Abstract
Objective
To examine the efficacy and maintenance of developmentally adapted prolonged Exposure (PE-A) compared to active control Time Limited Dynamic Therapy (TLDP-A) for reducing post-traumatic and depressive symptoms in adolescent victims of single event traumas.
Method
38 adolescents (age 12–18) were randomly assigned to receive either PE-A or TLDP-A.
Results
Both treatments resulted in decreased post-traumatic stress disorder and depression, and increased functioning. PE-A exhibited greater reduction of PTSD and depression symptom severity, and greater increase in global functioning than did TDLP-A. At post-treatment, 68.4% of adolescents beginning treatment with PE-A and 36.8% of those beginning treatment with TLDP-A no longer met diagnostic criteria for PTSD. Treatment gains were maintained at 6 and 17 months follow-up.
Conclusions
Brief individual therapy is effective in reducing post-traumatic distress and behavioral trauma-focused components enhance efficacy.
Keywords: PTSD, treatment-outcome, adolescence, CBT, dynamic therapy
Introduction
Adolescents are at high risk of exposure to traumatic events and of developing post traumatic stress disorder (PTSD).1 When untreated, PTSD can lead to difficulties that last into adulthood, including depression, increased suicide attempts, psychiatric hospitalizations, and substance abuse.2 Adolescents exhibit a unique clinical expression of posttraumatic distress characterized by significant emotional and behavioral dysregulation.3 Despite the uniqueness of the adolescence period, most previous research combined childhood and adolescent samples.4 In addition, treatment research in traumatized children and adolescents has focused mainly on victims of sexual abuse.5 However, survivors of child sexual abuse seem to differ from victims of single-event traumas both in their presenting symptomatic picture,6 and in the components that might be needed for an effective intervention.7 To fill this gap, in the present study we focused on treatment for adolescents with PTSD related to single-event traumas.
Only a few studies have examined the treatment of single event-traumas in pediatric populations.8–9 Two randomized controlled studies have examined the efficacy of cognitive-behavioral group treatment (CBGT) for children victims of single event traumas,10–11 and both reported that the experimental interventions were more efficacious than wait-list control (WL). In addition, Smith et al.4 compared the efficacy of individually delivered CBT and WL in a pediatric sample. Trauma-focused CBT resulted in a greater reduction of post-trauma, depression, anxiety symptoms, and greater loss of diagnostic status (92%) as compared to WL (42%). CBT gains were maintained at 6 months follow-up. To date, trauma-focused therapy for single-event pediatric trauma has not been compared to an active control treatment.
Prolonged exposure therapy (PE) is an extensively studied form of individual CBT, which has been shown to be highly effective in the treatment of chronic PTSD.12–13 Recently, the PE protocol has been adapted for adolescents (PE-A14), and the intervention has been shown to be efficacious in an open study of child and adolescent victims.15 The adaptation emphasizes developmental sensitivity, modularity, and flexibility. In addition to core PE components of psychoeducation and exposure, PE-A includes more extensive case management and relapse prevention components. In the present study we compared PE-A to a non-directive, non-trauma-focused time-limited psychodynamic psychotherapy (TLDP) which served as a stringent active control condition.
TLDP16–17 is a form of brief dynamic therapy whose focus is not on the reduction of symptoms per-se (although such improvements are expected to occur) but rather on changing entrenched patterns of inter- and intra-personal relatedness. TLDP is based on the notion of a “central issue” and focuses on an unresolved conflict (e.g., dependence-independence or passiveness-activeness), on the patient’s negative self-image, and on emotions associated with the conflict. TLDP and other forms of brief dynamic therapy have been shown to be efficacious in reducing emotional distress in adult populations.18 In one study, more children reached functioning within the normal range following brief dynamic interventions compared to wait list controls.19 In the present study, we adapted TLDP for adolescents with single trauma related PTSD (TLDP-A). A treatment manual was created based on the work of James Mann16 and Lester Luborsky.20
We hypothesized that both PE-A and TLDP-A would significantly reduce posttraumatic as well as depressive symptom severity. On the basis of recent research suggesting that trauma-focused CBT in children and adolescents is more efficacious than other interventions in alleviating anxiety symptoms,21–22 we further hypothesized that PE-A would result in greater reductions in posttraumatic and depressive symptoms than TLDP-A. Finally, we hypothesized that gains made in both treatments would be maintained during follow-up period.
Method
Participants
The characteristics of the sample are described in Table 1. Inclusion criteria were: age 12 to 18; primary diagnosis of PTSD related to a single traumatic event; fluency in Hebrew. Exclusion criteria were: organic brain damage; mental retardation; ongoing trauma-related threat; suicidal ideation posing imminent danger; current substance dependence; pending legal issues; initiation of treatment with psychotropic medication within the past 6 weeks; and ongoing psychological treatment. However, adolescents with a history of substance use, conduct disorder, or presence of suicidal thoughts were not excluded from the study.
Table 1.
Demographic and trauma-related measures for an intent to treat adolescent sample (n=38)
| Total Sample | PE-A (n=19) | TLDP-A (n=19) | df | Statistic | |
|---|---|---|---|---|---|
| Age | 14.05 (2.27) | 14.21 (2.35) | 13.89 (2.23) | (1,36) | F=0.18 |
| Gender (Female) | 24 (63%) | 11 (57%) | 13(68%) | 1 | χ2=0.45 |
| Family Status (Parents married) | 18 (47%) | 9 (47%) | 9 (47%) | 1 | χ2=0.00 |
| Trauma Type | 4 | χ2=3.09 | |||
| TA | 5 (13%) | 4 (21%) | 1(0.5%) | ||
| MVA | 16 (42%) | 8 (42%) | 8 (42%) | ||
| NSA | 2 (0.5) | 1 (0.5%) | 1(0.5%) | ||
| SA | 8 (21%) | 4 (21%) | 4 (21%) | ||
| Other | 7 (18%) | 2 (10.5%) | 5 (26.5%) | ||
| Physical Injury In Trauma | 6 (15%) | 4 (21%) | 2 (10.5%) | 1 | χ2=0.79 |
| Time since Trauma (in months) | 18.51 (17.36) | 16.50 (18.80) | 20.42 (16.16) | (1,35) | F=0.46 |
| One or more Comorbid Disorder | 31 (81%) | 15 (79%) | 16 (84%) | 1 | χ2=0.68 |
| # Treatment Hours with Patient | 16.84 (3.78) | 16.78 (3.75) | 16.90 (3.02) | (1,36) | F=0.05 |
| # Treatment Hours with Parents | 2.66 (1.59) | 2.17 (1.90) | 3.00 (1.27) | (1,27) | F=0.17 |
Note: MVA= motor vehicle accidents; NSA= non-sexual assault; PE-A = prolonged exposure for adolescents; SA= sexual assault; TA= terrorist attacks; TLDP-A = time-limited dynamic psychotherapy for adolescents.
Procedure
The study was approved by the Institutional Review Board of the Bar-Ilan University, and by the Helsinki Ethics Committee of Schneider Children’s Medical Center (41100BO).
Upon referral, a telephone screen was conducted and the possibility of participating in the study was discussed with parents. Consenting families were scheduled for an initial assessment, conducted by M.A. level clinicians who underwent 40 hours of training in study assessments. Participants and their parents read and signed informed assent/consent forms. Diagnosis of PTSD was based on a diagnostic interview administered to adolescents and their parent in one or two 1.5 hour sessions. All interviews were video-recorded, and each was discussed with senior psychologists and psychiatrists until a consensual decision was reached. If no consensus was reached following the initial intake procedure, the child and or the family were invited for an additional session.
Figure 1 illustrates participant flow. Between May 2005 and November 2007, 128 youth were assessed for possible inclusion in the trial. Sixty four did not meet criteria for PTSD, and 18 refused participation in the study. Of the 46 eligible and consented participants, 8 (17.4%) were not randomized and did not begin active treatment: Four changed their mind in the period between the intake and the beginning of treatment (1 preferred to receive treatment in the open clinic, 1 reported a spontaneous recovery and 2 reported difficulties commuting to the hospital). Four participants were excluded from the study before active treatment had begun because a pre-treatment meeting revealed problems that were more primary than PTSD: one developed transient psychotic symptoms, one developed a serious medical condition resulting in hospitalization, one revealed current substance dependence, and one was found to have a pending legal investigation. Those who did not begin active treatment did not differ from those who began treatment in terms of age, gender, type of trauma, time since trauma, or any self-report measures (all p values >0.05).
Figure 1.
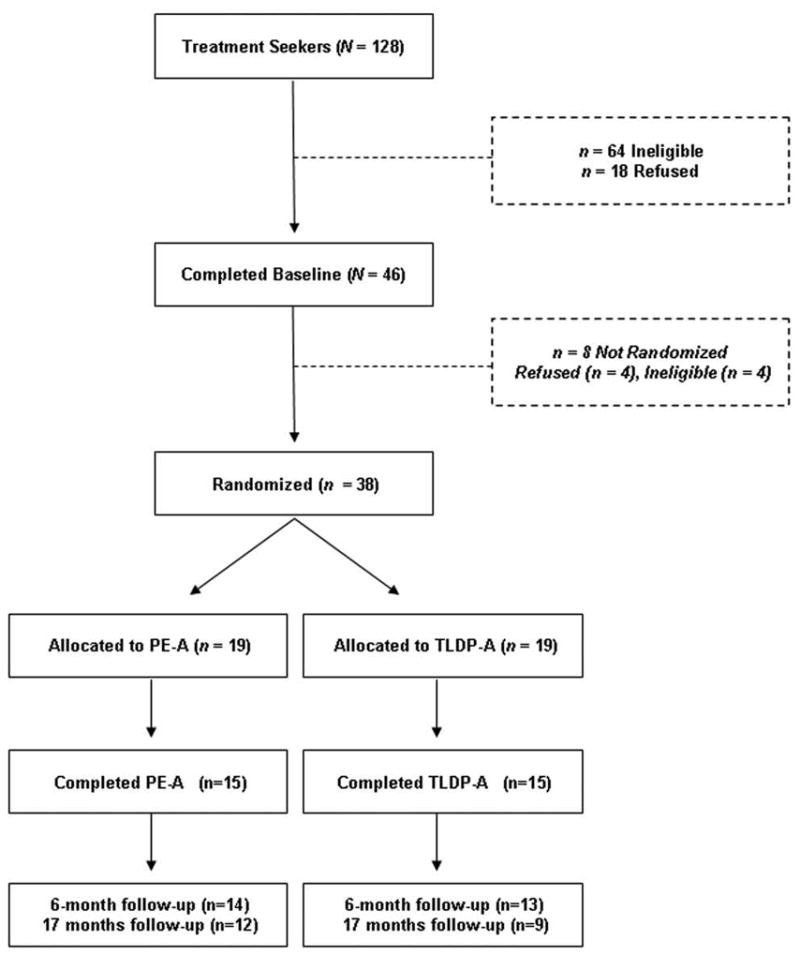
CONSORT diagram of participant flow through the protocol.
The remaining 38 adolescents were randomly assigned to either PE-A (n = 19) or TLDP-A (n = 19) using a block randomization method with a block size of 6. 23 The mean waiting time from intake to beginning of treatment was 1.5 months (range 0.3–3.2 months). Eight individuals (4 from PE-A and 4 from TLDP-A) dropped out of treatment: Four withdrew from treatment voluntarily, and an additional four were not included in the final sample as the clinical team deemed it necessary to initiate pharmacological treatment during the course of psychological treatment. Drop-outs did not differ from completers on any demographic, trauma-related or clinical variable (all ps > 0.05).
Participants completed the self-report measures assessing the severity of PTSD and depressive symptoms before every session. To examine the maintenance of treatment gains, participants were assessed at approximately 6 months post-treatment (average time since treatment termination 5.8 months, SD=2.4 months). Of the 30 treatment completers, 27 individuals (14 from PE and 13 from TLDP) completed 6 month follow-up. The post-treatment and follow-up assessments included a diagnostic interview, self-report measures of post-traumatic and depressive symptoms, and clinician rated global assessment of functioning. Twenty one participants (12 from PE and 9 from TLDP) completed a second follow-up approximately 17 months after treatment termination (M= 17.1; SD=1.7). Because of the difficulty in obtaining participants’ commitment for a long interview at this late point, PTSD diagnoses and clinician’s rated assessments were not obtained. Participants were assessed at pretreatment, post treatment, and follow-ups by assessors who were blind to the participants’ condition, did not deliver treatment, and were not involved in any other aspect of the trial. All assessments and treatment sessions were delivered as free services to the participants. No incentives were provided to participants for the assessments or treatment.
Treatments
The manualized treatments were provided by 11 MA-level clinicians (5 delivered PE and 6 TLDP) who received weekly group supervision. The PE-A therapists attended a 5-day training workshop conducted by E.F. and E.Y. The TLDP-A therapists attended a 2-day workshop conducted by L.R. Throughout the treatment, E.G.S. conducted weekly supervision meetings with the PE-A therapists, and L.R. conducted weekly supervision meetings with the TLDP-A therapists. All treatment sessions were videotaped and watched by supervisors to ensure treatment fidelity, and weekly verbal corrective feedback was provided to the therapists. Both treatments included 1–3 pre-treatment sessions devoted to case management with the adolescent and/or parents (For more details see Foa et al.14).
PE-A
PE-A consisted of 12 to 15 weekly sessions of 60–90 minutes, with the number and length of sessions determined according to the patients’ characteristics (e.g., shorter sessions for young patients and for participants with ADHD). The PE-A manual was comprised of 3 modules. The first module was devoted to psychoeducation and treatment planning and consisted of 2–3 sessions at the beginning of treatment. During these sessions, information was gathered, treatment rationale was presented and breathing exercises were conducted. The second module was devoted to exposure and consisted of 8–9 sessions. This module included presentation of the rationale of exposure, construction of an in-vivo exposure hierarchy, in-session exposure with the therapist, and assignment of in-vivo exposures as homework. Additional homework included in-vivo exposure to objectively safe situations that caused anxiety or that were avoided. In later sessions of this module homework was reviewed, imaginal exposure conducted, and homework for the next session was assigned. Imaginal exposure consisted of revisiting the traumatic event in imagination and recounting the memory verbally in the present tense. The revisiting of the traumatic memory was repeated if necessary in order to engage the memory of the trauma for 30–45 minutes. Imaginal exposure was tape-recorded, and participants were instructed to listen to the tapes daily at home. The third and final module focused on treatment termination and relapse prevention and consisted of 2 to 3 sessions. This module included a discussion of possible future challenges and ways of coping with them. In addition, a discussion of the treatment course, the gains made, and areas that require further work was conducted, thus summarizing treatment (for more details see Foa et al.14). Mean number of sessions in the PE-A condition was 13.42 and mean therapist hours per patient were 16.78.
TLDP-A
TLDP-A consisted of 15 to 18 50 minute sessions. In TLDP-A the initial sessions were primarily focused on building rapport and working alliance, as well as defining the central issue (2–3 sessions). The remaining sessions were devoted to “working through” the central issue. Patients were encouraged to share their inner thoughts, daily difficulties and free associations, while the therapist used selective listening and interpretation of themes related to the central issue. Therapists did not mention the traumatic event, and if the patient brought up details of the memory, they referred to the meaning of the event in the context of the central issue, without further encouragement to discuss the memory. Treatment termination and the upcoming separation was mentioned and discussed from early in the treatment, so that the processing of this as well as other meaningful separations in the patient’s life were understood and used in the context of the patient’s central issue. Mean number of sessions in the TLDP-A condition was 16.90 and thus mean therapist hours was 16.90. Thus, treatment hours were almost identical in both conditions.
Treatment Adherence
Adherence to treatment protocol was monitored during weekly supervision meetings. In addition, we randomly selected and rated videotapes of 20 therapy sessions (as in Foa et al.24). Using adherence manuals, three raters (who were unrelated to the study’s treatment process) were trained to conduct the adherence ratings. They reviewed session videotapes, rated each essential component as present or absent, and monitored for protocol violations. Of these sessions, 5 (25%) were rated independently by two raters. Inter-rater reliability was .92. Therapists completed 97% of the components prescribed in the protocol.
Measures
Schedule of Affective Disorders and Schizophrenia for School-Age Children–Revised for DSM—IV (K-SADS-PL25)
The K-SADS-PL is a semi-structured interview, covering current and lifetime disorders. The K-SADS-PL is administered separately to the parent and to the child. It has well validated psychometric properties: high inter-rater reliability, test-retest reliability, predictive validity and construct validity.26 The present study used the full validated Hebrew version of the K-SADS-PL.27
Children’s Global Assessment Scale (CGAS28)
The CGAS is a clinician rated scale evaluating children’s global functioning. The CGAS has been found to have excellent psychometric properties in general pediatric populations.29 The CGAS is highly correlated with children’s general functioning and is moderately correlated with other measures of symptom severity.30 In the present sample, inter-rater reliability of the CGAS was 0.9431.
Child PTSD Symptom Scale (CPSS32)
The CPSS is a self-report questionnaire with 17 items assessing PTSD symptoms according to the DSM-IV. Foa et al.32 reported high internal consistency (α = 0.89), and excellent test-retest reliability (r = 0.84) for the total scale.
The Beck Depression Inventory (BDI33)
The BDI is a 21-item self-report questionnaire tapping cognitive, behavioral, and affective facets of depression. In a large meta-analysis,34 the BDI has shown high validity and reliability scores and high internal consistency (α=0.81–0.86).
Treatment Expectancy
Treatment expectancy was assessed by adolescents’ ratings on a 7-point Likert scale ranging from 1 (“I don’t expect this treatment to make any difference in my condition”) to 7 (“I expect this treatment to help me a lot”).
Satisfaction with treatment
Treatment satisfaction was assessed by adolescents’ ratings on a 7-point Likert scale ranging from 1 (“I am not at all satisfied with this treatment, it did not help my condition”) to 7 (“I am extremely satisfied with this treatment, it helped me a great deal”).
Therapeutic alliance
Therapeutic alliance was measured by the original 36-item Working Alliance Inventory (WAI35) assessed at session 4 (as in Gaston36).
Results
Sample Characteristics
Descriptive statistics for the sample are presented in Table 1. Out of 38 participants, 24 (63%) were girls; 18 (47%) were living with both their biological parents, 5 (13%) were on stable psychiatric medication regiment, 31 (81%) had at least one comorbid disorder – 19 had one additional internalizing disorder, 5 had an additional externalizing disorder, and 6 had internalizing and externalizing disorders. No differences were found between treatment conditions at baseline on any demographic or trauma-related measure (see Table 1).
In the following section we first present treatment efficacy at post-treatment, followed by the presentation of maintenance of gains and categorical outcomes. Results for the completer sample were almost identical to those of the intent-to-treat (ITT) sample with missing data handled with the Last-Observation-Carried-Forward (LOCF) method. We thus report only ITT analyses.
Treatment Efficacy at Post-treatment
We conducted a series of repeated-measure ANOVAs to examine the efficacy of both treatments on severity of post-traumatic distress (CPSS), severity of depression (BDI) and clinician rated global functioning (CGAS). In each of the analyses, Time was a within subjects independent variable with 2 levels (pre-treatment vs. post-treatment) and Treatment Type was a between subjects independent variable with 2 levels (PE-A vs. TLDP-A). Descriptive statistics for outcome measures for ITT are presented in Table 2.
Table 2.
Clinical measures and between-groups effect sizes for the intent-to-treat sample (n=38)
| Total Sample | PE-A | TLDP-A | Group Effecta | Cohen’s d | |
|---|---|---|---|---|---|
| Posttraumatic symptoms (CPSS) | |||||
| Pre-treatment | 27.11 (11.05) | 28.37 (11.30) | 25.84 (10.94) | F(1,36) = 0.49 | 0.21 |
| Post-treatment | 12.03 (12.61) | 9.00 (12.41) | 15.05 (12.39) | F(1,35) = 4.15* | 0.45 |
| Follow-up 1 | 12.24 (12.95) | 8.84 (12.39) | 15.63 (12.92) | F(1,35) = 4.61* | 0.51 |
| Follow-up 2 | 12.71 (13.29) | 11.21 (13.39) | 14.21 (13.37) | F(1,35) = 1.32 | 0.21 |
| Depressive symptoms (BDI) | |||||
| Pre-treatment | 17.82 (11.79) | 20.95 (13.17) | 14.68 (9.57) | F(1,36) = 0.10 | 0.45 |
| Post-treatment | 7.37 (9.34) | 7.00 (9.08) | 7.74 (9.84) | F(1,35) = 1.38 | 0.07 |
| Follow-up 1 | 7.37 (8.44) | 6.53 (9.15) | 8.21 (7.82) | F(1,35) = 2.35 | 0.17 |
| Follow-up 2 | 7.97 (8.45) | 8.05 (9.66) | 7.89 (7.30) | F(1,35) = 0.74 | 0.02 |
| Global Functioning (CGAS) | |||||
| Pre-treatment | 54.53 (5.37) | 53.60 (5.82) | 55.47 (4.90) | F(1,36) = 0.30 | 0.28 |
| Post-treatment | 68.03 (12.15) | 71.84 (12.29) | 64.21 (11.03) | F(1,35) = 5.17* | 0.58 |
| Follow-up 1 | 66.34 (12.93) | 70.32 (13.70) | 62.37 (11.08) | F(1,35) = 5.72* | 0.55 |
| Treatment Expectancy | 5.13 (1.60) | 4.90 (1.73) | 5.29 (1.49) | F(1,36) = 0.34 | 0.16 |
| Therapeutic Alliance | 5.72 (0.79) | 5.79 (0.84) | 5.66 (0.76) | F(1,36) = 0.14 | 0.09 |
| Satisfaction with Treatment | 6.10 (1.26) | 6.33 (0.78) | 5.78 (1.72) | F(1,36) = 1.00 | 0.27 |
Note: Follow-up 1 took place 5.8 month following treatment termination (sd=2.4) and follow-up 2 took place 17.1 months following treatment termination (sd=1.7). BDI = Beck depression inventory; CGAS = children’s global assessment scale; CPSS = child posttraumatic stress disorder symptom scale; PE-A = prolonged exposure for adolescents; TLDP-A = time-limited dynamic psychotherapy for adolescents.
One-way Analyses of Variance (ANOVAs) were used to compare groups in pre-treatment scores; Analyses of Covariance (ANCOVAs) with pre-treatment scores as covariates were used to compare groups in post-treatment and follow-up scores.
p<0.05.
Post-traumatic Stress Symptoms (CPSS)
The results were consistent with our hypotheses. There was a main effect for Time (Wilks’s λ = 0.40, F(1,36)=55.06, p<0.001, η2=0.61) modified by a Time × Treatment Type interaction (Wilks’s λ = 0.89, F(1,36)=4.46, p<0.05, η2=0.11). For the whole sample, mean pre treatment scores were higher than post treatment scores (27.11 vs. 12.03). Participants in the PE-A condition reported a larger mean reduction in CPSS scores compared to individuals in the TLDP-A condition (19.4 vs. 10.8, respectively). Pre-post effect sizes (Cohen’s d) for the CPSS were 1.71 for PE-A and 0.87 for TLDP-A.
Depressive Symptoms (BDI)
Among the ITT sample there was a main effect for time (Wilks’s λ = 0.50, F(1,36)=36.42, p<0.001, η2=0.50) and a significant Time X Treatment interaction (Wilks’s λ = 0.90, F(1,36)=4.09, p<0.05, η2=0.10). For the whole sample, pre-treatment scores (17.82) were significantly higher than those in post-treatment (7.37). Also, participants in the PE-A condition reported greater reductions in BDI scores (13.95) compared to individuals in the TLDP-A condition (6.94), although the final scores for the two groups were almost identical (7.00 vs., 7.74, for PE-A and TLDP-A, respectively). Pre-post effect sizes for the BDI among the ITT sample were 1.06 for PE-A and 0.73 for TLDP-A. Thus, as hypothesized, both treatments significantly reduced depressive symptoms, but PE-A resulted in greater reductions compared to TLDP-A.
General functioning (CGAS)
As expected, CGAS scores were significantly higher at post-treatment (68.03) compared to pre-treatment (54.53; Wilks’s λ = 0.40, F(1,36)=53.22, p<0.001, η2=0.60). There was a significant Time X Treatment Type interaction (Wilks’s λ = 0.85, F(1,36)=6.33, p<0.05, η2=0.15). Participants in the PE-A condition reported a greater increase in CGAS scores (18.24) compared to individuals in the TLDP-A condition (8.74). Pre-post effect sizes of the CGAS among the ITT sample were 3.13 for PE-A and 1.78 for TLDP-A.
Treatment expectancy, satisfaction, and therapeutic alliance
We examined the difference in treatment expectancy, treatment satisfaction, and therapeutic alliance. As can be seen from Table 2, no differences were found between PE-A and TLDP-A on any of these measures (all Fs<1).
Maintenance of Gains
To examine whether gains achieved in treatment were maintained, we conducted a series of repeated-measures ANOVAs. Time was a within subjects independent variable with 3 levels (post-treatment vs. follow-up 1 vs. follow-up 2) and Treatment Type was a between-subjects variable with 2 levels (PE-A vs. TLDP-A). The dependent variables were CPSS, BDI and CGAS scores.
For both the CPSS and the BDI, no main effects or interaction effects were found (all ps >0.05). Thus, results suggest that gains are maintained during follow-up periods.
Because no CGAS data were collected at the second follow-up, we used an analysis with Time as a within subjects independent variable with 2 levels (post-treatment vs. follow-up) to examine general functioning. As before, Treatment Type was a between-subjects independent variable with 2 levels (PE-A vs. TLDP-A). A significant effect was found for Treatment Type (F(1,36)=4.34, p<0.05, η2=0.11) but not for Time or for the Time × Treatment Type interaction. This indicates that gains in global functioning were maintained during follow-up periods.
Clinically Meaningful Improvement
Diagnosis of PTSD
We assessed participants at post-treatment and at 6-months follow-up to examine if they met criteria for PTSD. In the PE-A condition 13 adolescents (68.4%) did not meet criteria for PTSD at post-treatment compared to 7 adolescents (36.8%) in the TLDP-A condition. This difference was on the verge of significance (χ2(1) = 3.80, p = 0.05). At the 6-month follow-up, 12 adolescents (63.2%) did not meet criteria for PTSD in the PE-A condition, compared to 5 adolescents (26.3%) in the TLDP-A condition. This difference was significant (χ2(1) = 5.22, p < 0.01). Diagnostic data were not available for the second follow-up.
Good end-state functioning
We defined good end-state functioning as (a) CGAS not in the clearly impaired range (CGAS>60) and low subjective distress as indicated by (b) CPSS<=11, and BDI<10 (clinical cutoffs for a diagnosis of PTSD and of mild depression). In the PE-A condition 14 adolescents (73.7%) met the criteria for good end-state at post-treatment compared to 6 adolescents (31.6%) in the TLDP-A condition. This difference was significant (χ2(1) = 6.76, p < 0.05). At the 6-months follow-up, 12 adolescents (63.2%) met the criteria for good end-state functioning in the PE-A condition, compared to 5 adolescents (26.3%) in the TLDP-A condition. This difference was significant as well (χ2(1) = 5.22, p < 0.01). No CGAS data were available for the second follow-up, and therefore good end-state functioning was not computed.
Discussion
The present study compared PE-A, a directive, trauma-focused cognitive-behavioral treatment, with TLDP-A, a non-directive, non trauma-focused psychodynamic treatment, among adolescents with PTSD resulting from single event trauma. The TLDP-A treatment served as a credible active control condition. Both interventions were successful in reducing distress and increasing functioning at posttreatment and at 6- and 17-month follow-up. Importantly, in an intent-to-treat sample, PE-A was superior to TLDP-A in reducing symptoms of PTSD and depression, enhancing functioning, facilitating loss of diagnostic status, and increasing overall improvement (e.g., exhibiting good end-state functioning) at post-treatment and 6 months following treatment termination. The advantage of PE-A over TLDP-A was observed at post treatment and at 6-months follow-up, but was no longer significant at 17 months post-treatment.
Importantly, the greater efficacy of PE-A in reducing post-traumatic symptoms and increasing overall level of functioning was observed despite the fact that treatment expectancy, treatment satisfaction, and therapeutic alliance were similar for both treatments. In addition, the drop-out rates from both treatments were identical (21%). These (relatively) low drop-out rates and significant clinical gains were obtained by clinicians with modest experience in treatment of trauma. This suggests that PE-A can be effectively disseminated to real-world settings.37
The findings of the present study suggest that adolescents benefit from developmentally adjusted PE and that their clinical benefit from treatment is similar to that observed in adults in reduction of PTSD and depression, and increase in functioning.13,23 Moreover, using a stringent definition of good end-state functioning, we found that 63.2% of adolescents met good end-state criteria at 6-month follow-up. In sum, we found meaningful and significant clinical changes in distress and in global functioning in a highly comorbid adolescent sample, heterogeneous with respect to trauma type and gender.
The substantial reductions in both posttraumatic and depressive symptoms observed in PE-A are congruent not only with the adult literature, but also with many previous studies regarding the efficacy of CBT among traumatized youth.4,9–11 Taken together, these findings suggest that individually administered CBT, with the common components of psychoeducation, exposure to trauma-related reminders, and revisiting of the traumatic experience, are highly effective for reduction of distress and enhancement of functioning in pediatric populations suffering from diverse traumas.
Consistent with our prediction, TLDP-A, while not as efficacious as PE-A, resulted in significant reductions in posttraumatic and depressive symptoms, and significant increases in clinician rated functioning. The percent of individuals with loss of PTSD diagnosis in the TLDP-A group was relatively low, and similar to the somewhat unusual and exceptionally effective waitlist condition in the Smith et al.4 study. Importantly, there are some significant differences between our results and those of Smith et al. First, the pre-post effect size for TLDP and Smith et al.’s WL are 0.87 and 0.27, respectively. Second, the reductions in PTSD severity scores in the TLDP and waitlist were 10.8 and 3 points, respectively. Moreover, the effects of TLDP-A are consistent with previous studies examining psychodynamic–oriented therapy in general17,38, and trauma related problems in adults.39
Some caveats should be noted. First, given our modest sample size, it is essential to replicate the efficacy of PE-A in a larger sample. Second, although our study employed a relatively long follow-up with a sub-sample of the participants, it is important to examine maintenance of treatment gains in an adolescent sample for a longer time as an early onset of anxiety and mood disorders is associated with a more pernicious course of psychopathology. In addition, future research should compare the effects of PE and TLDP with and without medication.
Several clinical implications emerged. First, both PE-A and TLDP-A were efficacious in reducing post-traumatic distress and increasing functioning for adolescent sufferers of PTSD following single-event traumas. Both treatments were well received by the patients and their families, and evinced positive pre-treatment expectancy, high therapeutic alliance and high satisfaction with clinical outcome. Second, directive trauma-focused intervention (PEA) showed superiority over psychodynamically oriented intervention immediately after treatment and at 6-months follow-up. Third, the interventions were efficacious even with highly comorbid, heterogeneous sample.
Acknowledgments
This study was funded by a NIMH R34 MH71660-01 awarded to Eva Gilboa-Schechtman.
The authors wish to thank all the therapists, the independent evaluators, and consultants for their help. In addition, we would like to thank Raya Mansour, Dr. Orit Krispin, Dr. Olga Goraly of Schneider Children’s Medical Center, and Dr. Kelly Chresman of University of Pennsylvania for their advice and support. Most of all we thank the adolescents and their families who participated in this project.
Footnotes
Clinical Trial Registry Information: Prolonged Exposure Therapy Versus Active Psychotherapy in Treating Post-Traumatic Stress Disorder in Adolescents; URL: http://clinicaltrials.gov; NCT00183690.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Eva Gilboa-Schechtman, Bar-Ilan University.
Dr. Edna Foa, University of Pennsylvania
Ms. Naama Shafran, Bar-Ilan University
Dr. Idan M. Aderka, Bar-Ilan University
Dr. Mark B. Powers, University of Pennsylvania
Dr. Lilach Rachamim, Schneider Children’s Medical Center.
Ms. Lea Rosenbach, Bar-Ilan University
Dr. Elna Yadin, University of Pennsylvania
Dr. Alan Apter, Schneider Children’s Medical Center
References
- 1.Hanson RF, Borntrager C, Self-Brown S, et al. Relations among gender, violence exposure, and mental health: The national survey of adolescents. Am J Orthopsychiatry. 2008;78:313–321. doi: 10.1037/a0014056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warshaw MG, Fierman E, Pratt L, et al. Quality of life and dissociation in anxiety disorder patients with histories of trauma or PTSD. Am J Psychiatry. 1993;150:1512–1516. doi: 10.1176/ajp.150.10.1512. [DOI] [PubMed] [Google Scholar]
- 3.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. J Consult Clin Psychol. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- 4.Smith P, Yule W, Perrin S, Tranah T, Dalgeish T, Clark DM. Cognitive behavior therapy for PTSD in children and adolescents: a preliminary randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2007;46:1051–61. doi: 10.1097/CHI.0b013e318067e288. [DOI] [PubMed] [Google Scholar]
- 5.Adler Nevo G, Manassis K. Psychosocial treatment of pediatric posttraumatic stress disorder: The neglected field of single-incident trauma. Depress Anxiety. 2005;22:177–189. doi: 10.1002/da.20123. [DOI] [PubMed] [Google Scholar]
- 6.Terr LC. Childhood traumas: An outline and overview. Am J Psychiatry. 1991;148(1):10–20. doi: 10.1176/ajp.148.1.10. [DOI] [PubMed] [Google Scholar]
- 7.Feeny NC, Foa EB, Treadwell KRH, March J. Posttraumatic Stress Disorder in Youth: A Critical Review of the Cognitive and Behavioral Treatment Outcome Literature. Prof Psychol Res Pr. 2004;35:466–476. [Google Scholar]
- 8.Goenjian AK, Karayan I, Pynoos RS, et al. Outcome of psychotherapy among early adolescents after trauma. Am J Psychiatry. 1997;154:536–542. doi: 10.1176/ajp.154.4.536. [DOI] [PubMed] [Google Scholar]
- 9.March JS, Amaya-Jackson L, Murray MC, Schulte A. Cognitive behavioral psychotherapy for children and adolescents with posttraumatic stress disorder after a single-incident stressor. J Am Acad Child Adolesc Psychiatry. 1998;37:585–593. doi: 10.1097/00004583-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Chemtob CM, Nakashima J, Carlson JG. Brief treatment for elementary school children with disaster-related posttraumatic stress disorder: A field study. J Clin Psychol. 2002;58:99–112. doi: 10.1002/jclp.1131. [DOI] [PubMed] [Google Scholar]
- 11.Stein BD, Jaycox LH, Kataoka SH, et al. A mental health intervention for school children exposed to violence: A randomized controlled trial. J Am Med Assoc. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- 12.Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- 13.Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J Consult Clin Psychol. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foa EB, Chrestman K, Gilboa-Schechtman E. Prolonged Exposure manual for children and adolescents suffering from PTSD. Oxford University Press; 2008. [Google Scholar]
- 15.Foa EB, Gilboa-Schechtman E, Powers MB, Shafran N. Efficacy of prolonged exposure therapy for PTSD in adolescents. Symposium at the annual meeting of the International Society of Traumatic Stress Studies; Chicago, Illinois. November 2008. [Google Scholar]
- 16.Mann J. Time limited psychotherapy. Oxford, England: Harvard University Press; 1973. [Google Scholar]
- 17.Shefler G, Dasberg H, Ben-Shakhar G. A randomized controlled outcome and follow-up study of Mann’s time-limited psychotherapy. J Consult Clin Psychol. 1995;63:585–593. doi: 10.1037//0022-006x.63.4.585. [DOI] [PubMed] [Google Scholar]
- 18.Lewis AJ, Dennerstein M, Gibbs PM. Short-term psychodynamic psychotherapy: Review of recent process and outcome studies. Aust N Z J Psychiatry. 2008;42:445–455. doi: 10.1080/00048670802050520. [DOI] [PubMed] [Google Scholar]
- 19.Muratori F, Picchi L, Casella C, Tancredi R, Milone A, Patarnello MG. Efficacy of brief dynamic psychotherapy for children with emotional disorders. Psychother Psychosom. 2002;71:28–38. doi: 10.1159/000049341. [DOI] [PubMed] [Google Scholar]
- 20.Luborsky L. Principles of psychoanalytic psychotherapy: A manual for supportive–expressive (SE) treatment. New York: Basic Books; 1984. [Google Scholar]
- 21.Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2004;43:393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: Initial treatment outcome findings. Child Maltreat. 1996;1:310–321. [Google Scholar]
- 23.Altman DG, Bland JM. How to randomise. BMJ. 1999;319:703–704. doi: 10.1136/bmj.319.7211.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Foa EB, Dancu CV, Hembree LA, Jaycox LH, Meadows EA, Stress GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. J Consult Clin Psychol. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- 25.Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Ambrosini PJ. Historical development and present status of the Schedule for Affective Disorders and Schizophrenia for school-age children (K-SADS) J Am Acad Child Adolesc Psychiatry. 2000;39:49–58. doi: 10.1097/00004583-200001000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Shanee N, Apter A, Weizman A. Psychometric properties of the K-SADS-PL in an Israeli adolescent clinical population. Isr J Psychiatry Relat Sci. 1997;34:179–186. [PubMed] [Google Scholar]
- 28.Shaffer D, Gould MS, Brasic J, et al. A children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 29.Schorre BEH, Vandvik IH. Global assessment of psychosocial functioning in child and adolescent psychiatry: A review of three unidimensional scales (CGAS, GAP, GAPD) Eur Child Adolesc Psychiatry. 2004;13:273–286. doi: 10.1007/s00787-004-0390-2. [DOI] [PubMed] [Google Scholar]
- 30.Green B, Shirk S, Hanze D, Wanstrath J. The Children’s Global Assessment Scale in clinical practice: an empirical evaluation. J Am Acad Child Adolesc Psychiatry. 1994;33:1158–1164. doi: 10.1097/00004583-199410000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Shafran N, Harish-Avidan S, Daie-Gabai A, Applebaum E, Shalit R, Gilboa-Schechtman E. Inter-Rater Reliability and External validity of the Children’s Global Assessment Scale (CGAS). Paper presented at the International Society for Traumatic Stress Studies; Chicago, IL. 2008. [Google Scholar]
- 32.Foa EB, Johnson KM, Feeny NC, Treadwell KRH. The child PTSD symptom scale: A preliminary examination of its psychometric properties. J Clin Child Psychol. 2001;30:376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- 33.Beck AT, Ward CH, Mendelson M, Mock JE, Erbaugh JK. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 34.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 35.Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. J Couns Psychol. 1989;36:223–233. [Google Scholar]
- 36.Gaston L. The concept of the alliance and its role in psychotherapy: Theoretical and empirical considerations. Psychotherapy: Theory, Research, Practice, Training. 1990;27:143–153. [Google Scholar]
- 37.Cook JM, Schnurr PP, Foa EB. Bridging the Gap Between Posttraumatic Stress Disorder Research and Clinical Practice: The Example of Exposure Therapy. Psychotherapy: Theory, Research, Practice, Training. 2004;41(4):374–387. [Google Scholar]
- 38.Leichsenring F, Rabung S, Leibing E. The efficacy of short-term psychodynamic psychotherapy in specific psychiatric disorders: A meta-analysis. Arch Gen Psychiatry. 2004;61:1208–1216. doi: 10.1001/archpsyc.61.12.1208. [DOI] [PubMed] [Google Scholar]
- 39.Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol. 1989;57:607–612. doi: 10.1037//0022-006x.57.5.607. [DOI] [PubMed] [Google Scholar]


