Abstract
Objective
To investigate whether the relationship between dental anxiety and referral for treatment under sedation is explained by attendance patterns and oral health.
Methods
Structural Equation Modeling was used on the covariance matrix of the covariates to test hypothesized inter-relationships. Subsequently, we modeled the probability of referral for treatment under sedation with a multiple logistic regression taking into account inter-relationships between the independent variables.
Results
A direct significant association of referral with dental anxiety and attendance patterns was detected but not with oral health status. However, oral health and anxiety were highly correlated. Also signaled were correlations between age and education and between gender and bad past experience.
Conclusion
Referral for treatment under sedation appears to be motivated by both fear and irregular patterns of attendance. Coupled with behavioral treatments to address dental fear and attendance, sedation can part of comprehensive care where curative treatments are long or unpleasant for patients.
Keywords: dental anxiety, structural equation modeling, logistic regression, utilization, sedation
Introduction
Severe dental anxiety, which affects 10 to 20 percent of the adult population (1–3), has a significant impact on dental attendance, dental treatment, and ultimately oral health. Individuals with high levels of dental anxiety often find themselves in a self-perpetuating cycle of fear whereby they avoid regular dental treatment, seek care only when they are in pain, and develop dental needs that are extensive for which necessary treatments are invasive. People caught in this cycle typically report poor oral health in addition to their anxiety (4).
Several factors consistently emerge as contributing factors to high dental anxiety. Gender plays an important role, as women typically report higher overall levels of dental fear (5–6) and more fear of specific dental procedures (7) than men, even though studies suggest that women seek more regular dental care than men (8–9). Individuals reporting high dental anxiety often attribute their anxiety to earlier dental experiences that they perceived as negative or traumatic (10–12), although the link between traumatic dental experiences and the development of dental anxiety may depend in part upon age (13) and temperament (14). Socioeconomic factors, such as low income (15–16) and living in rural areas (17) have been linked with higher dental anxiety. Individuals with lower education levels are more likely to experience high dental anxiety than those with more education (18–19).
Dental anxiety causes approximately 15 percent of adults to avoid regular dental care (20). It is a robust predictor of dental non-attendance (21), and surveys of irregular dental attenders find higher levels of anxiety than for regular attenders (22–23). Individuals high in dental anxiety not only avoid regular dental care, but may also avoid care in the case of a dental emergency, such as a toothache (24). Donaldson and colleagues (25) found that the relationship between socioeconomic status and the number of sound teeth a person has was partially explained by dental attendance, with dental anxiety acting as one barrier to regular attendance.
Due to avoidance of dental care, it is not surprising that those with high dental anxiety often experience significant oral health problems. Dental avoidance and anticipatory anxiety has been linked with a higher number of missing teeth (26–27). Mehrstedt and colleagues (28) found that individuals with high dental anxiety had significantly higher scores on the Oral Health Impact Profile (OHIP; 29), with feelings of self-consciousness and lack of life satisfaction occurring most often in anxious individuals. After controlling for socio-demographic variables, McGrath and Bedi (30) found that individuals with high dental anxiety were twice as likely to score poorly on the United Kingdom Oral Health Quality of Life measure. At the same time, regular dental attenders are more likely to report that their oral health improves their overall quality of life (31). Finally, individuals with high dental anxiety describe significant effects on their social, behavioral, and health functioning, including changes in oral health and poor sleep (32).
Dental treatment performed under sedation has allowed increasing numbers of anxious individuals to receive necessary dental care and improve their immediate oral health. In studies of both emergency dental patients (33–34) and in the general population (35), over half of respondents indicated a strong interest in receiving dental treatment with the aid of some type of sedative medication, particularly when anxiety was high. Desire for treatment under sedation varies by treatment type, with individuals requesting sedation more often for invasive treatments (e.g., periodontal surgery, endodontics) than for more routine procedures (e.g., cleanings, fillings) (36). While treatment performed under sedation addresses individuals’ current dental needs, however, there is little evidence for a long-term impact on dental attendance. When compared with dental anxiety treatment with behavior therapy, individuals completing dental treatment under general anesthesia reported significantly less regular dental attendance at two- and ten-year follow-up (37–38).
Dental anxiety, therefore, is typically related to demographic and historical variables, such as gender, education, and prior dental treatment experiences. High levels of anxiety can lead to avoidance of necessary dental care, which in turn negatively impacts oral health and quality of life. The purpose of the current paper is to investigate whether the relationship between dental anxiety and referral for treatment under sedation is explained by attendance patterns and oral health. In this study we test a formal model that incorporates factors previously demonstrated to be related to one another and dental anxiety but have not been used to examine the process of referral for treatment under sedation in the UK.
Materials and Methods
The Theoretical Model
The hypotheses tested were that dental anxiety, irregular attendance and poor oral health would exert direct and positive effects on referral for sedation, mediating the effects of gender, education and having had a bad experience. These last three covariates were expected to affect the risk of referral to sedation only indirectly. Poor oral health was considered to be directly related to referral for sedation because symptomatic users are likely to need emergency care that is available under sedation in the National Health Service.
Participants
Consecutive new patients referred for dental treatment under intravenous sedation in the Department of Sedation and Special Care Dentistry and patients attending new patient clinics in restorative dentistry at Guy’s and St Thomas NHS Foundation Trust were asked to participate until 100 sedation patients (3 refusers) and 50 restorative patients (no refusers) agreed to surveyed.. Patients being evaluated for the sedation clinic (SC) have been referred because their general dental practitioner has been unable to provide dental care due to their anxiety. Patients attending the restorative clinic (RC) have been referred for treatment of complex dental problems without sedation.
Patients were approached by a member of the staff while waiting to be seen by the dentist. At the sedation clinic they were told, “We hope that by finding out why people are anxious about coming to the dentist we will be able to improve our service.” At the restorative non-sedation clinic patients were given the same information but additionally told “You might not be very anxious yourself but we plan to compare results with people attending our anxiety clinics.” The number of people refusing to take part in each setting was documented. The study was reviewed and approved by the Research Ethics Committee of St Thomas’ Hospital. The survey was confidential and the informed consent of each participant was obtained.
Survey
A 34-item written questionnaire (39) was administered in English. The questionnaire included demographic information, self reported oral health (4-point Likert-like scale ranging from poor to excellent), self reported dental attendance (5-point Likert-like scale ranging from “only when I need to” to “more often than every 6 months”), history of a bad experience with a previous dentist (yes, no) and a general measure of dental fear (Dental Fear Survey (DFS, 20 items, 5-point scales) (40). Educational level was recorded as five levels ranging from O levels (score 1) to postgraduate degree (score 5).
Statistical Methods
We estimated the effect of the explanatory variables on the binary indicator for referral to sedation clinic, giving special attention to any mediating relationships and interactions. Structural Equation Modelling (SEM, 41) was used to confirm the hypothesized relationships among the covariates for the sub-model related to anxiety (DFS score), regularity of visits to the dentist (attendance) and self-reported oral health status (oral health), based on empirical evidence of the relationships between these covariates and the demographic and socio-economic variables (gender, education and having had a bad experience). The goodness of fit of the theoretical sub-model was explored, correcting for specification errors until a model that fits the data well was achieved. This involved eliminating parameters with small t-values (unless they had practical importance) and adding parameters with large modification indices if they were theoretically sound. Generalized least squares (GLS) and robust standard errors were used to validate the results. The principal model was a logistic regression modeling the probability of referral to sedation on the same variables intervening in the sub-model, to allow for direct and indirect effects of these covariates on referral to sedation. All the multivariate models were fitted in a stepwise manner with tests of mediation (42) and tests of interaction and non-linearity (43). The statistical packages used were STATA (version 9) and EQS (Multivariate Software, Inc., Encino, CA (40)).
Results
We present the descriptive statistics in Table 1. SEM was applied to the theoretical sub-model, with the postulated inter-relationships among the covariates. The Lagrange-Multiplier Test (LMtest) of EQS was used to attain a model that optimizes the goodness of fit. The distribution of the standardised residuals from this model was symmetrical around 0 (average standardized residual was 0.06). The independence model chi-square was 121 (df=21). A good fit was indicated by the (goodness of fit) chi-square statistic (chisquare (df=11)=11.7; p= 0.39) and the goodness of fit indices: comparative fit index CFI=0.99; normed fit index NFI=0.91 and the non-normed fit index NNFI=0.99.
Table 1.
Descriptive Statistics of Survey Participants by Referral for Sedation (N=150)
| Variable | Patients not referred for sedation | Patients referred for sedation |
|---|---|---|
| Self-Reported Oral Health (N, %) | ||
| Poor | 6 (12.0%) | 52 (52.0%) |
| Fair | 20 (40.0%) | 26 (25.0%) |
| Good | 18 (36.0%) | 20 (20.0%) |
| Excellent | 6 (12.0%) | 1 (1.0%) |
| Gender (% Male) | 23% | 48% |
| DFS score (mean, SD) | 35.1 (13.6) | 69.8 (18.9) |
| Bad Experience (s) with a dentist in the past (N, % Yes) | 11 (22.9%) | 61 (61.0%) |
| How often do you usually go to the dentist? (N,%) | ||
| More often than 6 months | 9 (18.0%) | 6 (6.0%) |
| About every 6 months | 33 (66.0%) | 20 (20.0%) |
| About once per year | 3 (6.0%) | 14 (14.0%) |
| Every 2–3 years | 3 (6.0%) | 8 (8.0%) |
| Only when I need to (when I am in pain or have been hurt) | 2 (4.0%) | 51 (51.0%) |
| Highest Education Level | ||
| Ordinary levels (O levels) | 8 (22.8%) | 57 (63.3%) |
| Advanced levels (A levels) | 7 (20.0%) | 10 (11.1%) |
| BTEC (technical training) | 3 (8.6%) | 12 (13.3%) |
| Degree | 8 (22.8%) | 8 (8.8%) |
| Postgraduate Qualifications | 9 (25.7%) | 3 (3.3%) |
| Missing | 15 | 10 |
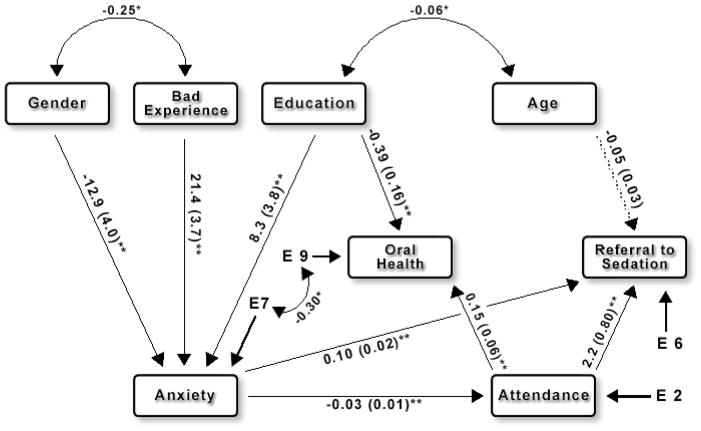
As observed from the maximum likelihood estimators of the regression coefficients and their standard errors (Figure 1), having an irregular attendance pattern was highly associated with the level of dental anxiety reported and dental anxiety in turn was highly associated with having a previous perceived bad experience, female gender, and level of education (dichotomized into above or below O-levels). In addition, poor or fair self-reported oral health status was significantly associated with having a irregular attendance pattern and with the level of education.
Figure 1.
Path diagram for the final model showing anxiety as the primary predictor of referral for sedation. The paths onto Referral to Sedation correspond to estimators of the log-odds-ratio and their standard errors of the model presented in Table 2.
The average decrease in the attendance scale produced by each unit increase in DFS score is 0.031 (SE=0.006). An increase of 10 units in the DFS score yields a decrease of almost a third of a unit scale in the attendance scale. The DFS score increases (indicating greater fear) on average by 21.4 (SE=3.7) scale units for patients that report having a bad experience in the past (in relation to those without such an experience) and by 8.3 (SE=3.8) scale units for those with educational attainment below O-levels. The DFS score is lower, on average, by approximately 13 (SE=3.9) scale units for men (in relation to women). Self-reported oral health status increases on average by 0.15 (SE=0.06) for each unit increase in the attendance scale (1 to 5 with 5 indicating more than one visit per 6 month period) and decreases by 0.39 (SE=0.16) for those with education attainment below O-levels. The effect of age on oral health was explored and found to be non significant. The LMtest signaled strong correlations between age and education, between gender and bad past experience and between oral health and anxiety; these correlations were judged to be theoretically reasonable and were fitted in the model. The maximum likelihood estimators and their standard errors were similar and the goodness of fit indices essentially unchanged when using GLS and robust standard errors.
A multivariate logistic regression (Table 2) was used to model the probability of referral to sedation in terms of the covariates and their interrelationships apparent in the SEM. Anxiety showed to be the most important determinant for referral to sedation. For each unit increase in the continuous anxiety scale (DFS), the odds of sedation referral increased by 11% (OR=1.11; 95% Confidence Interval (C.I.) 1.06 – 1.16; P<0.0001). The best threshold value for this factor turned out to be 37. The odds of sedation referral were more than 8 times as large for those with anxiety above 37 (OR=8.3; 95% C.I. 2.5–27; P=0.0001). Regularity in visiting the dentist was also an important predictor of referral to sedation. The odds of sedation referral increased 9-fold when the pattern of attendance falls from “at least once every six months” to “at most once in a 1–3 year period” (OR=9.2; 95% C.I. 1.9–44; P=0.01). Age had a borderline significant effect on referral to sedation with a 5% decrease in the odds of referral for each year increase in age (OR=0.95; 95% C.I. 0.90 – 1.0; P=0.07). The estimators of the log-odds-ratio and their standard errors for the effects of anxiety, attendance and age on sedation referral are also shown in Figure 1.
Table 2.
Estimates for the Multivariate Logistic Regression on Referral to Sedation
| Mediated effects included (ll=−24.4) | Mediated effects excluded (ll=−28.2) | |||||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% C. I. | P | Odds Ratio | 95% C.I. | P | |||
| Age | 0.95 | 0.89 | 1.02 | 0.15 | 0.95 | 0.90 | 1.00 | 0.07 |
| Gender | 0.84 | 0.16 | 4.37 | 0.84 | ||||
| Education | 1.60 | 0.33 | 7.72 | 0.56 | ||||
| Bad experience | 1.78 | 0.31 | 10.40 | 0.52 | ||||
| Anxiety | 1.09 | 1.03 | 1.15 | 0.002 | 1.11 | 1.06 | 1.16 | 0.0000 |
| Attendance | ||||||||
| Irregular vs Regular | 9.53 | 1.64 | 55.44 | 0.01 | 9.17 | 1.91 | 44.00 | 0.01 |
| Oral Health | ||||||||
| Good/Excellent vs Fair/Poor | 1.13 | 0.22 | 5.86 | 0.88 | 1.10 | 0.24 | 5.07 | 0.90 |
ll=log-likelihood
N=150
In the univariate analysis, when regularity of attendance or anxiety were not adjusted for, the covariates gender (OR=0.32; 95% C.I., 0.16–0.67; P=0.002), education (OR=5.5; 95% C.I., 2.2–13.4; P<0.001) and a past bad experience (OR=5.3; 95% C.I., 2.4–11.5; P<0.001) showed associations with referral to sedation but adding the direct effects of these variables to the principal model (Table 2) led to a very small change in the log-likelihood (ll). The reason for this can be seen from the interrelationships of these three variables with other variables in the sub-model (Figure 1). Past bad experiences, education and gender are significantly associated with anxiety. Past bad experience was found to be the most important determinant of anxiety. In a logistic regression the odds of a patient having a high level of anxiety (37+ in the DFS) are 7-fold for those patients recalling a bad past experience (OR=7; 95% C.I., 2.5–19.4; P=0.000). However, in multiple logistic regressions that adjust for anxiety, the significance of the effects on referral to sedation were completely lost for these three covariates: bad past experience (OR=1.7; 95% C.I., 0.44–6.2; P= 0.46), gender (OR=0.89; 95% C.I. 0.27–3; P=0.85) and education (OR=1.5; 95% C.I. 0.43– 5.5; P=0.51). This suggests that they are mediating relationships (42), and it is anxiety (and irregularity of attendance), rather than the mere presence of a bad experience or the level of education or the gender, which causes the patient to be referred for sedation. Thus, these three covariates (gender, education and a bad past experience) appear to affect the risk of referral to sedation only indirectly, via the level of anxiety. Likewise, in the presence of anxiety, dental health did not have a significant direct effect on referral to sedation.
Discussion
The hypothesis that, when controlling for gender, past bad experiences, and level of education, higher dental anxiety and previous irregular attendance directly impact the probability of referral for sedation within the NHS in London is supported. Poor self-reported oral health status per se is not an indicator of an increased probability of sedation referral: its apparent effect is one of mediation of anxiety and irregular attendance. We tested a formal model that incorporated factors previously demonstrated to be related to one another and dental anxiety (25) but had not been used to examine the process of referral for treatment under sedation in the UK.
These results are consistent with the observation that the dentally anxious find themselves in a cycle of anxiety, poor experiences, irregular attendance and declining oral health (4) that motivates practitioner referral for sedation for symptomatic care. The risk is that general practitioners interpret poor oral health not as a symptom of this cycle but rather as indication of dental indifference (44). While humane, the use of sedation treatment alone helps maintain the current cycle (37–38). There is a need for a model combining the use of sedation for anxious individuals with urgent treatment need with ongoing treatment based on graded exposure to assist the individual in overcoming their dental fear and encouraging regular attendance (45). These services need not be provided exclusively by psychologists; dentists and nurses can easily be trained, and fear reduction for many can be accomplished in as little as a single purposeful visit (46). Research in at least one referral center in the UK has shown that fearful patients will opt for this treatment if it is available (47). With reduced use of sedation for treatment of dental symptoms alone, it can become more widely available as part of comprehensive care where the curative treatments are long and arduous or unpleasant for patients.
The primary task of the NHS and other funders and organizers of dental care is then to expand population based and individual preventive services in order to reduce the burden of oral disease on the population. Better oral health will result in fewer poor treatment experiences that have been shown to be the root cause of much dental anxiety and avoidance (7). Because most individuals develop their fears of dentistry as children or adolescents (48), more effort needs to be expended at this stage.
Limitations of the current study lie in its cross-sectional design and single clinical location. However, creating a concurrent snapshot of patients’ anxiety, dental attendance, and oral health status within two different yet related clinical settings provides valuable information regarding patients’ motivation for dental care and their perceived ability to receive this care. Practitioners looking to provide additional behaviorally-oriented fear management strategies to patients can look to individual patient variables such as patient gender, education level, and history of negative dental experiences to help tailor such strategies to their patient population and ideally improve patient adherence to regular dental care. Since the sample is one of convenience, the proportion of individuals with high levels of dental fear in the study overall is higher than would be anticipated for a random survey of the population. As a result relationships between measures of anxiety and referral may have been more apparent than in a sample of the same size drawn from the population at random. While this study clearly demonstrates the relationship between fear, irregular attendance and referral for sedation, the magnitude of the relationship may be diminished in a random population survey. The results may be attributable in part to an imbalance in group sizes and care-seeking behavior not accounted for in the design of the study. Furthermore the generalisability of the findings may be limited by consideration of the location of the study, patients referred to a tertiary care centre for either sedation or advanced restorative treatment are likely to have greater treatment needs, and perhaps more severe levels of dental fear than individuals treated in primary care settings. However the extent to which this will modify the relationships described is an empirical question. There is a need to reproduce these studies in general population samples attending primary dental care services.
Conclusions
Treatment under sedation appears to be motivated by both fear and irregularity of attendance patterns. Instituting stronger community based and individual preventive services that address the root cause of symptomatic care and the development of fear as well as providing for dental anxiety treatment is needed.
Acknowledgments
Supported, in part, by a generous grant to King’s College London Dental Institute from the Society for the Advancement of Anaesthesia in Dentistry (www.saad.org.uk) and grant number T32DE07132 from the National Institute of Dental and Craniofacial Research, NIH, Bethesda, MD USA.
References
- 1.Milgrom P, Fiset L, Melnick S, Weinstein P. The prevalence and practice management consequences of dental fear in a major US city. J Am Dent Assoc. 1988 May;116(6):641–647. doi: 10.14219/jada.archive.1988.0030. [DOI] [PubMed] [Google Scholar]
- 2.Stouthard ME, Hoogstraten J. Prevalence of dental anxiety in The Netherlands. Community Dent Oral Epidemiol. 1990 Jun;18(3):139–142. doi: 10.1111/j.1600-0528.1990.tb00039.x. [DOI] [PubMed] [Google Scholar]
- 3.Armfield JM, Spencer AJ, Stewart JF. Dental fear in Australia: who’s afraid of the dentist? Aust Dent J. 2006 Mar;51(1):78–85. doi: 10.1111/j.1834-7819.2006.tb00405.x. [DOI] [PubMed] [Google Scholar]
- 4.Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007 Jan 14;7:1. doi: 10.1186/1472-6831-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heft MW, Meng X, Bradley MM, Lang PJ. Gender differences in reported dental fear and fear of dental pain. Community Dent Oral Epidemiol. 2007 Dec;35(6):421–428. doi: 10.1111/j.1600-0528.2006.00344.x. [DOI] [PubMed] [Google Scholar]
- 6.Rodríguez Vázquez LM, Rubiños López E, Varela Centelles A, Blanco Otero AI, Varela Otero F, Varela Centelles P. Stress amongst primary dental care patients. Med Oral Pathol Oral Cir Bucal. 2008 Apr 1;13(4):E253–256. [PubMed] [Google Scholar]
- 7.Oosterink FM, de Jongh A, Aartman IH. What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. Eur J Oral Sci. 2008 Feb;116(1):44–51. doi: 10.1111/j.1600-0722.2007.00500.x. [DOI] [PubMed] [Google Scholar]
- 8.Clarkson JE, Worthington HV. Association between untreated caries and age, gender and dental attendance in adults. Community Dent Oral Epidemiol. 1993 Jun;21(3):126–128. doi: 10.1111/j.1600-0528.1993.tb00735.x. [DOI] [PubMed] [Google Scholar]
- 9.Christensen LB, Petersen PE, Steding-Jessen M. Consumption of dental services among adults in Denmark 1994–2003. Eur J Oral Sci. 2007 Jun;115(3):174–179. doi: 10.1111/j.1600-0722.2007.00453.x. [DOI] [PubMed] [Google Scholar]
- 10.Locker D, Thomson WM, Poulton R. Psychological disorder, conditioning experiences, and the onset of dental anxiety in early adulthood. J Dent Res. 2001 Jun;80(6):1588–1592. doi: 10.1177/00220345010800062201. [DOI] [PubMed] [Google Scholar]
- 11.Maggirias J, Locker D. Five-year incidence of dental anxiety in an adult population. Community Dent Health. 2002 Sep;19(3):173–179. [PubMed] [Google Scholar]
- 12.Heaton LJ, Carlson CR, Smith TA, Baer RA, de Leeuw R. Predicting anxiety during dental treatment using patients’ self-reports: less is more. J Am Dent Assoc. 2007 Feb;138(2):188–195. doi: 10.14219/jada.archive.2007.0135. [DOI] [PubMed] [Google Scholar]
- 13.Poulton R, Waldie KE, Thomson WM, Locker D. Determinants of early- vs late-onset dental fear in a longitudinal-epidemiological study. Behav Res Ther. 2001 Jul;39(7):777–785. doi: 10.1016/s0005-7967(00)00060-7. [DOI] [PubMed] [Google Scholar]
- 14.Thomson WM, Locker D, Poulton R. Incidence of dental anxiety in young adults in relation to dental treatment experience. Community Dent Oral Epidemiol. 2000 Aug;28(4):289–294. doi: 10.1034/j.1600-0528.2000.280407.x. [DOI] [PubMed] [Google Scholar]
- 15.Doerr PA, Lang WP, Nyquist LV, Ronis DL. Factors associated with dental anxiety. J Am Dent Assoc. 1998 Aug;129(8):1111–1119. doi: 10.14219/jada.archive.1998.0386. Erratum in: J Am Dent Assoc 1998 Oct;129(10):1396. [DOI] [PubMed] [Google Scholar]
- 16.Woolfolk MW, Lang WP, Borgnakke WS, Taylor GW, Ronis DL, Nyquist LV. Determining dental checkup frequency. J Am Dent Assoc. 1999 May;130(5):715–723. doi: 10.14219/jada.archive.1999.0282. [DOI] [PubMed] [Google Scholar]
- 17.Ragnarsson E. Dental fear and anxiety in an adult Icelandic population. Acta Odontol Scand. 1998 Apr;56(2):100–104. doi: 10.1080/00016359850136067. [DOI] [PubMed] [Google Scholar]
- 18.Moore R, Birn H, Kirkegaard E, Brødsgaard I, Scheutz F. Prevalence and characteristics of dental anxiety in Danish adults. Community Dent Oral Epidemiol. 1993 Oct;21(5):292–296. doi: 10.1111/j.1600-0528.1993.tb00777.x. [DOI] [PubMed] [Google Scholar]
- 19.Acharya S. Factors affecting dental anxiety and beliefs in an Indian population. J Oral Rehabil. 2008 Apr;35(4):259–267. doi: 10.1111/j.1365-2842.2007.01777.x. [DOI] [PubMed] [Google Scholar]
- 20.Gatchel RJ, Ingersoll BD, Bowman L, Robertson MC, Walker C. The prevalence of dental fear and avoidance: a recent survey study. J Am Dent Assoc. 1983 Oct;107(4):609–610. doi: 10.14219/jada.archive.1983.0285. [DOI] [PubMed] [Google Scholar]
- 21.Liddell A, May B. Some characteristics of regular and irregular attenders for dental check-ups. Br J Clin Psychol. 1984 Feb;23( Pt 1):19–26. doi: 10.1111/j.2044-8260.1984.tb00622.x. [DOI] [PubMed] [Google Scholar]
- 22.Pohjola V, Lahti S, Vehkalahti MM, Tolvanen M, Hausen H. Association between dental fear and dental attendance among adults in Finland. Acta Odontol Scand. 2007 Aug;65(4):224–230. doi: 10.1080/00016350701373558. [DOI] [PubMed] [Google Scholar]
- 23.Pohjola V, Lahti S, Tolvanen M, Hausen H. Dental fear and oral health habits among adults in Finland. Acta Odontol Scand. 2008 Jun;66(3):148–153. doi: 10.1080/00016350802089459. [DOI] [PubMed] [Google Scholar]
- 24.Skaret E, Berg E, Kvale G, Raadal M. Psychological characteristics of Norwegian adolescents reporting no likelihood of visiting a dentist in a situation with toothache. Int J Paediatr Dent. 2007 Nov;17(6):430–438. doi: 10.1111/j.1365-263X.2007.00869.x. [DOI] [PubMed] [Google Scholar]
- 25.Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. The effects of social class and dental attendance on oral health. J Dent Res. 2008 Jan;87(1):60–64. doi: 10.1177/154405910808700110. [DOI] [PubMed] [Google Scholar]
- 26.Abrahamsson KH, Berggren U, Hakeberg M, Carlsson SG. Phobic avoidance and regular dental care in fearful dental patients: a comparative study. Acta Odontol Scand. 2001 Oct;59(5):273–279. doi: 10.1080/000163501750541129. [DOI] [PubMed] [Google Scholar]
- 27.Schuller AA, Willumsen T, Holst D. Are there differences in oral health and oral health behavior between individuals with high and low dental fear? Community Dent Oral Epidemiol. 2003 Apr;31(2):116–121. doi: 10.1034/j.1600-0528.2003.00026.x. [DOI] [PubMed] [Google Scholar]
- 28.Mehrstedt M, John MT, Tönnies S, Micheelis W. Oral health-related quality of life in patients with dental anxiety. Community Dent Oral Epidemiol. 2007 Oct;35(5):357–363. doi: 10.1111/j.1600-0528.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 29.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994 Mar;11(1):3–11. [PubMed] [Google Scholar]
- 30.McGrath C, Bedi R. The association between dental anxiety and oral health-related quality of life in Britain. Community Dent Oral Epidemiol. 2004 Feb;32(1):67–72. doi: 10.1111/j.1600-0528.2004.00119.x. [DOI] [PubMed] [Google Scholar]
- 31.McGrath C, Bedi R. Can dental attendance improve quality of life? Br Dent J. 2001 Mar 10;190(5):262–265. doi: 10.1038/sj.bdj.4800944. [DOI] [PubMed] [Google Scholar]
- 32.Cohen SM, Fiske J, Newton JT. The impact of dental anxiety on daily living. Br Dent J. 2000 Oct 14;189(7):385–390. doi: 10.1038/sj.bdj.4800777. [DOI] [PubMed] [Google Scholar]
- 33.Allen EM, Girdler NM. Attitudes to conscious sedation in patients attending an emergency dental clinic. Prim Dent Care. 2005 Jan;12(1):27–32. doi: 10.1308/1355761052894149. [DOI] [PubMed] [Google Scholar]
- 34.Baker RA, Farrer S, Perkins VJ, Sanders H. Emergency dental clinic patients in South Devon, their anxiety levels, expressed demand for treatment under sedation and suitability for management under sedation. Prim Dent Care. 2006 Jan;13(1):11–18. doi: 10.1308/135576106775193932. [DOI] [PubMed] [Google Scholar]
- 35.Dionne RA, Gordon SM, McCullagh LM, Phero JC. Assessing the need for anesthesia and sedation in the general population. J Am Dent Assoc. 1998 Feb;129(2):167–173. doi: 10.14219/jada.archive.1998.0173. [DOI] [PubMed] [Google Scholar]
- 36.Chanpong B, Haas DA, Locker D. Need and demand for sedation or general anesthesia in dentistry: a national survey of the Canadian population. Anesth Prog. 2005 Spring;52(1):3–11. doi: 10.2344/0003-3006(2005)52[3:NADFSO]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berggren U. Long-term effects of two different treatments for dental fear and avoidance. J Dent Res. 1986 Jun;65(6):874–876. doi: 10.1177/00220345860650060101. [DOI] [PubMed] [Google Scholar]
- 38.Hakeberg M, Berggren U, Carlsson SG, Gröndahl HG. Long-term effects on dental care behavior and dental health after treatments for dental fear. Anesth Prog. 1993;40(3):72–77. [PMC free article] [PubMed] [Google Scholar]
- 39.Boyle CA, Newton JT, Milgrom P. Who is referred for sedation for dentistry and why? Br Dent J. 2009 Mar 28;206(6):E12. doi: 10.1038/sj.bdj.2009.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kleinknecht RA, Thorndike RM, McGlynn FD, Harkavy J. Factor analysis of the dental fear survey with cross-validation. J Am Dent Assoc. 1984 Jan;108(1):59–61. doi: 10.14219/jada.archive.1984.0193. [DOI] [PubMed] [Google Scholar]
- 41.Baron R, Kenney D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 42.Aiken L, West S. Multiple regression: Testing and interpreting interaction effects. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 43.Bentler PM. EQS: Structural equations program manual. Los Angeles: BMDP Statistical Software Inc; 1989. [Google Scholar]
- 44.Nuttall NM. Initial development of a scale to measure dental indifference. Community Dent Oral Epidemiol. 1996 Apr;24(2):112–116. doi: 10.1111/j.1600-0528.1996.tb00825.x. [DOI] [PubMed] [Google Scholar]
- 45.Kvale G, Berggren U, Milgrom P. Dental fear in adults: A meta-analysis of behavioral interventions. Community Dent Oral Epidemiol. 2004;32(4):250–264. doi: 10.1111/j.1600-0528.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 46.Vika M, Skaret E, Raadal M, Ost LG, Kvale G. One- vs. five-session treatment of intra-oral injection phobia: a randomized clinical trial. Eur J Oral Sci. 2009 Jun;117(3):279–285. doi: 10.1111/j.1600-0722.2009.00628.x. [DOI] [PubMed] [Google Scholar]
- 47.McGoldrick P, Levitt J, deJongh A, Mason A, Evans D. Referrals to a secondary care dental clinic for anxious adult patients: implications for treatment. Brit Dent J. 2001;191:686–688. doi: 10.1038/sj.bdj.4801270. [DOI] [PubMed] [Google Scholar]
- 48.Locker D, Liddell A, Dempster L, Shapiro D. Age of onset of dental anxiety. J Dent Res. 1999 Mar;78(3):790–796. doi: 10.1177/00220345990780031201. [DOI] [PubMed] [Google Scholar]