health and Objectives for Improving Health. 2 vols. Washington, DC: U.S. Government Printing Office.
- Vadaparampil ST, Wideroff L, Breen N, Trapido E. The impact of acculturation on awareness of genetic testing for increased cancer risk among Hispanics in the year 2000 National Health Interview Survey. Cancer Epidemiol Biomark Prev. 2006;15(4):618–623. doi: 10.1158/1055-9965.EPI-05-0378. [DOI] [PubMed] [Google Scholar]
- Wang C, Gonzalez R, Milliron KJ, Strecher VJ, Merajver SD. Genetic counseling for BRCA1/2: a randomized controlled trial of two strategies to facilitate the education and counseling process. Am J Med Genet A. 2005;134A(1):66–73. doi: 10.1002/ajmg.a.30577. [DOI] [PubMed] [Google Scholar]
- Warner E, Goel V, Ondrusek N, Thiel EC, Lavina H, Lickley A, et al. Pilot study of an information aid for women with a family history of breast cancer. Health Expect. 1999;2(2):118–128. doi: 10.1046/j.1369-6513.1999.00038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner E, Carroll J, Heisey R, Goel V, Meschino W, Lickley H, et al. Educating women about breast cancer. An intervention for women with a family history of breast cancer. Can Fam Physician. 2003;49(1):56–63. [PMC free article] [PubMed] [Google Scholar]
- Weitzman EA. Analyzing qualitative data with computer software. Health Serv Res. 1999;34(5 Pt 2):1241–1263. [PMC free article] [PubMed] [Google Scholar]
- Weitzman EA, Miles MB. Computer programs for qualitative data analysis: a software sourcebook. Thousand Oaks: Sage; 1995. [Google Scholar]
- Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274(21):1677–1682. doi: 10.1001/jama.1995.03530210031026. [DOI] [PubMed] [Google Scholar]
- Zimmerman RK, Tabbarah M, Nowalk MP, Raymund M, Jewell IK, Wilson SA, et al. Racial differences in beliefs about genetic screening among patients at inner-city neighborhood health centers. J Natl Med Assoc. 2006;98(3):370–377. [PMC free article] [PubMed] [Google Scholar]


