Abstract
Objective
To present estimates of the lifetime prevalence of DSM-IV mental disorders with and without severe impairment, their comorbidity across broad classes of disorder, and their sociodemographic correlates.
Method
The National Comorbidity Survey-Adolescent Supplement NCS-A is a nationally representative face-to-face survey of 10,123 adolescents aged 13–18 years in the continental U.S. DSM-IV mental disorders were assessed using a modified version of the fully structured World Health Organization Composite International Diagnostic Interview.
Results
Anxiety disorders were the most common condition (31.9%), followed by behavior disorders (19.1%), mood disorders (14.3%), and substance use disorders (11.4%), with approximately 40% of those with one class of disorder also meeting criteria for another class of lifetime disorder. The overall prevalence of disorders with severe impairment and/or distress was 22.2%; (11.2% with mood disorders; 8.3% with anxiety disorders; 9.6% behavior disorders). The median age of onset for disorder classes was earliest for anxiety (6 years), followed by 11 years for behavior, 13 years for mood, and 15 years for substance use disorders.
Conclusions
These findings provide the first prevalence data on a broad range of mental disorders in a nationally representative sample of U.S. adolescents. Approximately one in every 4–5 youth in the U.S. meets criteria for a mental disorder with severe impairment across their lifetime. The likelihood that common mental disorders in adults first emerge in childhood and adolescence highlights the need for a transition from the common focus on treatment of U.S. youth to that of prevention and early intervention.
Keywords: Epidemiology, adolescents, mental disorders, National Comorbidity Survey, correlates
INTRODUCTION
There has been tremendous growth in the field of child psychiatric epidemiology over the past two decades.1 The results of numerous community surveys in specific regions of the U.S.2–8 have shown that about one in every three to four children suffers from a mental disorder and that about one in ten has a Serious Emotional Disturbance, 9–11 with few affected youth receiving adequate mental health care. However, there has been a lack of empirical data on the prevalence and distribution of a wide range of DSM-IV mental disorders from a nationally representative sample of children or adolescents. Such information is necessary to establish resource allocation priorities for prevention, treatment, and research.
Based on the recommendations of the landmark Surgeon General’s Report on Mental Health12 and the recommendations of a subgroup of the National Institute of Mental Health (NIMH) National Advisory Mental Health Council,13 the NIMH established several research initiatives to address the lack of national statistics on mental health in children. Instruments for assessing mental health were added to two large national surveys including the Strengths and Difficulties Questionnaire (SDQ) to the National Health Interview Survey,14 and selected modules from the National Institute of Mental Health Diagnostic Interview Schedule for Children (DISC) Version 415 to the National Health and Nutrition Examination Survey.11 In addition to these measures, the National Comorbidity Survey Replication (NCS-R)16 was extended to assess a broad range of DSM-IV disorders in a nationally representative sample of youth aged 13–18 years, referred to as the National Comorbidity Survey Adolescent Supplement (NCS-A).17–20
The goals of the present report are: (1) to present the lifetime prevalence estimates of mental disorders and the proportion of disorders that are associated with severe impairment in a nationally representative sample of U.S. adolescents; (2) to examine the magnitude of overlap in the major classes of mental disorders; and (3) to describe the individual and familial sociodemographic correlates of these disorders.
Method
Sample and Procedure
The NCS-A is a nationally representative, face-to-face survey of 10,123 adolescents aged 13–18 years in the continental US.17 The survey was administered by the professional interview staff of the Institute for Social Research at the University of Michigan. The NCS-A was carried out in a dual-frame sample that included a household sub-sample and a school sub-sample.18, 20, 21 The overall NCS-A adolescent response rate combining the two sub-samples was 82.9%. Comparisons of sample and population distributions on census sociodemographic variables and the school sample on school characteristics revealed only minor differences that were corrected with post-stratification weighting.
One parent or parent surrogate of each participating adolescent was asked to complete a self-administered questionnaire (SAQ) that contained informant questions about the adolescent’s mental health. The full SAQ was completed by 6,491 parents. These recruitment and consent procedures were approved by the Human Subjects Committees of both Harvard Medical School and the University of Michigan. Once the survey was completed, cases were weighted for variation in within-household probability of selection (in the household sub-sample) and for residual discrepancies between the sample and the US population on the basis of socio-demographic and geographic variables. These weighting procedures are discussed in more detail elsewhere.18, 20 Socio-demographic variables assessed in the NCS-A include age (in years), sex, race/ethnicity, parent education, urbanicity, and marital status of parents. A poverty index ratio, based on family size and the ratio of family income to the family’s poverty threshold level, (≤1.5 poor, ≤3, ≤6, and > 6) was also included.
Table 1 presents the weighted socio-demographic characteristics of the study sample. About half of the sample was male (51.3%) and the mean age was 15.2 years, with a larger proportion of youth aged 13–14 years (36.2%), and approximately equal distributions of youth aged 15 (20.5%), 16 (21.0%), and 17–18 (22.3%) years. The sample was comprised of 65.6% non-Hispanic Whites, 15.1% non-Hispanic Blacks, and 14.4% Hispanics. In terms of family characteristics, 84.5% of the sample had parents who had completed at least high school, 14.7% had a poverty index ratio at 1.5 or lower, nearly half of the sample resided in a metropolitan area, and 78.6% had parents who were married or cohabiting.
Table 1.
Sociodemographic Characteristics of the National Comorbidity Survey-Adolescent Supplement (NCS-A) (N=10,123)
| Sociodemographic Characteristics | Category | N | Weighted % |
|---|---|---|---|
| Sex | Male | 4,953 | 51.3 |
| Female | 5,170 | 48.7 | |
| Agea | 13–14 | 3,870 | 36.2 |
| 15 | 1,887 | 20.5 | |
| 16 | 2,010 | 21.0 | |
| 17–18 | 2,356 | 22.3 | |
| Race | Non hispanic white | 5,634 | 65.6 |
| Non hispanic black | 1,953 | 15.1 | |
| Hispanic | 1,914 | 14.4 | |
| Other | 622 | 5.0 | |
| Parental education | less than high school | 1,684 | 15.5 |
| High school | 3,081 | 29.7 | |
| Some college | 1,998 | 19.4 | |
| College grad | 3,360 | 35.3 | |
| Parental marital statusb | married/cohabiting | 4,602 | 78.6 |
| previous married | 1,009 | 17.5 | |
| never married | 308 | 3.9 | |
| Poverty Index Ratio (PIR) | PIR ≤ 1.5 poor | 1,717 | 14.7 |
| PIR ≤ 3.0 | 2,023 | 19.1 | |
| PIR ≤ 6.0 | 3,101 | 31.9 | |
| PIR > 6 | 3,282 | 34.3 | |
| Urbanicity | Metro | 4,508 | 47.5 |
| Other urban | 3,304 | 37.6 | |
| Rural | 2,311 | 14.9 |
Note:
weighted mean (SE) age = 15.2 (0.1);
other/unknown marital status are not presented
Measures
Diagnostic assessment
Details of the diagnostic and risk factor measures are described by Merikangas et al.17 Briefly, a modified version of the World Health Organization (WHO) Composite International Diagnostic Interview Version 3.0 (CIDI), a fully structured interview administered by trained lay interviewers to generate DSM-IV diagnoses16 was administered to adolescents. Modifications to the CIDI involved enhancing the wording and appropriateness of the instrument for assessment of adolescents. Lifetime disorders assessed in the CIDI included mood disorders and episodes (major depressive disorder [MDD] or dysthymic disorder, bipolar I or II [BPD]), anxiety disorders (panic disorder, agoraphobia, social phobia, specific phobia, generalized anxiety disorder [GAD], posttraumatic stress disorder [PTSD], separation anxiety disorder [SAD]), behavior disorders (attention deficit/hyperactivity disorder [ADHD], oppositional defiant disorder [ODD], and conduct disorder [CD]), substance use disorders (alcohol abuse/dependence, drug abuse/dependence), and eating disorders (anorexia nervosa, bulimia nervosa, and binge eating disorder). Parents (or parent surrogates) were mailed a self-administered questionnaire (SAQ) in order to collect additional information on adolescent sociodemographic characteristics, developmental background, mental and physical health, and other family- and community-level factors. Parents who completed the SAQ provided full DSM-IV diagnostic information about MDD and dysthymic disorder, SAD, ADHD, ODD, and CD, whereas those completing the abbreviated SAQ only reported on ADHD. Based on prior research that has documented the value of supplemental parent reports22, 23, information from both the parent and adolescent were combined for major depression and behavior problems and classified as positive if either informant endorsed the diagnostic criteria. Definitions of all psychiatric disorders adhered to DSM-IV criteria and diagnostic hierarchy rules were applied for every disorder, with the exception of oppositional defiant disorder and substance use disorders. Psychiatric disorders derived from the modified CIDI showed good concordance with a clinical reappraisal sub-sample.19
Impairment criteria embedded in DSM-IV required endorsement of some/a lot/extreme level of impairment or moderate/severe/very severe level of symptom severity. In order to more clearly identify disorders that were clinically significant, our definition of severe lifetime disorders used higher thresholds of impairment that required endorsement of “a lot” or “extreme” impairment in daily activities, or “severe or very severe” distress. Severe emotional disorders required both distress and impairment to be present, and severe behavior disorders (ADHD, ODD, and CD) required endorsement of symptom criteria by both the parent and the adolescent.
Statistical Analysis
All statistical analyses were completed with the SUDAAN software package and utilize the Taylor series linearization method to take into account the complex survey design. Cross-tabulations were used to calculate prevalence and comorbidity. Logistic regression analysis was used to examine demographic correlates of prevalence; regression models included all sociodemographic variables simultaneously, and adjusted odds ratios are presented. Age-of-onset curves were generated using the Kaplan-Meier survival analysis method. Multivariate significance tests were calculated using Wald Chi-Square tests based on coefficient variance-covariance matrices that were adjusted for design effects using the Taylor series method. Statistical significance was based on two-sided design-based tests evaluated at a level of significance of 0.05.
Results
Lifetime Prevalence
Table 2 presents the lifetime prevalence rates of DSM-IV mental disorders by sex, age group, total DSM-IV disorders and disorders with severe impairment. Mood disorders affected 14.3% of the total sample, corresponding to 11.7% who met criteria for MDD or dysthymia and 2.9% for BPD. Females were twice as likely to experience unipolar mood disorders as compared to males, and somewhat more likely to experience BPD. The prevalence of all mood disorders increased uniformly with age, with a nearly two-fold increase from the 13–14 year age group to the 17–18 year age group. Severe cases of mood disorder (11.2% of the total sample) represented 74.4% of all MDD or dysthymic disorders, and 89.7% of all cases of BPD. The sex-specific rates for severe disorders (not presented in the table) maintained the same general patterns as were observed for the overall prevalence rates.
Table 2.
Lifetime Prevalence of DSM-IV Disorders by Sex and Age Group and Severe Impairment in the National Comorbidity Survey-Adolescent Supplement (NCS-A)
| DSM-IV Disordera | DSM-IV Disorders | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Age | Total | with Severe Impairment | |||||||||||
| Female | Male | 13–14 yr | 15–16 yr | 17–18 yr | ||||||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |
| Mood disorders | ||||||||||||||
| Major depressive disorder or dysthymia | 15.9 | 1.3 | 7.7 | 0.8 | 8.4 | 1.3 | 12.6 | 1.3 | 15.4 | 1.4 | 11.7 | 0.9 | 8.7 | 0.8 |
| Bipolar I or II | 3.3 | 0.4 | 2.6 | 0.3 | 1.9 | 0.3 | 3.1 | 0.3 | 4.3 | 0.7 | 2.9 | 0.3 | 2.6 | 0.2 |
| Any mood disorder | 18.3 | 1.4 | 10.5 | 1.1 | 10.5 | 1.3 | 15.5 | 1.4 | 18.1 | 1.6 | 14.3 | 1.0 | 11.2 | 1.0 |
| Anxiety disorders | ||||||||||||||
| Agoraphobia | 3.4 | 0.4 | 1.4 | 0.3 | 2.5 | 0.4 | 2.5 | 0.4 | 2.0 | 0.5 | 2.4 | 0.2 | 2.4c | 0.2 |
| Generalized Anxiety Disorder | 3.0 | 0.6 | 1.5 | 0.3 | 1.0 | 0.3 | 2.8 | 0.6 | 3.0 | 0.5 | 2.2 | 0.3 | 0.9 | 0.2 |
| Social phobia | 11.2 | 0.7 | 7.0 | 0.5 | 7.7 | 0.6 | 9.7 | 0.7 | 10.1 | 1.0 | 9.1 | 0.4 | 1.3 | 0.2 |
| Specific phobia | 22.1 | 1.1 | 16.7 | 0.9 | 21.6 | 1.6 | 18.3 | 1.0 | 17.7 | 1.3 | 19.3 | 0.8 | 0.6 | 0.1 |
| Panic disorder | 2.6 | 0.3 | 2.0 | 0.3 | 1.8 | 0.4 | 2.3 | 0.3 | 3.3 | 0.7 | 2.3 | 0.2 | 2.3c | 0.2 |
| Post-traumatic stress disorder | 8.0 | 0.7 | 2.3 | 0.4 | 3.7 | 0.5 | 5.1 | 0.5 | 7.0 | 0.8 | 5.0 | 0.3 | 1.5 | 0.2 |
| Separation Anxiety disorder | 9.0 | 0.6 | 6.3 | 0.5 | 7.8 | 0.6 | 8.0 | 0.7 | 6.7 | 0.8 | 7.6 | 0.3 | 0.6 | 0.1 |
| Any anxiety disorder | 38.0 | 1.4 | 26.1 | 0.8 | 31.4 | 1.9 | 32.1 | 1.0 | 32.3 | 1.7 | 31.9 | 0.8 | 8.3 | 0.4 |
| Behavior disorders | ||||||||||||||
| Attention deficit hyperactivity disorder | 4.2 | 0.5 | 13.0 | 1.0 | 8.8 | 0.9 | 8.6 | 0.8 | 9.0 | 1.1 | 8.7 | 0.6 | 4.2 | 0.4 |
| Oppositional defiant disorder (ODD) | 11.3 | 0.9 | 13.9 | 1.2 | 12.0 | 1.2 | 12.6 | 1.3 | 13.6 | 1.4 | 12.6 | 0.9 | 6.5 | 0.7 |
| Conduct disorder | 5.8 | 1.1 | 7.9 | 1.2 | 4.4 | 1.2 | 7.5 | 1.2 | 9.6 | 1.3 | 6.8 | 0.9 | 2.2 | 0.4 |
| Any behavior disorder | 15.5 | 1.2 | 23.5 | 1.6 | 18.2 | 1.5 | 19.5 | 1.7 | 21.9 | 1.8 | 19.6 | 1.2 | 9.6 | 0.8 |
| Substance use disorders | ||||||||||||||
| Alcohol abuse/dependence | 5.8 | 0.5 | 7.0 | 0.6 | 1.3 | 0.3 | 6.5 | 0.6 | 14.5 | 1.2 | 6.4 | 0.4 | --- | --- |
| Drug abuse/dependence | 8.0 | 0.8 | 9.8 | 0.8 | 3.4 | 0.6 | 9.7 | 0.9 | 16.3 | 1.5 | 8.9 | 0.7 | --- | --- |
| Any substance use disorder | 10.2 | 0.9 | 12.5 | 0.8 | 3.7 | 0.6 | 12.2 | 0.9 | 22.3 | 1.6 | 11.4 | 0.7 | --- | --- |
| Other | ||||||||||||||
| Eating disorders | 3.8 | 0.4 | 1.5 | 0.3 | 2.4 | 0.4 | 2.8 | 0.3 | 3.0 | 0.4 | 2.7 | 0.2 | --- | --- |
| Any Classb | 51.0 | 1.4 | 48.1 | 1.6 | 45.3 | 2.1 | 49.3 | 1.9 | 56.7 | 2.7 | 49.5 | 1.2 | 22.2 d | 1.0 |
| 1 class | 30.3 | 1.3 | 30.3 | 1.3 | 31.2 | 1.8 | 29.4 | 1.4 | 30.4 | 2.3 | 30.3 | 0.9 | 16.2 | 0.6 |
| 2 classes | 12.6 | 0.9 | 12.1 | 1.2 | 9.2 | 1.0 | 13.0 | 1.3 | 16.5 | 1.7 | 12.4 | 0.9 | 5.2 | 0.7 |
| 3–4 classes | 8.1 | 1.1 | 5.7 | 0.6 | 5.0 | 1.1 | 6.9 | 0.9 | 9.9 | 1.3 | 6.9 | 0.7 | 0.8 | 0.2 |
Note:
Anxiety, eating, and substance use disorder diagnoses are based on child interview; mood, behavioral disorders and disorder classes are based on child interview and parent report;
excludes eating disorders;
rates are identical to total prevalence due to absence of inclusion of assessment of impairment
excluding substance use disorders; [with substance use disorders: Any class = 27.6 (1.0); 1 class = 18.1 (0.7); 2 classes = 6.7 (0.5); 3–4 classes = 2.9 (0.6)]
Nearly one in three adolescents (31.9%) met criteria for an anxiety disorder, with rates for individual disorders ranging from 2.2% for GAD to 19.3% for specific phobia. All anxiety disorder subtypes were more frequent in females (the greatest sex difference being observed for PTSD). The aggregate category of any anxiety disorder was stable across age groups, but considerable variance was observed by disorder subtype. In particular, the prevalence of PTSD, panic disorder, social phobia and GAD showed modest but consistent increases with age. Severe anxiety disorders were present in 8.3% of the total sample, representing all individuals with panic disorder or agoraphobia, a moderate proportion of individuals with GAD (54.5%) or PTSD (30%), and only a small proportion of individuals with social phobia (14.3%), SAD (7.9%) and specific phobia (3.1%); yielding prevalence rates of 1.3% for social phobia, and 0.6% for SAD and specific phobia, respectively.
The prevalence of ADHD was 8.7%, with three times as many males being affected by this condition as females. The prevalence of severe ADHD was 4.2%, or approximately half of all cases in the sample. ODD was present in 12.6% of the sample (6.5% for severe cases) and 6.8% met criteria for CD (2.2% for severe cases). Although the rates of ADHD and ODD remained relatively stable by age group, rates of CD increased to a peak of 9.6% among the oldest adolescents.
Substance use disorders were present in 11.4% of the sample, corresponding to 8.9% of adolescents with drug abuse/dependence and 6.4% with alcohol abuse/dependence. These disorders were somewhat more frequent in males, and a five to eleven-fold increase in prevalence was observed across increasing age groups. The rates for severe substance use disorders were identical to those of the DSM-IV disorders because impairment criteria were embedded in the diagnostic definitions for these disorders. Concerning other conditions, 2.7% of adolescents had manifested eating disorders at some point in their lifetime. These disorders were more than twice as prevalent among females and demonstrated modest increases with age.
Finally, 49.5% of the total sample was affected by at least one class of disorder, but less than half had disorders with severe impairment (27.6%), and only 22.2% exclusive of substance use disorders. Approximately 20% of the sample (40% of all affected individuals) also met criteria for a disorder from at least one additional class. These comorbidity rates were similar for males and females. No age differences were observed for adolescents affected by one class of disorder, but comorbidity with additional classes strongly increased with age.
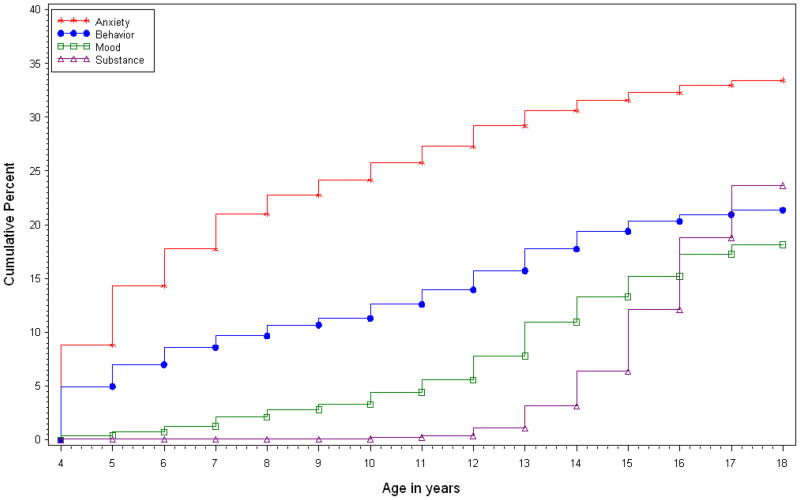
Figure 1 presents the age-specific incidence curves for each of the broad classes of lifetime mental disorder. Anxiety disorders occurred earliest with a steep slope beginning in early childhood, and leveling off after age 12. Risk was fairly low for mood and behavior disorders until early adolescence when it began to rise steadily. Substance use disorders appeared to have the latest age of onset with a steep increase in incidence after age 15. The estimated risk at age 18 was 17.6% for behavior disorders, 18.2% for mood disorders, 23.8% for substance use disorders, and 26.2% for anxiety disorders. The median age of disorder onset was 6 for anxiety disorders, 11 for behavior disorders, 13 for mood disorders, and 15 for substance use disorders (data not shown).
Figure 1.
Cumulative Lifetime Prevalence of Major Classes of DSM-IV Disorders Among Adolescents (N=10,123)
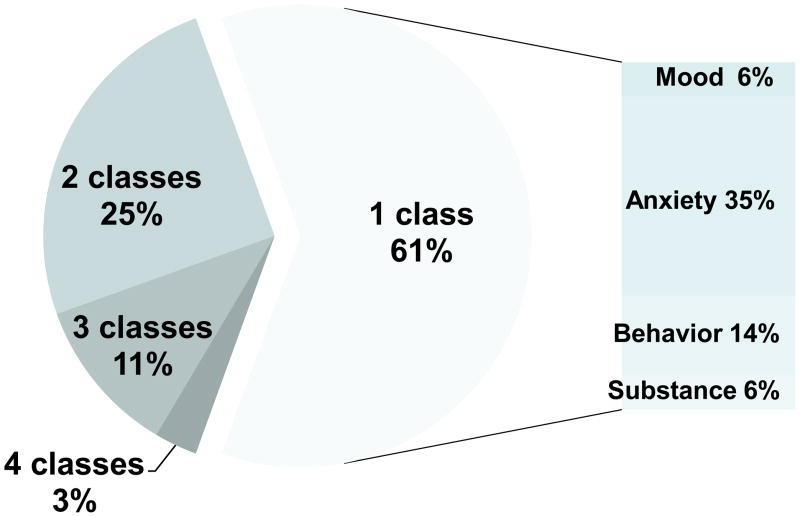
Figure 2 displays the proportion of adolescents affected by one or more broad classes of disorder among those with at least one DSM-IV disorder. A small majority of affected adolescents (61%) met criteria for disorders from one class only, with anxiety disorders being the most frequent condition to occur alone (35%) and smaller proportions having only behavior (14%), mood disorders (6%), or substance use disorders (6%). About one-quarter (25%) of adolescents affected by at least one class of disorder also met criteria for a disorder from one additional class, 11.0% were affected by three classes of disorders and 3% were affected by four classes of disorder.
Figure 2.
Distribution of the Major Classes of DSM-IV Disorders Among Adolescents with at Least One Disorder (N=5,163)
Socio-demographic Correlates
Table 3 presents the results of multivariate analyses of the association between individual and familial sociodemographic characteristics on classes of lifetime mental disorders in the adolescents. Mood and anxiety disorders were more prevalent among females in these multivariate analyses, whereas males had higher rates of behavior and substance use disorders. Rates of mood and substance use disorders were higher among older adolescents. There were few racial/ethnic differences in the major classes of mental disorders, with the exception of increased rates of anxiety disorders and lower rates of substance use disorder among non-Hispanic Black adolescents compared to non-Hispanic White adolescents, and higher rates of mood disorders among Hispanic adolescents compared to non-Hispanic Whites.
Table 3.
Multivariate Demographic Correlates of Lifetime Prevalence of DSM-IV Disorders in the National Comorbidity Survey-Adolescent Supplement (NCS-A)
| Correlates | Category | Mood | Anxiety | Behavior | Substance | Any class |
|---|---|---|---|---|---|---|
| OR (95% CI)a | ||||||
| SEX | Female | Reference | ||||
| Male | 0.5 (0.4–0.7) | 0.6 (0.5–0.7) | 1.7 (1.4–2.1) | 1.3 (1.1–1.6) | 0.9 (0.8–1.1) | |
| X21 [p] | 27.51 [0.000] | 50.65 [0.000] | 24.84 [0.000] | 8.38 [0.004] | 1.80 [0.179] | |
| AGE | 13–14 yr | Reference | ||||
| 15–16 yr | 1.5 (1.2–2.0) | 1.0 (0.8–1.3) | 1.2 (0.9–1.5) | 3.6 (2.5–5.2) | 1.2 (1.0–1.5) | |
| 17–18 yr | 1.8 (1.3–2.6) | 1.0 (0.8–1.3) | 1.3 (1.0–1.7) | 7.2 (5.1–10.1) | 1.6 (1.2–2.1) | |
| X22 [p] | 14.16 [0.001] | 0.12 [0.943] | 3.13 [0.209] | 163.68 [0.000] | 13.20 [0.001] | |
| RACE/ETHNICITY | Hispanic | 1.4 (1.1–1.8) | 1.1 (0.9–1.3) | 1.2 (0.8–1.9) | 1.0 (0.7–1.4) | 1.3 (0.9–1.9) |
| Non-Hispanic Black | 1.1 (0.8–1.5) | 1.3 (1.0–1.5) | 1.0 (0.7–1.5) | 0.4 (0.3–0.5) | 1.1 (0.8–1.5) | |
| Other | 1.3 (0.8–2.2) | 1.1 (0.8–1.4) | 0.8 (0.5–1.3) | 0.8 (0.5–1.2) | 1.2 (0.8–1.8) | |
| Non-Hispanic White | Reference | |||||
| X23 [p] | 12.00 [0.007] | 6.11 [0.106] | 2.54 [0.468] | 58.69 [0.000] | 2.58 [0.462] | |
| PARENT EDUCATION | < HS | 0.9 (0.7–1.3) | 1.3 (1.0–1.8) | 1.7 (1.1–2.7) | 1.5 (1.0–2.1) | 1.6 (1.0–2.4) |
| HS | 1.1 (0.8–1.7) | 1.3 (1.1–1.5) | 1.5 (1.1–2.1) | 1.4 (1.1–2.0) | 1.3 (1.0–1.7) | |
| Some college | 1.5 (1.1–2.2) | 1.3 (1.1–1.6) | 1.8 (1.4–2.4) | 1.6 (1.2–2.1) | 1.6 (1.3–1.9) | |
| College grad | Reference | |||||
| X23 [p] | 10.29 [0.016] | 12.92 [0.005] | 20.08 [0.000] | 11.80 [0.008] | 19.71 [0.000] | |
| PARENT MARITAL STATUSb | Currently married | Reference | ||||
| Previously married | 1.2 (0.9–1.7) | 1.3 (1.1–1.6) | 1.6 (1.1–2.2) | 1.8 (1.3–2.6) | 1.4 (1.1–1.8) | |
| Never married | 0.4 (0.2–0.8) | 1.0 (0.7–1.5) | 0.9 (0.5–1.5) | 1.2 (0.5–2.5) | 0.9 (0.6–1.4) | |
| X23 [p] | 11.23 [0.011] | 8.75 [0.033] | 8.74 [0.033] | 10.77 [0.013] | 11.93 [0.008] | |
| POVERTY INDEX | PIR ≤ 1.5 poor | 0.8 (0.5–1.3) | 1.1 (0.9–1.4) | 0.9 (0.6–1.3) | 0.7 (0.5–1.1) | 1.1 (0.8–1.6) |
| PIR ≤ 3 | 0.9 (0.7–1.3) | 1.2 (1.0–1.5) | 1.2 (0.9–1.7) | 0.9 (0.6–1.3) | 1.2 (1.0–1.5) | |
| PIR ≤ 6 | 1.0 (0.8–1.3) | 1.2 (1.0–1.4) | 0.9 (0.7–1.2) | 1.0 (0.8–1.4) | 1.1 (0.9–1.3) | |
| PIR > 6 | Reference | |||||
| X23 [p] | 1.27 [0.737] | 3.73 [0.292] | 6.49 [0.090] | 5.38 [0.146] | 3.03 [0.387] | |
| URBANICITY | Metro | 1.2 (0.7–2.0) | 1.2 (1.0–1.5) | 1.2 (0.9–1.7) | 1.3 (0.9–1.9) | 1.2 (0.9–1.5) |
| Other urban | 0.9 (0.6–1.5) | 1.2 (1.0–1.5) | 1.1 (0.8–1.5) | 1.0 (0.7–1.5) | 1.0 (0.7–1.4) | |
| Rural | Reference | |||||
| X22 [p] | 2.21 [0.331] | 5.43 [0.066] | 2.01 [0.366] | 5.28 [0.071] | 3.00 [0.223] | |
Note: HS = High school; PIR = Poverty Index Ratio.
Anxiety, eating, and substance use disorder diagnoses are based on child interview; mood, behavioral disorders and disorder classes are based on child interview and parent report;
excludes eating disorders;
rates are identical to total prevalence due to absence of continuous severity or impairment assessment
With respect to parental characteristics, the prevalence rates of anxiety disorders, substance use disorders and behavior disorders were higher for respondents whose parents were divorced or separated relative to respondents of currently married or cohabitating parents. Rates of mood disorders were lower among children of parents who were never married compared to currently married or cohabitating parents. Parental poverty level and urbanicity were not associated with any of the classes of mental disorder. However, the most consistent association between parental characteristics and mental disorders in children emerged for parental education. Adolescents whose parents were not college graduates were at increased risk for all disorder classes.
The findings from multivariate analyses for these sociodemographic characteristics and classes of severe mental disorders (results not shown, but available upon request) were highly similar to those of all mental disorders, with limited exceptions. In particular, anxiety disorders were more prevalent in older adolescents, among ‘other’ ethnic minorities, among adolescents whose parents were not college graduates, and among adolescents whose parents were divorced or separated.
Two-way interactions for any significant main effects were tested for each class of disorder. After adjusting for family-wise experimental errors with a Bonferroni correction, no interactions were observed between individual and parental demographic correlates and anxiety or behavior disorders. There were four significant interactions for other disorders: (1) the prevalence of mood disorders was higher in White adolescents in homes with higher levels of parental education than that in Blacks and Hispanics; (2) rates of substance use disorders increased more dramatically with age for males than females; (3) sex differences in substance use disorders were largest for Blacks compared to other ethnic groups; and (4) increased rates of substance use disorders were observed among Hispanic adolescents whose parents were divorced, however, rates were decreased among Blacks whose parents were never married or divorced.
Discussion
These findings provide the first lifetime prevalence data on a broad range of mental disorders in a nationally representative sample of U.S. adolescents. The prevalence rates reported here closely approximate those of our nationally representative sample of adults using nearly identical methods, suggesting that the majority of mental disorders in adults emerge prior to adulthood. These rates are somewhat higher than those of prior studies, but within the ranges of estimates summarized in a meta-analysis of international community surveys of mental disorders in youth.1 In addition, the NCS-A provides a more comprehensive assessment of a wide range of DSM-IV disorders and subtypes than most previous studies. Despite the high prevalence rates, however, only about one in every four-to-five youths meet criteria for a lifetime mental disorder that is associated with severe role impairment and/or distress. The prevalence of severe emotional and behavior disorders is even higher than the most frequent major physical conditions in adolescence, including asthma24 or diabetes25 which have received widespread public health attention.
The finding that only about half of youth with a lifetime DSM-IV disorder report severe impairment confirms previous research demonstrating that a smaller proportion of youth with mental disorders actually have sufficiently severe distress or impairment to warrant immediate intervention.9 According to prior research, about one out of every ten youths with a current mental disorder fulfill criteria for Serious Emotional Disorder (SED) based on the Substance Abuse and Mental Health Services Administration (SAMSHA) definition (e.g., a mental health problem that has a drastic impact on a child’s ability to function socially, academically, and emotionally). 9,26 While our study did not strictly assess all of the criteria for SED, our estimates of severe disorders were based on the full diagnostic criteria for DSM-IV disorders accompanied by severe impairment in major life roles.
Our data document the early onset of major classes of mental disorders. Among affected adolescents, 50% of disorders had their onset by age 6 for anxiety disorders, by age 11 for behavior disorders, by age 13 for mood disorders and by age 15 for substance use disorders. These findings closely approximate those of prospective studies of child and adolescent samples that have documented the incidence and progression of childhood mental disorders.2, 27–29 The early age of onset of anxiety has been well-established and our findings on specific subtypes of anxiety closely track those of prospective community-based research that reveal differential peak periods of onset of specific subtypes of anxiety. 29–31 Prospective studies have also shown that the average age of onset of major depression and dysthymia is between 11 and 14 years,6 with a steady increase in incidence across adolescence that continues through early adulthood. Our cross-sectional data reflect this increase with a near doubling of rates from 13–14 years (8.4%) to 17–18 years (15.4%). Also consistent with prior cross-sectional and prospective research, the median onset of behavior disorders is slightly earlier than that of mood disorders, with a later peak for conduct disorder than for oppositional defiant disorder. 32 Finally, the later onset and steeper increase in rates of substance use disorders across adolescence has been repeatedly demonstrated, despite different prevalence periods and assessment methods. 33
About 40% of affected youth in the NCS-A reported more than one class of lifetime disorder, with mood disorders being the most likely to co-occur with other classes. Non-random patterns of comorbidity between discrete classes of mental disorders have been documented extensively in prior community samples of youth.34–36 Future analyses of these data will investigate specific concurrent and prospective comorbidity patterns as well as their sociodemographic and clinical correlates.
In addition to providing prevalence estimates, the findings also confirm observations from previous U.S. and international investigations of adolescents concerning the association of sociodemographic characteristics and mental disorders.1 In particular, female adolescents were more likely than males to have mood and anxiety disorders, but less likely to have behavioral and substance use disorders. Non-Hispanic Blacks were less likely to have substance use disorders compared to Whites, a finding that is similar to prior community studies of adolescents and adults.37 The increased prevalence of mood and substance use disorders in older adolescents has also been observed in previous investigations,38 thus indicating the importance of prevention strategies for early and mid-adolescence. By contrast, the stability of certain anxiety and behavioral disorders across this same developmental period suggests that earlier interventions before puberty may be appropriate for many of these conditions.
The strong links between adolescent mental disorders and parental characteristics indicate the importance of the family context in the development of mental disorders. Our finding of a prominent effect of parental education on mental disorders has been well-documented for both child physical and mental health outcomes.39, 40 Divorce was often associated with mental disorders in youth, particularly anxiety, behavior and substance use disorders. The mechanisms underlying the impact of non-intact homes on mental disorders in youth, including both biologic or genetic vulnerability, and indirect influences on disruptions in the home environment, warrant further study.9, 41, 42 However, the significant interactions observed among several sociodemographic characteristics attest to the complexity of these associations. For example, increased rates of substance use disorders among Hispanic adolescents whose parents were divorced may reflect interactions of individual, familial and broader environmental influences that should be considered simultaneously in modeling the nature of risk and resilience in adolescent mental disorders.43, 44 The lack of strong effects for some sociodemographic characteristics, such as poverty, may also be attributable to the multivariate statistical approach that adjusted for confounded variables.
The present findings should be interpreted in the context of several study-specific limitations. First, the cross-sectional nature of the survey limits our ability to document temporal ordering of mental disorders and putative risk and protective factors. Second, assessment of lifetime disorders is based on retrospective recall that is subject to numerous types of bias. Although we employed a number of methods to increase the validity of retrospective reports of age of onset,21 it is unlikely that we were able to completely correct for recall biases. A third limitation is that surrogate information was obtained only from one parent using a self-administered questionnaire rather than a direct interview, and only for a limited number of disorders assessed in the survey. The lack of prior evidence for integrating parent and child reports based on different modes of administration led us to apply an empirical approach based on previous research on cross-informant diagnostic estimates.23 In addition to study-specific limitations, a critical view is warranted concerning current diagnostic nomenclature more generally. Adolescence is a period of change and maturation in which emotional and behavioral difficulties may be common, and it is difficult to establish universally acceptable definitions of disorder or severity thresholds. The high comorbidity across classes of disorders also raises questions regarding the permeability of diagnostic categories and the plasticity of adolescent development. The pertinence of current and alternative developmentally-appropriate diagnostic criteria for adolescent mental disorders deserves careful attention and would benefit from continued debate.
Despite these limitations, our findings document the high prevalence of mental disorders in youth, and specify that just over one in four-to-five adolescents in the general population suffers from disorders that result in severe impairment. Considered with recent estimates indicating that the annual economic burden of mental disorders on the well-being of American youth and their families approaches a quarter of one trillion dollars45, these findings underscore the key public health importance of mental health in American youth. The present data can inform and guide the development of priorities for future research and health policy by providing previously lacking prevalence estimates in a nationally representative sample of U.S. adolescents, as well as the individual, familial and environmental correlates of mental disorders. Prospective research is now needed to understand the risk factors for mental disorder onset in adolescence, as well as the predictors of the continuity of these disorders into adulthood.
Acknowledgments
The National Comorbidity Survey Adolescent Supplement (NCS-A) and the larger program of related NCS surveys are supported by the National Institute of Mental Health (U01-MH60220) and the National Institute of Drug Abuse (R01 DA016558) with supplemental support from Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust. The NCS-A was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative.
This work was supported by the Intramural Research Program of the National Institute of Mental Health. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or U.S. Government.
Footnotes
Disclosure: Drs. Merikangas, Burstein, Avenevoli, Benjet, Georgiades, and Swendsen, and Ms. He, Ms. Swanson, and Ms. Cui report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Kathleen Ries Merikangas, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health.
Ms. Jian-ping He, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health
Dr. Marcy Burstein, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health
Ms. Sonja A. Swanson, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health
Dr. Shelli Avenevoli, Division of Developmental Translational Research, National Institute of Mental Health
Ms. Lihong Cui, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health
Dr. Corina Benjet, National Institute of Psychiatry Ramón de la Fuente, Mexico
Dr. Katholiki Georgiades, McMaster University
Dr. Joel Swendsen, National Scientific Research Center (CNRS), Bordeaux, France
References
- 1.Costello E, Mustillo S, Keeler G, Angold A. Prevalence of psychiatric disorders in childhood and adolescence. In: Levin B, Petrila J, hennessy K, editors. Mental Health Services: A Public Health Perspective. Oxford: 2004. pp. 111–128. [Google Scholar]
- 2.Cohen P, Cohen J, Kasen S, et al. An epidemiological study of disorders in late childhood and adolescence--I. Age- and gender-specific prevalence. J Child Psychol Psychiatry 1993. 1993 Sep;34(6):851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- 3.Reinherz HZ, Giaconia RM, Lefkowitz ES, Pakiz B, Frost A. Prevalence of psychiatric disorders in a community population of older adolescents. J Am Acad Child Adolesc Psychiatry. 1993;32(2):369–377. doi: 10.1097/00004583-199303000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Costello J, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youths: Goals, design, methods, and the prevalence of DSM-III-R Disorders. Arch Gen Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 5.Lahey BB, Flagg EW, Bird HR, et al. The NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study: background and methodology. J Am Acad Child Adolesc Psychiatry. 1996 Jul;35(7):855–864. doi: 10.1097/00004583-199607000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clin Psychol Rev. 1998;18(7):765–794. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- 7.Canino G, Shrout PE, Rubio-Stipec M, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry. 2004 Jan;61(1):85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- 8.Roberts RE, Roberts CR, Xing Y. Rates of DSM-IV psychiatric disorders among adolescents in a large metropolitan area. J Psychiatr Res. 2007 Dec;41(11):959–967. doi: 10.1016/j.jpsychires.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brauner CB, Stephens CB. Estimating the prevalence of early childhood serious emotional/behavioral disorders: challenges and recommendations. Public Health Rep. 2006 May–Jun;121(3):303–310. doi: 10.1177/003335490612100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005 Oct;44(10):972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 11.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010 Jan;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: Substance Abuse and Mental Health Services Administration: Center for Mental Health Services; 1999. [Google Scholar]
- 13. [Accessed September 1, 2007.];An NIMH Oversight Board report to the National Advisory Mental Health Council. 1998 http://www.nimh.nih.gov/research/unoccap.htm.
- 14.Bourdon KH, Goodman R, Rae DS, Simpson G, Koretz DS. The Strengths and Difficulties Questionnaire: U.S. normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry. 2005 Jun;44(6):557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- 15.Shaffer D, Fisher P, Dulcan MK, Davies M. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. J Am Acad Child Adolesc Psychiatry. 1996;35(7):865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Merikangas K, Avenevoli S, Costello J, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009 Apr;48(4):367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kessler RC, Avenevoli S, Costello EJ, et al. National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry. 2009 Apr;48(4):380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Avenevoli S, Green J, et al. National comorbidity survey replication adolescent supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry. 2009 Apr;48(4):386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler RC, Avenevoli S, Costello EJ, et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009 Jun;18(2):69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13(2):60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. J Am Acad Child Adolesc Psychiatry. 1997 May;36(5):610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Grills AE, Ollendick TH. Issues in parent-child agreement: the case of structured diagnostic interviews. Clin Child Fam Psychol Rev. 2002 Mar;5(1):57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- 24.Akinbami LJ, Schoendorf KC, Parker J. US childhood asthma prevalence estimates: the Impact of the 1997 National Health Interview Survey redesign. Am J Epidemiol. 2003 Jul 15;158(2):99–104. doi: 10.1093/aje/kwg109. [DOI] [PubMed] [Google Scholar]
- 25.CDC. [Accessed January 25, 2010.];National Diabetes Fact Sheet. 2007 http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf.
- 26.Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: Substance Abuse and Mental Health Services Administration: Center for Mental Health Services; 1999. [Google Scholar]
- 27.McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. J Am Acad Child Adolesc Psychiatry. 1992 Jan;31(1):50–59. doi: 10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent Psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993;102(1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 29.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003 Jul;60(7):709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 30.Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- 31.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2005 Oct;14(4):631–648. vii. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 32.Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry. 2000 Dec;39(12):1468–1484. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: effects of timing and sex. J Clin Child Psychol. 1999 Sep;28(3):298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- 34.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999 Jan;40(1):57–87. [PubMed] [Google Scholar]
- 35.Brady EU, Kendall PC. Comorbidity of anxiety and depression in children and adolescents. Psychol Bull. 1992 Mar;111(2):244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- 36.Caron C, Rutter M. Comorbidity in child psychopathology: concepts, issues and research strategies. J Child Psychol Psychiatry. 1991 Nov;32(7):1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- 37.Kandel D, Single E, Kessler RC. The epidemiology of drug use among New York State high school students: Distribution, trends, and change in rates of use. Am J Public Health. 1976 Jan;66(1):43–53. doi: 10.2105/ajph.66.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cochrane SH, Leslie J, O’Hara DJ. Parental education and child health: intracountry evidence. Health Policy Educ. 1982 Mar;2(3–4):213–250. doi: 10.1016/0165-2281(82)90011-x. [DOI] [PubMed] [Google Scholar]
- 40.Velez C, Johnson J, Cohen P. A longitudinal analysis of selected risk factors for childhood psychopathology. J Am Acad Child Adolesc Psychiatry. 1989;28:861–864. doi: 10.1097/00004583-198911000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Shanahan L, Copeland W, Costello EJ, Angold A. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. J Child Psychol Psychiatry. 2008 Jan;49(1):34–42. doi: 10.1111/j.1469-7610.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- 42.Fergusson DM, Horwood LJ. The Christchurch Health and Development Study: review of findings on child and adolescent mental health. Aust N Z J Psychiatry. 2001 Jun;35(3):287–296. doi: 10.1046/j.1440-1614.2001.00902.x. [DOI] [PubMed] [Google Scholar]
- 43.Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Dev Psychol. 2003 Mar;39(2):349–371. doi: 10.1037//0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kumpfer KL, Summerhays JF. Prevention approaches to enhance resilience among high-risk youth: comments on the papers of Dishion & Connell and Greenberg. Ann N Y Acad Sci. 2006 Dec;1094:151–163. doi: 10.1196/annals.1376.014. [DOI] [PubMed] [Google Scholar]
- 45.O’Connell ME, Boat T, Warner K. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, D.C: The National Academies Press; 2009. [PubMed] [Google Scholar]