Abstract
Background
Inadequate participation in physical activity is a serious public health issue in the United States, with significant disparities among population groups. In particular, there is a scarcity of information about physical activity among Caribbean Hispanics, a group on the rise.
Methods
Our goal was to accumulate data on physical activity among Caribbean Hispanic women living in New York and determine the relation between physical activity and age, marital status, education, income, primary language, and children in the household. To this end, a survey adapted from the National Health Interview Survey of the National Center for Health Statistics assessing type, frequency, and duration of physical activity was administered.
Results
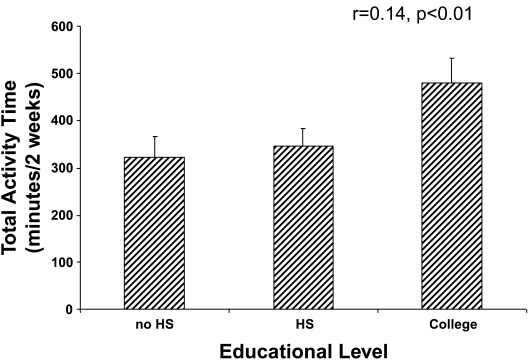
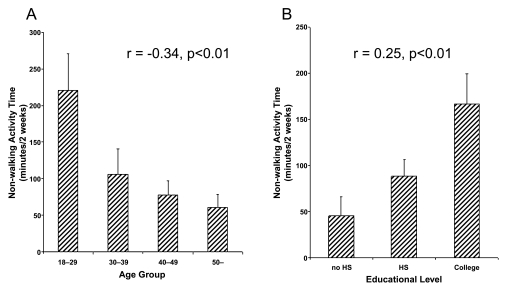
There were 318 self-identified Hispanic women who participated. Total activity time, mean 385 ± 26 minutes, and education (r = 0.14, p < 0.01) were significantly related. Women who had attended some college had greater total activity time than those with some high school education (p = 0.046) or < 8th grade education (p = 0.022). Walking as a form of transportation was the most frequent pursuit, 285 ± 21 minutes. Age (r = −0.34, p < 0.001) and education (r = 0.25, p < 0.001) correlated with nonwalking activity time (leisure time). Nonwalking activity times were greater in younger, that is, 18–29 years (p < 0.001) and college-educated women (p < 0.001). Physical activity recommendations were met by 11%; and 17% reported no physical activity.
Conclusions
Among Caribbean Hispanic women living in New York City, the current recommendations for physical activity are met by 11%, and physical activity and education are significantly related. Our observation that education is a critical factor related to physical activity suggests that programs to address the promotion of a physically active lifestyle are needed.
Introduction
Inadequate physical activity is a serious public health issue in the United States, and despite public health efforts, the proportion of the population engaging in healthful levels of physical activity is low.1 To address this, recommendations for adult physical activity, published over a decade ago, called for at least 30 minutes of moderate-intensity physical activity most days of the week.2–4 Since the original recommendations, reports have demonstrated a significant relation between physical activity and risk of cardiovascular disease (CVD) in both men and women.5,6 It has been suggested that some people have not accepted the original recommendations, others have misinterpreted them, and some may not be aware of the health benefits of activity to improve and maintain health. More recently, updated recommendations clarified moderate-intensity physical activity and identified 30 minutes on 5 days per week as the recommended minimum or vigorous-intensity aerobic activity for a minimum of 20 minutes on 3 days each week.7 More than 10 years have passed since the initial recommendations, yet physical inactivity remains a pressing public health issue.
There are significant disparities in activity levels among population groups in the United States. Reduced levels of leisure time physical activity are higher among women than men, higher among Hispanics and African Americans than whites, and higher among the less affluent.8–10 Despite increased leisure time physical activity during the recent past, Hispanics are the most physically inactive racial/ethnic group in the United States.11 Given that they are the fastest growing minority in the United States, the low rate of participation in physical activity is a public health concern.12 There are approximately 40 million Hispanics in the United States, representing 14% of the nation's population. These estimates are projected to reach 102 million by the year 2050, when they will comprise 24% of the US population.13 Hispanics from the Caribbean/Atlantic islands are the fastest rising subgroup, consisting of relatively recent immigrants from the Dominican Republic, Puerto Rico, and Cuba,14,15 with significant numbers residing in Washington Heights-Inwood and Northern Manhattan in New York City.16,17
Reports that patterns of physical activity among Hispanics vary with region of origin denote that effective interventions to improve physical activity should be based on an understanding of culture and environment.18 Despite the rapid growth of Caribbean Hispanics and their predisposition for vascular disease,19,20 there is scant information about their lifestyle activities impacting on vascular disease. Understanding physical activity patterns within this subsample should expand existing knowledge of activity practices currently based primarily on Mexican Americans.21,22 Accordingly, the aim of this work is to document the patterns of activity among Caribbean Hispanic women living in New York City and assess the relation between physical activity practices and education, age, marital status, household income, primary language, and number of children in the household.
Materials and Methods
Participants were healthy, adult, nonpregnant women attending outpatient health centers in Washington Heights-Inwood and Northern Manhattan of the New York Presbyterian Hospital, Columbia University Medical Center. Data were collected from the period July 2005 to July 2006; data from 40 subjects were included in a preliminary oral presentation.23 Informed consent was obtained after permission to approach participants was obtained from primary care physicians. The protocol and consent were approved by Columbia University's Institutional Review Board, and surveys were labeled with a three-digit code to protect subject identity. Participants underwent in-person evaluations to determine if they were ambulatory and did not have restrictions on physical activity that would bias participation in a physical activity survey, such as CVD (myocardial infarction, chest pain syndrome, angina pectoris, bypass surgery), neurological disease (stroke, transient ischemic attack, neuromotor diseases), pulmonary disease (emphysema or chronic bronchitis), arthritis or trauma, pregnancy, or any acute or chronic disease preventing activity within the preceding 2 weeks.
Physical activity assessment—determination of patterns of total activity time, walking time, and nonwalking activity time (leisure time)
A questionnaire adapted from the National Health Interview Survey of the National Center for Health Statistics,24,25 was used to measure recent physical activity. This survey has been found to be reliable in evaluating a variety of age groups, including elderly subjects.26,27 The questionnaire records the frequency and duration of different recreational activities during the 2-week period before the survey and whether this was typical. The physical activity assessments were not designed to evaluate lifelong exercise practices, exercise patterns at younger ages, physical conditioning, or quantitative estimations of energy expenditure. Our instrument measured physical activity during the preceding 2 weeks. The 2-week period of activity recall was deemed reliable, short enough to allow reasonably accurate recall, yet long enough to represent the usual activity patterns of most people.28 In the Northern Manhattan Stroke Study, construct validity for physical activity assessment was demonstrated by means of a significant negative correlation of physical activity and body mass index (BMI).25
Twenty-five questions, requiring 15–20 minutes to answer, were provided in Spanish or English depending on the primary language of participants. If subjects could not complete the questionnaire independently (n = 12) because of language comprehension, reading level, or other (e.g., forgot glasses), a study coordinator was available to read the survey. Questions about activities included walking, calisthenics, dancing, bowling, and gardening and more vigorous activity, such as hiking, tennis, swimming, bicycle riding, jogging, and aerobic dancing. An additional Other category was provided for activities that did not fit one of the specified activities. A series of yes/no responses was recorded for each of the questions, posed as: In the last 2 weeks, have you engaged in physical activity? Each affirmative response was followed by two other questions: On average, how many times did you perform this activity over the last 2 weeks? and On average, how many minutes each time? Participants were asked to record the frequency, duration, and intensity (strenuous, moderate, and mild) and whether this was typical. From these responses, the frequency and duration of each activity were computed. Lifestyle activities were categorized as (1) leisure time, such as sports and other exercise, (2) occupational, (3) transportation-related activity, such as walking, and (4) household activity. Minutes of physical activity were determined for (1) total activity time, (2) walking time, and (3) nonwalking activity time (leisure time activity). All activity time values are reported as mean ± standard error of the mean (SEM) for a 2-week period. An average of 150 or more minutes per week (300 minutes over 2 weeks) of moderate or strenuous activity was used as a cutoff point for comparison with previous reports regarding the amount of weekly exercise and fitting with the recommendations about physical activity and public health. The frequency and duration of each activity were computed as total activity time: the sum of the products for the number of sessions multiplied by the minutes per session for each activity over the preceding 2 weeks. When a range of minutes or number of sessions was given, the midpoint was used to calculate time. When information was missing regarding the number of minutes per session (7 occurrences), the mean duration among responders for that activity was used for calculation of total activity time. When the number of sessions for a particular activity was missing (11 occurrences), a single session was assumed.
Demographics
Race/ethnicity, age, marital status, education, native language, country of origin, and number of adults and children living in the household were examined. Race/ethnicity was defined by self-identification based on a series of interview questions modeled after the U.S. census. Race was mutually exclusive and defined by six categories: white, black, Indian (American), Eskimo, Asian or Pacific Islander, and other. Race/ethnic groupings were mutually exclusive. All participants responding affirmatively to being of Spanish origin or identifying themselves as Hispanic were classified as Hispanic, and the country of origin was determined.29 Social resources were defined by educational level and health insurance status. All subjects had insurance, including (1) Medicaid only or Medicaid/Medicare and no other insurance, (2) Medicare only, and (3) other types. Income data were derived using median household income according to ZIP code.
Statistical analysis
Spearman's rank correlation was used to determine the association of age and ordered categorical variables on total activity time as well as walking and nonwalking activity times recorded on the questionnaire. Total activity time was not normally distributed, and a square root transformation that provided suitable distributional characteristics, as judged by a Kolmogorov-Smirnov test of normality, a goodness-of-fit test (nonparametric method for comparing two samples), was performed.30 Multifactorial analysis of variance (ANOVA) models were used to jointly assess the effect of demographic characteristics and other recorded variables on total activity time and walking and nonwalking time. For the multivariable models, a backwards elimination technique was used for variable selection Candidate variables included age (categorized as < 30, 30–39, 40–49, and > 50 years), education (categorized as <8th grade, some level of high school including high school graduates, and some college or greater), income (<$30,000 and >$30,000), number of children (0, 1–2, > 3), and outpatient site. Values are reported as mean ± SEM or percent frequency, and p < 0.05 was considered significant for all analyses.
Results
There were 318 self-identified Hispanic women who completed the survey; participants averaged 44 ± 1 years (range 18–84 years) (Table 1). The country of birth or origin was determined in 286 (90%). Of these, 98% were from the Caribbean Atlantic islands of the Dominican Republic (72%), Puerto Rico (22%), Cuba (4%), and other regions (2%), including Venezuela (n = 3), Ecuador (n = 1), Peru (n = 1), and Mexico (n = 1). Thirty-one percent were married; 68% reported they were either single (34%), separated (15%) or divorced (14%), or widowed (5%) (Table 1). The number of children in the household was 0 (36%), 1 (23%), 2 (26%), and ≥3 (15%). Fourteen percent were graduates of college; the majority, however, had less education: ≤8th grade (28%), some high school (17%), high school graduate (20%), and some college (21%). Income was categorized as ≤$30,000 (41%) or >$30,000 (59%); the average household income was $30,841.
Table 1.
Demographic Data of Participants (n = 318)
| Number | % | |
|---|---|---|
| Birthplace or country of origin | ||
| Dominican Republic | 206 | 72 |
| Puerto Rico | 63 | 22 |
| Cuba | 11 | 3.9 |
| Other | 6 | 2.1 |
| Marital status | ||
| Single | 108 | 34.1 |
| Married | 98 | 30.9 |
| Widowed | 15 | 4.7 |
| Divorced | 44 | 13.9 |
| Separated | 46 | 14.5 |
| 6 | 1.9 | |
| Number of children | ||
| 0 | 111 | 35.8 |
| 1 | 71 | 22.9 |
| 2 | 80 | 25.8 |
| 3 | 35 | 11.3 |
| ≥4 | 13 | 4.2 |
| Education | ||
| ≤8th grade | 88 | 27.9 |
| Some high school | 55 | 17.5 |
| High school graduate | 62 | 19.7 |
| Some college | 66 | 21.0 |
| College graduate | 44 | 14.0 |
| Income | ||
| $10,000–30,000 | 127 | 41.0 |
| >$30,000 | 183 | 59.0 |
| Native language | ||
| Spanish | 276 | 84.4 |
| English | 39 | 12.3 |
| Other | 1 | 0.3 |
Physical activity: Total activity time, walking, and nonwalking activity time
The total activity time averaged 385 ± 26 minutes over 14 days. Eleven percent of participants met the physical activity recommendation of moderately intense activity for ≥30 minutes ≥ 5 times per week; 17% reported no participation in physical activity. Walking, a form of transportation, was the most frequent pursuit, averaging 285 ± 21 minutes. Total nonwalking exercise time averaged 106 ± 15 minutes. Total nonwalking activity time included jogging 25 ± 6 minutes, dancing 25 ± 4 minutes, calisthenics 18 ± 4 minutes, aerobics 18 ± 6 minutes, swimming 10 ± 4 minutes, and biking 6 ± 2 minutes.
Relation between total and nonwalking activity time and variables
There was a significant correlation between the total activity time and level of education (r = 0.14, p < 0.01) (Fig. 1). No significant association, however, was observed with age, income, primary or native language, or number of children. Similarly, the ANOVA demonstrated significant differences in total activity time only with education (Table 2). Greater total activity time was determined in women who had attended at least some college than in those with at least some high school education (p = 0.046) or those with ≤8th grade education (p = 0.022).
FIG. 1.
Total activity time and education level.
Table 2.
Analysis of Variance Models
| SSa | df | MS | f value | p value | |
|---|---|---|---|---|---|
| A. Total activity time | |||||
| Education categoryb | 1118.6 | 2 | 559.08 | 4.37 | 0.013 |
| Error | 39915.4 | 312 | 127.93 | ||
| B. Nonwalking time | |||||
| Age categoryc | 1105.7 | 3 | 368.6 | 5.28 | 0.002 |
| Education categoryb | 424.63 | 2 | 212.3 | 3.04 | 0.049 |
| Error | 21285.1 | 305 | 69.79 | ||
| C. Walking time | |||||
| Error | 33677.7 | 317 | 106.24 | ||
SS, sum of squares; df, degrees of freedom; MS, mean squares.
Education information missing in 3 subjects.
Age missing in 4 subjects.
Nonwalking activity time correlated significantly with age (r = −0.34, p < 0.001) (Fig. 2A) and level of education (r = 0.25, p < 0.001) (Fig. 2B). Both age (p = 0.002) and education (p = 0.049) were independently significant in the ANOVA model (Table 2). Nonwalking activity times were significantly greater in the 18–29-year age group than in older age groups and in college-educated women than in those with an ≤8th grade education (Fig. 2). No variable was significantly associated with walking times.
FIG. 2.
Nonwalking activity time and (A) age and (B) education level.
Discussion
Inadequate physical activity is a serious public health issue in the United States, and significant disparities in activity levels exist.1 In this cohort of adult women, less than one eighth meet the current national recommendations for physical activity estimated by total activity time, and 17% do not participate in any physical activity. Physical activity in this population is considerably less than currently recommended. Furthermore, most physical activity involves walking, which averaged 285 ± 21 minutes, rather than more strenuous endeavors. Our population had limited nonwalking activity (e.g., jogging, running, dancing) which averaged only 106 ± 15 minutes over 14 days.
Distinctions between Hispanic subgroups
Data concerning physical activity for women of minority racial and ethnic groups are sparse despite the fact that minority women are at risk for adverse vascular outcomes associated with limited physical activity.31 Overall, non-Hispanic white adults (65.7%) are more likely than non-Hispanic black adults (49.3%) and Hispanic adults (45%) to engage in some leisure time physical activity. Among Hispanics, gender differences exist, such that 69% of men but 89% women never engage in vigorous leisure time activity.32
The U.S. Census Bureau does not cross-tabulate specific Spanish-origin groups; breakdowns are presented only for Hispanics as a whole. Grouping Hispanics without consideration for social, historical, cultural, health, and socioeconomic distinctions33,34 hampers our understanding of lifestyle differences impacting behavior.35 It was our goal to describe physical activity among a subgroup on the rise, whose origins or ancestors derive primarily from the Caribbean/Atlantic islands. Hispanics from the Caribbean/Atlantic islands and coastal regions of Central and South America have nutritional habits and diet, traditions, and customs that differ from Mexicans, as well as distinctions in health and indicators of socioeconomic status.36,37 Only 20% of Caribbean Hispanics have an active level of daily activity compared with 31% of Mexicans.38 In our cohort, inactivity is greater (89%) than among non-Hispanic white women (79.7%) or Mexican American women (61.5%).39
Education
Among our subjects, greater total activity time was found among those who had attended at least some college compared with those with some high school education or ≤8th grade education. Moreover, age and education were correlated with nonwalking activity times (leisure time). Nonwalking activity times were significantly greater in the 18–29-year-old age group and in college-educated women than those with ≤8th grade education. Given the risk reduction associated with even minimal levels of physical activity, opportunities to educate and counsel on the value of activity are significant.40
Limitations
The study provides insight into a largely Caribbean Hispanic population living in New York City and may not be representative of all women from Caribbean/Atlantic islands. As physical activity was assessed by self-report, some misclassification due to recall is possible. Further, environmental barriers to activity, such as transportation, child care, isolation, character of the neighborhood, and safety, were not examined. Studies of increased sample size and larger geographic areas are needed.
Conclusions
Our findings describe low physical activity patterns among a subgroup of Hispanics whose origins or ancestors derive primarily from Caribbean/Atlantic islands. Current national recommendations for physical activity are met by 11%, and 17% do not participate in any physical activity. Our observation that education is a critical factor related to participation in physical activity suggests that programs are needed to address the promotion of a physically active lifestyle.
Footnotes
Presented in part at the 2nd International Conference on Women, Heart Disease and Stroke, Orlando, Florida, February 18, 2005.
Acknowledgments
This work was supported in part by the Department of Health and Human Services (HHCWH05003), the New York Presbyterian Hospital Auxiliary of the Columbia University Medical Center, and the Arlene and Joseph Taub and the Norman and Rosita Winston Foundations.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Centers for Disease Control Prevention. Trends in leisure-time physical inactivity by age, sex, and race/ethnicity—United States, 1994–2004. MMWR. 2005;54:991–994. [PubMed] [Google Scholar]
- 2.NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. Physical activity and cardiovascular health. JAMA. 1996;276:241–246. [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. Physical activity and health: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 1996. [Google Scholar]
- 4.Pate RR. Pratt M. Blair SN, et al. Physical activity and public health: A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 5.Manson JE. Greenland AZ. LaCroix , et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;341:650–658. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 6.Lee IM. Rexrode KM. Cook NR. Manson JE. Buring JE. Physical activity and coronary heart disease in women: Is “no pain, no gain” passe? JAMA. 2001;285:1447–1454. doi: 10.1001/jama.285.11.1447. [DOI] [PubMed] [Google Scholar]
- 7.Haskell WL. Lee IM. Pate R, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exer. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 8.Chapter 22. Physical activity and fitness: Physical activity in adults. Healthy People. 2010. www.healthy-people.gov/document/html/volume2/2physical.htm www.healthy-people.gov/document/html/volume2/2physical.htm
- 9.Estabrooks PA. Lee RE. Gyurcsik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Ann Behav Med. 2003;25:100–104. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- 10.Freeman G. Lethbridge-Cejku M. Access to health care among Hispanic or Latino women: United States, 2000–2002. Adv Data. 2006;368:1–25. [PubMed] [Google Scholar]
- 11.Trends in leisure time physical inactivity by age, sex, race/ethnicity—United States 1994–2004. MMWR. 2005;54:991–994. [PubMed] [Google Scholar]
- 12.Slattery ML. Sweeney C. Edwards S, et al. Physical activity patterns and obesity in Hispanic and non-Hispanic white women. Med Sci Sports Exerc. 2006;38:33–41. doi: 10.1249/01.mss.0000183202.09681.2a. [DOI] [PubMed] [Google Scholar]
- 13.Ramirez RR. de la Cruz GP. Current Population Report. Washington, DC: U.S. Census Bureau; 2002. The Hispanic population in the United States: March 2002; pp. P20–545. [Google Scholar]
- 14.National Coalition of Hispanic Health Human Services Organizations. Delivering preventive health care to Hispanics: A manual for providers. Washington, DC: US Government Printing Office; 1988. [Google Scholar]
- 15.Garfield R. Abramson D. Washington Heights/Inwood: The health of a community. New York: Columbia University; 1995. [Google Scholar]
- 16.Hernandez R. Rivera-Batiz F. Agodin R. Dominican New Yorkers: A socioeconomic profile. New York: CUNY Dominican Studies Institute; 1995. [Google Scholar]
- 17.Kerker BD. Kim M. Mostashari FM, et al. Women at risk: The health of women in New York City. New York: New York City Department of Health and Mental Hygiene; 2005. [Google Scholar]
- 18.Ham SA. Yore MM. Kruger J. Moeti R. Health GW. Physical activity patterns among Latinos in the United States: Putting the pieces together. Prev Chronic Dis. 2007;4(A92):1–13. [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez CJ. Sacco RL. Sciacca RR. Boden-Albala B. Homma S. DiTullio MR. Physical activity attenuates the effect of increased left ventricular mass on the risk of ischemic stroke. J Am Coll Cardiol. 2002;39:1482–1488. doi: 10.1016/s0735-1097(02)01799-0. [DOI] [PubMed] [Google Scholar]
- 20.Hu FB. Stampfer MJ. Colditz GA, et al. Physical activity and risk of stroke in women. JAMA. 2000;284:1784–1785. doi: 10.1001/jama.283.22.2961. [DOI] [PubMed] [Google Scholar]
- 21.Crespo CJ. Smit E. Carter-Pokras O. Andersen R. Acculturation and leisure time physical inactivity in Mexican American adults: Results from NHANES III, 1988–1994. Am J Public Health. 2001;91:1254–1257. doi: 10.2105/ajph.91.8.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abramson JH. Abramson AH. Survey methods in community medicine. 5th. Edinburgh & London: Livingstone; 2000. [Google Scholar]
- 23.Cassetta JA. Boden-Albala B. Sciacca R. Giardina E-G V. Effect of education and race/ethnicity on physical activity in an insured, urban population of women. Presented at the 2nd International Conference on Women, Heart Disease and Stroke; Orlando, FL. Feb 18;2005 . [Google Scholar]
- 24.Cassetta JA. Boden-Albala B. Sciacca RR. Giardina EGV. Association of education and race/ethnicity with physical activity in insured, urban women. J Womens Health. 2007;16:902–908. doi: 10.1089/jwh.2006.0141. [DOI] [PubMed] [Google Scholar]
- 25.Sacco R. Gan R. Boden-Albala B, et al. Leisure time physical activity and ischemic stroke risk: The Northern Manhattan Stroke Study. Stroke. 1998;29:380–387. doi: 10.1161/01.str.29.2.380. [DOI] [PubMed] [Google Scholar]
- 26.McPhillips JB. Pellettra KN. Barrett-Connor E, et al. Exercise patterns in a population of older adults. Am J Prev Med. 1989;2:65–72. [PubMed] [Google Scholar]
- 27.Sallis JF. Haskell WL. Wood PD, et al. Physical activity assessment methodology in the five city project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 28.Lamb KL. Brodie DA. Leisure-time physical activity as an estimate of physical fitness: A validation study. J Clin Epidemiol. 1991;44:41–52. doi: 10.1016/0895-4356(91)90199-j. [DOI] [PubMed] [Google Scholar]
- 29.Office of Management Budget. Race and ethnic standards for federal statistics and administrative reporting. Directive No.15. Fed Reg. 1978;43:19269. [PubMed] [Google Scholar]
- 30.Chakravarti IM. Laha RG. Roy J. Handbook of methods of applied statistics. Vol. 1. New York: John Wiley & Sons; 1967. pp. 392–394. [Google Scholar]
- 31.Crespo CJ. Smit E. Andersen RE. Race/ethnicity social class and their relation to physical inactivity during leisure time: Results from the Third National Health and Nutrition Examination Survey, 1980–1994. Am J Prev Med. 2000;18:46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- 32.Gonzales A. Keller C. Tiempo para mi: Family demands physical activity in older Latinas. South Online J Nurs Res. 2004. http://www.snrs.org/members/journal.html http://www.snrs.org/members/journal.html
- 33.Perez-Stable EJ. Ramirez A. Villareal R, et al. Cigarette smoking behavior among U.S. Latino men and women from different countries of origin. Am J Public Health. 2001;91:1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rodriguez RA. Hernandez GT. O'Hare AM. Glidden DV. Perez-Stable EJ. Creatinine levels among Mexican Americans, Puerto Ricans and Cuban Americans in the Hispanic Health and Nutrition Examination Survey. Kidney Int. 2004;66:2368–2373. doi: 10.1111/j.1523-1755.2004.66025.x. [DOI] [PubMed] [Google Scholar]
- 35.Poston WS., II Haddock CK. Olvera NE, et al. Evaluation of a culturally appropriate intervention to increase physical activity. Am J Health Behav. 2001;25:396–406. doi: 10.5993/ajhb.25.4.5. [DOI] [PubMed] [Google Scholar]
- 36.Hajat A. Lucas JB. Kington R. Health outcomes among Hispanic subgroups: Data from the National Health Interview Survey, 1992–95. Centers for Disease Control and Prevention, National Center for Health Statistics, Vital and Health Statistics. 2000;310:1–14. [PubMed] [Google Scholar]
- 37.National Center for Health Statistics. 2002 National Hispanic Health Leadership Summit. 2002.
- 38.National Health Interview Survey Data 2000. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; [May 16;2007 ]. [Google Scholar]
- 39.Heart disease and stroke statistics–2006 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 40.Thompson PD. Buchner D. Pina IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: A statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity) Circulation. 2003;107:3109–3116. doi: 10.1161/01.CIR.0000075572.40158.77. [DOI] [PubMed] [Google Scholar]