Abstract
Objective
To conduct the first rigorous evaluation of the long-term effect of the Comprehensive Rural Health Project on childhood mortality in rural Maharashtra.
Methods
Background information and full birth histories were collected by conducting household surveys and interviewing women. Control villages resembling project villages in terms of population size were randomly selected from an area enclosed by two ellipses centred around, but not including, the project area. An equal number of villages and approximately equal numbers of households and women were randomly sampled from both areas. Cox models with robust standard errors were used to compare the hazard of death among children under 5 years of age in project and control villages.
Findings
The hazard of death was reduced by 30% (95% confidence interval, CI: 6% to 48%) after the neonatal period in the project villages compared with control villages after adjustment for caste and religion of subjects and for availability of irrigation in the villages. During the neonatal period there was an increase of 3% in the hazard of death, but it was not statistically significant (95% CI: −18% to 29%).
Conclusion
Our methods provide useful tools for evaluating long-running community-based primary health care programmes. Our findings add to the growing debate on the long-term sustainability of community-based interventions designed to reduce child mortality.
ملخص
الغرض
إجراء أول تقييم دقيق للتأثير الطويل الأمد لمشروع صحي ريفي شامل على وفيات الأطفال في المناطق الريفية في مهراشتا.
الطريقة
جُمِعَت المعلومات الأساسية وتواريخ الولادة بالكامل من خلال إجراء مسوحات منزلية ومقابلات مع النساء. واختيرت عشوائياً قرى مماثلة في حجم السكان لتكون شواهد للقرى التي يجري فيها المشروع، واختيرت هذه القرى من منطقة جغرافية محاطة بهلالين يقع في مركزها منطقة المشروع، ولكن بدون إدراج منطقة المشروع فيها. واختير عشوائياً عدد مماثل من القرى وعدد شبه مماثل من المنازل والنساء في كلا المنطقتين. واستخدم في إجراء المقارنات بين المخاطر الصحية التي يتعرض لها الأطفال دون الخامسة من العمر في القرى التابعة للمشروع والقرى الشواهد نماذج كوكس Cox models مع معايير الخطأ.
الموجودات
انخفض خطر الوفاة بنسبة 30% (فاصلة الثقة 95%، حد الثقة: 6% إلى 48%) بعد الفترة التالية للولادة في القرى التي تطبق المشروع مقارنة بالقرى الشواهد بعد تصحيح الوضع الاجتماعي والديانة للأفراد، وتوفر مياه الري للقرى. وفي الفترة التالية للولادة كان هناك زيادة مقدارها 3% في المخاطر الصحية، ولكن هذه الزيادة لم يعتد بها إحصائياً (فاصلة الثفة 95%: -حد الثقة 18% إلى 29%).
الاستنتاج
تقدم الطرق التي اتبعها الباحثون أدوات مفيدة لتقييم برامج الرعاية الصحية الأولية المجتمعية الطويلة الأمد. وتضيف نتائج الدراسة المزيد إلى الجدل حول استدامة التدخلات المجتمعية المصممة للحد من وفيات الأطفال.
Résumé
Objectif
Mener la première évaluation rigoureuse de l'effet à long terme du Projet de Santé Rural Complet sur la mortalité infantile dans la région rurale de Maharashtra.
Méthodes
Les renseignements de base et l’historique complet des accouchements ont été recueillis en conduisant des sondages auprès des ménages et en interrogeant les femmes. Des villages témoins semblables aux villages du projet en termes de population ont été sélectionnés au hasard dans une région fermée par deux ellipses centrées autour de la région du projet, mais sans la contenir. Un nombre égal de villages et des nombres quasiment égaux de ménages et de femmes ont été échantillonnés au hasard dans les deux régions. Les modèles de Cox à erreurs types solides ont été utilisés pour comparer le risque de mortalité chez les enfants de moins de 5 ans dans les villages du projet et dans les villages témoins.
Résultats
Le risque de décès a diminué de 30% (intervalle de confiance de 95%, IC: 6% à 48%) après la période néo-natale dans les villages du projet comparés aux villages témoins après ajustement en matière de caste et de religion des sujets, mais aussi en matière de disponibilité de l'irrigation dans les villages. Une augmentation de 3% du risque de décès a été enregistrée au cours de la période néo-natale, ce qui n’est pas significatif du point de vue statistique (IC 95%: 18% à 29%).
Conclusions
Nos méthodes fournissent des outils qui permettent d’évaluer les programmes de soins médicaux communautaires primaires qui existent depuis longtemps. Nos conclusions s’ajoutent au débat croissant sur la durabilité à long terme des interventions communautaires conçues pour réduire la mortalité infantile.
Resumen
Objetivo
Llevar a cabo la primera evaluación rigurosa del efecto a largo plazo del Proyecto Global de Salud Rural sobre mortalidad infantil en las zonas rurales de Maharashtra (India).
Métodos
Se recopiló información general y se elaboró un registró completo de nacimientos mediante la realización de encuestas por hogares y entrevistas a mujeres. Se seleccionaron aleatoriamente aldeas control que se parecían a las aldeas del proyecto en lo que a tamaño de población se refiere y que estaban situadas en un área enmarcada por dos elipses con su centro en torno al área del proyecto, aunque sin incluirla. Se realizó un muestreo aleatorio del mismo número de aldeas y aproximadamente el mismo número de hogares de las dos áreas. Se utilizaron modelos de Cox con errores estándar robustos para comparar el riesgo instantáneo de muerte entre los niños menores de 5 años en las aldeas del proyecto y control.
Resultados
El riesgo instantáneo de muerte se redujo en un 30% (intervalo de confianza [IC], 95%: 6% al 48%) después del periodo neonatal en las aldeas del proyecto en comparación con los pueblos control después del ajuste por casta y religión de los sujetos y por disponibilidad de irrigación en las aldeas. Durante el periodo neonatal, se observó un aumento del 3% en el riesgo instantáneo de muerte, pero no era estadísticamente significativo (IC 95%: -18% al 29%).
Conclusión
Nuestros métodos proporcionan herramientas útiles para evaluar los programas de atención sanitaria primaria dentro de la comunidad que llevan mucho tiempo en funcionamiento. Nuestros resultados se suman al creciente debate sobre la sostenibilidad a largo plazo de las intervenciones en la comunidad diseñadas para reducir la mortalidad infantil.
Introduction
The Bellagio Child Survival Study Group brought the issue of child survival to the forefront of the global health care agenda in 2003 when it reported that 10 million children were dying every year.1 Reducing child mortality by two-thirds before 2015 is one of the United Nations Millennium Development Goals.2 As the Bellagio series and the Lancet neonatal survival series3 and Alma-Ata series4 all point out, most of these deaths are preventable. In India, as in many developing countries, providing even basic health care in rural areas is a major challenge for the government. Analyses of India’s health system have suggested that rural health care has been neglected by the government and that increasing privatization may further reduce health care in remote areas.5,6
Community-based primary health care provided by trained community residents has been shown to improve child survival in areas with high child mortality. The Warmi project in Bolivia and the Society for Education, Action and Research in Community Health (SEARCH) in Maharashtra, India, have demonstrated significant reductions in perinatal and neonatal mortality.7,8 Recent trials in Nepal and in Uttar Pradesh, India, have reported reductions in neonatal mortality of 30% and 52%, respectively.9,10
Many aid agencies strive to address the lack of health care and improve child survival in developing countries, but they rarely conduct rigorous independent evaluations of their work. Such evaluations are expensive, carry the risk of showing negative results and are under-appreciated by donors. Consequently, there are few credible data on the impact of ongoing aid work.11–15 Though randomized controlled interventions can generate such data,15 a study with prospectively assigned controls is seldom an option and retrospective approaches must therefore be used to assess the impact of aid efforts.
The Comprehensive Rural Health Project
The Comprehensive Rural Health Project (CRHP), one of the inspirations for the 1978 International Conference on Primary Health Care at Alma-Ata, has been working for the past 40 years to address the issues highlighted in the aforementioned Lancet series.1,3,4 It has had a major influence in health policy circles, including the World Health Organization (WHO) and schools of public health,16 and is a rare example of a long-term community-based primary health care project. The project was highlighted in the Alma-Ata Rebirth and Revival series as a model for delivering primary health care to poor rural regions,4 and – if found to be effective upon rigorous evaluation – could prove important for achieving the Millennium Development Goals on child mortality reduction elsewhere in India and in other vulnerable areas.
CRHP was founded in 1970 by physicians Mabelle and Rajnikant Arole, who envisioned a system that delivered both curative and preventative care to India’s most vulnerable people. Based in the town of Jamkhed, CRHP also serves surrounding areas in the central part of Maharashtra state. The area is predominantly rural, poor and drought-prone. Public health care and education are notoriously poor. CRHP has gradually expanded from a single hospital in Jamkhed and currently covers approximately 300 communities with a total population of over 500 000 people.17
Activities in project villages
The CRHP model, which focuses on community-centred primary health care, is described in detail elsewhere.17,18 Activities in the project villages are carried out at three levels: village health workers, mobile health teams and the secondary-care hospital in Jamkhed.
Village health workers, who are the cornerstone of the model, are local women selected by their communities, often from the lowest caste. They receive intensive training from CRHP trainers in primary health care and health promotion, including family planning, women’s and children’s health and home birth delivery. Training is also provided in community development, organization, communication skills and personal development. The primary role of these workers is to disseminate health knowledge in their respective communities through discussion groups and household visits, administer basic remedies and medications, perform safe deliveries and detect and refer high-risk pregnancies and deliveries to more qualified health care providers. During participatory discussions with community members, village health workers address issues such as care-seeking, family planning, adequate birth spacing, nutrition, hygiene, sanitation and safe drinking water.
Mobile health teams, comprising a nurse, a physician, a social worker and paramedics, visit project villages monthly to support and mentor village health workers and to refer complicated cases to the hospital. The secondary-care hospital in Jamkhed is a 40-bed low-cost facility operated by CRHP that provides quality emergency, medical, surgical and outpatient care to residents from the surrounding catchment area.
Research aims
Although many publications have praised CRHP’s work,4,18–23 to date no rigorous impact study has been conducted. Overall child survival has improved in Maharashtra over the past few decades,24–26 yet infant and child mortality rates in remote areas of Maharashtra remain much higher than for rural India overall.27,28 Rigorously evaluating the effect of CRHP will provide insight into the impact of community health interventions in such areas. Our primary aim was to compare mortality among children under 5 in CRHP villages of a typical size and in nearby control villages of similar size. Secondary aims were to compare sanitation; health knowledge; number of children per woman; place and type of delivery and type of birth attendant; indicators of antenatal, delivery and postnatal care; and child morbidity.
Methods
Study design
For statistical efficiency, we sampled equal numbers of villages in CRHP and control sites and approximately equal numbers of households, women and children within each village.
Surveys
Two surveys were conducted after a specially-hired team identified and numbered every household in all study villages. A household survey collected information on household-level indicators such as wealth, sanitation and water supply. Women in the surveyed households were interviewed and a full birth history was obtained, along with information on the woman’s background, history of pregnancy-related care, health care expenditure and morbidity of children under 5 years of age. Information on health knowledge was also collected for each eligible woman present in the household. These surveys were modelled on questionnaires from the third National Family Health Survey (NFHS-3)29 and were conducted by women hired locally from a women’s college near Jamkhed. They were trained for 10 days by a National Family Health Survey trainer and supervisor and supervised by locally-hired managers and a project manager. Training manuals, created by the authors, were based on the manuals for NFHS-3.30 Data collection took place between September 2007 and January 2008.
Sampling CRHP villages
The CRHP worked in four small administrative regions known as blocks or talukas: three in the core area near the hospital (Jamkhed, Ashti and Karjat) and one (Akole) approximately 220 km from the core area. We focused only on villages in the core area because Akole is distant and consists largely of tribal villages with characteristics different from those found in the core-area villages. We restricted eligibility to villages with a population of between 400 and 3000 in which a CRHP village health worker had been working for at least 5 years.
In the core area, CRHP implemented its comprehensive health intervention in 153 villages. Of these, 69 were excluded because village health workers had not worked for at least five years in the village. A further nine were excluded because their populations were outside the specified range. A total of 75 villages, all of them non-tribal, in the core area satisfied all criteria and were included in the study.
Sampling control villages
To select control villages with characteristics similar to those of CRHP villages while minimizing the risk of contamination bias owing to proximity to the CRHP intervention area, a buffer zone was drawn around the three core blocks of the project. Since the core intervention region is approximately elliptical in shape, we drew an elliptical buffer line that was never less than 5 km from any intervention village. A second ellipse, with the same foci, was drawn 25 km outside the first (Fig. 1). Control villages were selected from the area between the two ellipses. The 25 km width ensured that the number of eligible control villages in the area between the two ellipses was greater than the total number of eligible intervention villages. From the 135 non-tribal villages in this area with a population between 400 and 3000 according to the 2001 national census, 75 were selected at random for the study. CRHP was the only nongovernmental organization delivering home-based care, health education and clinical services in the study villages. Government health services were available in both intervention and control villages.
Fig. 1.
Map of control and intervention areas in retrospective study of the impact of the Comprehensive Rural Health Project (CRHP), Maharashtra state, India
a This area comprises the 153 CRHP villages, of which 75 satisfied all inclusion criteria.
b This area comprises the 135 eligible control villages, of which 75 were randomly selected to be surveyed. The inner ellipse is at a distance of at least 5 km from any CRHP village.
Sampling households and women
In each village, 30 households were randomly selected from the mapping list of all households. An additional 60 households were randomly selected as back-ups. Our survey teams attempted to interview all potentially eligible women in the 30 selected households in each village. They returned twice to the village to reach as many selected households as possible. If it was impossible to identify and interview at least one eligible woman after two visits to a selected household, the team approached the next household on the back-up list, continuing until at least 30 households were interviewed. As six interviewers were simultaneously conducting interviews, in some villages the team interviewed more than 30 households.
Eligible women and births
Women were eligible if they were between 15 and 59 years of age, were currently or previously married, had lived in the village for at least one year before the survey and had at least one child born alive in the village in the past 15 years. Some women who lived in intervention or control villages at the time of the survey had given birth and raised children in other villages. To minimize recall bias, we included only women who had given birth to a liveborn child between 1 September 1992 and 31 December 2007 in the same village in which they were interviewed. To allow sufficient time for CRHP to have had an impact, analyses in intervention villages were further restricted to women who had given birth five years after the project began operating in their villages.
Sample size
The sample size was calculated to attain 80% statistical power to detect a 25% reduction in under-5 mortality at the 5% significance level using a conventional 2-sided test. On the basis of data from the 1998–1999 National Family Health Survey for rural India,25 we assumed a 10% under-5 mortality rate in the control villages and hence 7.5% under-5 mortality in the CRHP villages, with an intra-cluster correlation coefficient of 0.0175, estimated from the National Family Health Survey data for the period 1985–1995 for the 81 non-tribal rural villages in Maharashtra state included in this data set.25
Under these assumptions, 54 eligible births were needed from each of the 75 sampled villages in both the CRHP and the control area during the 15 years before the interviews. At an assumed average of two eligible births per household, at least 27 households per village were required.
Data analysis
All data obtained for all eligible villages, women and children were analysed. Demographic and other characteristics at the village, household and mother level were summarized by type of village (CRHP or control). These included characteristics considered as confounders and/or secondary outcomes, such as the educational level of the woman, treatment of drinking water, toilet facilities, number of women reporting miscarriage and/or stillbirth, number of Caesarean deliveries, number of children per woman, number of antenatal and postnatal care visits, mean health knowledge score and its standard deviation, and health care-seeking activities.
The overall health knowledge score was derived by summing the total number of correct responses given to 10 health knowledge questions. Questions with more than one possible correct answer were weighted by the inverse of the total number of correct answers so that no single question contributed more than one point out of 10 to the score.
The percentages of villages with irrigation in the CRHP and control groups were compared using Fisher’s exact test. Mean ages and health knowledge scores were compared using linear regression models with robust standard errors (Huber-White sandwich estimator) to allow for clustering within villages. Categorical characteristics and secondary outcomes at household, woman and child level were compared using logistic regression models. Robust standard errors were used, and Wald tests for joint significance were performed. Village-specific crude neonatal, infant and under-5 mortality rates were estimated by the Kaplan–Meier method and are presented separately for control and CRHP villages. Crude mortality rates for the entire set of surveyed villages are given in 5-yearly intervals.
Cox regression models were used to compare hazard rates between CRHP and control villages using robust standard errors (Lin-Wei estimator) to account for clustering of women in villages and for the non-independent outcomes for children born to the same woman. As CRHP attempted to work in the most disadvantaged villages, most of which lacked irrigation and had relatively large proportions of low-caste inhabitants, we decided a priori to adjust for irrigation status of the villages and for women’s caste and religion. Interaction terms between the intervention and different age bands (neonatal, post-neonatal to 5 years of age) were included in the models to test the proportionality assumption – i.e. whether the intervention had a differential effect on mortality at different ages. When a statistically significant interaction was found, age-specific effects of the intervention are also reported.
Ethical approval
Ethical approval was obtained from the Institutional Ethics Committee of the Maharashtra Association of Anthropological Sciences in India and from the Ethics Committee of the London School of Hygiene and Tropical Medicine.
Results
Data on the study population are presented in Table 1. More women in CRHP villages belonged to less-advantaged castes, their families were less likely to own land and they were less likely to have irrigation available (Table 2). Factors that may have been influenced by the CRHP intervention are summarized in Table 3. In 2007, more households in CRHP villages had toilet facilities and treated drinking water. Women in the intervention villages achieved, on average, a health knowledge score that was 0.15 standard deviations higher (0.26 points higher in absolute score) than the score obtained by women in the control villages. The number of children per woman and the percentage of women who reported having a stillbirth or miscarriage were similar in the two groups. Indicators of antenatal and postnatal care and of location and type of delivery of the last child were also similar. Among women reporting that in the three months before the survey their child under 5 years of age had experienced symptoms of one of the main diseases that cause child death, there was no significant difference in the use of medical centres when seeking treatment.
Table 1. Study population data from a retrospective evaluation of the impact of the Comprehensive Rural Health Project (CRHP), Maharashtra state, India, September 1992–December 2007.
| Study population | Control villages (n = 75) |
CRHP villages (n = 75) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | No. per village |
Total | No. per village |
||||||
| Mean | SD | Range (min, max) | Mean | SD | Range (min, max) | ||||
| Total households | 12 466 | 166.2 | 68.3 | 67–366 | 13 647 | 182.0 | 70.7 | 34–443 | |
| Households visited | 5041 | 67.2 | 13.9 | 42–90 | 5441 | 72.5 | 13.8 | 41–90 | |
| Households with no one at home | 2369 | 31.6 | 14.6 | 10–58 | 2792 | 37.2 | 14.0 | 8–62 | |
| Households surveyed | 2672 | 35.6 | 3.4 | 28–46 | 2649 | 35.3 | 3.6 | 26–47 | |
| Households with at least one woman intervieweda | 2623 | 35.0 | 3.1 | 29–44 | 2590 | 34.5 | 3.4 | 24–46 | |
| Households with at least one eligible childb | 2294 | 30.6 | 1.3 | 26–34 | 2253 | 30.0 | 2.6 | 20–37 | |
| Interviewed womena | 3003 | 40.0 | 4.6 | 33–51 | 3002 | 40.0 | 5.3 | 27–54 | |
| Interviewed women with at least one eligible childb | 2508 | 33.4 | 2.6 | 26–41 | 2432 | 32.4 | 3.2 | 23–40 | |
| Eligible children per villageb | 5516 | 73.5 | 9.4 | 53–100 | 5380 | 71.7 | 9.1 | 50–93 | |
SD, standard deviation.
a Women were interviewed if they were currently or previously married, aged 15 to 59 and had at least one child born alive during the 15-year period preceding the survey.
b Children were eligible if they were born between 1 September 1992 and 31 December 2007 to a currently or previously married woman who was aged 15–59 at the time of the survey and had given birth in the village being surveyed. In CRHP villages the child had to have been born at least five years after project operations began in the village.
Table 2. Characteristics of control and intervention villages, households and mothers in a retrospective evaluation of the impact of the Comprehensive Rural Health Project (CRHP), Maharashtra state, India, 2007.
| Characteristic | Control villages |
CRHP villages |
P | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Villagesa | ||||||
| CRHP activities | ||||||
| < 10 yrs | – | – | 28 | 37.3 | – | |
| 10 to < 20 yrs | – | – | 21 | 8.0 | – | |
| 20+ yrs | – | – | 26 | 34.7 | – | |
| Irrigation | ||||||
| Yes | 19 | 25.3 | 9 | 12.0 | 0.06 | |
| No | 56 | 74.7 | 66 | 88.0 | ||
| Householdsb | ||||||
| Land owner | 2024 | 88.2 | 1794 | 79.6 | < 0.001 | |
| No information given | 3 | 0.1 | 4 | 0.2 | ||
| Mothersc | ||||||
| Aged | 29.5d | 7.0d | 29.3d | 7.0d | 0.24 | |
| Religion | 0.15 | |||||
| Hindu | 2363 | 94.2 | 2249 | 92.5 | ||
| Muslim | 79 | 3.2 | 124 | 5.1 | ||
| Other | 66 | 2.6 | 59 | 2.4 | ||
| Caste | 0.0005 | |||||
| Most backwarde caste/tribe | 293 | 11.7 | 415 | 17.1 | ||
| Other backward caste | 163 | 6.5 | 290 | 11.9 | ||
| Nomad | 457 | 18.2 | 424 | 17.5 | ||
| Non-backward | 1595 | 63.6 | 1298 | 53.5 | ||
| No information given | 0 | 0.0 | 5 | 0.2 | ||
a There were 75 control and 75 CRHP villages.
b There were 2294 households in control villages and 2253 households in CRHP villages.
c There were 2508 mothers in control villages and 2432 mothers in CRHP villages.
d Age is given as mean age in years and standard deviation. Age was missing for one woman in the control villages.
e Most backward: scheduled caste. Scheduled castes and tribes, formerly known as “depressed classes”, are groups explicitly recognized and afforded certain protections under the Constitution of India.
Table 3. Secondary outcomes for intervention and control villages at the household, mother and child level in retrospective evaluation of the impact of the Comprehensive Rural Health Project (CRHP), Maharashtra state, India.
| Level | Control villages |
CRHP villages |
P | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Householda | ||||||
| Has treated drinking water | 1202 | 52.3 | 1443 | 64.1 | < 0.001 | |
| No information | 0 | 0.0 | 2 | 0.09 | ||
| Has toilet facility | 180 | 7.8 | 314 | 13.9 | < 0.004 | |
| Motherb | ||||||
| Health knowledgec | 4.54c | 1.63c | 4.80c | 1.60c | 0.001 | |
| Children per woman | 0.6 | |||||
| 1 | 303 | 12.1 | 325 | 13.4 | ||
| 2 | 790 | 31.5 | 769 | 31.6 | ||
| 3 | 730 | 29.1 | 677 | 27.8 | ||
| 4+ | 685 | 27.3 | 661 | 27.2 | ||
| Mother ever had miscarriage/stillbirth | 0.6 | |||||
| Yes | 342 | 13.6 | 315 | 13.0 | ||
| No | 2153 | 85.9 | 2097 | 86.2 | ||
| No answer | 13 | 0.5 | 20 | 0.8 | ||
| Birth attendant at last birth | 0.15 | |||||
| Health professional | 986 | 39.3 | 1029 | 42.3 | ||
| Not a health professional | 1501 | 59.9 | 1388 | 57.1 | ||
| No one | 16 | 0.6 | 11 | 0.5 | ||
| No answer | 5 | 0.2 | 4 | 0.2 | ||
| Place of last birth | 0.4 | |||||
| Medical centre | 906 | 36.1 | 939 | 38.6 | ||
| Home | 1595 | 63.6 | 1488 | 61.2 | ||
| Other | 2 | 0.08 | 3 | 0.1 | ||
| No answer | 5 | 0.2 | 2 | 0.1 | ||
| Type of delivery at last birth | 0.5 | |||||
| Vaginal cephalic | 2396 | 95.5 | 2316 | 95.2 | ||
| Vaginal breech | 15 | 0.6 | 10 | 0.4 | ||
| Caesarean | 90 | 3.6 | 99 | 4.1 | ||
| No answer | 7 | 0.3 | 7 | 0.3 | ||
| Received antenatal care before last birth | 0.08 | |||||
| No | 317 | 12.6 | 244 | 10.0 | ||
| Yesd | 2186 | 87.2 | 2185 | 89.8 | ||
| No answer | 5 | 0.2 | 3 | 0.1 | ||
| Received postnatal care after last birth | 0.3 | |||||
| No | 1500 | 59.8 | 1392 | 57.2 | ||
| Yese | 1003 | 39.9 | 1031 | 42.4 | ||
| No answer | 5 | 0.2 | 9 | 0.4 | ||
| Childf | ||||||
| Medical treatment in the last 3 mo | 0.6 | |||||
| Yes | 656 | 46.7 | 667 | 45.6 | ||
| No | 696 | 49.5 | 745 | 50.9 | ||
| No answer | 54 | 3.8 | 51 | 3.5 | ||
| Place of treatment | 0.5 | |||||
| Medical centre | 646 | 98.5 | 652 | 97.8 | ||
| Home | 5 | 0.8 | 7 | 1.0 | ||
| Elsewhere | 3 | 0.5 | 8 | 1.2 | ||
| No answer | 2 | 0.3 | 0 | 0.0 | ||
a There were 2294 households in control villages and 2253 in CRHP villages.
b There were 2508 mothers in control villages and 2432 in CRHP villages.
c Health knowledge is given as mean scores and standard deviations. The scores were missing for five women in the control villages and two women in the intervention villages.
d Among women with at least one antenatal care visit, the median number of visits was 3 in both the control and the CRHP villages.
e Among women with at least one postnatal care visit, the median number of visits was 2 in both the control and the CRHP villages.
f Represents children under 5 years of age at the survey. There were 1406 children in control villages and 1463 in CRHP villages.
In control villages, 42.3% of women had no education at all compared to 39.3% of women in the CRHP villages. The mean (median) number of years of education in CRHP villages was 4.4 (4) for women. In control villages the figure was 4.3 (4).
Out of 10 896 eligible live births to 4940 eligible women during the evaluation period, 619 under-5 child deaths were reported. Of those deaths, 37 in control villages and 48 in intervention villages were reported to have occurred on the day of delivery. For 2 of the children reported dead, age at death was missing. Those children were excluded from the survival analyses. For an additional 11 children, the caste of the mother was not reported. Five-yearly estimates of age-specific mortality rates for the entire study area (CRHP and control villages) over the evaluation period are shown in Table 4.
Table 4. Age-specific child mortality rates,a by 5-yearly periods of birth, for the entire study area covered in retrospective evaluation of the impact of the Comprehensive Rural Health Project, Maharashtra state, India, September 1992–December 2007.
| Age | Period of birth |
|||||||
|---|---|---|---|---|---|---|---|---|
| Sep 1992–Aug 1997 |
Sep 1997–Aug 2002 |
Sep 2002–Dec 2007 |
||||||
| Rateb | 95% CI | Rateb | 95% CI | Rateb | 95% CI | |||
| Neonatal | 38.7 | 33.3–45.0 | 38.4 | 32.5–45.2 | 32.1 | 26.4–39.0 | ||
| Infant | 58.5 | 51.9–66.2 | 52.9 | 46.1–60.8 | 43.0 | 36.3–50.9 | ||
| Under 5 yr | 65.4 | 58.3–73.2 | 58.2 | 51.0–66.4 | 56.4 | 37.2–85.1 | ||
CI, confidence interval.
a Estimated by the Kaplan–Meier method.
b Deaths per 1000 live births.
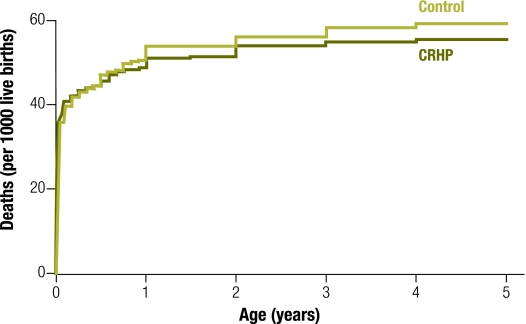
Fig. 2 shows that age-specific mortality rates in the CRHP and control groups run closely together in the neonatal period and then diverge, with consistently lower mortality in the CRHP villages from approximately 1 to 5 years of age. This pattern is also apparent when crude estimates of age-specific childhood mortality rates are compared (Table 5) and is confirmed by formal analysis using Cox regression models (Table 6).
Fig. 2.
Kaplan–Meier estimates of age-specific childhood mortality in control and intervention villages in retrospective evaluation of the impact of the Comprehensive Rural Health Project (CRHP), Maharashtra state, India, September 1992–December 2007a
a There were 5515 eligible live births in the control villages and 5379 eligible live births in the intervention villages.
Table 5. Age-specific child mortality ratesa in intervention and control villages for the 15 years preceding the survey to evaluate the impact of the Comprehensive Rural Health Project (CRHP), Maharashtra state, India, September 1992–December 2007.
| Age | Control villages (n = 5 515) |
CRHP villages (n = 5 379) |
|||
|---|---|---|---|---|---|
| Rateb | 95% CI | Rateb | 95% CI | ||
| Neonatal | 35.7 | 31.1–41.0 | 37.7 | 33.0–43.2 | |
| Infant | 53.8 | 48.1–60.1 | 50.9 | 45.3–57.2 | |
| Under 5 yr | 60.8 | 54.7–67.5 | 55.5 | 49.6–62.0 | |
CI, confidence interval.
a Estimated by the Kaplan–Meier method.
b Deaths per 1000 live births.
Table 6. Estimated effect of the Comprehensive Rural Health Project (CRPH) on under-5 child mortality, Maharashtra state, India, September 1992–December 2007a.
| Modelsb | HR | 95% CI |
|---|---|---|
| Under 5 yrc | ||
| Crude | 0.93 | 0.77–1.11 |
| Controlled for casted +religion + irrigation | 0.90 | 0.75–1.09 |
| Controlled for casted + religion + irrigation + birth period | 0.91 | 0.75–1.09 |
| Neonatale | ||
| Crude | 1.06 | 0.84–1.33 |
| Controlled for casted + religion + irrigation | 1.03 | 0.82–1.29 |
| Controlled for casted + religion + irrigation + birth period | 1.04 | 0.83–1.31 |
| Post-natal but under 5 yre | ||
| Crude | 0.72 | 0.54–0.96 |
| Controlled for casted + religion + irrigation | 0.70 | 0.52–0.94 |
| Controlled for casted + religion + irrigation + birth period | 0.70 | 0.52–0.95 |
CI, confidence interval; HR, hazard ratio.
a There were 10 883 children. Those with any missing data were excluded.
b Age at death was missing for 2 children.
c Under 5 yr estimated from the model including insteraction between age bands and CRHP intervention.
d Caste was missing for 11 children belonging to all age groups.
e Neonatal and post-natal but under 5 yr estimated from the model including interaction between age bands and CRHP intervention.
Overall, the hazard of death in CRHP villages was reduced by 10% for the period from birth to 5 years of age when the data were controlled for irrigation status of villages and the caste and religion of mothers. This effect was not significant at the 5% level, with the 95% confidence interval (CI) extending from a 25% reduction to a 9% increase. However, there was evidence (from the result of a test of the proportionality assumption implicit in the Cox model) that the ratio of the hazard in the CRHP villages to that in the control villages varied according to children’s age. For this reason we applied an interaction model in which the hazard ratio comparing the CRHP villages with the control villages differed in the neonatal and post-neonatal periods. This interaction was statistically significant (P < 0.04 for the model, adjusted for irrigation, caste and religion). The model provided no evidence that neonatal mortality was lower in CRHP villages (hazard ratio = 1.03; 95% CI: 0.82 to 1.29), but showed a statistically significant reduction (P < 0.02) in post-neonatal (up to 5 years) mortality (hazard ratio = 0.70; 95% CI: 0.52 to 0.94). Although childhood mortality rates declined over the birth periods covered by the study (Table 4, heterogeneity test for the effect of time period: P < 0.003 in Table 6), the hazard ratio for CRHP did not materially change when birth period was included as an additional covariate in the models. Further, there was no evidence that the hazard ratio for CRHP villages varied between birth periods (interaction test P > 0.1).
Discussion
In our evaluation of the effect of CRHP on childhood mortality over the period September 1992 to December 2007 we found a 30% reduction in the hazard of child death after the neonatal period for CRHP villages in comparison with villages in the control area; the reduction was significant at the 5% level. We did not, however, find a similar reduction in the hazard of neonatal death.
There are several possible explanations for this inconsistency. Causes of neonatal deaths in rural India – primarily birth asphyxiation, preterm birth and neonatal sepsis – are different from causes of post-neonatal child deaths – primarily pneumonia, diarrhoea and malaria.1,3,31,32 WHO-recommended first-line treatments for malaria, pneumonia and diarrhoea can be administered in the community.3,32 CRHP may have been more effective at ensuring prevention, early recognition and treatment of these diseases than it was at delivering clinical services, as suggested by superior levels of sanitation and water treatment in CRHP villages (Table 3).
There may also have been differential reporting of live and still births. A previous study found substantial underreporting of neonatal deaths in Maharashtra.33 In the CRHP villages, a higher number of deaths occurring on the day of delivery (48 versus 37 among controls) and a lower number of women with stillbirths (315 versus 342 among controls, Table 3) were reported. Women in control villages may have been more likely to classify early postpartum death as a stillbirth than those in intervention villages because the CRHP had sensitized women to the notion of neonatal death and its prevention.
Our childhood mortality estimates for the entire study area are in line with other survey estimates of mortality for the region, although they are somewhat higher than official estimates for Maharashtra from the National Family Health Surveys for 1994–199825 and 2001–2005.26 However, these surveys sample from both urban and rural areas and, since urban regions have lower mortality, they underestimate mortality for rural areas. Estimates based on the 1994–1998 National Family Health Survey data for rural Maharashtra only show much closer agreement with our results: neonatal, infant and under-5 mortality rates of 38.4, 52.3 and 67.6 deaths per 1000 live births, respectively.34
The main strength of this study is that it provides the most carefully collected evidence to date that the hazard of child death was lower in CRHP recipient villages than in nearby non-intervention villages several years after the project was implemented. Our findings suggest that a community-based programme that trains village health workers to improve community knowledge can have long-lasting impacts on child mortality. We designed the study carefully to minimize the risk of bias when controls are selected retrospectively. We believe the methods used here could contribute to future evaluations of similar long-term projects.
Our study had several limitations. Reported mortality may have been impacted by migration. Movement of women from intervention to control villages may have reduced the mortality rate in their new residence and the inverse may also have occurred when women moved from control to intervention villages. We were only able to reduce this dilution partially by restricting our analyses to children whose mothers were resident in the same village at the time of both delivery and survey.
Despite careful selection of the controls, women from CRHP villages may have answered some of the questions in the survey differently from women in control villages because of their improved knowledge. As noted above, this differential reporting could have hindered our ability to show a reduction in neonatal mortality in CRHP villages, if such a reduction did indeed exist.
CRHP may also have been more effective when the disease burden was higher. When the project began in 1970, the child mortality rate in India was 192 deaths per 1000 live births. By 2000 the rate had dropped by more than half,35 partly owing to a reduced incidence of malaria, improved treatment of diarrhoea and pneumonia and increased access to clinical services, including safer birthing practices, as a result of programmes introduced by the Government of India and by Maharashtra state.36 Although these programmes and the clinical and health services provided by the government affected both our intervention and control villages equally, the large improvement in child mortality might have reduced the scope for measuring CRHP-generated improvements in recent years.
Funding cuts have forced CRHP to stop its work in 44 of our 75 study villages at some point in the past 25 years. Thus, at the time of our surveys only 31 (i.e. less than half) of the study villages had CRHP-led activities. If CRHP had run intensively in all study villages from its inception to the end of our survey period, we might have seen greater impact. Nevertheless, we have found that the project area continues to have better child survival outcomes and health knowledge among mothers than surrounding areas. Our results contrast with the reported failure of voluntary village health worker programmes in other studies.37 Since CRHP village workers received only minor monetary compensation, remuneration is unlikely to account for the difference. Future studies should look specifically at the effect of compensation (versus, for example, empowerment of village health workers to give them a sense of “ownership” of the programme) on the success of community-based primary health care programmes. We believe that appropriate retrospective evaluation of the lasting impact of such programmes will make an important contribution to the evidence for short-term effects from randomized control trials.
Acknowledgements
We thank the following individuals for their contributions: Raj, Ravi and Shobha Arole from CRHP for allowing us to conduct our field work in the CRHP villages; the mapping team for mapping the villages; our interviewers and supervisors for their hard work conducting the surveys; Prakash Fulpagare for his excellent training of interviewers and advice; Mark Fisher for designing the database; SITES India for entering the vast amount of data; the Ethics Committee of the Maharashtra Association of Anthropological Sciences for excellent advice, encouragement and approval; and the panel of experts convened in Pune in November 2006, who helped conceive the study: Hemant Apte, Ravi DeSouza, BS Garg, Michelle Kermode, RK Mutatkar, Chandrakant S Pandav, Henry Perry and Brahma Reddy.
Funding:
This study was funded by Effective Intervention (located in the Centre for Economic Performance in the London School of Economics).
Competing interests:
Ramaswamy Premkumar taught in CRHP training programmes and conducted research for CRHP between 1999 and 2001. During this study he had no involvement in any CRHP activity in the project villages.
References
- 1.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Millennium Declaration New York: United Nations; 2000 (A/RES/55/2). Available from: http://www.un.org/millennium/declaration/ares552e.htm [accessed 12 July 2010].
- 3.Lawn JE, Cousens S, Zupan J, Lancet Neonatal Survival Steering Team 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 4.Rosato M, Laverack G, Grabman LH, Tripathy P, Nair N, Mwansambo C, et al. Community participation: lessons for maternal, newborn, and child health. Lancet. 2008;372:962–71. doi: 10.1016/S0140-6736(08)61406-3. [DOI] [PubMed] [Google Scholar]
- 5.Ray AS, Bhaduri S. Political economy of rural health care in India. In: Gangopadhyay P, Chatterji M, eds. Economic globalization in Asia Hampshire: Ashgate Publishing Ltd.; 2005. pp. 261–72. [Google Scholar]
- 6.Purohit BC. Private initiatives and policy options: recent health system experience in India. Health Policy Plan. 2001;16:87–97. doi: 10.1093/heapol/16.1.87. [DOI] [PubMed] [Google Scholar]
- 7.Howard-Grabman L, Seoane G, Davenport C. The Warmi Project: a participatory approach to improve maternal and neonatal health – an implementor’s manual Westport: John Snow International, Mothercare Project & Save the Children; 2002. [Google Scholar]
- 8.Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999;354:1955–61. doi: 10.1016/S0140-6736(99)03046-9. [DOI] [PubMed] [Google Scholar]
- 9.Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Members of the MIRA Makwanpur trial team Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364:970–9. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 10.Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, et al. Saksham Study Group Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372:1151–62. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 11.Easterly W.The cartel of good intentions: the problem of bureaucracy in foreign aid. J Pol Reform 20025223–50.doi:10.1080/1384128032000096823 10.1080/1384128032000096823 [DOI] [Google Scholar]
- 12.Tvedt T. Angels of mercy or development diplomats? NGOs and foreign aid Oxford: James Currey; 1998. [Google Scholar]
- 13.Vaux T. The selfish altruist: relief work in famine and war. London: Earthscan; 2001. [Google Scholar]
- 14.De Waal A. Famine crimes: politics and the disaster relief industry in Africa London: James Currey; 1997. [Google Scholar]
- 15.Banerjee A. Making aid work Cambridge: MIT Press; 2007. [Google Scholar]
- 16.Arole M, Arole R. A comprehensive rural health project in Jamkhed (India). In: Newell KW, ed. Health by the people Geneva: World Health Organization; 1975. pp. 70–90. [Google Scholar]
- 17.Comprehensive Rural Health Project [Internet site]. Available from: http://jamkhed.org/ [accessed 13 August 2010].
- 18.Arole M, Arole R. Jamkhed: a comprehensive rural health project London: Macmillan; 1994. [Google Scholar]
- 19.Hossain SMM, Bhuiya A, Khan AR, Uhaa I. Community development and its impact on health: South Asian experience. BMJ. 2004;328:830–3. doi: 10.1136/bmj.328.7443.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma M, Bhatia G. The voluntary community health movement in India: a strengths, weaknesses, opportunities, and threats (SWOT) analysis. J Community Health. 1996;21:453–64. doi: 10.1007/BF01702605. [DOI] [PubMed] [Google Scholar]
- 21.Kermode M, Herrman H, Arole R, White J, Premkumar R, Patel V. Empowerment of women and mental health promotion: a qualitative study in rural Maharashtra, India. BMC Public Health. 2007;7:225. doi: 10.1186/1471-2458-7-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCord C, Premkumar R, Arole S, Arole R. Efficient and effective emergency obstetric care in a rural Indian community where most deliveries are at home. Int J Gynaecol Obstet. 2001;75:297–307, discussion 308-9. doi: 10.1016/S0020-7292(01)00526-4. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberg T.Necessary angels. Natl Geogr Mag 20081266–85.Available from: http://ngm.nationalgeographic.com/print/2008/12/community-doctors/rosenberg-text[accessed 13 August 2010]. [Google Scholar]
- 24.International Institute of Population Studies. National Family Health Survey, India, 1992–93 Bombay: IIPS; 1995. [Google Scholar]
- 25.International Institute for Population Sciences & ORC Macro. National Family Health Survey (NFHS-2), 1998-99: India Mumbai: IIPS; 2000. Available from: http://measuredhs.com/countries/metadata.cfm?surv_id=156&ctry_id=57&SrvyTp=ctry&cn=India [accessed 12 July 2010].
- 26.International Institute for Population Sciences & Macro International. National Family Health Survey (NFHS-3), 2005–06: India Mumbai: IIPS; 2007. Available from: http://measuredhs.com/countries/metadata.cfm?surv_id=264&ctry_id=57&SrvyTp=ctry&cn=India [accessed 12 July 2010].
- 27.Singh R, Singh P. A study on high mortality of children in Melghat region of Amravati (Maharashtra). Stud Tribes Tribals. 2008;6:35–43. [Google Scholar]
- 28.Ashtekar S, Mankad D, Raimane K. Child mortality determinants in three backward districts of Maharashtra 2003–2004, Nandurbar, Jalna and Yavatmal Mumbai: Indira Gandhi Institute of Development Research; 2004. [Google Scholar]
- 29.National Family Health Survey, India. NFHS-3 questionnaires Mumbai: Available from: http://nfhsindia.org/questionnaires.html [accessed 13 August 2010]
- 30.National Family Health Survey, India. NFHS-3 manuals Mumbai: International Institute for Population Sciences. Available from: http://nfhsindia.org/manuals.html [accessed 13 August 2008].
- 31.Bryce J, Boschi-Pinto C, Shibuya K, Black RE, WHO Child Health Epidemiology Reference Group WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 32.Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bull World Health Organ. 2000;78:1246–55. [PMC free article] [PubMed] [Google Scholar]
- 33.Bang AT, Reddy MH, Deshmukh MD. Child mortality in Maharashtra. Econ Polit Wkly. 2002;37:4947–65. [Google Scholar]
- 34.van der Klaauw B, Wang L. Child mortality in rural India Washington: The World Bank; 2004 (World Bank Policy Research Working Paper Series No. 3281).
- 35.The World Bank. World Development Indicators [online database]. Available from: http://data.worldbank.org/indicator [accessed 12 July 2010].
- 36.Maharashtra state – health status Mumbai: Integrated Population and Development Project, United Nations Population Fund; 2009. Available from: http://hetv.org/india/mh/healthstatus/index.html [accessed 28 August 2009].
- 37.Bhattacharyya K, Winch P, LeBan K, Tien M. Community health worker incentives and disincentives: how they affect motivation, retention, and sustainability Arlington: Basic Support for Institutionalizing Child Survival Project (BASICS II), United States Agency for International Development; 2001. [Google Scholar]