Abstract
Objective
Examine effects of newborn screening (NBS) and neonatal diagnosis on the quality of mother-infant interactions in the context of feeding.
Methods
Study compared the quality of mother-infant feeding interactions among four groups of infants classified by severity of NBS and diagnostic results: cystic fibrosis (CF), congenital hypothyroidism, heterozygote CF carrier, and healthy with normal NBS. The Parent-Child Early Relational Assessment and a task-oriented item measured the quality of feeding interactions for 130 dyads, infant ages 3–19 weeks (M=9.19, SD=3.28). The Center for Epidemiologic Studies Depression Scale and State-Trait Anxiety Inventory measured maternal depression and anxiety.
Results
Composite Indicator Structure Equation Modeling showed that infant diagnostic status and, to a lesser extent, maternal education predicted feeding method. Mothers of infants with CF were most likely to bottle feed, which was associated with more task-oriented maternal behavior than breastfeeding. Mothers with low task-oriented behavior showed more sensitivity and responsiveness to infant cues, as well as less negative affect and behavior in their interactions with their infants than mothers with high task-oriented scores. Mothers of infants with CF were significantly more likely to have clinically significant anxiety and depression than the other groups. However, maternal psychological profile did not predict feeding method or interaction quality.
Conclusions
Mothers in the CF group were the least likely to breastfeed. Research is needed to explicate long-term effects of feeding methods on quality of mother-child relationship and ways to promote continued breastfeeding following a neonatal CF diagnosis.
The recent expansion of newborn screening (NBS) programs offers enormous potential for improving infant health by identifying serious metabolic or genetic conditions and offering prompt intervention. Despite these benefits, questions remain about the impact of a neonatal diagnosis or false-positive NBS result on the quality of a mother’s relationship with her infant. This report details the results of a study that examined the effects of a range of NBS results on the quality of mother-infant interactions during feeding.
Feeding as Context for Mother-Infant Relationship
Observations of mothers feeding their infants provide an ideal context for gaining insights about the evolving parent-child relationship. Feeding provides nurturance as well as nourishment. It also consumes most of very young infants’ wakeful interactions with their mothers. If the infant has a medical diagnosis requiring special nutritional needs, the mother might feel pressure to control her child’s nutrient intake leading to infant dysregulation, and tense dyadic interactions. Most children referred to specialists for feeding difficulties have medical conditions, including Cystic Fibrosis (CF).1–3 Several studies implicated the quality of parent-child interactions as the genesis of behavioral feeding problems in children with CF. Simmons et al4 found associations among attachment disturbances, feeding problems, and poor growth in young children with CF. Studies of mealtime interactions between parents and their young children with CF have repeatedly documented problematic behaviors involving parents’ attempts to increase their children’s food intake while children engage in food avoidance behavior.5–9 Study samples included infants as young as 7 months suggesting that such feeding difficulties begin very early in the child’s life. Our study examined early mother-infant feeding interactions to gain a better understanding of the etiology of such interactions and ultimately mother-child relationships.
The importance of breastfeeding to the physical health of children is well documented10 and internationally considered to be the biological norm for feeding infants.11 There is also a widely held belief that breastfeeding provides a path to favorable mother-infant relationships, but surprisingly little empirical evidence supports this assertion. In a recent review, Jansen and colleagues12 found only five data-based articles published since 1985 that addressed this topic, and the findings were equivocal. However, Farrow and Blissett13 found that breastfeeding during infancy was a predictor of greater maternal sensitivity, less controlling feeding behavior and fewer mealtime conflicts between mothers and their children at 1 year than formula feeding. Additionally, Strathearn and Mamun14 observed a relationship between non-breastfeeding mothers and child maltreatment. These findings suggest a potential interaction between maternal feeding methods and the quality of mother-infant relationship.
Postpartum Depression, Anxiety, and Neonatal Diagnosis
NBS results are typically shared with parents during the first days following the infant’s birth when women are at risk for postpartum depression15 and anxiety.16 A preliminary analysis of early data for this study found that mothers of infants recently diagnosed with CF had higher levels of anxiety and depression than mothers of infants diagnosed with congenital hypothyroidism, infants identified as CF carriers or infants with normal NBS results.17 Glasscoe, Lancaster, Smyth, et al.18 found that a CF diagnosis in early infancy was associated with parental depression. Maternal depression has been identified as a risk factor for parent-child relationship disturbances. Depressed mothers in the general population show diminished capacities to provide their infants with sensitive and responsive caregiving,19 which is essential for infants to develop secure attachments to their mothers, regulate their emotions, and form close interpersonal relationships later in childhood and adolescence.20,21 In a recent review article, Dennis and McQueen22 reported that depressed women tended to experience more difficulties with breastfeeding, were less likely to initiate and more likely to discontinue breastfeeding earlier than non-depressed women. Therefore, the presence of a neonatal diagnosis combined with maternal depression or anxiety poses a risk to the quality of interactions between mothers and their infants, and ultimately their relationships.
Purpose of Study
The purpose of this study was to examine the potential effect of abnormal NBS results and subsequent diagnosis on the quality of mother-infant interactions, particularly during feeding. The concern was that mothers of infants with a neonatal diagnosis might focus more on the medical needs of their newborns than on their infants’ emotional cues. Bowlby's Attachment Theory23 suggests that a pattern of task-oriented and emotionally unresponsive maternal caregiving established early in the parent-infant relationship could result in dysregulated mother-infant interactions characterized by increased tension and reduced reciprocity in dyadic interactions, which, over time, contribute to insecurity in the attachment relationship. Dysregulated mother-infant interactions combined with grief related to the infant’s diagnosis might further interfere with the normal attachment process resulting in early parent-child relationship disturbances. Thus, we hypothesized that there would be significant relationships between/among (a) infant diagnostic status and maternal psychological profile (depression and anxiety) and feeding method (breast versus bottle); (b) maternal psychological profile and quality of maternal interactions with infants; (c) the level of task-oriented caregiving during feeding and quality of maternal interactions with infants and the quality of dyadic interactions; as well as (d) mother and infant contributions to interactions and the quality of dyadic interactions.
METHODS
This study included data from the first of three data points in a longitudinal, mixed-method investigation17 that combined self-reports with videotaped observations of mother-infant feeding interactions. Data were collected during in-home assessments conducted when infants were between 3 and 19 weeks old. We chose four comparison groups that formed a continuum of infant health status based on NBS results: (a) cystic fibrosis, (b) congenital hypothyroidism, (c) heterozygote carriers of one CF mutation, and (d) healthy infants with normal NBS results. Cystic fibrosis (CF) is a serious life-shortening genetic condition that has no cure.24 The emphasis on high caloric intake for children with CF has been associated with behavioral feeding problems later in life.5, 6 CF has only recently been added to NBS nationally, whereas NBS for congenital hypothyroidism (CH) has been standard practice throughout the United States for about four decades. CH is similar to CF in prevalence and the lack of obvious manifestations of the disorder during the neonatal period. However, there are several important differences. Unlike the time and labor intense medical treatments required for infants with CF, infants with CH require a single daily oral medication and CH is associated with a more favorable prognosis than CF. Infants with false-positive NBS results for CF are usually found to be heterozygote carriers of one CF gene mutation. The CF carrier group (CF-C) was included because parents’ knowledge of their infants’ genetic status has been associated with lingering doubts about infant health25 that might alter parenting behavior. Finally, a group of mothers and their healthy infants with normal NBS results was included as a comparison group. The Institutional Review Boards of all four participating mid-western medical centers approved this project.
Recruitment
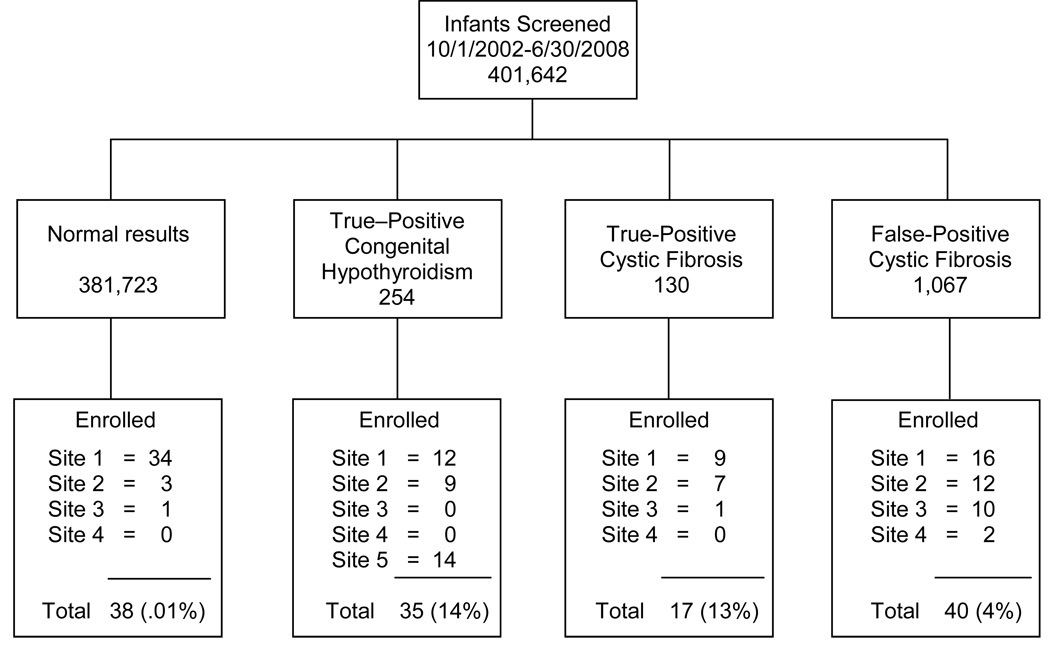
Between October 2002 and June 2008, convenience sampling methods were used to recruit families throughout Wisconsin. Health professionals identified and recruited potential participants during regularly scheduled appointments in specialty and primary care clinics at each of four recruitment sites that geographically spanned the entire state. Additionally, staff from the Wisconsin State Laboratory of Hygiene mailed recruitment materials to primary care providers to share with families who had infants with congenital hypothyroidism (CH), as about half of infants with CH in Wisconsin have their thyroid levels exclusively monitored by their primary care providers rather than endocrinologists. Figure 1 shows recruitment rates for each study group with the State Laboratory listed as site 5. All study participants provided written informed consent to enroll in this research.
FIGURE 1.
Recruitment Algorithm by Site and Study Group
Sample
Based on NBS and subsequent diagnostic results, the sample consisted of 130 families divided into the following four groups of mother-infant dyads representing a continuum of diagnostic severity resulting from NBS: healthy (H, n=38), CF carriers (CF-C, n=40), congenital hypothyroidism (CH, n=35), and cystic fibrosis (CF, n=17). Mother and infant characteristics are described in Table 1. The CF group included two infants, who had abnormal NBS results plus two CF mutations and normal or intermediate sweat test results. The CH group included one infant with borderline thyroid levels and one infant with CH who had a false-negative NBS but abnormal thyroid levels documented at 6 weeks in response to a review of family history. Infants who had serious co-morbid diagnoses (e.g. Down syndrome), significant perinatal complications, or were less than 32 weeks gestation were excluded.
Table 1.
Sample Demographics by Group
| Healthy n=38 |
CF-C n=40 |
CH n=35 |
CF n=17 |
Total N=130 |
|
|---|---|---|---|---|---|
| MATERNAL DATA | |||||
| Age in Years | 29.95 | 28.68* | 35.62 | 29.06 | 29.72** |
| SD=4.61 | SD=5.65 | SD=4.71 | SD=7.16 | SD=5.36 | |
| Married | 36 (94.7%) | 30 (75.0%) | 31 (88.6%) | 11 (64.7%) | 108 (83.1%) |
| Ethnicity | |||||
| European American | 37 (97.4%) | 40 (100%) | 30 (85.7%) | 16 (94.1%) | 123 (94.6%) |
| African American | 1 (2.6%) | 0 (0%) | 1 (2.9%) | 1 (5.9%) | 3 (2.3%) |
| Hispanic American | 0 (0%) | 0 (0%) | 2 (5.7%) | 0 (0%) | 2 (1.5%) |
| Asian American | 0 (0%) | 0 (0%) | 1 (2.9%) | 0 (0%) | 1 (0.8%) |
| Mixed | 0 (0%) | 0 (0%) | 1 (2.9%) | 0 (0%) | 1 (0.8%) |
| Education | |||||
| High School/GED | 2 (5.3%) | 8 (20.0%) | 3 (8.6%) | 5 (29.4%) | 18 (13.8%) |
| Community College/ Trade School |
4 (10.5%) | 12 (30.0%) | 13 (37.1%) | 4 (23.5%) | 33 (25.4%) |
| Baccalaureate College Degree | 23 (60.5%) | 12 (30.0%) | 13 (37.1%) | 4 (23.5%) | 52 (40.0%) |
| Graduate/Professional Degree | 9 (23.7%) | 8 (20.0%) | 6 (17.1%) | 4 (23.5%) | 27 (20.8%) |
| Income | |||||
| Less than $20,000 | 1 (2.6%) | 6 (15.0%) | 3 (8.6%) | 5 (29.4%) | 15 (11.5%) |
| $20,000 – $40,000 | 5 (13.2%) | 11 (27.5%) | 7 (20.0%) | 3 (17.6%) | 26 (20.0%) |
| $41,000 – $60,000 | 10 (26.3%) | 7 (17.5%) | 8 (22.9%) | 6 (35.3%) | 31 (23.8%) |
| $61,000 – $80,000 | 12 (31.6%) | 6 (15.0%) | 4 (11.4%) | 1 (5.9%) | 23 (17.7%) |
| $81,000 – $100,000 | 2 (5.3%) | 4 (10.0%) | 3 (8.6%) | 1 (5.9%) | 10 (7.7%) |
| More than $100,000 | 8 (21.1%) | 6 (15.0%) | 10 (28.6%) | 1 (5.9%) | 25 (19.2%) |
| Breastfeeding Mothers | 30 (78.9%) | 22 (55.0%) | 18 (51.4%) | 4 (23.5%) | 74 (56.9%) |
| INFANT DATA | |||||
| Infant Male/Female Gender | 21/17 | 18/22 | 15/20 | 7/10 | 61/69 |
| Infant Mean Age in Weeks | 8.17 | 9.25 | 10.01 | 9.65 | 9.19 |
| SD=3.45 | SD=2.39 | SD=3.37 | SD=4.11 | SD=3.28 | |
CF-C, cystic fibrosis carrier; CH, congenital hypothyroidism; CF, cystic fibrosis
n = 38 for mean age calculation, two subjects did not report age.
n = 128 for mean age calculation, two subjects did not report age.
Data Collection Measures
The Parent-Child Early Relational Assessment26 (PCERA) is a 65-item instrument designed to assess the affective and behavioral quality of interactions between parents and their infants or young children from birth to 4 years or more. Items are divided into parent, infant, and dyadic domains. Six factors, listed in Table 2, were developed from a normative sample of 381 parents feeding their four month old infants: Factor I Parental Positive Affective Involvement, Sensitivity, and Responsiveness, Factor II Parental Negative Affect and Behavior, Factor III Infant Positive Affect, Communicative and Social Skills, Factor IV Infant Dysregulation and Irritability, Factor V Dyadic Mutuality and Reciprocity, Factor VI Dyadic Tension. Cronbach’s alphas for these factors ranged from 0.85 to 0.94.26 The PCERA has been used in more than 400 programs and research projects internationally. The psychometric properties of the PCERA have been documented in high-risk as well as normative populations.27, 28
Table 2.
PCERA Factors for Four-Month Feeding
| Factor I – Parental Positive Affective Involvement, Sensitivity & Responsiveness | |
|---|---|
| Item number and name | |
| 2) expressive, non-flat voice tone | 16) amount of verbalization |
| 3) warm, kind tone of voice | 17) quality of verbalization |
| 4) expressed positive affect | 18) social initiative |
| 7) lack of depression, withdrawn mood | 19) contingent responsivity to positive behavior |
| 9) enthusiastic mood | 22) sensitivity, reads cues and responds |
| 12) enjoyment, pleasure | 23) connectedness |
| 13) positive physical contact | 24) mirroring |
| 15) visual contact | 26) creativity |
| Factor II – Parental Negative Affect and Behavior | |
|---|---|
| Item number and name | |
| 1) angry hostile tone of voice | 20) contingent responsivity to negative behavior |
| 3) warm, kind tone of voice | 21) lack of structure & mediating child’s environment |
| 5) expressed negative affect | 22) lack of sensitivity & responsivity |
| 6) angry, hostile mood | 25) rigidity |
| 11) displeasure | 27) intrustiveness |
| 14) negative physical contact | 28) inconsistency/unpredictability |
| 16) amount of verbalization | |
| Factor III – Infant Positive Affect, Communicative and Social Skills | |
|---|---|
| Item number and name | |
| 30) expressed positive affect | 45) exploratory play |
| 32) happy, pleasant | 47) robustness |
| 33) apathetic, withdrawn | 55) visual contact |
| 38) alertness | 56) communicative competence |
| 39) social initiative | 57) readability |
| 40) social responsiveness | |
| Factor IV – Infant Dysregulation and Irritability | |
|---|---|
| Item number and name | |
| 31) expressed negative affect | 41) avoiding/averting |
| 34) anxiety | 46) attentional abilities |
| 35) irritable, angry | 50) self regulation, organization |
| 37) emotional lability | 51) consolability/soothability |
| Factor V – Dyadic Mutuality and Reciprocity | |
|---|---|
| Item number and name | |
| 59) no flat, empty, constricted | 63) reciprocity |
| 61) enthusiasm, joie de vivre | |
| Factor VI – Dyadic Tension | |
|---|---|
| Item number and name | |
| 58) anger, hostility | 64) disorganization |
| 60) tension, anxiety | 65) state dissimilarity |
| 62) no joint attention, activity | |
We made every effort to videotape a typical feeding. In-home data collections were schedule completely at parents’ convenience (usually late afternoon or early evening for all groups), and when infants were likely to be fed. We avoided scheduling data collections when infants or parents were ill or within 24 hours of an infant’s immunizations. Initiation of videotaping during the visit was based on the mother’s appraisal of the infant’s readiness to feed. If the infant was asleep or not hungry when the data collector arrived, other data were collected until the mother indicated that the infant was ready to eat. On rare occasions when an infant slept through the 1 ½ to 2 hour visit, the data collector scheduled another time to perform the videotaping. Data collectors followed the instructions in PCERA manual26 to introduce the videotaping by stating, “This is a snapshot of one point in time. We’ll be interested in your sharing with us how it is alike or different from how things usually go. We are interested in seeing (infant’s name) and you during a feeding together. Please be with (infant’s name) just as you usually would.” We also encouraged mothers to feed their infants in their usual contexts, e.g. chair, room, etc. Mothers tended to describe the feedings as very typical.
We followed the PCERA manual instructions for modifying tasks and coding each item based on the child’s age. Thus, there were different expectations for a 3 week-old versus 3 month-old infant. In addition, coders for this study had educational backgrounds in infant and child development. Although coders remained blind to study groups, they were informed about each infant’s age (corrected for prematurity when relevant) and carefully considered the developmental appropriateness of the infant’s behaviors for each item. When coding young infants coders focused largely on the quality of the mother’s interaction with her infant. Coding also included feeding method (breast versus bottle).
The central premise of this study was that the degree to which mothers focused on the task of feeding, rather than their infants’ social-emotional cues and need for regulation, would mediate the overall quality of interactions between mothers and their infants. Although there is some support for this position in the literature,29, 30 to our knowledge, task-oriented caregiving has never been systematically isolated and empirically examined. The PCERA contains several conceptually similar items, e. g., item 21, parent effectively structures and mediates the environment to provide a quality of assistance that facilitate the child’s mastery of age-appropriate skills; item 22, parent empathically reads child’s cues and responds sensitively and appropriately. However, no item explicitly measures the level of parental task-oriented behavior and no other instrument could be found that measures this concept. Therefore, we developed a single item to exclusively measure the degree of task-oriented care-giving in this study (Table 3). As with the PCERA coding system, a high score signified a favorable rating and less task-oriented behavior. When rating the task-oriented variable the coder assessed how well the parent was able to accomplish the feeding task while providing nurturance, social engagement, and caregiving that was responsive to the infant’s cues. If parental behaviors appeared to show a need to simply get the infant to ingest food, thus overlooking the socio-emotional aspects of feeding, the interaction was coded as high task-oriented (lower score). By contrast, interactions were rated as low task-oriented (higher score) when mothers approached feeding as an opportunity to connect with their infants socially and emotionally through affectionate words, eye-contact, smiling, and gentle physical contact. These mothers also adjusted the duration and amount of feeding, as well as the infant’s position in response to the infant’s apparent needs.
Table 3.
Measure of Task-Oriented Behaviors
| Degree to which parent focuses on task emphasizing some aspect of the task over the interest of the child, e.g. cajoling child to eat during feeding, teaching child task in free play. This may include vocalizations or gestures. Both the quality and quantity of the task-oriented behaviors should be assessed. |
| 1 = Only focuses on task (child’s successful completion of task is main objective regardless of child’s preferences) |
| 2 = Primarily focuses on task |
| 3 = Focuses on child half the time and task half the time |
| 4 = More than minimal focus on task |
| 5 = Primarily focuses on child rather than task (task is only a means to engaging child in mutually enjoyable interaction) |
Specially trained raters coded the amount, duration, and intensity of interactions during five-minute videotaped mother-infant feeding segments using a Likert scale (1=area of concern; 5=area of strength). High scores indicated favorable ratings on all six PCERA factors and the assessment of task-orientation. The task-oriented item was included in the inter-rater reliability evaluations for the PCERA items. Inter-rater agreement was established through 40 hours of reliability training. Thereafter, 13% of segments were checked to maintain reliability. The average coder reliability was 81% for exact items and 89% for clustered within one scale point scores. Coders reviewed and discussed discrepant ratings to attain consensus scores.
The Center for Epidemiologic Studies Depression Scale31 (CES-D) is a 20-item self-report screening tool that measures the frequency of cognitive, affective, and, to a lesser extent, physical depressive symptoms during the past week (0=rarely; 3=most of the time). Scores ≥ 16 suggest clinical levels of symptoms. Internal consistency coefficients have been 0.85 in non-clinical samples and 0.90 in clinical samples, with a test-retest reliability coefficient of 0.54.
The State-Trait Anxiety Inventory32 (STAI) assesses anxiety with two 20-item self-report scales using a two-factor model of anxiety present or absent. The State scale measures levels of worry or apprehension in the present and the Trait scale assesses the persistence of these feelings. Respondents rate symptom frequency on a Likert scale (1=not at all; 4=very much so). The median internal consistency reliability coefficients for the State Scale and Trait Scale have been 0.92 and 0.90 respectively. Item remainder correlation coefficients for both scales have been consistently high (≥ .90).33 Scores ≥ 40 have been considered within a clinical range.33, 34
Analysis
We recognized that even with developmentally sensitive coding, some factors could be non-invariant, as most of the infants in this study were younger than the four month age on which the PCERA factors were confirmed. Therefore, invariant tests were conducted to assess the adequacy of fit between the existing factors and our study sample. Indications of good fit35 include: Chi-square/df ratio typically < 3.00, Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) >0.95, Cronbach’s alpha for lower bound of reliability > 0.8, and the composite reliability for true reliability > 0.8. Additionally, if the average invariant extracted (AVE) is less than 0.50, the invariance due to measurement error is larger than the invariance captured by the factors, and the validity of the individual indicators as well as the factor are suspect.36
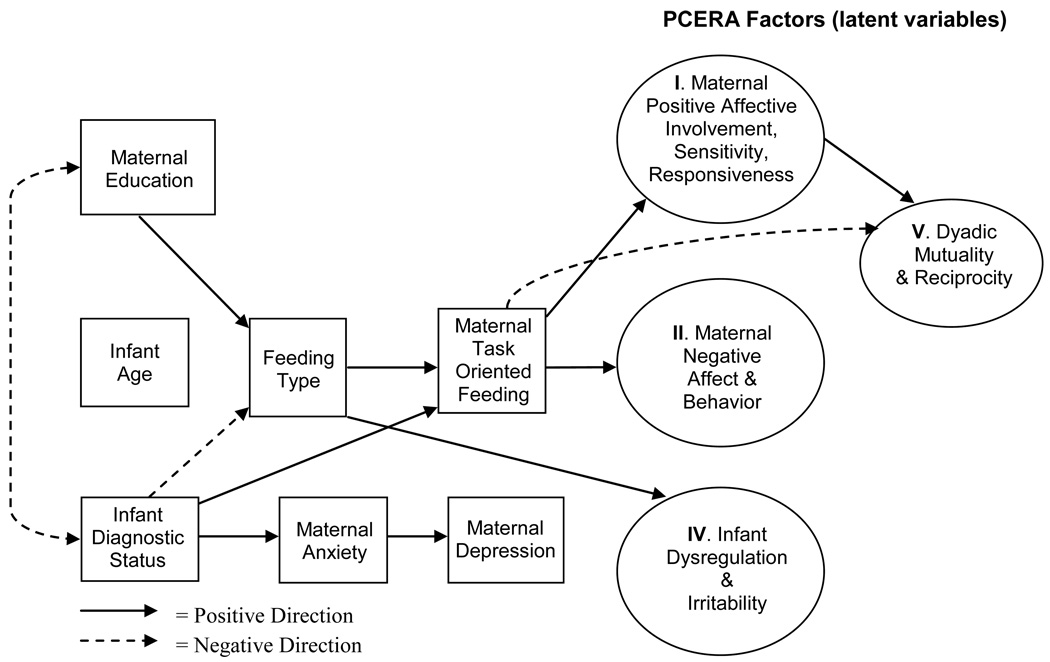
The analysis also used a subset of Structural Equation Modeling known as single Composite Indicator Structure Equation (CISE) modeling.37, 38 Based on our hypotheses, the model included the CESD and STAI as measures of maternal depression and anxiety, feeding method (breast versus bottle), PCERA factors and the task-oriented measure as assessment of the quality of mother-infant interactions. Due to the age variability in infants, infant age was added to the model. We also included maternal education level because research has shown a positive correlation between maternal education and rate of breastfeeding.39, 40
The CISE approach is based on item parceling to examine a recursive set of linear relationships between the exogenous variables (i.e., variables unrelated to other variables in the model) and endogenous variables (i.e., variables dependent upon one or more variables in the model) using maximum likelihood estimation. CISE modeling was used to (1) improve normality of the indicators, (2) reduce number of parameters estimated, (3) improve internal consistency of parameters, and (4) improve the variable to sample size ratio.37,38 In this approach, measurement errors for the composite indicators were fixed to an estimate of measurement error based on an estimate of reliability (1 - Cronbach's alpha*σ̣2 of composite variable).41 Measurement errors for individual items in the model were set to zero. This strategy provided disattenuated estimates of measurement error.
This project used a subset of data from a larger data set in which some values were missing. The structural equation modeling package Mplus Version 542 was used to implement the full information maximum likelihood (FIML) algorithm developed by Little and Rubin.43 There were no missing data for the subset used in this analysis in accordance with our practical survey of the visit records.
RESULTS
The results of the invariant analysis shown in Table 4 suggested that Factor I- Parental Positive Affective Involvement, Sensitivity & Responsiveness, Factor IV- Infant Dysregulation and Irritability, and Factor V- Dyadic Mutuality and Reciprocity had a good fit with the four month PCERA factors and Factor II- Parental Negative Affect and Behavior was acceptable based on standards used by Hu and Bentler.44 We excluded Factor III- Infant Positive Affect, Communicative and Social Skills and VI - Dyadic Tension because of poor fit. Results from the CISE model are diagrammed in Figure 2. The unstandardized parameter estimates are shown in Table 5 along with standard error and 95% confidence intervals for direct effects, covariates and indirect effects. Using clinical cut points to dichotomize depression and anxiety scores, infant diagnostic status was significantly associated with maternal anxiety in the predicted direction. As infant diagnostic status increased in severity, the clinical levels of maternal anxiety increased along with the clinical levels of depression. However, there was no significant association between maternal psychological profile and PCERA factors. Findings also indicated that infant diagnostic status was associated with feeding method. Mothers of infants with CF were the least likely to breastfeed. Bottle feeding was associated with significantly more task-oriented behavior than breastfeeding. However, the results suggested that mothers in the CF group also had the least task-oriented behavior. A closer examination of the data explained this apparent contradiction as resulting from the minority of breastfeeding mothers (23.5%) in the CF group. These breastfeeding mothers had the most favorable scores on the task-oriented item. Additionally, breastfed infants, regardless of group, showed less dysregulation and irritability than bottle fed infants.
Table 4.
PCERA Invariance Analysis
| 2 Month Feeding Sample (N=131) |
4 Month Feeding Sample (N=381)* |
||||||
|---|---|---|---|---|---|---|---|
| Scale | Chi Square/df |
CFI | TLI | Cronbach Alpha |
Composite Reliability |
AVE | Cronbach Alpha |
| Parental Positive Affective Involvement, Sensitivity and Responsiveness |
173.13/32 | 0.949 | 0.970 | 0.94 | 0.969 | 0.670 | 0.94 |
| Parental Negative Affect and Behavior |
173.8/23 | 0.850 | 0.883 | 0.85 | 0.938 | 0.564 | 0.86 |
| Infant Positive Affect, Communicative and Social Skills |
202.4/18 | 0.794 | 0.771 | 0.75 | 0.877 | 0.420 | 0.88 |
| Infant Dysregulation and Irritability |
17.93/12 | 0.995 | 0.996 | 0.83 | 0.925 | 0.617 | 0.91 |
| Dyadic Mutuality and Reciprocity |
54.63/12 | 0.918 | 0.912 | 0.80 | 0.877 | 0.708 | 0.85 |
| Dyadic Tension | 54.63/12 | 0.918 | 0.912 | 0.66 | 0.795 | 0.450 | 0.87 |
PCERA, Parent-Child Early Relational Assessment; df, degrees of freedom; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; AVE, average variance extracted
from Clark, 1985, 2006
FIGURE 2.
CISE Predictive Model for Mother-Infant Feeding Interactions
CISE, Composite Indicator Structure Equation; PCERA, Parent-Child Early Relational Assessment
Table 5.
PCERA Unstandardized Parameters, Standard Error and Confidence Intervals (CI)
| Direct Effect Paths | Parameter | Standard Error | 95% CI |
|---|---|---|---|
| Infant Diagnostic Status → Maternal Anxiety | 0.789* | 0.295 | 0.210, 1.367 |
| Infant Diagnostic Status → Maternal Depression | 0.246 | 0.309 | −0.360, 0.852 |
| Maternal Anxiety → Maternal Depression | 2.980* | 0.680 | 1.648, 4.312 |
| Maternal Depression → Maternal Positive Affect | 0.013 | 0.019 | −0.024, 0.049 |
| Maternal Anxiety → Maternal Positive Affect | −0.032 | 0.022 | −0.075, 0.012 |
| Feeding Type → Maternal Positive Affect | 0.017 | 0.013 | −0.008, 0.042 |
| Maternal Education → Maternal Positive Affect | −0.002 | 0.006 | −0.013, 0.010 |
| Maternal Task-Oriented Behavior → Maternal Positive Affect |
0.383* | 0.050 | 0.286, 0.480 |
| Infant Age → Maternal Positive Affect | 0.000 | 0.002 | −0.004, 0.004 |
| Maternal Depression → Maternal Negative Affect | −0.073 | 0.100 | −0.268, 0.122 |
| Maternal Anxiety → Maternal Negative Affect | −0.052 | 0.098 | −0.243, 0.140 |
| Feeding Type → Maternal Negative Affect | 0.058 | 0.058 | −0.055, 0.171 |
| Maternal Education → Maternal Negative Affect | 0.012 | 0.031 | −0.048, 0.073 |
| Maternal Task-Oriented Behavior → Maternal Negative Affect |
0.250* | 0.029 | 0.194, 0.306 |
| Infant Age → Maternal Negative Affect | 0.000 | 0.001 | −0.002, 0.002 |
| Maternal Depression → Infant Dysregulation | 4.571 | 7.932 | −10.975, 20.117 |
| Maternal Anxiety → Infant Dysregulation | −14.275 | 7.908 | −29.775, 1.225 |
| Feeding Type → Infant Dysregulation | 10.518* | 4.697 | 1.311, 19.725 |
| Maternal Education → Infant Dysregulation | −2.891 | 2.459 | −7.711, 1.929 |
| Infant Diagnostic Status → Infant Dysregulation | 3.329 | 1.966 | −0.525, 7.182 |
| Infant Age → Infant Dysregulation | 0.054 | 0.095 | −0.133, 0.241 |
| Infant Diagnostic Status → Maternal Task- Oriented Behavior |
0.191* | 0.088 | 0.020, 0.363 |
| Feeding Type → Maternal Task-Oriented Behavior | 0.608* | 0.176 | 0.262, 0.953 |
| Infant Age → Maternal Task-Oriented Behavior | 0.002 | 0.004 | −0.005, 0.009 |
| Infant Diagnostic Status → Feeding Type | −0.680* | 0.202 | −1.077, −0.284 |
| Maternal Education → Feeding Type | 0.556* | 0.209 | 0.147, 0.965 |
| Maternal Task-Oriented Behavior → Dyadic Mutuality |
−2.586* | 0.568 | −3.699, −1.473 |
| Infant Age → Dyadic Mutuality | −0.001 | 0.015 | −0.031, 0.029 |
| Maternal Positive Affect → Dyadic Mutuality | 7.830* | 1.208 | 5.461, 10.198 |
| Maternal Negative Affect → Dyadic Mutuality | −0.088 | 0.441 | −0.953, 0.776 |
| Infant Dysregulation → Dyadic Mutuality | −0.010 | 0.008 | −0.025, 0.006 |
| Covariance | |||
| Infant Diagnostic Status with Maternal Education | −0.063* | 0.025 | −0.111, −0.015 |
| Indirect Effect Paths | |||
| Maternal Task-Oriented Behavior → Maternal Positive Affect → Dyadic Mutuality |
2.995* | 0.605 | 1.81, 4.18 |
| Feeding Type → Maternal Task-Oriented Behavior → Maternal Positive Affect |
0.232* | 0.074 | 0.088, 0.377 |
| Feeding Type → Maternal Task-Oriented Behavior → Maternal Negative Affect |
0.152* | 0.047 | 0.059, 0.245 |
| Infant Diagnostic Status → Maternal Task- Oriented Behavior → Maternal Positive Affect |
0.073* | 0.035 | 0.005, 0.142 |
| Infant Diagnostic Status → Maternal Task- Oriented Behavior → Maternal Negative Affect |
0.048* | 0.023 | 0.004, 0.092 |
| Infant Diagnostic Status → Feeding Type → Maternal Task-Oriented Behavior |
−0.206a | 0.107 | −0.415, 0.002 |
| Maternal Education → Feeding Type → Maternal Task-Oriented Behavior |
0.076a | 0.054 | −0.030, 0.182 |
| Infant Diagnostic Status → Maternal Anxiety → Maternal Depression |
0.617a | 0.388 | −0.046, 1.279 |
PCERA, Parent-Child Early Relational Assessment
p < .05
To assess the indirect effect for these paths, the model was changed to the WLSMV estimator with theta parameterization.32
The findings showed the level of maternal task-oriented behavior had a significant, positive, direct effect on PCERA Factors I and II. In other words, mothers who had low task-oriented caregiving were more affectively involved, sensitive and responsive to their infants’ cues, whereas those with high task-oriented behavior showed more negative affect and behavior. Mothers with high task-oriented behavior made few vocalizations to, or about, their infants during the feeding. The comments they made focused on the feeding task rather than attempts to initiate social interactions or reflect the infant’s affective or behavioral state. Task-oriented mothers’ facial expressions also tended to show little animation or enthusiasm. Task-oriented behavior had a significant, positive, indirect effect on PCERA Factor V- Dyadic Mutuality and Reciprocity. Task-oriented behavior also significantly mediated the effects of feeding type and diagnostic status on the quality of maternal behaviors of PCERA Factors I - Parental Positive Affective Involvement, Sensitivity & Responsiveness and II - Parental Negative Affect and Behavior. Significant, positive effects were found between Factor I Parental Positive Affective Involvement, Sensitivity & Responsiveness and Dyadic Factor V- Dyadic Mutuality and Reciprocity. The indirect relationship between task-oriented behavior and PCERA Factor V- Dyadic Mutuality and Reciprocity was the only finding not supporting our hypothesis. Otherwise, the relationships were in the hypothesized direction.
The analysis of the effects of maternal demographics on feeding method revealed that mothers in the healthy comparison group had higher education levels and were most likely to breastfeed. Given the potential confound of maternal education in regards to feeding choice, a Wall test (parameter divided by standard error) was performed to examine the relative magnitude of the effect of maternal education in comparison with infant diagnostic status. Results showed that infant diagnostic status (−3.336) had a stronger effect than maternal education (2.814) on maternal feeding choice. Infant age was not associated with any variable.
DISCUSSION
Feeding as Context for Mother-Infant Relationship
Findings in this report offer empirical evidence of an association between breastfeeding and the quality of mother-infant interactions, expressed in maternal task-oriented behaviors. These results also provide new evidence that this relationship extends to mother-infant dyads in the presence of a neonatal diagnosis for CF or CH. The mechanism for the favorable mother-infant interactions associated with breastfeeding remains unclear. One theory suggests oxytocin and prolactin released during lactation mediate stress reactivity and enhance maternal mood.45 If this protective physiologic buffer is lacking due to bottle feeding, women might be more susceptible to stress and consequently interact negatively with their infants. An alternative theory posits that the intimacy of breastfeeding interactions helps mothers learn their infants’ cues and become more attuned to their needs.46 However, women who are innately sensitive caregivers might be more likely to nurse their infants than mothers without these characteristics. There might actually be a synergistic effect of maternal social psychology combined with endocrine physiology that accounts for the favorable effects of breastfeeding as compared with bottle feeding in regards to the quality of mother-infant interactions.
As hypothesized, mothers who expressed a cheerful affect towards their infants and provided sensitive, responsive caregiving based on their infant’s cues had dyadic social exchanges with their infants characterized by reciprocal and mutual enjoyment. This observation is consistent with Bowlby’s Attachment Theory. However, this framework fails to recognize how medically fragile infants with limited self-regulation capacities or poor oral motor coordination might influence maternal feeding behavior. Mother-infant feeding interactions most likely involve multiple contexts that can include, but are not limited to, the infant’s temperament and health needs, the mother’s cultural and familial values, socially prescribed behavior, her psychological state, and the personal meaning that she ascribes to food and the feeding interaction. A transactional perspective47 might be a more appropriate model for future studies of mother-infant feeding interaction because it acknowledges the infant’s contribution to the quality of interactions.
Breastfeeding Infants with Health Problems
Very little research has been conducted with breastfeeding in mother-infant dyads with CF and none with infants who have CH. The few studies found for the CF population focus on the nutritional or pulmonary effects, not the relational aspect of breastfeeding. Results show similar weight gain patterns46–51 and nutritional laboratory values48 in breastfed and formula fed infants with CF as well as pulmonary benefits for breastfed infants with CF.49, 51 Although the CF Foundation Evidence-Based Guidelines recommend “human milk” for neonates diagnosed with CF,52 the high rate of formula feeding in the CF group found in our study is consistent with the literature.48, 51 Young children with CF can require 120% of the normal Dietary Reference Intake for calories to maintain normal growth52 and evidence shows a relationship between favorable nutritional status and pulmonary health in children with CF.53 Feeling pressure to achieve this nutritional goal, mothers might switch from breastfeeding to high calorie formula. Given the documented health and relational benefits for breastfeeding, it may be especially important for mothers to continue breastfeeding, even in the presence of a neonatal diagnosis. With the national implementation of NBS for CF, significantly more mothers will be faced with a decision about feeding method that may be counter to their original plans. These mothers might require extra support, such as certified lactation consultants with specialized knowledge and experience working with mother-infant dyads following a neonatal CF diagnosis. It might also be beneficial to provide mothers with infant scales so they can measure the amount of breast milk the infant ingests. Additional research is needed to examine the long-term health outcomes associated with early infant feeding methods for children with CF.
Some toddlers and children with CF develop feeding problems characterized by food refusal, parental coaxing behavior, prolonged mealtime, and tense interactions between the children and their parents.5, 6 These behaviors are consistent with the task-oriented construct which offers a framework for understanding the potential etiology of feeding problems, particularly among children with chronic health conditions that require intense nutritional intervention. Farrow and Blissett54 posit that highly controlled feeding practices adversely affect infants’ capacities to recognize their physiologic signals for hunger and satiety. Interestingly, Farrow and Blissett13 also report findings that breast fed infants consumed more solid food at one year than bottle fed infants. Such outcomes could be particularly beneficial to children with CF. Other studies show similar results that over-controlling feeding practices have counterproductive results that can lead to childhood eating problem.55–57 Establishing optimal affective and behavioral patterns of parent-child interactions within the feeding/eating context early in life may be critical to the physical health as well as the psychosocial development of children with CF. A breastfeeding mother who responds to her infant’s cues by allowing the infant to control the feeding pace, duration and quantity of milk ingested might offer infants greater opportunities to learn internal cues and develop self-regulation capacities, especially important to infants with CF who are at risk for nutritional deficiencies.
It would be especially informative to investigate whether the early benefits of breastfeeding and low task-oriented parental feeding behavior continue when children enter toddlerhood. At about 12-months, children strive to accomplish developmental tasks involving separation and individuation from their parents. Toddlers’ emerging independence can be challenging for many aspects of parenting, but particularly at mealtimes because it requires parental scaffolding with respect for the child’s strivings towards autonomy. In the next phase of our longitudinal project we plan to examine factors affecting the quality of parent-child feeding interactions when infants reach 12 months of age.
Task-oriented Caregiving and Maternal-Infant Interactions
The strong association between task-oriented behavior and PCERA Factor I- Parental Positive Affective Involvement, Sensitivity & Responsiveness and Factor II- Parental Negative Affect and Behavior provide evidence in support of the variable’s construct validity and its impact on the quality of parental caregiving behaviors. Although there is some conceptual overlap between the PCERA factors and the task-oriented item, no PCERA item consistently received the same rating as the task-oriented item which suggests that the task-oriented item assesses phenomena not completely captured by the PCERA. The level of task-oriented behavior also represents the central link in the model suggesting that this construct could be critical to enhancing our understanding of parent-child feeding interactions and a potential focal point for interventions.
The inverse relationship between task-oriented maternal behavior and dyadic mutuality and reciprocity was unanticipated. The new item was designed to assess only maternal behavior, whereas, dyadic items assess the quality of mother and infant interactions as a single unit. Consequently, an infant’s favorable contribution to the interaction could produce better ratings on dyadic items than ratings on maternal items that assess similar constructs. Task-oriented feeding behavior is presumptively motivated by the goal of persuading the infant to ingest nutrients. Perhaps, during early infancy when the infant feeding is reflexive, the task is better facilitated by coordinated turn-taking, e.g. mother feeding and infant eating, that is expressed as mutually satisfying, particularly for the infant. Thus, dyadic reciprocity is appraised favorably.
It is important to note that high task-oriented feeding behavior was not exclusively observed in the bottle feeding mothers. A few breastfeeding mothers were also highly task-oriented. Thus, feeding method does not completely explain the origins of this parenting behavior. The following examples were considered high task-oriented behaviors. The mother paid so much attention to the amount of formula in the bottle that she failed to see her infant reaching up to her or attempting to make eye contact. A breastfeeding mother's only interactions with her infant involved tapping the infant's cheek to persuade the infant to continue sucking. Despite the infant’s signs of dysregulation (squirming in mother’s arms, avoiding or withdrawing from feeding), a mother insisted on continuing the feeding rather than give the infant a break, help the infant reorganize, and then resume feeding. The task-oriented behavior was not always directed towards controlling food intake. A bottle-feeding mother repeatedly interrupted the feeding to wipe dribbled formula from around the infant’s mouth. A disruptive cycle ensued in which the mother became increasingly intrusive and aggressing with wiping and the infant became increasingly emotionally dysregulated, with diminished oral-motor coordination and greater formula leakage. Finally the infant became very distressed and the mother stopped feeding.
It is also possible that the expression of task-oriented care-giving varies by the infant’s diagnosis and the activity shared by mother and child. For example, a mother of an infant with CF might be motivated by concerns about her child’s weight gain and therefore use much task-oriented behavior to increase the infant’s food intake. When engaged in other interactions, such as play or diaper changes, this mother might show very little task-oriented behavior. Additional research is needed to delineate the multiplicity of task-oriented behavior and the degree to which such behavior is a function of infant health status, maternal characteristics and shared circumstances.
Maternal Psychological Functioning
The analysis showed that mothers of infants with a neonatal CF diagnosis were most likely to report anxiety in the clinical range and high anxiety was associated with high depression scores. Anxiety as a mediator for clinical depression following the infant’s birth has only recently gained recognition.58, 59 These studies showed a relationship between anxiety and depression in women experiencing clinical levels of symptoms for which prenatal anxiety predicted early postpartum depression. However, our study measured depression and anxiety concurrently. In contrast to previous research,19, 22 the results of this study showed no association between maternal anxiety or depression and the quality of mothers’ interactions with their infants. However, the inclusion criteria for this study were based on the infant’s health status rather than the mother’s psychological profile. Therefore, it is likely that the number of women with clinical levels of anxiety or depression in this study was too small to detect such a relationship.
Another explanation is that other psychological processes have a greater influence over maternal feeding decisions and behavior. Farrow and Blissett60 found a constellation of pre and post natal maternal cognitions to be associated with feeding difficulties when infants were 6 months. Maternal representation implicated during pregnancy included emotional deprivation, sense of entitlement, and enmeshed beliefs; postpartum variables included feeling socially isolated, low self worth, and perceiving the infant as temperamentally difficult. Yet another possibility is that the cause-effect relationship between maternal mood and infant feeding is actually bidirectional. Perhaps, infant skill and regulation capacity influence maternal mood. In the case of CF, the infant’s heath, as measured by food intake and weight gain could affect the mother’s sense of competence and efficacy that alter her mood as well as her relationship with her infant. A transactional theoretical model would better guide future exploration of maternal and infant characteristics that contribute to the quality of interactions, regardless of feeding method. We also need a better understanding of the instrumental and psychosocial support that mothers require following a neonatal diagnosis that will foster nurturing caregiving.
Limitations
There were several notable limitations in this study. The assessment of task orientation was a single item developed for this study and lacks historical psychometric data. The non-random convenience sampling methods could have introduced bias. Due to the relatively small subgroup size, some parameters, e.g., maternal anxiety and depression, may lack sensitivity. We did not track feeding method, e.g., exclusive breast feeding vs. supplemental feeding or the duration of breastfeeding, throughout this study because the investigation was designed to evaluate the quality of parent-infant interactions relative to NBS results; it was not designed to be a feeding study per se. We chose the context of feeding because of its developmental salience for this age group and research documenting feeding problems in children with CF. The group differences in rates of breast feeding were serendipitous findings that point to the need for additional inquiry about mothers’ decision-making process about feeding following a neonatal diagnosis. Finally, the mother-infant interaction data analyzed for this study represented only a snapshot in time. It would be valuable to learn whether repeated task-oriented caregiving has long-term effects on the parent-child relationship.
Clinical Implications
Neither a neonatal diagnosis of CF, CH, nor false-positive CF NBS result directly affect the quality of early mother-infant feeding interactions. None the less, it is concerning that the majority of mothers of infants with CF did not breast feed given the findings of a favorable relationship between breastfeeding and the quality of mother-infant interactions. With an emphasis on caloric intake for infants with pancreatic insufficiency, perhaps mothers discontinue breastfeeding in favor of calorie-dense, predigested formulas. As NBS programs expand, increasing number of neonates will be diagnosed with serious health conditions. Health care professionals can support the parent-infant relationship following a neonatal CF diagnosis by supporting mothers’ efforts to breastfeed and emphasizing the importance of focusing on their infants’ affective and regulatory cues for their infant’s well-being while attending to the child’s nutritional needs.
CONCLUSION
Breastfeeding was associated with less task-oriented caregiving behavior and therefore more favorable mother-infant interactions than bottle feeding. Contrary to our hypothesis, high task-oriented feeding was indirectly associated with higher levels of dyadic reciprocity. This finding may be the result of the infant’s contribution to the interaction. Mothers in the CF group were the least likely to breastfeed. Although mothers of infants with CF were also most likely to report clinical anxiety levels, this finding did not appear to influence the quality of interactions. Further research is needed to (a) elucidate the origins of task-oriented caregiving, (b) identify types of support mothers require to continue breastfeeding in the presence of a neonatal CF diagnosis, and (c) explicate the long-term impact of early feeding methods on child feeding behaviors later in life and the quality of the mother-child relationship.
ACKNOWLEDGEMENTS
We thank the families who participated in this study. We also gratefully acknowledge the research teams from the University of Wisconsin-Madison, the American Family Children’s Hospital, the Children’s Hospital of Wisconsin, the Marshfield Clinic, Gunderson-Lutheran Medical Center, and the Wisconsin State Laboratory of Hygiene. Special thanks for Karen Pridham, PhD, RN, FAAN, Philip M. Farrell, MD, PhD, and Laura Hogan, PhD for their editorial wisdom.
Funding
This project was supported by National Institute of Child Health and Human Development (K23HD42098); the University of Wisconsin-Madison School of Nursing; the University of Wisconsin Graduate School; and the Clinical and Translational Science Award program of the National Center for Research Resources, National Institutes of Health (1UL1RR025011).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Burklow KA, McGrath AM, Valerius KS, et al. Relationship between feeding difficulties, medical complexity, and gestational age. Nutr Clin Pract. 2002;17:373–378. doi: 10.1177/0115426502017006373. [DOI] [PubMed] [Google Scholar]
- 2.Field D, Garland M, Williams K. Correlates of specific childhood feeding problems. J Paediatr Child Health. 2003;39:299–304. doi: 10.1046/j.1440-1754.2003.00151.x. [DOI] [PubMed] [Google Scholar]
- 3.Rommel N, De Meyer AM, Feenstra L, et al. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. J Pediatr Gastroenterol Nutr. 2003;37:75–84. doi: 10.1097/00005176-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Simmons R, Goldberg S, Washington J, et al. Infant-mother attachment and nutrition in children with CF. J Dev Behav Pediatr. 1995;16:183–186. [PubMed] [Google Scholar]
- 5.Mitchell MJ, Powers SW, Byars KC, et al. Family functioning in young children with cystic fibrosis: Observations of interactions at mealtime. J Dev Behav Pediatr. 2004;25:335–346. doi: 10.1097/00004703-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Powers SW, Patton SR, Byars KC, et al. Caloric intake and eating behavior in infants and toddlers with cystic fibrosis. Pediatrics. 2002;109:e75. doi: 10.1542/peds.109.5.e75. [DOI] [PubMed] [Google Scholar]
- 7.Powers SW, Mitchell MJ, Patton SR, et al. Mealtime behaviors in families of infants and toddlers with cystic fibrosis. J Cystic Fibrosis. 2005;4:175–182. doi: 10.1016/j.jcf.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 8.Stark LJ, Jelalian E, Powers SW, et al. Parent and child mealtime behavior in families of children with cystic fibrosis. J Pediatr. 2000;136:195–200. doi: 10.1016/s0022-3476(00)70101-6. [DOI] [PubMed] [Google Scholar]
- 9.Stark LJ, Opipari LC, Jelalian E, et al. Child behavior and parent management strategies at mealtime in families with a schoolage child with cystic fibrosis. Health Psychol. 2005;24:274–280. doi: 10.1037/0278-6133.24.3.274. [DOI] [PubMed] [Google Scholar]
- 10.Toma TS, Rea MF. Benefits of breastfeeding for maternal and child health: An essay on the scientific evidence. Cad Saude Publica. 2008;24:S235–S246. doi: 10.1590/s0102-311x2008001400009. [DOI] [PubMed] [Google Scholar]
- 11.Berry NJ, Gribble KD. Breast is no longer best: promoting normal infant feeding. Matern Child Nutr. 2008;4:74–79. doi: 10.1111/j.1740-8709.2007.00100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jansen J, de Weerth C, Riksen-Walraven JM. Breastfeeding and the mother-infant relationship—A review. Dev Rev. 2008;28:503–521. [Google Scholar]
- 13.Farrow C, Blissett J. Breast-feeding, maternal feeding practices and mealtime negativity at one year. Appetite. 2006;46:49–56. doi: 10.1016/j.appet.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Strathearn L, Mamun AA, Najman JM, et al. Does breastfeeding protect against substantiated child abuse and neglect? A 15-year cohort study. Pediatrics. 2009;123:483–493. doi: 10.1542/peds.2007-3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leahy-Warren P, McCarthy G. Postnatal depression: prevalence, mothers’ perspectives, and treatments. Arch Psychiatr Nurs. 2007;21:91–100. doi: 10.1016/j.apnu.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. J Clin Psychiatry. 2006;67:1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- 17.Tluczek A, Clark R, Kosick RL, et al. Mother-infant relationship in the context of neonatal CF diagnosis: Preliminary findings. Pediatr Pulmonol Suppl. 2005;28:179–180. [Google Scholar]
- 18.Glasscoe C, Lancaster GA, Smyth RL, et al. Parental depression following the early diagnosis of cystic fibrosis: a matched, prospective study. J Pediatr. 2007;150:185–191. doi: 10.1016/j.jpeds.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 19.Goodman SH. Depression in mothers. Annu Rev Clin Psychol. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- 20.Grossmann K, Grossman KE, Kinder H. Early care and the roots of attachment and partnership representations: the Bielefeld and Regensburg longitudinal studies. Ch. 5. In: Grossmann KE, Grossman K, Waters E, editors. Attachment from Infancy to Adulthood: The Major Longitudinal Studies. New York, NY: The Guilford Press; 2005. pp. 98–136. [Google Scholar]
- 21.DeKlyen M, Greenberg MT. Attachment and Psychopathology in Childhood. In: Cassidy J, Shaver PR, editors. Handbook of Attachment: Theory, Research, and Clinical Applications. Ch. 272nd ed. New York, NY: The Guilford Press; 2008. pp. 637–665. [Google Scholar]
- 22.Dennis CL, McQueen K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics. 2009;123:e736–e751. doi: 10.1542/peds.2008-1629. [DOI] [PubMed] [Google Scholar]
- 23.Bowlby J. Attachment and Loss: Loss, Sadness, and Depression. Vol 3. New York, NY: Basic Books; 1980. [Google Scholar]
- 24.Strausbaugh SD, Davis PB. Cystic fibrosis: a review of epidemiology and pathobiology. Clin Chest Med. 2007;28:279–288. doi: 10.1016/j.ccm.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Tluczek A, Murphy K, Cavanagh L. Psychosocial consequences of false-positive newborn screen for cystic fibrosis. Journal of Qualitative Research. doi: 10.1177/1049732310382919. (accepted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clark R. The Parent-Child Early Relational Assessment. Madison: Department of Psychiatry, University of Wisconsin Medical School; 1985. p. 2006. Unpublished instrument. [Google Scholar]
- 27.Clark R. The parent-child early relational assessment: a factorial validity study. Educ Psychol Meas. 1999;59:821–846. [Google Scholar]
- 28.Clark R, Tluczek A, Gallagher KC. Assessment of Parent-Child Early Relational Disturbances. Ch. 3. In: DelCarmen-Wiggins R, Carter A, editors. Assessment of Mental Health Disorders in Infants and Toddlers. New York, NY: Oxford University Press; 2004. pp. 25–60. [Google Scholar]
- 29.Pridham K, Lin CY, Brown R. Mothers' evaluation of their caregiving for premature and full-term infants through the first year: contributing factors. Res Nurs Health. 2001;24:157–169. doi: 10.1002/nur.1019. [DOI] [PubMed] [Google Scholar]
- 30.Pridham KF, Brown R, Clark R, et al. Infant and caregiving factors affecting weight-for-age and motor development of full-term and premature infants at 1 year post-term. Res Nurs Health. 2002;25:394–410. doi: 10.1002/nur.10047. [DOI] [PubMed] [Google Scholar]
- 31.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 32.Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 33.Grant KA, McMahon C, Austin MP. Maternal anxiety during the transition to parenthood: A prospective study. J Affect Disord. 2008;108:101–111. doi: 10.1016/j.jad.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 34.Kvaal K, Macijauskiene J, Engedal K, et al. High prevalence of anxiety in hospitalized geriatric patients. Int J Geriatr Psychiatry. 2001;16:690–693. doi: 10.1002/gps.405. [DOI] [PubMed] [Google Scholar]
- 35.Yu CY, Muthen BO. Technical Report, Muthen, UCLA; Evaluation of model fit indices for latent variable models with categorical and continuous outcomes. 2001
- 36.Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18:39–50. [Google Scholar]
- 37.Bandalos DL. The effects of item parceling on goodness-of-fit and parameter estimate bias in structural equation modeling. SEM. 2002;9:78–102. [Google Scholar]
- 38.Bandalos DL, Finney SJ. Item parceling issues in structural equation modeling. In: Marcoulides GA, Schumacker RE, editors. Advanced Structural Equation Modeling: New Developments and Techniques. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2001. [Google Scholar]
- 39.Li R, Ogden C, Ballew C, et al. Prevalence of exclusive breastfeeding among US infants: The Third National Health and Nutrition Examination Survey (Phase II, 1991–1994) Am J Public Health. 2002;92:1107–1110. doi: 10.2105/ajph.92.7.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bertini G, Perugi S, Dani C, et al. Maternal Education and the Incidence and Duration of Breast Feeding: A Prospective Study. J of Pediatric Gastroenterology and Nutrition. 2003;37:447–452. doi: 10.1097/00005176-200310000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Hayduk LA. Structural Equations Modeling with LISREL: Essentials and Advances. Baltimore, MD: Johns Hopkins University Press; 1987. [Google Scholar]
- 42.Muthen LK, Muthen BO. Mplus: Statistical Analysis with Latent Variables User’s Guide. 5th Edition. Los Angeles, CA: Muthen and Muthen; 2007. [Google Scholar]
- 43.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2nd edition. New York, NY: Wiley-Interscience; 2002. [Google Scholar]
- 44.Hu L, Bentler P. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 45.Michaelsen KF, Lauritzen L, Mortensen EL. Effects of breast-feeding on cognitive functioning. In: Goldberg GR, Prentice A, Prentice A, Filteau S, Simondon K, editors. Breast-Feeding: Early Influences on Later Health: Advances in Experimental Medicine and Biology. Copenhagen, Denmark: Springer Science & Business Media BV; 2009. pp. 199–215. [DOI] [PubMed] [Google Scholar]
- 46.Britton JR, Britton HL, Gronwaldt V. Breastfeeding, sensitivity, and attachment. Pediatrics. 2006;118:e1436–e1443. doi: 10.1542/peds.2005-2916. [DOI] [PubMed] [Google Scholar]
- 47.Sameroff A. The transactional model of development. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 48.Bronstein MN, Sokol RJ, Abman SH, et al. Pancreatic insufficiency, growth, and nutrition in infants identified by newborn screening as having cystic fibrosis. J Pediatr. 1992;120:533–540. doi: 10.1016/s0022-3476(05)82478-3. [DOI] [PubMed] [Google Scholar]
- 49.Colombo C, Costantini D, Zazzeron L, et al. Benefits of breastfeeding in cystic fibrosis: A single-centre follow-up survey. Acta Paediatr. 2007;96:1228–1232. doi: 10.1111/j.1651-2227.2007.00397.x. [DOI] [PubMed] [Google Scholar]
- 50.Holliday KE, Allen JR, Waters DL, et al. Growth of human milk-fed and formula-fed infants with cystic fibrosis. J Pediatr. 1991;118:77–79. doi: 10.1016/s0022-3476(05)81850-5. [DOI] [PubMed] [Google Scholar]
- 51.Parker EM, O’Sullivan BP, Shea JC, et al. Survey of breast-feeding practices and outcomes in the cystic fibrosis population. Pediatr Pulmonol. 2004;37:362–367. doi: 10.1002/ppul.10450. [DOI] [PubMed] [Google Scholar]
- 52.Borowitz D, Robinson KA, Rosenfeld M, Davis SD, Sabadosa KA, Spear SL, Michel SH, Parad RB, White TB, Farrell PM, Marshall BC, Accurso FJ. Cystic Fibrosis Foundation evidence-based guidelines for management of infants with cystic fibrosis. J Pediatr. 2009;155(6 Suppl):S73–S93. doi: 10.1016/j.jpeds.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Konstan MW, Butler SM, Wohl ME, Stoddard M, Matousek R, Wagener JS, et al. Growth and nutritional indexes in early life predict pulmonary function in cystic fibrosis. J Pediatr. 2003;142:624–630. doi: 10.1067/mpd.2003.152. [DOI] [PubMed] [Google Scholar]
- 54.Farrow C, Blissett J. Does maternal control during feeding moderate early infant weight gain? Pediatrics. 2006;118:e293–e298. doi: 10.1542/peds.2005-2919. [DOI] [PubMed] [Google Scholar]
- 55.Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 56.Fsher JO, Birch LL, Smiciklas-Wright H, et al. Breast-feeding through the first year predicts maternal control in feeding and subsequent toddler energy intakes. J Am Diet Assoc. 2000;100:641–646. doi: 10.1016/S0002-8223(00)00190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.O’Connor TM, Hughes SO, Watson KB, et al. Parenting practices are associated with fruit and vegetable consumption in pre-school children. Pub Health Nutr. 2010;13:91–101. doi: 10.1017/S1368980009005916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Heron J, O’Connor TG, Evans J, et al. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80:65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 59.Skouteris H, Wertheim EH, Rallis S, et al. Depression and anxiety through pregnancy and the early postpartum: An examination of prospective relationships. J Affect Disord. 2009;113:303–308. doi: 10.1016/j.jad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 60.Farrow C, Blissett J. Maternal cognitions, psychopathologic symptoms, and infant temperament as predictors of early infant feeding problems: a longitudinal study. Int J Eat Disord. 2006;39:128–134. doi: 10.1002/eat.20220. [DOI] [PubMed] [Google Scholar]