Abstract
This study investigated intrinsic motivation as a mediator of the relationship between clinical symptoms and functioning. The mediation model was tested with a sample of 166 adults with schizophrenia spectrum disorders attending psychosocial rehabilitation programs in a diverse urban community. Ethnic minority status was examined as a moderator of the mediation model. Motivation was measured using items reflecting intrapsychic drive. Symptoms were assessed with the expanded Brief Psychiatric Rating Scale and functioning with the Role Functioning Scale. Motivation was a significant mediator of the relationship between functioning and all symptom scores; fully mediating the relationship between functioning and negative, disorganized, and global symptoms, and partially mediating the relationship between positive symptoms and functioning. Motivation scores between ethnic minority and nonminority individuals differed significantly (p < 0.05), but no moderation effect was indicated. The strong mediation effect schizophrenia of motivation on the symptoms-functioning relationship supports future work to translate findings into effective recovery-oriented services.
Keywords: Mediation model, psychosocial rehabilitation, functional outcomes, ethnic minority status, moderated mediation
A rise in recovery-oriented psychosocial rehabilitation services for individuals with schizophrenia has spurred a broadening of treatment priorities from basic disease management to addressing real world functional outcomes such as independent living (Nelson et al., 2007), social skill development (Kopelowicz et al., 2006), and employment/vocational goals (Mueser et al., 2001). Functional outcomes, such as these, have been posited to be more accurate indicators of recovery than psychiatric symptoms (Liberman et al., 2002). Yet, clinical status (quantity and severity of psychiatric symptoms) remains a key focus of effective medication-based illness management.
Together, pharmacotherapy and psychosocial interventions constitute the cornerstone of evidence-based treatment of schizophrenia (Lehman et al., 2004). The former aims to reduce and stabilize psychiatric symptoms, while the latter addresses functioning to promote community integration and enhance quality of life. This dual treatment outcome focus has spurred a need for research to more firmly clarify the nature of the relationship between clinical status and psychosocial functioning. Some studies have reported a significant association between clinical status and various functional outcomes (Anthony et al., 1995; Breier et al., 1991; Trauer, 2001). Other studies have reported minimal to no association (Henry et al., 2001; Patterson et al., 1998; Perivoliotis et al., 2004). The inconsistent findings are, in part, due to variations in sample characteristics, the nature of the symptoms (e.g., positive, negative, disorganized) or the type of functional domains assessed. A greater understanding of other mechanisms contributing to the mixed findings could inform the development of treatments that more effectively target both outcomes.
Another direction of inquiry that could account for these divergent findings involves identifying contextual variables that may intervene and mediate the relationship between clinical symptoms and functioning. Motivation is one such contextual variable that has been studied extensively throughout the social science literature (Bandura, 1991; Pittman, 1998; Shah and Gardner, 2008) and has been increasingly linked with a variety of health behaviors and substance abuse treatment outcomes (Burke et al., 2003; Dunn et al., 2001; Miller and Rollnick, 2002). In particular, intrinsic motivation, referring to internal processes that drive one to seek new activities and stimulation (Bruner, 1996), has been posited to be a promising construct for application to schizophrenia (Barch, 2005). Interest and enjoyment of an activity for its own sake is the core element that differentiates intrinsic motivation from other types of motivation driven by external rewards (Deci and Ryan, 1985).
One barrier to studying intrinsic motivation has been the lack of a brief self report measure for use in schizophrenia research (Choi et al., 2009). Although the Motivational Trait Questionnaire (Kanfer and Ackerman, 2000) has been used with persons with schizophrenia (Barch et al., 2008), the measure assesses 3 traits (personal mastery, competitive excellence, and motivation related to anxiety) that may underlie intrapsychic drive rather than the strength of intrinsic motivation. Another approach would be to use the Intrinsic Motivation Inventory (Ryan, 1982), a lengthy measure of interest/enjoyment one has while performing a specific task/activity. This measure has been primarily used in experimental research and is not suited for determining a cross-situational level of intrinsic motivation. One viable alternative approach is to use content within an existing clinical outcome measure. A 3-item Scale derived from the Quality of Life Scale (QLS; Heinrichs et al., 1984) shows promise as it has performed well for assessing the core construct of intrinsic motivation when used with persons with schizophrenia (Nakagami et al., 2008).
Within the psychosocial rehabilitation domain, few studies have examined the extent to which clinical status or functional outcomes are directly impacted by motivation. There is some evidence of a negative association between motivation and clinical status (Boydell et al., 2003; Fowles, 1994; Schmand et al., 1994). The work of Bowie et al. (2006) demonstrates a decrease in level of motivation as clinical symptoms increase. Reports based on first-hand accounts of individuals with schizophrenia implicate psychiatric symptoms (positive and negative symptoms) as contributors to a general lack of motivation to improve quality of life (Boydell et al., 2003). The empirical data linking motivation to functional outcomes is slightly more established than that for clinical status (Fogel, 1996; Mee and Sumsion, 2001; Summerfelt et al., 1991). Intrinsic motivation has been mostly studied in relation to specific arenas of functioning, such as maintaining employment (Anthony et al., 1995; Breier et al., 1991), and reducing substance abuse among individuals with dual diagnoses (Carey et al., 2002; Carey et al., 2001). To a lesser degree, motivation has been linked to overall psychosocial functioning (Barch, 2005; Bowie et al., 2006). Ferdinandi et al. (1998) studied motivation in terms of overall readiness for psychosocial rehabilitation; a positive relationship between rehabilitation readiness scores and functional outcomes in the areas of living, learning, working, and socializing was reported. In a study examining how motivation mediated the relationship between neuro-cognition and functioning, Nakagami et al. (2008) found that intrinsic motivation was strongly related to psychosocial functioning. Medalia and Richardson (2005) have discussed the importance of motivation to cognitive remediation interventions in schizophrenia.
To summarize, while intrinsic motivation has been conceptually implicated as a powerful indicator of recovery, the state of empirical evidence is very limited (Barch et al., 2008). Studies have not examined motivation in relation to both clinical status and functional outcomes. As such, the evidence for motivation’s role as a contextual variable that might mediate the relationship between clinical status and functional outcomes is indirect. There remains a need to test these relationships.
The primary purpose of this study was to examine whether intrinsic motivation mediated the relationship between clinical status and functional outcomes among adults with schizophrenia. We also tested the hypotheses that intrinsic motivation would be associated with both clinical status and functional outcomes. Finally, we conducted a post hoc analysis to examine whether ethnic minority status moderated any mediation effects on the relationship between clinical status and functional outcome. This aim was guided by previous literature demonstrating ethnic variation in clinical status and functional outcomes with diverse samples of persons with schizophrenia (e.g., Bae et al., 2004; Barrio, 2001; Barrio et al., 2003; Brekke and Barrio, 1997; Phillips et al., 2001).
METHOD
Sample
The sample consisted of 166 adults, diagnosed with schizophrenia or schizoaffective disorder, who completed the baseline observation of a prospective longitudinal study (Bae et al., 2004; Brekke et al., 2007). Participants were recruited upon entry to one of 4 community-based psychosocial rehabilitation programs in ethnically/racially diverse urban neighborhoods in Los Angeles. Although participants had yet to receive the intensive services offered through these programs, their sociodemographic and clinical characteristics are comparable to other samples of people with schizophrenia in routine outpatient care (Brekke et al., 1997; Heinrichs and Zakzanis, 1998). Diagnoses were determined using clinical records, a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition checklist (American Psychiatric Association, 1994), and collateral reports from the admitting clinicians and on-site psychiatrists. Participants were excluded if they met criteria for alcohol or drug dependence in the previous 6 months or if they had an identified neurological disorder. No individuals were hospitalized and all were living in noninstitutional community settings when the data were gathered. All participants provided written informed consent, under protocols approved by the Institutional Review Board at the University of Southern California and the Research Committee for the Los Angeles County Department of Mental Health.
Measures
Measures were administered to participants in face-to-face interviews, typically at a program site or their residence. The interviewers were masters-level clinicians trained using a protocol described in detail elsewhere (Brekke et al., 1993).
Clinical Status
The severity of psychiatric symptoms were measured using the Extended Brief Psychiatric Rating Scale (BPRS-E; Lukoff et al., 1986). Interviewers were trained on the BPRS-E, using an established protocol (Ventura et al., 1993). Means were computed for the BPRS-E Global score (α = 0.73) and summed scores for the Negative (α = 0.79), Positive (α = 0.71), Affect (α = 0.73), and Activation (α = 0.73) symptom items based on a standardized four-factor model (Velligan et al., 2005) established with ethnically/racially diverse clinical populations (Kopelowicz et al., 2008; Velligan et al., 2005). We also computed a 4-item disorganization factor (α = 0.64) based on previous factor analyses of the BPRS (Liddle and Barnes, 1990; Mueser et al., 1997; Van der Does et al., 1993).
Functional Outcomes
The Role Functioning Scale (RFS: Goodman et al., 1993) represents a global outcome measure of community functioning for persons with severe mental illness (Wieduwilt and Jerrell, 1998). The RFS provides anchored descriptions ranging from 1 (severe impairment in an area of functioning) to 7 (optimal functioning in the area) and captures both the quantity and quality of community-based functioning as the interviewer produces ratings of work, social functioning, and independent living functioning. These 3 ratings were summed to calculate the total RFS score as previous work suggests use of a global score based on item loadings on a single factor (Brekke et al., 2005). As detailed elsewhere, intraclass correlations among raters on the RFS items after training was >0.8 (Brekke et al., 1997).
Intrinsic Motivation
Intrinsic motivation was conceptualized as internal processes such as curiosity and sense of purpose that drive one to seek new activities and stimulation (Bruner, 1996; Murphy and Roopchand, 2003). An intrinsic motivation (IM) score was developed from ratings from the QLS(Heinrichs et al., 1984). The QLS is a semi-structured interview that is administered by a trained interviewer who asks a series of probes related to domains such as degree of motivation (e.g., “How motivated have you been?” or “Do you have much enthusiasm, energy, and drive?”). The interviewer uses the data gathered from these open-ended probes to create one quantitative score for each domain. The individual ratings are made using a Likert scale ranging from 0 (e.g., significant lack of motivation interferes with routine tasks) to 6 (e.g., no evidence of significant lack of motivation). Each rating then can be considered as an “item,” whether used to assess outcomes or in our case, as a mediating variable.
The IM score was calculated as a sum of 3 intrapsychic deficit ratings from the QLS (purpose, motivation, and curiosity) based on our recent psychometric analyses (Nakagami et al., 2008) that indicate these items load together on one factor (loadings >0.7) with acceptable internal consistency (α = 0.74). The IM scale scores were normally distributed. Given the possible conceptual overlap between motivation and negative symptoms, we conducted preliminary analyses and found that the Pearson correlation between motivation and the negative symptom factor of the BPRS-E in this sample (r = 0.19, p < 0.01) did not approach a level that would be considered psychometric convergence; suggesting that as conceptualized and measured, intrinsic motivation is not a proxy for negative symptoms.
Ethnic Minority Status
Our sample consisted of persons of diverse ethnic or racial backgrounds, yet cross-group comparisons were not feasible due to the small sample size of certain groups. Instead, ethnic minority status was used as a proxy variable for cultural influences associated with ethnic or racial groups (Brekke and Barrio, 1997). This potential moderator was examined to determine whether intrinsic motivation differentially mediated clinical status and functional outcomes for persons identified either as ethnic or racial minorities (i.e., African Americans, Asians, Latinos, and unspecified “others”) versus nonminorities (i.e., European Americans not of Latino heritage).
Data Analysis
Preliminary descriptive analyses of the sociodemographic and clinical characteristics of the sample were conducted. Pearson correlation analyses were performed to test the hypotheses and to determine if the conditions required to test the mediation model were met.
Mediation Model
We used multiple regression to address the mediation effect of intrinsic motivation on the relationship between clinical status and functional outcomes, using Baron and Kenny’s (1986) mediation model. This model proposes that intrinsic motivation can be considered a mediator of a relationship between clinical symptoms and functional outcomes only if 4 conditions are met: (1) the bivariate relationship between the independent variables (clinical status) and the dependent variable (functional outcome) must be statistically significant; (2) the bivariate relationship between the independent variables (clinical status) and the mediator (intrinsic motivation) must be statistically significant; (3) the bivariate relationship between the mediator (intrinsic motivation) and dependent variable (functional outcome) must be statistically significant, controlling for the independent variables (clinical status); and (4) when the mediator (intrinsic motivation) is controlled for, the effects of the independent variables (clinical status) on the dependent variable (functional outcome) must be significantly attenuated or rendered nonsignificant. To explore variation in the efficacy of the model for the indicators of clinical status, the mediation model was tested independently for each BPRS-E scale score that met Baron and Kenny’s criteria for full mediation. In addition, as recommended to test the significance of mediation models (Mallinckrodt et al., 2006), we used Prodclin 2.0 software (MacKinnon et al., 2007b) to calculate asymmetric confidence intervals. A mediated effect is supported if the confidence interval does not include a 0 value.
Moderated Mediation Model
To determine if there was ethnic minority status variation in outcomes on study variables, multivariate analyses of variance (MANOVA) was first performed. Then, the moderated mediation model approach (Edwards and Lambert, 2007) was used to determine if the mediator exerted the same influence when minority status was considered. In moderated mediation, the strength of the indirect effect of the mediator is affected by the level of the moderator (MacKinnon et al., 2007a). To prevent multicollinearity, each variable was mean-centered, and interaction terms were computed from these centered variables (Aiken and West, 1991).
RESULTS
Sample Characteristics
One hundred twelve (67.5%) participants were male, with an average age of 38 (±9) years. The ethnic/racial breakdown consisted of 70 (42.2%) European-Americans, 66 (39.8%) African-Americans, 19 (11.4%) Latinos, 7 (4.2%) Asians, and 4 (2.4%) “otherwise classified.” On average participants reported 11.94 (±2) years of education. No statistically significant differences in the sociodemographic characteristics between ethnic minority (n = 96) and non-minority (n = 70) participants were found.
The means and standard deviation of functional status indicators (symptoms, functioning, and intrinsic motivation) of the sample are presented in Table 1. The sample reflects individuals with a relatively stable clinical presentation, with an average length of illness of 13.68 (±9.91) years. Mean scores on the BPRS-E clinical status variables indicate the presence of relatively mild to moderate psychiatric symptoms while the RFS score represents fairly severe impairment in functioning. For example, nearly 60% of the current sample had scores on the RFS indicating severely limited productivity, 65% had limited self care and independent living skills, and approximately 66% had score indicative of limited social interaction. The mean IM score suggests a rather low degree of motivation that may moderately impair performing tasks or completing goals; approximately 75% of the sample reported significant underachievement in some life domains.
TABLE 1.
Pearson Correlations, Means and Standard Deviations of the Clinical Status,a Mediator (Intrinsic Motivation),b and Functional Outcomesc
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1 BPRS-E Positive | — | |||||||
| 2 BPRS-E Negative | −0.046 | — | ||||||
| 3 BPRS-E Activation | 0.426* | −0.053 | — | |||||
| 4 BPRS-E Affectd | 0.099 | −0.006 | −.020 | — | ||||
| 5 BPRS-E Disorge | 0.611* | 0.053 | 0.795* | −0.081 | — | |||
| 6 BPRS-E Global | 0.774* | 0.105 | 0.632* | 0.522* | 0.634* | — | ||
| 7 Motivation | −0.305* | −0.198** | −0.271* | 0.038 | −0.362* | −0.282* | — | |
| 8 RSF total | −0.282* | −0.150** | −0.146 | 0.072 | −0.234* | −0.189** | 0.508* | — |
| Mean | 11.295 | 4.307 | 8.699 | 8.139 | 5.843 | 39.271 | 8.434 | 8.319 |
| Standard deviation | 5.432 | 2.094 | 3.805 | 4.076 | 2.781 | 10.522 | 4.034 | 3.552 |
Expanded Brief Psychiatric Rating Scale (Lukoff et al., 1986).
Intrinsic Motivation subscale from the Quality of Life Scale (Heinrichs et al., 1984).
Role Functioning Scale (Goodman et al., 1993).
Affect = the Anxiety/Depression factor of the BPRS-E.
Disorg = the Disorganization factor of the BPRS-E.
p < 0.01;
p ≤ 0.05; two-tailed.
No significant differences based on ethnic minority status were found on any functional status indicators except for intrinsic motivation (T [164] = 2.44, p = 0.016). Persons assigned to the ethnic minority category (M = 7.88 ± 3.99) had a lower IM scale score than did persons without this designation (M = 9.31 ± 4.14).
Bivariate Analyses to Test the Hypotheses
Our hypothesis testing was supported by the strength and significance of the correlation analyses (Table 1). With the exception of the BPRS-E affect factor, all clinical status variables correlated with the IM scale score. The RFS score was strongly correlated with the IM scale score.
Bivariate Analyses to Test the Conditions for the Mediation Model
Table 1 also illustrates which correlations were statistically significant and established necessary conditions for testing the meditational model. Clinical status was negatively associated with functional outcomes for all BPRS-E scores, except for those from the Affect and Activation factors. In not correlating with the RFS scale score, these 2 factors did not meet the first criterion for the meditational model and were not tested further. Based on findings of a statistically significant association (p ≤ 0.05) between clinical status and the mediator variable, intrinsic motivation (2nd criterion of the mediation model), the mediation model was testable for the remaining 4 most diagnostically relevant types of symptoms for schizophrenia: Global BPRS-E score, and the Positive, Negative, and Disorganized symptom factor scores.
Intrinsic Motivation Mediation Model
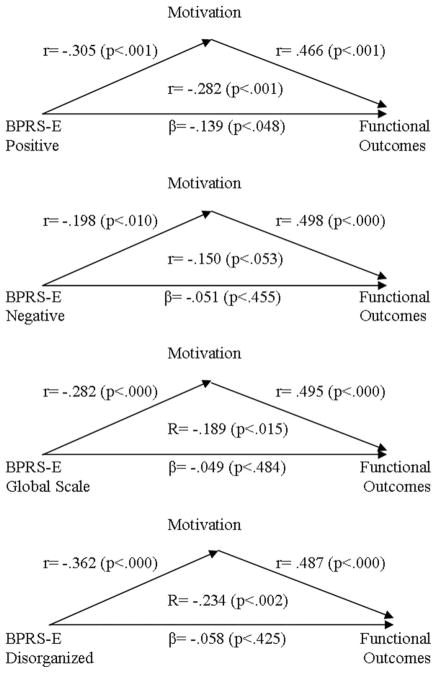
As indicated in Figure 1, the Positive symptom score was significantly associated with the global RFS score. Individuals with higher positive symptoms tended to report lower functioning. The Positive score was also negatively related to the IM score, reflecting that the greater the severity of positive psychotic symptoms, the lower the level of intrinsic motivation. A greater degree of motivation was also associated with higher functioning. The relationship between the Positive factor score and the RFS Total score was significantly reduced, though not eliminated, after controlling for the effect of the IM score, indicating a significant mediation effect (95% asymmetric CI range from −0.155 to −0.043). We conducted a post hoc analysis and determined that after controlling for the effects of intrinsic motivation, the item tapping symptoms of grandiosity continued to correlate significantly with functioning (partial r = −0.22).
FIGURE 1.
Based on the Mediation Model (Baron and Kenny, 1986), relationships between clinical status (BPRS-E scores: Positive factor, Negative factor, and Global Scale scores) and functional outcomes (RFS total score) and as mediated by Intrinsic Motivation. Standardized regression coefficients (βs) are presented. For the direct paths from the clinical status to functional outcome scores, coefficients from the unmediated models were presented inside the diagram, with the coefficients from the mediated models underneath, outside of the triangle.
Following the same steps, the findings indicated a statistically significant relationship between the BPRS-E Negative score and the RFS Total score. This relationship became nonsignificant after including the IM score as a mediating variable; this suggests a full mediation effect (95% asymmetric CI range from −0.248 to −0.001). The significant association between the BPRS-E Global scale score and the RFS Total score became nonsignificant after controlling for the effect of the IM score indicating a full mediation effect (95% asymmetric CI range from −0.078 to −0.021). Likewise, there was a significant relationship between the BPRS-E Disorganized factor score and the RFS Total score which became nonsignificant after including the IM score as a mediating variable (95% asymmetric CI range from −0.364 to −0.114).
Moderated Mediation Model for Ethnic Minority Status
The results of our analyses did not support a moderation effect of ethnic minority status on the relationship between the clinical status variables and the RFS Total score after controlling for the IM score. We also tested whether the relationship between the IM score and the RFS Total score differed by ethnic minority status and there was no statistically significant moderation effect on the relationship between motivation and functional outcomes (p > 0.05 for all interaction effects).
DISCUSSION
This study extends previous literature by establishing the relationship of intrinsic motivation as a mediator between clinical status and functional outcomes among an ethnically/racially diverse sample of treatment-seeking individuals with schizophrenia spectrum disorders. Motivation was a statistically significant mediator of the relationship between functioning and global, positive, negative, and disorganized symptom scores. Further, with the exception of the positive symptom score, we found that the impact of psychiatric symptoms on functioning is fully mediated by intrinsic motivation. The results suggest that intrinsic motivation exerts strong influence on functional outcomes, largely beyond that of clinical status. While this is similar to findings from previous studies (Bellack, 2006) which suggest that symptoms are not a strong determinant of functioning in community samples, we extend these findings by suggesting that the impact that symptoms might have on functioning is through their relationship with intrinsic motivation.
Our results suggest that intrinsic motivation may be part of the explanation for the relationship observed between clinical status and functional outcomes, yet much work is needed to determine the underlying mechanisms. A vast pool of interdisciplinary literature exists to inform the study of intrinsic motivation for schizophrenia. Possible approaches include: application of social psychological theories (Shah and Gardner, 2008) that appear to fit well within the recovery framework for individuals with schizophrenia; review of clinical practice literature from within health and allied sciences, stretching back into the early 1970s (Lane and Barry, 1970; Swanson and Woolson, 1973); greater integration of basic science literature on motivation in the context of attitudes-behaviors into clinical practice (Fishbein, 1980); examination of the potential generalizability of outcomes established with children with developmental disabilities (e.g., Lecavalier and Tassé, 2002); and consideration of underlying neurocognitive and physiological components (e.g., Murray et al., 2008; Nakagami et al., 2008).
By examining ethnic minority status as a moderator in the mediation model we were able to approximate whether underlying sociocultural issues tied to ethnic/racial minority status might influence the findings. Differences in culture that influence self views were not assessed in this study, but have been found in a similar sample of individuals with schizophrenia (Brekke and Barrio, 1997). For example, European Americans with independent, individualistic views of self tend to be internally motivated by self-interest and curiosity, while ethnic minorities in the United States tend to have higher interdependent self views and place great value on social relationships and external influences on their behavior (Gaines et al., 1997; Markus and Kitayama, 1991). If such a difference in self views exists in the current sample, it might help explain why persons in the ethnic minority group scored lower on intrinsic motivation than did individuals in the nonethnic minority group. The lack of moderation effect for ethnic minority status could reflect the sample characteristics; Latinos were likely to be well acculturated as they were proficient in English, able to use mental health services and to meet enrollment criteria for the research study.
Given the strong impact of intrinsic motivation on functioning, our findings suggest several treatment implications for individuals with schizophrenia. Drawing from social psychological research (Shah and Gardner, 2008), we highlight possible ways that intrinsic motivation could be considered in designing theory based interventions for increasing functioning of individuals with schizophrenia. These approaches are designed to address functioning regardless of the level of most clinical symptoms. The presence of severe positive symptoms such as grandiosity may require additional interventions beyond the scope of our discussion.
Motivational interviewing (Miller and Rollick, 2002) based on the Stages of Change theory (Prochaska and DiClemente, 1983), has been recognized as one technique to facilitate goal setting and illness management required to increase functioning (Carey et al., 2001). There is some empirical evidence of the effectiveness of motivational interviewing techniques for people with schizophrenia (Kemp et al., 1996; Barrowclough et al., 2001); these techniques have been effectively adapted as a part of best-practices for the treatment of people with dual diagnoses (Drake et al., 2001; Ziedonis et al., 2005). Intrinsic motivation can be embedded as an element of established interventions. Cognitive-training interventions to increase self-efficacy have been shown to be more effective when motivation is included as a primary focus (Medalia and Richardson, 2005; Silverstein and Wilkniss, 2004). Intrinsic motivation also can be considered as a core feature that can impact the process of delivering psychosocial interventions. Motivation is enhanced when the social context makes an individual feel autonomous and in control of his or her outcomes and when information is provided about the individual’s competence at navigating the social environment (Ryan and Deci, 2000). Self-determination theory which suggests that competence, autonomy, and relatedness are necessary conditions to foster intrinsic motivation (Ryan and Deci, 2000) could guide efforts to enhance these components embedded within the recovery model. The full extent of how to translate research findings on intrinsic motivation into clinical practice approaches to improve functional outcomes is an area in need of further study.
Several limitations warrant consideration in terms of interpreting our findings and also as indicators for future research directions. Our cross-sectional study design measured clinical status and functional outcomes prior to receipt of psychosocial rehabilitation services. Further research is needed to examine whether intrinsic motivation affects the rate or degree of change in symptoms and functioning throughout the course of treatment.
Our findings may not generalize to individuals with unstable or significant clinical symptoms or to persons of specific ethnic or racial subgroups as our sample size and composition precluded examination of a broad spectrum of these populations. While ethnic minority status provided one way to explore variation in intrinsic motivation, we were unable to directly test the effects of culture. Cultural values that may affect the extent to which intrapsychic processes, such as intrinsic motivation, are emphasized and drive behavior (Silverthorne, 2005) could be tested. In addition, future studies should examine the mediation model among people with varying severity of symptoms or other clinical and sociocultural characteristics.
Our measure of intrinsic motivation was not specifically designed for this purpose. Development of an intrinsic motivation scale specific to individuals with severe and persistent mental illness, particularly for use in community-based services within complex ethnically diverse urban environments could improve the translation of these findings to practice (Barch et al., 2008). Nonetheless, our use of a brief measure consisting of scores derived from open-ended interview probes permitted a personally elaborated view of intrinsic motivation and expanded the literature concerning individuals with schizophrenia.
We have much to learn about intrinsic motivation in the context of schizophrenia. While intrinsic motivation appears to be related to external reinforcers (Deci et al., 1999), the optimal level or arrangement of motivation and reinforcers for sustaining functional outcomes is not known. Exploration of the additive effect and types of positive symptoms and their relationships to intrinsic motivation may be one avenue to pursue. Testing of various mediating or moderating variables would also contribute to our understanding of the influence of intrinsic motivation. Potential variables of interest include: clinical and sociodemographic characteristics or intrapsychic factors such as emotions, empowerment, self efficacy, autonomy, and illness insight (Bandura, 1991; Gharabawi et al., 2007; Herbener, 2008; Ryan, 2007).
CONCLUSION
Within the psychosocial rehabilitation domain, there remains a need to establish an evidence-base supporting the value of intrinsic motivation for provision of effective services to individuals with schizophrenia (e.g., Choi and Medalia, 2005; Sells et al., 2006). Recovery-oriented psychosocial services are positioned to directly evaluate, monitor, and when necessary intervene to enhance the intrinsic motivation level of individuals with schizophrenia. This study highlights the critical role of intrinsic motivation as an explanatory variable in the course and outcome of schizophrenia. Our findings have the potential to move the field forward by opening up a new avenue of research to explore this construct further as well as to develop both psychosocial and pharmacological interventions that target intrinsic motivation.
Acknowledgments
The authors thank Patricia C. Seaborg, MSW, LCSW; Kimmy Kee, PhD; and Eri Nakagami, PhD, for contributions to previous drafts; and Leigh Quijada, MSW, for editorial assistance.
Supported by the following NIMH grant: R-01 MH 53282 Predicting Psychosocial Rehabilitation Service Outcomes (J. Brekke, PI).
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interaction. Newbury Park (CA): Sage; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington (DC): American Psychiatric Association; 1994. [Google Scholar]
- Anthony WA, Rogers ES, Cohen M, Davies RR. Relationships between psychiatric symptomatology, work skills and future vocational performance. Psychiatr Serv. 1995;46:353–358. doi: 10.1176/ps.46.4.353. [DOI] [PubMed] [Google Scholar]
- Bae SW, Brekke JS, Bola JR. Ethnicity and treatment outcome variation in schizophrenia: A longitudinal study of community based psychosocial rehabilitation interventions. J Nerv Ment Dis. 2004;192:623–628. doi: 10.1097/01.nmd.0000140035.36075.7f. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self regulation of motivation through anticipatory and self regulatory mechanisms. In: Dienstbier RA, editor. Perspectives on Motivation: Nebraska Symposium on Motivation. Vol. 38. Lincoln (NE): University of Nebraska Press; 1991. pp. 69–164. [PubMed] [Google Scholar]
- Barch DM. The relationships among cognition, motivation and emotion in schizophrenia: How little we know. Schizophr Bull. 2005;31:875–881. doi: 10.1093/schbul/sbi040. [DOI] [PubMed] [Google Scholar]
- Barch DM, Yodkovik N, Sypher-Locke H, Hanewinkel M. Intrinsic motivation in schizophrenia: Relationships to cognitive function, depression, anxiety and personality. J Abnorm Psychol. 2008;117:776–787. doi: 10.1037/a0013944. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrio C. Culture and schizophrenia: A cross ethnic growth curve analysis. J Nerv Ment Dis. 2001;189:676–684. doi: 10.1097/00005053-200110000-00004. [DOI] [PubMed] [Google Scholar]
- Barrio C, Yamada AM, Hough R, Hawthorne W, Garcia P, Jeste DV. Ethnic disparities in use of public mental health case management services among patients with schizophrenia. Psychiatr Serv. 2003;54:1264–1270. doi: 10.1176/appi.ps.54.9.1264. [DOI] [PubMed] [Google Scholar]
- Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O’Brien R, Schofield N, McGovern J. Randomized controlled trial of motivational interviewing, cognitive behavior therapy and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psychiatry. 2001;158:1706–1713. doi: 10.1176/appi.ajp.158.10.1706. [DOI] [PubMed] [Google Scholar]
- Bellack AS. Scientific and consumer models of recovery in schizophrenia: Concordance, contrasts and implications. Schizophr Bull. 2006;32:432–442. doi: 10.1093/schbul/sbj044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real world functional performance in schizophrenia subjects: Correlations with cognition, functional capacity and symptoms. Am J Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- Boydell KM, Gladstone BM, Volpe T. Interpreting narratives of motivation and schizophrenia: A biopsychosocial understanding. Psychiatr Rehabil J. 2003;26:422–426. doi: 10.2975/26.2003.422.426. [DOI] [PubMed] [Google Scholar]
- Breier A, Schreiber JL, Dyer J, Pickar D. National institute of mental health longitudinal study of chronic schizophrenia. Prognosis and predictors of outcome. Arch Gen Psychiatry. 1991;48:239–246. doi: 10.1001/archpsyc.1991.01810270051007. [DOI] [PubMed] [Google Scholar]
- Brekke J, Barrio C. Cross-ethnic symptom differences in schizophrenia: The influence of culture and minority status. Schizophr Bull. 1997;23:305–316. doi: 10.1093/schbul/23.2.305. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Hoe M, Long J, Green MF. How neurocognition and social cognition influence functional change during community based psychosocial rehabilitation for individuals with schizophrenia. Schizophr Bull. 2007;33:1247–1256. doi: 10.1093/schbul/sbl072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brekke JS, Kay DD, Kee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–235. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Levin S, Wolkon GH, Sobel E, Slade ES. Psychosocial functioning and subjective experience in schizophrenia. Schizophr Bull. 1993;19:599–608. doi: 10.1093/schbul/19.3.599. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Long JD, Nesbitt N, Sobel E. The impact of service characteristics on functional outcomes from community support programs for persons with schizophrenia: A growth curve analysis. J Consult Clin Psychol. 1997;65:464–475. doi: 10.1037//0022-006x.65.3.464. [DOI] [PubMed] [Google Scholar]
- Bruner JS. The Culture of Education. Cambridge (MA): Harvard University Press; 1996. [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Purnine DM. The feasibility of enhancing psychiatric outpatients’ readiness to change their substance use. Psychiatr Serv. 2002;53:602–608. doi: 10.1176/appi.ps.53.5.602. [DOI] [PubMed] [Google Scholar]
- Carey KB, Purnine DM, Maisto SA, Carey MP. Enhancing readiness to change substance abuse in persons with schizophrenia. A four session motivation based intervention. Behav Modif. 2001;25:331–384. doi: 10.1177/0145445501253001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Medalia A. Factors associated with a positive response to cognitive remediation in a community psychiatric sample. Psychiatr Serv. 2005;56:602–604. doi: 10.1176/appi.ps.56.5.602. [DOI] [PubMed] [Google Scholar]
- Choi J, Mogami T, Medalia A. Intrinsic motivation inventory: An adapted measure for schizophrenia research. Schizophr Bull. doi: 10.1093/schbul/sbp030. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, Koestner R, Ryan R. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull. 1999;125:627–668. doi: 10.1037/0033-2909.125.6.627. [DOI] [PubMed] [Google Scholar]
- Deci E, Ryan RM. Intrinsic Motivation and Self-Determination in Human Behavior. New York (NY): Plenum; 1985. [Google Scholar]
- Drake RE, Essock SM, Shaner A, Carey KB, Minkoff K, Kola L, Lynde D, Osher FC, Clark RE, Rickards L. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr Serv. 2001;52:469–476. doi: 10.1176/appi.ps.52.4.469. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Edwards JR, Lambert LS. Methods for integrating moderation and mediation: A general analytical framework using moderated path analysis. Psychol Methods. 2007;12:1–22. doi: 10.1037/1082-989X.12.1.1. [DOI] [PubMed] [Google Scholar]
- Ferdinandi AD, Yoottanasumpun V, Pollack S, Bermanzohn PC. Predicting rehabilitation outcome among patients with schizophrenia. Psychiatr Serv. 1998;49:907–909. doi: 10.1176/ps.49.7.907. [DOI] [PubMed] [Google Scholar]
- Fishbein M. A theory of reasoned action: Some applications and implications, Nebraska symposium on motivation 1979: Beliefs, attitudes and values. Lincoln (NE/London): University of Nebraska Press; 1980. [PubMed] [Google Scholar]
- Fogel BS. A neuropsychiatric approach to impairment of goal directed behavior. Am Psychiatr Press Rev Psychiatry. 1996;15:163–173. [Google Scholar]
- Fowles DC. A Motivational Theory of Psychopathology. Lincoln (NE): University of Nebraska Press; 1994. [PubMed] [Google Scholar]
- Gaines SO, Marelich WD, Bledsoe KL, Steers WN, Henderson MC, Granrose CS, Barajas L, Hicks D, Lyde M, Takahashi Y, Yum N, Rios DL, Garcia BF, Farris KR, Page MS. Links between race/ethnicity and cultural values as mediated by racial/ethnic identity and moderated by gender. J Pers Soc Psychol. 1997;72:1460–1476. doi: 10.1037//0022-3514.72.6.1460. [DOI] [PubMed] [Google Scholar]
- Gharabawi G, Bossie C, Turkoz I, Kujawa M, Mahmoud R, Simpson G. The impact of insight on functioning in patients with schizophrenia or schizo-affective disorder receiving risperidone long acting injectable. J Nerv Ment Dis. 2007;195:976–982. doi: 10.1097/NMD.0b013e31815c1982. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Sewell DR, Cooley EL, Leavitt N. Assessing levels of adaptive functioning: The role functioning scale. Community Ment Health J. 1993;29:119–131. doi: 10.1007/BF00756338. [DOI] [PubMed] [Google Scholar]
- Heinrichs DW, Hanlon TE, Carpenter WT., Jr The quality of life scale: An instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: A quantitative review of the evidence. Neuropsychology. 1998;12:426–445. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- Henry AD, Barreira P, Banks S, Brown JM, McKay C. A retrospective study of clubhouse based transitional employment. Psychiatr Rehabil J. 2001;24:344–354. doi: 10.1037/h0095070. [DOI] [PubMed] [Google Scholar]
- Herbener ES, Song W, Khine TT, Sweeney JA. What aspects of emotional functioning are impaired in schizophrenia? Schizophr Res. 2008;98:239–246. doi: 10.1016/j.schres.2007.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanfer R, Ackerman PL. Individual differences in work motivation: Further explorations of a trait framework. Appl Psychol: An Int Rev. 2000;49:470–482. [Google Scholar]
- Kemp R, Hayyward P, Applewhaite G, Everitt B, David A. Compliance therapy in psychotic patients: Randomised controlled trial. BMJ. 1996;312:345–349. doi: 10.1136/bmj.312.7027.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopelowicz A, Liberman RP, Zarate R. Recent advances in social skills training for schizophrenia. Schizophr Bull. 2006;32(suppl 1):S12–S23. doi: 10.1093/schbul/sbl023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopelowicz A, Ventura J, Liberman RP, Mintz J. Consistency of brief psychiatric rating scale factor structure across a broad spectrum of schizophrenia patients. Psychopathology. 2008;41:77–84. doi: 10.1159/000111551. [DOI] [PubMed] [Google Scholar]
- Lane JM, Barry JR. Recent research on client motivation. Rehabil Res Pract Rev. 1970;1:5–25. [Google Scholar]
- Lecavalier L, Tassé MJ. Sensitivity theory of motivation and psychopathology: An exploratory study. Am J Ment Retard. 2002;107:105–115. doi: 10.1352/0895-8017(2002)107<0105:STOMAP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB, Goldberg R, Green Paden LD, Tenhula WN, Boerescu D, Tek C, Sandson N, Steinwachs DM. The Schizophrenia Patient Outcomes Research Team (PORT): Updated treatment recommendations 2003. Schizophr Bull. 2004;30:193–217. doi: 10.1093/oxfordjournals.schbul.a007071. [DOI] [PubMed] [Google Scholar]
- Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry. 2002;14:256–272. [Google Scholar]
- Liddle PF, Barnes TR. Syndromes of chronic schizophrenia. Br J Psychol. 1990;157:558–561. doi: 10.1192/bjp.157.4.558. [DOI] [PubMed] [Google Scholar]
- Lukoff D, Nuechterlein KH, Ventura J. Manual for expanded Brief Psychiatric Rating Scale (BPRS) Schizophr Bull. 1986;12:594–602. [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007a;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behav Res Methods. 2007b;39:384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallinckrodt B, Abraham WT, Wei M, Russell DW. Advances in testing the statistical significance of mediation effects. J Couns Psychol. 2006;53:372–378. [Google Scholar]
- Markus H, Kitayama S. Culture and the self: Implications for cognitive, emotion and motivation. Psychol Rev. 1991;98:224–253. [Google Scholar]
- Medalia A, Richardson R. What predicts a good response to cognitive remediation interventions? Schizophr Bull. 2005;31:942–953. doi: 10.1093/schbul/sbi045. [DOI] [PubMed] [Google Scholar]
- Mee J, Sumsion T. Mental health clients confirm the motivating power of occupation. Br J Occup Ther. 2001;64:121–128. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2. New York (NY): Guilford; 2002. [Google Scholar]
- Mueser KT, Curran PJ, McHugo GJ. Factor structure of the brief psychiatric rating scale in schizophrenia. Psychol Assess. 1997;9:196–204. [Google Scholar]
- Mueser KT, Salyers MP, Mueser PR. A prospective analysis of work in schizophrenia. Schizophr Bull. 2001;27:281–296. doi: 10.1093/oxfordjournals.schbul.a006874. [DOI] [PubMed] [Google Scholar]
- Murphy H, Roopchand N. Intrinsic motivation and self-esteem in traditional and mature students at a post-1992 university in the north-east of England. Educ Stud. 2003;29:243–259. [Google Scholar]
- Murray GK, Clark L, Corlett PR, Blackwell AD, Cools R, Jones PB, Robbins TW, Poustka L. Incentive motivation in first-episode psychosis: A behavioural study. BMC Psychiatry. 2008;8:1–7. doi: 10.1186/1471-244X-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: Testing mediator and moderator effects. Schizophr Res. 2008;105:95–104. doi: 10.1016/j.schres.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Nelson G, Aubry T, Lafrance A. A review of the literature on the effectiveness of housing and support, assertive community treatment and intensive case management interventions for persons with mental illness who have been homeless. Am J Orthopsychiatry. 2007;77:350–361. doi: 10.1037/0002-9432.77.3.350. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Klapow JC, Eastham JH, Heaton RK, Evans JD, Koch WL, Jeste DV. Correlates of functional status in older patients with schizophrenia. Psychiatry Res. 1998;80:41–52. doi: 10.1016/s0165-1781(98)00060-2. [DOI] [PubMed] [Google Scholar]
- Perivoliotis D, Granholm E, Patterson TL. Psychosocial functioning on the independent living skills survey in older outpatients with schizophrenia. Schizophr Res. 2004;69:307–316. doi: 10.1016/j.schres.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Phillips E, Barrio C, Brekke J. The impact of ethnicity on prospective functional outcomes from community based psychosocial rehabilitation for persons with schizophrenia. J Community Psychol. 2001;29:657–673. [Google Scholar]
- Pittman TS. Motivation. In: Gilbert DT, Fiske ST, Lindzey G, editors. The Handbook of Social Psychology. Vol. 4. New York (NY): Oxford University Press; 1998. pp. 549–590. [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Ryan RM. Control and information in the intrapersonal sphere: An extension of cognitive evaluation theory. J Pers Soc Psychol. 1982;43:450–461. [Google Scholar]
- Ryan RM. Motivation and emotion: A new look and approach for two reemerging fields. Motiv Emot. 2007;31:1–3. [Google Scholar]
- Ryan RM, Deci EL. Self determination theory and the facilitation of intrinsic motivation, social development and well being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Schmand B, Kuipers T, Van der Gaag M, Bosveld J, Bulthuis F, Jellema M. Cognitive disorders and negative symptoms as correlates of motivational deficits in psychotic patients. Psychol Med. 1994;24:869–884. doi: 10.1017/s0033291700028968. [DOI] [PubMed] [Google Scholar]
- Sells D, Davidson L, Jewell C, Falzer P, Rowe M. The treatment relationship in peer based and regular case management for clients with severe mental illness. Psychiatr Serv. 2006;57:1179–1184. doi: 10.1176/ps.2006.57.8.1179. [DOI] [PubMed] [Google Scholar]
- Shah JY, Gardner WL. Handbook of Motivation Science. New York (NY): Guilford; 2008. [Google Scholar]
- Silverstein SM, Wilkniss SM. At issue: The future of cognitive rehabilitation of schizophrenia. Schizophr Bull. 2004;30:679–692. doi: 10.1093/oxfordjournals.schbul.a007122. [DOI] [PubMed] [Google Scholar]
- Silverthorne CP. Organizational Psychology in Cross-Cultural Perspective. New York (NY): New York University Press; 2005. [Google Scholar]
- Summerfelt AT, Alphs LD, Funderburk FR, Strauss ME, Wagman AM. Impaired wisconsin card sort performance in schizophrenia may reflect motivational deficits. Arch Gen Psychiatry. 1991;48:282–283. doi: 10.1001/archpsyc.1991.01810270094019. [DOI] [PubMed] [Google Scholar]
- Swanson MG, Woolson AM. Psychotherapy with the unmotivated patient. Psychother: Theor Res Pract. 1973;10:175–183. [Google Scholar]
- Trauer T. Symptom severity and personal functioning among patients with schizophrenia discharged from long term hospital care into the community. Community Ment Health J. 2001;37:145–155. doi: 10.1023/a:1002761732040. [DOI] [PubMed] [Google Scholar]
- Van der Does AJ, Linszen DH, Dingemans PM, Nugter MA, Scholte WF. A dimensional and categorical approach to the symptomatology of recent onset schizophrenia. J Nerv Ment Dis. 1993;181:744–749. doi: 10.1097/00005053-199312000-00006. [DOI] [PubMed] [Google Scholar]
- Velligan D, Prihoda T, Dennehy E, Biggs M, Shores Wilson K, Crismon ML, Rush AJ, Miller A, Suppes T, Trivedi M, Kashner TM, Witte B, Toprac M, Carmody T, Chiles J, Shon S. Brief psychiatric rating scale expanded version: How do new items affect factor structure? Psychiatry Res. 2005;135:217–228. doi: 10.1016/j.psychres.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the brief psychiatric rating scale: ‘The drift busters.’. Int J Methods Psychiatr Res. 1993;3:221–244. [Google Scholar]
- Wieduwilt KM, Jerrell JM. Measuring sensitivity to change of the role functioning scale using the RCID index. Int J Methods Psychiatr Res. 1998;7:163–170. [Google Scholar]
- Ziedonis DM, Smelson D, Rosenthal RN, Batki SL, Green AI, Henry RJ, Montoya I, Parks J, Weiss RD. Improving the care of individuals with schizophrenia and substance use disorders: Consensus recommendations. J Psychiatr Pract. 2005;11:315–339. doi: 10.1097/00131746-200509000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]