Abstract
Although previous studies have shown that milk intake has some protective effects on metabolic syndrome (MS), there are few data on the relation between MS and milk consumption in Korean. To evaluate the association between milk intake frequency and MS, 4,890 subjects (2,052 men and 2,838 women) were included in the analysis, based on the national data from representative random sample of the third Korea National Health and Nutrition Examination Survey (KNHANES III) in 2005. We conducted both univariate and multivariate logistic regression analysis with adjustment for confounding factors associated with MS. Mean (±SD) age of subjects was 47.1±15.5 yr. In univariate analysis, the risk of MS was inversely associated with the frequency of milk intake, but this relation was attenuated in multivariate regression. In the individuals with BMI ≥23 kg/m2, those with highest quartile of milk consumption (once daily or more) had significantly lower risk of MS (OR [95% CI] 0.72 [0.57-0.92] compared with lowest quartile [those rarely consumed]) after adjustment, but not among leaner individuals (BMI <23 kg/m2). Korean overweight adults who drink milk more frequently may be protected against MS. But it seems that this relation is somewhat different among MS components.
Keywords: Metabolic Syndrome X, Obesity, Milk
INTRODUCTION
The mean daily milk intake of Koreans is reported as 66.5 mg per day and total dairy intake is up to 90 g per day, which is far less than those of western countries (1). Milk is in the limelight as the perfect food and recognized as main source to provide many important nutrients such as protein, essential vitamins, and minerals. In this background, Korean Ministry of Health and Welfare published dietary guideline for Koreans to recommend regular intake of various dairy foods (2). The effects of milk consumption on health have been vigorously discussed, especially in the aspect of bone mineralization, cancer, allergy, and lactose intolerance. Recently, the effects of milk intake on obesity, metabolic syndrome (MS), cardiovascular disease, and cerebrovascular disease have been published, but the results were inconsistent (3-6).
In some previous cross-sectional studies during the late 20th century, milk intake was reported to increase the cerebro- and cardiovascular diseases, but recent prospective studies (7-9) contradicted to those previous studies. It is not proven yet whether milk did increase the risk of vascular disease or not (10-14). Some (15, 16) reported that milk intake was associated with low prevalence of hypertension and diabetes. However others recommended to limit milk intake because milk contains approximately 60 kcal per 100 mL and high proportion of fat and high milk intake might result in obesity and cardiovascular disease. Milk consumption of Koreans is relatively lower than that of western countries. Daily milk drinker is 32.9% at most and those who drink less than once per week is up to 34.3% (1). In Korea, although some advocate various beneficial effects of milk considering relatively lower consumption, others refute this argument due to the concern of obesity. Because there are few studies on the relation between milk intake and MS in Korean, we aimed to verify the association between milk consumption and MS, using nationwide data from random samples of the third Korea National Health and Nutrition Examination Survey (KNHANES III).
MATERIALS AND METHODS
Study population
The general aim of KNHANES was to assess the health and nutritional status of the Korean population. The KNHANES had begun in 1998 and has been conducted as a series of surveys: 1998 (1st), 2001 (2nd), and 2005 (3rd). Specific aims were, in a cross-sectional study of nationally representative samples of the non-institutionalized civilian Korean population aged ≥1 yr, to monitor the trends of prevalence, awareness, treatment, and control of selected chronic diseases, to monitor the trends in nutritional status and risk behaviors, and to analyze risk factors for chronic diseases. For these purposes, with standardized high-quality methods, extensive data on health and nutrition are collected by health interview, health examination (physical examination, clinical measurements, and tests), and dietary interview. Dietary interview contains various questions on food frequency (rarely, 6-11/yr, once monthly, 2-3/month, once/week, 2-3/week, 4-6/week, once daily, twice daily, and trice daily).
In the third survey (2005), a stratified multistage probability sampling was used. Of 13,345 households selected, nutritional survey was performed among 9,047 persons from 3,994 households (17).
We used the data of 3rd survey, extracted nutritional data of adults aged 19 or more, and matched them with health examination and health interview data, which included height, weight, waist circumference, blood pressure, triglyceride (TG), high-density lipoprotein (HDL)-cholesterol, blood glucose, smoking history, physical activity, alcohol drinking, and past medical history. Finally 4,890 individuals with complete health examination data and health interview data were included for this analysis. The study was approved by the Institutional Review Boards of the Seoul National University Hospital (H-1003-014-311).
Measurement and data processing
Height was measured by 0.1 cm unit and weight was measured by 0.1 kg unit. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Waist circumference was measured according to WHO guideline (18) at the end of a normal expiration, with the arms relaxed at the sides, under the midline of the participant's armpit, at the midpoint between the lower part of the last rib and the top of the hip. Blood pressure was measured manually two times 30 sec interval after minimum 5 min rest in a sitting chair, and mean value was taken.
Gender, age, educational level, household income, and occupation of the subjects were asked. Educational level was further classified into no education, under 6 yr of education, 7-9 yr of education, 10-12 yr of education (high school level), 13-16 yr of education (university level), and more than 16 yr of education. Occupation was classified according to Korean standard job classifications. Household income was excluded from final analysis because of low reply rate.
Smoking status was classified as current smoking, ex-smoking, and non-smoking. Physical activity was assessed by regular exercise or not. The alcohol consumption was measured through 24-hr recall.
Current medications on hypertension, diabetes, and dyslipidemia were also asked.
Frequency of milk and dairy food intake such as yogurt and ice cream was assessed from nutritional data. Also daily intake of total calorie, protein, fat, carbohydrate, and fiber were assessed through 24-hr recall by well-trained nutritionist or interviewer.
Fasting blood glucose (FBS), HDL-cholesterol, and TG were measured from venous blood after midnight fasting (longer than 10 hr). MS was diagnosed according to the National Cholesterol Education Program-Adult Treatment Panel III criteria (19), modified with Korean abdominal obesity criterion (waist circumference ≥90 cm in men and ≥85 cm in women) (20).
Statistical analysis
Cutoffs for quartiles of milk intake were calculated, and subjects were categorized according to the quartiles as 'rarely', 'once weekly or less', '2-6 times/week', and 'once daily or more'. Chi-square test and chi-square test for linear by linear association were used to detect any significant differences in the distribution of subjects across the quartiles of milk intake with regard to categorical variables (sex, occupation, smoking, physical activity, BMI category, MS, and its components). Significant differences in continuous variables (age, total energy intake, alcohol intake, and fiber intake) across quartiles of milk intake were searched by using one-way analysis of variance. To ascertain the association of milk intakes with MS and its components, we used logistic regression models; 1) unadjusted, 2) age-adjusted, 3) adjusted for age, sex, BMI, education level, smoking status, regular exercise, daily amount of alcohol, fiber, and total energy intake.
We made stratified analysis with the cutoff point of BMI of 25 kg/m2 (obesity criterion for Koreans) first and repeated the same analysis with the cutoff point of BMI of 23 kg/m2 (overweight criterion for Koreans). We used STATA software (version 11.0) for all statistical analyses. Statistical significance was defined as a P<0.05.
RESULTS
General characteristics of subjects
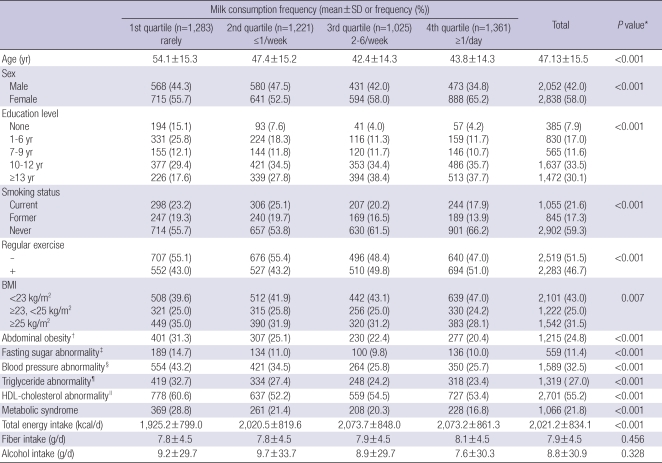
The characteristics of the study population are presented in Table 1. A total of 4,890 subjects (2,052 men, 2,838 women) was available for analysis. Mean age was 47.1 yr; mean alcohol intake was 7.6 g/day; 21.6% of subjects were currently smoking; 31.5% were obese (BMI ≥25 kg/m2); 24.8% had abdominal obesity; and 21.8% had MS.
Table 1.
General characteristics of subjects according to milk consumption frequency
*χ2 test for categorical variables; ANOVA for continuous variables; †Abdominal circumference ≥90 cm for men and ≥85 cm for women; ‡Fasting blood glucose ≥110 mg/dL or on diabetes medication; §Systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg or on hypertension medication; ¶Triglycerides ≥150 mg/dL or on triglycerides medication; ∥HDL-cholesterol <40 mg/dL for men, <50 mg/dL for women, or on HDL-cholesterol medication.
Significant differences were observed across the quartiles of milk intake frequency with regard to age, educational level, smoking status, physical activity, BMI category, MS, and its components. Especially, subjects in the first quartile were older, more obese, and had lower educational level, more MS and its components. They also took lower total calorie than subjects in other three quartiles. The prevalence of MS was 28.8% in the 1st quartile, while 21.8% in the 4th quartile. There was also significant linear by linear association between milk intake frequency and MS and its components (by chi-squared test for linear by linear association).
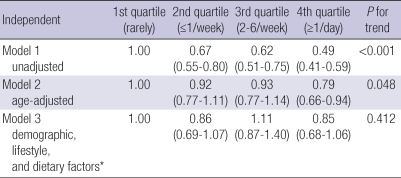
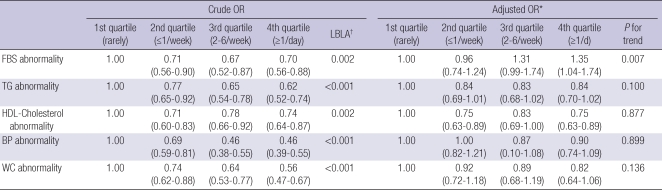
Relation between milk intake frequency and MS
Favorable effect of milk intake against MS was shown in model 1 (unadjusted) but this effect was attenuated after adjustment for age (model 2) and further variables (model 3). A significant trend was observed in model 1 toward the incidence of MS, but was attenuated in model 2 and 3 (Table 2). For each component of MS, there was also significant favorable effect and trend in model 1, but was attenuated in model 2 and 3. Moreover, there was positive significant trend toward FBS abnormality in model 3 (fully adjusted model), and significant increased risk (OR 1.35, 95% CI 1.04-1.74) in 4th quartile over 1st quartile. But for HDL-cholesterol abnormality, significant effect was observed in 2nd quartile (OR 0.75, 95% CI 0.63-0.89) and 4th quartile (OR 0.75 95% CI 0.63-0.89) over 1st quartile (Table 3). For TG and blood pressure, mild protective effect was observed but there was no significant trend.
Table 2.
Odds ratio for metabolic syndrome according to milk intake frequency
*demographic include age, sex, body mass index, education level; lifestyle include smoking, physical activity, daily alcohol intake; dietary factors include daily energy intake, daily fiber intake.
Table 3.
Crude and adjusted odds ratio (OR) for metabolic syndrome components according to milk intake
*adjusted for age, sex, BMI, education level, smoking status, regular exercise, daily amount of alcohol intake, daily amount of total energy intake, daily amount of fiber; †linear by linear association. FBS, fasting blood sugar; TG, triglycerides; HDL, high-density lipoprotein; BP, blood pressure; WC, waist circumference.
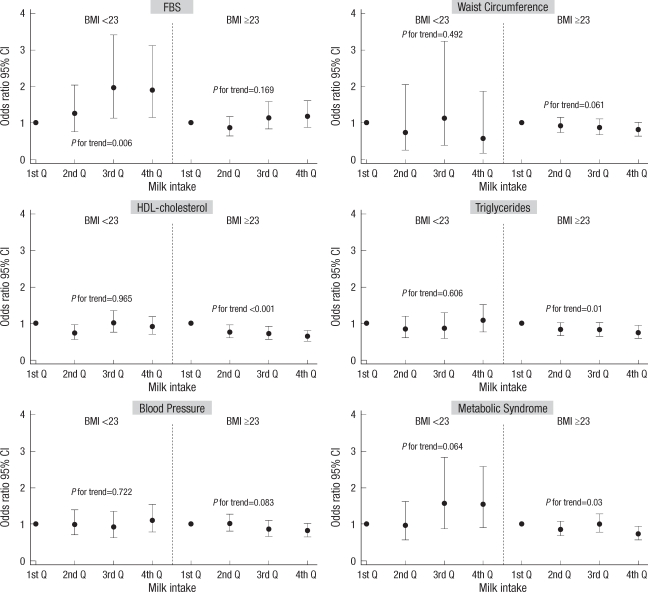
When we stratified the subjects according to BMI, frequent milk intake showed significant favorable effect among subjects with BMI ≥23 kg/m2 against MS and its components except for FBS and waist circumference (Fig. 1). This effect was more prominent in lipid profiles (TG, and HDL-cholesterol). For waist circumference, there was only mild, statistically insignificant favorable effect. Meanwhile, increased milk intake frequency showed significant effect among subjects with BMI <23 kg/m2 on FBS (OR 1.89, 95% CI 1.14-3.11, 4th quartile compared with 1st quartile), and also showed mild increased risk of MS (OR 1.52, 95% CI 0.90-2.57, 4th quartile compared with 1st quartile).
Fig. 1.
Adjusted odds ratio of metabolic syndrome and its components according to milk intake (BMI <23 kg/m2 vs. BMI ≥23 kg/m2).
FBS, fasting blood sugar; HDL, high-density lipoprotein.
DISCUSSION
Previous studies have reported that milk intake was inversely associated with prevalence of MS, but we did not find clear relation of milk intake on MS in Korean people using the KNHANES III data. In univariate analysis, the prevalence of MS and its components decreased as the frequency of milk intake increased. But in multivariate analysis adjusted for several risk factors related with MS, this favorable effect was decreased and there was no clear dose-response relationship. In the individuals with BMI ≥23 kg/m2, those with highest quartile of milk consumption (once daily or more) had significantly lower risk of MS (OR [95% CI] 0.72 [0.57-0.92] compared with lowest quartile [those rarely consumed]) after adjustment, but not among lean individuals (BMI <23 kg/m2).
There have been many debates on the effects of milk consumption on cardiovascular disease, cerebrovascular disease, and MS (21). While several observational studies (22, 23) in the past century have reported that people who drink milk frequently have relatively high prevalence of both cerebrovascular and cardiovascular disease due to atherosclerosis, recent prospective researches retorted an argument against the previous studies. Elwood et al. (8) reported that milk drink did not incur any risk of vascular disease because a pooled estimate of odds ratio for any vascular event when compared with the risk in those with the lowest consumption was 0.84 (95% CI; 0.78-0.90) in subjects with highest intakes of milk. In Carphilly cohort study (9), in which were 665 elderly men followed up for 20 yr, the odds ratio when compared with those with lower intakes of milk, was 0.52 (0.27-0.99) for ischemic stroke in men whose milk consumption was the median or higher. In case of MS, one cohort study, followed up 2,375 men, reported that increased milk consumption was inversely associated with the decrease incidence of MS (11) and also CARDIA study (10), followed up 3,157 young adults, in which dairy consumption was inversely associated with the incidence of insulin resistance syndrome among individuals who was overweight (BMI ≥25 kg/m2) at baseline but not among leaner individuals (BMI <25 kg/m2).
Several studies suggested beneficial effect of milk intake on diabetes mellitus both in men (16) and women (24, 25). However Lawlor DA et al. (13) reported that individuals who did not drink milk had lower prevalence of insulin resistance and MS, also one cross-sectional study (12) reported that milk intake was associated with high incidence of abnormal blood pressure while not associated with body weight, blood glucose, and lipid.
There have been some controversies on the effect of milk on obesity. On one hand milk consumption can cause over-nutrition and weight gain, on the other hand milk intake, especially by calcium intake, can help obese people to lose their weight. Data from cross-sectional epidemiological studies support the hypothesis that a dairy food-rich diet is associated with low fat accumulation in adults and children. But prospective studies and randomized controlled intervention trials have yielded inconsistent results (4, 26).
In our study, frequent milk intake was significantly associated with low risk of MS in univariate analysis; however, after adjustment for several confounding factors, we could not find same results.
Recent Hoorn study (27) investigated the association between dairy intake and change in metabolic risk factors over 6.4 yr; baseline dairy consumption was neither associated with the changes in blood glucose, lipid levels, or blood pressure, nor with the risk of developing the MS. Especially in subjects with BMI <25 kg/m2, higher dairy consumption was significantly associated with an increase in BMI, weight, waist circumference, and a decrease in HDL-cholesterol.
Several studies (10, 24) analyzed the effect of total dairy intake including fermented milk, cheese, and ice cream and compared the effects of low fat or skim milk and high fat milk. In these studies, low fat milk was related with low prevalence of MS. In this connection, there were no data on consumption of fermented milk or low fat/skim milk in KNHANES III, and also there was no total dairy intake frequency. Therefore, we took milk as representative of dairy food in this study. According to the KNHANES III, total dairy consumption per day was 89.7 g, which was consisted of 66.5 g of milk, 13.3 g of yogurt, 6.9 g of ice cream, and others (1).
There have been a few studies investigating the effect of milk drinking in Asians. One cross-sectional study (28) for 988 Hong Kong Chinese reported that dietary habits might not be a strong risk factor for the glucose intolerance. Another study (29) for 2,106 Japanese reported that dietary pattern characterized by frequent consumption of dairy products might be associated with a decreased risk of glucose intolerance. However, this study had a limitation because combined effect of overall healthy-eating pattern including high intake of milk, fruits and vegetables, and low alcohol drinking was analyzed. In a population-based cross-sectional study for 827 Iranian (15), dairy consumption was inversely associated with the risk of having MS, while ethnic difference was described in relation between milk intake and MS (14).
Several studies analyzed the association between dairy intake and MS according to the degree of obesity. In CARDIA study (10), dairy consumption was inversely associated with the incidence of insulin resistance syndrome components only in overweight adults (BMI ≥25 kg/m2). However, Hoorn study (27) reported that high dairy consumption showed no effect on risk factors of MS in overweight; and was significantly associated with an increase in BMI, weight, waist, and lipids. When we analyzed data according to the degree of BMI, risk of abnormal blood glucose and MS significantly increased as the frequency of milk intake increased in the subjects with BMI <23 kg/m2. But in the subjects with BMI ≥23 kg/m2, higher milk intake was significantly associated with low prevalence of high blood pressure, high triglyceride, low HDL-cholesterol, and MS. Pereira et al. suggested that because individuals who are not overweight (BMI <23 kg/m2) might be protected from insulin resistance and obesity by other lifestyle or genetic factors, the association between dairy intake and MS cannot be observed (10). Additionally in the stratified analysis by the age group or sex, there was no significant association between the risk of MS and milk intake frequency.
Because our study was observational, we cannot rule out residual confounding, and we cannot conclude that frequent milk intake in overweight individual reduced the incidence of MS. Nevertheless the strength of this study is that we analyze nationwide representative data of Korea and adjusted various factors associated with MS. In summary, our study suggested that dietary patterns with increased frequency of milk had an inverse relationship with MS among overweight adults. But this effect was variable according to MS components. Because of high prevalence of lactase deficiency, Koreans drink less amount of milk, and may weaken the relation between milk intake frequency and MS. In addition, carbohydrate-rich food of traditional Korean eating pattern can increase the risk of abnormal glucose test (17). For more accurate evaluation, prospective study will be needed, especially in subjects with higher milk intake and various kinds of dairy foods.
References
- 1.Korea Institute for Health and Social Affairs. Ministry of Health and Welfare; 2006. [accessed on 2 March 2010]. The Third Korea national Health and Nutrition Examination Survey (KNHANES III), 2005 - Summary. Available at http://knhanes.cdc.go.kr/ [Google Scholar]
- 2.The Korean Nutrition Society. Dietary Reference Intakes for Korean. Seoul: Hanarum; 2005. pp. 199–207. [Google Scholar]
- 3.Alvarez-Leon EE, Roman-Vinas B, Serra-Majem L. Dairy products and health: a review of the epidemiological evidence. Br J Nutr. 2006;96(Suppl 1):S94–S99. doi: 10.1079/bjn20061709. [DOI] [PubMed] [Google Scholar]
- 4.Barba G, Russo P. Dairy foods, dietary calcium and obesity: a short review of the evidence. Nutr Metab Cardiovasc Dis. 2006;16:445–451. doi: 10.1016/j.numecd.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Tholstrup T. Dairy products and cardiovascular disease. Curr Opin Lipidol. 2006;17:1–10. doi: 10.1097/01.mol.0000199813.08602.58. [DOI] [PubMed] [Google Scholar]
- 6.Huth PJ, DiRienzo DB, Miller GD. Major scientific advances with dairy foods in nutrition and health. J Dairy Sci. 2006;89:1207–1221. doi: 10.3168/jds.S0022-0302(06)72190-7. [DOI] [PubMed] [Google Scholar]
- 7.Elwood PC, Pickering JE, Fehily AM, Hughes J, Ness AR. Milk drinking, ischaemic heart disease and ischaemic stroke I. Evidence from the Caerphilly cohort. Eur J Clin Nutr. 2004;58:711–717. doi: 10.1038/sj.ejcn.1601868. [DOI] [PubMed] [Google Scholar]
- 8.Elwood PC, Pickering JE, Hughes J, Fehily AM, Ness AR. Milk drinking, ischaemic heart disease and ischaemic stroke II. Evidence from cohort studies. Eur J Clin Nutr. 2004;58:718–724. doi: 10.1038/sj.ejcn.1601869. [DOI] [PubMed] [Google Scholar]
- 9.Elwood PC, Strain JJ, Robson PJ, Fehily AM, Hughes J, Pickering J, Ness A. Milk consumption, stroke, and heart attack risk: evidence from the Caerphilly cohort of older men. J Epidemiol Community Health. 2005;59:502–505. doi: 10.1136/jech.2004.027904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002;287:2081–2089. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 11.Elwood PC, Pickering JE, Fehily AM. Milk and dairy consumption, diabetes and the metabolic syndrome: the Caerphilly prospective study. J Epidemiol Community Health. 2007;61:695–698. doi: 10.1136/jech.2006.053157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snijder MB, van der Heijden AA, van Dam RM, Stehouwer CD, Hiddink GJ, Nijpels G, Heine RJ, Bouter LM, Dekker JM. Is higher dairy consumption associated with lower body weight and fewer metabolic disturbances? The Hoorn Study. Am J Clin Nutr. 2007;85:989–995. doi: 10.1093/ajcn/85.4.989. [DOI] [PubMed] [Google Scholar]
- 13.Lawlor DA, Ebrahim S, Timpson N, Davey Smith G. Avoiding milk is associated with a reduced risk of insulin resistance and the metabolic syndrome: findings from the British Women's Heart and Health Study. Diabet Med. 2005;22:808–811. doi: 10.1111/j.1464-5491.2005.01537.x. [DOI] [PubMed] [Google Scholar]
- 14.Beydoun MA, Gary TL, Caballero BH, Lawrence RS, Cheskin LJ, Wang Y. Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr. 2008;87:1914–1925. doi: 10.1093/ajcn/87.6.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dairy consumption is inversely associated with the prevalence of the metabolic syndrome in Tehranian adults. Am J Clin Nutr. 2005;82:523–530. doi: 10.1093/ajcn.82.3.523. [DOI] [PubMed] [Google Scholar]
- 16.Liu S, Choi HK, Ford E, Song Y, Klevak A, Buring JE, Manson JE. A prospective study of dairy intake and the risk of type 2 diabetes in women. Diabetes Care. 2006;29:1579–1584. doi: 10.2337/dc06-0256. [DOI] [PubMed] [Google Scholar]
- 17.Park SH, Lee KS, Park HY. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: Analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III) Int J Cardiol. 2010;139:234–240. doi: 10.1016/j.ijcard.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization Western Pacific Region. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney, Australia: Health Communications Australia Pty Limit; 2000. [Google Scholar]
- 19.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 20.Lee S, Park HS, Kim SM, Kwon HS, Kim DY, Kim DJ, Cho GJ, Han JH, Kim SR, Park CY, Oh SJ, Lee CB, Kim KS, Oh SW, Kim YS, Choi WH, Yoo HJ. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. Korean J Obes. 2006;15:1–9. [Google Scholar]
- 21.Nutritional aspects of cardiovascular disease. Report of the Cardiovascular Review Group Committee on Medical Aspects of Food Policy. Rep Health Soc Subj (Lond) 1994;46:1–186. [PubMed] [Google Scholar]
- 22.Moss M, Freed D. The cow and the coronary: epidemiology, biochemistry and immunology. Int J Cardiol. 2003;87:203–216. doi: 10.1016/s0167-5273(02)00201-2. [DOI] [PubMed] [Google Scholar]
- 23.Segall JJ. Is milk a coronary health hazard? Br J Prev Soc Med. 1977;31:81–85. doi: 10.1136/jech.31.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi HK, Willett WC, Stampfer MJ, Rimm E, Hu FB. Dairy consumption and risk of type 2 diabetes mellitus in men: a prospective study. Arch Intern Med. 2005;165:997–1003. doi: 10.1001/archinte.165.9.997. [DOI] [PubMed] [Google Scholar]
- 25.Wirfalt E, Hedblad B, Gullberg B, Mattisson I, Andren C, Rosander U, Janzon L, Berglund G. Food patterns and components of the metabolic syndrome in men and women: a cross-sectional study within the Malmo Diet and Cancer cohort. Am J Epidemiol. 2001;154:1150–1159. doi: 10.1093/aje/154.12.1150. [DOI] [PubMed] [Google Scholar]
- 26.Schrager S. Dietary calcium intake and obesity. J Am Board Fam Pract. 2005;18:205–210. doi: 10.3122/jabfm.18.3.205. [DOI] [PubMed] [Google Scholar]
- 27.Snijder MB, van Dam RM, Stehouwer CD, Hiddink GJ, Heine RJ, Dekker JM. A prospective study of dairy consumption in relation to changes in metabolic risk factors: the Hoorn Study. Obesity (Silver Spring) 2008;16:706–709. doi: 10.1038/oby.2007.93. [DOI] [PubMed] [Google Scholar]
- 28.Woo J, Ho SC, Sham A, Sea MM, Lam KS, Lam TH, Janus ED. Diet and glucose tolerance in a Chinese population. Eur J Clin Nutr. 2003;57:523–530. doi: 10.1038/sj.ejcn.1601586. [DOI] [PubMed] [Google Scholar]
- 29.Mizoue T, Yamaji T, Tabata S, Yamaguchi K, Ogawa S, Mineshita M, Kono S. Dietary patterns and glucose tolerance abnormalities in Japanese men. J Nutr. 2006;136:1352–1358. doi: 10.1093/jn/136.5.1352. [DOI] [PubMed] [Google Scholar]