Abstract
Multiple studies suggest an association of marijuana use with increased rates of sexual risk behavior and sexually transmitted diseases (STDs). Most studies have focused on global associations of marijuana use with sexual risk outcomes and few have examined relevant cognitive variables. Adolescents in the juvenile justice system are at elevated risk for HIV/STDs and preliminary evidence suggests that marijuana is a potentially important cofactor for sexual risk behavior in this population. This study evaluated global, situational and event-level associations of marijuana use and sex-related marijuana expectancies with sexual risk outcomes in a large, racially diverse sample of adjudicated youth (n = 656, 66% male, mean age = 16.7 years). Cross-sectional and prospective analyses identified associations of marijuana use and dependence symptoms with sexual risk outcomes, including lower frequency of condom use and higher STD incidence. Stronger sex-related marijuana expectancies predicted greater intentions for and frequency of marijuana use in sexual situations. In event-level analyses that controlled for alcohol, marijuana use predicted a significantly decreased likelihood of condom use; this association was moderated by sex-related marijuana expectancies. Mediation analyses suggested that behavioral intentions partly accounted for the prospective association of expectancies with marijuana use before sex. These results provide further evidence that marijuana use is a potentially important cofactor for HIV/STD transmission in high-risk adolescents and suggest that cognitive factors could be important for characterizing this association.
Keywords: Marijuana, cannabis, alcohol, sexual risk behavior, HIV, expectancies
Adolescents and young adults are among the groups at highest risk for acquiring HIV and other sexually transmitted diseases (STDs; CDC, 2005). The number of young people living with AIDS in the United States increased 42% from 2000–2004 and recent surveillance data indicate that adolescents incur a substantial proportion of new STD infections (CDC, 2009). Compared with adolescents in the general population, those involved with the juvenile justice system are at substantially higher risk for HIV/STDs and are considered an important focal group from a public health standpoint (Malow, Dévieux, Jennings, Lucenko, & Kalichman, 2001; Malow, Rosenberg, Donenberg, & Dévieux, 2006; Teplin, Mericle, McClelland, & Abram, 2003; Robbins & Bryan, 2004). Adjudicated youth report earlier sexual initiation, more lifetime sexual partners, lower rates of condom use, and higher incidence of STDs than the general adolescent population (e.g., Hammett, Gaiter, & Crawford, 1998; Teplin et al., 2003). Moreover, high rates of substance use, psychiatric comorbidity and externalizing behaviors are presumed to exacerbate HIV/STD risk in this group (Bryan & Stallings, 2002; Malow et al., 2001; 2006).
Although substance use is invariably cited as an important cofactor for HIV/STD risk, the co-occurrence of substance use and risky sex is a particularly prominent issue among adjudicated youth given a high prevalence of both behaviors (Malow et al., 2006). Whereas alcohol use has been studied extensively in relation to sexual risk behavior among adolescents (Cooper, 2002), some findings indicate that marijuana use is more prevalent than alcohol use among adjudicated youth (Kingree & Betz, 2003; Malow et al., 2001; Teplin et al., 2003). This finding is noteworthy given a growing literature documenting covariation among marijuana use and sexual risk behaviors. For instance, several studies suggest significantly higher STD incidence among marijuana users compared to non-users (e.g., Boyer et al., 1999; De Genna, Cornelius, & Cook, 2007; Mertz et al., 2000; Shrier, Harris, Sternberg, & Beardslee, 2001; Smith et al., in press; Wu, Ringwalt, Patkar, Hubbard, & Blazer, 2009). Although most studies have focused on dichotomous indicators of marijuana use, some evidence suggests greater STD rates as a function of increasing levels of use (De Genna et al., 2007; Smith et al., in press). The majority of these studies included adolescent or young adult samples, suggesting that marijuana use is a marker for HIV/STD risk in these groups.
Although covariation between marijuana use and STD incidence has been documented, an important question is whether marijuana use predicts specific behavioral patterns that confer increased risk for STDs. Studies addressing this question using global association analyses (i.e., examining basic covariation between marijuana use and sexual risk behaviors) generally report positive associations of marijuana use with sexual risk indices, including earlier sexual initiation (Bellis et al., 2008; Guo et al., 2005; Scivoletto et al., 2002), more lifetime sexual partners (Bellis et al., 2008; Brodbeck, Matter, & Moggi, 2006; Guo et al., 2002; Shrier, Emans, Woods, & DuRant, 1997; Yan, Chiu, Stoesen, & Wang, 2007; Wingood & DiClemente, 1998), sex with casual partners (Brodbeck et al., 2008; Mertz et al., 2000), and lower rates of abstinence (Malow et al., 2001). Findings specific to condom use are somewhat mixed; marijuana use is associated with reduced frequency or incidence of condom use in most (Adefuye, Abiona, Balogun, & Lukobo-Durrell, 2009; Bellis et al., 2008; Crosby, DiClemente, Wingood, Rose, & Lang, 2003; Guo et al., 2002; Kingree, Braithwaite, & Woodring, 2000; Scivoletto et al., 2002; Shrier et al., 2001; Yan et al., 2007), but not all studies (Mertz et al., 2000; Wingood & DiClemente, 1998; Smith et al., in press). Compared to global association studies, situational association analyses offer the relative advantage of assessing substance use in sexual contexts (e.g., frequency of marijuana use before sex). One study using both approaches found that marijuana use in sexual contexts showed a stronger association with risky sex than did global marijuana use (Kingree et al., 2000). In addition, prospective studies have reported that marijuana use trajectories in adolescence predict differences HIV risk behaviors several years later (Guo et al., 2002; Griffin, Botvin, & Nichols, 2006).
Event-level approaches are important for assessing covariation of substance use and risk behavior during specific sexual episodes (Weinhardt & Carey, 2000). In a large population-based study of heterosexual adults, incidence of marijuana use before sex did not differ significantly across recent protected (5.8%) and unprotected (7.2%) sexual events, a finding inconsistent with a significant global association reported in the same study (Brodbeck et al., 2006). In contrast, two studies with adjudicated adolescents found that marijuana use before sex predicted a roughly threefold increase in the likelihood of condom nonuse, after controlling for alcohol use and other event-level influences (Kingree et al., 2000; Kingree & Betz, 2003). Moreover, in these two studies event-level marijuana use was endorsed more frequently (40% and 45% of events, respectively) than alcohol use (16% and 11% of events) and alcohol did not predict condom use. Event-level studies therefore suggest that marijuana use is potentially a more prominent situational cofactor for sexual risk behavior than alcohol use among high-risk youth.
Studies of marijuana and sexual risk behavior have seldom examined individual difference factors relevant for these associations. One potentially important variable is individual differences in expectancies about the effects of substance use on sexual risk outcomes. For instance, studies of alcohol-related sexual risk behavior often examine sex-related alcohol expectancies (i.e., beliefs that alcohol facilitates sexual enhancement or risk taking) as a predictor of alcohol use during sexual events or a moderator of alcohol’s association with risky sex. Stronger sex-related alcohol expectancies are associated with more frequent alcohol use before sex (Brown & Vanable, 2007; Bryan, Ray, & Cooper, 2007; Dermen & Cooper, 1994b) and a higher likelihood of condom nonuse during drinking events (Bryan et al., 2007; Corbin & Fromme, 2000; Dermen, Cooper, & Agocha, 1998). The importance of sex-related alcohol expectancies is further demonstrated by experimental studies showing increases in sexual interest (George et al., 2000) and reductions in safe sex negotiation skills (Maisto, Carey, Carey, & Gordon, 2002) under alcohol placebo versus control beverage conditions.
Relative to alcohol expectancies, marijuana expectancies have been studied infrequently. However, expectancies appear important in predicting patterns of marijuana use among young adults (e.g., Gaher & Simons, 2007; Neighbors, Geisner, & Lee, 2008; Simons, Dvorak, & Lau-Barraco, 2009). Additionally, two independent survey studies found that a sizable proportion of participants endorsed marijuana use to enhance sexual experiences, lower inhibitions and/or increase the likelihood of sex (Bellis et al., 2008; Sumnall et al., 2007). Though not formally assessed, the relevance of sex-related marijuana expectancies is implicit in these results. One study (Kingree and Thompson, 2007) evaluated sex-related alcohol expectancies in adolescents by adapting a measure of sex-related alcohol expectancies (Dermen & Cooper, 1994a). Stronger beliefs that marijuana enhances sexual experience predicted marijuana use at last intercourse, whereas expectancies that marijuana leads to risk-taking did not (Kingree and Thompson, 2007). In focusing on marijuana use at last intercourse, the study did not examine expectancies in relation to event-level condom use or broader patterns of sexual risk behaviors.
In addition to expectancies, intentions for sexual risk and protective behaviors are potentially relevant for studies of marijuana and HIV/STD risk. One study found that marijuana users reported reduced intentions for future condom use, which mediated the global association of marijuana use and risky sex (Brodbeck et al., 2006). Also, intentions to use marijuana during sex have been associated with intentions for unprotected sex (Kingree et al., 2000). While the correlation of marijuana use with lower intentions for condom could have several explanations, this association could be partly explained by expectancies; that is, individuals who expect that marijuana use reduces the likelihood of condom use might report behavioral intentions consistent with those expectancies. This hypothesis is consistent with health behavior theories stipulating that the influence of expectancies on behavior is mediated by intentions (Ajzen, 1991; Hennessey et al., in press).
In summary, multiple studies have reported associations of marijuana with increased sexual risk behaviors or STD incidence. Available evidence suggests that marijuana use is prevalent among adolescents involved in the juvenile justice system and could be an important cofactor for HIV/STD risk in this group. The majority of studies have evaluated global associations and utilized dichotomous measures of marijuana use; as a result, there is little information on how situational marijuana use (i.e., during sexual events) or severity of use (e.g., marijuana dependence symptoms) are related to patterns of sexual risk behavior. Additionally, few studies have evaluated relevant cognitive factors in the context of these associations. The present study evaluated global, situational and event-level associations of marijuana use and sex-related marijuana expectancies with sexual risk outcomes in a large sample of high-risk adolescents involved in the juvenile justice system. The study extends prior work by examining multiple indicators of marijuana use (including frequency, use in sexual contexts, and dependence symptoms) and sexual risk outcomes (e.g., number of sexual partners, frequency of condom use, STD diagnoses) using both cross-sectional and prospective analyses. Associations of alcohol variables with sexual risk outcomes were also examined to evaluate the possibility that marijuana use is a more robust indicator of sexual risk than alcohol use among adjudicated youth. Finally, we examined intentions for marijuana-related sexual risk behaviors in relation to sex-related marijuana expectancies and risk outcomes.
Method
Participants
Data for these analyses were taken from a larger longitudinal study assessing substance-use and sexual risk among participants (n=728) recruited from juvenile probation offices in the Denver metropolitan area. Participants who enrolled in the study completed interviews assessing substance use and sexual risk behavior at 0, 6, 12, 18 and 24-month assessment points. The present study utilized the 12- and 24-month assessments points; therefore, those participants who completed one or both of these assessments are included in these analyses (n=656).
At the 12-month assessment, participants (434 male and 222 female) were 16.71 years of age (SD=1.13; range: 14–19). The sample was ethnically diverse: 41% were Hispanic (40.9%), followed by African-American (24.5%), White (15.7%), multi-racial (11.6%), American-Indian/Alaskan Native (3.4%), an unidentified ethnicity (2.9%) and Asian/Pacific Islander (1.1%). Approximately half (53.5%) of the youth reported being on probation at the 12-month assessment; 18.7% were currently in a facility (i.e., detention, treatment, jail), and 19.5% reported having been in a facility at some point during the prior six months.
Procedures
Research staff approached potential participants in the waiting rooms of youth probation offices and provided information about a longitudinal research study about health and risk behaviors. A brief description of the study was provided to those who were interested. To be eligible to participate, individuals had to be 1) 13–18 years old, 2) currently on probation, 4) able to speak and read English, 5) be cognitively capable of understanding the assent information, and 6) have fully informed consent of a parent or legal guardian. Written informed consent was obtained from each participant and recorded verbal consent (via tape-recorded phone calls) was obtained from each parent/guardian for youth under the age of 18. Probation and juvenile justice staff had no involvement in recruitment, and participation had no impact on adolescents’ probation status. Participants received $50 for both the 12- and the 24-month assessment.
Questionnaire data were collected using Audio Computer-Assisted Self-Interviewing (ACASI) technology programmed on individual laptop computers. Questions were displayed on the computer screen while respondents heard the recorded questions over headphones. Previous experience with this high-risk population indicates that literacy can be a problem; ACASI technology eliminates many issues with comprehension and aids in navigating skip patterns (Bryan, Rocheleau, Robbins, & Hutchison, 2005; Schmiege, Broaddus, Levin, & Bryan, 2009).
Measures
Substance use and sexual risk behavior variables were assessed for the six months preceding each assessment. Sexual behavior and sexual risk variables included engaging in sexual intercourse in the prior 6 months; number of lifetime sexual partners; frequency of condom use during intercourse (never=1 to always =5); reported diagnosis of a STD; and reported HIV testing. Alcohol use variables were assessed using a measure designed for assessing drinking behavior in adolescents (White & Labouvie, 1989). Items included frequency of engaging in alcohol use (never=1 to everyday=9), typical number of drinks consumed at one time (none=1 to more than 20 drinks=10), frequency of using alcohol before intercourse (never=1 to always =5), and alcohol-use at the last sexual event (yes/no). Marijuana use variables included marijuana use (yes/no), frequency of marijuana use (occasionally to every day), frequency of using marijuana before intercourse (never=1 to always =5), and engaging in marijuana-use at the last sexual event.
Sex-Related Marijuana Expectancies
Sex-related marijuana expectancies were evaluated using an adapted measure of sex-related alcohol expectancies (Dermen & Cooper, 1994). The adapted measure was identical to the original measure except that items were modified to reflect marijuana rather than alcohol. The measure includes three subscales: sexual enhancement (e.g., “After smoking marijuana, I am more sexually responsive”), sexual risk (e.g., “After smoking marijuana, I am less likely to use birth control”), and sexual disinhibition (e.g., “After smoking marijuana, I find it hard to say no to sexual advances”). Expectancies were assessed on a 5-point scale (1=disagree a lot to 5=agree a lot), with higher numbers indicating relatively stronger expectancies about marijuana’s effects on sexual enhancement, risk or disinhibition. Inter-item correlations showed good reliability coefficients for the enhancement (α = .91), risk (α = .82) and disinhibition (α = .84) subscales.
Marijuana-Related Problems Index
Marijuana-related problems were assessed with the Rutgers Marijuana Problem Index (RMPI), which is adapted from the Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 1989). Participants rated how often they experienced various negative occurrences during the last year as a result of their smoking marijuana (e.g., “Caused shame or embarrassment to someone”). Ratings were made on a 5-point scale (1=never to 5=more than 10 times). Responses to items were dichotomized to reflect whether a given problem was endorsed or not and then summed (possible score: 0–23). The RMPI has been validated as a measure of marijuana-related problems in other studies (e.g., Simons, Correia; Carey, & Borsari, 1998; White, Labouvie, & Papadaratsakis, 2005).
Marijuana Dependence
Marijuana dependence symptoms were assessed using the Marijuana Dependence Scale (MDS; Stephens, Roffman, & Curtin, 2000), which queries DSM-IV dependence symptoms (e.g., “The need to smoke more marijuana to achieve the same high”). Symptoms were assessed over the past six months. Total scores ranged from 0–7, reflecting the number of the 7 DSM-IV symptoms endorsed.
Behavioral intentions
Three items assessed intentions for having intercourse while using marijuana (“How likely is it that you will have sex after smoking marijuana at least once in the next six months? ”), intentions for using condoms while using marijuana (“How likely is it that you will use a condom when you have been smoking marijuana?”) and global intentions for condom use (“How likely is it that you will use a condom every time you have sexual intercourse in the next six months?”). These items were rated using a 4-point scale (1=will not happen to 4=definitely will happen).
Data analysis plan
Initial analyses examined the distributional properties and descriptive characteristics of primary variables. In addition, before conducting analyses on sex-related marijuana expectancies, we evaluated whether the three-factor structure originally reported in a study of sex-related alcohol expectancies (Dermen and Cooper, 1994a) held when examining marijuana expectancies in the current sample. Primary analyses included evaluating cross-sectional (12-month) associations of a) global and situational marijuana use with sexual risk outcomes, and b) marijuana expectancies with marijuana use, behavioral intentions and sexual risk outcomes. The event-level association of marijuana use and expectancies with sexual risk behavior was evaluated using a multivariate logistic regression model predicting condom use at last intercourse. Prospective analyses examined associations of baseline marijuana use and intentions with sexual risk outcomes at the follow-up assessment. Finally, prospective analyses examined whether intentions mediated associations of expectancies with behavioral outcomes. When appropriate, alcohol use variables were included to evaluate a) whether sex-related marijuana expectancies showed discriminative associations with marijuana-related versus alcohol-related outcomes, and b) possible differences in the association of marijuana and alcohol with risk outcomes.
Results
Risk Behavior
There were sporadic missing data for various behavioral items (<2.2% per item), reflecting participants’ option to not answer particular questions. Thus, descriptive statistics reported here are based on the total number of valid responses for each item. At the 12-month assessment, 76.0% reported having sexual intercourse in the past six months and 34.3% of these individuals reported always using condoms during intercourse. A small percentage (4.9%) reported being diagnosed with an STD and nearly half (45.1%) reported being tested for HIV in the past six months. The majority of participants (66.2%) reported consuming at least one drink and these participants reported typically consuming, on average, 4–6 drinks per occasion. Over half of the participants (56.8%) reported using alcohol before having intercourse at least once in the past six months; 18.9% reported using alcohol before their last sexual event. The majority of participants (52.4%) reported smoking marijuana in the past six months; these participants reported smoking 2–3 times a week, on average, and 40.8% reported smoking every day. Additionally, half of participants (49.4%) reported using marijuana before having intercourse at least once in the past six months and 29.7% reported using marijuana at their last sexual event. On average, participants had moderate sex-related marijuana expectancies for sexual enhancement (M=2.53, SD=1.19), sexual risk (M=2.24, SD=1.13) and sexual disinhibition (M=2.09, SD=1.13). Additionally, participants who endorsed marijuana use reported a mean of 10.13 (SD=6.12) marijuana-related problems and endorsed a mean of 1.85 (SD=1.86) marijuana dependence symptoms.
Factor structure and internal consistency for sex-related marijuana expectancies
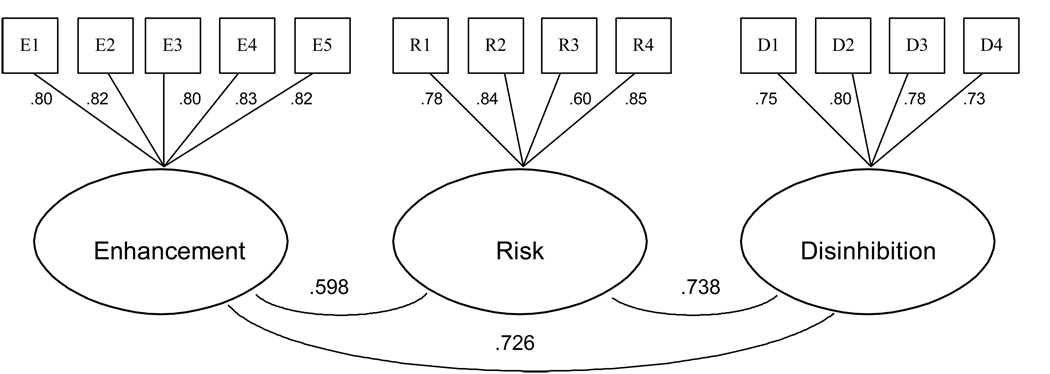
A confirmatory factor analysis (CFA) of sex-related marijuana expectancy items was conducted using structural equation modeling. This analysis included all participants with complete data on expectancy items (n= 580). The three-factor model specifying enhancement, risk and disinhibition subscales fit the data very well (χ2[62] = 244.606, p < .0001, CFI = .957, RMSEA = .073 [90% CI: .063 – .082], SRMR = .043; Figure 1). However, two prior studies that used this measure to evaluate adolescent sex-related expectancies for alcohol (Bryan et al., 2007) and marijuana (Kingree & Thompson, 2007) found evidence in favor of a two-factor structure, such that items from the disinhibition subscale did not emerge as a unique factor. Given these findings, we tested alternative two-factor models in which disinhibition items were estimated as loading on a) the enhancement factor (χ2[63] = 252.076, p < .0001, CFI = .955, RMSEA = .074 [90% CI: .064 – .083], SRMR = .088, χ2Δ[1] = 7.47, p < .05) or b) the risk factor χ2[63] = 258.406, p < .0001, CFI = .954, RMSEA = .075 [90% CI: .065 – .084], SRMR = .11, χ2Δ[1] = 13.48, p < .05. A three-factor model provided a slightly but significantly better fit compared to each of the alternative models as assessed by 1 degree of freedom χ2Δ tests for nested models comparing the alternative models to the original model. Therefore, subsequent analyses presumed a three-factor model of sex-related marijuana expectancies for this sample.
Figure 1.
Confirmatory factor model of sex-related marijuana expectancies.
Cross-sectional analyses
Using data from the 12-month assessment, cross-sectional analyses evaluated global and situational associations of marijuana use with sexual risk outcomes using linear regression. Cross-sectional associations of sex-related marijuana expectancies with marijuana variables, alcohol variables and behavioral intentions were also evaluated. Logistic regression was used for dichotomous outcomes (e.g., marijuana use and alcohol use during the most recent sexual event). For analyses on expectancies, the three subscales were evaluated separately to test the discriminative characteristics of different expectancy domains on the different outcomes. Alcohol variables, although not hypothesized to relate to marijuana-specific expectancies or risk outcomes, were included to evaluate whether sex-related marijuana expectancies showed discriminative associations with marijuana-related versus alcohol-related outcomes. Analyses that focused on marijuana use frequency included participants who reported any use in the past six months (n=316). Analyses that focused on sexual behavior included participants who reported sex in the previous six months (n = 459).
When comparing marijuana users to abstainers, those who reported any marijuana use reported a lower frequency of condom use (β = −11, p < .05) than non-users. Associations of marijuana use frequency (among those reporting any use), problems and dependence symptoms with sexual risk outcomes are presented in Table 1. Frequency of use, number of problems and number of dependence symptoms each predicted some of the risk outcomes. For example, a one-unit increase in either frequency of marijuana use or number of dependence symptoms was associated with about a 33% increase in the likelihood of marijuana use at last intercourse. Associations of sex-related marijuana expectancies with risk outcomes are shown in Table 2. Sexual enhancement expectancies showed significant, positive associations with frequency of marijuana use, marijuana use at last intercourse, and intentions to have sex while using marijuana in the future. Higher sexual risk expectancies predicted significantly lower intentions to use condoms while having sex under the influence of marijuana in the future (p = .02). Additionally, risk expectancies showed marginal associations with lower self-reported frequency of condom use (p = .09) and lower intentions for general condom use in the future (p = .06). Disinhibition expectancies were not associated with any outcomes. Thus, the general pattern of results suggested that enhancement expectancies related primarily to behaviors/intentions concerning marijuana use in sexual situations, whereas risk expectancies related primarily to behaviors/intentions for condom use. Sex-related marijuana expectancies did not show significant associations with alcohol-related outcomes, providing support for discriminant validity.
Table 1.
Cross-sectional association of marijuana use frequency, dependence symptoms and problems with sexual risk outcomes
| Frequency of condom use |
Frequency of marijuana use before sex |
Marijuana use at last intercourse |
|||||
|---|---|---|---|---|---|---|---|
| B (SE) | β | B (SE) | β | B (SE) | Exp(B) | 95% CI | |
| Frequency of use | −.04 (.03) | −.08 | .23 (.03)** | .47 | .28 (.05)** | 1.32 | 1.20 – 1.46 |
| Dependence symptoms | −.11 (.04)* | −.14 | .26 (.03)** | .34 | .33 (.06)** | 1.37 | 1.24 – 1.55 |
| Marijuana problems | −.02 (.01)* | −.11 | .06 (.01)** | .27 | .07 (.02)** | 1.07 | 1.04 – 1.11 |
Note. All variables assessed for the prior 6 months. Marijuana use at the last sexual event was evaluated using logistic regression; all other variables evaluated using linear regression.
p < .05.
p < .001
Table 2.
Cross-sectional association of sex-related marijuana expectancies with sexual risk outcomes and behavioral intentions
| Expectancy subscale | ||||||
|---|---|---|---|---|---|---|
| Enhancement | Risk | Disinhibition | ||||
| B (SE) | β/Exp(B) | B (SE) | β/Exp (B) | B (SE) |
β/Exp(B ) |
|
| Frequency of marijuana use | .29 (.14)* | .12 | .03 (.15) | .01 | .20 (.15) | .08 |
| Frequency of marijuana use during sex | .24 (.06)** | .20 | −.01 (.06) | −.01 | .06 (.06) | .04 |
| Marijuana use at last sexual event | .25 (.09)* | 1.28 | .06 (.09) | 1.07 | .12 (.09) | 1.13 |
| Frequency of condom use | .03 (.06) | .02 | −.09 (.06) | −.07 | .02 (.06) | .01 |
| Frequency of alcohol use during sex | .08 (.04) | .08 | .06 (.05) | .06 | .05 (.05) | .06 |
| Alcohol use at last sexual event | .03 (.10) | 1.03 | .09 (.10) | 1.10 | .08 (.11) | 1.08 |
| Intentions for future condom use | −.02 (.04) | −.02 | −.07 (.04) | −.08 | −.03 (.04) | −.04 |
| Intentions for having sex while using marijuana | .19 (.04)** | .20 | .03 (.04) | .03 | .07 (.04) | .07 |
| Intentions for condom use while using marijuana | .03 (.04) | .03 | −.10 (.04)* | −.10 | −.08 (.04) | −.08 |
Note. Frequency variables assessed for the past 6 months. Marijuana and alcohol use at the last sexual event evaluated using logistic regression; all other variables evaluated using linear regression.
p < .05.
p < .001
Event-level analyses
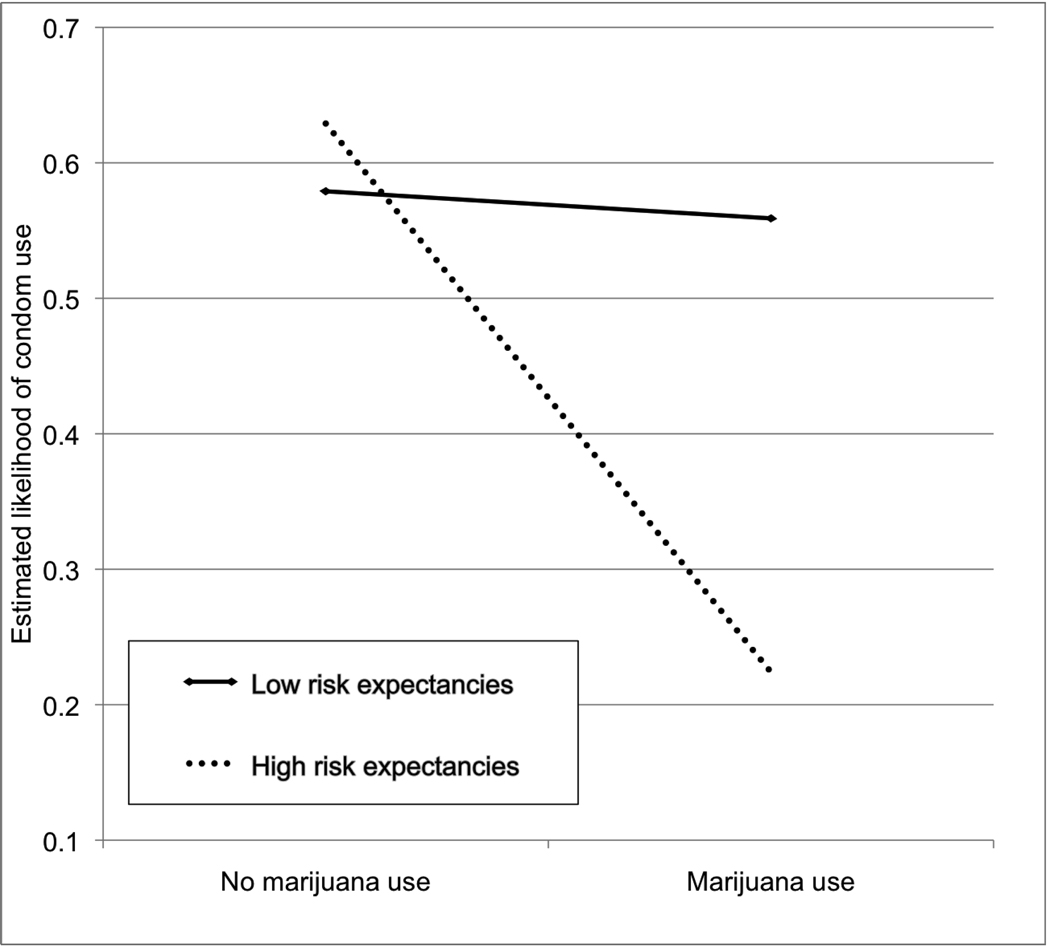
A multivariate model was used to evaluate expectancies and event-level factors as predictors of condom use at last intercourse. These analyses included 443 participants who reported having sex in the past six months, provided information on condom use at their most recent sexual event, and did not have missing data for any of the predictor variables. The model included background factors (gender and risk expectancies, entered at Step 1); situational variables (partner type, alcohol use before sex and marijuana use before sex, entered at Step 2) and interactions of event-level marijuana use with three variables (gender, partner type, and risk expectancies, entered at Step 3). Partner type at last sex was a dichotomous variable reflecting whether the event involved a steady partner (coded 0) or a new or casual partner (coded 1). With regard to expectancies, the primary analysis focused on expectancies for sexual risk because this subscale is of greatest relevance for condom use, consistent with the patterns evidenced in cross-sectional analyses. The overall model was significant (χ2 (8) = 44.87, p < .001). As depicted in Table 3, significant predictors of condom non-use included male gender and higher expectancies for sexual risk (Step 1); use of marijuana before sex and having sex with a regular partner (Step 2); and the interaction of marijuana use with expectancies (Step 3). With the interaction terms included in the model, the effect of risk expectancies remained significant (p < .001) whereas the effect of marijuana use did not (p = .86). A plot of the interaction showed that marijuana use was associated with a lower likelihood of condom use for individuals high in risk expectancies, but not those low in expectancies (Figure 1). To estimate the likelihood of condom use as a function of high versus low expectancies, we re-estimated the model separately for individuals above and below the median for risk expectancies. For adolescents with low expectancies, the likelihood of condom use at last intercourse was not significantly different for those who reported marijuana use (27%) and those who did not (Exp(B) = 1.22; 95% CI = .85 – 1.74; p = .29). For participants with high expectancies, those who used marijuana at last sexual intercourse (31%) were about half as likely to report having used a condom compared to those who did not use marijuana (Exp(B) = .47, 95% CI = .34 – .66; p < .001).
Table 3.
Logistic regression model predicting condom use at last intercourse.
| B (SE) | Exp (B) | 95% CI | p | ||
|---|---|---|---|---|---|
| Step 1 | Gender | .31 (.10) | 1.36 | 1.12 – 1.66 | .003 |
| Sex-related marijuana expectancies | −.18 (.09) | 0.84 | .71 − .1.0 | .045 | |
| Step 2 | Partner type | .56 (.23) | 1.74 | 1.11 – 2.74 | .016 |
| Alcohol use prior to sex | −.12 (.27) | 0.89 | 0.52 – 1.50 | .653 | |
| Marijuana use prior to sex | −.33 (.12) | 0.72 | 0.57 – 0.91 | .005 | |
| Step 3 | Marijuana use × gender | .08 (.13) | 1.08 | 0.84 – 1.39 | .559 |
| Marijuana use × partner type | −.24 (.25) | 0.79 | 0.49 – 1.29 | .342 | |
| Marijuana use × expectancies | −.47 (.12) | 0.63 | 0.49 – 0.79 | <.001 |
Note. Step 1: χ2 = 12.36, p = .002; Step 2: χ2 = 13.09, p =.004; Step 3: χ2 = 19.41; p < .001. Gender coded 1 = Female, 2 = Male. Sex-related marijuana expectancies: Risk subscale. Partner type coded 1 = Regular, 2 = Casual or stranger. Alcohol and marijuana use prior to sex coded 0 = No, 1 = Yes.
To evaluate whether other expectancy domains showed associations with event-level condom use, the model was re-estimated by substituting main effect and interaction terms for risk expectancies with those for enhancement and disinhibition expectancies. Enhancement expectancies showed no direct or interactive effects on condom use (ps > .05). Disinhibition expectancies had no direct association with condom use at Step 1 (B = −.08, SE = .09, p = .38), but interacted with marijuana use to predict condom use at Step 3 (B = −.23, SE = .11, p = .042). Examination of the interaction plot showed the same pattern as was evident for risk expectancies. When the model was estimated separately among individuals above and below the median score for disinhibition expectancies, there was no association of marijuana use with condom use among participants with low expectancies (24% reported marijuana use; Exp(B) = 1.09, 95% CI = .76–1.55, p = .65). Among participants with high expectancies, those who reported using marijuana (33%) were approximately half as likely to report using a condom (Exp(B) = .55, 95% CI = .40 – .75) compared to those who did not.
Prospective associations of marijuana use and intentions with sexual risk outcomes
In prospective analyses, marijuana use, expectancies, dependence symptoms, and intentions (assessed at 12 months) were examined in relation to sexual risk outcomes (assessed at 24-months). These analyses were conducted to evaluate prospective associations of marijuana use with sexual behavior, as well as prospective associations of marijuana-related sexual risk intentions with behavioral outcomes. These analyses included 279 participants who provided relevant data at 12 months and who reported sexual intercourse in the past 6 months at follow-up. Outcomes included frequency of condom use, marijuana/alcohol use during sex, number of sexual partners, and whether participants reported diagnosis of a sexually transmitted disease (STD) at follow-up. Any marijuana use, frequency of use (among users), dependence symptoms and marijuana problems at 12 months were each significantly predictive of frequency of marijuana use during sex at 24 months. A higher number of dependence symptoms and problems predicted lower condom use, and frequency of marijuana use predicted the likelihood of a self-reported STD at follow-up (Table 4).
Table 4.
Prospective association of marijuana use with sexual risk outcomes.
| 12-month marijuana use | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Any marijuana use | Frequency of marijuana use |
Marijuana use prior to sex |
Dependence symptoms |
Marijuana Problems | ||||||
| 24-month outcomes | B (SE) | β/ExpB | B (SE) | β/ExpB | B (SE) | β/ExpB | B (SE) | β/ExpB | B (SE) | β/ExpB |
| Frequency of condom use | −.18 (.16) | −.06 | −.02 (.04) | −.05 | −.01 (.06) | −.01 | −.10 (.04)* | −.12 | −.04 (.01)* | −.17 |
| Marijuana use prior to sex | .84 (.14)** | .32 | .14 (.03)** | .30 | - | - | .17 (.04)** | .23 | .04 (.01)** | .20 |
| Number of sexual partners | 2.54 (2.06) | .07 | −.46 (.65) | −.06 | .09 (.84) | .01 | .32 (.58) | .03 | −.11(.16) | −.04 |
| STD diagnosis† | .32 (.30) | 1.39 | .21 (.09)* | 1.23 | .11 (.11) | 1.11 | .02 (.08) | 1.02 | .01 (.02) | 1.01 |
Note. Logistic regression (Exp(B) reported).
p < .05
p < .001
Prospective analyses also examined associations of 12-month intentions (for sex-related marijuana use, marijuana-related condom use and general condom use) with a) frequency of marijuana use during intercourse and b) frequency of condom use at 24 months. Results indicated that 12-month intentions for marijuana use during sex significantly predicted frequency of marijuana use during sex during the follow-up period (B (SE) = .47 (.06), β= .38, p < .001). Also, marijuana-specific condom use intentions (B (SE) = .42 (.07), β= .33, p < .001) and general condom use intentions (B (SE) = .45 (.07), β= .33, p < .001) were significant predictors of frequency of condom use at 24 months.
Mediation tests for marijuana-related expectancies, intentions and sexual risk behaviors
Additional analyses evaluated whether behavioral intentions mediated associations of expectancies (assessed at 12 months) with risk outcomes at 24 months. Two mediation models were tested. In the first model, intentions for marijuana-related sex were evaluated as mediating the association of enhancement expectancies with frequency of marijuana use during sex. In the second model, intentions for condom use during marijuana events were evaluated as mediating the association of risk expectancies with frequency of condom use. Consistent with health behavior models such as the Theory of Planned Behavior (Ajzen, 1991), we utilized selected intentions items so that the measure of intentions and measure of behavior were focused on the exact same behavior.
Each mediation model consisted of a two-part linear regression analysis in which a) intentions were regressed on expectancies, and b) sexual risk outcomes were regressed on intentions while controlling for expectancies. Following procedures outlined by Preacher and Hayes (2004), Sobel tests were used to estimate the significance of the indirect effect, ab, which denotes the product of coefficients of the paths from the independent variable to the mediator (a) and the mediator to the outcome variable (b). Because ab typically shows non-normal distributions, bootstrap resampling was used as an additional nonparametric approach for testing significance of indirect effects (Preacher & Hayes, 2004); 95% confidence intervals for ab were estimated using 1000 bootstrap resamples. Model 1 supported intentions as mediating the association of enhancement expectancies with frequency of marijuana use during sex, with Sobel tests indicating a significant indirect effect, ab = .085 (95% CI = .035 – .135), SE = .03, p = .001 (n = 323). The indirect effect for model 2 fell short of significance, ab = −.039 (95% CI = −.079 – .002), SE = .02, p = .065 (n = 316). Using bootstrap resampling the estimates of these effects were virtually identical. Thus, mediation analyses indicated that intentions partly mediated the influence of marijuana-related sexual enhancement expectancies, but not marijuana-related risk expectancies, on marijuana-related sexual risk outcomes.
Discussion
Health risks associated with marijuana use have not been studied extensively in comparison to the literature on alcohol-related health outcomes (Cunningham, Bondy, & Walsh, 2000; Hall & Babor, 2000). However, reported associations of marijuana use with sexual risk behaviors or STD diagnoses, particularly in adolescent samples, suggest the possibility that marijuana is an important cofactor for HIV/STD risk. This study evaluated global, situational and event-level associations of marijuana use with sexual risk behaviors in a sample of high-risk adolescents. Frequency of marijuana use and number of dependence symptoms each predicted a higher frequency of marijuana use before sex and lower rates of condom use in cross-sectional analyses. Prospective analyses spanning a one-year follow-up period showed that a higher number of dependence symptoms predicted lower rates of condom use, while higher frequency of use was associated with a higher likelihood of STD diagnoses. Event-level analyses showed that marijuana use was associated with a significantly decreased likelihood of condom use at last intercourse, whereas alcohol use was not. Overall, these findings provide further evidence that marijuana use is a potentially important marker for HIV/STD risk among high-risk youth.
Among the main goals of this study was to evaluate sex-related marijuana expectancies as a cognitive factor that could be relevant for predicting marijuana use and related sexual risk behaviors. A validated measure of sex-related alcohol expectancies (Dermen & Cooper, 1994a) showed good psychometric properties when adapted to assess marijuana expectancies in this sample. Evidence also suggested differential associations of expectancy subscales with specific risk outcomes, providing preliminary evidence of discriminant validity in predicting marijuana-related risk-taking. Stronger expectancies that marijuana facilitates sexual enhancement predicted more frequent marijuana use (but not alcohol use) in sexual contexts, whereas expectancies that marijuana leads to unsafe sex predicted a significantly lower likelihood of condom use at last intercourse. Moreover, risk and disinhibition expectancies interacted with marijuana use to predict condom use at the event level. This result parallels findings concerning interactions of sex-related alcohol expectancies with alcohol use in predicting event-level condom use (e.g., Bryan et al., 2007; Corbin & Fromme, 2000; Dermen, Cooper, & Agocha, 1998). Therefore, sex-related marijuana expectancies appear relevant for characterizing marijuana-related sexual risk behavior.
Behavioral intentions also showed significant associations with expectancies and risk outcomes. To our knowledge, this is the first study to report on intentions for sexual risk and protective behaviors specifically in the context of marijuana use. Intentions for marijuana use in sexual situations were associated with enhancement expectancies and, in prospective analyses, frequency of marijuana use during sex. Additionally, intentions for condom use during marijuana-related sexual events were associated with risk expectancies and with frequency of condom use at 24 months. Mediation tests showed that intentions to use marijuana in sexual contexts accounted for a significant indirect effect of enhancement expectancies on future marijuana use in sexual situations. These findings provide preliminary evidence that sex-related expectancies may predict risk behavior through behavioral intentions, consistent with social-cognitive theories (Ajzen, 1991), and suggest a possible explanation for reported associations of marijuana use with reduced condom use intentions (e.g., Brodbeck et al., 2006).
Despite increasing evidence for covariation of marijuana use and sexual risk outcomes, it is important to note that most studies have relied on global association analyses, which have significant limitations in terms of inferring causal associations. The joint use of global, situational and event-level approaches in the current study allowed a relatively more comprehensive assessment than has been typical in most studies. In particular, event-level assessments are an important adjunct to association analyses in that they can allow greater precision in evaluating temporal associations of substance use with risk-taking. Notably, analyses in this study and two others (Kingree et al., 2000; Kingree & Betz, 2003) converge to support an event-level association of marijuana use with condom nonuse in high-risk adolescents. Additionally, evidence for convergent findings across different survey methods in the current study provides support for the possibility that marijuana use could show consistent associations with HIV risk behavior in at-risk adolescents.
Although causal effects of marijuana on sexual risk-taking are possible, existing studies cannot rule out the possibility that associations of marijuana and sexual behavior are attributable to individual difference factors that correlate with both outcomes. The high co-occurrence of sexual risk-taking and other externalizing behaviors among adjudicated adolescents (Bryan & Stallings, 2002; Malow et al., 2006) is likely to partly reflect common biological and behavioral vulnerability factors, for instance, those predisposing toward a general tendency for behavioral disinhibition (c.f. Young et al., 2009). Further, trait characteristics related to disinhibition are hypothesized to influence the acquisition and development of drug-related expectancies (McCarthy, Kroll, & Smith, 2001; Simons et al., 2009). An implication is that future studies evaluating marijuana and sexual risk behavior should examine the influence of individual difference factors (e.g., behavioral disinhibition and related traits) as they relate to associations among marijuana use, sexual risk and drug-related expectancies.
Given the limitations of global and situational analyses, another important direction is to incorporate approaches in which risk-taking behaviors are assessed following random assignment to active drug versus control conditions. This strategy has been fruitful in evaluating effects of acute alcohol intoxication on theoretical antecedents of sexual risk behavior in controlled settings (Hendershot & George, 2007; Maisto et al., 2002). Although experimental studies of marijuana and risk-taking behavior are relatively few, acute administration of Δ9-THC has been associated with increased risk-taking in decision-making tasks (Lane, Cherek, Tcheremissine, Lieving, & Pietras, 2005; Lane, Yechiam, & Busemeyer, 2006). Furthermore, functional imaging studies suggest that both chronic marijuana use and acute Δ9-THC administration predict differences in regional cerebral blood flow during resting conditions, as well as differential activation in functionally relevant regions during neurocognitive tasks requiring attentional control and response inhibition (for reviews see Chang & Chronicle, 2007; Martín-Santos et al., 2010). Neurobiological mechanisms implicated in acute and chronic effects of Δ9-THC on inhibitory control and decision-making are potentially relevant for studying associations of marijuana with sexual decision-making.
Randomized studies could also be important for evaluating effects of marijuana expectancies on risk-taking through manipulation of expectancy set. For example, increased risk-taking in response to marijuana placebo would strengthen the argument that expectancies can steer behavior. Consistent with this approach, a recent experimental study showed that implicit marijuana primes influenced cognitive processing among individuals who had high baseline expectancies that marijuana leads to cognitive impairment (Hicks, Pedersen, McCarthy, & Friedman, 2009). Similarly, activation of alcohol expectancies by way of implicit primes or placebo manipulations has led to increases in sexual interest (Friedman, McCarthy, Förster, & Denzler, 2005; George et al., 2000) or decreases in safe sex behaviors (Maisto et al., 2002). While the aforementioned studies of marijuana and risk-taking (e.g., Lane et al., 2005) did not manipulate expectancy set, the recent adaptation of the balanced placebo design in marijuana administration paradigms (Metrik et al., 2009) suggests that such studies will be possible.
There have been few published intervention trials that target both sexual risk behavior and substance use in non-treatment seeking samples (Bryan, Schmiege, & Broaddus, 2009). Interventions explicitly targeting marijuana-related sexual risk and have not, to our knowledge, been reported. However, this study and others with adjudicated youth (Kingree & Betz, 2003; Malow et al., 2001; Teplin et al., 2003) offer convergent evidence that, relative to alcohol, marijuana is potentially more prevalent and more predictive of condom non-use at the event level. While these findings have yet to be widely replicated, they offer a provisional rationale for the inclusion of marijuana-specific content in HIV/STD risk reduction interventions for high-risk youth. Given the feasibility of incorporating alcohol-specific sexual risk content in theory-based HIV/STD interventions for juvenile offenders (Bryan, et al., 2009; Schmiege et al., 2009), incorporating marijuana content in similar trials represents a possible next step. The present findings further suggest that interventions could benefit from including content on sex-related marijuana expectancies or by targeting individuals with stronger expectancies.
The current findings should be taken in context with the limitations of this study. A limitation of the event-level analyses was the focus on a single sexual event, whereas assessment of multiple sexual events can facilitate within-subjects analyses (e.g., Weinhardt & Carey, 2000). Thus, future studies would benefit from multiple-event assessments. Our examination of sex-related marijuana expectancies presumed that these expectancies operate similarly to sex-related alcohol expectancies. Although an alcohol expectancy measure showed stable psychometric properties and predictive validity when adapted for marijuana in this study, the extent to which sexuality-specific expectancy domains for alcohol and marijuana coincide is unknown. Future studies could use qualitative methods to identify sex-related marijuana expectancy domains that might not be reflected by the measure used in this study. Although our focus on a highly vulnerable population engaging in high rates of marijuana use and risky sexual behavior is important, there are some limitations to this approach. First, it is not clear that our findings regarding the associations of marijuana use and sexual risk would generalize to other adolescents. Second, this is a sample of supervised adolescents in that they were on probation for at least some portion of the time during the study, which could have influenced their substance use (Feldstein Ewing, Schmiege, & Bryan, 2010). Therefore, patterns of substance use reported by participants could differ from patterns of use in other contexts. Another possible limitation concerns the use of ordinal measures, as opposed to frequency counts, for assessing substance use. Advantages of this study include the use of a large, racially diverse sample, the incorporation of cross-sectional and prospective data, and the examination of marijuana variables with sexual risk variables at multiple levels of analysis. Additionally, we evaluated specific behaviors (e.g., condom nonuse; marijuana use prior to sex; number of sexual partners) that might partly account for associations of marijuana use with STD risk.
The current findings extend prior research by examining associations of marijuana use and sex-related marijuana expectancies with HIV/STD risk behavior in a sizable sample of adjudicated youth. The results of this study converge with prior reports suggesting that marijuana use is a likely marker for HIV/STD risk, particularly in high-risk adolescent populations. The present findings further suggest that associations of marijuana use and sexual risk behavior can be moderated by individual difference variables, including marijuana expectancies. Broader dispositional factors, including those related to behavioral disinhibition, could also be relevant for characterizing these associations. The use of methodological approaches that account for possible confounds related to individual difference variables will be important for addressing the possibility of causal associations of marijuana with sexual risk outcomes in future studies.
Figure 2.
Estimated likelihood of condom use at last intercourse as a function of event-level marijuana use and sex-related marijuana expectancies
Acknowledgments
This research was supported by grants R01DA019139 from the National Institute on Drug Abuse and F32AA018629 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
References
- Adefuye AS, Abiona TC, Balogun JA, Lukobo-Durrell M. HIV sexual risk behaviors and perception of risk among college students: Implications for planning interventions. BMC Public Health. 2009;9:281. doi: 10.1186/1471-2458-9-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Bellis MA, Hughes K, Calafat A, Juan M, Ramon A, Rodriguez JA, et al. Sexual uses of alcohol and drugs and the associated health risks: A cross sectional study of young people in nine European cities. BMC Public Health. 2008;8:155. doi: 10.1186/1471-2458-8-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyer CB, Shafer MA, Teitle E, Wibbelsman CJ, Seeberg D, Schachter J. Sexually transmitted diseases in a health maintenance organization teen clinic: Associations of race, partner's age, and marijuana use. Archives of Pediatrics & Adolescent Medicine. 1999;153:838–844. doi: 10.1001/archpedi.153.8.838. [DOI] [PubMed] [Google Scholar]
- Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS and Behavior. 2006;10:599–605. doi: 10.1007/s10461-006-9103-9. [DOI] [PubMed] [Google Scholar]
- Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: Findings from an event-level study. Addictive Behaviors. 2007;32:2940–2952. doi: 10.1016/j.addbeh.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan A, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2007;68:327–335. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- Bryan A, Rocheleau CA, Robbins RN, Hutchison KE. Condom use among high-risk adolescents: Testing the influence of alcohol use on the relationship of cognitive correlates of behavior. Health Psychology. 2005;24:133–142. doi: 10.1037/0278-6133.24.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Broaddus MR. HIV/STD risk reduction among detained adolescents: A randomized controlled trial. Pediatrics. 2009;124:e1180–e1188. doi: 10.1542/peds.2009-0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan A, Stallings MC. A case control study of adolescent risky sexual behavior and its relationship to personality dimensions, conduct disorder, and substance use. Journal of Youth and Adolescence. 2002;31:387–396. [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: U.S. Department of Health and Human Services; HIV/AIDS Surveillance Report, 2004. 2005;16 Also available at: http://www.cdc.gov/hiv/stats/hasrlink.htm.
- Centers for Disease Control and Prevention. Atlanta, GA: U.S. Department of Health and Human Services; Sexually Transmitted Disease Surveillance, 2008. 2009 Also available at: http://www.cdc.gov/std/stats08/main.htm.
- Chang L, Chronicle EP. Functional imaging studies in cannabis users. The Neuroscientist. 2007;13:422–432. doi: 10.1177/1073858406296601. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol. 2002;14 Suppl:101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Current Directions in Psychological Science. 2006;15:19–23. [Google Scholar]
- Corbin WR, Fromme K. Alcohol use and serial monogamy as risks for sexually transmitted diseases in young adults. Health Psychology. 2002;21:229–236. doi: 10.1037//0278-6133.21.3.229. [DOI] [PubMed] [Google Scholar]
- Crosby RA, DiClemente RJ, Wingood GM, Rose E, Lang D. Correlates of continued risky sex among pregnant African American teens: Implications for STD prevention. Sexually Transmitted Diseases. 2003;30:57–63. doi: 10.1097/00007435-200301000-00012. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Bondy SJ, Walsh GW. The risks of cannabis use: evidence of a dose-response relationship. Drug and Alcohol Review. 2000;19:137–142. [Google Scholar]
- De Genna NM, Cornelius MD, Cook RL. Marijuana use and sexually transmitted infections in young women who were teenage mothers. Womens Health Issues. 2007;17:300–309. doi: 10.1016/j.whi.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: I. Scale development. Psychology of Addictive Behaviors. 1994a;8:152–160. [Google Scholar]
- Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: II. Prediction of drinking in social and sexual situations. Psychology of Addictive Behaviors. 1994b;8:161–168. [Google Scholar]
- Dermen KH, Cooper ML, Agocha VB. Sex-related alcohol expectancies as moderators of the relationship between alcohol use and risky sex in adolescents. Journal of Studies on Alcohol. 1998;59:71–77. doi: 10.15288/jsa.1998.59.71. [DOI] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Schmiege SJ, Bryan AD. The influence of externalizing on substance use trajectories among justice-involved adolescents. Manuscript under review. 2010 [Google Scholar]
- Friedman RS, McCarthy DM, Förster J, Denzler M. Automatic effects of alcohol cues on sexual attraction. Addiction. 2005;100:672–681. doi: 10.1111/j.1360-0443.2005.01056.x. [DOI] [PubMed] [Google Scholar]
- Gaher RM, Simons JS. Evaluations and expectancies of alcohol and marijuana problems among college students. Psychology of Addictive Behaviors. 2007;21:545–554. doi: 10.1037/0893-164X.21.4.545. [DOI] [PubMed] [Google Scholar]
- George WH, Stoner SA, Norris J, Lopez PA, Lehman GL. Alcohol expectancies and sexuality: A self-fulfilling prophecy analysis of dyadic perceptions and behavior. Journal of Studies on Alcohol. 2000;61:168–176. doi: 10.15288/jsa.2000.61.168. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ, Nichols TR. Effects of a school-based drug abuse prevention program for adolescents on HIV risk behavior in young adulthood. Prevention Science. 2006;7:103–112. doi: 10.1007/s11121-006-0025-6. [DOI] [PubMed] [Google Scholar]
- Guo JT, Stanton B, Clemens RL, Li X, Harris C, Marshall S, et al. Substance use among rural adolescent virgins as a predictor of sexual initiation. Journal of Adolescent Health. 2005;37:252–255. doi: 10.1016/j.jadohealth.2004.11.124. [DOI] [PubMed] [Google Scholar]
- Hall W, Babor TF. Cannabis use and public health: Assessing the burden. Addiction. 2000;95:485–490. doi: 10.1046/j.1360-0443.2000.9544851.x. [DOI] [PubMed] [Google Scholar]
- Hammett TM, Gaiter JL, Crawford C. Reaching seriously at-risk populations: Health interventions in criminal justice settings. Health Education & Behavior. 1998;25:99–120. doi: 10.1177/109019819802500108. [DOI] [PubMed] [Google Scholar]
- Hendershot CS, George WH. Alcohol and sexuality research in the AIDS era: Trends in publication activity, target populations and research design. AIDS and Behavior. 2007;11:217–226. doi: 10.1007/s10461-006-9130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessy M, Bleakley A, Fishbein M, Brown L, DiClemente R, Romer D, et al. Differentiating between precursor and control variables when analyzing reasoned action theories. AIDS and Behavior. doi: 10.1007/s10461-009-9560-z. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks JA, Pedersen SL, McCarthy DM, Friedman RS. Marijuana primes, marijuana expectancies, and arithmetic efficiency. Journal of Studies on Alcohol and Drugs. 2009;70:391–399. doi: 10.15288/jsad.2009.70.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingree JB, Betz H. Risky sexual behavior in relation to marijuana and alcohol use among African-American, male adolescent detainees and their female partners. Drug and Alcohol Dependence. 2003;72:197–203. doi: 10.1016/s0376-8716(03)00196-0. [DOI] [PubMed] [Google Scholar]
- Kingree JB, Braithwaite R, Woodring T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. Journal of Adolescent Health. 2000;27:179–185. doi: 10.1016/s1054-139x(00)00101-4. [DOI] [PubMed] [Google Scholar]
- Kingree JB, Thompson M. Sexually-related expectancies for alcohol use and marijuana use among juvenile detainees. Addictive Behaviors. 2007;32:1936–1942. doi: 10.1016/j.addbeh.2006.12.020. [DOI] [PubMed] [Google Scholar]
- Lane SD, Cherek DR, Tcheremissine OV, Lieving LM, Pietras CJ. Acute marijuana effects on human risk taking. Neuropsychopharmacology. 2005;30:800–809. doi: 10.1038/sj.npp.1300620. [DOI] [PubMed] [Google Scholar]
- Lane SD, Yechiam E, Busemeyer JR. Application of a computational decision model to examine acute drug effects on human risk taking. Experimental and Clinical Psychopharmacology. 2006;14:254–264. doi: 10.1037/1064-1297.14.2.254. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. Journal of Studies on Alcohol. 2002;63:476–485. doi: 10.15288/jsa.2002.63.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malow RM, Devieux JG, Jennings T, Lucenko BA, Kalichman SC. Substance-abusing adolescents at varying levels of HIV risk: Psychosocial characteristics, drug use, and sexual behavior. Journal of Substance Abuse. 2001;13:103–117. doi: 10.1016/s0899-3289(01)00069-4. [DOI] [PubMed] [Google Scholar]
- Malow RM, Rosenberg R, Donenberg G, Dévieux JG. Interventions and patterns of risk inadolescent HIV/AIDS prevention. American Journal of Infectious Diseases. 2006;2:80–89. doi: 10.3844/ajidsp.2006.80.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-Santos R, Fagundo AB, Crippa JA, Atakan Z, Bhattacharyya S, et al. Neuroimaging in cannabis use: A systematic review of the literature. Psychological Medicine. 2010;40:383–398. doi: 10.1017/S0033291709990729. [DOI] [PubMed] [Google Scholar]
- McCarthy DM, Kroll LS, Smith GT. Integrating disinhibition and learning risk for alcohol use. Experimental and Clinical Psychopharmacology. 2001;9:389–398. doi: 10.1037//1064-1297.9.4.389. [DOI] [PubMed] [Google Scholar]
- Mertz KJ, Finelli L, Levine WC, Mognoni RC, Berman SM, Fishbein M, et al. Gonorrhea in male adolescents and young adults in Newark, New Jersey: Implications of risk factors and patient preferences for prevention strategies. Sexually Transmitted Diseases. 2000;27:201–207. doi: 10.1097/00007435-200004000-00004. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Geisner IM, Lee CM. Perceived marijuana norms and social expectancies among entering college student marijuana users. Psychology of Addictive Behaviors. 2008;22:433–438. doi: 10.1037/0893-164X.22.3.433. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods Instruments & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Robbins RN, Bryan A. Relationships between future orientation, impulsive sensation seeking, and risk behavior among adjudicated adolescents. Journal of Adolescent Research. 2004;19:428–445. doi: 10.1177/0743558403258860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmiege SJ, Broaddus MR, Levin M, Bryan AD. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. Journal of Consulting and Clinical Psychology. 2009;77:38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scivoletto S, Tsuji RK, Najjar CH, de Queiroz S, de Andrade AG, Gattaz WF. Use of psychoactive substances and sexual risk behavior in adolescents. Substance Use & Misuse. 2002;37:381–398. doi: 10.1081/ja-120002484. [DOI] [PubMed] [Google Scholar]
- Shrier LA, Emans J, Woods ER, DuRant RH. The association of sexual risk behaviors and problem drug behaviors in high school students. Journal of Adolescent Health. 1997;20:377–383. doi: 10.1016/S1054-139X(96)00180-2. [DOI] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Sternberg M, Beardslee WR. Associations of depression, self-esteem, and substance use with sexual risk among adolescents. Preventive Medicine. 2001;33:179–189. doi: 10.1006/pmed.2001.0869. [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology. 1998;45:265–273. [Google Scholar]
- Simons JS, Dvorak RD, Lau-Barraco C. Behavioral inhibition and activation systems: Differences in substance use expectancy organization and activation in memory. Psychology of Addictive Behaviors. 2009;23:315–328. doi: 10.1037/a0015834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AMA, Ferris JA, Simpson JM, Shelley J, Pitts MK, Richters J. Cannabis use and sexual health. The Journal of Sexual Medicine. doi: 10.1111/j.1743-6109.2009.01453.x. (in press) [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Sumnall HR, Beynon CM, Conchie SM, Riley SCE, Cole JC. An investigation of the subjective experiences of sex after alcohol or drug intoxication. Journal of Psychopharmacology. 2007;21:525–537. doi: 10.1177/0269881106075590. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Mericle AA, McClelland GM, Abram KM. HIV and AIDS risk behaviors in juvenile detainees: Implications for public health policy. American Journal of Public Health. 2003;93:906–912. doi: 10.2105/ajph.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW, Papadaratsakis V. Changes in substance use during the transition to adulthood: A comparison of college students and their noncollege age peers. Journal of Drug Issues. 2005;35:281–305. [Google Scholar]
- Wingood GM, DiClemente RJ. The influence of psychosocial factors, alcohol, drug use on African-American women’s high-risk sexual behavior. American Journal of Preventive Medicine. 1998;15:54–59. doi: 10.1016/s0749-3797(98)00027-0. [DOI] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL, Patkar AA, Hubbard RL, Blazer DG. Association of MDMA/ecstasy and other substance use with self-reported sexually transmitted diseases among college-aged adults: A national study. Public Health. 2009;123:557–564. doi: 10.1016/j.puhe.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan AF, Chiu YW, Stoesen CA, Wang MQ. STD-/HIV-Related sexual risk behaviors and substance use among US rural adolescents. Journal of the National Medical Association. 2007;99:1386–1394. [PMC free article] [PubMed] [Google Scholar]
- Young SE, Friedman NP, Miyake A, Willcutt EG, Corley RP, Haberstick BC, Hewitt JK. Behavioral disinhibition: Liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. Journal of Abnormal Psychology. 2009;118:117–130. doi: 10.1037/a0014657. [DOI] [PMC free article] [PubMed] [Google Scholar]