Abstract
Critical questions arise about misunderstandings of genetics. We interviewed for 2 h each, 64 individuals who had or were at risk for Huntington’s disease (HD), breast cancer or Alpha-1 antitrypsin deficiency. These individuals revealed various misunderstandings that can affect coping, and testing, treatment and reproductive decisions. A therapeutic misconception about testing appeared: that testing would be helpful in and of itself. Many believed they could control genetic disorders (even HD), yet these beliefs were often incorrect, and could impede coping, testing, and treatment. Misunderstandings about statistics and genetics often fueled each other, and reflected denial, and desires for hope and control. Emotional needs can thus outweigh understandings of genetics and statistics, and providers’ input. Individuals often maintained non-scientific beliefs, though embarrassed by these. These data have implications for care, and public and professional education. Misunderstandings’ persistence, despite realization of their inaccuracy, suggests that providers need to address not just cognitive facts, but underlying emotional issues.
Keywords: Health education, Doctor-patient communication, Decision-making, Health benefits, Genetic information, Genetic testing, Genetic counseling
Introduction
The increasing use of genetic tests through both providers and direct-to-consumer marketing raises critical questions of how individuals at risk for various diseases in fact view and understand genetic information that they may receive. Research has suggested that individuals undergo a process through which they “personalize” genetic risks and develop a personal sense of their vulnerability (Walter and Emery 2005), but what if these individuals’ views represent misunderstandings? A few studies have suggested that physicians, patients, and the public have deficiencies in knowledge about certain aspects of genetics (deVries et al. 2005; Emery et al. 1999; Kessler et al. 2007; Walter et al. 2004). But the full extent and impact of misperceptions of genetics have received relatively little systematic, focused attention. Increasingly, physicians, genetic counselors and other health care providers will have to interact with patients about genetics, and hence they may benefit from being as aware and sensitive as possible concerning patients’ misunderstandings.
Public Understanding of Genetics
Studies have suggested that most members of the public do not know basic aspects of genetics (e.g., that genes in fact reside in every cell in the body (Lanie et al. 2004; Shaw and Hurst 2008), and that humans have 46 chromosomes (Kessler et al. 2007). Many individuals do not understand that genes are in chromosomes (Kessler et al. 2007; Lanie et al. 2004). British-Pakistani genetic counseling patients revealed beliefs in religious explanations of diseases that have a genetic etiology, and notions that fathers contributed more genetic material than did mothers (Shaw and Hurst 2008). Some patients have been noted to believe that a child is more likely to inherit a disease mutation if s/he more physically resembles the parent with the mutation (Emslie et al. 2003), though many aspects of this phenomenon have not been explored. Most of the public also view “mutations” negatively (Condit et al. 2004). In Australia, knowledge of genetics was found to be associated with amount of education and income (Molster et al. 2009).
In addition, patients have been found to misunderstand several aspects of statistics—both broadly, and as related to genetic data—encountering difficulties in quantifying risk, and tending to overestimate it (Sivell et al. 2008). Researchers have suggested that patients “experience,” and “construct” perceptions of risk based on both their own and their family members’ medical experiences. Individuals may overestimate their risk for hereditary cancer (deVries et al. 2005), which may affect healthcare decisions and lead to inappropriate use of prevention and surveillance (d’Agincourt-Canning 2005; Sivell et al. 2008).
Models of Disease Risk Perceptions
Several models have been proposed to make sense of how individuals subjectively view the nature and cause of disease and “personalize” their risk for familial disease (Walter et al. 2004). Walter et al. (2004) reviewed 11 articles that examined lay understandings of familial risk for common chronic diseases (e.g., diabetes and heart disease), and they proposed a model of familial risk perception in which individuals assess the salience of family history of disease—i.e., the extent to which they believe they are at increased risk of disease. This process shapes coping, and senses of control, and can in turn influence the importance that patients give to genetic information. Yet questions remain of how individuals who themselves are at risk for a disease for which a genetic test exists and has been marketed (as opposed to diabetes and hypercholesterolemia, for which definitive genetic tests have not been yet marketed) view the risk and genetics involved. It is possible that the existence of a definitive test and/or undergoing genetic counseling may make these cognitive processes less subjective in certain ways.
Shiloh (2006) proposed Self Regulatory Theory as a framework for genetic counseling whereby clients process information actively, and “perceive risk” influenced by factors such as identity, consequences, cause, control, and timeline. Several theoretical models have also been suggested regarding representations of risks of illness in general. Etchegary and Perrier (2007) advocate a Heuristic-Systematic Model (HSM), which suggests that individuals base risk perceptions either superficially on heuristics, or more systematically (i.e., in a more exhaustive and deliberate way). These authors also advise that individuals’ perceived self-efficacy (i.e., perceived personal control regarding a risk or threat) can potentially reduce defensiveness toward, and heighten acceptance of, risk (Etchegary and Perrier 2007).
Purpose of the Present Study
Many critical questions remain about the potential roles of misunderstandings in these existing theoretical models. Though a few studies have probed how individuals construct their understandings of disease, questions emerge as to whether these conceptions may at times in fact represent misconceptions, and if so, whether such inaccuracies may impede health behaviors, and if so, how. Prior research has thus tended to focus on one of several areas (e.g., aspects of factual misunderstandings of genetics, or views of quantitative risk statistics, or personalizations of genetic risks) but has explored to a much lesser extent how these separate areas may possibly inter-relate.
It remains unclear what range and types of misunderstandings arise regarding the mechanisms of genes and their relationships to disease. Furthermore, it is unclear whether and how misunderstandings about statistics and genetics, respectively, interact and affect each other as well as affecting coping, testing, treatment, disclosure and reproductive decisions. Questions also persist about the kinds of misunderstandings, if any, patients have about genetics after genetic counseling, why such beliefs continue in the face of evidence to the contrary, and how patients view these misunderstandings. Moreover, much of the prior research has explored familial diseases for which no genetic tests exist, and/or the studies were conducted over 20 years ago. Since that time the amount of genetic information has burgeoned.
The extent to which the current availability of more definitive genetic information affects patient understandings is unknown. Though not all beliefs about a disease represent “misunderstandings,” some may, raising questions as to which, when, how, and with what implications. These issues are of increasing importance since misunderstandings may impede health decisions, but they may potentially be addressed through appropriate, targeted education. Therefore, as part of a study exploring several critical aspects and experiences of individuals confronting genetic disease (Klitzman 2010, Klitzman et al. 2007a, b, c), I decided to probe these issues concerning misunderstandings. The purpose of this research effort was to investigate the range of possible misunderstandings related to genetics that patients may have, the reasons why these may persist, and the implications that these may have.
Methods
Sample and Procedures
As shown in Table 1, I interviewed for 2 h each, 64 individuals, who had or were at risk for one of 3 disorders—Huntington’s disease (HD), breast cancer (BC), and Alpha-1 antitrypsin deficiency (AATD, or as participants refer to it, “Alpha”). As described elsewhere (Klitzman 2010), I selected a heterogeneous group in order to investigate more fully the ranges of issues and perspectives that could arise regarding genetic issues. To recruit participants, I distributed information about the study through clinics, other research studies at our institution, newsletters, flyers displayed on bulletin boards of our institution, and word of mouth. Individuals contacted the principal investigator if they were interested in participating.
Table 1.
Sample Characteristics (N=64)
| Disease |
Total | ||||
|---|---|---|---|---|---|
| BRCA | HD | Alpha | |||
| Gender | Female | 32 | 9 | 7 | 48 |
| Male | 0 | 12 | 4 | 16 | |
| Age | 20–29 | 3 | 3 | 0 | 6 |
| 30–39 | 8 | 12 | 0 | 20 | |
| 40–49 | 13 | 3 | 1 | 17 | |
| 50–59 | 3 | 3 | 5 | 11 | |
| 60–69 | 5 | 0 | 3 | 8 | |
| 70–79 | 0 | 0 | 2 | 2 | |
| Ethnicity | White | 21 | 18 | 11 | 50 |
| Black | 6 | 2 | 0 | 8 | |
| Asian | 2 | 0 | 0 | 2 | |
| Hispanic | 2 | 1 | 0 | 3 | |
| Other | 1 | 0 | 0 | 1 | |
| Education | High School | 4 | 4 | 2 | 10 |
| College | 15 | 10 | 8 | 33 | |
| Grad School | 9 | 7 | 1 | 17 | |
| Unknown | 4 | 0 | 0 | 4 | |
| Symptom Status | Symptomatic | 20 | 6 | 11 | 37 |
| Asymptomatic | 12 | 15 | 0 | 27 | |
| Test Status | Positive | 8 | 10 | 11 | 29 |
| Negative | 11 | 4 | 0 | 15 | |
| Indeterminate | 1 | 0 | 0 | 1 | |
| Not Tested | 12 | 7 | 0 | 19 | |
| Total | 32 | 21 | 11 | 64 | |
On theoretical grounds, Geertz (1973) has advocated studying aspects of individuals’ lives and social situations not by imposing external theoretical structures, but by trying to understand individuals’ own experiences, drawing on their own words and perspectives to obtain a “thick description.” Hence, to understand most fully the range of factors and issues that may be involved in genetic testing decisions, we used qualitative methods.
I conducted a confidential in-depth semi-structured interview with each participant. The interview concerned experiences of having, or being at risk for one of these three diseases. Interviews were conducted in the PI’s office and took approximately two hours, though varying somewhat in length. My Institutional Review Board approved the study, and all participants gave informed consent.
Interview Protocol
Relevant sample sections of the semi-structured interview guide are attached (see Appendix), through which I sought to obtain detailed descriptions of individuals’ views and decisions concerning genetic risk and testing, and related issues. I piloted the interview guide by refining it as I used it with each disease group, particularly with the first three to five participants in each group; and I used follow-up questions, as needed.
Data Analysis
Elements from Grounded Theory, as described by Strauss and Corbin (1990), were adapted for this study because I was interested in understanding a complex social process. These adapted methods are used in several other studies (Klitzman 2008; 2010; Klitzman and Bayer 2003). Specifically, grounded theory involves both deductive and inductive thinking, building inductively from the data to an understanding of themes and patterns within the data, and deductively drawing on frameworks from previous research and theories. The specific approach involved informed constant comparison in which data from different individuals were compared for similarities and differences to see whether these suggested hypotheses. Transcriptions and initial analyses of interviews were done during the period in which the interviews were being conducted and helped guide subsequent interviews. Interviews were conducted until saturation (redundancy of themes) was reached.
Once the full set of interviews was completed, subsequent analyses were conducted in two phases, primarily by the author together with a research assistant (RA) who had social science training. In phase I of the coding, we independently examined a subset of interviews to assess factors that shaped participants’ experiences, identifying categories of recurrent themes and issues that were subsequently given codes. Each of us assessed similarities and differences between participants, examining themes and categories that emerged, ranges of variation within categories, and variables that may be involved. We systematically coded blocks of text to assign “core” codes or categories. While reading the interviews, we inserted a topic name (code) beside each excerpt of the interview to indicate the themes being discussed. Next, we worked together to reconcile the two independently developed coding schemes into a single scheme, developing a coding manual and examining areas of disagreement until reaching consensus. New themes that did not fit into the original coding framework were discussed, and modifications were made in the manual when deemed appropriate.
In the next phase of the analysis, we subdivided thematic categories into secondary or subcodes, and then refined and merged these, when suggested by associations or overlap in the data. Codes and subcodes were then used in analysis of all of the interviews. Major codes (or categories) of text included, for example: mention of statistics, genetic mechanisms, and accuracy of genetic tests. Subcodes (or subthemes) were conceptual and thematic subdivisions of these larger categories, including, for example, specific types of misunderstandings of genetic mechanisms (e.g., receiving more genes from one parent or the other) and of statistics (e.g., that the existence of two options means that the odds of each occurring are 50%).
To ensure coding reliability, two coders analyzed all interviews. We examined areas of disagreement until consensus was reached. To enhance reliability, we triangulated the data with existing literature relating to understandings of genetic risks. These data also have a certain face validity. The Results section contains verbatim examples of text from the interviews. For each quotation, the participant is noted as: having or being at risk for Huntington’s disease (HD), breast cancer (BC) or Alpha 1 antitrypsin deficiency (A); being symptomatic (Sx) or asymptomatic (Asx); and being untested (Unt), or having had genetic tests that were mutation-positive (+), negative (−), or inconclusive. These respondents all knew of other individuals who confronted genetic risks—whether family members (e.g., parents and siblings) or fellow patients (often members of support groups or disease organizations). These interviewees revealed and discussed both their own understandings and misunderstandings, and those of these other people.
Results
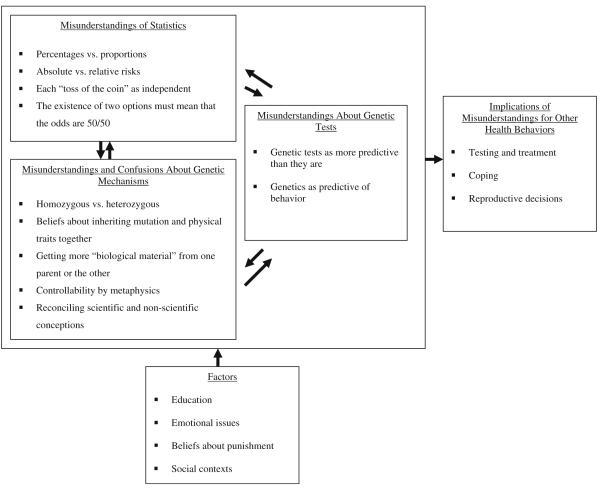
As shown in Fig. 1, individuals confronting genetic disease revealed a wide variety of misunderstandings about genetics, shaped by several factors, and in turn having several critical implications. As shown in Fig. 1, three main types of misunderstandings were extracted, concerning: (1) genetic tests, (2) genetic mechanisms, and (3) statistics. In addition, major themes arose concerning (1) factors that influenced these misunderstandings, and (2) implications of these misunderstandings for other health behaviors.
Fig. 1.
Themes Concerning Misunderstandings of Genetics.
Misunderstandings About Genetic Tests
Two broad types of misunderstandings about genetic tests arose: that genetic tests were more predictive than they actually are, and that they are predictive of behaviors for which no markers have in fact yet been discovered.
Genetic Tests as More Predictive Than They Are
Misunderstandings arose concerning the predictiveness and definitiveness of tests—usually that these tests were more predictive than they in fact were, and provided more certainty than they in fact did. One participant said,
My sister thought that if she got tested, she would know whether she was going to get breast cancer. She had a total misapprehension [sic] about what the test was about. It was complicated, because her gynecologist was encouraging her to get tested. BC7 (Sx/Unt)
Here, as elsewhere, physicians may have contributed to these beliefs in the predictiveness of these tests. At times, patients assume here that a test must be worthwhile if a physician encouraged it—that physicians consider a test important because of its relative predictiveness. This misunderstanding existed before and after undergoing genetic counseling. Individuals may sense these limitations intellectually, but nevertheless seek and desire certainty, leading to conflicting perspectives, or anxiety. The previous participant, a well-educated author, knew that scientific evidence can shift over time. She said:
People think the test will tell you whether you will get the disease or not, rather than it being a piece of information that says, “You’re probably at higher risk for getting this disease, but it doesn’t mean you’re going to get it.” Intellectually, I understand that. But emotionally, even that is hard to wrap my head around. Part of me is afraid that at some point, they’ll find out that if you have the gene, you will get breast and ovarian cancer—that at some point, with enough information, we’ll find it is inevitable. I totally believe those numbers. But part of me, this Nervous Nelly in the background, says, “Someday those numbers are going to be different.” BC7 (Sx/Unt)
This notion that the cause is both simple and single may reflect both common beliefs in genetic determinism (as seen in certain reports about genetics in the popular press) (Rothman 1998) and broader desires for certitude.
Many participants felt the identification of a gene implied that treatment existed, or would soon be developed—that prevention and treatment were possible, as is generally the case with other clinical tests that have been developed and used. Yet, genetic tests, though increasingly available, may differ substantially in their utility from other, long-established clinical tests.
Still, several interviewees assumed that tests for breast cancer, if encouraged by physicians, must be valuable.
Genetics as Predictive of Behavior
Popular myths exist, too, in part disseminated through the media, that behavioral genetics can uncover clear genetic explanations for certain complex behaviors.
You hear a lot about predispositions for drug addiction and alcoholism, and “the gay gene”—folk information. My wife works with scientists. They know what’s going on, but are the minority. HD7 (Asx/+)
She refers here to “folk information,” suggesting the existence of wide popular conceptions that may be incorrect. Interviewees who had studied basic biology at a college or advanced high school level appeared to grasp basic genetic concepts more, and be more wary than others of such claims.
Misunderstandings and Confusions About Genetic Mechanisms
Five main types of misunderstandings about genetic mechanisms emerged, related to: homozygosity vs. heterozygosity, beliefs about diseases and other physical traits being inherited together, individuals receiving more genes from one parent or the other, metaphysics affecting genetics, and ways of trying to reconcile scientific and non-scientific conceptions.
Homozygotes vs. Heterozygotes
For most interviewees, genetic concepts were too abstract, concerning statistical probabilities that are not part of their lived experiences. A few had vague or partial understandings of aspects of genetic mechanisms, struggling to grasp notions of, for example, dominance and recessivity. A woman with breast cancer and bipolar disorder said,
I don’t know: Is there such a thing as genes being just slightly there—you have this gene in a minute way, not a more dominant way? I don’t know how that works. BC12 (Sx/Unt)
Yet many more had problems grasping basic aspects of Mendelian patterns of inheritance. With Alpha, for example, homozygous patients often do not comprehend that all of their children would be at least heterozygotes.
Even the people who have Alpha don’t understand: First, that their children are going to be carriers. It happens all the time on the e-lists. They say: we want our children tested. And the children turn out to be carriers. Instead, they could have had the husband tested. There’s no need to test the child and to have it in his or her record! A8 (Sx/−)
This participant suggested that misunderstandings can have serious consequences, prompting testing that could in turn lead to discrimination, confusion and unnecessary stress.
Beliefs About Inheriting Mutations and Physical Traits Together
Many participants mistakenly thought that an individual more likely receives the mutation for a disease if he or she physically most resembles a parent with the disease. Even individuals with scientific training often failed to realize that such genes in fact sorted independently.
I always thought that because I looked more like my mother, I was at risk of getting the disease. HD18 (Sx/−)
Similarly, some felt they were “mutation-positive” because of psychological similarities to an affected family member (e.g., “because me and her are like two peas in a pod”). HD1 (Sx/+)
Others struggled to grasp these issues, drawing on their observations of their family over time, which may or may not lead to consistent conclusions. Many tried to articulate these similarities and differences. For instance, one man sought to describe how he looked physically more like his father and uncle than did his sister.
As a man, I’m obviously physically more like my father and uncle than is my sister. But there is also a certain way I move. I’ve always thought that my sister and I are much different. Something physically in her, the way that she carries herself, was different. HD15 (Asx/+)
Conversely, some felt that since they looked less like their affected parent than did a sibling, they therefore had escaped the gene. Such beliefs provided a sense of definitiveness one way or the other, as well as perhaps a sense of closeness to an affected, but beloved parent.
These conceptions of inheriting genes jointly for diseases and other traits extended across types of diseases, and appeared to suggest broader views of behavioral genetics and physiognomy (e.g., the notion that a child “takes after” one parent or whole side of the family more than the other). As one man said,
My oldest son is obviously his mother’s child. I always thought of him as more his mother than me, and my younger son as more me than my ex-wife. It’s obvious in body construction, and the problems they have—related to her lineage vs. mine. A4 (Sx/+)
These perceptions that behavior and physical traits sorted together, along with predispositions for disease, proved strong, leading to assumptions about one’s own and others’ test results, even in the face of contrary evidence and education. As one woman at-risk for breast cancer said,
When my sister came up positive, I thought, “I’m probably going to be positive as well.” I know it’s not logical, but I figured I probably got a good, big healthy dose of the genes from that side. I remember my high school biology, about what the percentages would be. But, it still struck me as probably a good chance. BC26 (Asx/−)
This woman in fact said she even wanted to have the mutation, because it was associated with intelligence.
I was a little disappointed that I didn’t have these mutations because they’re also supposed to give you a really high IQ. BC26 (Asx/−)
Folk beliefs (i.e., that the mutation is “supposed to give you a high IQ”), and personal observations grounded in apparent visual evidence and common sense (i.e. “it’s obvious in body construction”), rather than abstract intellectual understandings of genetic mechanisms, prove persuasive. As we shall see, despite contrary evidence, and recognition of their illogicality, these beliefs can prevail, in part due to desires for certainty in the face of uncertainty and anxiety. The persistence of these misunderstandings indicates their strength, and the challenges that health care providers face in addressing and correcting these.
In the face of fear, desires for certitude and explanation rather than randomness, chaos and confusion led some to extend such beliefs even to past generations, with searches through family history and pictures for answers regarding the source of disease:
I sat down and looked through all these old family pictures—a box of old black and whites. I tried to trace the disease through us—like “She’s got it.” Of course, all these people look just like me. So, by the end, I didn’t believe it anymore. HD12 (Asx/−)
Though this particular woman eventually questioned her hypothesis that she resembled affected relatives, her comments illustrate a desire to find links to other relatives.
Other individuals recognized the fallacy of their assumptions, but continued to hold them—as they were sources of hope that those who resembled unaffected family members would themselves be unaffected. Still, they struggled with the possible illogicality of these beliefs.
I look more like my father’s side of the family. I think that’s stupid, because I don’t think it really makes a difference who you look like. But I guess I’m hoping for the best. HD14 (Asx/+)
This interviewee acknowledges that this belief is not valid (is “stupid”), but he maintains it because of hope. The desire to avoid fatalism and despair can thus outweigh rational assessment. A few individuals balanced an acknowledgement of genetic risks vs. desires for hope, by believing that genetic diseases could skip generations. As one woman said about breast cancer: “There’s a strong possibility it runs in the family. I’m hoping it will skip a few generations. If it doesn’t, I hope it gets caught in time.” BC17 (Asx/Unt)
Getting More “Biological Material” From One Parent or the Other
Participants conceived of other mechanisms, involved with genetics, in a variety of ways that could mutually reinforce each other. For instance, as a mechanism for resembling one parent more than the other, many individuals imagined that they received “more” biological material (e.g., “cells” or genes) from one parent than the other. Similarly, one woman spoke of different “doses” of genetics, as if genes were drugs.
Outsiders may point out resemblances between a parent and a child, socially supporting these beliefs that offspring receive more material from one parent or the other. As one man said,
As you grow up, you start hearing, “You’re just like me when I was a kid.” So you assume: if I look more like him or her, then I’m probably going to get what he or she has. In high school, hereditary means: two parents come together and pass on what they have. Whatever they have, you have. So, if you look like your dad, then most likely, if he has green eyes, I have green eyes. My dad’s got big teeth, I got big teeth. My dad had pretty big hands, I have big hands. He was a pretty fast runner, I was a pretty fast runner. Now, you hear my dad has that disease and it’s hereditary, so “I got the disease.” You explain it in your head by saying, “I probably have more of his cells than her cells.” HD3 (Asx/Unt)
As a lawyer, he is highly educated and cites high school biology, but suggests the potency of these misunderstandings, and their inter-relationships to complex behavioral facts (e.g., athleticism) as genetic.
Many participants searched for metaphors to understand the nature, meanings and implications of genetics, which may nonetheless remain unclear. Individuals struggled to grasp notions of chromosomes.
There’s something wrong with me that’s not even physical—like my body or the blueprints of my body don’t work well. The computer that determines the functions of my body, the central processing unit, doesn’t work right. At any time, something can go wrong. It’s like I’m walking on one leg. I don’t have the checks and balances most people have. I have one chance to get it right. It was explained to me how the genes work. There are two: one from your mom, one from your dad. The one from my mom doesn’t really do its job. They’re supposed to take turns, but the other one is doing the job all the time. One is shooting blanks or something. BC13 (Asx/+)
This participant grappled with metaphors of architecture (blueprints), computers, and guns, but the exact details of chromosomes eluded her.
Controllability by Metaphysics
Beliefs arose that metaphysics, or the power of the mind over the body, could also control the “fatedness” of genetic disease. “New Age” beliefs emerged, reflecting “the power of positive thinking” to alter disease—that a patient can “will” the outcome of disease processes. Against perceptions of cruel randomness, many individuals yearned for a sense of control. Many were aware of the lack of scientific grounding for such beliefs, but espoused them nonetheless.
If I deal with my resentment, and not let myself get hopeless, why do I have to manifest this thing? It doesn’t have to happen…Maybe I can take a supplement, and not try to change or resent people. Maybe I don’t have to get it. HD12 (Asx/−)
This participant’s comments further suggest a possible antidote from unproven complementary and alternative medicine.
Altruistic wishes arose, invoking metaphysics, that others would not carry a gene because one does not wish them to. For example:
My siblings are never going to get anything because they’re my siblings, and I don’t want them to. BC11 (Sx/Unt)
Similarly, notions emerged that a parent would simply not give his or her children a mutation—as if it were a conscious choice—or that an individual has the power to eliminate a mutation from the family. Individuals thus assigned volition to genetics and inheritance. For instance, one woman felt that her dad was here on earth to get rid of the disease in the family. She believed her father willfully, stoically and heroically, “took on HD” to eliminate it.
I had this real strong feeling that my dad had come to clean it up, to finish off this nasty, ugly business, and that my sister and I were going to be fine. He took this thing on, and was gonna wrestle it down for us. I also thought that if anybody has it, it would probably be her. Three days after my dad’s funeral, she was going to get her results. She sat in front of me in the car. I put my hands on her, and thought, “Take it away. Make me have it, so you don’t have to.” My dad was the best support I ever had. I just really thought that he wouldn’t have given me such a thing. HD12 (Asx/−)
Reconciling Scientific and Nonscientific Conceptions
Even when undergoing genetic testing and counseling, individuals may maintain their earlier misunderstandings. They may even, in fact, seek ways of supporting these prior views. For example, one woman continued to believe that a child acquires more DNA from one parent or the other; she then tried to reconcile the seeming contradiction of physically resembling one parent’s family more, but receiving a mutation from the other side. She imagined a distinction between the inside vs. the outside of the body, distinguishing between surface and depth, with each coming more from one parent or the other. Her comments highlight patients’ needs often to understand these issues in simple, concrete ways.
I suppose I look more like my father’s family on the inside, and my mother’s side on the outside. BC26 (Asx/−)
To reconcile conflicting conceptions, and account for why one would or would not develop a disease, these individuals often drew, too, on beliefs about “triggers” that get “pulled.” At times, these beliefs resembled those concerning other non-genetic diseases, but differed somewhat, since genetics implies in itself a sense of causality. Yet this sense of causality then raised questions of how to assign blame for the disease. Some thought that a genetic basis of a disease did not make the diagnosis ineluctable, but gave a “head start,” facilitating it, and that other aspects of one’sbody or behavior could prompt symptoms. While some individuals had misunderstandings about this area, others struggled to comprehend the relative roles of genetics vs. other factors, reflecting potential confusion.
Some interviewees invoked metaphors of infection, which appeared to be more readily and concretely understood than genetics. Hence, mutations could be seen as lying dormant—as if they were invading life-forms. As one woman said, “If you’re genetically prone, maybe you have the genes, but they can stay dormant in the body for 30 years, and then be [like] Mad Cow disease.” BC1 (Asx/Unt) She and others groped for analogies from particular kinds of infectious agents—e.g., prions that can have decades-long incubation periods. The fact that she was at risk, but had not had cancer bolstered this view, which in turn helped dissuade her from testing. Though not explicitly misunderstanding genetics, she nonetheless reflected a search to grasp the uncertainties involved. She and others often sought concrete answers.
Misunderstandings of Statistics
Patients often had confusion and misunderstandings about not only genetics, but statistics as well, and they had difficulty knowing how to conceptualize and thus weigh this information. Four main subthemes arose here, related to: percentages vs. proportions, absolute vs. relative risks, each “toss of the coin” being independent, and the existence of two options meaning that the odds must be 50/50.
Percentages vs. Proportions
Participants did not always grasp differences between percentages and proportions, potentially exacerbating confusion and miscomprehension. Due to his long years of professional experience, an engineer with Alpha perceived confusion about genetics among his fellow patients. He described these misunderstandings:
A lot of people don’t understand arithmetic odds. I’m an engineer. I’ll say, “There’s a 3% chance that your mate is going to be a carrier.” They say, “Well, talk to me in real numbers.” So, then I have to say: “There’s a one in 35 chance.” Maybe they understand it. I try to explain it in simple terms. They don’t understand percent. I’ve always worked with numbers. I’m kind of anal. A10 (Sx/+)
Both his work as an engineer, and his psychological and cognitive predisposition (“kind of anal”) helped him here, but distinguished him from most other patients that he encountered and that I interviewed.
Absolute vs. Relative Risks
As suggested previously, confusion emerged as well concerning interpretations of absolute vs. relative risks. A positive genetic test may double a patient’s risk from 1/1000 to 2/1000, though the odds of occurrence in fact remain relatively rare, raising questions as to why individuals may give and/or accept only one of these sets of statistics about a situation, rather than wanting both. One woman had degrees in both Mathematics and Business and had been a banker and, at the time of the interview, was teaching math. She described how other patients may frequently confuse these two sets of statistics. One such patient:
…said that if I took Tamoxifen, I was going to double my chances of uterine cancer. That was scary. But then I said, well what are my chances if I don’t take it? They said: one in 10,000. I said: “That means it could be two in 10,000?” I said, “Fine, just give it to me.” People sometimes throw numbers out, and if you don’t understand or question it, it could be pretty scary. BC23 (Sx/−)
Thus, one needs to look at both sets of numbers. Yet even health care providers may fail to do so, and use statistics incompletely and sub-optimally. This woman knew, because she had advanced quantitative education, to ask about absolute risks that were still small.
With graduate school training, she felt that doctors spoke to her in a way that enabled her to make an informed decision, yet she wondered how less educated patients handled all of the information.
In the waiting room, there are a wide range of socioeconomic levels. How do some of these people deal with this information? How is it presented to them? A lot of information comes at you fast and furious, and you’re trying to decide: what applies to me? BC23 (Sx/−)
Each “Toss of the Coin” as Independent
Misunderstandings of genetics and of statistics often occurred together—e.g., when even well-educated individuals felt that the probabilities of susceptibility among siblings were not independent, but rather linked. Hence, some thought that of two siblings at risk for HD, if one had the gene, then the other would not have it, or vice versa.
Many at risk for HD, in particular, found this notion (i.e., that each “coin toss,” or birth, was independent) to be counter-intuitive, in part because of countervailing emotional desires, and beliefs in cosmic justice and fairness. As one man said about his brother,
He tested negative, which scared me. Irrationally, I thought for sure we couldn’t both get away unscathed. I know they’re independent events, so the fact that he tested negative does not influence my testing at all. But emotionally, it didn’t feel that way at all. HD11 (Asx/−)
Many felt that they must be mutation-positive if a sibling is negative. This belief may be said to represent emotions overriding rationality. A very self-aware individual may recognize that his or her feelings are overtaking his or her reasoning and risk comprehension. However, this participant and others held these beliefs for a period of time, despite recognition of the irrationality. Questions may thus arise of the definition of “misunderstandings.” One may hold irrational, incorrect beliefs and recognize that these are irrational, but continue to hold them nonetheless, perhaps due to anxiety. However, these are nonetheless incorrect beliefs that can potentially affect these individuals in various ways, and about which providers should be aware.
Several individuals felt that an inherent logic of cosmic fate operated here. “You can’t escape twice.” HD12 (Asx/−)
With Alpha, too, an engineer saw this misunderstanding, and often had to correct it among patients in support groups and family members, saying to them, “It’s the same odds every time you flip the coin.” A10 (Sx/+)
These beliefs appear widespread, tapping into ostensibly common sense notions of statistics and risks. Even disease communities (e.g., support groups and patient advocacy organizations) disseminated these ideas, even if not always stating them explicitly.
When my sister didn’t have it, it was like, “Oh geez, it couldn’t really be that we would both escape—to have two escapees in one family.” I gather it’s not that unusual. But when you’re sitting in a group of at-risk people, and tell them that—they all go “Mmm…” because the likelihood is not high that if you have two or three siblings in a family, they all escaped. HD12 (Asx/−)
Here, misunderstandings of statistics and of genetics reinforce each other. Individuals may be aware of Mendelian principles, but misinterpret them. One former nursing student explicitly cited Mendel’s law, but misconstrued it. She explained why her relatives who were both sickle cell carriers attempted successfully to have a child without the mutation.
They finally tried again to have a kid naturally, because nothing was going to work out. We went back to old Mendel’s law about 4. They said you have two there, you need to hit it this time or we miss it altogether. So they tried it once more. BC19 (Sx/Unt)
The Existence of Two Options Must Mean That the Odds are 50/50
Some assumed that the existence of two outcomes—in this case, having or not having a gene—meant that the odds of either outcome must be 50/50, regardless of epidemiological data to the contrary. These individuals thought that the number of options predicted the odds, again reflecting misunderstandings of both statistics and the predictiveness of a particular test. While 50% odds apply for HD, they do not for other tests such as BRCA. As one woman with breast cancer said, “I guess there’s a 50/50 chance that I have the mutation.” BC4 (Sx/+)
Yet, the risk of breast cancer in the general population is approximately 12% (National Cancer Institute 2009), and the prevalence of BRCA 1/2 mutations is approximately 0.24% among non-Ashkenazi Caucasians, and 1.2% among Ashkenazi Caucasians (Whittemore et al. 2004). Among women with diagnosed breast cancer, the prevalence of BRCA mutations ranges from 8.3% among Ashkenazi Jews, to 2.2% among non-Hispanic Caucasians, and 1.3% among African-Americans (John et al. 2007). This woman in fact has less than a 10% chance of having the mutation.
Similarly, an asymptomatic woman with a family history of breast cancer, who turned out to have a BRCA mutation, said,
If you test negative, you have the same risk as the general population, so there’s a 50% chance that I really didn’t need to be going through all this, because I might be negative. BC13 (Asx/+)
This woman appeared to confuse two phenomena. The risk of breast cancer in the general population is 12%, and the chance of her being mutation-negative is over 98%—not 50%. But her misunderstanding led her to think that she could perhaps have avoided testing.
Factors
Four main categories may be involved in shaping the types and likelihood of misunderstandings, related to: education, emotional issues, beliefs about punishment, and social contexts.
Education
As suggested earlier, education, both generally and specifically in science, may potentially reduce these misperceptions—but not necessarily in entirety. Irrational beliefs (e.g., desires that one’s family or oneself can avoid disease) can still foster misunderstandings. Individuals may realize intellectually that their beliefs are irrational, but nonetheless hold, or be swayed by them.
Emotional Issues
Emotional factors, particularly minimization, denial and hope, can also bolster these misunderstandings. Denial, in particular, can perpetuate misunderstandings and myths about genetics and genetic risks. At times, misunderstandings may also reflect socially and culturally widespread beliefs. The term “denial” suggests a psychodynamic defense mechanism, and can be seen as part of psychosis that is a direct symptom of HD, or as part of a psychological response to any of these three disorders. The term has also entered general parlance more widely, and was mentioned by several interviewees. This term may refer to a range of complex emotional states. One woman, for example, did not think that the fact that her grandmother and aunt had breast cancer might increase her own chances of developing the disease.
One of my siblings said: “It’s good you’re having aggressive treatment because of the history in our family.” I was a little startled, because I had never thought of it that way. I didn’t think it was related to their cancer. I knew my maternal grandmother died of breast cancer. But I didn’t know how it was related genetically. I was in incredible denial, and didn’t reallywantto know too much about it. BC11 (Sx/Unt)
Individuals may have little desire to counter such minimization of genetic risk. Yet such avoidance, if challenged by external events, can prove devastating. This woman continued,
When it did hit me, it hit me like a ton of bricks…I was a wreck—angry, frightened, crazed. BC11 (Sx/Unt)
Beliefs About Punishment
Several individuals believed that they had received a mutation or a disease as punishment—because they deserved it. Questions arose about the accuracy of such metaphysical notions as causes of genetic disease. One woman said,
I felt I must have really fucked up. Did I fuck up because I had done immoral things? I was living an immoral life, not eating well, not exercising, not paying attention to my body. Am I being punished? I also had an affair while I was with my partner. If I hadn’t had an affair or if I lived a more morally upstanding life, I wouldn’t have gotten cancer. The rabbi said, “I don’t think about God as punishing in that kind of way.” I’m 95% over that. BC7 (Sx/Unt)
Some may argue that these beliefs, though unscientific, are not necessarily misunderstandings per se, and may merely reflect religious beliefs. Nonetheless, these concepts may inadvertently impede health behaviors, and therefore are of note in this context, and important for providers to recognize.
The Roles of Social Contexts
Various social contexts may support, fuel, or challenge patients’ beliefs. Patient self-help groups, the media, rumor and hearsay can all actively promulgate certain concepts, bolstering notions of hope, and cosmic fairness, and relatedly, casual explanations of natural phenomenon. On the one hand, participants felt that in certain social contexts, such beliefs were embarrassing because other people viewed them as irrational. Interviewees realized that certain beliefs could be seen as inaccurate, and even verge on the mystical and magical
I’m from California, so you can take this with a grain of California salt—it’s a little embarrassing to me—I was very much a part of New Age claptrap for a long time. A friend sent me a guru healing tape—this woman believed some people came into the world to extinguish a genetic disease from the family. HD12 (Asx/−)
An individual may uphold these notions, despite realization of their limitations. Family members, friends and health care providers may also challenge such conceptualizations. Interpersonal tensions can ensue.
My boyfriend is Mr. Holistic Vitamin Guru, crazy nut. He thought my breast cancer could just be treated with vitamins. He is dead against everything I’ve done, downright mad that all this has gone on, which has been difficult. He doesn’t really understand that in every single gene in my body, this one gene is mutated. He just thought there’s this one mutation on one something, but it’s not on every chromosome. I had to have the doctor tell him: this is in every single gene in my body. That one particular gene on the chromosome is mutated. It cannot be fixed. He just thought it was just a small corruption of some sort that can be corrected in one place in my body, like my breast. So he didn’t understand why all this stuff had to happen, having my breasts and ovaries removed. BC14 (Sx/+)
This patient confused “gene” and “cell,” but her larger point was that misunderstandings may exist about the fact that the problem can’t readily be repaired.
An individual’s disease can emotionally distress a partner who struggles with his or her own anxieties about the diagnosis, or misunderstandings, or desires not to understand. The fact that disease can result from a mutation can be both frightening and counterintuitive. The woman above continued,
I don’t think he wants to understand. I had to have my breasts and ovaries removed, but those genes are still lingering there. Anything can happen. Despite the fact that most everything is gone I could still get cancer. It could still metastasize to another part of my body. BC14 (Sx/+)
Implications of Misunderstandings for Other Health Behaviors
These misunderstandings have implications in three broad areas, concerning: testing and treatment, coping, and reproductive decisions.
Testing and Treatment
As indicated previously, these misunderstandings can impede health behaviors. For example, miscomprehensions can prompt individuals at risk for a genetic disease to avoid testing and treatment (e.g., preventive screening). One woman said,
I thought: if I didn’t have a mammogram, I wouldn’t have breast cancer. [Laughs]. So I’ve never had a mammogram. I always thought breast cancer was over-treated—that the whole thing was a crock. That strategy did not work. Why not get a mammogram? Foolish risk-taking—it was exciting. I also did exercise and diet. BC11 (Sx/Unt)
She felt that her behavior, rather than biology, controlled her disease, and she suggests magical thinking. Yet her diagnosis with breast cancer forced her to realize that her prior behavior and beliefs were “foolish.”
Coping
These beliefs can also affect coping, and expectations about whether one is mutation-positive. Misunderstandings can thus influence responses to one’s own test results, and those of others.
When my brother told me that he had tested negative, I was devastated, I couldn’t talk to him. I got off the phone, and cried, thinking, “I’ve got it for sure.” I knew it was irrational. I told him a few days later, “Look, I just can’t celebrate this with you. I’m sorry. It is good news. But I’m having this irrational response, you’re just going to have to enjoy this without me.” HD11 (Asx/−)
She was distressed because she assumed inaccurately that if he did not have the mutation that she then certainly had it. She recognized the irrationality of her thoughts, but found it difficult to alter her emotional response.
Genetic counseling can help alter these beliefs, but individuals may still get genetic tests through either providers or direct-to-consumer advertising, and receive little, if any counseling. Hence, individuals may make testing and other health care decisions drawing on these misunderstandings, without counseling. These misconceptions can later be found false and prove overwhelming.
One woman in my support group had a sister, and convinced herself that this sister had the gene—because she was so much like their father in personality. Then this sister got tested, and didn’t have it—so this woman flips out. She had never worried about HD. She was 45, had this 8 year-old kid, and suddenly thought, “Holy shit, I got it all wrong!” She was a wreck, very agitated. I was worried. HD11 (Asx/−)
This interviewee also suggests how medical events concerning oneself and one’s family members can impinge on, and potentially alter, one’s beliefs and understanding about one’s own risk.
Reproductive Decisions
Beliefs about the inheritability of certain traits, including mental health related problems, could affect reproductive decisions as well. Misunderstandings of genetics can shape views about past or future reproductive choices based on misunderstandings of a disease. For instance, at risk individuals may decide not to get married and/or have children. One man, for example, concluded that he might not have married his wife, if he had known about her family history of depression.
Had I known my wife’s history when I was dating her in college, I might not have gotten in as deep. Her father had had two nervous breakdowns—obviously manic depression. She had an older sister commit suicide, and another one hospitalized. My older son got her family genes. Everyone has something genetic, but you assess how dangerous you think it may be, what percent chance your children would be afflicted. If I knew her family, I might have seen the odds as not so good. A4 (Sx/+)
Discussion
These data suggest that individuals who are at risk for genetic disease confront a range of difficulties in struggling to comprehend their predicaments, leading to a wide variety of misunderstandings about genetic tests and mechanisms, and statistics. Genetic tests were seen as being more predictive than they actually were, and genetics were viewed as able to predict even behaviors and traits for which no markers have yet been identified. The misunderstandings that arose about genetic mechanisms related, for example, to carrier states, homozygosity vs. heterogeneity (i.e., that carrier states could result in disease, even if the disorder was autosomal recessive), and individuals resembling one parent or side of the family more than the other. Misconceptions emerged about statistics as well, concerning percentages vs. proportions, absolute vs. relative risk, and independence of odds, with many individuals not recognizing that odds were independent. These misunderstandings had important implications for these interviewees’ coping, testing, treatment, and reproductive decisions.
These data suggest that a spectrum of misunderstandings exist that vary in their extent. Individuals also range in the degrees to which they are aware of these miscomprehensions. Indeed, these data reflect definitions of “understanding” and “misunderstanding”. The Oxford English Dictionary (Brown 1973) defines “understand” as “perceive the meaning; grasp the idea of…be conversant or familiar with, have mastery of”—i.e., suggesting a broad range from being “conversant with” to having “mastery of.” Similarly, “misunderstand” is described as “to fail to understand rightly…take in a wrong sense…misinterpret…”—indicating a range from complete failure of comprehension to partial misunderstanding. Indeed, the data here suggest that misunderstanding of genetics may not be “all or nothing”, but rather, varied in its degree and specific aspects.
These issues are of increasing importance as the direct marketing of genetic tests to both providers and patients heightens. Private companies, scientists, journalists, and doctors may overly encourage genetic testing, taking advantage of, and contributing to, some of these misunderstandings (i.e., beliefs in the inherent value of this knowledge) in ways that can have unintended negative consequences.
Earlier studies have shown that the general public often miscomprehends genetics (Lanie et al. 2004; Shaw and Hurst 2008; Kessler et al. 2007), and that individuals at risk of common chronic familial diseases for which no definitive genetic markers have yet been identified (e.g., hypercholesterolemia and diabetes) undergo a highly subjective personalizing process (Walter and Emery 2005). The present data suggest that individuals at risk for other disorders, for which definitive tests do exist, and who had often already interacted with genetic counselors and other providers regarding these issues and undergone testing, nonetheless display a broad array of misconceptions as well. Even in the presence of objective markers, and after genetic counseling, patients frequently misunderstand genetic mechanisms, risks, and tests.
Moreover, while this earlier literature has suggested that individuals personalize their views of genetics (Walter and Emery 2005), the present data highlight the importance of examining not just the ways in which views of risk may be subjective, based on particular personal experiences and context, but the specific content involved—of what specific elements these beliefs actually consist, and how they may in fact be misunderstandings that can impede health behaviors. Moreover, these data suggest how misconceptions are not always wholly idiosyncratic, but may reveal several patterns, related to miscomprehensions of several specific areas, and can reflect underlying psychological desires. Clearly, not all subjective impressions of genetics are inaccurate, but some are, and patients may benefit from providers recognizing and trying to remedy these misunderstandings.
In addition, while prior literature has proposed possible frameworks for genetic counseling that include perceptions of risk (Etchegary and Perrier 2007; Shiloh 2006), the present data suggest how such perceptions of risk may be based in part on misunderstandings. While this prior literature suggests that multiple factors, such as views of cause, control, and family influence, may also be involved and affect perceived risk, the interviewees here suggest how some of these factors actually interact, and how these issues can vary, based, for example, on emotional needs. These needs can in turn collide with and override intellectual understandings of genetics. Of note, most of these interviewees had attended at least some college, but nonetheless indicated misunderstandings. Indeed, it appeared that the specific amount of science education, more than education overall, may prove key here. Prior research has tended to assess total overall amount of education, but not science education per se (Molster et al. 2009). Moreover, the present data underscore how broader cultural and social myths and misunderstandings can affect these perceptions as well, in ways that require more attention.
Several of the themes here have received little, if any, attention in extant literature. For instance, while prior articles have tended to separately view issues concerning perceptions of statistics, genetic tests, and genetic mechanisms, the present data illustrate how these three respective sets of misperceptions can in fact inter-relate, reinforcing each other in ways that can impede patients’ subsequent health decisions and behaviors. Specifically, for example, patients’ difficulties comprehending risk emerge in part because of misunderstandings of not just statistics, but of genetic tests and mechanisms as well. Similarly, the notion that genetic tests are more predictive than they actually are can also result from, and contribute to, misconceptions about statistics. The present sample of patients overestimated not only their risk, but also the predictiveness of genetic tests. These overcalculations can bolster, and be bolstered by, beliefs about genetic mechanisms (e.g., that if one resembles one parent more than the other, one will be more like that parent in most ways). Difficulties grasping complicated statistics can further fuel misunderstandings about genetics.
While the notion that disease mutations were linked with physical resemblances to an affected parent have been suggested among individuals at risk for HD (Emslie et al. 2003), the present participants elucidated ways in which this misconception arises with other diseases. Past studies have tended to examine this belief in isolation, without considering other sets of misperceptions and their implications for health behaviors. The present data illustrate how this misperception can support, and be supported by, misunderstandings about genetic mechanisms, and reflect desires for a sense of order and an organizing principle in the face of anxiety and health threats. Moreover, this belief can persist despite awareness that it is, or may well be, illogical.
Uncertainty itself can foster anxiety, as demonstrated with HIV (Sieff et al. 1999), and it can clearly do so with genetics, furthering denial, minimization, guilt, or other emotional responses to risk that can then abet these misconceptions. Indeed, asymptomatic individuals at risk for HIV have been found to be more anxious before learning their test result than 10 weeks after finding out that they were actually infected with the virus (Sieff et al. 1999). Similarly, individuals who are at risk of a genetic disorder may feel more anxious before testing than after learning that they do in fact have a mutation. Hence, before testing, to lower this anxiety, they may assume that they have the mutation, and look for explanations to justify or support that belief.
Thus, while much prior literature has focused on cognitive models and processes involved in risk assessments and genetic counseling, the present data highlight the critical roles that complex emotional factors may play. Specifically, misperceptions of both statistics and genetics may reflect a variety of emotional states and psychological desires related not only to fear, but to denial, hope, guilt, and wishes to avoid despair and control the disease. While at times, individuals recognize their perceptions and/or emotional responses are inconsistent with the facts, their reasoning does not always prevail over their conflicting emotional and psychological needs. As Freud and others have argued, self-awareness is not always sufficient to override emotional drives, since unconscious conflicts may be involved, and may first need to be addressed and made conscious (Freud 1905). Several interviewees spoke of “denial,” yet this term can get used to refer to a spectrum of responses such as disbelief and dismissal of unwanted news (Lubinsky 1994). Still, each of these specific types of responses can potentially affect patients’ understandings of genetics and health decisions.
Of note, these emotions can potentially outweigh both educated understandings of how genetics and statistics actually work, and input from health care providers. Yet irrational beliefs can potentially be reduced by probing the underlying psychological conflicts involved (i.e., making patients more aware of them). Thus, genetic counselors should be as aware as possible of these phenomena and attempt to address them with patients.
Additional factors that contribute to misunderstandings about genetic causes include inherent scientific uncertainties, personal experiences, social contexts, and various medical events over time. While much research has viewed an individual’s understandings of his or her genetic risk as static, the present data underscore how understanding is a highly dynamic process. Patients confront and respond to medical events (e.g., new diagnoses, symptoms, and treatments) in both themselves and family members. When test results challenge prior assumptions (e.g., that physical resemblance among family members determines the presence or absence of a disease mutation), some individuals conclude that their prior assumptions were incorrect, while others try to maintain these prior assumptions, and imagine mechanisms for reconciling these divergent conclusions. Variability in responses may arise in part due to the strength of prior vs. later evidence (e.g., a sibling’s definitive test result can “devastate” prior beliefs that were based merely on an assumption about his or her mutation status). Misunderstandings, when they are corrected, can also be emotionally “devastating,” illustrating how misconceptions can affect psychological coping.
Self-regulatory theory (Shiloh 2006) offers one model for conceptualizing genetic counseling. This theory includes as factors perceived risk, identity, beliefs about consequences of testing, causes of disease, control, and efficacy of testing. The present data demonstrate that misunderstanding can affect each of these components in crucial ways, potentially hampering a patient’s overall information processing. These misunderstandings can result from both knowledge deficits and defensive reactions, and can persist even after genetic counseling.
These data underscore, too, how social influences, such as misperceptions of family members, fellow patients, and others, can shape these processes. Media reports of genetic discoveries (Rothman 1998), popular films such as Gattaca and The Twilight of the Golds, and physicians’ implicit or explicit attitudes can potentially bolster beliefs concerning, for instance, the predictiveness of genes. These beliefs can potentially encourage or discourage patients about pursuing testing. For instance, at times, views of testing seemed somewhat akin to “therapeutic misconception” (in which patients assume that they will benefit from treatment provided in a research protocol even if they are participating in a randomly controlled clinical trial in which they may in fact be receiving a placebo) (Appelbaum et al. 1982). Here, some patients felt that that to undergo genetic testing would be helpful in and of itself. Individuals frequently overestimated the power of genetics (e.g., believing in genetic bases for behavioral traits for which no genetic markers have been found), thinking that testing was inherently beneficial—that knowledge was invariably power. Patients often felt that physicians would only offer medical tests if these were generally beneficial. The value of genetic tests for a particular patient, however, may be far more equivocal, especially if no treatment is available for the condition.
Individuals often sought to believe they had control over their destiny and resisted the notion that they lacked this control. These data suggest that one of the most difficult aspects of genetic disorders is perceived uncontrollability, due to the fact that genetics are by definition inherited, and thus seen as “givens.” Patients then face dilemmas regarding how to cope with such seemingly irrevocable fate. Not surprisingly, many came to believe that they could in some way control genetic disorders (even HD), and that the disease would not necessarily manifest itself. These findings are consistent with Berkenstadt et al.’s (1999) assertion that patients seek personal control. These data further indicate that patients’ perceptions of control may at times be incorrect, impeding coping and health behaviors (e.g., testing, disclosure, treatment, and reproductive decisions).
Psychological and sociological research has explored, in domains outside of genetics, how individuals frequently need to establish a sense of social order and justice by attributing responsibility for events, and how these efforts can be shaped by factors such as expectations of social roles (Hamilton 1978). Within genetics, individuals may seek order that is less related to social justice than to cosmological or metaphysical concerns—since mutations do not result from social interactions, but may be seen by patients as “divinely” given. Individuals also vary in their psychological toleration of ambiguity and need for closure (with need for closure being associated with religiosity) (Saroglou 2002). A need for closure can foster misunderstandings that reduce uncertainty, despite being incorrect. These factors have received limited attention with regard to genetic testing decisions, but they may play important roles.
Tversky and Kahneman (1974, 1981) describe difficulties people experience grappling with statistics, including the use of unreliable heuristics. These authors suggest that humans are generally risk averse. Relatedly, the present sample tried to frame genetic information positively, seeking hope. But these data also illustrate other ways in which individuals eschew potential risks. For example, the inherent uncertainty can be reduced by viewing genetic tests as more predictive than they actually are, and by making assumptions about eventual test results, even if these assumptions are incorrect. While Tversky and Kahneman explore decisions regarding more emotionally neutral situations (e.g., hypothetical amounts of money won or lost in a game), the anxiety of uncertainty can lead people to make assumptions that involve greater future risks to themselves and others, but decrease anxiety at the moment. Specifically, patients at times seek to avoid the anxiety of uncertainty at present by assuming that they have a mutation.
Interviewees’ beliefs varied in the extent to which they were widespread and culturally or scientifically supported vs. personal. Both cultural views and scientific uncertainties (i.e., about genetic and other biological factors involved in disease) can potentially promote misunderstandings. The anthropologist Arthur Kleinman (1980) and others (Kagawa-Singer and Blackhall 2001; Sue 1998) have highlighted how, in general, culturally-sanctioned beliefs that may not be scientifically-based can affect patients’ attitudes and approaches toward medical treatment. These cultural beliefs have been explored with regard to end of life decisions (Kagawa-Singer and Blackhall 2001) and mental illness (Kleinman 1980), but have received less attention with regard to genetics. However, the present data suggest that such beliefs may play roles here as well, and may be particularly important for providers to be aware of as more patients in more communities and countries, which have diverse cultural traditions, undergo genetic testing. As mentioned above, notions that genes are highly predictive, and that metaphysics can alter health, can reflect wide-spread cultural beliefs (disseminated in part by the media), that further enhance personal views. Culturally, themes of helplessness and searches for order in the face of fate and chaos are long-standing and deeply-embedded, filling literature from the ancient Greeks to Shakespeare and Camus. Similarly, folk beliefs about free will vs. determinism are deeply imbued in our culture, with Greek, Hebraic, and Germanic mythologies all speaking of external forces molding us beyond our will. Interviewees often railed against the notion that a force beyond their volition (i.e., a mutation) had power over them. Instead, they sought to believe that they maintained some influence over their fate.
This social reinforcement underscores the need for targeted public education about genetics. Genetic counselors and other providers need to recognize that patients’ misperceptions may stem in part from larger social views, and that these broader societal roots may need to be addressed. A patient may recognize the inaccuracy of socially-disseminated ideas about genetics, yet still maintain them. Alternatively, patients may hold incorrect personal beliefs despite efforts by providers (or public education campaigns) to reverse these. The present results suggest that inaccurate perceptions may persist, in part due to deficits in scientific knowledge, and/or emotional needs.
Prior research suggested that individuals who were at risk for Huntington’s disease, whether symptomatic or asymptomatic, generally had lower levels of distress than expected (Almqvist et al. 2003). The present data elucidate how some individuals in fact may manage to incorporate positive test results and symptomatology into their lives: through miscomprehensions that can impede health behaviors in other ways.
Among the three diseases represented in the current sample, some possible differences emerged. Specifically, as an autosomal dominant condition, the genetics of HD involve, in some regards, less ambiguity than the other two disorders. BRCA mutations involve more uncertainties, given the reduced penetrance of these mutations, and the potential effects of other, non-genetic factors in disease onset and severity. Similarly, for Alpha, confusion can result from the fact that environmental toxins may contribute to symptoms, and heterozygotes for the mutation can themselves potentially display symptoms, though less severely than do homozygotes. As a result, misunderstandings about absolute vs. relative risks arose for breast cancer and Alpha, but not for HD. Nevertheless, as indicated above, similar key patterns emerged across these disorders.
Study Limitations
This study has several limitations. The sample includes more Caucasians than African-Americans or Latinos, and participants self-identified as being at-risk. Nevertheless, these data shed light on a wide variety of misunderstandings that future studies can further examine among larger, more heterogeneous samples. Several interviewees described the misunderstandings of their family members and other patients, rather than their own misunderstanding (or lack thereof). However, in this kind of qualitative, exploratory research, their observations about other at-risk individuals are valuable, given the relatively small number of studies that have been published on these issues. At times, participants may have hesitated to reveal their own miscomprehension of genetics. Hence, the extent of their misunderstanding may under-represent the actual amount. Finally, qualitative data are not necessarily generalizable to other populations of interest. Research is needed to further explore the patterns found in this study.
Practice Implications
As suggested above, these data have valuable implications for clinical care, and for public and professional education. Health care providers should address patients’ misbeliefs concerning three domains—genetic tests, genetic mechanisms, and statistics. Potentially, correct perceptions in one domain may help counterbalance misperceptions in the others. Health care providers should also be aware of and address potential broader social and cultural beliefs that can reinforce an individual’s misunderstandings. Yet while genetic counselors may have some training in probing and addressing such misunderstandings, physicians and other providers may be less aware of, or sensitive to, the breadth and prevalence of these misconceptions, and the ways that these misperceptions can shape patients’ decisions. Addressing patient needs for order and organization might also reduce misunderstandings. However, to the extent that certain of these factors (e.g., needs for closure vs. toleration of ambiguity) represent relatively enduring personality traits, the possibility of change may prove limited. Nonetheless, future research can examine whether, when, and to what degree these factors can be altered through interventions.
Misunderstandings might best be reduced by addressing the emotions that may underlie them (e.g., difficulties confronting perceived lack of control and seemingly irrevocable fate, desires to frame genetic information positively in order to avoid despair and helplessness and seek hope, and efforts to reduce anxiety by finding order in the face of fate and seeming randomness). Given that emotional conflicts may not be fully conscious, providers should proceed very carefully in addressing them. Certain aspects of psychodynamic or other psychotherapeutic approaches may be beneficial, but genetic counselors and other health providers likely would need specific training in order to effectively implement such approaches.
The present data suggest, too, that even some patient communities (e.g., support groups) may not check or challenge incorrect information. Consequently, genetic counselors and other health care providers, both as individuals and through professional organizations, can potentially play important roles in working with patient groups to address these misconceptions. These data also highlight needs for public education to improve patient and broader public understandings of genetics.
Research Recommendations
These data have critical implications for future research. Researchers should investigate how often and when these different types of misunderstanding arise for other diseases with different genetic bases, and whether there are variations among different disorders. Researchers should also examine how providers can most effectively intervene to reduce these misunderstandings and assess which miscomprehensions are more or less amenable to correction. Additional investigations are warranted to determine how best to address emotional issues such as denial or avoidance that may fuel misunderstandings of genetics. Future studies should also examine as factors amounts of education both in general, and specifically in science.
Various outcome measures of clinical genetic services have been employed, mostly quantifying anxiety and distress, though some of these instruments have probed several aspects of genetic knowledge. But many methodological questions about these measures remain (Payne et al. 2008). The present data suggest the range of types of misunderstandings (e.g., concerning metaphysical or other non-scientific attitudes and beliefs) that questionnaires used heretofore may not fully or adequately take into account. Indeed, such types of misunderstandings may be intrinsically subjective and hence difficult to measure (Klitzman and Daya 2005), but can nonetheless influence patients’ decisions. Quantitative assessments of misunderstandings thus pose challenges that future researchers should consider, and address as well. Finally, since misperceptions may arise and persist over time, subsequently affecting decisions by patients and their families, the effects of genetic counseling should be studied longitudinally.
Conclusion
The findings of this study illustrate several types of misunderstandings patients may have about genetics. Such misperceptions may shape their health behaviors in significant ways. Thus, genetic counselors and other health providers should address these misunderstandings.
Acknowledgements
This work was funded through a grant from the National Human Genome Research Institute (R01-HG002431-01). I would also like to thank Meghan Sweeney, Melissa Conley, Lisa Chin, and Sarah Dion for their assistance with the manuscript.
Appendix: Sample Questions from Semi-Structured Interview
When did you first learn that you were at risk of a genetic disease?
What was your reaction to it at that time?
What is your understanding of your genetic risk?
Have you undergone genetic testing?
How did you decide whether to undergo genetic testing or not?
Why did you decide to [undergo/not undergo] testing?
What is your understanding of what the genetic test [might tell/told] you?
References
- Almqvist EW, Brinkman RR, Wiggins S, Hayden MR. Psychological consequences and predictors of adverse events in the first 5 years after predictive testing for Huntington’s disease. Clinical Genetics. 2003;64(4):300–309. doi: 10.1034/j.1399-0004.2003.00157.x. [DOI] [PubMed] [Google Scholar]
- Appelbaum PS, Roth LH, Lidz C. The therapeutic misconception: informed consent in psychiatric research. International Journal of Law & Psychiatry. 1982;5(3-4):319–329. doi: 10.1016/0160-2527(82)90026-7. [DOI] [PubMed] [Google Scholar]
- Berkenstadt M, Shiloh S, Barkai G, Katznelson M, Goldman B. Perceived personal control (PPC): a new concept in measuring outcome of genetic counseling. American Journal of Medical Genetics. 1999;82:53–59. doi: 10.1002/(sici)1096-8628(19990101)82:1<53::aid-ajmg11>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Brown L, editor. The new shorter Oxford English dictionary on historical principles. Vol. 1, A-M. Oxford University Press Inc.; New York: 1973. [Google Scholar]
- Condit CM, Dubriwny T, Lynch J, Parrott R. Lay people’s understanding of and preference against the word “mutation”. American Journal of Medical Genetics. 2004;130A:245–250. doi: 10.1002/ajmg.a.30264. [DOI] [PubMed] [Google Scholar]
- d’Agincourt-Canning L. The effect of experiential knowledge on construction of risk perception in hereditary breast/ovarian cancer. Journal of Genetic Counseling. 2005;14(1):55–69. doi: 10.1007/s10897-005-1500-0. [DOI] [PubMed] [Google Scholar]
- deVries H, Mesters I, van de Steeg H, Honing C. The general public’s information needs and perceptions regarding hereditary cancer: an application of the Integrated Change Model. Patient Education & Counseling. 2005;56:154–165. doi: 10.1016/j.pec.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Emery J, Watson E, Rose P, Andermann A. A systematic review of the literature exploring the role of primary care in genetic services. Family Practice. 1999;16(4):426–445. doi: 10.1093/fampra/16.4.426. [DOI] [PubMed] [Google Scholar]
- Emslie C, Hunt K, Watt G. A chip off the old block? Lay understandings of inheritance among men and women in mid-life. Public Understanding of Science. 2003;12:47–65. [Google Scholar]
- Etchegary H, Perrier C. Information processing in the context of genetic risk: implications for genetic-risk communication. Journal of Genetic Counseling. 2007;16(4):419–432. doi: 10.1007/s10897-006-9082-z. doi:10.1007/s10897-006-9082-z. [DOI] [PubMed] [Google Scholar]
- Freud S. In: Three essays on the theory of sexuality. Strachey James., translator. Basic Books; New York: 1905. 1962. [Google Scholar]
- Geertz C. Interpretation of cultures: Selected essays. Basic Books; New York: 1973. [Google Scholar]
- Hamilton VL. Who is responsible? Toward a social psychology of responsibility attribution. Social Psychology. 1978;41(4):316–328. [Google Scholar]
- John EM, Miron A, Gong G, Phipps AI, Felberg A, Li FP, et al. Prevalence of pathogenic BrCa1 mutation carriers in 5 racial/ethnic groups. Journal of the American Medical Association. 2007;298(24):2869–2876. doi: 10.1001/jama.298.24.2869. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Blackhall LJ. Negotiating cross-cultural issues at the end of life: “you got to go where he lives. Journal of the American Medical Association. 2001;286(23):2993–3001. doi: 10.1001/jama.286.23.2993. [DOI] [PubMed] [Google Scholar]
- Kessler L, Collier A, Halbert C. Hughes. Knowledge about genetics among African-Americans. Journal of Genetic Counseling. 2007;16(2):191–200. doi: 10.1007/s10897-006-9054-3. doi:10.1007/s10897-006-9054-3. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Patients and healers in the context of culture: An exploration of the borderland between anthropology, medicine, and psychiatry. University of California Press; Berkeley: 1980. [Google Scholar]
- Klitzman R. When doctors become patients. Oxford University Press; New York: 2008. [Google Scholar]
- Klitzman R. Views of discrimination among individuals confronting genetic disease. Journal of Genetic Counseling. 2010;19(1):68–83. doi: 10.1007/s10897-009-9262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R, Bayer R. Mortal secrets: truth and lies in the age of AIDS. Johns Hopkins University Press; Baltimore: 2003. [Google Scholar]
- Klitzman R, Daya S. Challenges and changes in spirituality among doctors who become patients. Social Science & Medicine. 2005;61(11):2396–2406. doi: 10.1016/j.socscimed.2005.04.031. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Chung W, Marder K. Decision-making about reproductive choices among individuals at-risk for huntington’s disease. Journal of Genetic Counseling. 2007a;16(3):347–362. doi: 10.1007/s10897-006-9080-1. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Marder K. The roles of family members, health care workers and others in decision-making processes about genetic testing among individuals at risk for Huntington’s disease. Genetics in Medicine. 2007b;9(6):358–371. doi: 10.1097/GIM.0b013e3180653c5a. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Chung W, Marder K. Disclosures of Huntington’s disease risk within families: patterns of decision-making and implications. American Journal of Medical Genetics. 2007c;143:1835–1849. doi: 10.1002/ajmg.a.31864. [DOI] [PubMed] [Google Scholar]
- Lanie AD, Jayaratne TE, Sheldon JP, Kardia SLR, Anderson ES, Feldbaum M, et al. Exploring the public understanding of basic genetic concepts. Journal of Genetic Counseling. 2004;13(4):305–320. doi: 10.1023/b:jogc.0000035524.66944.6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubinsky MS. Bearing bad news: dealing with the mimics of denial. Journal of Genetic Counseling. 1994;3(1):5–12. doi: 10.1007/BF01414602. [DOI] [PubMed] [Google Scholar]
- Molster C, Charles T, Samanek A, O’Leary P. Australian study on public knowledge of human genetics and health. Public Health Genomics. 2009;12:84–91. doi: 10.1159/000164684. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute BRCA1 and BRCA2: Cancer risk and genetic testing. National Cancer Institute FactSheet. 2009 Retrieved from http://www.cancer.gov/cancertopics/factsheet/Risk/BRCA.
- Payne K, Nicholls S, McAllister M, MacLeod R, Donnai D, Davies LM. Outcome measurement in clinical genetics services: a systematic review of validated measures. Value in Health. 2008;11(3):497–508. doi: 10.1111/j.1524-4733.2007.00259.x. [DOI] [PubMed] [Google Scholar]
- Rothman BK. Genetic maps and human imaginations: The limits of science in understanding who we are. Norton; New York: 1998. [Google Scholar]
- Saroglou V. Beyond dogmatism: the need for closure as related to religion. Mental Health, Religion & Culture. 2002;5(2):183–194. [Google Scholar]
- Shaw A, Hurst JA. “What is this genetics, anyway?” Understandings of genetics, illness causality and inheritance among British Pakistani users of genetic services. Journal of Genetic Counseling. 2008;17:373–383. doi: 10.1007/s10897-008-9156-1. [DOI] [PubMed] [Google Scholar]
- Shiloh S. Illness representations, self-regulation, and genetic counseling: a theoretical review. Journal of Genetic Counseling. 2006;15(5):325–337. doi: 10.1007/s10897-006-9044-5. [DOI] [PubMed] [Google Scholar]
- Sieff EM, Dawes RM, Loewenstein G. Anticipated versus actual reaction to HIV test results. The American Journal of Psychology. 1999;112:297–311. [PubMed] [Google Scholar]
- Sivell S, Elwyn G, Gaff CL, Clarke AJ, Iredale R, Shaw C, et al. How risk is perceived, constructed and interpreted by clients in clinical genetics, and the effects on decision-making: systematic review. Journal of Genetic Counseling. 2008;17:30–63. doi: 10.1007/s10897-007-9132-1. doi:10.1007/s10897-007-9132-1. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research—techniques and procedures for developing grounded theory. Sage; Newbury Park: 1990. [Google Scholar]
- Sue S. In search of cultural competence in psychotherapy and counseling. The American Psychologist. 1998;53(4):440–448. doi: 10.1037//0003-066x.53.4.440. [DOI] [PubMed] [Google Scholar]
- Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. Science. 1974;184:1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- Walter FM, Emery J. “Coming down the line”—patients’ understanding of their family history of common chronic disease. Annals of Family Medicine. 2005;3(5):405–414. doi: 10.1370/afm.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter FM, Emery J, Braithwaite D, Marteau TM. Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research. Annals of Family Medicine. 2004;2(6):583–593. doi: 10.1370/afm.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore AS, Gong G, John EM, McGuire V, Li FP, Ostrow KL, et al. Prevalence of BrCa1 mutation carrers among U.S. non-Hispanic whites. Cancer Epidemiology, Biomarkers & Prevention. 2004;13(12):2078–2083. [PubMed] [Google Scholar]