Abstract
Objective
To summarize the prevalence of retinal vein occlusion (RVO) from studies in the United States, Europe, Asia, and Australia.
Design
Pooled analysis using individual population-based data.
Participants
Individual participant data from population-based studies around the world that had ascertained RVO from fundus photographs.
Methods
Each study provided data on branch RVO and central RVO by age, sex, and ethnicity. Prevalence rates were directly age and sex standardized to the 2008 world population aged 30 years and older. Estimates were calculated by study and, after pooling, by ethnicity. Summary estimates included studies in which RVO was assessed from fundus photographs on ≥2 fields of both eyes.
Main Outcome Measures
Any RVO, CRVO, or BRVO.
Results
The combined pooled data contained 68,751 individuals from 15 studies, with participants’ ages ranging from 30 to 101 years. In analyses of 11 studies that assessed ≥2 fundus fields of both eyes (n=49,869), the age- and sex-standardized prevalence was 5.20 per 1000 (confidence interval [CI], 4.40–5.99) for any RVO, 4.42 per 1000 (CI, 3.65–5.19) for BRVO, and 0.80 per 1000 (CI, 0.61–0.99) for CRVO. Prevalence varied by race/ethnicity and increased with age, but did not differ by gender. The age- and sex-standardized prevalence of any RVO was 3.7 per 1000 (CI, 2.8–4.6) in whites (5 studies), 3.9 per 1000 (CI, 1.8–6.0) in blacks (1 study), 5.7 per 1000 (CI, 4.5–6.8) in Asians (6 studies), and 6.9 per 1000 (CI, 5.7–8.3) in Hispanics (3 studies). Prevalence for CRVO was lower than BRVO in all ethnic populations. On the basis of these data, an estimated 16.4 million (CI, 13.9–18.9) adults are affected by RVO, with 2.5 million (CI, 1.9–3.1) affected by CRVO and 13.9 million (CI, 11.5–16.4) affected by BRVO. Study limitations include non-uniform sampling frames in identifying study participants and in acquisition and grading of RVO data.
Conclusions
Our study provides summary data on the prevalence of RVO and suggests that approximately 16 million people may have this condition. Research on preventive and treatment strategies for this sight-threatening eye disease is needed.
Retinal vein occlusion (RVO) is one of the most common causes of acquired retinal vascular abnormality in adults and a frequent cause of visual loss. Despite being recognized at least as early as 18551 and the subject of more than 3000 publications, there are few data on the prevalence of RVO in the general population, with current estimates derived largely from studies in white populations.2–4 More recently, population data have emerged from other racial/ethnic groups, such as in Chinese,5 Hispanics,6 and Asian Malays.7 The reported prevalence of RVO varies between 0.3%4 and 1.6%.3 The variability in prevalence rates is likely related to the small number of RVO cases in any single study, differing study methodologies (e.g., retinal photography), and possible racial/ethnic differences in distributions of RVO risk factors.
Because of these limitations, estimates of RVO prevalence have been imprecise. Furthermore, most single studies rarely reported on the prevalence of different RVO subtypes, namely, central retinal vein occlusion (CRVO) and branch retinal vein occlusion (BRVO), which are important to distinguish because they have different risk factors,8,9 prognosis, and treatment.10–12
In this report, we combined individual-level data from 15 major population-based studies around the world and estimated the prevalence of BRVO and CRVO and their relationships with age, gender, and race/ethnicity.
Materials and Methods
Study Selection and Inclusion
A systematic review of the literature for all relevant population-based studies that undertook retinal photography was conducted. We searched all English language and human subject articles using a keyword search of MEDLINE (1950 to November 13, 2008), EMBASE (<1966 to December 18, 2008), Current Contents (1999 to December 18, 2008), and the Cochrane Library (to December 18, 2008) using the following search terms: retinal photography OR retinal images OR fundus photography AND population based. A total of 1585 citations were identified as of December 18, 2008. Irrelevant and duplicate articles were excluded on the basis of a review of the titles and abstracts. The full text of the remaining articles was reviewed to ensure all studies met the inclusion criteria and did not meet the exclusion criteria. In addition, we further consulted with experts to identify population-based studies that had assessed the presence of RVO from fundus photographs, but which may not have published results examining RVO or in which assessment of RVO from retinal photographs was still ongoing.
Studies were excluded if they were not population-based (i.e., excluding studies of clinic patient samples), fundus photographs were not taken or were not taken for all subjects, or images were not graded for RVO or the grading did not distinguish RVO subtype. Studies included in this review were those population-based studies in which RVO diagnosis was based on retinal photographic grading by a trained grader. We identified 21 population-based studies in which fundus photographs were potentially graded for RVO; of these, 7 had reported on the prevalence of RVO.2–7
We then contacted the lead investigators of the identified studies to request collaboration. Collaborators were requested to provide data on the following: presence of RVO and subtypes (CRVO, BRVO), age, sex, and race/ethnicity. All studies had prior institutional review board approval and provided appropriately de-identified data for analysis.
In total, investigators from 15 of the 21 identified studies provided data: Atherosclerosis Risk in Communities Study, Beaver Dam Eye Study, Cardiovascular Health Study (CHS), Los Angeles Latino Eye Study, Multi-Ethnic Study of Atherosclerosis (MESA), and the Arizona Project on Vision, Evaluation, Research from the United States; EUREYE and Rotterdam Eye Study from Europe; Beijing Eye Study, Funagata Study, Handan Eye Study, Hisayama Study, Shihpai Eye Study, and Singapore Malay Eye Study from Asia; and the Blue Mountains Eye Study from Australia. Investigators of the remaining 6 studies that did not contribute data to this study did not want to participate, did not respond, or could not be contacted.
Definition of Retinal Vein Occlusion
All 15 studies had retinal photography performed to a standardized protocol. All photographs were graded for RVO on the basis of standard definitions, and the majority of studies used 1 of 4 fundus photograph reading centers: United States (Ocular Epidemiology Reading Center at the University of Wisconsin-Madison), The Netherlands (Rotterdam Grading Centre), and Australia (Centre for Vision Research, University of Sydney and the Centre for Eye Research Australia, University of Melbourne), where the RVO grading procedures were standardized.
Central retinal vein occlusion was defined to be present if there was retinal edema, optic disc hyperemia or edema, scattered superficial and deep retinal hemorrhages, and venous dilation.2–7 Long-standing CRVO was defined to be present if occluded or sheathed retinal veins or vascular anastomoses at the optic disc were detected. Branch retinal vein occlusion was defined as the presence of localized retinal edema, superficial and deep retinal hemorrhages, intraretinal microvascular abnormalities or anastomotic vessels, and venous dilation or venous sheathing within a sector of the retina corresponding to the obstructed vein.2–7 Retinal vein occlusion was defined as present when either BRVO or CRVO was detected in at least 1 eye.
Appraisal of Quality of Studies
Because there were no established guidelines on evaluating prevalence studies, we adopted and further modified the quality assessment criteria by de Weerd et al.13 The quality of all studies was assessed for the following attributes:
Representation of the general population, whereby participants selected should ideally by representative of the general population. Methods of achieving this may involve using population registries, inhabitants of a defined area, and people registered with a general practice. Participants attending health checkups may be biased and only cover certain population groups.
Appropriate recruitment of the population. Recruitment was considered appropriate if recruitment of participants was random or consecutive rather than performed for convenience.
Adequate response rate (>70%).
Objective documentation of the outcome, in this case, documentation by retinal photography performed according to standardized protocols and graded according to standard definitions.
A score of 3 or higher was considered adequate quality.
Statistical Analysis
Data from each study were checked for consistency in variable definitions before pooling. Race/ethnicity was categorized as Asian (Chinese, Chinese-American, Malay, people of Asian origin and Europeans of Indian, Indonesian, or Asian origin), black (African-Americans), Hispanic (Hispanic-Americans), and white (Europeans, and those of European origin).
Study-specific and pooled-data estimation of RVO prevalence rates were obtained using the direct method of age-sex-standardization to the 2008 world population aged 30 years and older.14 This standardization involved 6 age categories (30–39 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, and ≥80 years) in men and women separately. The calculation of 95% confidence intervals (CIs) for the standardized prevalence rates used a normal approximation and Breslow-Day standard errors, after being modified to use a binomial assumption for the variance of the crude stratum-specific rates.15 Crude prevalence rates per 1000 and Agresti-Coull modified Wald CIs were also calculated.
Initial analyses included data from all 15 studies. Subsequent analyses used only the 11 studies that had assessed RVO with 2 or more retinal photographic fields from both eyes of participants (considered to have high sensitivity in detection).
Supplementary analysis included logistic regression of the effect of number of photographic fields per eye and the number of eyes with photographs taken per participant and the effect of pharmacologic mydriasis on the likelihood of an RVO diagnosis (adjusted for study, age, sex, and ethnicity).
Results
Overall, we collated data for 68,751 participants from 15 studies from the United States, Europe, Asia, and Australia. Of these participants, 43.7% were male, 48.4% were white, 27.1% were Asian, 17.2% were Hispanic, and 7.2% were black. Summary characteristics of each of the included studies are presented in Table 1; detailed characteristics of the participants in each of these studies have been described in previous publications (Table 1).
Table 1.
Characteristics of Included Studies
| Country | N Subjects (% Male) | Mean Age (Range) | Ethnicity* | Eyes/Subject | Fields per Eye (Degree, Dilation, Camera Type) | Image Grading Center | No. of Quality Criteria† | |
|---|---|---|---|---|---|---|---|---|
| ARIC4,23 | USA | 12,604 (44.6) | 59.9 (49–73) | 77% were white, 23% were black | 1 eye | 1 field (45 degrees undilated, non-mydriatic, non-stereo) | Graded OERC | 3 (3) |
| BDES2 | USA | 4896 (43.8) | 62.1 (43–86) | 100% were white | Both | ≥3† fields (30 degrees dilated, mydriatic, 2 stereo, ≥1 non-stereo) | Graded OERC | 4 |
| Beijing Eye Study5,24 | China | 4439 (43.6) | 56.2 (40–101) | 100% were Asian (Chinese) | Both | 2 fields (45 degrees dilated, mydriatic, non-stereo) | Graded at study site; confirmed AGC | 4 |
| BMES3,25 | Australia | 3651 (43.3) | 66.2 (45–97) | 99% were white | Both | 6 fields (30 degrees dilated, mydriatic, 2 stereo, 4 non-stereo) | Graded AGC | 4 |
| CHS4,26 | USA | 4249 (37.9) | 78.7 (69–101) | 83% were white, 17% were black | 1 eye | 1 field (45 degrees undilated, non-mydriatic, non-stereo) | Graded OERC | |
| EUREYE Study27 | European | 4753 (44.8) | 72.7 (64–99) | 100% were white | Both | 2 fields (35 degrees dilated, mydriatic, stereo) | Graded RGC | 3 (3) |
| Funagata Study28 | Japan | 1638 (43.5) | 60.0 (34–96) | 100% were Asian (Japanese) | 1 eye | 1 field (45 degrees undilated, non-mydriatic, non-stereo) | Graded AGC | 3 (3) |
| HandanEye Study29,30 | China | 6716 (46.5) | 52.0 (30–97) | 100% were Asian (Chinese) | Both | 2 fields (45 degrees dilated, non-mydriatic, non-stereo) | Graded at study site | 4 |
| Hisayama Study31 | Japan | 1775 (38.8) | 61.9 (40–96) | 100% were Asian (Japanese) | Both | 1 field (45 degrees dilated, non-mydriatic, non-stereo) | Graded at study site | 3 (3) |
| LALES32 | USA | 6357 (41.4) | 54.9 (40–98) | 100% were Hispanic | Both | ≥3† fields (30 degrees dilated, mydriatic, stereo) | Graded OERC | 4 |
| MESA6,33 | USA | 6176 (47.7) | 63.5 (46–87) | 39% were white, 27% were black, 22% were Hispanic, 12% were Asian (Chinese) | Both | 2 fields (45 degrees undilated, non-mydriatic, non-stereo) | Graded OERC | |
| Proyecto VER Study34 | USA | 4774 (38.8) | 56.9 (40–96) | 100% were Hispanic | Both | 3 fields (30 degrees dilated, mydriatic, stereo) | Graded OERC | 4 |
| Rotterdam Study35,36 | The Netherlands | 6418 (40.7) | 69.0 (55–99) | 98% were white, 1% were Asian (“Asian,” Indonesian, Indian) | Both | 2 fields (35 degrees dilated, mydriatic, stereo) | Graded RGC | 3 (3) |
| ShihpaiEye Study37 | Taiwan | 1058 (62.0) | 71.8 (65–90) | 100% were Asian (Chinese) | Both | ≥2† fields (35 degrees dilated, mydriatic, non-stereo) | Graded at study site | 3 (3) |
| SiMES7,38 | Singapore | 3280 (48.1) | 58.7 (40–80) | 100% were Asian (Malay) | Both | 2 fields (45 degrees dilated, non-mydriatic, non-stereo) | Graded AGC | 4 |
AGC = Australian Grading Centre (Centre for Vision Research, University of Sydney and the Centre for Eye Research Australia, University of Melbourne; ARIC = Atherosclerosis Risk in Communities Study; BDES = Beaver Damn Eye Study; BMES = Blue Mountains Eye Study; CHS = Cardiovascular Health Study; LALES = Los Angeles Latino Eye; OERC = Ocular Epidemiology Reading Center at the University of Wisconsin; RGC = Rotterdam Grading Centre; SiMES = Singapore Malay Eye Study; VER = Vision Evaluation and Research.
Totals for ethnicity may not equal 100%; some studies had subjects from other ethnic groups not included in this analysis.
The quality criteria failed: 1 = representation of the general population, 2 = appropriate recruitment of the population (random or consecutive), 3 = adequate response rate (>70%), 4 = objective outcome measurement by retinal photography performed to standard protocol and graded to standard criteria.
The majority of studies were conducted in only 1 ethnic group, except for the Atherosclerosis Risk in Communities Study, CHS, MESA, and Rotterdam studies, which had more than 1 ethnic group. Of the 15 studies, 11 assessed RVO from 2 or more retinal photographic fields of both eyes of each subject; of these 11 studies, retinal photographs were taken after pharmacologic mydriasis in 10 (the MESA differed). Of the studies that had 2 retinal fields photographed, 1 was centered at the optic disc (Early Treatment for Diabetic Retinopathy Study Field 1) and the other was centered on the macula (Early Treatment for Diabetic Retinopathy Study Field 2). Cameras varied between studies, ranging from a stereoscopic film-based mydriatic camera (Zeiss FF3 camera, Carl Zeiss, Oberkochen, Germany) to a digital non-mydriatic retinal camera (Canon CR-DGi with a 10D SLR backing, Canon, Tokyo, Japan).
The age- and sex-standardized prevalence (per 1000 persons) was 3.77 (CI, 3.08–4.46) for BRVO and 0.65 (CI, 0.49–0.80) for CRVO in the pooled analysis (Table 2). The standardized prevalence rates for CRVO in individual studies varied from 0.04 per 1000 (CI, 0–0.12) in CHS to 1.59 per 1000 (CI, 0.83–2.35) in the Blue Mountains Eye Study. Corresponding standardized BRVO prevalence ranged from 0.26 (CI, 0.07–0.45) in CHS to 9.32 (CI, 5.96–12.67) in Hisayama. There was no discernible difference between the age-standardized prevalence rates in men and women.
Table 2.
Age- and Sex-Standardized Prevalence of Central, Branch, and Any Retinal Vein Occlusion by Study
| Eyes/Subject | Field/Eye | CRVO |
BRVO |
Any RVO |
Standardized Prevalence* (/1000) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N (Total) | N (RVO) | N (Total) | N (RVO) | N (Total) | N (RVO) | CRVO | BRVO | Any RVO | |||
| All (15 studies) | Any | Any | 68,700 | 92 | 68,721 | 466 | 68,751 | 555 | 0.65 (0.49–0.80) | 3.77 (3.08–4.46) | 4.40 (3.69–5.11) |
| All (11 studies) | Both | ≥2 | 49,818 | 83 | 49,839 | 395 | 49,869 | 475 | 0.80 (0.61–0.99) | 4.42 (3.65–5.19) | 5.20 (4.40–5.99) |
| Men (15 studies) | Any | Any | 30,318 | 39 | 30,329 | 214 | 30,340 | 251 | 0.58 (0.35–0.80)† | 3.19 (2.66–3.71)† | 3.74 (3.17–4.31)† |
| Women (15 studies) | Any | Any | 38,382 | 53 | 38,392 | 252 | 38,411 | 304 | 0.72 (0.50–0.93)† | 4.33 (3.07–5.60)† | 5.04 (3.75–6.32)† |
| Men (11 studies) | Both | ≥2 | 22,170 | 35 | 22,181 | 180 | 22,192 | 213 | 0.71 (0.43–0.99)† | 3.76 (3.11–4.40)† | 4.43 (3.74–5.13)† |
| Women (11 studies) | Both | ≥2 | 27,648 | 48 | 27,658 | 215 | 27,677 | 262 | 0.89 (0.61–1.16)† | 5.07 (3.69–6.45)† | 5.93 (4.52–7.34)† |
| By Study | |||||||||||
| ARIC | 1 eye | 1 | 12,604 | 4 | 12,604 | 19 | 12,604 | 23 | 0.10 (0–0.19) | 0.45 (0.24–0.65) | 0.54 (0.32–0.77) |
| BDES | Both | 3 | 4792 | 8 | 4792 | 29 | 4792 | 37 | 0.99 (0.21–1.78) | 2.82 (1.65–4.00) | 3.82 (2.40–5.23) |
| Beijing Eye Study | Both | 2 | 4335 | 5 | 4335 | 31 | 4439 | 35 | 0.70 (0.04–1.35) | 4.67 (2.48–6.85) | 5.27 (2.99–7.55) |
| BMES | Both | 6 | 3492 | 17 | 3525 | 50 | 3542 | 67 | 1.59 (0.83–2.35) | 5.63 (3.94–7.32) | 7.14 (5.31–8.98) |
| CHS | 1 eye | 1 | 2824 | 1 | 2824 | 7 | 2824 | 8 | 0.04 (0–0.12) | 0.26 (0.07–0.45) | 0.30 (0.09–0.50) |
| EUREYE Study | Both | 2 | 4753 | 9 | 4753 | 30 | 4753 | 39 | 0.42 (0.12–0.72) | 1.48 (0.91–2.05) | 1.90 (1.25–2.54) |
| Funagata Study | 1 eye | 1 | 1502 | 1 | 1502 | 8 | 1502 | 9 | 0.21 (0–0.64) | 3.87 (0.13–7.61) | 4.09 (0.32–7.85) |
| Handan Eye Study | Both | 2 | 6716 | 6 | 6716 | 52 | 6716 | 58 | 0.55 (0.10–0.99) | 6.16 (4.30–8.01) | 6.70 (4.79–8.61) |
| Hisayama Study | Both | 1 | 1775 | 3 | 1775 | 35 | 1775 | 38 | 0.77 (0–1.64) | 9.32 (5.96–12.67) | 10.09 (6.62–13.55) |
| LALES | Both | 3 | 6013 | 7 | 6011 | 51 | 6013 | 58 | 0.79 (0.2–1.39) | 6.02 (4.31–7.73) | 6.75 (4.95–8.55) |
| MESA | Both | 2 | 6141 | 7 | 6132 | 35 | 6142 | 42 | 0.38 (0.09–0.66) | 2.87 (1.56–4.19) | 3.24 (1.90–4.58) |
| Proyecto VER Study | Both | 3 | 2909 | 10 | 2908 | 48 | 2909 | 58 | 1.52 (0.54–2.50) | 6.85 (4.89–8.81) | 8.37 (6.17–10.56) |
| Rotterdam Study | Both | 2 | 6418 | 6 | 6418 | 34 | 6418 | 39 | 0.39 (0.02–0.75) | 1.60 (0.98–2.22) | 1.94 (1.23–2.64) |
| Shihpai Eye Study | Both | 2 | 1058 | 3 | 1058 | 19 | 1058 | 22 | 0.38 (0–0.84) | 3.45 (1.72–5.18) | 3.83 (2.04–5.62) |
| SiMES | Both | 2 | 3265 | 5 | 3265 | 18 | 3265 | 22 | 0.82 (0.07–1.57) | 2.82 (1.46–4.19) | 3.56 (2.01–5.11) |
ARIC = Atherosclerosis Risk in Communities Study; BDES = Beaver Damn Eye Study; BMES = Blue Mountains Eye Study; BRVO = branch retinal vein occlusion; CHS = Cardiovascular Health Study; CRVO = central retinal vein occlusion; LALES = Los Angeles Latino Eye; n = study sample size; RVO = retinal vein occlusion; SiMES = Singapore Malay Eye Study; VER = Vision Evaluation and Research.
Prevalence per 1000 adults. Prevalence has been directly age- and sex-standardized to the 2008 world population aged ≥ 30 years (population data extracted from Ref. 14).
Denotes sex-specific estimates of prevalence are directly age standardized using the method and population as above.
Analyses confined to 11 studies that assessed 2 or more fields of both eyes, involving 49,869 participants, generated slightly higher prevalence estimates: Prevalence was 4.42 (CI, 3.65–5.19) for BRVO, 0.80 (CI, 0.61–0.99) for CRVO, and 5.20 (CI, 4.40–5.99) for any RVO per 1000 adults. By using these prevalence rates and the 2008 world population,14 we estimated that 16.4 million (CI, 13.9–18.9) adults worldwide are affected by RVO, 2.5 million (CI, 1.9–3.1) adults are affected by CRVO, and 13.9 million (CI, 11.5–16.4) adults are affected by BRVO. Analyses repeated including only the 10 studies in which pharmacologic mydriasis was performed resulted in similar estimates (data not shown).
The crude prevalence of all types of RVO increased with age (all P for trend <0.001; Table 3). This pattern was seen overall and in men and women separately. In studies that undertook photography of 2 or more fields in both eyes per subject, the age- and sex-standardized prevalence of BRVO varied across ethnic groups, with Asian and Hispanic groups exhibiting the highest prevalence and whites exhibiting the lowest prevalence (Fig 1). There were no obvious ethnic differences in CRVO prevalence.
Table 3.
Crude Prevalence of Central, Branch, and Any Retinal Vein Occlusion By Age and Gender
| Men |
Women |
All |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N (Total) | n (RVO) | Crude Prevalence/1000 (95% CI) | N (Total) | n (RVO) | Crude Prevalence/1000 (95% CI) | N (Total) | n (RVO) | Crude Prevalence/1000 (95% CI) | |
| CRVO | |||||||||
| Age 30–39 yrs | 560 | 0 | 0 (0–0) | 676 | 0 | 0 (0–0) | 1236 | 0 | 0 (0–0) |
| Age 40–49 yrs | 3184 | 1 | 0.31 (0–0.93) | 4101 | 1 | 0.24 (0–0.72) | 7285 | 2 | 0.27 (0–0.65) |
| Age 50–59 yrs | 5668 | 4 | 0.71 (0.01–1.4) | 7297 | 5 | 0.69 (0.08–1.29) | 12,965 | 9 | 0.69 (0.24–1.15) |
| Age 60–69 yrs | 6658 | 8 | 1.2 (0.37–2.03) | 7749 | 16 | 2.06 (1.05–3.08) | 14,407 | 24 | 1.67 (1–2.33) |
| Age 70–79 yrs | 5093 | 16 | 3.14 (1.6–4.68) | 6069 | 16 | 2.64 (1.35–3.93) | 11,162 | 32 | 2.87 (1.87–3.86) |
| Aged 80+ yrs | 1067 | 6 | 5.62 (1.14–10.11) | 1873 | 10 | 5.34 (2.04–8.64) | 2940 | 16 | 5.44 (2.78–8.1) |
| P trend* | <0.001 | <0.001 | <0.001 | ||||||
| BRVO | |||||||||
| Age 30–39 yrs | 560 | 0 | 0 (0–0) | 676 | 2 | 2.96 (0–7.05) | 1236 | 2 | 1.62 (0–3.86) |
| Age 40–49 yrs | 3184 | 5 | 1.57 (0.19–2.95) | 4101 | 5 | 1.22 (0.15–2.29) | 7285 | 10 | 1.37 (0.52–2.22) |
| Age 50–59 yrs | 5673 | 26 | 4.58 (2.83–6.34) | 7301 | 53 | 7.26 (5.31–9.21) | 12,974 | 79 | 6.09 (4.75–7.43) |
| Age 60–69 yrs | 6663 | 74 | 11.11 (8.59–13.62) | 7756 | 60 | 7.74 (5.79–9.69) | 14,419 | 134 | 9.29 (7.73–10.86) |
| Age 70–79 yrs | 5095 | 65 | 12.76 (9.68–15.84) | 6072 | 72 | 11.86 (9.14–14.58) | 11,167 | 137 | 12.27 (10.23–14.31) |
| Aged 80+ yrs | 1066 | 11 | 10.32 (4.25–16.39) | 1869 | 24 | 12.84 (7.74–17.95) | 2935 | 35 | 11.93 (8–15.85) |
| P trend* | <0.001 | <0.001 | <0.001 | ||||||
| Any RVO | |||||||||
| Age 30–39 yrs | 560 | 0 | 0 (0–0) | 676 | 2 | 2.96 (0–7.05) | 1236 | 2 | 1.62 (0–3.86) |
| Age 40–49 yrs | 3184 | 6 | 1.88 (0.38–3.39) | 4101 | 6 | 1.46 (0.29–2.63) | 7285 | 12 | 1.65 (0.72–2.58) |
| Age 50–59 yrs | 5673 | 30 | 5.29 (3.4–7.18) | 7301 | 58 | 7.94 (5.91–9.98) | 12,974 | 88 | 6.78 (5.37–8.2) |
| Age 60–69 yrs | 6666 | 81 | 12.15 (9.52–14.78) | 7758 | 75 | 9.67 (7.49–11.84) | 14,424 | 156 | 10.82 (9.13–12.5) |
| Age 70–79 yrs | 5100 | 80 | 15.69 (12.28–19.1) | 6078 | 88 | 14.48 (11.48–17.48) | 11,178 | 168 | 15.03 (12.77–17.29) |
| Aged 80+ yrs | 1069 | 17 | 15.9 (8.4–23.4) | 1880 | 34 | 18.09 (12.06–24.11) | 2949 | 51 | 17.29 (12.59–22) |
| P trend* | <0.001 | <0.001 | <0.001 | ||||||
BRVO = branch retinal vein occlusion; CI = confidence interval; CRVO = central retinal vein occlusion; RVO = retinal vein occlusion. Tables includes information from only those 11 studies that assessed ≥ 2 fields from both eyes per subject.
P relates to Cusick nonparametric test for trend across age groups.
Figure 1.
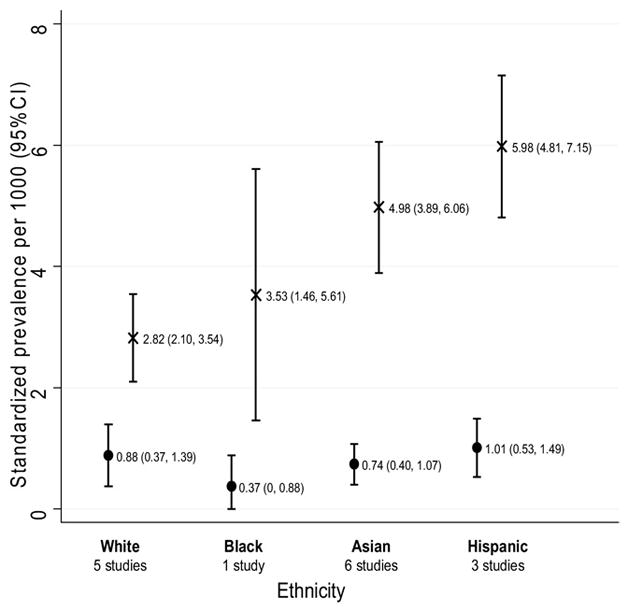
Age- and sex-standardized prevalence of CRVO and BRVO by ethnicity. Prevalence rates shown are per 1000 adults and include data from only those studies that assessed ≥2 fields of both eyes for each subject. Prevalence rates have been directly age- and sex-standardized to the 2008 world population aged ≥30 years (population data extracted from Ref. 15). CRVO (circles); BRVO (crosses); 95% CIs for prevalence estimates (capped vertical lines). BRVO = branch retinal vein occlusion; CI = confidence interval; CRVO = central retinal vein occlusion.
Discussion
The pooling of individual-level data from studies from the United States, Europe, Asia, and Australia allowed us to estimate more precisely the prevalence of RVO in the general adult population. On the basis of approximately 50,000 people from 11 studies that had assessed RVO from fundus photographs of 2 or more fields taken from each of the 2 eyes per participant, we estimate an age- and sex-standardized prevalence of 4.42 per 1000 persons for BRVO and 0.80 per 1000 persons for CRVO. The prevalence of RVO was similar between men and women, and increased with age. The prevalence of BRVO was highest in Asians and Hispanics and lowest in whites.
Previous population-based studies on RVO have provided rough estimates of RVO prevalence in their respective countries, often based on data from 1 region or city.2–7 This is the first synthesis of individual-level data from major population-based studies on RVO, with a sufficiently large sample to allow more precise estimation by age, sex, and ethnicity. The studies included had distinguished BRVO and CRVO using standardized retinal photographic grading; thus, we were able to provide prevalence estimates by subtypes of vein occlusion. Projected to the world population, approximately 16 million people may have occlusive venous disease in at least 1 eye. This estimated projection should be interpreted with caution because we did not have estimates of RVO from population-based studies in South America or Africa.
In keeping with findings from previous studies,2–7 our study found that age is an important risk factor for RVO.16 This likely reflects an increase in arteriosclerosis and in age-related vascular (e.g., systemic hypertension)17 and ocular (e.g., glaucoma or increased intraocular pressure) risk factors.9
Overall, these pooled data show the highest prevalence of BRVO in Asians and Hispanics and the lowest prevalence in whites, although the overlapping CIs suggest racial/ethnic differences are not statistically significant. In the MESA,6 the only study with 4 racial ethnic groups examined in 1 study, the crude prevalence of any RVO was similar across whites, blacks, Chinese, and Hispanics. It is worth noting that in the MESA, sample sizes of each ethnic group were relatively small, particularly the Chinese subgroup (n=724), and that all participants were US residents who were free of clinical cardiovascular disease (i.e., generally healthier study samples). Therefore, the MESA might not be sufficiently powered to detect meaningful ethnic difference in RVO prevalence and should not be expected to represent different ethnic groups outside the United States. Other studies of multiple ethnic samples, as a single study, also did not have sufficient numbers of RVO cases to examine racial/ethnic differences by RVO subtypes. The higher prevalence of BRVO in some racial/ethnic groups may reflect different population distributions of RVO risk factors. For example, the prevalence of hypertension and uncontrolled hypertension is reported to be higher in Asians18 and Hispanics19 than in whites.20,21
Strengths of the present study include the uniquely large sample size, inclusion of studies from different ethnic populations around the world, estimates of RVO subtypes (BRVO and CRVO), and inclusion of only those studies that used photographic documentation. These data provide a more precise estimate of the prevalence in the general population because they included RVO cases of both known, presumably symptomatic, and unknown (undiagnosed) causes. However, pooling data from many sources has many potential sources of heterogeneity.22 First, there could be substantial variations in study inclusion criteria, sample selection, and participation rates. Second, there were differences in methods used to detect and diagnose RVO across studies, including the use of mydriasis, choice of retinal photographic fields per eye, number of eyes examined per subject, photographic quality, case definitions (e.g., questionable or old RVOs), and the exclusion of other ocular pathologies. Third, given that most of the included studies are of subjects from 1 ethnic group, observed ethnic differences in prevalence should be interpreted with caution because these differences could be mostly due to differing study methodologies rather than true ethnic differences. Furthermore, definitions of particular ethnic group may differ across studies. For example, most studies used self-reported ethnicity, whereas the Rotterdam study used grand-parental country of birth to define ethnicity. Also, all of the included Hispanic participants were US residents, whereas the majority of Asian participants reside in Asian countries. Finally, the 2 studies that have assessed RVO in blacks have been in America and not Africa.
In conclusion, by using pooled data involving approximately 50,000 participants from the United States, Europe, Asia, and Australia, our study shows that BRVO affects 4 per 1000 persons and that CRVO affects 0.8 per 1000 persons. On the basis of these rates, projected to the world population, approximately 16 million adults are affected by RVO. We show that the prevalence of both BRVO and CRVO increases significantly with age but does not differ by gender. Possible racial/ethnic differences in the prevalence of BRVO may reflect differences in the prevalence of RVO risk factors. Understanding the key roles of the principal systemic and ocular factors, particularly hypertension for both RVO subtypes and glaucoma for CRVO, across these different populations will be important. Finally, our data suggest the need for further research to better understand the epidemiology of RVO, which could translate into the design of appropriate preventive and treatment strategies.
Acknowledgments
Funding for the data pooling analysis was provided by Global Health Outcomes Research, Allergan, Inc, Irvine, California.
Appendix 1. The International Eye Disease Consortium
Sophie Rogers, Rachel L. McIntosh, Ning Cheung, Lyndell Lim, Jie Jin Wang, Paul Mitchell, Ronald Klein, Barbara E. K. Klein, Liang Xu, Jost Jonas, Usha Chakravarthy, Astrid Fletcher, Ryo Kawasaki, Hidetoshi Yamashita, Takamasa Kayama, Ningli Wang, Yuanbo Liang, Miho Miyazaki-Yasuda, Tatsuro Ishibashi, Yutaka Kiyohara, Rohit Varma, Mary Frances Cotch, Sheila West, Beatriz Munoz, Johannes Vingerling, Lintje Ho, Paulus de Jong, Ching-Yu Cheng, Shih-Jen Chen, Seang Mei Saw, Tin Aung, Jonathan W. Kowalski, Hiep P. Nguyen, and Tien Y. Wong.
Footnotes
Presented at: Association for Research in Vision and Ophthalmology, 2008, Fort Lauderdale, Florida.
Financial Disclosure(s):
The author(s) have made the following disclosure(s):
Authors Kowalski and Nguyen are both employees of Allergan Inc., which provided funding for this project.
References
- 1.Liebreich R. Ophthalmoskopische Notizen: Ueber die Farbe des Augengrundes. Albrecht Von Graefes Arch Ophthalmol. 1855;1:333–43. [Google Scholar]
- 2.Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2000;98:133–41. [PMC free article] [PubMed] [Google Scholar]
- 3.Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia: the Blue Mountains Eye Study. Arch Ophthalmol. 1996;114:1243–7. doi: 10.1001/archopht.1996.01100140443012. [DOI] [PubMed] [Google Scholar]
- 4.Wong TY, Larsen EK, Klein R, et al. Cardiovascular risk factors for retinal vein occlusion and arteriolar emboli: the Atherosclerosis Risk in Communities & Cardiovascular Health studies. Ophthalmology. 2005;112:540–7. doi: 10.1016/j.ophtha.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 5.Liu W, Xu L, Jonas JB. Vein occlusion in Chinese subjects [letter] Ophthalmology. 2007;114:1795–6. doi: 10.1016/j.ophtha.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Cheung N, Klein R, Wang JJ, et al. Traditional and novel cardiovascular risk factors for retinal vein occlusion: the multiethnic study of atherosclerosis. Invest Ophthalmol Vis Sci. 2008;49:4297–302. doi: 10.1167/iovs.08-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lim LL, Cheung N, Wang JJ, et al. Prevalence and risk factors of retinal vein occlusion in an Asian population. Br J Ophthalmol. 2008;92:1316–9. doi: 10.1136/bjo.2008.140640. [DOI] [PubMed] [Google Scholar]
- 8.Hayreh SS, Zimmerman B, McCarthy MJ, Podhajsky P. Systemic diseases associated with various types of retinal vein occlusion. Am J Ophthalmol. 2001;131:61–77. doi: 10.1016/s0002-9394(00)00709-1. [DOI] [PubMed] [Google Scholar]
- 9.O’Mahoney PR, Wong DT, Ray JG. Retinal vein occlusion and traditional risk factors for atherosclerosis. Arch Ophthalmol. 2008;126:692–9. doi: 10.1001/archopht.126.5.692. [DOI] [PubMed] [Google Scholar]
- 10.Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005;24:493–519. doi: 10.1016/j.preteyeres.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 11.McIntosh RL, Mohamed Q, Saw SM, Wong TY. Interventions for branch retinal vein occlusion: an evidence-based systemic review. Ophthalmology. 2007;114:835–54. doi: 10.1016/j.ophtha.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Mohamed Q, McIntosh RL, Saw SM, Wong TY. Interventions for central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2007;114:507–19. 524. doi: 10.1016/j.ophtha.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 13.de Weerd M, Greving JP, de Jong AW, et al. Prevalence of asymptomatic carotid artery stenosis according to age and sex: systematic review and metaregression analysis. Stroke. 2009;40:1105–13. doi: 10.1161/STROKEAHA.108.532218. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Census Bureau. International Data Base. [Accessed July 7, 2009.];Total Midyear Population for the World: 1950–2050. Available at: http://www.census.gov/ipc/www/idb/region.php.
- 15.Keyfitz N. 3. Sampling variance of standardized mortality rates. Hum Biol. 1966;38:309–17. [PubMed] [Google Scholar]
- 16.Verougstraete C. Is change of the vessel wall a risk factor for venous thrombosis [letter]? Lancet. 1999;353:2158. doi: 10.1016/S0140-6736(05)75596-3. [DOI] [PubMed] [Google Scholar]
- 17.Wong TY, Mitchell P. The eye in hypertension. Lancet. 2007;369:425–35. doi: 10.1016/S0140-6736(07)60198-6. [DOI] [PubMed] [Google Scholar]
- 18.Leenen FH, Dumais J, McInnis NH, et al. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ. 2008;178:1441–9. doi: 10.1503/cmaj.071340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Read JG, Gorman BK. Racial/ethnic differences in hypertension and depression among US adult women. Ethn Dis. 2007;17:389–96. [PubMed] [Google Scholar]
- 20.Giles T, Aranda JM, Jr, Suh DC, et al. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens (Greenwich) 2007;9:345–54. doi: 10.1111/j.1524-6175.2007.06432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ostchega Y, Hughes JP, Wright JD, et al. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008;21:159–65. doi: 10.1038/ajh.2007.32. [DOI] [PubMed] [Google Scholar]
- 22.Wong TY, Hyman L. Population-based studies in ophthalmology. Am J Ophthalmol. 2008;146:656–63. doi: 10.1016/j.ajo.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 23.ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 24.Xu L, Cui T, Zhang S, et al. Prevalence and risk factors of lens opacities in urban and rural Chinese in Beijing. Ophthalmology. 2006;113:747–55. doi: 10.1016/j.ophtha.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell P, Smith W, Attebo K, Wang JJ. Prevalence of age-related maculopathy in Australia: the Blue Mountains Eye Study. Ophthalmology. 1995;102:1450–60. doi: 10.1016/s0161-6420(95)30846-9. [DOI] [PubMed] [Google Scholar]
- 26.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–76. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 27.Augood C, Fletcher A, Bentham G, et al. Methods for a population-based study of the prevalence of and risk factors for age-related maculopathy and macular degeneration in elderly European populations: the EUREYE Study. Ophthalmic Epidemiol. 2004;11:117–29. doi: 10.1076/opep.11.2.117.28160. [DOI] [PubMed] [Google Scholar]
- 28.Kawasaki R, Wang JJ, Rochtchina E, et al. Cardiovascular risk factors and retinal microvascular signs in an adult Japanese population: the Funagata Study. Ophthalmology. 2006;113:1378–84. doi: 10.1016/j.ophtha.2006.02.052. [DOI] [PubMed] [Google Scholar]
- 29.Liang YB, Friedman DS, Wong TY, et al. Handan Eye Study Group. Prevalence and causes of low vision and blindness in a rural Chinese adult population: the Handan Eye Study. Ophthalmology. 2008;115:1965–72. doi: 10.1016/j.ophtha.2008.05.030. [DOI] [PubMed] [Google Scholar]
- 30.Wang FH, Liang YB, Zhang F, et al. Prevalence of diabetic retinopathy in rural China: the Handan Eye Study. Ophthalmology. 2009;116:461–7. doi: 10.1016/j.ophtha.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Oshima Y, Ishibashi T, Murata T, et al. Prevalence of age related maculopathy in a representative Japanese population: the Hisayama study. Br J Ophthalmol. 2001;85:1153–7. doi: 10.1136/bjo.85.10.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varma R, Paz SH, Azen SP, et al. Los Angeles Latino Eye Study Group. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111:1121–31. doi: 10.1016/j.ophtha.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Klein R, Klein BE, Knudtson MD, et al. Prevalence of age-related macular degeneration in 4 racial/ethnic groups in the multi-ethnic study of atherosclerosis. Ophthalmology. 2006;113:373–80. doi: 10.1016/j.ophtha.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 34.West SK, Klein R, Rodriguez J, et al. Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care. 2001;24:1204–9. doi: 10.2337/diacare.24.7.1204. [DOI] [PubMed] [Google Scholar]
- 35.Hofman A, Breteler MM, van Duijn CM, et al. The Rotterdam Study: objectives and design update. Eur J Epidemiol. 2007;22:819–29. doi: 10.1007/s10654-007-9199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Leeuwen R, Klaver CC, Vingerling JR, et al. The risk and natural course of age-related maculopathy: follow-up at 6 1/2 years in the Rotterdam study. Arch Ophthalmol. 2003;121:519–26. doi: 10.1001/archopht.121.4.519. [DOI] [PubMed] [Google Scholar]
- 37.Chen SJ, Cheng CY, Peng KL, et al. Prevalence and associated risk factors of age-related macular degeneration in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Invest Ophthalmol Vis Sci. 2008;49:3126–33. doi: 10.1167/iovs.08-1803. [DOI] [PubMed] [Google Scholar]
- 38.Foong AW, Saw SM, Loo JL, et al. Rationale and methodology for a population-based study of eye diseases in Malay people: the Singapore Malay Eye Study (SiMES) Ophthalmic Epidemiol. 2007;14:25–35. doi: 10.1080/09286580600878844. [DOI] [PubMed] [Google Scholar]


