Abstract
Background
Effective surveillance for infectious diseases is an essential component of public health. There are few studies estimating the cost-effectiveness of starting or improving disease surveillance. We present a cost-effectiveness analysis the Integrated Disease Surveillance and Response (IDSR) strategy in Africa.
Methodology/Principal Findings
To assess the impact of the IDSR in Africa, we used pre- and post- IDSR meningococcal meningitis surveillance data from Burkina Faso (1996–2002 and 2003–2007). IDSR implementation was correlated with a median reduction of 2 weeks to peak of outbreaks (25th percentile 1 week; 75th percentile 4 weeks). IDSR was also correlated with a reduction of 43 meningitis cases per 100,000 (25th–40: 75th-129). Assuming the correlations between reductions in time to peak of outbreaks and cases are related, the cost-effectiveness of IDSR was $23 per case averted (25th-$30; 75th - cost saving), and $98 per meningitis-related death averted (25th-$140: 75th – cost saving).
Conclusions/Significance
We cannot absolutely claim that the measured differences were due to IDSR. We believe, however, that it is reasonable to claim that IDSR can improve the cost-effectiveness of public health surveillance.
Introduction
More than 1.5 million children die each year in sub-Saharan Africa, from diarrhea, malaria, measles, meningitis, respiratory infections, yellow fever, and HIV/AIDS [1]–[6]. Well known and effective interventions are available for controlling and preventing the diseases that cause these deaths but they are often not applied to their maximum potential [7]–[10]. The resulting deaths and the associated economic costs to society could be reduced if timely detection and control measures are implemented [11]–[13]. In response to this problem, in 1998, countries in the World Health Organization (WHO) African region adopted a regional strategy named Integrated Disease Surveillance and Response (IDSR) [14–16, Table S1]. IDSR is a strategy that seeks to strengthen the ability of national and regional public health surveillance programs. The goal of IDSR is to integrate a number of surveillance systems, both existing and newly formed. This integration should encompass all levels of public health (from the basic district-level through to the national level), and should achieve efficiencies by avoiding duplication of efforts. Areas of activity that IDSR focuses on to improve efficiency include detection and identification of public health problems, increased speed of reporting and notification (especially for immediately notifiable diseases), analysis of data and interpretation of trends, laboratory confirmation when required, decision-making about responses, monitoring of progress and regular evaluation of the surveillance system's quality (14–16). The net results of IDSR-implemented reforms in surveillance systems should be that outbreaks are detected earlier, allowing quicker public health response (e.g., vaccination campaigns).
Although considerable progress had been achieved with implementation of the IDSR strategy (see http://www.cdc.gov/idsr/implementation.htm#progress), the associated economic benefits (e.g., cases and death prevented, costs of medical treatments saved by the society, and the value of avoided year of life lost) are poorly documented. Most studies on economic evaluation of public health intervention programs in sub-Saharan Africa have focused on individual disease-specific intervention activities [17]–[23]. Relatively few studies have looked at the economic benefits of surveillance and response activities [24], [25]. In a previous study, we analyzed the costs of establishing and subsequently operating activities for detection and response to the priority diseases under the IDSR strategy [26]. We add to the literature by presenting a cost effectiveness analysis of IDSR, in which we will assume that any average reductions in health outcomes (e.g., incidence of cases and deaths, outbreak duration) were due to implementation of IDSR.
Methods
To model the cost-effectiveness of IDSR, we used data from Burkina Faso because that country had fully established IDSR leadership and structures at the national level by 2002, with implementation at regional and district levels in 2003. Burkina Faso had data, collected using the IDSR-supported surveillance systems, on several meningitis outbreaks.
The nature of disease surveillance systems makes it impossible to have a randomly controlled experiment to measure the impact of IDSR on public health outcomes. We were unable to readily collect comparable data from another country (e.g., one without IDSR systems, or one that implemented IDSR systems after Burkina Faso), and thus we were unable to conduct a comparison between countries. We therefore relied on observational (before-and-after) data from outbreaks of meningococcal meningitis to assess the possible impact of IDSR-related activities in Burkina Faso. We assumed that any correlations between the start of IDSR activities, which includes both surveillance and response to disease activity detected, and changes in the epidemiology of meningitis outbreaks were due primarily to IDSR. With this assumption, we calculated, on an outbreak basis, costs per case, per death and per sequelae prevented. There could be other reasons for any correlations that we measured (see discussion section).
As most health care and IDSR activities in Burkina Faso are funded by the government, we took the perspective of the government-funded public health care system (i.e., we only recorded costs and savings incurred by the national government); costs incurred by households were not included. All cost data were recorded in local currency values and then converted into US dollar values using the mean annual exchange rate. We used the general consumer price index from Burkina Faso [27] and a discount rate of 3% to adjust all costs into 2002 US dollars equivalent.
Epidemiological data
We obtained from the WHO Multi-Diseases Surveillance Center in Ouagadougou annual population data and district level reports of weekly meningitis cases and deaths from Burkina Faso for the years 1996–2007 (see Table S2). We then calculated the weekly incidence and mortality, expressed as cases and deaths per 100,000 inhabitants, by dividing the number of new cases and deaths occurring per week by the mean annual population of each reporting district. A 1988 study in The Gambia found that 27 out of 154 (17.5%) survivors of bacterial meningitis had generalized neurological sequelae [28] We therefore assumed 20% of meningitis survivors would have neurological defects (sequelae).
We sorted the data into two groups: before (1996–2002) and after (2003–2007) IDSR implementation at district level. During this study period, all meningitis outbreaks in Burkina Faso only occurred between January and June (23-week period). For each group, we examined the weekly incidence rates in relation to the WHO recommended alert threshold (5 cases per 100,000) and epidemic threshold (10 cases per 100,000) [29]. We defined the start (end)of an outbreak when cases in a district exceeded (returned below) the epidemic threshold. For each outbreak, we calculated the time-to-peak of the outbreak as the number of weeks elapsed from the first alert threshold to the week with the maximum weekly incidence (i.e., the peak of the outbreak). We also calculated the time to reach the median, 25th and 75th percentiles of cumulative total incidence and mortality.
For each group of outbreaks before and after IDSR implementation (start 2003), we calculated the median, 25th and 75th percentile for each of the following health outcomes: weekly and cumulative total incidence, mortality and sequelae.
Data analysis
We first plotted the average weekly incidence rates over the time period studied and the median weekly incidence and mortality before and after IDSR implementation over the 23-week period of meningitis outbreaks. We then compared the health outcomes (i.e., incidence, mortality, time to peak and time to reach a set percentile of total cases per outbreak) using the Mann-Whitney test using SAS statistical software version 9.1 (SAS Institute Inc., Cary, NC, USA). In 1996 there was an “unusually” large epidemic of meningitis in Burkina Faso. We therefore examined the influence of 1996 data on the IDSR effectiveness measures by re-running the analyses excluding 1996 data.
Response to outbreaks: Vaccine importation
As IDSR encompasses a deliberate response factor, it is plausible that vaccine imports may increase post-IDSR implementation. In order to assess potential correlation between IDSR implementation and meningococcal vaccine importation, we obtained estimates of the doses of vaccine imported by the Burkina Faso government from the WHO International Consultative Group, UNICEF, and GlaxoSmithKline Biologicals. Vaccine data were also collected from the WHO disease outbreak website (http://www.who.int/csr/don/en/index.html) (Tables S3 and S4). We statistically tested if annual importation of doses was impacted by IDSR implementation using the following general linear regression:
Where IDSR implementation period was recorded as a dummy variable (Pre-IDSR = 0; Post-IDSR = 1). We ran six models, each time varying the dependent variable (doses imported) as follows: Total annual doses imported (including 1996 data); Total annual doses imported (excluding 1996 data); Doses per 100,000 population in whole country (including 1996 data);
Doses per 100,000 population in whole country (excluding 1996 data); Doses per 100,000 population in districts where outbreaks occurred (including 1996 data); and, doses per 100,000 population in districts where outbreaks occurred (excluding 1996 data). To check for autocorrelation, we calculated the Durbin-Watson statistic for each regression.
Costs
We used the costs of IDSR-related activities reported in our previous study [26; see also Table S5]. The costs include those due to surveillance and response. In the case of meningitis, response is mostly treatment of those ill and vaccination of populations near a victim (e.g., those in the same village). The cost data for each activity included personnel, transportation items, office consumable goods, public awareness campaigns, laboratory and response materials and supplies, and capital items [26].
We also obtained direct medical care costs incurred by the government to treat a patient with meningitis related-illness at district health facility ($53) and regional hospital ($71) during the 2002 epidemic situation (unpublished data, Ministry of Health, Burkina Faso; see Table S6)). These estimates include only the immediate costs of meningitis case management (e.g., consultation and hospitalization fees, drugs and other essential consumables, and laboratory specimen testing). As the study perspective is the government-funded public health care system, we did not include the costs for transportation to the health facility, provision of long-term care for patients with severe sequelae and loss of productivity due to morbidity and premature death.
Cost-effectiveness analysis
Assuming that any measured differences between health outcomes (i.e., after IDSR minus before IDSR) are due to IDSR, we calculated the cost-effectiveness in net cost (in dollars) per outcome averted using the following general formula:
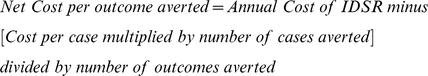 |
where outcomes averted were cases, deaths or sequelae.
We used the above formula to calculate the cost-effectiveness ratios for the median, 25th, and 75th percentiles differences in cases, deaths or sequelae averted before and after IDSR. The median (25th, 75th) cost effectiveness ratio was calculated using the median (25th, 75th) annual cost of IDSR activities In this equation, a negative result indicates net cost savings, when the cost savings of IDSR (i.e., cost of treatments avoided due to cases averted) outweigh the costs of IDSR activities (surveillance and response).
We also determined the net cost per capita of IDSR as follow:
 |
In this equation, the per capita IDSR costs were calculated using data from the whole country [26] while the costs of treatment averted come from districts that reported outbreaks.
Sensitivity analysis
Regardless of IDSR activities, any measured alteration in the epidemiology of meningitis, including any reduction in cases, could have been due to naturally occurring disease cycles. To remove any unknown effect of disease cycles or specific years, we individually compared health outcomes (incidence of cases, mortality, sequelae, and time-to-peak of outbreak) between each outbreak before IDSR and each outbreak that occurred after IDSR implementation. This analysis removes the element of time sequence, and we only compare outcomes before-versus-after the
start of IDSR. Specifically, we used the following general formula:
where X is a particular outbreak occurring after IDSR started in 2003, and Y is a particular outbreak before IDSR started.
Using this formula, we generated 9,030 paired comparisons (105 outbreaks before IDSR x 86 outbreaks after IDSR) in outcomes for each of the following variables: incidence of cases, mortality, sequelae, and time-to-peak of outbreak. We also examined the influence of 1996 data on these comparisons by re-running the simulation excluding all outbreaks that occurred in 1996 (giving 7,052 paired comparisons).
We then plotted the distribution of the differences between the paired comparisons (with and without the 1996 data) for the time to peak, and incidence of cases and mortality. We also calculated the median, 25th and 75th percentiles for the cases, deaths and sequelae averted (with and without the 1996 data). Similarly, we calculated the simple average, minimum and maximum of the differences in these health outcomes. Finally, we used the data from the paired comparisons to calculate cost-effectiveness ratios as described earlier.
Results
Health outcomes and effectiveness measures
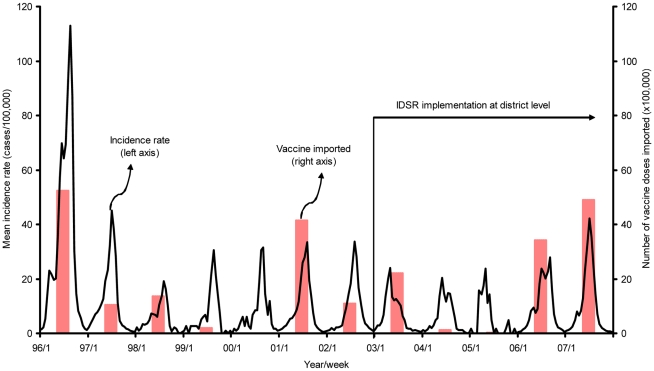
Based on our definition of outbreaks (10 per 100,000 – see earlier), we identified 105 outbreaks before adoption of IDSR and 86 after adoption of IDSR (Table S2). The mean weekly meningitis cases per outbreak recorded from 1996 to 2007 at district level in Burkina Faso are represented in Figure 1. Detailed total incidence and mortality, time-to-peak of outbreak, and time to reach a fixed percentage of total incidence and mortality rates per outbreak are showed in Table S2. The size of these outbreaks was variable and 1996 was the largest epidemic year recorded (Figure 1). We observed from Figure 1 some evidence that, after IDSR implementation in 2003, there were lower peaks-of-incidence and possibly lower cumulative total incidence-per-outbreak. However, lower peak incidence after IDSR is not uniform, as we note that the peak incidence in 2007 is greater than the peaks in all but two years (1996 and 1997) before IDSR implementation.
Figure 1. Weekly number of meningococcal meningitis cases (all serotypes) reported during the meningitis season (week 1 to 23) and number of doses of meningococcal vaccine imported from 1996 to 2007 in Burkina Faso.
Note: District level weekly new meningitis cases from Burkina Faso for the years 1996–2007 were obtained from the WHO Multi-Diseases Surveillance Center in Ouagadougou, Burkina Faso. Incidence recorded in a particular district experiencing a meningitis outbreak - the incidence data do not apply to the entire country. For list of districts reporting outbreaks recorded in this Figure, see Table S2. Doses of vaccine include all bivalent (AC), trivalent (ACW), and tetravalent (ACWY) polysaccharides imported by the government of Burkina Faso through different organizations (WHO-ICG, UNICEF, MSF, and GlaxoSmithKline Biologicals). Dates of vaccine shipment are representation for purpose of graphing (see also Tables S3 and S4).
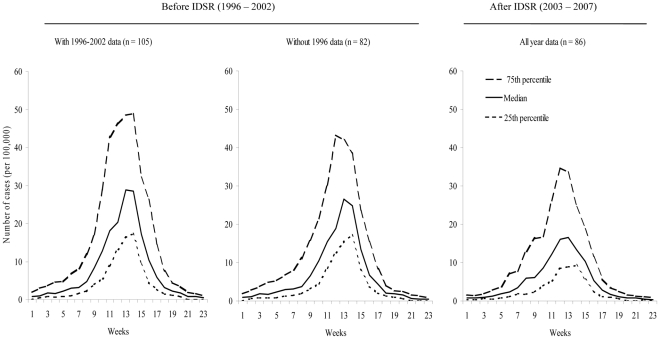
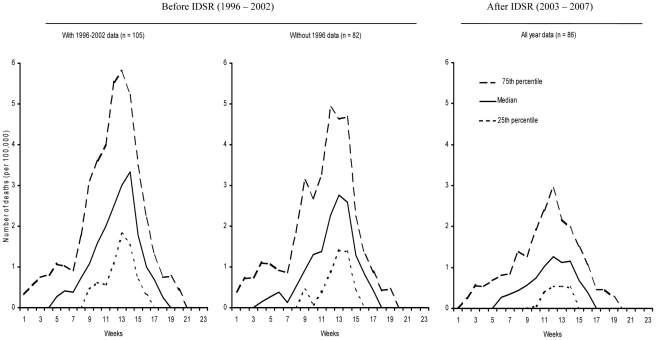
The median and the 25th and 75th percentiles of the weekly number of meningitis cases and deaths before and after IDSR implementation are presented in Figures 2 and 3, respectively. The peak of the median value of the number of meningitis cases and deaths after IDSR implementation is lower than the peaks of the before IDSR median values (with and without 1996 data). However, the 75th percentile after IDSR implementation is greater than some of the median values before IDSR, indicating that IDSR implementation does not always equate with lower number of cases (Figures 2 and 3).
Figure 2. Comparison before (1996–2002) and after (2003–2007) IDSR implementation: weekly median (25th and 75th percentiles) of new cases of meningitis per outbreak.
Note: Data source: WHO Multi-Diseases Surveillance Center, Ouagadougou, Burkina Faso. For each weekly incidence rate, we calculated the median, 25th and 75th percentile of the 105 and 82 outbreaks before IDSR and 86 outbreaks after IDSR. Before IDSR, the median (25th and 75th percentile) cumulative number of meningitis cases per outbreak was 185.0 (139.5 and 377.0) per 100,000 inhabitants when 1996 data were included and was 167.9 (135.3 and 281.0) per 100,000 inhabitants when 1996 data were excluded. After IDSR, the median (25th and 75th percentile) cumulative number of deaths per outbreak was 142.0 (100.3 and 248.2) per 100,000 inhabitants.
Figure 3. Comparison before (1996–2002) and after (2003–2007) IDSR implementation: weekly median (25th and 75th percentiles) of number of meningitis deaths per outbreak.
Data source: WHO Multi-Diseases Surveillance Center, Ouagadougou, Burkina Faso. For each weekly mortality rate, we calculated the median, 25th and 75th percentile of the 105 and 82 outbreaks before IDSR and 86 outbreaks after IDSR. Before IDSR, the median (25th and 75th percentile) cumulative number of deaths per outbreak was 23.8 (17.9 and 35.9) per 100,000 inhabitants when 1996 data were included and was 20.5 (16.1 and 30.3) per 100,000 inhabitants when 1996 data were excluded. After IDSR, the median (25th and 75th percentile) cumulative number of deaths per outbreak was 12.6 (8.8 and 21.3) per 100,000 inhabitants.
The pattern of differences in peaks is also seen when comparing cumulative cases. After IDSR implementation, the average and median (50th percentile) incidences per outbreak dropped by 135 per 100,000 and 40 per 100,000 (p-value 0.0001, Table 1), respectively. Time-to-peak, time to reach a set percentage of total cases, and time to reach a set percentage of total deaths were all reduced after IDSR; however, some p-values of the difference were greater than 0.05 (Table 1). The removal of 1996 data did reduce the size of the differences, but differences did remain, showing that IDSR implementation was correlated with reduction in incidence of cases and mortality, and time-to-peak (Table 1).
Table 1. Comparison before (1996–2002) and after (2003–2007) IDSR implementation: Total number of meningitis cases and deaths, time to peak of outbreak, and time to reach total cases and deaths.
| Including 1996 data | Excluding 1996 data | ||||||||
| Outcome measures | Before | After | Difference | p-value* | Before | After | Difference | p-value* | |
| (n = 105) | (n = 86) | (n = 82) | (n = 86) | ||||||
| Total cumulative cases (per 100,000) | |||||||||
| Mean | 346 | 211 | −135 | 0.0267 | 228 | 211 | −17 | 0.034 | |
| 25th percentile† | 140 | 100 | −40 | 135 | 100 | −35 | |||
| 50th percentile† | 185 | 142 | −43 | 168 | 142 | −26 | |||
| 75th percentile† | 377 | 248 | −129 | 281 | 248 | −33 | |||
| Total cumulative deaths (per 100,000) | |||||||||
| Mean | 35 | 16 | −19 | <0.0001 | 26 | 16 | −10 | <0.0001 | |
| 25th percentile† | 18 | 9 | −9 | 16 | 9 | −7 | |||
| 50th percentile† | 23 | 13 | −10 | 21 | 13 | −8 | |||
| 75th percentile† | 36 | 21 | −15 | 30 | 21 | −9 | |||
| Time-to-peak of outbreak§ (weeks) | |||||||||
| Mean | 6 | 4 | −2 | <0.0001 | 6 | 4 | −2 | <0.0001 | |
| 25th percentile† | 4 | 3 | −1 | 3 | 3 | 0 | |||
| 50th percentile† | 6 | 4 | −2 | 6 | 4 | −2 | |||
| 75th percentile† | 9 | 5 | −4 | 8 | 5 | −3 | |||
| Time to reach % total cases# (weeks) | |||||||||
| 25% of cases¶ | 10.5 | 10.2 | −0.3 | 0.1578 | 10.4 | 10.2 | −0.2 | 0.2954 | |
| 50% of cases¶ | 12.6 | 12 | −0.7 | 0.0123 | 12.5 | 12 | −0.5 | 0.1081 | |
| 75% of cases¶ | 14.4 | 13.6 | −0.7 | 0.015 | 14.1 | 13.6 | −0.5 | 0.0404 | |
| Time to reach % total deaths# (weeks) | |||||||||
| 25% of deaths¶ | 9.9 | 9 | −0.9 | 0.0052 | 9.6 | 9 | −0.6 | 0.0361 | |
| 50% of deaths¶ | 12.2 | 11.6 | −0.6 | 0.0193 | 11.9 | 11.6 | −0.3 | 0.1313 | |
| 75% of deaths¶ | 14 | 13.6 | −0.4 | 0.0609 | 13.7 | 13.6 | −0.1 | 0.4307 | |
*p-value of Mann-Whitney score test for two-sample groups. We compared health outcomes for each of the 105 outbreaks before IDSR with each of the 86 outbreaks after IDSR implementation. We then re-ran these paired comparisons excluding the 1996, before IDSR data. Negative figure indicates lower number per outbreak after IDSR than before IDSR implementation.
These represented the 25th percentile, 50th percentile, and 75th percentile of the total number of cases and deaths and the time to peak before and after IDSR.
Time to peak of outbreak represented the time elapsed from reaching the alert threshold of a weekly incidence of 5 cases per 100,000 inhabitants to the week with the maximum weekly incidence.
Time to reach total cases and deaths represented the time interval between the first week of each calendar year and the week during the outbreak period when the total cases and deaths were reached.
These are the average time for outbreaks to reach the 25th, 50th, and 75th percent of total cases and deaths. For example, before IDSR it took 10.5 weeks during an outbreak to reach 25% of all cases attributed to that outbreak.
Data source: WHO Multi-Disease Surveillance Center, Ouagadougou, Burkina Faso (see Table S2).
Vaccine imports
We did not find any evidence of a statistically significant correlation associated between doses of vaccine imported and outbreaks (Figure 1, Table S7). There were some obvious increases in recorded importation of vaccine in some of the years that had “large” outbreaks (e.g., 1996, 2001, and 2007). On the other hand, in some years there were little or no recorded imports, regardless of peak incidence (e.g., 1999, 2000, and 2005). We note that we had difficulty in obtaining some of the vaccine import data, particularly for the earlier years examined. We conclude that IDSR has not had an appreciable impact on doses of vaccine imported. Thus, when we considered costs associated with IDSR we did not include any costs associated with increased doses of vaccine used.
Cost-effectiveness analysis
The median net cost of averting a case of meningitis was $23 per meningitis case averted (25th percentile: $30; 75th percentile: cost savings), and the median cost per death and sequelae averted were $98 and $126, respectively (Table 2). The median cost of operating IDSR was $0.01 per capita (25th: $0.01; 75th: cost saving) (Table 2). Excluding the 1996 data notably impacted most estimated cost-effectiveness ratios. For example, excluding 1996 data caused the median cost per case averted to approximately quadruple to $80 per case averted (Table 2). We also found that removing the 1996 data increased the median cost per capita to $0.02 (Table 2).
Table 2. Cost-effectiveness (2002 US $) correlated with IDSR impact on meningitis cases and deaths averted per outbreak in Burkina Faso.
| Including 1996 data Median* | Excluding 1996 data Median* | |
| (25th 75th percentiles) | (25th 75th percentiles) | |
| Total cost of IDSR§ | 3,684 | 3,684 |
| Activities (per 100,000) | ||
| Treatment costs# | 2,675 | 1,609 |
| Avoided (per 100,000) | (2,473 8,018) | (2,175 2,037) |
| Net IDSR costs | 1,009 | 2,075 |
| (per 100,000) | (1,211 savings) | (1,509 1,647) |
| Cost per case | 23 | 80 |
| Averted | (30 savings) | (43 25) |
| Cost per death | 98 | 263 |
| Averted | (140 savings) | (207 182) |
| Cost per sequelae¶ | 126 | 669 |
| Averted | (212 savings) | (296 358) |
| Cost per capita | 0.01 | 0.02 |
| (0.01 savings) | (0.02 0.02) |
Note: We took the perspective of the government-funded public health care system. We compared health outcomes for each of the 105 outbreaks before IDSR with each of the 86 outbreaks after IDSR implementation. We then re-ran these paired comparisons excluding the 1996, before IDSR data.
*The median cost-effectiveness was calculated using the median cost of IDSR activities and the difference in the number of outcomes of the median (25th percentile –75th percentile) outbreak before and the median (25th percentile –75th percentile) after IDSR implementation, respectively.
See reference 26. No vaccine cost included because no evidence found of incremental importation of vaccine doses correlated with implementation of IDSR (see Figure 1 and also Table S7).
We estimated the treatment cost-saving by multiplying the mean medical cost ($62.25) per meningitis patient by the difference in the number of cases per outbreak that occurred before IDSR versus after IDSR.
We calculated the number of sequelae by assuming 20% of all meningitis illness-related survivors have neurological defects.
Data Source: IDSR cost data (see reference 26). We obtained annual population data and district level weekly meningitis cases and deaths from the WhO-MDSC in Ouagadougou, Burkina Faso.
Sensitivity analysis
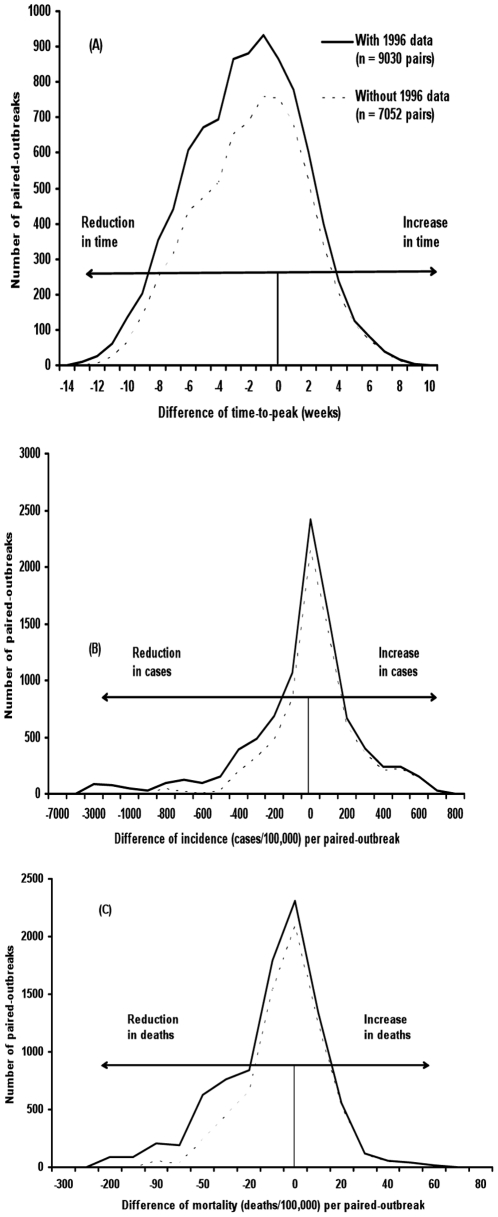
In more than 50% of the pairings in the paired outbreak analysis, which removes the influence of time and disease cycles, the outbreaks after IDSR implementation had lower incidence of cases and mortality, as well as shorter time-to-peak (Figure 4). The median, mean, maximum, and 75th percentiles of all the paired outbreaks all showed a reduction in incidence of cases, deaths and sequelae associated with outbreaks occurring after IDSR implementation (Table 3). However, the data from paired-outbreak comparisons resulted in some lower (i.e., cheaper) median cost-effectiveness estimates (Table 4).
Figure 4. Sensitivity analysis: Distribution of paired comparison of outbreaks before and after IDSR: Difference in time-to-peak, incidence rate, and mortality rate.
Note: Comparison of data of each of the 105 outbreaks before IDSR with each of the 86 outbreaks after IDSR. Removing 1996 data reduces total outbreaks before IDSR to 82. Effects on outcomes correlated with IDSR are represented on the horizontal axes: negative numbers indicated reducing effects and positive numbers indicated increasing effects on time-to-peak of outbreak (Panel A), number of cases per outbreak (Panel B), and number of deaths per outbreak (Panel C).
Table 3. Sensitivity analysis of number of meningitis cases, deaths and sequelae averted correlated with introduction of IDSR: Paired-comparison of outbreaks before (1996–2002) and after (2003–2007) IDSR implementation:
| Outcomes measures# | Including 1996 data† | Excluding 1996 data† | ||
| Median¶ | Average¶ * | Median¶ | Average¶ * | |
| (25th percentile 75th percentile) | (minimum maximum) | (25th percentile 75th percentile) | (minimum maximum) | |
| Total cumulative cases averted (per 100,000) | −48(58 −201) | −134(666 −4,769) | −27(80 −115) | −17(666 −877) |
| Total cumulative deaths averted (per 100,000) | −10(−1 −25) | −19(61 −250) | −8(1 −17) | −10(61 −102) |
| Total cumulative sequelae averted (per 100,000) | −15(18 −65) | −44(267 −2,092) | −8(25 −38) | −6(267 −375) |
We compared health outcomes for each of the 105 outbreaks before IDSR with each of the 86 outbreaks after IDSR implementation. We then re-ran these paired comparisons excluding the 1996, before IDSR data.
Number of health outcomes averted was calculated using the following equation: Outcome outbreak X after IDSR – Outcome outbreak Y before IDSR, where X for outbreak after IDSR and Y for outbreak before IDSR.
We calculated the number of sequelae by assuming 20% of all meningitis illness-related survivors have neurological defects (see main text).
Negative figure indicates reduction in cases, deaths, and sequelae per outbreak after IDSR implementation.
*These columns present the simple average, minimum and maximum of the differences in health outcomes between paired outbreaks.
Data Source: WHO Multi-Diseases Surveillance Center, Ouagadougou, Burkina Faso.
Table 4. Sensitivity analysis of total cost of IDSR, treatment cost of meningitis cases avoided, and cost-effectiveness*: Paired comparison of outbreaks before (1996–2002) and after (2003–2007) IDSR implementation.
| Including 1996 data | Excluding 1996 data | |
| Median† | Median† | |
| (25th percentile 75th percentile) | (25th percentile 75th percentile) | |
| Total cost of IDSR | 3,684 | 3,684 |
| Activities (per 100,000) | ||
| Treatment costs# | 2,982 | 1,662 |
| Avoided (per 100,000) | (−3,592 12,503) | (−4,999 7,159) |
| Net IDSR costs | 568 | 2,022 |
| (per 100,000) | (7,276 savings) | (8,683 savings) |
| Cost per case | 15 | 76 |
| Averted | (126 savings) | (108 savings) |
| Cost per death | 68 | 270 |
| Averted | (7,276 savings) | (6,679 savings) |
| Cost per sequelae | 46 | 239 |
| Averted | (408 savings) | (346 savings) |
| Cost per capita | 0.01 | 0.02 |
| (0.07 savings) | (0.09 savings) |
*We took the perspective of the government-funded public health care system. We measured the effectiveness by subtracting the number of cases, deaths, and sequelae of each of the 86 outbreaks after IDSR from each of the 105 outbreaks before IDSR. We then re-ran the analysis excluding the 1996, before IDSR data.
We calculated the median, 25th and 75th percentile cost-effectiveness based on the difference of the generated health outcomes (after IDSR versus before IDSR) distribution.
We estimated the treatment costs avoided by multiplying the mean medical cost ($62.25) per meningitis patient by the number of cases averted.
Data Source: WHO Multi-Diseases Surveillance Center, Ouagadougou, Burkina Faso. We calculated the number of sequelae by assuming 20% of all meningitis illness-related survivors have neurological defects.
Discussion
The IDSR strategy is focused on improving the collection and analysis of infectious disease surveillance data to more rapidly and accurately detect, and respond to, disease outbreaks. This should hopefully reduce the overall burden of disease [14]–[16]. Our results show that, in Burkina Faso, IDSR implementation at a district level was correlated with statistically significant reductions in time-to-peak of outbreak and reductions in total cumulative incidence of cases and mortality. Assuming that such correlations are indicative of causation, our analysis determined that the cost-effectiveness of IDSR ranged from cost savings to cost of $80 per case averted, and from cost savings to $263 per death averted. Our cost-effectiveness estimates were lower (i.e., cheaper), but not dissimilar, than earlier estimates for a meningococcal meningitis mass vaccination campaign in Burkina Faso [21], [30]. These earlier studies estimated US $133 per case and US $2,397 per death averted, uncorrected for inflation [21], [30]. Immunization campaigns in the region for yellow fever, neonatal tetanus, poliomyelitis, and diphtheria reported cost effectiveness ratios of US $281 to $20,591 per death averted [31], [32].
We could not find any statistically significant evidence of an increase in vaccine imports. We can only speculate that the reduced incidence of cases and deaths are due to IDSR allowing public health officials to better target existing resources to outbreaks. That is, the IDSR system enables public health officials to identify and get to an outbreak sooner, and be more certain which villages and areas need interventions.
The study's main limitation is the uncertainty in assuming that the reductions in cases were due to IDSR. We do not have enough evidence to claim the degree that the differences that we measured were due to IDSR. As mentioned earlier, the nature of a public health system such as IDSR prevents us from designing and conducting a controlled scientific experiment. It is possible that the changes in epidemiology that we recorded were due to changes in other factors, such as a change in the circulating serogroups and strains of Neisseria meningitidis. For the time period studied, an examination of the WHO data shows that the main circulating strain was serogroup A, although serogroup W135 co-circulated [33, Table S8]. Two studies, which analyzed in greater detail the specimens and data, found that there were some differences in strains (sequence types) of circulating serogroup A over time, with serogroup 7 recorded more frequently after 1995 – though both strains were from the same clonal group [34, 35, Table S8]. However, the sample sizes used in the studies are very small (typically less than 20 isolates per year) and are collected in a non-random fashion (i.e., convenience samples).
Other limitations include the fact that our retrospective survey may not have fully captured all data. This would be due to the limitations of public data records (e.g., no vaccine distribution and use records at country level) or “readily” accessible program records of specific public health projects (such as meningitis specific vaccine program) that run parallel to the national public health system. Further, we assumed that the accuracy of recording cases and deaths due to meningitis remained unchanged during the period studied. The implementation of IDSR could have improved accuracy, potentially increasing the estimated impact of IDSR. However, it is impossible to assess the degree, and therefore impact, of any changes in accuracy over time.
We believe, even with the study limitations, that these results indicate that IDSR is likely to be a cost-effective public health system. A completely accurate accounting of its benefits to society, such as money and lives saved has yet to be documented. It is also clear, however, that IDSR is not a complete solution to eliminating the burden of meningococcal meningitis. Given the difficulty of measuring the impact of surveillance and response systems, it may well be that policy-makers will have to make assessments of the value of IDSR and similar systems using the type of data we presented here.
Supporting Information
List of IDSR priority diseases and diseases of public health importance weekly or monthly reported in Burkina Faso during the study period.
(0.02 MB DOC)
Health outcomes and duration of meningococcal meningitis outbreak in selected districts before (1996-2002) and after (2003–2007) IDSR implementation in Burkina Faso.
(0.28 MB DOC)
Pattern of annual vaccines imported into Burkina Faso before (1996–2002) and after (2003–2008) IDSR implementation.
(0.04 MB DOC)
Pattern of annual vaccines delivered to region before (1996–2002) and after (2003–2008) IDSR implementation.
(0.04 MB DOC)
Annual costs (in 2002 US $) of all public health-related surveillance and IDSR-related activities per category of resources and health structure level in Burkina Faso: 2002 to 2005.
(0.07 MB DOC)
Cost of treating a meningitis-related illness at regional hospital and district health facility levels in Burkina Faso during the 2002 epidemic season.
(0.03 MB DOC)
Results of statistical analyses of doses of vaccine imported into Burkina Faso from 1996 to 2008: Impact of IDSR on amounts of vaccine imported.
(0.03 MB DOC)
Pathogens identified by PCR, Latex, and Culture of CSF and serum samples in countries under enhanced surveillance (IDSR) of meningitis in the WHO African region.
(0.17 MB DOC)
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC, the World Health Organization Africa region (WHO-AFRO), and the Ministry of Health of Burkina Faso.
We thank our colleagues on the integrated disease surveillance and response teams at the WHO Regional Office for Africa, the WHO headquarters, and the Centers for Disease Control and Prevention for their comments during the development and implementation of the study. We wish to acknowledge, specifically, William Perea and Alejandro Javier Costa (WHO-HQ) and Montse Soriano-Gabarro (GlaxoSmithKline Biologicals) for providing important vaccine data for this study. We also thank Dr. Jay Wenger, DPEI/NCEZID/CDC, for detailed comments on earlier versions of this manuscript.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This research was supported by the U.S. Centers for Disease Control and Prevention (CDC) with funding from USAID Global Surveillance and Africa Bureaus. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Fauci AS. Infectious diseases: considerations for the 21st century. Clin Infect Dis. 2001;32:657–685. doi: 10.1086/319235. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 3.Worrall E, Rietveld A, De la Collette C. The burden of malaria epidemics and cost-effectiveness of interventions in epidemic situation in Africa. Am J Trop Med Hyg. 2004;71(suppl. 2):136–140. [PubMed] [Google Scholar]
- 4.Campagne G, Schuchat A, Djibo S, Ousséini A, Cissé L, et al. Epidemiology of bacterial meningitis in Niamey, Niger, 1981-1996. Bull World Health Organ. 1999;77:499–508. [PMC free article] [PubMed] [Google Scholar]
- 5.Mohammed I, Nasidi A, Alkali AS, Garbati MA, Ajayi-Obe EK, et al. A severe epidemic of meningococcal meningitis in Nigeria, 1996. Trans Royal Soc Trop Med Hyg. 2000;94:265–270. doi: 10.1016/s0035-9203(00)90316-x. [DOI] [PubMed] [Google Scholar]
- 6.Lapeyssonnie L. La meningite cerebro-spinale en Afrique. Bull World Health Organ. 1963;28(suppl):3–114. [PMC free article] [PubMed] [Google Scholar]
- 7.Kaninda AV, Belanger F, Lewis R, Batchassi E, Aplogan A, et al. Effectiveness of incidence thresholds for detection and control of meningococcal meningitis epidemics in northern Togo. Int J Epidemiol. 2000;29:933–940. doi: 10.1093/ije/29.5.933. [DOI] [PubMed] [Google Scholar]
- 8.Lewis R, Nathan N, Diarra L, Belanger F, Paquet C. Timely detection of meningococcal meningitis epidemics in Africa. The Lancet. 2001;358:287–293. doi: 10.1016/S0140-6736(01)05484-8. [DOI] [PubMed] [Google Scholar]
- 9.Robbins J, Towe DW, Gotschlich EC, Schneerson R. “Love's labours lost”: failure to implement mass vaccination against Group A meningococcal meningitis in sub-Saharan Africa. The Lancet. 1997;350:880–882. doi: 10.1016/S0140-6736(97)03227-3. [DOI] [PubMed] [Google Scholar]
- 10.Morel CM, Lauer JA, Evans DB. Achieving the millennium development goals for health: Cost effectiveness analysis of strategies to combat malaria in developing countries. BMJ. 2005 doi: 10.1136/bmj.38639.702384.AE. doi: 10.1136/bmj.38639.702384.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415:680–685. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 12.Chima RI, Goodman CA Mills A. The economic impact of malaria in Africa: a critical review of the evidence. Health Policy. 2003;63:17–36. doi: 10.1016/s0168-8510(02)00036-2. [DOI] [PubMed] [Google Scholar]
- 13.Russel S. The economic burden of illness for households in developing countries: A review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. Am J Trop Med Hyg. 2004;71(Suppl 2):147–155. [PubMed] [Google Scholar]
- 14.World Health Organization, Regional Office for Africa. Integrated Disease Surveillance and Response: A Regional Strategy for Communicable Diseases 1999 – 2003. 1999 Available: http://www.afro.who.int/en/clusters-a-programmes/dpc/integrated-disease-surveillance/cds-publications.html. Accessed 2010 Sept 05. [Google Scholar]
- 15.World Health Organization, Regional Office for Africa, Centers for disease Control and Prevention. Technical Guidelines for Integrated Disease Surveillance and Response in the African Region. 2002 Available: http://www.cdc.gov/idsr/resources.html. Accessed 2010 Sept 05. [Google Scholar]
- 16.Perry NH, McDonnell MS, Alemu W, Nsubuga P, Chungong S, et al. Planning an integrated disease surveillance and response system: a matrix of skills and activities. BMC Medicine. 2007;5:24. doi: 10.1186/1741-7015-5-24. doi: 10.1186/1741-7015-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker D, Fox-Rushby JA. Economic evaluation of communicable disease interventions in developing countries: A critical review of the published literature. Health Economics. 2000;9:681–698. doi: 10.1002/1099-1050(200012)9:8<681::aid-hec545>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 18.Hutibessy RCW, Bendib LM, Evans DB. Critical issues in the economic evaluation of interventions against communicable diseases. Acta Tropica. 2001;78:191–206. doi: 10.1016/s0001-706x(00)00176-5. [DOI] [PubMed] [Google Scholar]
- 19.Uzicanin A, Zhou F, Eggers R, Webb E, Strebel P. Economic Analysis of the 1996-1997 mass measles immunization campaigns in South African. Vaccine. 2004;22:3419–3426. doi: 10.1016/j.vaccine.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 20.Wilkins JJ, Folb PI, Valentine N, Barnes KI. An economic comparison of chloroquine and sulfadoxine-pyrimethamine as first-line treatment for malaria in South Africa: development of a model for estimating the recurrent direct costs. Trans R Soc Trop Med Hyg. 2002;96:85–90. doi: 10.1016/s0035-9203(02)90251-8. [DOI] [PubMed] [Google Scholar]
- 21.Parent du Chatelet I, Gessner BD, da Silva A. Comparison of cost-effectiveness of preventive and reactive mass immunization campaigns against meningococcal meningitis in West Africa: a theoretical modeling analysis. Vaccine. 2001;19:3420–3431. doi: 10.1016/s0264-410x(01)00066-4. [DOI] [PubMed] [Google Scholar]
- 22.Khan MM, Khan SH, Walker D, Fox-Rushby J, Cutts F, et al. Cost of delivering child immunization services in urban Bangladesh: a study based on facility-level surveys. J Health Popul Nutr. 2004;22:404–412. [PubMed] [Google Scholar]
- 23.Miller MA, Shahab CA. Review of the cost effectiveness of immunization strategies for the control of epidemic of meningococcal meningitis. Pharmacoecon. 2006;23:333–343. doi: 10.2165/00019053-200523040-00004. [DOI] [PubMed] [Google Scholar]
- 24.John TJ, Samuel, Balraj V, John R. Disease surveillance at district level: a model for developing countries. The Lancet. 1998;352:58–61. doi: 10.1016/s0140-6736(97)10494-9. [DOI] [PubMed] [Google Scholar]
- 25.Elbasha EH, Fitzsimmons TD, Meltzer MI. Costs and benefits of a subtype-specific surveillance system for identifying Escherichia coli o157:H7 outbreaks. Emerg Infect Dis. 2000;6:293–297. doi: 10.3201/eid0603.000310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Somda ZC, Meltzer MI, Perry HN, Messonnier NE, Abdulmumini U. Cost analysis of an integrated disease surveillance and response system: case of Burkina Faso, Eritrea and Mali. Cost Eff Resour Alloc. 2009;7:1. doi: 10.1186/1478-7547-7-1. doi: 10.1186/1478-7547-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.International Monetary Fund. World Economic and Financial Surveys, World Economic Outlook Database. Available: http://www.imf.org/external/pubs/ft/weo/2006/02/data/index.aspx. Accessed 2006 November 7. [Google Scholar]
- 28.Smith AW, Bradley AK, Wall RA, McPherson B, Secka A, et al. Sequelae of epidemic meningococcal meningitis in Africa. Trans R Soc Trop Med Hyg. 1988;82:312:320. doi: 10.1016/0035-9203(88)90459-2. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. Detecting meningococcal meningitis epidemics in highly-endemic African countries: WHO recommendation. Weekly Epidemiol Rep. 2000;75:306–309. [PubMed] [Google Scholar]
- 30.Bovier PA, Wyss K, Au HJ. A cost-effectiveness analysis of vaccination strategies against N. meningitidis meningitis in sub-Saharan African countries. Soc Sci Med. 1999;48:1205–1220. doi: 10.1016/s0277-9536(98)00419-5. [DOI] [PubMed] [Google Scholar]
- 31.Monath TP, Nasidi A. Should yellow fever vaccine be included in the expanded program of immunization in Africa? A cost-effectiveness analysis for Nigeria. Am J Trop Med Hyg 1993. 48:247–299. doi: 10.4269/ajtmh.1993.48.274. [DOI] [PubMed] [Google Scholar]
- 32.Robertson RL, Foster SO, Hull HF, Williams PJ. Cost-effectiveness of immunization in The Gambia. J Trop Med Hyg. 1985;88:343–351. [PubMed] [Google Scholar]
- 33.Taha M-K, Parent du Chatelet I, Schlumberger M, Sanou I, Djibo S, et al. Neisseria meningitidis Serogroups W135 and A were equally prevalent among meningitis cases occurring at the end of the 2001 epidemics in Burkina Faso and Niger. J Clin Microbiol. 2002;40:1083–1084. doi: 10.1128/JCM.40.3.1083-1084.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nicolas P, Norheim G, Garnotel E, Djibo S, Caugant DA. Molecular epidemiology of Neisseria meningitidis isolated in the African meningitis belt between 1988 and 2003 shows dominance of sequence type 5 (ST-5) and ST-11 complexes. J Clin Microbiol. 2005;43:5129–5135. doi: 10.1128/JCM.43.10.5129-5135.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nicolas P, Décousset L, Riglet V, Castelli P, Stor R, et al. Clonal expansion of sequence type (ST-)5 and emergence of ST-7 in Serogroup A meningococci, Africa. Emerg Infect Dis. 2001;7:849–854. doi: 10.3201/eid0705.010513. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of IDSR priority diseases and diseases of public health importance weekly or monthly reported in Burkina Faso during the study period.
(0.02 MB DOC)
Health outcomes and duration of meningococcal meningitis outbreak in selected districts before (1996-2002) and after (2003–2007) IDSR implementation in Burkina Faso.
(0.28 MB DOC)
Pattern of annual vaccines imported into Burkina Faso before (1996–2002) and after (2003–2008) IDSR implementation.
(0.04 MB DOC)
Pattern of annual vaccines delivered to region before (1996–2002) and after (2003–2008) IDSR implementation.
(0.04 MB DOC)
Annual costs (in 2002 US $) of all public health-related surveillance and IDSR-related activities per category of resources and health structure level in Burkina Faso: 2002 to 2005.
(0.07 MB DOC)
Cost of treating a meningitis-related illness at regional hospital and district health facility levels in Burkina Faso during the 2002 epidemic season.
(0.03 MB DOC)
Results of statistical analyses of doses of vaccine imported into Burkina Faso from 1996 to 2008: Impact of IDSR on amounts of vaccine imported.
(0.03 MB DOC)
Pathogens identified by PCR, Latex, and Culture of CSF and serum samples in countries under enhanced surveillance (IDSR) of meningitis in the WHO African region.
(0.17 MB DOC)