Abstract
Objectives
To assess how reductions in length of stay associated with hospitalist care vary by patient and hospital characteristics and explore whether these reductions in length of stay changed over time in the Medicare population.
Design
Retrospective cohort study using data from a 5% national sample of Medicare beneficiaries.
Setting
Hospital.
Participants
To examine temporal trends, 1,981,654 Medicare admissions in 2001 to 2006 at 5036 U.S. hospitals were used. To examine the influence of patient and hospital characteristics, 314,590 admissions in 2006 were used.
Measurements
Hospital length of stay.
Results
In multivariable analyses controlling for patient and hospital characteristics, the reductions in length of stay associated with hospitalist care increased from 0.02 days in 2001-02 to 0.22 days in 2003-04, and 0.35 days in 2005-06. For 2006 admissions, reductions in length of stay were greater in older patients and patients with a higher DRG weight. The reductions were three times greater for medical than for surgical DRGs, with greater reductions in length of stay at non-profit vs. for profit hospitals, and at community vs. teaching hospitals.
Conclusion
The reductions in length of stay associated with hospitalist care would appear to be greatest in older, complicated, non-surgical patients cared for at community hospitals.
Keywords: Hospitalist, Length of Stay, Medicare
INTRODUCTION
In the U.S. the growth of hospitalists started in the 1990s, coincident with the shift to managed care and pressures to reduce costs (1-4). Prospective trials and observational or quasi experimental studies have compared hospitalists to non-hospitalists in caring for general medical admissions (1-2, 5-12). Almost all of these studies found that patients cared for by hospitalists experienced a modest decrease in hospital length of stay. It is not yet clear what effect this shift in care delivery will have on the care of the elderly population. The elderly tend to have multiple hospitalizations and longer lengths of stay due to their complex disease status and multiple comorbidities. This poses substantial challenges and opportunities for hospitalists (13-14).
Almost all prior studies of hospitalist care were from single institutions, and from academic hospitals. Because of that, there is little information on whether the impact of hospitalists varies by type of hospital. For example, academic hospitals are typically less efficient because of the presence of trainees (15-16). One might posit that hospitalists would have a greater impact in academic than in community hospitals. Lindenauer et al. (12) recently studied patients cared for by hospitalists and non-hospitalists at 45 hospitals, and reported little variation in the effect of hospitalists on length of stay. Specifically, they found no variation by teaching status of the hospital in the differences in length of stay of patients cared for by hospitalists vs. non-hospitalist general internists or family physicians.
In addition, very little investigation has focused on how the impact of hospitalists might vary by patient characteristics, such as advanced age and higher number of comorbidities (17). Also, hospitalists initially were utilized in the care of general medical patients, but have increasingly been involved in co-management of surgical patients (4, 18). Is the impact on length of stay similar in both groups?
Finally, no information exists on whether the impact of hospitalists on length of stay has been maintained over time. It is possible that the physicians who participated in the early trials of hospitalist care were enthusiasts, motivated to show that this model was superior. Such bias, if present, should diminish over time.
In this report we examine the effect of hospitalists on length of stay in Medicare patients hospitalized at 5036 U.S. hospitals from 2001 to 2006. The availability of the national Medicare data allows us to examine the influence of time, and patient and hospital characteristics on the effect of hospitalists on length of stay. We hypothesized that reductions in length of stay associated with care by hospitalists would be greater in more complex cases, greater in teaching than in non-teaching hospitals, and that differences in length of stay between patients cared for by hospitalists vs. non-hospitalists would decrease over time.
METHODS
Source of Data
Claims from the period 2001 to 2006 from a 5% national sample of Medicare beneficiaries were used. We used Medicare enrollment files, Medicare Provider Analysis and Review (MEDPAR) files, Outpatient Statistical Analysis File (OUTSAF), Medicare Carrier files, Provider of Services (POS) file, and DRG weight files.
Establishment of the Study Cohort
All 3,811,864 hospital admissions from 2001 to 2006 in MEDPAR were selected. Because our study focused on hospitalist care, and >95% hospitalists treating adult patients are generalist physicians (19), admissions not involving an Evaluation and Management (E&M) charge by a general internist, family physician, general practitioner or geriatrician were excluded (n=1,628,912). Also excluded were 10,158 admissions which could not be linked to the POS file and 191,140 admissions in which patients received care from both hospitalists and non-hospitalists, leaving 1,981,654 admissions in 2001-2006.
Analyses examining the influence of hospital and patient characteristics on reductions in length of stay associated with hospitalist care were limited to 2006 data, the most recent year available. For those analyses, beneficiaries enrolled in HMOs or without both Medicare Parts A and B for the entire 12 months prior to the admission (n=22,899) were excluded. Also excluded were 5,986 admissions which could not be linked to the DRG weight file. This left 91,065 admissions cared for by hospitalists and 223,525 admissions cared for by non-hospitalists in 2006.
Measures
Medicare enrollment files were used to categorize patients by age, gender and ethnicity (White, Black, other). A Medicaid indication in the enrollment file was used as a proxy for low socioeconomic status. Information regarding origin of admission (emergency department vs. other), weekend vs. weekday admission, admission with intensive care unit (ICU) stay and discharge diagnosis-related group (DRG) were obtained from the Medicare Provider Analysis and Review (MEDPAR) files. DRG weight reflects the average amount of resource utilization for each DRG. Residence in a nursing facility prior to admission, and discharge to home or to another health care facility was obtained from the MEDPAR files, as well as by searching for any evaluation and management codes associated with nursing facilities (20) in the 3 months prior to admission. Elixhauser comorbidity measures (21) were generated using both inpatient and physician claims from MEDPAR, Outpatient Statistical Analysis File (OUTSAF), and Carrier files. Total number of hospitalizations and total number of outpatient visits in the year prior to the index hospitalization were generated from MEDPAR and Carrier files.
Hospital information — zip code, county, state, total number of hospital beds, type of hospital and medical school affiliation — were obtained from the POS file. Metropolitan size was generated from 2000 Census data. Both metropolitan size and total number of hospital beds were categorized by quartiles; states were grouped by census region; type of hospital was categorized as non-profit, for profit or public; and medical school affiliation was categorized as none, minor or major.
Hospitalists were identified as generalist physicians who had at least five Medicare Evaluation and Management claims and generated ≥ 90% of these claims from care provided to hospitalized patients in the years studied. This definition was shown to have 84.2% sensitivity and 96.5% specificity when validated at seven hospitals (4).
Study Outcome
Our study outcome was hospital length of stay, obtained from MEDPAR files.
Statistical Analyses
The relationship of hospitalist care to length of stay was evaluated using generalized estimating equations (GEE) with log link normal distribution. These models accounted for the clustering of patients within hospitals and controlled for both hospital characteristics (region, metropolitan size, total number of beds, type of hospital and teaching affiliation) and patient characteristics (age, gender, race, socioeconomic status, DRG group, ER admission, admission with ICU stay, weekend admission, comorbidity, DRG weight and total number of hospitalizations and provider visits in the 12 months before the index admission). The interactions between hospitalist care and hospital/patient characteristics on length of stay were tested. To reduce skew and account for outliers, we repeated our analyses, excluding admissions in which length of stay was > 3 standard deviations above the mean. To remove the cluster effect within patients, analyses were repeated to include only the first admission in a year for each patient.
We assessed the association between decrease in length of stay associated with hospitalist care and overall length of stay by linear regression using the top 25 medical and 15 surgical DRGs, which accounted for 57.5% of all admissions. All tests of statistical significance were 2-sided. Bonferonni corrected p-values and 95% confidence intervals corresponding to corrected p-values were reported to account for multiple comparisons. Analyses were performed with SAS version 9.1 (SAS Inc., Cary, NC).
Selection Bias: In preliminary analyses we found that patients cared for by hospitalists were less likely to have an identified primary care physician (PCP) prior to admission (22). Patients with an established PCP differ from those without, in that they are younger and have fewer comorbidities. Therefore, in order to reduce the baseline differences between the cohorts of patients receiving hospitalist care vs. non-hospitalist care, we repeated all analyses restricting the cohort to patients with an identified PCP.
Additionally, propensity score analyses were conducted (23, 24) for admissions cared for by hospitalists and non-hospitalists in 2006. The propensity that an admission would be cared for by a hospitalist was generated from a logistic regression model that incorporated the potential confounders listed in Table 1. We grouped the admissions into 5 strata representing quintiles of the propensity score. The Cochran-Mantel-Haenszel Chi-square was used to determine whether the covariance was balanced after adjusting for propensity quintiles. Covariates that retained a significant difference between patients cared for by hospitalists and non-hospitalists were age (p=0.005), the comorbidities of alcohol use (p=0.040) and drug abuse (p=0.008), the number of provider visits in the 12 months before admission (p=0.013), ER admission (p<0.001), hospital size (p<0.001), hospital medical school affiliation (p<0.001) and metropolitan size (p<0.001). These variables were adjusted together with the propensity score in the GEE models. The association between hospitalist care and length of stay within each quintile of propensity were reported.
Table 1.
Hospital and patient characteristics* stratified by whether hospitalized Medicare patients were cared for by hospitalists or non-hospitalists in 4359 hospitals in 2006.
| Characteristics | Non-hospitalist | Hospitalist | p-value** | |
|---|---|---|---|---|
| (n = 223525) | (n = 91065) | |||
| Age | < 65 | 12.8% | 15.5% | |
| 65 - 74 | 24.9% | 24.9% | ||
| 75 - 84 | 36.6% | 35.0% | ||
| 85 + | 25.7% | 24.6% | ||
| Mean age | 76.2±12.2 | 75.3±13.0 | <0.001 | |
| Gender | Male | 40.5% | 41.9% | <0.001 |
| Female | 59.5% | 58.1% | ||
| Race/ethnicity | White | 84.3% | 82.2% | <0.001 |
| Black | 11.2% | 13.0% | ||
| Other | 4.5% | 4.9% | ||
| Low socioeconomic status | 26.2% | 28.7% | <0.001 | |
| Emergency admission | 66.5% | 72.3% | <0.001 | |
| Weekend admission | 25.6% | 25.5% | 1.000 | |
| Diagnosis related group | Surgical Orthopedic | 7.4% | 8.9% | <0.001 |
| Surgical Gastroenterology | 2.8% | 2.2% | ||
| Surgical Cardiology | 4.3% | 3.9% | ||
| Surgical Other | 4.4% | 4.6% | ||
| Medical Neurology | 5.6% | 6.7% | ||
| Medical Pulmonary | 16.3% | 15.3% | ||
| Medical Cardiology | 19.7% | 17.9% | ||
| Medical Gastroenterology | 11.1% | 10.4% | ||
| Medical Other | 28.4% | 30.2% | ||
| Diagnosis related group weight | 1.4±1.3 | 1.3±1.2 | <0.001 | |
| Elixhauser Comorbidity | Congestive heart failure | 28.5% | 26.1% | <0.001 |
| Valve disease | 12.6% | 11.9% | <0.001 | |
| Pulmonary circulation disease | 2.3% | 2.3% | 1.000 | |
| Peripheral vascular disease | 16.0% | 17.0% | <0.001 | |
| Hypertension | 71.5% | 68.8% | <0.001 | |
| Paralysis | 3.5% | 3.9% | <0.001 | |
| Neurological disorders | 12.4% | 13.5% | <0.001 | |
| Chronic pulmonary disease | 30.7% | 28.3% | <0.001 | |
| Diabetes Mellitus without complication | 34.3% | 32.8% | <0.001 | |
| Diabetes Mellitus with complication | 12.4% | 12.0% | 0.122 | |
| Hypothyroidism | 15.4% | 15.1% | 0.587 | |
| Renal failure | 14.6% | 15.0% | 0.210 | |
| Liver disease | 2.1% | 2.4% | <0.001 | |
| Peptic ulcer | 0.1% | 0.1% | 1.000 | |
| Acquired Immune Deficiency Syndrome | 0.3% | 0.5% | <0.001 | |
| Lymphoma | 1.4% | 1.3% | 1.000 | |
| Metastatic cancer | 2.4% | 2.3% | 1.000 | |
| Solid tumor w/out metastasis | 10.6% | 10.2% | 0.208 | |
| Rheumatoid arthritis | 4.8% | 4.7% | 0.999 | |
| Coagulopathy | 5.3% | 5.7% | <0.001 | |
| Obese | 5.1% | 5.2% | 0.988 | |
| Weight loss | 5.4% | 5.9% | <0.001 | |
| Fluid and electrolyte disorders | 25.4% | 26.9% | <0.001 | |
| Chronic blood loss anemia | 3.5% | 3.4% | 1.000 | |
| Deficiency Anemia’s | 29.0% | 28.3% | 0.004 | |
| Alcohol abuse | 2.2% | 2.9% | <0.001 | |
| Drug abuse | 1.6% | 2.4% | <0.001 | |
| Psychoses | 8.2% | 9.1% | <0.001 | |
| Depression | 12.8% | 13.3% | <0.001 | |
| Total number of comorbidities | 3.7± 2.8 | 3.8 ± 2.7 | <0.001 | |
| Mean number of hospitalizations in 1 year prior to studied admission | 1.8 ± 2.8 | 1.8 ± 2.6 | 1.000 | |
| Mean number of doctor visits in 1 year prior to studied admission | 16.3 ± 17.2 | 17.4 ± 16.8 | <0.001 | |
| Geographic region | Middle Atlantic | 15.0% | 11.9% | <0.001 |
| New England | 4.0% | 6.7% | ||
| East North Central | 21.2% | 15.3% | ||
| West North Central | 8.1% | 7.6% | ||
| South Atlantic | 20.1% | 24.6% | ||
| East South Central | 9.0% | 7.3% | ||
| West South Central | 11.6% | 11.0% | ||
| Mountain | 3.5% | 6.5% | ||
| Pacific | 7.4% | 9.1% | ||
| Size of metropolitan area | <100,000 | 26.7% | 19.0% | <0.001 |
| 100,000 - 249,999 | 9.9% | 8.3% | ||
| 250,000 - 999,999 | 17.7% | 18.9% | ||
| >=1,000,000 | 45.7% | 53.8% | ||
| Medical school affiliation | None | 61.7% | 54.6% | <0.001 |
| Minor | 21.5% | 22.5% | ||
| Major | 16.8% | 22.9% | ||
| Hospital Size, No. of beds | < 200 | 35.7% | 26.9% | <0.001 |
| 200 – 349 | 27.7% | 25.1% | ||
| 350 – 499 | 17.6% | 20.3% | ||
| >= 500 | 19.0% | 27.7% | ||
| Type of Hospital | Nonprofit | 73.4% | 75.9% | <0.001 |
| For profit | 11.6% | 11.1% | ||
| Public | 15.0% | 13.0% | ||
| Admission with Intensive care unit stay | No | 68.1% | 67.4% | 0.006 |
| Yes | 31.9% | 32.6% | ||
| Inpatient mortality | 3.5% | 3.6% | 1.000 | |
| PCP prior to admission*** | 63.3% | 48.3% | <0.001 | |
| Admitted from nursing facility | 11.3% | 12.8% | <0.001 | |
| Discharge to home | 61.6% | 59.1% | <0.001 | |
Race/ethnicity was self-reported during initial enrollment with Social Security Administration. Low socioeconomic status was defined as whether the beneficiary applied for eligibility and met the low income requirement for Medicaid. See “Methods” section for definition of Elixhauser comorbidity measure. Medical and Surgical diagnosis related group was based on the groupings published in our previous study (18).
p-value was from chi-square test for categorical variables and from t-test for continuous variables. A Bonferonni correction was used to account for multiple comparisons. P-values shown have been calculated by using the following formula: 1 − (1 − original p-value)50. There are a total of 50 comparisons in the table. The p-values listed as 1.000 on the table have been rounded from >0.9999.
A general practitioner, family physician, general internist, or a geriatrician who had billed an outpatient E&M code for the patient on 3 or more occasions in the 12 months before the hospitalization.
RESULTS
Table 1 provides hospital and patient characteristics stratified by whether patients received hospital care from a hospitalist or non-hospitalist in the 2006 cohort. The two groups differed by number of comorbidities, average number of doctor visit in the year before index admission, DRG weight, percentages with ER admission, ICU utilization, residence in a nursing home prior to admission, discharge location, and by hospital teaching status, hospital size, and size of the metropolitan area. Because of the very large sample size, almost all differences between the two groups were statistically significant. It is more important to focus on the magnitude of any differences rather than their level of statistical significance. Inpatient mortality was similar (3.6% vs. 3.5%) between the two groups.
Table 2 shows the differences in length of stay between patients cared for by hospitalists and those cared for by non-hospitalists for all hospital admissions and for the top 10 DRG admissions in 2006. The table presents the unadjusted mean lengths of stay for patient cared for by hospitalists vs. non-hospitalists, plus the difference in length of stay between the two groups, unadjusted and also adjusted for all the variables in Table 1. For all admissions, the adjusted average length of stay was 0.36 (95% CI: 0.26-0.46) days shorter for patients cared for by hospitalists, a reduction of 7.1%. A significantly shorter length of stay was associated with hospitalist care for nine out of the top 10 DRGs, ranging from 0.18 to 0.88 days. There were only small differences between the unadjusted and adjusted differences in length of stay.
Table 2.
Average length of stay for patients cared for by hospitalists vs. non-hospitalists, and differences in adjusted average length of stay* between the two groups for all admissions and for the top ten DRGs in 4359 hospitals in 2006.
| DRG | Non-Hospitalist | Hospitalist | Unadjusted difference (95% CI**) | Adjusted difference (95% CI**) | |
|---|---|---|---|---|---|
| All | # of admissions | 223525 | 91065 | ||
| Mean | 5.51 ± 5.27 | 5.17 ± 5.27 | 0.34 (0.28, 0.40) 0.36 | (0.26, 0.46) | |
| Median (Q1-Q3) | 4 (3 – 7) | 4 (2 – 6) | |||
| Heart Failure & Shock | # of admissions | 15177 | 5274 | ||
| Mean | 5.19 ± 3.91 | 4.53 ± 3.29 | 0.66 (0.49, 0.83) 0.60 | (0.43, 0.77) | |
| Median (Q1-Q3) | 4 (3 – 6) | 4 (2 – 6) | |||
| Simple Pneumonia & Pleurisy, age >17 W CC | # of admissions | 12741 | 4777 | ||
| Mean | 5.44 ± 3.51 | 4.66 ± 3.14 | 0.77 (0.61, 0.94) 0.74 | (0.57, 0.90) | |
| Median (Q1-Q3) | 5 (3 – 7) | 4 (3 – 6) | |||
| Chronic Obstructive Pulmonary Disease | # of admissions | 9794 | 3349 | ||
| Mean | 4.82 ± 3.29 | 4.15 ± 3.01 | 0.66 (0.48, 0.85) 0.66 | (0.46, 0.85) | |
| Median (Q1-Q3) | 4 (3 – 6) | 3 (2 – 5) | |||
| Major Joint & Limb Reattachment Procedures of Lower Extremity | # of admissions | 7322 | 3338 | ||
| Mean | 4.70 ± 2.70 | 4.62 ± 2.46 | 0.08 (-0.07, 0.24) 0.18 | (0.01, 0.35) | |
| Median (Q1-Q3) | 4 (3 – 5) | 4 (3 – 5) | |||
| Esophagitis, Gastroenteritis & Miscellaneous Digestive Disorders, age >17 W CC | # of admissions | 7871 | 2967 | ||
| Mean | 4.45 ± 3.85 | 4.10 ± 3.49 | 0.35 (0.12, 0.58) 0.41 | (0.17, 0.64) | |
| Median (Q1-Q3) | 3 (2 – 5) | 3 (2 – 5) | |||
| Intracranial Hemorrhage or Cerebral Infarction | # of admissions | 5848 | 2801 | ||
| Mean | 5.19 ± 4.01 | 4.89 ± 3.89 | 0.30 (0.04, 0.56) 0.36 | (0.07, 0.63) | |
| Median (Q1-Q3) | 4 (3 – 6) | 4 (3 – 6) | |||
| Renal Failure | # of admissions | 4809 | 2661 | ||
| Mean | 6.09 ± 4.97 | 5.29 ± 4.68 | 0.81 (0.47, 1.14) 0.76 | (0.29, 1.19) | |
| Median (Q1-Q3) | 5 (3 – 8) | 4 (3 – 7) | |||
| Kidney & Urinary Tract Infections, age >17 W CC | # of admissions | 6026 | 2567 | ||
| Mean | 4.90 ± 3.48 | 4.63 ± 4.67 | 0.27 (0.01, 0.53) 0.29 | (-0.06, 0.62) | |
| Median (Q1-Q3) | 4 (3 – 6) | 4 (3 – 5) | |||
| G.I. Hemorrhage W CC | # of admissions | 6034 | 2464 | ||
| Mean | 4.68 ± 3.5 | 4.22 ± 3.23 | 0.47 (0.23, 0.70) 0.48 | (0.23, 0.71) | |
| Median (Q1-Q3) | 4 (3 – 6) | 3 (2 – 5) | |||
| Septicemia, age >17 | # of admissions | 5029 | 2453 | ||
| Mean | 7.39 ± 6.01 | 6.62 ± 5.14 | 0.77 (0.37, 1.17) 0.88 | (0.46. 1.26) | |
| Median (Q1-Q3) | 6 (4 – 9) | 5 (3 – 8) |
Differences in length of stay are adjusted for covariates, while the average lengths of stay presented for hospitalists and non-hospitalists are unadjusted. Differences in adjusted length of stay are the antilog of mean values of length of stay for admissions cared for by hospitalists and non-hospitalists, adjusting for all covariates - age, gender, race, low socioeconomic status, Elixhauser comorbidity measures, DRG group, DRG weight, number of hospitalizations in 1 year prior to admission, number of doctor visits in 1 year prior to admission, emergency admission, weekend admission, admission with intensive care unit stay, and the cluster effect of hospital and hospital characteristics of geographic regions, metropolitans sizes, type of hospital, hospital size, and medical school affiliation.
The 95% confidence intervals were adjusted with a Bonferonni correction.
Abbreviation: DRG, diagnosis related group; LOS, length of stay; CI, confidence interval; CC, complications and comorbidites; GI, gastrointestinal.
We repeated the analyses shown in Table 2 twice: 1) restricting it to data on a maximum of one admission per patient per year, and 2) excluding admissions with lengths of stay or total charges greater than three standard deviations above the mean. These modifications had little effect on the results in Table 2. To reduce baseline differences between the hospitalist and non-hospitalist groups, we also restricted the analyses to admissions where the patient had an identifiable PCP prior to admission. In those analyses, the difference in adjusted length of stay between the hospitalist and non-hospitalist groups was 0.44 days (95% CI: 0.35-0.52), compared to the 0.36 days reported in Table 2. We also performed propensity analyses, stratifying admissions in quintiles based on propensity to receive hospitalist care. The differences in length of stay between the hospitalist and non-hospitalist group ranged from 0.25 days (95% CI: 0.12-0.37) to 0.52 days (95% CI: 0.38-0.65), with greater differences in length of stay in the quintiles with the highest propensity to receive hospitalist care.
To examine whether the shorter length of stay associated with hospitalist care varied by patient and hospital characteristics, two-way interactions were performed between hospitalist care and each of the characteristics included in the models in Table 2. The impact of hospitalist care on length of stay varied significantly by age, medical vs. surgical DRG, DRG weight, type of hospital, hospital teaching status, and ICU stay, but did not vary significantly by region, metropolitan size or patient socioeconomic status. Table 3 shows the differences in adjusted average length of stay between those cared for by hospitalists vs. non-hospitalists, stratified by each of those characteristics. The reductions are expressed as adjusted differences in days and also as the percent decrease in length of stay.
Table 3.
Differences in adjusted length of stay* between admissions with hospitalist care and non-hospitalist care, and percent decrease in adjusted length of stay** associated with hospitalist care, stratified by hospital and patient characteristics, in 4359 hospitals in 2006.
| Adjusted LOS for admissions with non-hospitalist care | Difference in adjusted LOS | (95% CI) | % decrease in Adjusted LOS associated with hospitalist care | ||
|---|---|---|---|---|---|
| Age | < 65 | 5.03 | 0.41 | (0.29, 0.53) | 8.2% |
| 65 – 74 | 4.97 | 0.42 | (0.33, 0.50) | 8.4% | |
| 75 – 84 | 5.09 | 0.47 | (0.39, 0.54) | 9.2% | |
| 85 + | 5.22 | 0.63 | (0.55, 0.71) | 12.1% | |
| Admission with ICU stay | No | 4.59 | 0.52 | (0.46, 0.58) | 11.3% |
| Yes | 6.31 | 0.37 | (0.27, 0.47) | 5.9% | |
| Diagnosis related group | Surgical | 5.85 | 0.19 | (0.05, 0.32) | 3.2% |
| Medical | 4.92 | 0.54 | (0.49, 0.60) | 11.1% | |
| Diagnosis related group weight | Q1 | 3.70 | 0.26 | (0.19, 0.32) | 6.9% |
| Q2 | 4.76 | 0.45 | (0.38, 0.52) | 9.5% | |
| Q3 | 5.28 | 0.56 | (0.49, 0.63) | 10.6% | |
| Q4 | 7.01 | 0.78 | (0.66, 0.89) | 11.1% | |
| Type of Hospital | Nonprofit | 5.06 | 0.48 | (0.41, 0.54) | 9.5% |
| For profit | 4.97 | 0.34 | (0.16, 0.51) | 6.8% | |
| Public | 5.32 | 0.67 | (0.51, 0.82) | 12.5% | |
| Medical school affiliation | Non | 4.96 | 0.55 | (0.47, 0.62) | 11.0% |
| Minor | 5.08 | 0.38 | (0.24, 0.53) | 7.6% | |
| Major | 5.50 | 0.41 | (0.25, 0.57) | 7.5% |
Differences in adjusted length of stay were estimated from the model including all significant two-way interactions (p<0.0001) between the characteristics listed on table and hospitalist care, and their main effects, adjusting for additional hospital characteristics (metropolitan size, total number of beds) and patient characteristics (gender, race/ethnicity, low socioeconomic status, weekend admission, total number of hospitalizations and total number of provider visits in one year prior to admission).
Percent decrease in adjusted length of stay was calculated by difference in adjusted LOS divided by adjusted LOS for admissions with non-hospitalist care.
Abbreviation: LOS, length of stay; CI, confidence interval.
The differences in length of stay were greater in older patients and in those without an ICU stay (Table 3). Adjusted length of stay differences between patients cared for by hospitalists and non-hospitalists were about three times as great for medical patients as for surgical patients. Similarly, there was a strong association between DRG weight and the impact of hospitalist care on length of stay. Length of stay differences between hospitalist and non-hospitalist care were three times greater in the highest vs. lowest quartile of DRG weight (0.26 vs. 0.78 days). Lengths of stay differences were greater in public and non-profit vs. for profit hospitals, and in non-teaching vs. teaching hospitals.
In Table 3, the results expressed as a percent reduction in average adjusted length of stay were similar to the results expressed as difference in length of stay in days, with the exception of DRG weight. Because underlying length of stay increased with increasing DRG weight, the percent reductions in length of stay did not vary as greatly by DRG weight.
Figure 1 presents analyses for the top 25 medical and top 15 surgical DRGs. The adjusted differences in length of stay between hospitalist and non-hospitalist care are plotted against the average total length of stay for patients receiving non-hospitalist care. Two findings are apparent. First, there is a strong association between the magnitude of the decrease in length of stay associated with hospitalist care and overall length of stay. Second, the association is different for admissions with surgical DRGs vs. medical DRGs.
Figure 1.
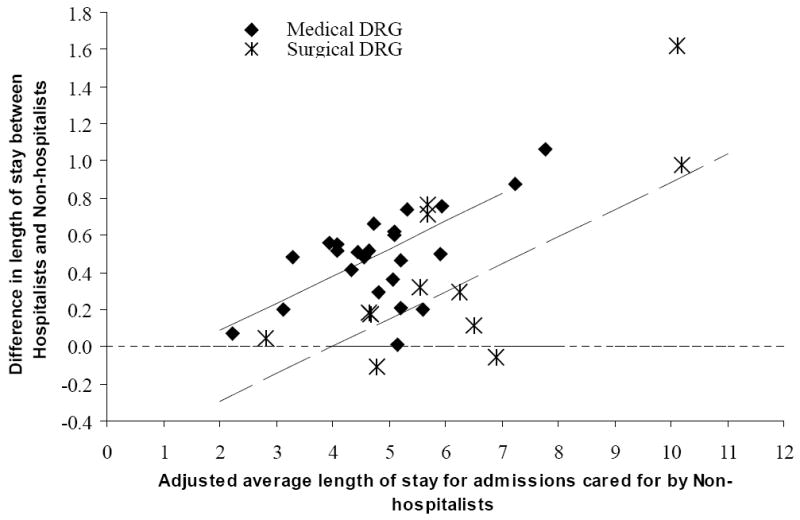
Differences in adjusted length of stay between patients cared for by hospitalists and non-hospitalists versus adjusted average length of stay for non-hospitalists, among the top 25 Medical DRGs and top 15 Surgical DRGs for 199,280 admissions in 4272 hospitals in 2006. The linear regression lines for Medical and Surgical DRGs were fitted separately.
For both medical and surgical DRGs, the correlation between decrease in length of stay and overall length of stay is strong (r=0.67 for medical DRGs and r=0.73 for surgical DRGs). Also, the slopes of the two regression lines do not differ significantly (P>0.56). However, the intercepts of the two curves are quite different (p=0.001). In the case of surgical DRGs, the impact of hospitalists on length of stay became apparent only when the overall length of stay for a given DRG was approximately 4 days or longer. With medical admissions, the impact of hospitalist care was apparent even in DRGs with very short overall mean lengths of stay.
Compared to patients cared for by non-hospitalists, patients cared for by hospitalists were less likely to be discharged to home (59.1% vs. 61.6%). We assessed whether the reduction in length of stay was associated with discharge location. The unadjusted differences in length of stay between patients cared for by hospitalists and non-hospitalists were similar for those discharged to home (0.39 days, 95 CI: 0.36-0.43) and those discharged to another health care facility (0.41 days, 95% CI: 0.33-0.49). Also, the interaction between hospitalist care and discharge location on length of stay was not significant (p=0.6826) in the multivariable GEE model.
We next assessed whether the impact of hospitalists on length of stay decreased over time. We compared the effect of hospitalist care on reduction of length of stay in 2001-2002, 2003-2004, and 2005-2006. The difference in adjusted average length of stay associated with hospitalist care was 0.02 (95% CI: 0.09-0.12) days in 2001-2002, 0.22 (95% CI: 0.14-0.30) days in 2003-2004, and 0.35 (95% CI: 0.29-0.41) days in 2005-2006 (p<0.001).
DISCUSSION
The reductions in length of stay associated with hospitalist care in 5036 hospitals nationally in the Medicare population are in line with findings from prospective trials and observational studies (1, 2, 7-11). In an observational study of 47 hospitals, Lindenauer et al. (12) reported an adjusted 0.4 days shorter length of stay. A prospective trial by Meltzer et al. (8) found an adjusted length of stay 0.49 days shorter in the second year of the trial, while the trial by Wachter et al. (5) reported a decrease of 0.6 days. Since reductions in length of stay associated with hospitalist care differ by DRG and hospital type (Table 2, Figure 1), differences among studies might be explained by hospital difference or differences in the distribution of diagnoses in the studied populations.
The amount of decrease in length of stay associated with hospitalist care varied significantly by age, complexity of disease and whether the patient had an ICU stay during admission. As hypothesized, reductions in length of stay were greater among older patients and those with complex disease. This is consistent with analyses from one academic hospital showing a greater impact of hospitalists in more complicated patients (17). These results support the concept that hospitalist care has a meaningful effect on reducing length of stay in geriatric medicine. Among the 25 most common medical and 15 most common surgical DRGs, there was a strong linear association between reductions in length of stay associated with hospitalist care and average length of stay for that DRG. Overall, the reduction in length of stay associated with hospitalist care was lower among surgical DRGs than medical DRGs. A number of investigators have reported on hospitalist care in surgical patients, particularly in orthopedic surgery, and have found reductions in length of stay (25-27), but no prior studies have compared the impact of hospitalists on surgical vs. medical patients, or by specific DRGs.
We also hypothesized that the effect of hospitalists on length of stay would be greater in academic than community hospitals, given the inefficiencies in care associated with teaching services (15, 16). In fact, the opposite was the case; community hospitals had greater length of stay reductions associated with hospitalist care. Hospitalist care was associated with greater reductions in length of stay at non-profit than at for-profit hospitals. This may be because for-profit hospitals have multiple mechanisms in place to reduce length of stay in addition to hospitalist care (28). Alternatively, different types of hospitals may attract different kinds of patients, and these differences may not be entirely controlled for in multivariable analyses.
We hypothesized that the magnitude of length of stay reductions associated with hospitalist care would diminish over time. We reasoned that the prospective trials of hospitalist care would have attracted highly motivated physicians as hospitalists, which may have resulted in decreases in length of stay resulting more from increased physician motivation than from the hospitalist model per se. In fact, we found that the association of hospitalist care with reduction in length of stay actually increased over time, from 0.02 days in 2001-2002 to 0.22 days in 2003-2004, and 0.35 days in 2005-2006. This finding argues against any Hawthorne effect, and is more consistent with the concept proposed by Meltzer et al. (8) and Auerbach et al. (11) that hospitalists get more efficient with experience. We recently reported that career stability and experience of hospitalists improved during the 2001 to 2006 period (4).
Our research has certain limitations. First, we did not assess hospital costs. Medicare claims data only provide information on charges, which are variably related to costs (29). In preliminary analyses, we found that the correlation of total hospital charges to length of stay was 0.73. We focused on length of stay because we felt it to be a more direct measure of resource utilization than charges. Second, we used a functional definition of a hospitalist, a generalist physician who derived ≥ 90% of Evaluation and Management charges from hospitalized patients (4). Prior works on hospitalists have used different definitions (5-8). Our definition did not reflect physician’s experience, nor did it take into account physician’s time spent on teaching and research. This definition also excluded medical subspecialists who are hospitalists (30, 31). Third, our study has a very large sample size. This allows us to test many interactions and control for multiple covariates, but the large sample size also causes the analyses to be overpowered. However, we focused on the magnitude of differences between two groups, not statistical significance. We feel that the 0.36 day reduction in mean length of stay likely translates into meaningful cost savings. Lindenauer et al. (12) reported a $268 average lower cost among patients cared for by hospitalists with a similar reduction in length of stay as our study.
Another limitation is that patients cared for by hospitalists differed from those cared for by non-hospitalists. For example, they were on average slightly younger and more likely to be in large hospitals and large metropolitan areas. We addressed these differences in several ways. First, we adjusted for these differences in patient and hospital characteristics in multilevel, multivariable analyses. Second, we repeated our analyses, restricting them to patients with an identified PCP, reducing the baseline differences between patients seen by hospitalists and non-hospitalists. Third, we stratified admissions into quintiles based on propensity to receive hospitalist care. These maneuvers did not substantially affect the estimates of reductions in length of stay associated with hospitalist care. Overall, we did not address the quality of hospitalist care, patient and family satisfaction with care, regional variation in length of stay associated with hospitalist care, and the outcomes of hospitalist care such as readmission rates. Further studies in these areas will give a more comprehensive understanding of hospitalist care.
In summary, the overall reduction in length of stay associated with hospitalist care in the Medicare population is modest, but has increased over time. The reduction varies by patient and hospital characteristics, with the greatest percent reductions in length of stay found in the very old and those with complicated disease.
Acknowledgments
This work was supported by grants K05CA134923 from the National Cancer Institute and grant R01AG033134 and P30AG024832 from the National Institute on Aging.
Sponsor’s Role: The funding agencies had no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: All authors participated in study design, analysis, and manuscript preparation. Dr. Kuo was primary responsible for study design, data analysis, and drafting the manuscript. Dr. Goodwin provided advice on study design/analysis, content expertise throughout the evolution of the study, and preparation of manuscript.
Conflict of Interest: All of authors have no conflict interest with this manuscript.
References
- 1.Coffman J, Rundall TG. The impact of hospitalists on the cost and quality of inpatient care in the United States: A research synthesis. Med Care Res Rev. 2005;62:379–406. doi: 10.1177/1077558705277379. [DOI] [PubMed] [Google Scholar]
- 2.Freed D. Hospitalists, evolution, evidence and eventualities. Health Care Manag. 2004;23:238–256. doi: 10.1097/00126450-200407000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517. doi: 10.1056/NEJM199608153350713. [DOI] [PubMed] [Google Scholar]
- 4.Kuo YF, Sharma G, Freeman JL, et al. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wachter RM, Katz P, Showstack J, et al. Reorganizing an academic medical service - Impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565. doi: 10.1001/jama.279.19.1560. [DOI] [PubMed] [Google Scholar]
- 6.Palmer HC, Armistead NS, Elnicki M, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627–632. doi: 10.1016/s0002-9343(01)00976-7. [DOI] [PubMed] [Google Scholar]
- 7.Kearns PJ, Wang CC, Morris WJ, et al. Hospital care by hospital-based and clinic-based faculty - a prospective, controlled trial. Arch Intern Med. 2001;161:235–241. doi: 10.1001/archinte.161.2.235. [DOI] [PubMed] [Google Scholar]
- 8.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: Results of a trial of hospitalists. Ann Intern Med. 2002;137:866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 9.Halasyamani LK, Valenstein PN, Friedlander MP, et al. A comparison of two hospitalist models with traditional care in a community teaching hospital. Am J Med. 2005;118:536–543. doi: 10.1016/j.amjmed.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 10.Rifkin WD, Holmboe E, Scherer H, et al. Comparison of hospitalists and nonhospitalists in inpatient length of stay adjusting for patient and physician characteristics. J Gen Intern Med. 2004;19:1127–1132. doi: 10.1111/j.1525-1497.2004.1930415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Auerbach AD, Wachter RM, Katz P, et al. Implementation of a voluntary hospitalist service at a community teaching hospital: Improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859–865. doi: 10.7326/0003-4819-137-11-200212030-00006. [DOI] [PubMed] [Google Scholar]
- 12.Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589–2600. doi: 10.1056/NEJMsa067735. [DOI] [PubMed] [Google Scholar]
- 13.Landefeld CS. Care of Hospitalized older patients: Opportunities for hospital-based physicians. J Hosp Med. 2006;1:42–47. doi: 10.1002/jhm.11. [DOI] [PubMed] [Google Scholar]
- 14.Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? J Hosp Med. 2006;1:29–35. doi: 10.1002/jhm.9. [DOI] [PubMed] [Google Scholar]
- 15.Koenig L, Dobson A, Book R, et al. Comparing hospital costs: Adjusting for differences in teaching status and other hospital characteristics. [June 22, 2008];Leapfrog Group. 2005 Apr; at http://www.leapfroggroup.org/media/file/Hospital_efficiency_adjustment_factors.pdf.
- 16.Rosko MD. Performance of US teaching hospitals: A panel analysis of cost inefficiency. Health Care Manag Sci. 2004;7:7–16. doi: 10.1023/b:hcms.0000005393.24012.1c. [DOI] [PubMed] [Google Scholar]
- 17.Southern WN, Berger MA, Bellin EY, et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2004;167:1869–1874. doi: 10.1001/archinte.167.17.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma G, Kuo YF, Freeman JL, et al. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170:363–368. doi: 10.1001/archinternmed.2009.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. [June 22, 2008];2007-2008 SHM survey, the authoritative source on the state of hospital medicine: highlights/executive summary. at http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=18782.
- 20.Koroukian SM, Xu F, Murray P. Ability of Medicare claims data to identify nursing home patients – a validataion study. Med Care. 2008;46:1184–1187. doi: 10.1097/MLR.0b013e31817925d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris RD, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Sharma G, Fletcher KE, Zhang D, et al. Continuity of outpatient and inpatient care by primary care physician for hospitalized older adults. JAMA. 2009;301:1671–1680. doi: 10.1001/jama.2009.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 24.DiAgostino RB., Jr Propensity score methods for bias reduction in the comparisons of a treatment to a nonrandomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 25.Huddleston JM, Long KH, Naessens M, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141:28–38. doi: 10.7326/0003-4819-141-1-200407060-00012. [DOI] [PubMed] [Google Scholar]
- 26.Phy MP, Vanness DJ, Melton J, et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165:796–801. doi: 10.1001/archinte.165.7.796. [DOI] [PubMed] [Google Scholar]
- 27.Nigwekar SU, Rajda J, Navaneethan SD. Hospitalist care and length of stay in patients with hip fracture: A systematic review. Arch Intern Med. 2008;168:1010–1011. doi: 10.1001/archinte.168.9.1010. [DOI] [PubMed] [Google Scholar]
- 28.Kessler DP, McClenllan MB. The effects of hospital ownership on medical productivity. Rand J Econ. 2002;33:488–506. [PubMed] [Google Scholar]
- 29.Friedman B, De La Mare J, Andrews R, et al. Practical options for estimating cost of hospital inpatient stays. J Health Care Financ. 2002;29:1–13. [PubMed] [Google Scholar]
- 30.Freed GL, Brzoznowski K, Neighbors K, et al. Characteristics of the pediatric hospitalist workforce: its roles and work environment. Pediatrics. 2007;120:33–39. doi: 10.1542/peds.2007-0304. [DOI] [PubMed] [Google Scholar]
- 31.Landrigan CP, Conway PH, Edwards S, et al. Pediatric hospitalists: A systematic review of the literature. Pediatrics. 2006;117:1736–1744. doi: 10.1542/peds.2005-0609. [DOI] [PubMed] [Google Scholar]


