Abstract
A 28-year-old woman presented with extensive erythematous lesions on her back after visiting Malawi. Skin biopsies showed ova, which could belong to Schistosoma spp. Sequencing of the Schistosoma 28S rRNA gene, extracted and amplified from paraffin biopsies, identified DNA of Schistosoma haematobium. Cutaneous ectopic schistosomiasis can present with extensive lesions and should be considered in the differential diagnosis of skin lesions in returning travelers. Microscopy and serology are the classical methods to obtain a diagnosis. Alternatively, molecular methods can be a valuable new tool for diagnosis and species determination.
Introduction
Schistosomiasis is endemic throughout wide areas of the tropics and subtropics, with an infection rate of about 200 million people, mainly in Africa.1 In the endemic population Schistosoma spp. cause pathology of different organ systems, the urogenital and gastrointestinal tract, liver, and lungs, as a result of repeated exposure over prolonged periods of time. In travelers, schistosomiasis mostly runs an asymptomatic course with low parasite load and remains underdiagnosed. However, a low worm burden can still bring unexpected morbidity.2 The most common clinical manifestation in a traveler is acute (or invasive) schistosomiasis (“Katayama syndrome”). Sometimes ectopic migration of schistosomal ova can occur to other tissues than their usual habitats, such as brain, spinal cord, and skin. In these cases the diagnosis is often difficult, and species determination by microscopy is sometimes impossible.3 Here we report a patient with cutaneous ectopic schistosomiasis (CES) and describe the potential of molecular methods in this diagnosis.
Case
A 28-year-old woman visited Africa and had been swimming in Lake Malawi frequently. Five months after her visit she presented with itchy papular lesions on her back. She had abdominal cramps and flatulence, but a normal defecation pattern and no dysuria or hematuria.
Physical examination showed extensive grouped papular lesions interscapularly, which were 2 to 4 mm in size, round and partly skin colored, partly erythematous (Figure 1A). Further physical examination was normal.
Figure 1.
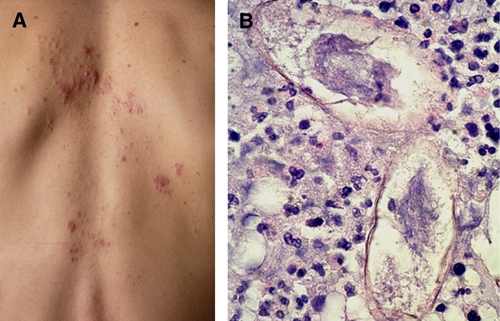
(A) Grouped erythematous itchy papular lesions caused by cutaneous ectopic schistosomiasis. (B) Ova of Schistosoma species in the dermis. This figure appears in color at www.ajtmh.org.
Blood count was normal. Hemoglobin was 7.7 mmol/L, white blood cell count was 7.6 × 109/L with 4.19 × 109/L neutrophils, 2.69 × 109/L lymphocytes, and 0.26 × 109/L eosinophils.
Microscopic examination of feces was negative for intestinal parasites as was urine collected over 24 hours. Serology for schistosomiasis was positive. The titer of specific antibodies against adult worm antigens used in an indirect hemagglutination test was 1:160 (cutoff = 1:80) and the titer against egg-antigen in an enzyme-linked immunosorbent assay (ELISA) was OD 351 (cutoff = 222).4 Serology for Entamoeba histolytica and Strongyloides was negative.
Microscopy of skin biopsies showed granulomatous inflammation with lymphocytes, histiocytes, and plasmacells. Parasitological ova were observed with a size comparable to ova of Schistosoma mansoni or Schistosoma haematobium (~112 by 52 μm) (Figure 1B). Because the spine of the ova was not visible, no definite diagnosis could be made by microscopy. Therefore, DNA was isolated from the paraffin biopsies. Genus-specific polymerase chain reaction (PCR)5 was positive for Schistosoma spp. A semi-nested PCR of the Schistosoma 28S ribosomal RNA (rRNA) gene was performed with primers CF2/CR2 followed by CF1/CR2.6 Sequence analysis showed DNA of S. haematobium (GenBank accession no. FJ455437).
The patient was treated with a single dose of praziquantel (40 mg/kg). The papular lesions disappeared within 2 months, as well as the intestinal complaints.
Discussion
Because of increased tourism to tropical areas, schistosomiasis is more frequently observed in travelers.2 The reported patient presented with extensive skin lesions, diagnosed as CES. This atypical presentation of schistosomiasis has only been described in 15 cases; 7 cases were caused by S. haematobium,3,7–11 7 cases caused by S. mansoni,9,12–16 and in one case species determination was not mentioned.3 CES occurs 4 weeks to 2 years after infection and is characterized by grouped, erythematous, itchy papular lesions or nodules, with a diameter up to 1 cm. Often this is accompanied by eosinophilia. CES is caused by deposition of ova from female worms, which have taken an aberrant route. Instead of the normal route from the portal vein by the caval vein to the plexus around the bladder (S. haematobium) or intestine (S. mansoni), in case of CES, worms deposit their ova in a vein that irrigates the skin. The lesions most often occur at the lower torso and the pelvic area10; especially in women the genital skin is often affected and therefore, distinction from malignancies and sexually transmitted diseases can be difficult. In the presented case the worms probably moved by the pelvine and vertebral plexus to the spinal veins. Alternatively, worms may have passed through portosystemic anastomoses in the pelvic veins to the inferior caval vein. Deposition of ova in the skin inflicts local inflammation of the dermis and subcutis.
Cutaneous ectopic schistosomiasis, caused by ectopic ova should be distinguished from cercaria dermatitis and acute schistosomiasis, which can also present with skin manifestations. Cercarial dermatitis, a hypersensitivity reaction of the skin mostly on penetrating cercariae of avian and human schistosomes, lasts less than 48 hours and should not be mistaken for CES, which is caused by ectopic ova.1 Acute schistosomiasis appears 2 to 8 weeks after infection and is a temporarily appearing immunological reaction to a variety of circulating antigens in early stages of infection, which presents with fever, urticaria, maiaise hepatosplenomegaly, and peripheral eosinophilia.
No eosinophilia was present in our patient, as previously reported in patients with CES. Fifty-seven percent of patients with CES present with eosinophilia.3,7,8,10–12,16 In the described case no ova were observed in urine and in feces, which is in accordance with earlier reports.3,8,9,12
Our patient presented with gastrointestinal complaints, but sequence analysis showed DNA of S. haematobium, which causes urinary schistosomiasis. Gastrointestinal complaints in a patient with CES caused by S. haematobium are uncommon, but have been reported previously by MacDonald and others.9
Molecular methods have been used to test urine and feces samples for Schistosoma spp.5 To our knowledge the present case is the first to describe molecular methods to confirm the diagnosis of CES and to determine the Schistosoma species causing the skin lesions.
Conclusion
Cutaneous ectopic schistosomiasis caused by deposition of ova in the skin can pose a difficult diagnosis. Microscopy on feces or urine and specific serology can support initial diagnosis. Direct microscopy of skin biopsies can reveal the Schistosoma species involved. When inconclusive, molecular methods can be a valuable new tool for diagnosis and species determination.
Acknowledgments
We thank J. J. Verweij, Department of Parasitology, University Medical Center Leiden, The Netherlands for performing the genus-specific PCR for Schistosoma, L. A. Smit, Department of Pathology, Academic Medical Center, Amsterdam, and N. Verhaar, Section Parasitology, Department of Medical Microbiology, Academic Medical Center, Amsterdam for excellent technical support.
Footnotes
Authors' addresses: Karin van Dijk, Aldert Bart, and Tom van Gool, Section Parasitology, Department of Medical Microbiology, Academic Medical Center, Amsterdam, The Netherlands, E-mails: K.vanDijk@amc.uva.nl, A.Bart@amc.uva.nl, and T.vanGool@amc.uva.nl. Markus V. Starink and Henry J. C. de Vries, Department of Dermatology, Academic Medical Center, Amsterdam, The Netherlands, E-mails: M.V.Starink@amc.uva.nl and H.J.deVries@amc.uva.nl. Erik W. P. Nijhuis, Department of Pathology, Onze Lieve Vrouwe Gasthuis, Amsterdam, The Netherlands, E-mail: E.W.P.Nijhuis@olvg.nl. Allard C. van der Wal, Department of Pathology, Academic Medical Center, Amsterdam, The Netherlands, E-mail: A.C.vanderWal@amc.uva.nl. Pieter P. A. M. van Thiel, Department of Infectious Diseases, Tropical Medicine and AIDS, Academic Medical Center, Amsterdam, The Netherlands, E-mail: P.P.vanThiel@amc.uva.nl.
References
- 1.Davis A. In: Manson's Tropical Diseases. 23rd Edition. Cook GC, Zumla A, editors. London, UK: Saunders; 2009. pp. 1425–1460. (Schistosomiasis). [Google Scholar]
- 2.Bierman WF, Wetsteyn JC, Van Gool T. Presentation and diagnosis of imported schistosomiasis: relevance of eosinophilia, microscopy for ova, and serology. J Travel Med. 2005;12:9–13. doi: 10.2310/7060.2005.00003. [DOI] [PubMed] [Google Scholar]
- 3.Leman JA, Small G, Wilks D, Tidman MJ. Localized papular cutaneous schistosomiasis: two cases in travellers. Clin Exp Dermatol. 2001;26:50–52. doi: 10.1046/j.1365-2230.2001.00761.x. [DOI] [PubMed] [Google Scholar]
- 4.Van Gool T, Vetter H, Vervoort T, Doenhoff MJ, Wetsteijn J, Overbosch D. Serodiagnosis of imported schistosomiasis by a combination of a commercial indirect hemagglutination test with Schistosoma mansoni adult worm antigens and an enzyme-linked immunosorbent assay with S. mansoni egg antigens. J Clin Microbiol. 2002;40:3432–3437. doi: 10.1128/JCM.40.9.3432-3437.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ten Hove RJ, Verweij JJ, Vereecken K, Polman K, Dieye L, van Lieshout L. Multiplex real-time PCR for the detection and quantification of Schistosoma mansoni and S. haematobium infection in stool samples collected in northern Senegal. Trans R Soc Trop Med Hyg. 2008;102:179–185. doi: 10.1016/j.trstmh.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Sandoval N, Siles-Lucas M, Perez-Arellano JL, Carranza C, Puente S, Lopez-Alban J, Muro A. A new PCR-based approach for the specific amplification of DNA from different Schistosoma species applicable to human urine samples. Parasitology. 2006;133:581–587. doi: 10.1017/S0031182006000898. [DOI] [PubMed] [Google Scholar]
- 7.Al-Karawi KS, Al-Amro Al-Akloby OM, Mugharbel RM. Ectopic cutaneous schistosomiasis. Int J Dermatol. 2004;43:550–551. doi: 10.1111/j.1365-4632.2004.01728.x. [DOI] [PubMed] [Google Scholar]
- 8.Farrell AM, Woodrow D, Bryceson AD, Bunker CB, Cream JJ. Ectopic cutaneous schistosomiasis: extragenital involvement with progressive upward spread. Br J Dermatol. 1996;135:110–112. [PubMed] [Google Scholar]
- 9.MacDonald DM, Morrison JG. Cutaneous ectopic schistosomiasis. BMJ. 1976;2:619–620. doi: 10.1136/bmj.2.6036.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Obasi OE. Cutaneous schistosomiasis in Nigeria. An update. Br J Dermatol. 1986;114:597–602. doi: 10.1111/j.1365-2133.1986.tb04067.x. [DOI] [PubMed] [Google Scholar]
- 11.Pistone T, Ezzedine K, Accoceberry I, Receveur MC, Juguet F, Malvy D. Ectopic cutaneous schistosomiasis-perigenital infiltrative granulomata in a 34-year-old French pregnant woman. Travel Med Infect Dis. 2008;6:155–157. doi: 10.1016/j.tmaid.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Andrade Filho JS, Lopes MS, Corgozinho Filho AA, Pena GP. Ectopic cutaneous schistosomiasis: report of two cases and a review of the literature. Rev Inst Med Trop Sao Paulo. 1998;40:253–257. doi: 10.1590/s0036-46651998000400009. [DOI] [PubMed] [Google Scholar]
- 13.Clyti E, Faye O, Huerre M, Cisse L, N'Diaye A, Konare-Diawara H, Keita S. Case for diagnosis. Ectopic cutaneous schistosomiasis. Ann Dermatol Venereol. 1998;125:737–738. [PubMed] [Google Scholar]
- 14.Do Vale EC, Furtado T. Ectopic cutaneous schistosomiasis caused by Schistosoma mansoni. Med Cutan Ibero Lat Am. 1987;15:233–237. [PubMed] [Google Scholar]
- 15.Kick G, Schaller M, Korting HC. Late cutaneous schistosomiasis representing an isolated skin manifestation of Schistosoma mansoni infection. Dermatology. 2000;200:144–146. doi: 10.1159/000018349. [DOI] [PubMed] [Google Scholar]
- 16.Milligan A, Burns DA. Ectopic cutaneous schistosomiasis and schistosomal ocular inflammatory disease. Br J Dermatol. 1988;119:793–798. doi: 10.1111/j.1365-2133.1988.tb03506.x. [DOI] [PubMed] [Google Scholar]


