Abstract
Purpose
Large scale databases that offer a reflection of clinical negligence are rare. By assessing commonly occuring cases of negligence, we hope to highlight areas where pediatric orthopedic care might be improved. One such database is the National Health Service Litigation Authority, which deals with claims brought against all health trusts in England. By collating their data we aimed to highlight areas of commonly occurring clinical negligence and then suggest ways to avoid similar happening again.
Method
We reviewed all cases pertaining to pediatric orthopedic claims between 1995 to 2006 as provided by the NHSLA.
Results
Of those considered in our study (341), by far the most common cause of litigation is missed or incorrectly diagnosed injuries/ conditions—accounting for 57% of all cases. 44% of those are upper limb injuries, mainly fractures around the elbow. Misdiagnosed disorders of the hip such as hip dysplasia and SCFE also represent a frequent reason for litigation (11%). Other common causes are poor plaster application and removal (7.3%) and non-surgical site specific errors such as chemical burns from skin prep.
Conclusion
Although specific to the English system, these findings are likely to mirror that found in other countries. Highlighting these commonly occurring errors, better education of doctors in targeted areas and due care in simple procedures may have significant improvement of child orthopedic care.
Keywords: Litigation, Clinical governance, Health improvement, Orthopaedic
Introduction
There were well over 7,000,000 elective and trauma orthopaedic procedures performed between 1995 and 2006 in the UK. Compared to the number of cases performed, the frequency of successful litigation is relatively low but is financially costly to the National Health Service (NHS). In 2007/2008, a total of over £65 million was paid by the NHS Litigation Authority (NHSLA) in all orthopaedic-related settlements. In comparison, the numbers of cases brought to successful litigation are scarce. Nonetheless, the costs both financially and emotionally to patients is high.
The NHSLA was established on 20th November 1995 to indemnify English NHS bodies against claims for clinical negligence. As such, it is a Special Health Authority and part of the English NHS. Initially, its sole function is to administer the “Clinical Negligence Scheme for Trusts” (CNST), a risk-pooling scheme in respect of clinical claims arising from incidents on or after 1st April 1995 [1].
Figure 1 demonstrates the number of new incidences filed and illustrates that litigation attempts are increasing. The apparent decline over the last few years reflects the fact that claims are usually filed several years after the incident occurred. In actual fact, the amount of payments for clinical and non-clinical negligence continues to increase year on year. In 2006/2007, the total payment was £613 million, in 2007/2008, it was £661 million and in 2008/2009, it was £807 million, with 8,885 cases claimed [2] for all clinical and non-clinical cases [3, 4].
Fig. 1.
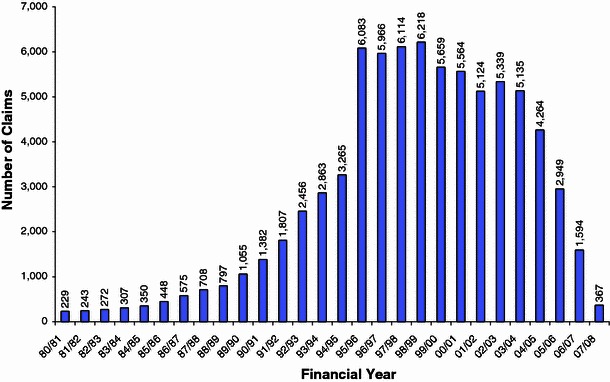
Total number of clinical negligence claims by financial year of incident as at 31st March 2008
The lack of international databases recording clinical negligence in orthopaedics means that there is a rarity of literature detailing why surgeons and institutions are sued. The NHSLA’s collated data offers a rare insight into the problems and instances of clinical negligence.
Individual doctors and health care professionals employed by an NHS hospital are indemnified by that hospital (this is the principle of “vicarious liability”). Here, NHS bodies are legally liable for the negligent acts and omissions of their employees, and should have arrangements for meeting this liability. Nonetheless, doctors are also encouraged to seek additional medico-legal cover to protect against negligence. “Medical negligence” is when an injury/death was caused or contributed to by “the breach of a duty of care” in the provision of clinical or medical services. A subtype of negligence is medical malpractice. This is professional negligence by an act (or omission) by a health care provider in which care deviates from accepted standards of practice in the medical community and causes injury to the patient. Standards and regulations for medical malpractice vary by country and jurisdiction within countries. England and the US, as with many other countries, follow Tort Law. This is a body of rights, obligations and remedies that is applied by courts in civil proceedings to provide relief for persons who have suffered harm from the wrongful acts of others. Torts arising out of negligence are civil wrongs caused by negligent behaviour or a failure to practice due diligence. Three elements must be established in every tort action:
The plaintiff must establish that the defendant was under a legal duty to act in a particular fashion.
The plaintiff must demonstrate that the defendant breached this duty by failing to conform his or her behaviour accordingly.
The plaintiff must prove that he suffered injury or loss as a direct result of the defendant’s breach.
Methods
In this review, the NHSLA was approached and, using the Freedom of Information Act [5], a request for all legal claims of negligence against English health trusts was made for claimants under the age of 16 years which involved orthopaedic departments between 1995 and 2005.
The results were sent as a Microsoft Excel® sheet with each case detailing the following:
The location of the incident (i.e. in A&E, clinic, theatres etc.)
The nature of the claim (e.g. negligence, poor care, failure to diagnose, intra-operative errors etc.)
Whether the case has reached a conclusion (open or closed)
An explanation of the case (e.g. “Abrasion to skin from plaster saw”)
- Total costs paid, broken down into:
- Defence costs
- Claimants’ legal fees
- Damages paid (if any)
Each of the individual cases was reviewed to ascertain the nature of the claim, and the data digested to a more easily understood summary to identify the significant trends. To allow ease of understanding, only the “Total Payments” were recorded in our results and not the full breakdown.
Results
Over a 10-year period, the NHSLA dealt with 519 cases of clinical negligence against orthopaedic departments involving children below 16 years of age. Of these, 111 were still open (unresolved) cases and, therefore, excluded from the study. Some of the data was insufficient to ascertain the reason for litigation and, therefore, those results were also excluded (67 cases).
To identify trends, the remaining 341 cases were assessed and divided into groups of causes depending on the body part and, in some cases, whether they were trauma or elective cases.
It is clear that the most common reason for litigation is incorrect or delayed diagnoses of orthopaedic conditions and fractures, representing 44% of all cases. The majority of those are of the elbow and forearm and wrist (20.5%).
• Trauma of the Upper limb total of 90 cases
By far the most commonly mistreated/misdiagnosed injury was that of humeral supracondylar fractures and other elbow injuries. There were 46 cases (13% of all litigation cases), of which 82% ended with a payout of some form.
Additional to the aforementioned 46 cases of misdiagnosed supracondylar injuries were another 11 cases of intra-operative error during the fixation of elbow fractures. Eight of these were poor fixation and three were iatrogenic ulnar nerve palsy.
As well as supracondylar fractures, misdiagnosis/mistreatment of injuries affecting the wrist/radius and ulna were also common: 22 cases (7% of all cases) with 87% of those having a high payout rate.
• Non-traumatic conditions of the hip joint total of 53 cases
Missed and poor treatment of slipped capital femoral epiphyses (SCFE) and developmental dysplasia of the hip (DDH) were the most common cases, accounting for payouts approaching £3,000,000 in total. Another consideration is the number of cases of infection, both osteomyelitis and septic arthritis, which are relatively uncommon but resulted in payouts of greater than £500,000.
• Spinal surgery total of 14 cases
There were ten cases associated with the management of scoliosis; of these, four were successful with a payout. In one example, a family brought about litigation claiming negligence because surgery was not performed on a severely scoliotic spine and the patient died. There was no payout in this particular case.
• Lower limb trauma cases total of 22 cases
Missed fractures around the knee joint formed the majority of cases in this category. A high payout was also awarded for a missed compartment syndrome. Other successful payouts were awarded for a mixture of cases, including missed nerve injuries and tendon ruptures. Rates were much lower than for injuries of the upper limb.
• Other litigation
These are divided into surgical site-specific and those not associated with the surgical site. Table 1 represents those associated with surgical negligence. Conversely, Table 2 shows those not directly associated with surgery (such as poor plaster technique).
Table 1.
Examples of intra-operative surgical site-specific litigation
| Anatomical site | No. of cases | Examples of cases | Total payout (£) |
|---|---|---|---|
| Upper limb | 18 | Mal-union after supracondylar fixation (×8) Ulnar nerve palsy during supracondylar fixation (×3) Incomplete excision of exostoses (×2) |
154,802 |
| Hips | 6 | Malreduction of SCFE Sciatic nerve palsy during DDH surgery |
236,995 |
Table 2.
Examples of “other” causes of litigation with examples of each category
| Reason for litigation | No. of cases | Examples of cases | Total payout (£) |
|---|---|---|---|
| Poor plaster application | 25 | Skin laceration using plaster saw (×6) Bad plastering→ulceration (×) |
36,190 |
| Non-SSS intra-operative errors | 13 | Burns—chemical and pressure (under tourniquet) and diathermy | 154,802 |
| Delay in operating | 11 | Delay in reduction of SCFE (×2) Delay in reduction of the radial head |
340,530 |
| Unnecessary surgery | 3 | Blount’s disease unnecessarily operated on with complications |
Non-SSS non-surgical site-specific
By far the most common reason related directly to the surgical site was that related to the elbow. These have been discussed previously.
There were 25 claims associated with poor plastering technique—both in application and removal. Six of these were from wounds from using a plaster saw. Claims from this group tended to be successful, with an average payout of £16,044.
There were 13 intra-operative errors that were non-surgical site-specific (NSSS). These included diathermy burns and chemical burns (nine cases), pressure sores and problems related to intra-operative devices, e.g. foot pumps leading to compartment syndrome.
Administrative errors proved expensive in terms of the average payout (£16,519); an example of this is a patient treated for DDH who had a delay in booking an ultrasound scan following an attempted reduction of the hip. Subsequent dislocation resulted in a total payment of £49,434.
Infection is a common concern of surgeons; 12 cases were identified, with success associated with a failure to treat conditions with antimicrobials. The majority of these are post-operative infections and are distinct from the mistreatment of de novo infections. Despite this, the total payout (£36,190) is low in comparison to other, less commonly considered errors.
Table 3 illustrates the “top 10” most frequently occurring causes of paediatric orthopaedics litigation. The misdiagnosis/mistreatment again represents the most common of these. Methods to improve these statistics (via better education etc.) are highlighted in the "Discussion" section.
Table 3.
Top 10 most frequently occurring causes of litigation
| Cause of litigation | No. of cases | Average payout (£) |
|---|---|---|
| Missed/misdiagnosed supracondylar fracture | 44 | 27,998 |
| Poor plaster technique | 25 | 16,044 |
| Missed/misdiagnosed DDH | 24 | 48,534 |
| Missed/misdiagnosed distal radial fracture | 22 | 56,770 |
| Missed/misdiagnosed SCFE | 14 | 56,035 |
| NSSS injuries (including from tourniquets/skin prep/diathermy) | 13 | 11,907 |
| Post-operative infections | 12 | 3,015 |
| Mal-union/nerve injury during surgery for supracondylar fracture | 11 | 8,602 |
| Missed/misdiagnosed scoliosis | 10 | 32,869 |
| Missed/misdiagnosed fractures concerning the knee | 9 | 22,093 |
Discussion
Litigation is an issue that affects surgeons around the world in both private and public health care systems. To the authors’ best knowledge, the NHSLA provides the largest database of clinical negligence. The aim of this work is to identify trends from the data to help reduce poor outcomes in the treatment of paediatric patients. Although this data is specific to the English health service and legal system, the findings may reflect issues in other heath systems around the world.
One should note that the vast majority of claims are abandoned by the claimant (41%)—usually on legal advice and 42% settle out of court. Only 4% are settled within a courtroom (Fig. 2) [5]. Most cases are brought to the attention of the NHSLA via lawyers, who advise the best course of action.
Fig. 2.
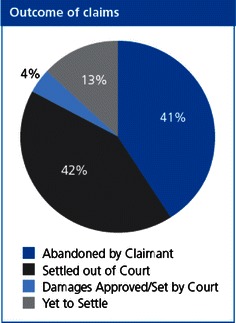
The outcome of all litigation cases brought against the NHS
Cases brought about for the negligence or poor management of children is deemed particularly noteworthy and expensive to hospitals. Highlighting where errors are being made and preventing those errors from occurring again is paramount to good practice.
It is known that many errors in management occur in the primary care setting before they are seen by an orthopaedic surgeon. This may be because of the scarcity of presentation of those conditions (e.g. SCFE), making them unfamiliar. Because litigation against primary care providers falls outside the remit of the NHSLA, this data of mistreated injuries is solely focused on the hospital setting.
The problems associated with the care of children in orthopaedics are a recognised phenomenon. The British Orthopaedic Association publication “Children’s orthopaedics and fracture care” has provided information on the shortcomings currently present within the NHS, highlighting the inadequacies caused by a number of factors, including sub-specialisation, training and the recruitment of specialists. The ‘hub and spoke’ ideology of paediatric care has been suggested, where a tertiary referral centre with dedicated specialist paediatric orthopaedic services (the hub) provide a service for a number of district general hospitals (the spokes).
The key message from this review is to highlight specific injuries/conditions to all medical staff. The frequency of misdiagnosis of trauma and orthopaedic conditions identifies areas where education can be improved. For example, the misdiagnosis of paediatric fractures, particularly those around the elbow, are well known [6, 7] but continue to lead to errors. This may be due to the appearance of ossific nuclei at different ages and subsequent incorrect interpretation of radiographs [8]. Importantly, there have been previous papers [9, 10] highlighting missed injuries around the elbow, especially due to the junior rank of doctors working in the emergency department and those orthopaedic surgeons sent to initially assess children. These papers have already heeded the importance of targeted education, but over a quarter of a century on, it is evident that similar errors are still being made. By once again increasing vigilance and education of this area amongst junior doctors (along with better knowledge of the conditions of the paediatric hip and other common paediatric fractures), errors may be limited.
Further areas of concern are highlighted from the data.
Plaster application and removal by doctors/technicians in both theatre and clinic is an area where due care could avoid unnecessary errors. A compulsory competence certificate of plaster care by doctors and other involved practitioners may be useful at the start of training. Similarly, being alert to the NSSS areas (such as burns around tourniquets [11], pressure sores) by following checklists could also limit avoidable errors. These are all basic principles taught to surgeons as part of basic surgical training, but the message of importance, perhaps, should be stronger in view of the NHSLA data.
With regards to intra-operative errors in paediatric trauma, it is difficult to come to a conclusion without comparing this data to that of the adult population, as any particular case can be challenging. It would be possible to state that certain fracture patterns, particularly injuries of the knee or elbow, should have an appropriately trained surgeon as the lead, which again ties with the idea of the ‘hub and spoke.’ Rates of litigation because of intra-operative error relating to the surgical site are relatively low. Similarly, of those cases that are brought forward, few are successful in paying settlement costs. This may be due to pre-operative consent. Much emphasis is placed on consenting patients. In paediatric patients, errors of consenting infrequently result in litigation, suggesting that, as a specialty, we are more vigilant in this area as compared to our adult colleagues.
The total payments for litigation are mentioned in this article only to illustrate the cost of negligence to the NHS. As payments are individual and reflect patients’ age, outcome and negligence, these figures cannot be used to set “standard” settlement costs.
Limitations of the study
We recognise that one of the major drawbacks of the study is that the collected data was not done so for clinical research. Instead, it represents the sum of all successful litigations against the English NHS as documented by legal clerks. In some of the cases, the information was not detailed enough to be included; this may offer some bias to the result. Our data does not include any litigation arising from primary care providers that may contribute to a large number of orthopaedics cases. Similarly, the information does not inform us whether the negligence events were carried out by emergency department doctors, surgeons or others. It does, however, define where those cases occurred (e.g in the emergency department, theatres, outpatient clinic etc.).
Despite this, we feel that the data which has been incorporated into the study shows common trends.
References
- 1.The National Health Service Litigation Authority. Factsheet 2: financial information. Available online at: http://www.nhsla.com/NR/rdonlyres/465D7ABD-239F-4273-A01E-C0CED557453D/0/NHSLAFactsheet2financialinformation200910.doc
- 2.The National Health Service Litigation Authority. Factsheet 1: background information. Available online at: http://www.nhsla.com/NR/rdonlyres/C9A80E89-2BFA-44F5-A01C-90B86D765B2D/0/NHSLAFactsheet1backgroundinformation200809.pdf
- 3.The National Health Service Litigation Authority. Factsheet 3: information on claims. Available online at: http://www.nhsla.com/NR/rdonlyres/C1B3F310-E13D-4C71-B248-C5384438E603/0/Factsheet30809.doc
- 4.The National Health Service Litigation Authority. Report and accounts 2009. Printed by the UK Stationary Office, on behalf of the controller of HMSO, ID 5797845 07/08 or available online at: http://www.nhsla.com/NR/rdonlyres/3F5DFA84-2463-468B-890C-42C0FC16D4D6/0/NHSLAAnnualReport2008.pdf
- 5.Office of Public Sector Information. Freedom of information act 2000—Chap. 36. Available online at: http://www.opsi.gov.uk/Acts/acts2000/ukpga_20000036_en_1
- 6.O’Hara LJ, Barlow JW, Clarke NM. Displaced supracondylar fractures of the humerus in children. Audit changes practice. J Bone Joint Surg Br. 2000;204:204–210. doi: 10.1302/0301-620X.82B2.9570. [DOI] [PubMed] [Google Scholar]
- 7.Ryan LM, DePiero AD, Sadow JB, Warmink CA, Chamberlain JM, Teach SJ, Johns CM. Recognition and management of pediatric fractures by pediatric residents. Pediatrics. 2004;114:1530–1533. doi: 10.1542/peds.2004-0120. [DOI] [PubMed] [Google Scholar]
- 8.Sharma H, Bhagat S, Gaine WJ. Reducing diagnostic errors in musculoskeletal trauma by reviewing non-admission orthopaedic referrals in the next-day trauma meeting. Ann R Coll Surg Engl. 2007;89(7):692–695. doi: 10.1308/003588407X205305. [DOI] [Google Scholar]
- 9.Freed HA, Shields NN. Most frequently overlooked radiographically apparent fractures in a teaching hospital emergency department. Ann Emerg Med. 1984;13(10):900–904. doi: 10.1016/S0196-0644(84)80666-6. [DOI] [PubMed] [Google Scholar]
- 10.Fontenatta P, Mackenzie DA, Rosman M. Missed, maluniting, and malunited fractures of the lateral humeral condyle in children. J Trauma. 1978;18(5):329–335. doi: 10.1097/00005373-197805000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Demir E, O’Dey DM, Pallua N. Accidental burns during surgery. J Burn Care Res. 2006;27(6):895–900. doi: 10.1097/01.BCR.0000245650.67130.5C. [DOI] [PubMed] [Google Scholar]


