Abstract
The paired-like homeobox 2B gene (PHOX2B) is the disease-defining gene for congenital central hypoventilation syndrome (CCHS). Individuals with CCHS typically present in the newborn period with alveolar hypoventilation during sleep and often during wakefulness, altered respiratory control including reduced or absent ventilatory responses to hypercarbia and hypoxemia, and autonomic nervous system (ANS) dysregulation; however, a subset of individuals present well into adulthood. Thermoregulation is altered and perception of shortness of breath is absent, but voluntary breathing is retained. Structural and functional magnetic resonance imaging (MRI) and limited post-mortem studies in subjects with CCHS reveal abnormalities in both forebrain and brainstem. MRI changes appear in the hypothalamus (responsible for thermal drive to breathing), posterior thalamus and midbrain (mediating O2 and oscillatory motor patterns), caudal raphé and locus coeruleus (regulating serotonergic and noradrenergic systems), the lateral medulla, parabrachial pons, and cerebellum (coordinating chemoreceptor and somatic afferent activity with breathing), and insular and cingulate cortices (mediating shortness of breath perception). Structural and functional alterations in these sites may result from PHOX2B mutations or be secondary to hypoxia/perfusion alterations from suboptimal management/compliance. The study of CCHS, with collaboration between physician-scientists and basic scientists, offers a rare opportunity to investigate control of breathing within the complex physiological network of the ANS.
Keywords: Congenital Central Hypoventilation Syndrome (CCHS), Control of breathing disorders, PHOX2B gene, Autonomic dysregulation
1. Introduction
Congenital Central Hypoventilation Syndrome (CCHS), first described in 1970 (Mellins et al., 1970), is a prototypical example of respiratory control disorders occurring with related autonomic nervous system dysregulation (ANSD). This unique and growing group of rare diseases termed respiratory and autonomic disorders of infancy, childhood, and adulthood (RADICA; Weese-Mayer et al., 2009), has served to broaden our understanding of respiratory and autonomic function and developmental changes from infancy through adulthood. Improved non-invasive monitoring technologies, advances in providing respiratory support, and increased awareness of autonomic medicine have improved care for and study of individuals with RADICA; this includes the ability to perform end tidal CO2 monitoring, portable pocket-sized pulse oximetry, beat-to-beat blood pressure measures, continuous temperature recording, smaller home ventilators, and even minimally invasive thoracoscopic diaphragm pacer implantation. Collectively, these disorders share the risk of sudden death, altered neurocognitive outcomes, and varied long-term quality of life. The study of RADICA, with collaboration between physician-scientists and basic scientists, offers a rare opportunity to investigate control of breathing within the complex physiological network of the autonomic nervous system (ANS).
The CCHS phenotype offers a unique model for elucidation of a variety of crucial processes, including interactions between behavioral states and control of breathing, anatomic sites of central chemoreception, and integration of ancillary drives to breathing processes. Specifically, the study of individuals with CCHS offers a means to determine if the observed chemosensory impairment results from a deficit in sensory input processes, integration of sensory input with respiratory motor output, brain processes that mediate influences of quiet versus active sleep on brainstem respiratory rhythm generators, or a combination of all these processes. Research in this disorder may also guide identification of anatomic sites contributing to affective drive in shortness of breath. Identifying deficient autonomic regulatory sites and understanding dysfunctional interactive processes binding respiratory and autonomic regulatory areas would also help expose essential mechanisms underlying integration of cardiovascular and respiratory functions. The multiple processes that contribute to breathing, combined with the widespread nature of involved brain sites responsive to the principal drive of CO2 (Nattie and Li, 2009; Teppema and Dahan, 2005; Williams et al., 2007), indicate that no single brain locus is responsible for respiratory dysfunction. Collectively, CCHS patients who have been diagnosed early and optimally managed offer a singular opportunity to understand crucial elements of respiratory and autonomic regulation.
2. Background
CCHS, first characterized by Mellins et al. (1970), was described primarily as case reports as CCHS-focused care at major medical centers did not become prominent until decades later. Familial cases of CCHS, association with disorders of anatomic ANS development (aganglionosis of the distal intestine, i.e., Hirschsprung disease, and neural crest tumors), and consideration of candidate genes in animal models helped refine the search for genetic causes (Weese-Mayer et al., 2009). In 2003, the paired-like homeobox 2B gene (PHOX2B), which encodes a homeodomain transcription factor with an important role in murine ANS reflex circuit development (Pattyn et al., 1997, 1999), was identified as the disease-defining gene for CCHS (Amiel et al., 2003; Matera et al., 2004; Sasaki et al., 2003; Weese-Mayer et al., 2003). PHOX2B has been shown to determine eventual cell fate as a sympathetic, parasympathetic, or enteric neuron. Located at 4p12, PHOX2B normally contains a 20 alanine repeat sequence on exon 3; so an unaffected individual would have the PHOX2B genotype denoted as 20/20, reflecting the normal number of alanines on each allele. However, individuals with CCHS are heterozygous for a PHOX2B mutation. The specificity of the association between mutations in the PHOX2B gene and the CCHS phenotype is supported by Hung et al. (2007), who failed to identify PHOX2B mutations in ~2000 Taiwanese controls. The majority (90-92%) of individuals with CCHS have a polyalanine repeat expansion mutation (PARM) in the PHOX2B gene (Weese-Mayer et al., 2009). For those CCHS patients with PARMs, the number of polyalanine repeats on the affected allele range from 24 to 33 repeats. In addition, PHOX2B alterations including missense, nonsense, and frameshift mutations, termed non-polyalanine repeat mutations (NPARM), make up the remaining 8-10% of CCHS cases. The new American Thoracic Society Statement on CCHS provides additional details regarding CCHS, with focus on the past decade of advances (Weese-Mayer et al., 2010).
Internationally, nearly 1000 cases with PHOX2B mutation-confirmed CCHS have been diagnosed as of early 2010 (Weese-Mayer et al., 2009, 2010). Along with confirmation of a PHOX2B mutation, CCHS is diagnosed in the absence of primary lung, cardiac, neuromuscular disease, or an identifiable brainstem lesion accounting for the central hypoventilation and overall phenotype. CCHS is a life-long disease in which an individual is unable to appropriately adapt her/his ventilation to environmental demands nor arouse from sleep in response to physiologic compromise. These patients will also have altered or absent perception of shortness of breath when awake (Shea et al., 1993c). Consequently, they have diminished tidal volumes and monotonous respiratory rates in both behavior states (Weese-Mayer et al., 2010), with more profound and life-threatening hypoventilation during sleep. Accordingly, these individuals require a tracheostomy with mechanical ventilation during sleep and, in severe cases, additional mechanical ventilation or diaphragm pacing while awake. Along with respiratory control abnormalities, CCHS is associated with both anatomic and physiologic symptoms of ANSD. Anatomic symptoms of ANSD can include presence of Hirschsprung disease (HSCR) and neural crest tumors (such as neuroblastoma). Physiologic symptoms can include diminished pupillary response, esophageal dysmotility, profound constipation even in the absence of HSCR, breath-holding spells, reduced basal body temperature control, sporadic profuse diaphoresis, lack of perception to dyspnea, altered perception of anxiety and pain, and lack of physiologic responsiveness to the challenges of exercise and environmental stressors (Faure et al., 2002; Goldberg and Ludwig, 1996; Marazita et al., 2001; O'Brien et al., 2005; Paton et al., 1993; Pine et al., 1994; Shea et al., 1993a, 1993b, 1993c; Silvestri et al., 1995; Spengler et al., 1998; Trang et al., 2005; Weese-Mayer et al., 1992, 2001, 2010). Thus, a constellation of features is emerging that defines the PHOX2B-genotype/CCHS-phenotype correlation, including severity of facial dysmorphology, ventilatory dependence, symptoms of autonomic dysregulation, cardiac asystoles, relation to age at presentation, HSCR, and neural crest tumors (Berry-Kravis et al., 2006; Gronli et al., 2008; Matera et al., 2004; Repetto et al., 2009; Todd et al., 2006; Trang et al., 2004; Trochet et al., 2005; Weese-Mayer et al., 2003, 2005).
A subgroup of PHOX2B mutation-confirmed CCHS cases have recently been identified outside the newborn period (Weese-Mayer et al., 2009, 2010). Many of these cases (termed later-onset congenital central hypoventilation syndrome, LO-CCHS) have a more subtle phenotypic profile and, genotypically, have the shorter PARMs (heterozygous with genotypes 20/24 and 20/25) or a variant of NPARM that minimally alters the protein product (Parodi et al., 2008; Trochet et al., 2005). While these individuals are often diagnosed in infancy and childhood, they can remain undiagnosed even to adulthood. In these individuals, discovery of hypoventilation may, at times, require an environmental cofactor such as sedation, anesthesia, anticonvulsants, severe respiratory illness, treated obstructive sleep apnea (Antic et al., 2006; Weese-Mayer et al., 2005) or the homozygous condition (Trochet et al., 2008) to elicit overt clinical events like hypoventilation and/or respiratory arrest. Thus far, fewer than 50 LO-CCHS cases have been reported, but considering the subtlety of the clinical profile in those cases, the prevalence in the general population is likely to be significantly higher than suggested by these few cases.
3. Mosaicism, mode of inheritance, and clinical testing
While de novo germline mutations cause the majority of CCHS cases, the existence ofmosaicism has been identified in a subset (5-10%) of parents of CCHS probands (Trochet et al., 2005; Weese-Mayer et al., 2003). An autosomal-dominant inheritance from these mosaic parents (Weese-Mayer et al., 2003), as well as from probands (Trochet et al., 2005; Weese-Mayer et al., 2003), has also been established. This knowledge has led to improved educational efforts and genetic counseling in CCHS families regarding reproductive risks. The PHOX2B Screening Test (Weese-Mayer et al., 2003) (also known as fragment analysis) is a clinically available method using targeted mutation analysis for detection and sizing of the repeat sequence associated with the polyalanine tract expansion (patented; proceeds support CCHS research). This test is now widely used for prenatal diagnosis, family testing to ascertain mosaicism and disease, and diagnosis of individuals with relevant symptoms. With a negative PHOX2B Screening Test and a strong clinical suspicion of CCHS, the ATS Statement on CCHS recommends the whole-gene PHOX2B Sequencing Test as a subsequent test (Weese-Mayer et al., 2010). Both methods of clinical testing are available at www.genetests.org.
4. Carbon dioxide chemoreception and CCHS
The defining feature of CCHS is reduced physiological response to elevated CO2, especially during quiet or non-rapid eye movement (NREM) sleep. Table 1 summarizes relevant publications describing reports of individuals with CCHS who underwent hypercarbic challenges, either from exogenous manipulation of breathing gases or from spontaneously arising endogenous hypercarbia events during wakefulness, sleep, or ventilator withdrawal, excluding case studies with insufficiently detailed challenges (reproduced with permission; Carroll et al., 2010). Several limitations of this body of research cited in Table 1 are immediately apparent. These include the following: small sample size, variable experimental and analytic methods, infrequent age, gender and ethnicity-matched control subjects, and inconsistent documentation of a PHOX2B mutation. Most of the cited studies report cases with (likely) the mildest phenotypes judging by the complexity of the protocols and the need for adequate awake spontaneous breathing, and paucity of analyses stratified by PHOX2B genotype. Despite identification of PHOX2B as the disease-defining gene for CCHS in 2003, authors have continued to publish research absent PHOX2B confirmation (Harper et al., 2005; Kumar et al., 2005, 2008b; Macey et al., 2003, 2004a, 2004b, 2005a), to include patients with non-CCHS diagnoses in grouped data analysis (Huang et al., 2008), and to analyze phenotype data without stratification by PHOX2B genotype. With the aim to better understand the role of specific PHOX2B genotypes/mutations in the development and function of CO2 chemoreception, autonomic dysregulation, and CCHS phenotype, it is essential that future studies include PHOX2B genotype information and that the cohorts be of ample size to analyze the results by genotype.
Table 1.
CCHS publications including CO2 challenge, in chronological order (note no PHOX2B testing available until 2003).
| Citation | N | Type of study | Genotype | Age at onset | Age at test | Challenge method | State | Gas mixtures CO2/O2/N2 | Results & comments |
|---|---|---|---|---|---|---|---|---|---|
| Mellins, et al. 1970 | 1 | CR | NA | 12 do | 12 mo | RB SP: >100 |
W | 4%/U/U | Case compared to 30 previous mostly adult onset cases with reduced CO2 sensitivity. Established definitional diagnostic criteria and behavioral state dependence. |
| Shannon, et al. 1976 | 2 | CR | NA | birth | 4 mo | D | R | 5%/U/U | Compared 6 unmatched controls. Decreased Vt to challenge. |
| Haddad, et al. 1978 | 2 | CR | NA | birth | 1-2 mo | SP:48-75 D |
W/R/N | 2%/U/U | No response in f or Vt to challenge. |
| Wells, et al. 1980 | 1 | CR | NA | birth | 19 mo | SP: 71 | W/S | U/A & 100% | No ventilatory response in R or N |
| Fleming, et al. 1980 | 1 | CR | NA | birth | 9 mo | D | W/R/N | 4%/U/U | No ventilatory response in W or R, small response in N. Parents also challenged; mother shows very low-normal response. |
| Guilleminault, et al. 1982 | 2 | CR | NA | early | 2 mo, 16 mo | D | W/S | 4.75%/U/U 7.25%/ U/U 2%/ U/U 5%/ U/U |
Minimal ventilatory response to 4.75%; some response to 7.25%. Some response to 5%; stage-dependent arousals. |
| Oren, et al. 1987 | 6 | CR/CU | NA | early | 5 wo + follow-up | D | W | 3.5%/A | Ventilatory response muted or absent |
| Paton, et al. 1989 | 5 | CU | NA | <1 yo | 6-11 yo | RB-13 | W | 5%/95% | No consistent ventilatory response to challenge |
| Marcus, et al. 1991 | 8 | CU | NA | <1 yo | 0.4-12 yo | D/RB | S | 10%/A | 7/8 cases aroused to challenge with no ventilatory response, but required more time (reached higher Pet CO2) |
| Weese-Mayer, et al. 1992 | 32 | CU | NA | early | median: 3mo | SP: >70 CB |
W/S | U | No ventilatory response to challenge. |
| Shea, 1993 | 5 | CU | NA | birth | 8-17 yo | RB-2 CB |
W | 14%/A | Blunted ventilatory response. No subjective ‘breathlessness’. |
| Gozal, et al. 1993 | 5 | CM | NA | <1yo | 9-14 yo | RB-U | W | 15%/ U/U 5%/95% 5%/0%/95% |
Designed to elicit mainly transient peripherally mediated response. No significant case-control differences in CO2 response slopes; significant changes in Vt (and f in some challenges). |
| Nakahara, et al. 1995 | 1 | CR | NA | birth | birth | U | W/S | U | Normal response in W; flat in S. |
| Kerbl, et al. 1996 | 1 | CR | NA | birth | 8mo | RB | W/S | U | Blunted f and arousal response to challenge. |
| Croaker, et al. 1998 | 5 | CR | NA | birth | birth | SP: varied | W/S | U | No ventilatory response to hypercapnia. |
| Macey, et al. 2003 | 14 | CA | NA | U | 8-15 yo | D | W | 5%/95% 0%/15%/85% |
Measured fMRI global BOLD response. Gases measured in subset. Muted hypercapnic response in cases. |
| Macey, et al. 2004 | 12 | CM | U | U | 8-15 yo | D | W | 5%/95% 0%/15%/85% |
Slow/muted response. Slow f response to hypercapnia. |
| Bajaj, et al. 2005 | 1 | CR | NPARM | pre | pre | SP: 120 | S | No ventilatory response in extreme preterm with Hirschsprung disease. | |
| Chiaretti, et al. 2005 | 3 | CM | U | 1-4 wo | 1-3 mo | SP: 75 | S | No ventilatory response. | |
| Harper, et al. 2005 | 14 | CA | U | U | 8-15 yo | D | W | 5%/95% 0%/15%/85% |
Measured fMRI localized BOLD response. Most areas muted or inverse response in cases. Group differences in midline dorsal medulla, etc. |
| Chen, et al. 2005 | 5 | CA | U | <1 yo | mean: 21 yo | RB-13 | W | 5% | No ventilatory response, with normal cardiovascular response. BP response preserved. |
| Antic, et al. 2006 | 5 | CR | 20/25 | varied | 22-36yo | CB SP: 60-82 |
W/S | Mild phenotype in adult diagnoses (LO-CCHS) with possible antecedent symptoms. | |
| Bachetti, et al. 2006 | 2 | CR | U | birth | 3 mo <15 mo |
V | N | U | No ventilatory response. |
| Barratt, et al. 2007 | 1 | CR | 20/25 | 32 yo? | 41 yo | RB | W | U | No quantification. |
| Diedrich, et al. 2007 | 1 | CR | 20/25 | U | 27 yo | CB | W | U | Blunted response to challenges. No EMG response to breath hold. Reduction in some HRV measures. BP similar to control. |
| Doherty, et al. 2007 | 5 | CR | 20/25 | varied | 4-41 yo | RB-5 | W | 7%/93% | LO-CCHS. Reduced response in all PHOX2B mutation-confirmed family members. |
| Huang, et al. 2008 | 7 | CM | 20/25-27 | U | mean: 13 yo | V | W/N/R | U | More severe hypoventilation in N and R. Arousals in 41% of sleep trials. Summary data pooled from 7 CCHS and 2 non-CCHS with normal genotype. |
| Lee, et al. 2009 | 3 | CU | 20/25 | 22-30 yo | 22-53 yo | RB-7 | W | 5% | Reduced slope response to CO2 challenge |
| Fine-Goulden, et al. 2009 | 1 | CR | 20/25 | 12 yo | 12 yo | SP: >112 | S | Respiratory failure after anesthesia. |
Reproduced with permission from Carroll et al., (2010)
Abbreviations:
N: Number of subjects exposed to hypercapnic challenges
Type of Study: CR: Case report CU: Cohort, unmatched CA: Cohort, approximately matched CM: Cohort, matched
PHOX2B Genotype: NA: not available pre 2003 U: unknown; not tested NPARM: non-polyalanine repeat mutation
Challenge Method: D: Direct through ventilator, pneumotach or mask RB-X: Rebreathing, with X liter reservoir CB: Voluntarily controlled breathing rate V: Ventilator withdrawal SP: X: Spontaneous hypercapnia to X mm Hg.
Behavioral State: W: Wake S: Sleep, unspecified stage N: Non-REM R: REM
Gas Mixtures: xx/xx/xx: Specific blend of CO2/O2/N2 U: Unspecified A: Ambient room air
Comments: f: Respiratory frequency Vt: End-tidal volume HRV: Heart-rate variability EMG: Electromyograph Pet: End-tidal partial pressure fMRI: Functional magnetic resonance imaging BOLD: Blood-oxygen-level dependent BP: Blood pressure LO-CCHS: Late onset CCHS
5. Carbon dioxide chemoreception and PHOX2B in the animal model
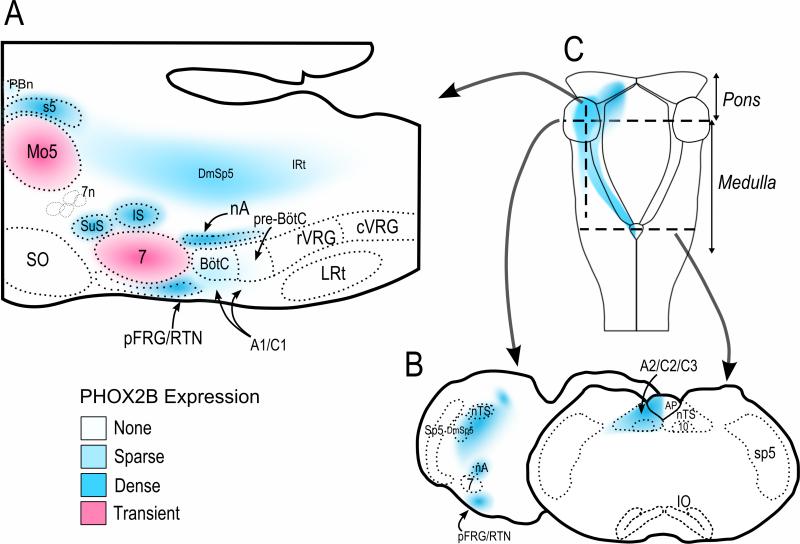
Early mouse studies from homozygous phox2b-/- knock-out models showed dramatic circuit specific anatomic deficits along the chemosensory reflex arc, including peripheral afferent ganglia and central integration sites (Dauger et al., 2003). While these mice were non-viable, heterozygous knockouts survived and showed a transient neonatal physiological phenotype, consisting of a reduced ventilation response to hypercapnia and hypoxia with recovery of wild-type responses by postnatal day 10, thus highlighting the discordance between this model and the clinical presentation in humans (Dauger et al., 2003). These concerns led to the development of knock-in models which inserted the most common CCHS-associated human variant, the PARM 20/27 phox2b genotype (Dubreuil et al., 2008). These mice may more accurately reproduce the toxic gain-of-function suggested by human genotype-phenotype association and inheritance patterns, in contrast to the loss-of-function generated by the heterozygous knock-out models (Dubreuil et al., 2008). In fact, these mice show site-specific loss of a group of medullary neurons known alternately as the retrotrapezoid nucleus (RTN; Guyenet et al., 2008) or the parafacial respiratory group (pFRG; Dubreuil et al., 2008; Onimaru et al., 2009). These neurons have been shown to be important for integration and/or relay of chemosensory drive to respiratory rhythm and pattern generating circuits (Stornetta et al., 2006). The difficulty with this model, however, is that it is short-lived and, as true for the human with the PHOX2B 20/27 genotype, would require artificial respiratory support to survive beyond the neonatal period. If longer survival becomes possible, it would be useful to evaluate these mice for the presence of several human-CCHS-phenotypic features, such a HSCR, cardiac asystoles, or symptoms of physiologic autonomic dysregulation, which are all associated with the PHOX2B 20/27 genotype in humans. As is clear, animal studies have improved our understanding of the importance of phox2b in CO2 chemoreception (Abbott et al., 2009; Takakura et al., 2008), but are limited in direct translation to the human CCHS clinical phenotype. A set of schematic diagrams outlining current concepts of brainstem sites expressing phox2b and the role of maturation in those sites found in basic animal studies is shown in Figure 1. Recent findings of phox2b expression in cerebellar and forebrain sites, which likely contribute to respiratory/autonomic deficits, and overlap the MRI structural and functional findings of altered tissue, described in the Allen (Lein et al., 2007), and GenSat (Gong et al., 2003) atlases, are not outlined in Figure 1.
Figure 1.
Schematic representation of expression profile and developmental dependence on phox2b in rodent pontomedullary structures associated with autonomic regulation and respiratory control. (A) Schematic representation of phox2b along sagittal plane illustrated in dorsal view outlined at right (C). Expression patterns are color-coded within individual cell groups as noted below (sparse and dense refer to proportions of positive cell nuclei within a region; transient refers to fetal/neonatal expression lost in adult animals). (B) Schematic of two coronal sections showing expression profile at the level of the pontomedullary border and dorsal vagal complex. (C) Illustration of dorsal view of brainstem indicating location of sagittal and coronal sections and schematized expression gradients. Omitted from this figure for simplicity, the locus coeruleus has also been identified as expressing phox2b in the GenSat mouse gene atlas (Gong et al., 2003), though these findings contradict a null result in adult rats from Kang et al. (2007). Abbreviations: 7n, facial nerve tracts; 7, facial nucleus; 10, vagal nucleus; A1/2/5, norepinephrine cell groups; AP, area postrema; BötC, Bötzinger Complex; C1/2/3, epinephrine cell groups; cVRG, caudal ventral respiratory group; DmSp5, dorsomedial nucleus of the spinal trigeminal nerve; IS, inferior salivatory nucleus; IRt, intermediate reticular nucleus; LRt, lateral reticular nucleus; nA, nucleus ambiguous; nTS, nucleus of the solitary tract; PBn, parabrachial nucleus; pFRG/RTN, para-facial respiratory group/retrotrapazoid nucleus; pre-BötC, pre-Bötzinger Complex; rVRG, rostral ventral respiratory group; Sp5, spinal trigeminal nucleus; SO, superior olive; s5, supratrigeminal nucleus; Mo5, trigeminal motor nucleus.
Figure redrawn and adapted from Alheid et al. (2004), Kang et al. (2007), and Stornetta et al. (2006). Recent findings of cerebellar and forebrain sites described in the Allen (Lein et al., 2007) and GenSat (Gong et al., 2003) atlases are not included in this Figure 1. (Figure created by MSC and CMR).
6. Waking and sleep influences on chemoreception
As noted recently by Carroll et al. (2010), description of the precise nature of altered central chemoreception in CCHS in the published literature is limited, because the studied subjects likely have the “mildest” of the PHOX2B genotypes. Specifically, to be physiologically able to complete the described protocols safely, it is likely that the subjects in most studies showing ventilatory facilitation with exercise, limb movement, or mental exercise (Gozal et al., 1993; Paton et al., 1993; Shea et al., 1993c) had the 20/25 genotype. Such facilitation of breathing indicates that other, non-chemoreceptor influences enhance the rhythmogenesis of breathing. However, we do not know if similar compensatory mechanisms exist in patients with the more “severe” genotypes who require 24 hour/day artificial ventilation. In addition to CO2 insensitivity, individuals with CCHS have an absent perception of shortness of breath in response to heavy exercise (Spengler et al., 1998), intercurrent illness, such as pneumonia (Weese-Mayer et al., 2010), and hypoxia. The loss leads to an absence of enhanced respiration (inspiratory effort or respiratory rate) with an apparent failure to sense the affective associations of shortness of breath.
Severity of hypoventilation in CCHS differs between wakefulness and sleep, and even within sleep, with more severe hypoventilation appearing during quiet (NREM) sleep, and more moderate breathing deficits during REM sleep (Fleming et al., 1980). Brain structures that induce and maintain quiet sleep are principally located in the basal forebrain (Suntsova et al., 2007; Szymusiak et al., 2007; Szymusiak and McGinty, 2008), while structures that generate REM sleep lie below the forebrain, in pontine areas (Jouvet, 1967). The state-dependent hypoventilation relationship in CCHS suggests inhibitory or loss of excitatory influences on breathing stemming from basal forebrain mechanisms on brainstem rhythmogenesis or neurotransmitter sites. Furthermore, other facilitatory or disinhibitory neural influences on breathing operate during REM sleep. Sleep-state changes in neuromodulatory tone, such as the loss of dorsal raphé serotonergic discharge during REM sleep (McGinty and Harper, 1976), may exert direct effects on medullary respiratory rhythm generators (Doi and Ramirez, 2008). The CCHS sleep-state breathing relationships, however, may be largely related to the specific PHOX2B mutation, potentially impacting normal CO2 influences on breathing that are known to be reduced during NREM sleep compared to wakefulness (Skatrud and Dempsey, 1983). These state-related breathing patterns pose several issues for consideration in interactions with CO2 processing: although multiple forebrain sites, including cortical regions, can act to suppress respiratory muscle action (Marks et al., 1987), other forebrain areas, such as the prefrontal and cingulate cortex involved in vocalization, interact with midbrain periaqueductal gray and medullary regions to regulate breathing patterns (Holstege, 1992; Subramanian et al., 2008; Subramanian and Holstege, 2009, 2010). Moreover, the caudal hypothalamus participates in hypoxic influences on breathing (Horn and Waldrop, 1997). The basal forebrain, prefrontal and cingulate cortex, hypothalamus, and midbrain periaqueductal gray areas are all affected in children with CCHS (Kumar et al., 2005, 2008b, 2010), and may contribute to multiple CCHS respiratory deficits, or be the sequelae of inadequately treated hypoventilation and resultant physiologic compromise.
7. Autonomic dysregulation: relevance to breathing
Although the immediate concern for patients with CCHS is the loss of respiratory drive, pronounced dysfunction in global autonomic regulation is also a major characteristic of the disorder (Marazita et al., 2001; Weese-Mayer et al., 2001). This characteristic is likely a consequence of mutations in the PHOX2B gene, which principally targets progenitors of neurons in autonomic ganglia (Amiel et al., 2003; Pattyn et al., 1999, 2000). Although not yet prospectively studied in a large cohort of children with PHOX2B mutation-confirmed CCHS, we do have a basic understanding of the interrelationship in non-CCHS subjects between breathing and systems affected by the ANS. Deficiencies in autonomic regulation can interact with impaired respiratory regulatory sites, partially by pharmacologic alteration of blood pressure/somatic respiratory interactions. These interactions have been illustrated in the adult cat, where transient elevation of arterial pressure elicits apnea (Trelease et al., 1985), and in the adult dog, where transient hypotension enhances ventilation (Ohtake and Jennings, 1992). The autonomic/respiratory interactions are especially important during sleep, with the exaggerated sympathetic bursts and blood pressure swings in REM sleep, and the enhanced inspiratory efforts during NREM sleep, which can modify vagal outflow as demonstrated in both dogs and infants (Verrier and Harper, 2009). Since both sympathetic and parasympathetic systems are affected in CCHS, studies must consider sites affecting both control of breathing and integration of autonomic regulatory systems.
8. Brain structural and functional deficits in CCHS
This section must be prefaced by recognition that the cohort studied thus far with structural and functional magnetic resonance imaging is small (13-16 subjects in any given study), of variable age (7-21 years), until very recently of unknown PHOX2B genotype, and without partitioning by specific PHOX2B variant. Although the results are compelling, they must be interpreted with caution, and cannot be applied to all children with CCHS. Nevertheless, the affected structures underlying control of breathing in CCHS can be assessed non-invasively by magnetic resonance imaging (MRI) techniques. MRI procedures can evaluate individual brain structures (Kumar et al., 2009a, 2009b), and whole-brain regional tissue injury through local changes in free water content, indicative of primary cell and white matter damage (Kumar et al., 2005); and through assessment of directional diffusion properties of water in axons that can indicate integrity of myelin or axons (Kumar et al., 2008b, 2010). The functional integrity of regional structures can be determined by evaluating local changes in arterial deoxyhemoglobin relative to oxyhemoglobin, by using differences in their magnetic properties as contrast; this is referred to as the blood-oxygen-level-dependent (BOLD) procedure for functional MRI (fMRI). All of these structural and functional procedures have been used to supplement the very limited data available from autopsy material (Cutz et al., 1997; Folgering et al., 1979; Liu et al., 1978; Tomycz et al., 2010).
9. Structural brain findings in CCHS
Early MRI studies of structural injury showed no anatomic findings sufficient to account for the respiratory and autonomic characteristics of CCHS (Weese-Mayer et al., 1988). Examination of autopsy material from a few available cases (Cutz et al., 1997; Folgering et al., 1979; Liu et al., 1978; Tomycz et al., 2010), showed insufficient or inconsistent tissue changes that could potentially underlie many features of the CCHS phenotype. A recent autopsy case study of an infant with alveolar hypoventilation and HSCR (although without confirmation by PHOX2B testing), reported findings in the locus coeruleus, retrotrapezoid nucleus, temporal and frontal cortex, as well as in other areas (Tomycz et al., 2010); the first two structures have been implicated in CO2 sensitivity, and the latter cortical areas assist cognitive and autonomic regulation (among many other functions).
MRI studies that evaluate the total amount and distribution of water and its interaction with the surrounding microstructural environment (T2-relaxometry procedures), diffusion of water in the tissue (mean-diffusivity measures), and volumetric procedures that assess precise regional tissue changes, show relatively consistent, although still variable abnormalities in multiple brain structures in a cohort of CCHS subjects, aged 7 to 21, breathing spontaneously during a waking study, with inclusion of 13-16 subjects in each study. Moreover, the advent of more-sophisticated diffusion tensor imaging (DTI) procedures, with variants of analysis allowing evaluation of axons to reveal myelin or axonal integrity, showed substantial axonal injury or depletion of myelin in locus coeruleus and parabrachial pons, and caudal raphé, lateral medulla, posterior thalamus and midbrain (Kumar et al., 2008b, 2010). Using T2-relaxometry measures (Figure 2; Kumar et al., 2005), structural changes appear in multiple sites, including the cerebellum, cingulate and insular cortex, anterior hypothalamus, and hippocampus. These structures serve a great many functions, including the ability to respond to hypercapnia (cerebellum), mediate the sensation (and thus, drive) to breathe from shortness of breath (cingulate, insular cortex), and mediate temperature drive to breathing (anterior hypothalamus). However, the T2-relaxometry techniques used in the early MRI studies provided only relatively low spatial resolution. More-recently developed DTI techniques show alterations in the parabrachial pons (a principal respiratory phase-switching area, i.e., an area responsible for switching from inspiration to expiration, a pattern essential for respiratory cycling), and also show maldevelopment/injury in the nearby locus coeruleus, an area affected in a CCHS autopsy case report (Tomycz et al., 2010). The locus coeruleus provides noradrenergic innervation to brain structures, and may play a significant role in state-related breathing deficiencies in CCHS. The higher-resolution DTI procedures also showed alterations in a portion of the lateral medulla, which has significant cardiovascular regulatory roles, and the caudal midline raphé (Figure 3). A region extending from the posterior thalamus, important for oxygen processing in the lamb (Koos et al., 1998), through the ventral midbrain and mid pons, and portions of the hippocampus, also showed anatomical differences in CCHS. A loss of tissue in CCHS within regional areas of the hippocampus has been outlined with manual tracing and surface morphometric techniques using T1-weighted structural images (providing much higher-resolution) (Macey et al., 2009), together with loss of fibers in the fornix and volume of the mammillary bodies (Kumar et al., 2009b).
Figure 2.
T2-relaxometry procedures, which quantify free water content, indicate neural injury or failed development of neurons in CCHS children; alterations appear in the cerebellum, a column extending from the preoptic areas through the hypothalamus, the cingulate cortex, medial prefrontal cortex, and hippocampus. Specific functions related to physiological deficits in CCHS are noted for the structures; the functions represent only selected actions served by those structures. Adapted from Kumar et al. 2005, reproduced with permission.
Figure 3.
Increased axial diffusivity from diffusion tensor imaging (DTI) in children with CCHS. Abnormalities appear in the midbrain (A), raphé (B), midline of the caudal basal pons (C), and the right lateral medulla (D, E, and F). Adapted from Kumar et al. (2008b), reproduced with permission).
10. Normal brain responses to CO2
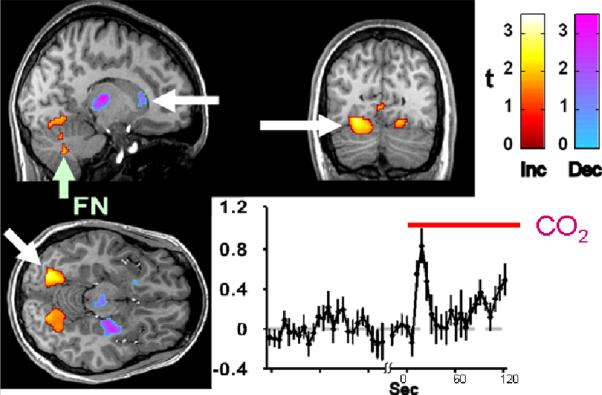
To determine inappropriate brain responses to chemoreceptor stimulation, response patterns to CO2 need to be evaluated in healthy controls from infancy to adulthood. Normal responses of the brainstem and cerebellum to 5% CO2-95% O2 challenges using fMRI have been described over multiple sites in the brain in healthy adolescents (Harper et al., 2005) and adults (Gozal et al., 1994; McKay et al., 2010). Responses in normal adolescents appear in multiple brain areas, extending from the cerebellum to diencephalic structures (Harper et al., 2005). The brain responses to CO2 vary substantially from site-to-site; signal increases appear in some areas, and decline in others, with responses in some sites being transient, occurring only at the onset of the challenge, and other signals maintained during the entire course of CO2 exposure. A subset of the responses is shown in Figure 4. In healthy adolescent subjects, as in the case for adults, 5% CO2-95% O2 challenges induced a substantial signal rise in the cerebellar cortex and deep nuclei. The responses were transient in the cerebellum, rapidly increasing after onset of CO2 exposure, and rapidly declining with continued CO2 exposure. Other regions showed declining signals at onset of exposure to increased CO2, which typically remained lower during continued exposure-- particularly in the head of the caudate nucleus, putamen, and hippocampus, posterior thalamus, parabrachial pons, and midbrain tegmentum. The dorsal medulla, amygdala, and right insular cortex showed signal increases. High levels of CO2 elicit the intense sensation of shortness of breath in normal subjects, and thus recruit limbic sites, e.g., cingulate, insula, hippocampus, amygdala, serving that perception (Evans et al., 2002; Peiffer et al., 2001); the emotions could also be considered stressful, and activate structures involved in mediating such stimuli (Schneider et al., 2009).
Figure 4.
fMRI responses to 5% CO2/95% O2 (red bar) in control adolescents. Signal increases in yellow-red scale appear in the cerebellar cortex as indicated with arrows. “FN” is cerebellar fastigial nucleus. Signal decreases in blue-green scale appear in the caudate nucleus, posterior thalamus, hippocampus and medial midbrain. Adapted from Harper et al. (2005), reproduced with permission.
The patterns of CO2 responses in the healthy adolescent have several implications for understanding central processing of chemoreception. Integration of the afferent CO2 information is served by multiple structures in widespread areas of the brain. The integration involves sites serving comparison of motor output with sensory input roles, important for comparing responses of chemosensitivity with respiratory muscle action within the cerebellum and basal ganglia, and a number of limbic sites often associated with autonomic regulation and the perception of shortness of breath, including the insular cortex (Evans et al., 2002; Peiffer et al., 2001). The 5% CO2-95% O2 challenge in the healthy adolescents also evoked a response in the posterior thalamus, a region remarkable for roles in hypoxic responses in neonatal sheep (Koos et al., 1998).
11. Impaired responses to CO2 in CCHS
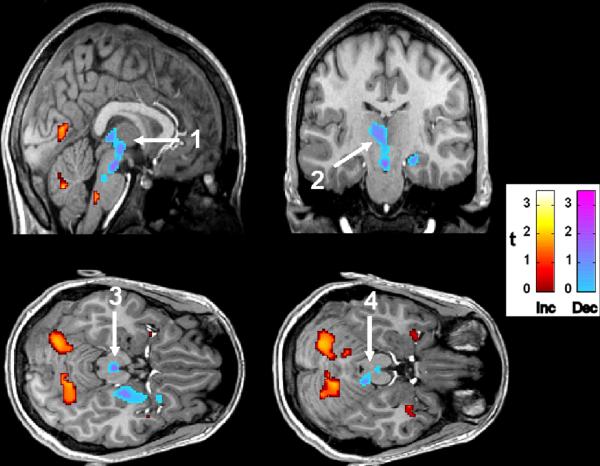
In a cohort of CCHS subjects (n=14), 5% CO2-95% O2 challenges revealed enhanced participation of the cerebellum and dorsal medulla (Figures 3 and 4) compared to healthy controls, and even greater declines in the caudate, insular cortex, hippocampus, posterior thalamus, and caudate (Figure 5) over healthy controls.
Figure 5.
fMRI responses to 5% CO2 in CCHS subjects, compared to age- and gender-matched control adolescents. Signals increase (yellow-red scale), in CCHS subjects (relative to controls), in the dorsal medulla, cerebellum, and amygdala. In the parabrachial pons/locus coeruleus, midbrain and hippocampus, signals decline (blue-green scale). Arrows indicate response differences in the posterior and medial thalamus (1 and 2), medial midbrain (3), and dorsolateral pons (4). The warm colors represent an increase in signal responses in CCHS cases compared to controls, the cool colors represent a greater decline in CCHS over values in controls. Adopted from Harper et al (2005), reproduced with permission.
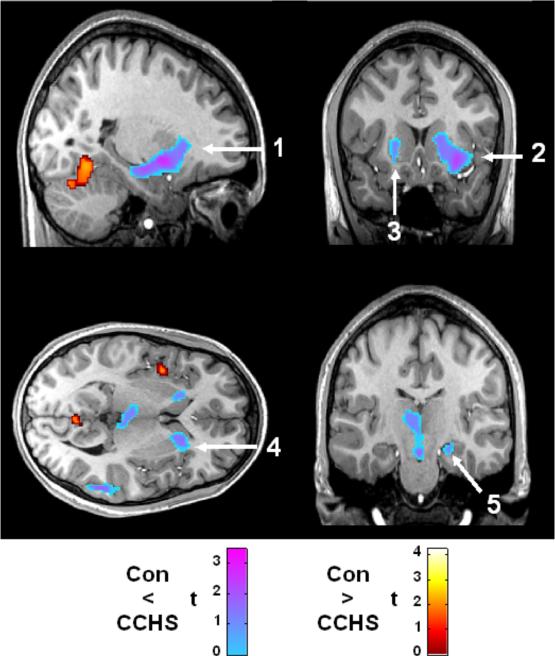
A region of deficient responses to CO2 extended from the posterior thalamus through the ventral midbrain and medial pons (Figure 5). A notable aspect of the differences in CCHS responses emerged in a region extending from the mid insular cortex to, and including, the mid hippocampus (Figure 6).
Figure 6.
fMRI responses to 5% CO2 in CCHS subjects relative to control adolescents, demonstrating other significant clusters of enhanced signals. In CCHS subjects, signal increases (yellow-red scale) appear unilaterally in the insula and cerebellar cortex. Arrows indicate response differences in globus pallidus, putamen, and thalamus (1, 2, 3), caudate (4), and hippocampus (5). Color coding of responses as in Figure 4. Adopted from Harper et al. (2005), reproduced with permission.
The fMRI studies suggest relatively consistent major changes, including phase shifts and pattern reversals in responses to multiple challenges in CCHS, and appear after matching for age and gender. Substantial developmental changes occur normally in brain structural organization over the first 20 years of life (Gogtay et al., 2004), matching for age an essential component of analysis. However, the cohort sizes were insufficient to partition effects by extent of PHOX2B mutation, and adequacy of ventilator management was unknown. Thus, distinguishing between maldevelopmental effects of a specific PHOX2B mutation and injury from recurrent hypercarbia/hypoxia consequent to suboptimal ventilatory management is not achievable. Moreover, fMRI signals derived from BOLD procedures provide relatively low temporal and spatial resolution of signal change, and T2-relaxometry procedures also do not provide fine resolution. The specialized DTI procedures outlined earlier, however, allow higher-resolution fiber structure analysis and the nature of such changes. Measures of water diffusion perpendicular to axons (radial diffusivity) versus parallel to axons (axial diffusivity), can demonstrate myelin vs. axonal integrity, respectively. When areas of structural changes in CCHS, assessed by axial and radial diffusivity techniques, are compared to sites showing functional deficits in response to acute hypercapnic, hypoxic, and cold pressor challenges (with fMRI), a remarkable overlap between the structural and functional deficits appear (Figure 7). Taken together, the findings suggest that the structural deficits may elicit functional consequences in the condition.
Figure 7.
DTI and fMRI images of structural injury (yellow areas), as assessed by axial and radial diffusivity, and functional deficits (blue areas; both blue and yellow areas are highlighted with circles to show comparable regions in structural and functional panels) for hypercapnic, hypoxic, and cold pressor challenges in CCHS patients. Structural injury and functional deficits appear in cerebellum, lateral medulla, and a region of tissue extending from the posterior thalamus through the midbrain. Adopted from Harper et al. (2005), Kumar et al. (2008b), Macey et al. (2005a, b), reproduced with permission.
12. Overlap of brain areas showing deficits and PHOX2B expression
A portion of the fMRI findings in CCHS may develop from consequences of the innate PHOX2B mutations in addition to direct changes in cell differentiation resulting from altered action by the gene. Further dysfunction in CCHS likely results from age at diagnosis and intervention, and variability in ventilatory support and compliance with clinical recommendations. Determination of brain areas potentially affected by mutations in PHOX2B and consequences of gene dysfunction are both of interest, since hypoventilation, the hallmark of CCHS, leads to injury from physiological compromise if not adequately supported with artificial ventilation. The extent of injury consequent to suboptimally managed hypoventilation may be severe in brain areas that serve essential coordination roles for respiratory musculature or blood pressure regulation. For example, injury from intermittent hypoxia can develop within a very short period of time, within 5 hours in the rodent cerebellum (Pae et al., 2005). The extent of recurrent hypercarbic and hypoxic exposure in CCHS varies, depending on initial age at diagnosis, attention to appropriate intervention, nature of the PHOX2B mutation, and duration of exposure to physiologic compromise—with variations from the healthy age-, gender-, and ethnicity-matched control. The consequences of hypercarbic/hypoxic exposure may also be enhanced in CCHS by alterations in autonomic regulatory nuclei resulting from PHOX2B mutations, changes which may include impaired sympathetic control of the vasculature in the child with CCHS. Impaired vascular control can result in pathological changes in regional central nervous system tissue. An example of that potential is found in the vasculature in CCHS patients, with the basilar artery showing substantial dilation in a small cohort of patients (Kumar et al., 2009c), an outcome that can significantly alter perfusion to supplied tissue.
Based on absence of phox2b-expressing neurons in early phox2b knock-out rodent models, the presence of structural deficits in the cerebellum and in many of the forebrain structures on MRI in humans with CCHS was initially believed to develop solely from hypoxic consequences of the disorder. Similarly, alterations in more rostral structures in CCHS were assumed to result from either hypoxia or from failure of vascularization or perfusion as a consequence of embryonic PHOX2B effects on autonomic ganglia development. However, in addition to medullary sites, recent findings in the Allen Brain (Lein et al., 2007) and GenSat (Gong et al., 2003) projects indicate the presence of phox2b neurons in the mouse in widespread regions at some developmental stages. These regions include areas that overlap sites of maldevelopment/injury in the human MRI studies in CCHS, including the cerebellum (http://mouse.brain-map.org/viewImage.do?imageId=125550 and http://www.gensat.org/imagenavigator.jsp?imageID=69648), locus coeruleus (http://www.gensat.org/imagenavigator.jsp?imageID=72012), midbrain, and many of the cortical, limbic, thalamic and basal ganglia structures. Nevertheless, evidence from the GenePaint Atlas (Visel et al., 2004) (http://134.76.20.6/cgibin/mgrqcgi94?APPNAME=genepaint&PRGNAME=analysis_viewer&ARGUMENTS=-AQ70603276209201,-AMH,-A1217,-Asetstart,-A10:) fails to support the presence of phox2b expression in E14.5 and P7 mice in the rostral regions identified in the previously-cited atlases. Further experiments are necessary to resolve the disparities between these data sets as well as to define possible developmental dependencies in expression. Results from these studies should help resolve whether the MRI findings in CCHS result from primary or secondary effects of the PHOX2B mutation.
Despite some similarities in rodent phox2b expression and human CCHS MRI alterations, the distribution of PHOX2B expression is unknown in the human; moreover, phox2b expression in murine models may vary significantly with age. Comparison of the fMRI and structural MRI findings in CCHS in the child/young adult with the animal phox2b expression data (Figure 1; also gene atlas data) may allow for improved understanding of the human condition. Comparison aside, three factors hinder understanding of the human fMRI findings in relation to the anticipated sites of PHOX2B expression in the human: 1) the specific sites of PHOX2B expression based on neuropathological studies in the adolescent human with and without CCHS are unknown, 2) the role of recurrent hypercarbia/hypoxemia as might occur in the less-than-optimally managed patient with CCHS may have incalculable effects on the brain, and 3) the limitations of MRI technology may hinder precise delineation of regions of PHOX2B expression, as demonstrated in animal studies.
13. Ancillary drives to breathing
A remarkable aspect of regulatory control of breathing in CCHS is the absence of the perception of shortness of breath. Brain structures mediating that perception are described in adults (Evans et al., 2002; Peiffer et al., 2001), and include the insular and cingulate cortices, hippocampus, and portions of the cerebellum; all of these structures are affected in CCHS (Kumar et al., 2005, 2006, 2008b). Those structures are in the forebrain and diencephalon, except for the cerebellum; presumably, the cerebellar effects are mediated through cortical projections, since only cortical areas can mediate conscious perception. The perception of shortness of breath is a powerful drive to inspiratory effort, and the absence of that drive in CCHS suggests a significant role for cortical areas in influencing respiratory effort.
Contributions from limbic and cerebellar structures to breathing may not be limited to periods of shortness of breath. A potential state-dependent influence on breathing can develop from limbic projections to respiratory phase switching areas, such as the amygdala projections to the parabrachial pons. Single pulse stimulation of the amygdala in animals will entrain breathing, a relationship that disappears with onset of sleep (Harper et al., 1984). The cingulate cortex, hippocampus, and cerebellum all are recruited to inspiratory efforts following apneic periods in Cheyne-Stokes breathing (Henderson et al., 2006). The Cheyne-Stokes pattern can result from a failure of coordination of central vs. peripheral CO2 afferent information, potentially triggered by alterations in a number of drives, including descending hypothalamic temperature drive or delayed stimulation of peripheral chemoreceptors by lengthening of circulation times. Injury in those areas would have the potential to modify resumption of breathing after breathing cessation, indicating that the concept of modifying breathing by chemoreceptor drive must consider integrative effects from cortical, diencephalic, and cerebellar systems used to initiate breathing.
Alteration of hypothalamic areas in CCHS (Kumar et al., 2005, 2010) is of particular interest because of the lower basal body temperature in CCHS, coupled with recognition that temperature is a major drive to breathing. In addition, return of chemosensitivity appeared in two female adult CCHS patients following administration of the contraceptive desogestrel, which has a 3-fold binding affinity over progesterone receptors (Straus et al., 2010). Recognizing that progesterone can induce increased ventilation, an outcome dependent on the structural integrity of the hypothalamus (Bayliss and Millhorn, 1992), the facilitation of breathing in these two women with CCHS may be consequent to stimulation of residual CO2-sensitive neurons. These new observations should be considered with caution, as changes in normal levels of progesterone, e.g., with pregnancy, have little effect on breathing in CCHS (Sritippayawan et al., 2002); the effect may depend on the enhanced binding of desogestrel to progesterone receptors. The findings do emphasize the potential contributions to chemosensitivity from unexpected sources.
14. Relationship to other sleep-disordered breathing conditions
To understand the processes underlying neural alterations in CCHS, it is useful to examine changes in brain tissue in other sleep-disordered conditions that might result in recurrent hypoxemia and hypercarbia, such as obstructive sleep apnea (OSA), though the age and severity of such physiologic compromise will not be directly comparable to the individual with CCHS whose symptoms began at birth. Presumably, the largest contributions to brain alterations in OSA develop from consequences of successive exposure to intermittent hypoxia or extreme changes in perfusion from arterial pressure swings accompanying apnea in the syndrome, although sleep deprivation and inflammatory processes likely play additional roles (Gozal, 2009; Vecsey et al., 2009). Neural alterations in adult OSA subjects studied by structural and functional MRI techniques share sites with those reported in adolescent subjects with CCHS, and include ventromedial frontal, cingulate, and insular cortex, cerebellar cortex and deep nuclei, hippocampus, fornix, and mammillary bodies (Kumar et al., 2008a; Macey et al., 2002, 2009). However, significant differences emerge; the midbrain, hypothalamic and caudal raphé findings are much more extensive in CCHS than OSA, and the lateral medullary alterations appear thus far only in CCHS (Kumar et al., 2008b, 2010; Macey et al., 2002, 2009). The extreme dilation of the brain vasculature found in CCHS (Kumar et al., 2009c) was not apparent in the adult subjects with OSA. Since the CCHS-specific findings, occurring outside OSA-specific regions, appear in sites that are normally well-perfused, e.g., hypothalamus, and less subject to hypoxic damage, one might conjecture that those sites are more likely to have been affected by PHOX2B mutations rather than sequelae of recurrent hypoxemia/hypercarbia.
15. Conclusions
Multiple impaired processes appear to underlie the breathing and autonomic dysregulation characteristics of CCHS. Deficiencies appear in awake ventilatory sensitivity to CO2 and O2, rhythmogenesis during sleep (preferentially in quiet, NREM sleep over REM sleep), affective excitatory influences from shortness of breath on inspiration, influences of reduced body temperature on breathing, and respiratory-cardiovascular interactions. Other influences on breathing are retained, including voluntary breathing efforts, and in a small subset of cases, accentuated breathing with exercise or peripheral limb motion, even during sleep. A unitary neural lesion underlying all of these processes would be unlikely. Evaluation of structural tissue loss or injury in the brain using functional or structural MRI procedures reveals alterations in multiple sites mediating cardiovascular, breathing and emotive functions, and areas that would interfere with prominent neuromodulators that modify breathing patterns, including the pontine and caudal raphé (serotonin), the locus coeruleus (noradrenalin), the ventral midbrain (dopamine), the basal forebrain (acetylcholine) and the hypothalamus (orexin, progesterone). In addition, areas that coordinate respiratory musculature (cerebellum), mediate emotional drive for inspiration from shortness of breath (insula, cingulate, and hippocampus), or axons that project from these structures (cerebellar peduncle, fornix) are significantly altered. The Allen atlas shows phox2b-expressing neurons in these areas, including both cortical and limbic structures in the rostral brain, as well as locus coeruleus, midbrain and cerebellar areas in mice. However, this expression is not fully supported by the GenePaint, and only partially supported by the GenSat atlases. Thus, the findings, although affecting multiple processes, may develop largely from failed neurogenesis consequent to PHOX2B mutations in the human embryo or PHOX2B effects on glia. Alternatively, findings may be secondary to hypoxic, hypercarbic, or perfusion damage confounded by known PHOX2B effects on autonomic ganglia, potentially resulting in impaired vascularization and functional deficits in blood pressure regulation.
CCHS offers a unique opportunity to assess the neural processing underlying CO2 chemoreception. Continued study of CCHS will undoubtedly lead to a more clear understanding of mechanisms and manifestations of CO2 chemoreception, central and peripheral segregation of function, the importance of feedback and feedforward effects, and the role of human analogs of affected medullary sites, such as the RTN/pFRG. Animal models that reproduce as much of the CCHS clinical profile as possible will improve the therapeutic relevance of basic research in this disease, and help decipher such issues as the differences between neonatal and adult age-at-diagnosis, or the role of neural plasticity in the presentation of the mildest phenotypes (and 20/24 and 20/25 genotypes).
The future of understanding neural substrates of CO2 chemoreception in RADICA lies with the continued study of these diseases and mechanisms both in clinical and laboratory settings, and collaborative efforts between both. CCHS can be seen as a model for such a cooperative effort, elucidating essential mechanisms of respiratory control while improving patient care. The study of RADICA in general will allow us to learn about control of breathing in health as well as disease, thereby providing for these special needs patients while furthering an understanding of the basic science underlying CO2 chemoreception and its relationship to the ANS. However, such success depends upon completion of careful protocols, targeting specific questions, and application in large cohorts of PHOX2B mutation-confirmed cases of CCHS and matched controls--with a clear hypothesis driving the analysis. Respiratory and autonomic disorders can be life-threatening if left undiagnosed or inadequately monitored and treated. Therefore, it behooves clinicians and scientists to work in unison to address fundamental research questions with application to the human condition; ultimately, leading to progress in the fields of respiratory neurobiology, autonomic medicine, and more.
Acknowledgements
This research was supported by NIH HD-22695 (RMH) and the PHOX2B Patent Fund (CMR and MSC).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Pallavi P. Patwari, Assistant Professor of Pediatrics, Northwestern University Feinberg School of Medicine, Assistant Director, Center for Autonomic Medicine in Pediatrics, Children's Memorial Hospital, 2300 Children's Plaza—Mailstop #165 Chicago, IL 60614 PPatwari@ChildrensMemorial.org.
Michael S. Carroll, Center for Autonomic Medicine in Pediatrics, Children's Memorial Hospital, 2300 Children's Plaza—Mailstop #165 Chicago, IL 60614 MSCarroll@ChildrensMemorial.org.
Casey M. Rand, Center for Autonomic Medicine in Pediatrics, Children's Memorial Hospital, 2300 Children's Plaza—Mailstop #165 Chicago, IL 60614 CRand@ChildrensMemorial.org.
Rajesh Kumar, Department of Neurobiology, David Geffen School of Medicine at UCLA, Los Angeles, CA 90095-1763 Rkumar@mednet.ucla.edu.
Ronald M. Harper, Distinguished Professor of Neurobiology, David Geffen School of Medicine at UCLA, Los Angeles, CA 90095-1763 Tel: (310) 825-5303 Fax:(310) 825-2224 RHarper@UCLA.edu.
Debra E. Weese-Mayer, Professor of Pediatrics, Northwestern University Feinberg School of Medicine, Director, Center for Autonomic Medicine in Pediatrics, Children's Memorial Hospital, 2300 Children's Plaza—Mailstop #165 Chicago, IL 60614 DWeese-Mayer@ChildrensMemorial.org.
Literature Cited
- Abbott SB, Stornetta RL, Fortuna MG, Depuy SD, West GH, Harris TE, Guyenet PG. Photostimulation of retrotrapezoid nucleus phox2b-expressing neurons in vivo produces long-lasting activation of breathing in rats. J Neurosci. 2009;29:5806–5819. doi: 10.1523/JNEUROSCI.1106-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alheid GF, Milsom WK, McCrimmon DR. Pontine influences on breathing: an overview. Respir Physiol Neurobiol. 2004;143:105–114. doi: 10.1016/j.resp.2004.06.016. [DOI] [PubMed] [Google Scholar]
- Amiel J, Laudier B, Attie-Bitach T, Trang H, de Pontual L, Gener B, Trochet D, Etchevers H, Ray P, Simonneau M, Vekemans M, Munnich A, Gaultier C, Lyonnet S. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Genet. 2003;33:459–461. doi: 10.1038/ng1130. [DOI] [PubMed] [Google Scholar]
- Antic NA, Malow BA, Lange N, McEvoy RD, Olson AL, Turkington P, Windisch W, Samuels M, Stevens CA, Berry-Kravis EM, Weese-Mayer DE. PHOX2B mutation-confirmed congenital central hypoventilation syndrome: presentation in adulthood. Am J Respir Crit Care Med. 2006;174:923–927. doi: 10.1164/rccm.200605-607CR. [DOI] [PubMed] [Google Scholar]
- Bachetti T, Robbiano A, Parodi S, Matera I, Merello E, Capra V, Baglietto MP, Rossi A, Ceccherini I, Ottonello G. Brainstem anomalies in two patients affected by congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 2006;174:706–709. doi: 10.1164/rccm.200602-266CR. [DOI] [PubMed] [Google Scholar]
- Bajaj R, Smith J, Trochet D, Pitkin J, Ouvrier R, Graf N, Sillence D, Kluckow M. Congenital central hypoventilation syndrome and Hirschsprung's disease in an extremely preterm infant. Pediatrics. 2005;115:e737–738. doi: 10.1542/peds.2004-1910. [DOI] [PubMed] [Google Scholar]
- Barratt S, Kendrick AH, Buchanan F, Whittle AT. Central hypoventilation with PHOX2B expansion mutation presenting in adulthood. Thorax. 2007;62:919–920. doi: 10.1136/thx.2006.068908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayliss DA, Millhorn DE. Central neural mechanisms of progesterone action: application to the respiratory system. J Appl Physiol. 1992;73:393–404. doi: 10.1152/jappl.1992.73.2.393. [DOI] [PubMed] [Google Scholar]
- Berry-Kravis EM, Zhou L, Rand CM, Weese-Mayer DE. Congenital central hypoventilation syndrome: PHOX2B mutations and phenotype. Am J Respir Crit Care Med. 2006;174:1139–1144. doi: 10.1164/rccm.200602-305OC. [DOI] [PubMed] [Google Scholar]
- Carroll MS, Patwari PP, Weese-Mayer DE. Carbon Dioxide Chemoreception and Hypoventilation Syndromes with Autonomic Dysregulation. J Appl Physiol. 2010;108:979–988. doi: 10.1152/japplphysiol.00004.2010. [DOI] [PubMed] [Google Scholar]
- Chen ML, Tablizo MA, Kun S, Keens TG. Diaphragm pacers as a treatment for congenital central hypoventilation syndrome. Expert Rev Med Devices. 2005;2:577–585. doi: 10.1586/17434440.2.5.577. [DOI] [PubMed] [Google Scholar]
- Chiaretti A, Zorzi G, Di Rocco C, Genovese O, Antonelli A, Piastra M, Polidori G, Aloe L. Neurotrophic factor expression in three infants with Ondine's curse. Pediatr Neurol. 2005;33:331–336. doi: 10.1016/j.pediatrneurol.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Croaker GD, Shi E, Simpson E, Cartmill T, Cass DT. Congenital central hypoventilation syndrome and Hirschsprung's disease. Arch Dis Child. 1998;78:316–322. doi: 10.1136/adc.78.4.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutz E, Ma TK, Perrin DG, Moore AM, Becker LE. Peripheral chemoreceptors in congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 1997;155:358–363. doi: 10.1164/ajrccm.155.1.9001336. [DOI] [PubMed] [Google Scholar]
- Dauger S, Pattyn A, Lofaso F, Gaultier C, Goridis C, Gallego J, Brunet JF. Phox2b controls the development of peripheral chemoreceptors and afferent visceral pathways. Development. 2003;130:6635–6642. doi: 10.1242/dev.00866. [DOI] [PubMed] [Google Scholar]
- Diedrich A, Malow BA, Antic NA, Sato K, McEvoy RD, Mathias CJ, Robertson D, Berry-Kravis EM, Weese-Mayer DE. Vagal and sympathetic heart rate and blood pressure control in adult onset PHOX2B mutation-confirmed congenital central hypoventilation syndrome. Clin Auton Res. 2007;17:177–185. doi: 10.1007/s10286-007-0421-4. [DOI] [PubMed] [Google Scholar]
- Doherty LS, Kiely JL, Deegan PC, Nolan G, McCabe S, Green AJ, Ennis S, McNicholas WT. Late-onset central hypoventilation syndrome: a family genetic study. Eur Respir J. 2007;29:312–316. doi: 10.1183/09031936.00001606. [DOI] [PubMed] [Google Scholar]
- Doi A, Ramirez JM. Neuromodulation and the orchestration of the respiratory rhythm. Respir Physiol Neurobiol. 2008;164:96–104. doi: 10.1016/j.resp.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubreuil V, Ramanantsoa N, Trochet D, Vaubourg V, Amiel J, Gallego J, Brunet JF, Goridis C. A human mutation in Phox2b causes lack of CO2 chemosensitivity, fatal central apnea, and specific loss of parafacial neurons. Proc Natl Acad Sci U S A. 2008;105:1067–1072. doi: 10.1073/pnas.0709115105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans KC, Banzett RB, Adams L, McKay L, Frackowiak RS, Corfield DR. BOLD fMRI identifies limbic, paralimbic, and cerebellar activation during air hunger. J Neurophysiol. 2002;88:1500–1511. doi: 10.1152/jn.2002.88.3.1500. [DOI] [PubMed] [Google Scholar]
- Faure C, Viarme F, Cargill G, Navarro J, Gaultier C, Trang H. Abnormal esophageal motility in children with congenital central hypoventilation syndrome. Gastroenterology. 2002;122:1258–1263. doi: 10.1053/gast.2002.33062. [DOI] [PubMed] [Google Scholar]
- Fine-Goulden MR, Manna S, Durward A. Cor pulmonale due to congenital central hypoventilation syndrome presenting in adolescence. Pediatr Crit Care Med. 2009;10:e41–42. doi: 10.1097/PCC.0b013e318198b219. [DOI] [PubMed] [Google Scholar]
- Fleming PJ, Cade D, Bryan MH, Bryan AC. Congenital central hypoventilation and sleep state. Pediatrics. 1980;66:425–428. [PubMed] [Google Scholar]
- Folgering H, Kuyper F, Kille JF. Primary alveolar hypoventilation (Ondine's curse syndrome) in an infant without external arcuate nucleus. Case report. Bull Eur Physiopathol Respir. 1979;15:659–665. [PubMed] [Google Scholar]
- Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF, 3rd, Herman DH, Clasen LS, Toga AW, Rapoport JL, Thompson PM. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DS, Ludwig IH. Congenital central hypoventilation syndrome: ocular findings in 37 children. J Pediatr Ophthalmol Strabismus. 1996;33:175–180. doi: 10.3928/0191-3913-19960501-11. [DOI] [PubMed] [Google Scholar]
- Gong S, Zheng C, Doughty ML, Losos K, Didkovsky N, Schambra UB, Nowak NJ, Joyner A, Leblanc G, Hatten ME, Heintz N. A gene expression atlas of the central nervous system based on bacterial artificial chromosomes. Nature. 2003;425:917–925. doi: 10.1038/nature02033. [DOI] [PubMed] [Google Scholar]
- Gozal D. Sleep, sleep disorders and inflammation in children. Sleep Med. 2009;10(Suppl 1):S12–16. doi: 10.1016/j.sleep.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Gozal D, Hathout GM, Kirlew KA, Tang H, Woo MS, Zhang J, Lufkin RB, Harper RM. Localization of putative neural respiratory regions in the human by functional magnetic resonance imaging. J Appl Physiol. 1994;76:2076–2083. doi: 10.1152/jappl.1994.76.5.2076. [DOI] [PubMed] [Google Scholar]
- Gozal D, Marcus CL, Shoseyov D, Keens TG. Peripheral chemoreceptor function in children with the congenital central hypoventilation syndrome. J Appl Physiol. 1993;74:379–387. doi: 10.1152/jappl.1993.74.1.379. [DOI] [PubMed] [Google Scholar]
- Gronli JO, Santucci BA, Leurgans SE, Berry-Kravis EM, Weese-Mayer DE. Congenital central hypoventilation syndrome: PHOX2B genotype determines risk for sudden death. Pediatr Pulmonol. 2008;43:77–86. doi: 10.1002/ppul.20744. [DOI] [PubMed] [Google Scholar]
- Guilleminault C, McQuitty J, Ariagno RL, Challamel MJ, Korobkin R, McClead RE., Jr. Congenital central alveolar hypoventilation syndrome in six infants. Pediatrics. 1982;70:684–694. [PubMed] [Google Scholar]
- Guyenet PG, Bayliss DA, Mulkey DK, Stornetta RL, Moreira TS, Takakura AT. The retrotrapezoid nucleus and central chemoreception. Adv Exp Med Biol. 2008;605:327–332. doi: 10.1007/978-0-387-73693-8_57. [DOI] [PubMed] [Google Scholar]
- Haddad GG, Mazza NM, Defendini R, Blanc WA, Driscoll JM, Epstein MA, Epstein RA, Mellins RB. Congenital failure of automatic control of ventilation, gastrointestinal motility and heart rate. Medicine (Baltimore) 1978;57:517–526. doi: 10.1097/00005792-197811000-00003. [DOI] [PubMed] [Google Scholar]
- Harper RM, Frysinger RC, Trelease RB, Marks JD. State-dependent alteration of respiratory cycle timing by stimulation of the central nucleus of the amygdala. Brain Res. 1984;306(1-2):1–8. doi: 10.1016/0006-8993(84)90350-0. [DOI] [PubMed] [Google Scholar]
- Harper RM, Macey PM, Woo MA, Macey KE, Keens TG, Gozal D, Alger JR. Hypercapnic exposure in congenital central hypoventilation syndrome reveals CNS respiratory control mechanisms. J Neurophysiol. 2005;93:1647–1658. doi: 10.1152/jn.00863.2004. [DOI] [PubMed] [Google Scholar]
- Henderson LA, Macey KE, Macey PM, Woo MA, Yan-Go FL, Harper RM. Regional brain response patterns to Cheyne-Stokes breathing. Respir Physiol Neurobiol. 2006;150:87–93. doi: 10.1016/j.resp.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Holstege G. The emotional motor system. Eur J Morphol. 1992;30:67–79. [PubMed] [Google Scholar]
- Horn EM, Waldrop TG. Oxygen-sensing neurons in the caudal hypothalamus and their role in cardiorespiratory control. Respir Physiol. 1997;110:219–228. doi: 10.1016/s0034-5687(97)00086-8. [DOI] [PubMed] [Google Scholar]
- Huang J, Colrain IM, Panitch HB, Tapia IE, Schwartz MS, Samuel J, Pepe M, Bandla P, Bradford R, Mosse YP, Maris JM, Marcus CL. Effect of sleep stage on breathing in children with central hypoventilation. J Appl Physiol. 2008;105:44–53. doi: 10.1152/japplphysiol.01269.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung CC, Su YN, Tsao PN, Chen PC, Lin SJ, Lin CH, Mu SC, Liu CA, Chang YC, Lin WL, Hsieh WS, Hsu SM. Unequal crossover recombination - population screening for PHOX2B gene polyalanine polymorphism using CE. Electrophoresis. 2007;28:894–899. doi: 10.1002/elps.200600383. [DOI] [PubMed] [Google Scholar]
- Jouvet M. Neurophysiology of the states of sleep. Physiol Rev. 1967;47:117–177. doi: 10.1152/physrev.1967.47.2.117. [DOI] [PubMed] [Google Scholar]
- Kerbl R, Litscher H, Grubbauer HM, Reiterer F, Zobel G, Trop M, Urlesberger B, Eber E, Kurz R. Congenital central hypoventilation syndrome (Ondine's curse syndrome) in two siblings: delayed diagnosis and successful noninvasive treatment. Eur J Pediatr. 1996;155:977–980. doi: 10.1007/BF02282890. [DOI] [PubMed] [Google Scholar]
- Kang BJ, Chang DA, Mackay DD, West GH, Moreira TS, Takakura AC, Gwilt JM, Guyenet PG, Stornetta RL. Central nervous system distribution of the transcription factor Phox2b in the adult rat. J Comp Neurol. 2007;503:627–641. doi: 10.1002/cne.21409. [DOI] [PubMed] [Google Scholar]
- Koos BJ, Chau A, Matsuura M, Punla O, Kruger L. Thalamic locus mediates hypoxic inhibition of breathing in fetal sheep. J Neurophysiol. 1998;79:2383–2393. doi: 10.1152/jn.1998.79.5.2383. [DOI] [PubMed] [Google Scholar]
- Kumar R, Ahdout R, Macey PM, Woo MA, Avedissian C, Thompson PM, Harper RM. Reduced caudate nuclei volumes in patients with congenital central hypoventilation syndrome. Neuroscience. 2009a;163:1373–1379. doi: 10.1016/j.neuroscience.2009.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R, Birrer BV, Macey PM, Woo MA, Gupta RK, Yan-Go FL, Harper RM. Reduced mammillary body volume in patients with obstructive sleep apnea. Neurosci. Lett. 2008a;438(3):330–334. doi: 10.1016/j.neulet.2008.04.071. [DOI] [PubMed] [Google Scholar]
- Kumar R, Lee K, Macey PM, Woo MA, Harper RM. Mammillary body and fornix injury in congenital central hypoventilation syndrome. Pediatr Res. 2009b;66:429–434. doi: 10.1203/PDR.0b013e3181b3b363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R, Macey PM, Woo MA, Alger JR, Harper RM. Elevated mean diffusivity in widespread brain regions in congenital central hypoventilation syndrome. J Magn Reson Imaging. 2006;24:1252–1258. doi: 10.1002/jmri.20759. [DOI] [PubMed] [Google Scholar]
- Kumar R, Macey PM, Woo MA, Alger JR, Harper RM. Diffusion tensor imaging demonstrates brainstem and cerebellar abnormalities in congenital central hypoventilation syndrome. Pediatr Res. 2008b;64:275–280. doi: 10.1203/PDR.0b013e31817da10a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R, Macey PM, Woo MA, Alger JR, Keens TG, Harper RM. Neuroanatomic deficits in congenital central hypoventilation syndrome. J Comp Neurol. 2005;487:361–371. doi: 10.1002/cne.20565. [DOI] [PubMed] [Google Scholar]
- Kumar R, Macey PM, Woo MA, Harper RM. Rostral brain axonal injury in congenital central hypoventilation syndrome. J Neurosci Res. 2010;88(10):2146–54. doi: 10.1002/jnr.22385. [DOI] [PubMed] [Google Scholar]
- Kumar R, Nguyen HD, Macey PM, Woo MA, Harper RM. Dilated basilar arteries in patients with congenital central hypoventilation syndrome. Neurosci Lett. 2009c;467:139–143. doi: 10.1016/j.neulet.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P, Su YN, Yu CJ, Yang PC, Wu HD. PHOX2B mutation-confirmed congenital central hypoventilation syndrome in a Chinese family: presentation from newborn to adulthood. Chest. 2009;135:537–544. doi: 10.1378/chest.08-1664. [DOI] [PubMed] [Google Scholar]
- Lein ES, Hawrylycz MJ, Ao N, Ayres M, Bensinger A, Bernard A, Boe AF, Boguski MS, Brockway KS, Byrnes EJ, Chen L, Chen TM, Chin MC, Chong J, Crook BE, Czaplinska A, Dang CN, Datta S, Dee NR, Desaki AL, Desta T, Diep E, Dolbeare TA, Donelan MJ, Dong HW, Dougherty JG, Duncan BJ, Ebbert AJ, Eichele G, Estin LK, Faber C, Facer BA, Fields R, Fischer SR, Fliss TP, Frensley C, Gates SN, Glattfelder KJ, Halverson KR, Hart MR, Hohmann JG, Howell MP, Jeung DP, Johnson RA, Karr PT, Kawal R, Kidney JM, Knapik RH, Kuan CL, Lake JH, Laramee AR, Larsen KD, Lau C, Lemon TA, Liang AJ, Liu Y, Luong LT, Michaels J, Morgan JJ, Morgan RJ, Mortrud MT, Mosqueda NF, Ng LL, Ng R, Orta GJ, Overly CC, Pak TH, Parry SE, Pathak SD, Pearson OC, Puchalski RB, Riley ZL, Rockett HR, Rowland SA, Royall JJ, Ruiz MJ, Sarno NR, Schaffnit K, Shapovalova NV, Sivisay T, Slaughterbeck CR, Smith SC, Smith KA, Smith BI, Sodt AJ, Stewart NN, Stumpf KR, Sunkin SM, Sutram M, Tam A, Teemer CD, Thaller C, Thompson CL, Varnam LR, Visel A, Whitlock RM, Wohnoutka PE, Wolkey CK, Wong VY, Wood M, Yaylaoglu MB, Young RC, Youngstrom BL, Yuan XF, Zhang B, Zwingman TA, Jones AR. Genome-wide atlas of gene expression in the adult mouse brain. Nature. 2007;445:168–176. doi: 10.1038/nature05453. [DOI] [PubMed] [Google Scholar]
- Liu HM, Loew JM, Hunt CE. Congenital central hypoventilation syndrome: a pathologic study of the neuromuscular system. Neurology. 1978;28:1013–1019. doi: 10.1212/wnl.28.10.1013. [DOI] [PubMed] [Google Scholar]
- Macey KE, Macey PM, Woo MA, Harper RK, Alger JR, Keens TG, Harper RM. fMRI signal changes in response to forced expiratory loading in congenital central hypoventilation syndrome. J Appl Physiol. 2004;97:1897–1907. doi: 10.1152/japplphysiol.00359.2004. [DOI] [PubMed] [Google Scholar]
- Macey PM, Alger JR, Kumar R, Macey KE, Woo MA, Harper RM. Global BOLD MRI changes to ventilatory challenges in congenital central hypoventilation syndrome. Respir Physiol Neurobiol. 2003;139:41–50. doi: 10.1016/j.resp.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Macey PM, Henderson LA, Macey KE, Alger JR, Frysinger RC, Woo MA, Harper RK, Yan-Go FL, Harper RM. Brain morphology associated with obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166:1382–1387. doi: 10.1164/rccm.200201-050OC. [DOI] [PubMed] [Google Scholar]
- Macey PM, Macey KE, Woo MA, Keens TG, Harper RM. Aberrant neural responses to cold pressor challenges in congenital central hypoventilation syndrome. Pediatr Res. 2005a;57:500–509. doi: 10.1203/01.PDR.0000155757.98389.53. [DOI] [PubMed] [Google Scholar]
- Macey PM, Richard CA, Kumar R, Woo MA, Ogren JA, Avedissian C, Thompson PM, Harper RM. Hippocampal volume reduction in congenital central hypoventilation syndrome. PLoS One. 2009;4:e6436. doi: 10.1371/journal.pone.0006436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macey PM, Valderama C, Kim AH, Woo MA, Gozal D, Keens TG, Harper RK, Harper RM. Temporal trends of cardiac and respiratory responses to ventilatory challenges in congenital central hypoventilation syndrome. Pediatr Res. 2004;55:953–959. doi: 10.1203/01.PDR.0000125262.82405.3C. [DOI] [PubMed] [Google Scholar]
- Macey PM, Woo MA, Macey KE, Keens TG, Saeed MM, Alger JR, Harper RM. Hypoxia reveals posterior thalamic, cerebellar, midbrain, and limbic deficits in congenital central hypoventilation syndrome. J Appl Physiol. 2005b;98:958–969. doi: 10.1152/japplphysiol.00969.2004. [DOI] [PubMed] [Google Scholar]
- Marazita ML, Maher BS, Cooper ME, Silvestri JM, Huffman AD, Smok-Pearsall SM, Kowal MH, Weese-Mayer DE. Genetic segregation analysis of autonomic nervous system dysfunction in families of probands with idiopathic congenital central hypoventilation syndrome. Am J Med Genet. 2001;100:229–236. doi: 10.1002/ajmg.1284. [DOI] [PubMed] [Google Scholar]
- Marcus CL, Bautista DB, Amihyia A, Ward SL, Keens TG. Hypercapneic arousal responses in children with congenital central hypoventilation syndrome. Pediatrics. 1991;88:993–998. [PubMed] [Google Scholar]
- Marks JD, Frysinger RC, Harper RM. State-dependent respiratory depression elicited by stimulation of the orbital frontal cortex. Exp Neurol. 1987;95:714–729. doi: 10.1016/0014-4886(87)90311-6. [DOI] [PubMed] [Google Scholar]
- Matera I, Bachetti T, Puppo F, Di Duca M, Morandi F, Casiraghi GM, Cilio MR, Hennekam R, Hofstra R, Schober JG, Ravazzolo R, Ottonello G, Ceccherini I. PHOX2B mutations and polyalanine expansions correlate with the severity of the respiratory phenotype and associated symptoms in both congenital and late onset Central Hypoventilation syndrome. J Med Genet. 2004;41:373–380. doi: 10.1136/jmg.2003.015412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty DJ, Harper RM. Dorsal raphe neurons: depression of firing during sleep in cats. Brain Res. 1976;101:569–575. doi: 10.1016/0006-8993(76)90480-7. [DOI] [PubMed] [Google Scholar]
- McKay LC, Critchley HD, Murphy K, Frackowiak RS, Corfield DR. Sub-cortical and brainstem sites associated with chemo-stimulated increases in ventilation in humans. Neuroimage. 2010;49:2526–2535. doi: 10.1016/j.neuroimage.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Mellins RB, Balfour HH, Jr., Turino GM, Winters RW. Failure of automatic control of ventilation (Ondine's curse). Report of an infant born with this syndrome and review of the literature. Medicine (Baltimore) 1970;49:487–504. [PubMed] [Google Scholar]
- Nakahara S, Yokomori K, Tamura K, Oku K, Tsuchida Y. Hirschsprung's disease associated with Ondine's curse: a special subgroup? J Pediatr Surg. 1995;30:1481–1484. doi: 10.1016/0022-3468(95)90413-1. [DOI] [PubMed] [Google Scholar]
- Nattie E, Li A. Central chemoreception is a complex system function that involves multiple brain stem sites. J Appl Physiol. 2009;106:1464–1466. doi: 10.1152/japplphysiol.00112.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien LM, Holbrook CR, Vanderlaan M, Amiel J, Gozal D. Autonomic function in children with congenital central hypoventilation syndrome and their families. Chest. 2005;128:2478–2484. doi: 10.1378/chest.128.4.2478. [DOI] [PubMed] [Google Scholar]
- Ohtake PJ, Jennings DB. Ventilation is stimulated by small reductions in arterial pressure in the awake dog. J Appl Physiol. 1992;73:1549–1557. doi: 10.1152/jappl.1992.73.4.1549. [DOI] [PubMed] [Google Scholar]
- Onimaru H, Ikeda K, Kawakami K. Phox2b, RTN/pFRG neurons and respiratory rhythmogenesis. Respir Physiol Neurobiol. 2009;168:13–18. doi: 10.1016/j.resp.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Oren J, Kelly DH, Shannon DC. Long-term follow-up of children with congenital central hypoventilation syndrome. Pediatrics. 1987;80:375–380. [PubMed] [Google Scholar]
- Pae EK, Chien P, Harper RM. Intermittent hypoxia damages cerebellar cortex and deep nuclei. Neurosci Lett. 2005;375:123–128. doi: 10.1016/j.neulet.2004.10.091. [DOI] [PubMed] [Google Scholar]
- Parodi S, Bachetti T, Lantieri F, Di Duca M, Santamaria G, Ottonello G, Matera I, Ravazzolo R, Ceccherini I. Parental origin and somatic mosaicism of PHOX2B mutations in Congenital Central Hypoventilation Syndrome. Hum Mutat. 2008;29:206. doi: 10.1002/humu.9516. [DOI] [PubMed] [Google Scholar]
- Paton JY, Swaminathan S, Sargent CW, Hawksworth A, Keens TG. Ventilatory response to exercise in children with congenital central hypoventilation syndrome. Am Rev Respir Dis. 1993;147:1185–1191. doi: 10.1164/ajrccm/147.5.1185. [DOI] [PubMed] [Google Scholar]
- Paton JY, Swaminathan S, Sargent CW, Keens TG. Hypoxic and hypercapnic ventilatory responses in awake children with congenital central hypoventilation syndrome. Am Rev Respir Dis. 1989;140:368–372. doi: 10.1164/ajrccm/140.2.368. [DOI] [PubMed] [Google Scholar]
- Pattyn A, Goridis C, Brunet JF. Specification of the central noradrenergic phenotype by the homeobox gene Phox2b. Mol Cell Neurosci. 2000;15:235–243. doi: 10.1006/mcne.1999.0826. [DOI] [PubMed] [Google Scholar]
- Pattyn A, Morin X, Cremer H, Goridis C, Brunet JF. Expression and interactions of the two closely related homeobox genes Phox2a and Phox2b during neurogenesis. Development. 1997;124:4065–4075. doi: 10.1242/dev.124.20.4065. [DOI] [PubMed] [Google Scholar]
- Pattyn A, Morin X, Cremer H, Goridis C, Brunet JF. The homeobox gene Phox2b is essential for the development of autonomic neural crest derivatives. Nature. 1999;399:366–370. doi: 10.1038/20700. [DOI] [PubMed] [Google Scholar]
- Peiffer C, Poline JB, Thivard L, Aubier M, Samson Y. Neural substrates for the perception of acutely induced dyspnea. Am J Respir Crit Care Med. 2001;163:951–957. doi: 10.1164/ajrccm.163.4.2005057. [DOI] [PubMed] [Google Scholar]
- Pine DS, Weese-Mayer DE, Silvestri JM, Davies M, Whitaker AH, Klein DF. Anxiety and congenital central hypoventilation syndrome. American Journal of Psychiatry. 1994;151:864–870. doi: 10.1176/ajp.151.6.864. [DOI] [PubMed] [Google Scholar]
- Repetto GM, Corrales RJ, Abara SG, Zhou L, Berry-Kravis EM, Rand CM, Weese-Mayer DE. Later-onset congenital central hypoventilation syndrome due to a heterozygous 24-polyalanine repeat expansion mutation in the PHOX2B gene. Acta Paediatr. 2009;98:192–195. doi: 10.1111/j.1651-2227.2008.01039.x. [DOI] [PubMed] [Google Scholar]
- Sasaki A, Kanai M, Kijima K, Akaba K, Hashimoto M, Hasegawa H, Otaki S, Koizumi T, Kusuda S, Ogawa Y, Tuchiya K, Yamamoto W, Nakamura T, Hayasaka K. Molecular analysis of congenital central hypoventilation syndrome. Hum Genet. 2003;114:22–26. doi: 10.1007/s00439-003-1036-z. [DOI] [PubMed] [Google Scholar]
- Schneider CB, Ziemssen T, Schuster B, Seo HS, Haehner A, Hummel T. Pupillary responses to intranasal trigeminal and olfactory stimulation. J Neural Transm. 2009;116:885–889. doi: 10.1007/s00702-009-0244-7. [DOI] [PubMed] [Google Scholar]
- Shannon DC, Marsland DW, Gould JB, Callahan B, Todres ID, Dennis J. Central hypoventilation during quiet sleep in two infants. Pediatrics. 1976;57:342–346. [PubMed] [Google Scholar]
- Shea SA, Andres LP, Paydarfar D, Banzett RB, Shannon DC. Effect of mental activity on breathing in congenital central hypoventilation syndrome. Respir Physiol. 1993a;94:251–263. doi: 10.1016/0034-5687(93)90022-3. [DOI] [PubMed] [Google Scholar]
- Shea SA, Andres LP, Shannon DC, Banzett RB. Ventilatory responses to exercise in humans lacking ventilatory chemosensitivity. J Physiol. 1993b;468:623–640. doi: 10.1113/jphysiol.1993.sp019792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea SA, Andres LP, Shannon DC, Guz A, Banzett RB. Respiratory sensations in subjects who lack a ventilatory response to CO2. Respir Physiol. 1993c;93:203–219. doi: 10.1016/0034-5687(93)90006-v. [DOI] [PubMed] [Google Scholar]
- Silvestri JM, Weese-Mayer DE, Flanagan EA. Congenital central hypoventilation syndrome: cardiorespiratory responses to moderate exercise, simulating daily activity. Pediatric Pulmonology. 1995;20:89–93. doi: 10.1002/ppul.1950200207. [DOI] [PubMed] [Google Scholar]
- Skatrud JB, Dempsey JA. Interaction of sleep state and chemical stimuli in sustaining rhythmic ventilation. J Appl Physiol. 1983;55:813–822. doi: 10.1152/jappl.1983.55.3.813. [DOI] [PubMed] [Google Scholar]
- Spengler CM, Banzett RB, Systrom DM, Shannon DC, Shea SA, Spengler CM, Banzett RB, Systrom DM, Shannon DC, Shea SA. Respiratory sensations during heavy exercise in subjects without respiratory chemosensitivity. Respiration Physiology. 1998;114:65–74. doi: 10.1016/s0034-5687(98)00073-5. [DOI] [PubMed] [Google Scholar]
- Sritippayawan S, Hamutcu R, Kun SS, Ner Z, Ponce M, Keens TG. Mother-daughter transmission of congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 2002;166:367–369. doi: 10.1164/rccm.2112087. [DOI] [PubMed] [Google Scholar]
- Stornetta RL, Moreira TS, Takakura AC, Kang BJ, Chang DA, West GH, Brunet JF, Mulkey DK, Bayliss DA, Guyenet PG. Expression of Phox2b by brainstem neurons involved in chemosensory integration in the adult rat. J Neurosci. 2006;26:10305–10314. doi: 10.1523/JNEUROSCI.2917-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus C, Trang H, Becquemin MH, Touraine P, Similowski T. Chemosensitivity recovery in Ondine's curse syndrome under treatment with desogestrel. Respir Physiol Neurobiol. 2010;171:171–174. doi: 10.1016/j.resp.2010.03.015. [DOI] [PubMed] [Google Scholar]
- Subramanian HH, Balnave RJ, Holstege G. The midbrain periaqueductal gray control of respiration. J Neurosci. 2008;28:12274–12283. doi: 10.1523/JNEUROSCI.4168-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian HH, Holstege G. The nucleus retroambiguus control of respiration. J Neurosci. 2009;29:3824–3832. doi: 10.1523/JNEUROSCI.0607-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian HH, Holstege G. Periaqueductal gray control of breathing. Adv Exp Med Biol. 2010;669:353–358. doi: 10.1007/978-1-4419-5692-7_72. [DOI] [PubMed] [Google Scholar]
- Suntsova N, Guzman-Marin R, Kumar S, Alam MN, Szymusiak R, McGinty D. The median preoptic nucleus reciprocally modulates activity of arousal-related and sleep-related neurons in the perifornical lateral hypothalamus. J Neurosci. 2007;27:1616–1630. doi: 10.1523/JNEUROSCI.3498-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szymusiak R, Gvilia I, McGinty D. Hypothalamic control of sleep. Sleep Med. 2007;8:291–301. doi: 10.1016/j.sleep.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Szymusiak R, McGinty D. Hypothalamic regulation of sleep and arousal. Ann N Y Acad Sci. 2008;1129:275–286. doi: 10.1196/annals.1417.027. [DOI] [PubMed] [Google Scholar]
- Takakura AC, Moreira TS, Stornetta RL, West GH, Gwilt JM, Guyenet PG. Selective lesion of retrotrapezoid Phox2b-expressing neurons raises the apnoeic threshold in rats. J Physiol. 2008;586:2975–2991. doi: 10.1113/jphysiol.2008.153163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teppema LJ, Dahan A. Central chemoreceptors. In: Teppema LJ, Dahan A, Ward DS, editors. Pharmacology and Pathophysiology of the Control of Breathing. Informa Healthcare; New York: 2005. [Google Scholar]
- Todd ES, Weinberg SM, Berry-Kravis EM, Silvestri JM, Kenny AS, Rand CM, Zhou L, Maher BS, Marazita ML, Weese-Mayer DE. Facial phenotype in children and young adults with PHOX2B-determined congenital central hypoventilation syndrome: quantitative pattern of dysmorphology. Pediatric Research. 2006;59:39–45. doi: 10.1203/01.pdr.0000191814.73340.1d. [DOI] [PubMed] [Google Scholar]
- Tomycz ND, Haynes RL, Schmidt EF, Ackerson K, Kinney HC. Novel neuropathologic findings in the Haddad syndrome. Acta Neuropathol. 2010;119:261–269. doi: 10.1007/s00401-009-0599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trang H, Girard A, Laude D, Elghozi JL. Short-term blood pressure and heart rate variability in congenital central hypoventilation syndrome (Ondine's curse). Clin Sci (Lond) 2005;108:225–230. doi: 10.1042/CS20040282. [DOI] [PubMed] [Google Scholar]
- Trang H, Laudier B, Trochet D, Munnich A, Lyonnet S, Gaultier C, Amiel J. PHOX2B gene mutation in a patient with late-onset central hypoventilation. Pediatr Pulmonol. 2004;38:349–351. doi: 10.1002/ppul.20074. [DOI] [PubMed] [Google Scholar]
- Trelease RB, Sieck GC, Marks JD, Harper RM. Respiratory inhibition induced by transient hypertension during sleep in unrestrained cats. Exp Neurol. 1985;90:173–186. doi: 10.1016/0014-4886(85)90050-0. [DOI] [PubMed] [Google Scholar]
- Trochet D, de Pontual L, Estevao MH, Mathieu Y, Munnich A, Feingold J, Goridis C, Lyonnet S, Amiel J. Homozygous mutation of the PHOX2B gene in congenital central hypoventilation syndrome (Ondine's Curse). Hum Mutat. 2008;29:770. doi: 10.1002/humu.20727. [DOI] [PubMed] [Google Scholar]
- Trochet D, O'Brien LM, Gozal D, Trang H, Nordenskjold A, Laudier B, Svensson PJ, Uhrig S, Cole T, Niemann S, Munnich A, Gaultier C, Lyonnet S, Amiel J. PHOX2B genotype allows for prediction of tumor risk in congenital central hypoventilation syndrome. Am J Hum Genet. 2005;76:421–426. doi: 10.1086/428366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vecsey CG, Baillie GS, Jaganath D, Havekes R, Daniels A, Wimmer M, Huang T, Brown KM, Li XY, Descalzi G, Kim SS, Chen T, Shang YZ, Zhuo M, Houslay MD, Abel T. Sleep deprivation impairs cAMP signalling in the hippocampus. Nature. 2009;461:1122–1125. doi: 10.1038/nature08488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verrier RL, Harper RM. Cardiovascular physiology: Central and autonomic regulation. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 5th ed. Elsevier Saunders; Philadelphia: 2009. pp. 192–202. [Google Scholar]
- Visel A, Thaller C, Eichele G. GenePaint.org: an atlas of gene expression patterns in the mouse embryo. Nucleic Acids Res. 2004;32:D552–556. doi: 10.1093/nar/gkh029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keens TG, Loghmanee DA, Trang H. An official ATS clinical policy statement: Congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am J Respir Crit Care Med. 2010;181:626–644. doi: 10.1164/rccm.200807-1069ST. [DOI] [PubMed] [Google Scholar]
- Weese-Mayer DE, Berry-Kravis EM, Zhou L. Adult identified with congenital central hypoventilation syndrome--mutation in PHOX2b gene and late-onset CHS.[comment]. American Journal of Respiratory & Critical Care Medicine. 2005;171:88. doi: 10.1164/ajrccm.171.1.950. [DOI] [PubMed] [Google Scholar]
- Weese-Mayer DE, Berry-Kravis EM, Zhou L, Maher BS, Silvestri JM, Curran ME, Marazita ML. Idiopathic congenital central hypoventilation syndrome: analysis of genes pertinent to early autonomic nervous system embryologic development and identification of mutations in PHOX2b. Am J Med Genet A. 2003;123A:267–278. doi: 10.1002/ajmg.a.20527. [DOI] [PubMed] [Google Scholar]
- Weese-Mayer DE, Brouillette RT, Naidich TP, McLone DG, Hunt CE. Magnetic resonance imaging and computerized tomography in central hypoventilation. American Review of Respiratory Disease. 1988;137:393–398. doi: 10.1164/ajrccm/137.2.393. [DOI] [PubMed] [Google Scholar]
- Weese-Mayer DE, Rand CM, Berry-Kravis EM, Jennings LJ, Loghmanee DA, Patwari PP, Ceccherini I. Congenital central hypoventilation syndrome from past to future: Model for translational and transitional autonomic medicine. Pediatr Pulmonol. 2009;44:521–535. doi: 10.1002/ppul.21045. [DOI] [PubMed] [Google Scholar]
- Weese-Mayer DE, Silvestri JM, Huffman AD, Smok-Pearsall SM, Kowal MH, Maher BS, Cooper ME, Marazita ML. Case/control family study of autonomic nervous system dysfunction in idiopathic congenital central hypoventilation syndrome. Am J Med Genet. 2001;100:237–245. doi: 10.1002/ajmg.1249. [DOI] [PubMed] [Google Scholar]
- Weese-Mayer DE, Silvestri JM, Menzies LJ, Morrow-Kenny AS, Hunt CE, Hauptman SA. Congenital central hypoventilation syndrome: diagnosis, management, and long-term outcome in thirty-two children. J Pediatr. 1992;120:381–387. doi: 10.1016/s0022-3476(05)80901-1. [DOI] [PubMed] [Google Scholar]
- Wells HH, Kattwinkel J, Morrow JD. Control of ventilation of Ondine's curse. J Pediatr. 1980;96:865–867. doi: 10.1016/s0022-3476(80)80560-9. [DOI] [PubMed] [Google Scholar]
- Williams RH, Jensen LT, Verkhratsky A, Fugger L, Burdakov D. Control of hypothalamic orexin neurons by acid and CO2. Proc Natl Acad Sci U S A. 2007;104:10685–10690. doi: 10.1073/pnas.0702676104. [DOI] [PMC free article] [PubMed] [Google Scholar]