Abstract
Although the role of type I interferon (IFN) in the protection against viral infections has been known and studied for decades, its role in other immunologically relevant scenarios, including bacterial infections, shock, autoimmunity, and cancer, is less well defined and potentially much more complicated.
Type 1 IFN was first described over 50 yr ago as the factor responsible for the phenomenon of viral interference (the ability of infection with a virus to induce resistance to infection with a different virus; Isaacs and Lindenmann, 1957; Nagano and Kojima, 1958). Of all the members of the type I IFN family of class II α-helical cytokines in human and mice, IFN-α (represented by several partially homologous genes) and IFN-β (represented by a single gene) are the best characterized and most broadly expressed (Decker et al., 2005). Other type I IFN subtypes are less well characterized, may be more tissue restricted, and may not be represented in all the species. All type I IFN share a ubiquitously expressed heterodimeric receptor composed of two chains, IFNAR1 and IFNAR2, which signal through two Janus family kinases, Tyk2 and Jak1, resulting in recruitment of STAT1 to receptor-bound STAT2 and formation of STAT1-STAT2 heterodimers that dissociate from the receptors and migrate into the nucleus (Li et al., 1996, 1997; Decker et al., 2005). In the nucleus, STAT1-STAT2 heterodimers associate with the transcription factor IFN regulatory factor (IRF) 9 (p48) to form the heterotrimeric complex IFN-stimulated gene factor 3 (ISGF3), which binds to upstream sequence elements (IFN-stimulated response elements) and activates the transcription of IFN-inducible genes. IFNAR can also signal by inducing the activation and nuclear translocation of STAT1 homodimers that bind to IFN-γ–activated sequences in the promoters of IFN-γ–induced genes (Decker et al., 2005).
A distinct category of type I–like IFN, also referred to as type III IFN, is the IFN-λ family, which includes IFN-λ1, -λ2, and -λ3 (also called IL-28A, IL-28B, and IL-29). IFN-λs bind to a receptor comprised of a specific ligand-binding chain (IL-28R) and the IL-10R2 chain, which is shared by the IL-10 family of cytokines (Uzé and Monneron, 2007). The IFN-λ receptors, like the IFNARs, activate the ISGF3 complex, but unlike the IFNARs, they are restricted in their tissue distribution, are not highly expressed in hematopoietic cells, and act predominantly at epithelial surfaces.
The type II IFN subtype is represented by a single gene product, IFN-γ, which binds to a distinct heterodimeric receptor formed by the two chains IFNGR1 and IFNGR2 that signal through Jak1 and Jak2 to phosphorylate STAT1 homodimers (Young and Bream, 2007). STAT1 homodimers then bind to IFN-γ–activated sequences in the promoters of IFN-γ–induced genes. The IFN-γ receptors are ubiquitous, but their expression on different cell types can be modulated.
Production of type I IFN
Type I IFNs can be produced by almost any cell type in the body in response to stimulation of an array of transmembrane and cytosolic receptors. In most cell types, the prevalent pathway of type I IFN induction is the activation of cytosolic receptors that recognize viral or other xenogeneic or autologous nucleic acid, particularly double-stranded RNA (dsRNA; Kawai and Akira, 2010; Fig. 1). The RNA helicases retinoic acid–inducible gene I (RIG-I) and melanoma differentiation-associated gene 5 are the prevalent cytoplasmic receptors responsible for triggering type I IFN secretion. These receptors (RIG-I–like receptors) transmit signals through the mitochondria-localized adaptor molecule IPS-1 or MAVS and the kinases TBK1 and IKKi to activate IRF3 and induce transcription of the type I IFN genes (Kawai and Akira, 2010). A cytosolic DNA sensor, DNA-dependent activator of IRFs (DAI) or Z-DNA binding protein 1, was shown to induce type I IFN in response to the right-handed dsDNA conformation (B-DNA) in a TBK1- and IRF3-mediated mechanism (Kawai and Akira, 2010). However, DAI may not be a unique DNA sensor and may not be active on all cell types. The existence of other cytoplasmic DNA sensors is also suggested by the ability of the bacterial second messenger cyclic-di-GMP to potently induce type I IFN via a mechanism that is independent of DAI or other known cytoplasmic receptors but requires TBK1 and IRF3 (McWhirter et al., 2009). An alternative mechanism of dsDNA sensing depends on the ability of cytosolic DNA-dependent RNA-polymerase III to transcribe B-DNA into 5′-ppp RNA, which then activates type I IFN transcription through RIG-I (Chiu et al., 2009).
Figure 1.
Mechanisms of type I IFN production. Type I IFN production can be triggered by recognition of dsRNA by the cytosolic receptors MDA5 and RIG-I or of dsDNA (B-DNA) by DAI or as yet unknown cytosolic DNA receptors (DNA-RX), leading to activation of the IRF3 via the kinase TBK-1 (or IKKi) and culminating in production of type I IFN (IFNβ/α4). dsDNA can also be transcribed by RNA-polymerase III into 5′-pppRNA, which triggers RIG-I. The ability of the bacterial product cyclic-di-GMP to induce type I IFN suggests the existence of additional DNA sensors. The production of type I IFN can be amplified by a positive feedback loop in which the early produced IFN-β and IFN-α4 trigger the transcription of IRF7 and, at least in DCs, IRF8. In macrophages and DCs, ligation of TLR3, TLR4, TLR7, and TLR9 triggers type I IFN production via signaling through adaptor molecules, including MyD88, TIRAP, TRAM, and TRIF. TRIF associates with TBK1 to activate IRF3, whereas TLR7 and TLR9 signal through MyD88 and IRAK4 to activate IRF7. The cytoplasmic NOD receptors can also induce type I IFN production in response to bacterial cell wall components via activation of the kinase RICK and downstream signaling molecules including NF-κB and TBK-1.
The production of type I IFN is further regulated by a positive feedback loop that is based on the ability of IFN-β and IFN-α4 to induce the transcription of IRF7 and, at least in DCs, IRF8 (Marié et al., 1998; Tailor et al., 2007; Fig. 1). Once phosphorylated, these transcription factors help drive the expression of all genes of the type I IFN family, thereby amplifying type I IFN production.
In some cell types (e.g., macrophages and DCs), type I IFN is produced in response to triggering of the transmembrane receptors Toll-like receptor 3 (TLR3) and TLR4 by dsRNA and lipopolysaccharide, respectively (Fig. 1). TLR3 and TLR4 signal through the adaptor molecule TRIF, which associates with TBK1 and activates IRF3 (Kawai and Akira, 2010). TNF receptor-associated factor 3 (TRAF3) associates with TRIF, as well as TBK1 and IKKi, and is required for production of type I IFN and IL-10, but not other cytokines, in the response to TLR signaling. Thus, TRAF3 links TLR adaptors and downstream regulatory kinases important for IRF activation (Häcker et al., 2006; Oganesyan et al., 2006).
Although all or most cell types can produce type I IFN, the existence of a cell type specialized for the production of large amounts of type I IFN and required for NK cell–mediated killing of virus-infected cells (natural IFN-producing cell) was identified in humans over 30 yr ago (Trinchieri et al., 1978), and more recently was discovered in the mouse (Asselin-Paturel et al., 2001). Natural IFN-producing cells are now usually referred to as plasmacytoid DCs (pDCs) because of their round morphology, eccentric nucleus, and abundant endoplasmic reticulum (Colonna et al., 2004). pDCs preferentially express the intracellular endosomal receptors TLR7 and TLR9, allowing them to respond to single-stranded RNA and DNA viruses, respectively, by triggering signal transduction through the adaptor protein MyD88 (Colonna et al., 2004). These receptors are efficient in inducing type I IFN only in pDCs because these cells constitutively express IRF7 (and IRF8), and the MyD88–IRF7 complex undergoes a spatiotemporal regulation upon TLR ligation such that it is retained in the endosomal compartment, where it induces type I IFN production (Colonna et al., 2004). Bacterial DNA can activate TLR9 in these cells, and it has recently been shown that phagosomal bacteria such as group B streptococcus, but not cytosolic bacteria, also induce type I IFN in conventional DCs via TLR7, MyD88, and IRF1 (Mancuso et al., 2009). In many (but not all) viral infections, pDCs are important for the production of most early circulating type I IFN, but are not essential for antiviral innate resistance, as many other cell types are able to produce type I IFN during the infection (Colonna et al., 2004).
A novel mechanism of type I IFN production by cytoplasmic ligands was shown to involve the nucleotide-binding oligomerization domain–containing protein (NOD) 1 and NOD2 receptors (Pandey et al., 2009; Watanabe et al., 2010). NODs are CARD-containing cytoplasmic molecules in epithelial and hematopoietic cells that contain leucine-rich repeats recognizing related muropeptide subunits of the bacterial wall. NODs signal through the kinase Rip2 (also called RICK) and activate NF-κB and other transcription factors, resulting in the production of proinflammatory cytokines. It has recently been observed, however, that RICK can interact with TRAF3 and MAVS, thus inducing the activation of TBK1 and IKKi, phosphorylation of IRF5 or IRF7, and transcription of the IFN-β gene (Fig. 1). Type I IFN can be induced by Mycobacterium tuberculosis through the activation of NOD2 in macrophages (Pandey et al., 2009) and by Helicobacter pylori through NOD1 in epithelial cells (Watanabe et al., 2010).
Role of type I IFN in viral versus bacterial infections
Exposure of cells to IFN before infection induces an antiviral state that prevents productive viral infection. IFN receptor signaling induces and activates intrinsic antiviral factors such as RNA-activated protein kinase, the 2-5A system, and the Mx proteins. In addition, IFNs potently regulate both innate and adaptive immune responses, acting directly or indirectly on NK cells, T cells, B cells, DCs, and phagocytic cells (Prchal et al., 2009). In most or all pathogenic virus infections, early production of type I IFN is required to limit initial viral replication before effective humoral or cellular adaptive immune mechanisms become operational. Not surprisingly, many viruses have evolved molecular mechanisms to either prevent type I IFN induction or block the signaling through its receptors (Bowie and Unterholzner, 2008). However, in addition to their cell intrinsic or extrinsic antiviral effects, IFNs mediate many anticellular effects by modulating cell viability and function (e.g., induction of apoptosis, autophagy, differentiation, cell migration, and inhibition of cell proliferation and angiogenesis; Bekisz et al., 2010; Mattei et al., 2010). Thus, IFN produced during viral infection, other pathological conditions, or in the presence of DNA released by dying cells may mediate unwanted toxicity or induce pathological damage and inflammatory or autoimmune syndromes (Pascual et al., 2010). A typical example is the role of type I IFN in chronic HIV infection. HIV induces type I IFN, which together with tryptophan catabolism, may drive T cell dysfunction, and also contribute to other aspects of the disease pathogenesis (Boasso et al., 2008).
In bacterial infections, type I IFN is often produced, but its effects are complicated and do not always favor the immune response of the host against the infection. As in viral infections, IFNs sometimes participate in the resistance against bacterial infections. The first observation of the ability of type I IFN to prevent the intracellular replication of bacteria was for pathogens of the genus Chlamydia replicating in nonhematopoietic human cells (de la Maza et al., 1985). In this case, rather than inducing intracellular killing of the bacteria, type I IFN inhibits the Chlamydia growth cycle at the point of transformation from elementary to reticulate body, resulting in chronic infection and failure to produce infectious organisms (Ishihara et al., 2005). The anti-Chlamydia effect of type I IFN is reversed by exogenous l-tryptophan and iron, which are essential for chlamydial growth, possibly secondary to induction of Indoleamine 2,3-dioxygenase (Ishihara et al., 2005; Puccetti, 2007). In human endothelial cells, MAVS, IRF3, IRF7, and endogenous IFN-β are necessary for the control of C. pneumoniae replication (Buss et al., 2010). Similarly, the limited ability of Legionella pneumophila to replicate in murine macrophages is caused by an effective innate response involving autocrine type I IFN signaling. In these cells, IFN suppresses intracellular replication of L. pneumophila via a STAT1-, 2-, and 3-independent pathway that induces the differentiation of classically activated macrophages as well as the production of nitric oxide, which is required for the antibacterial effect (Plumlee et al., 2009). Type I IFN also protects mice against Salmonella typhimurium infection by activating IFN-γ production via STAT4 activation in an IL-12-independent way (Freudenberg et al., 2002). Phagosomal bacteria such as group B streptococci can induce type I IFN via TLR7, and this is important for production of proinflammatory cytokines by macrophages and resistance to the infection (Mancuso et al., 2007, 2009). Other possible antibacterial effects of type I IFN have been postulated based on its ability to modulate innate and adaptive response against bacteria, e.g., NK cell activation, antibody production, and DC activation (Decker et al., 2005).
Often, however, the production of type I IFN is associated with suppression of the innate response to the bacterial infections. Indeed, type I IFN receptor–deficient mice (IFNAR−/−) are more resistant to infection with Francisella tularensis and Listeria monocytogenes than are WT mice (Fehr et al., 1997; Auerbuch et al., 2004; Carrero et al., 2004; Stockinger and Decker, 2008; O’Connor et al., 2009; Henry et al., 2010). Furthermore, the ability of Mycobacterium tuberculosis strains to induce type I IFN production has been proposed to correlate with bacterial virulence (Manca et al., 2001, 2005). M. tuberculosis–infected IFNAR−/− mice have decreased and late mortality compared with WT animals (Manca et al., 2005); however, at least in the first 2–3 mo after infection, their bacterial load was similar in the lungs and only slightly lower in the spleen (Cooper et al., 2000; Manca et al., 2005; Stanley et al., 2007). Modular and pathway analysis of the transcriptomes from the blood of patients with tuberculosis revealed that the signature was dominated by a neutrophil-driven IFN-inducible gene profile, consistent with both type I and type II IFN signaling, suggesting both changes in cellular composition and altered gene expression (Berry et al., 2010). Thus, type I IFN has a hitherto underappreciated role in tuberculosis pathogenesis, which has implications for vaccine, diagnostic, and therapeutic development.
Several mechanisms may account for the deleterious effects of type I IFN in bacterial infections. Type I IFN increases the susceptibility of different cell types to apoptosis-inducing stimuli, in particular macrophages and lymphocytes. This is well described in infection with Listeria, Mycobacteria, Brucella, and Chlamydia spp (Carrero et al., 2004; Gold et al., 2004; O’Connell et al., 2004; Decker et al., 2005; Qiu et al., 2008). In L. monocytogenes infection, the pore-forming virulence factor Listeriolysin O is required for IFN induction in response to infection, and IFN in turn facilitates the Listeriolysin O–induced lysis of lymphocytes and macrophages (Carrero et al., 2004, 2006). Indeed, more virulent strains induce a higher level of type I IFN than do less virulent strains, and the difference in virulence disappears in IFNAR−/− mice (Reutterer et al., 2008).
The mechanisms behind the proapoptotic effects of type I IFN are not fully known. Type I IFN alone is not sufficient to induce apoptosis in most cell types; rather, its effects likely involve up-regulation of caspases and pro-apoptotic innate sensors, such as TLRs and the inflammasomes. For example, production of type I IFN is required for Francisella spp to induce inflammasome activation, possibly caused by the IFN-driven up-regulation of the cytosolic AIM2 inflammasome (Choubey et al., 2010; Fernandes-Alnemri et al., 2010). Activation of AIM2 then results in caspase1 activation and in the production of IL-1β and IL-18 as well as inflammasome-mediated cell death in infected cells. Type I IFN is also important to induce the up-regulation of RIG-I and melanoma differentiation-associated gene 5 in epithelial and other cells and this may represent a type I IFN amplifying loop in several types of infections (Haller et al., 2006; Jaitin and Schreiber, 2007). These receptors respond to foreign nucleic acids and initiate a type I IFN-dependent proapoptotic signaling pathway that requires the mitochondrial adapter IPS-1, induces the production of the proapoptotic BH3-only proteins Puma and Noxa, and culminates in the efficient activation of caspase-9- and Apaf-1-dependent mitochondrial apoptosis (Besch et al., 2009). Type I IFN is also required for the apoptosis resulting from infection-induced activation of the TRIF-associated receptors TLR3 and TLR4, in part by suppressing Akt signaling and degradation of the CDK inhibitor p27 (Hasan et al., 2007; Salaun et al., 2007).
Type I IFN may also interfere with intracellular bactericidal mechanisms. For example, type I IFN, may prevent the ability of IFN-γ to activate antibacterial function of macrophages either by directly interfering with IFN-γ signaling, as discussed or by lowering IFN-γ production. Type I IFN also exerts direct effects on phagocytic cells thus decreasing the activation of anti-microbial products and favoring bacterial replication and release (Rayamajhi et al., 2010). Thus, the evolutionary pressure for a rapid and strong innate resistance in the early stages of aggressive viral infections may have been stronger than that exerted by the relative decrease in resistance to bacterial infections.
Type 1 IFN also directly affects T cell responses. It constrains the secretion of IL-17 by T cells, as observed in F. tularensis and L. monocytogenes infections (Henry et al., 2010) and limits Th1 immune responses to M. tuberculosis in part by inducing negative regulator molecules such as suppressor of cytokine signaling proteins (Manca et al., 2005). Type I IFN can also suppress Th17 responses by inducing the expression of IL-27, which then suppresses IL-17 production (Guo et al., 2008). Type I IFN also triggers the generation of IL-10–producing regulatory T (TR1) cells that dampen both innate and adaptive resistance to infection (Dikopoulos et al., 2005; Levings et al., 2001).
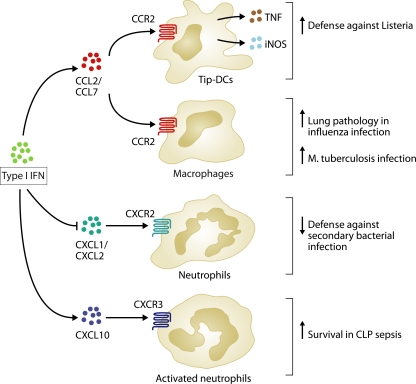
Type 1 IFN might also affect antibacterial resistance by modifying the recruitment and activation of myeloid cells at the site of infection. Resistance to L. monocytogenes infection requires the CCL2- and CCL7-dependent recruitment of a class of activated monocytes/DCs that produces TNF and inducible nitric oxide synthase (Tip-DCs; Fig. 2) and mediates innate immune defense (Jia et al., 2009). Signals through MyD88 are involved in the recruitment and activation of Tip-DCs, but these signals can be replaced in part by type I IFN. Thus, the deletion of IFNAR in MyD88-deficient mice results in increased rather than decreased susceptibility to infection (Jia et al., 2009), indicating that type I IFN has both positive and negative effects on the resistance to L. monocytogenes infection.
Figure 2.
Effects of type I IFN on chemokine production and leukocyte recruitment. Type I IFN drives the production of chemokines, such as CCL2 and CCL7, which recruits CCR2-expressing TNF and inducible nitric oxide synthase–producing DCs (Tip-DCs) that are required for defense against Listeria infection. CCR2-expressing macrophages also contribute to lung pathology during influenza infection and are highly permissive to infection with M. tuberculosis. During influenza infection, type I IFN inhibits the production of the CXCR2 ligands CXCL1 and CXCL2, thus decreasing neutrophil recruitment and dampening host defense against secondary bacterial infections. However, type I IFN also drives the production of CXCL10, which recruits activated CXCR3-expressing neutrophils, thus protecting against sepsis in response to CLP.
The opposing roles of type I IFN are illustrated by influenza virus and secondary bacterial infections (Fig. 2). Type I IFN is important for limiting influenza virus replication. However, IFN also induces chemokines such as CCL2 that recruit CCR2+ monocyte-derived DCs and macrophages to the site of infection, resulting in infection-associated pulmonary pathology and mortality (Lin et al., 2008). On the other hand, type I IFN inhibits the production of CXCR2 ligands, thus reducing neutrophil recruitment and facilitating the development of secondary bacterial pneumonia (Shahangian et al., 2009). A similar type I IFN–mediated decrease in neutrophil numbers was observed in mice infected with lymphocytic choriomeningitis virus and was associated with susceptibility to bacterial infection (Navarini et al., 2006). In addition, IFN induced by intranasal poly-IC treatment exacerbates tuberculosis in mice by recruiting a population of CCR2-expressing macrophages that is highly permissive for M. tuberculosis proliferation (Antonelli et al., 2010).
Role of type I IFN in endotoxin shock
Type I IFN also has complex and often opposing effects in controlling susceptibility and lethality in various models of sepsis or endotoxic shock. During endotoxic shock in mice, type I IFN deficiency reduces LPS-induced lethality but not the production of other proinflammatory cytokines or nitric oxide (Karaghiosoff et al., 2003). Similar results were reported in a model of high lethality septic peritonitis induced by colon ascendens stent, as well as in a model of liver injury after ischemia and reperfusion (Weighardt et al., 2006; Zhai et al., 2008). In the septic peritonitis model, IFNAR−/− mice displayed a significantly increased peritoneal neutrophil recruitment and activation, which is perplexing given that IFNAR−/− mice had increased local production of CCL2, which primarily recruits macrophages, decreased CXCL10, which recruits NK cells and activated Th1 cells, and unaltered CXCL1, which recruits neutrophils (Weighardt et al., 2006). However, despite their increased endotoxin resistance, IFNAR−/− mice have increased late mortality in a low lethality model of cecal ligation and puncture (CLP)–induced sepsis (Fig. 2). Increased mortality in the CLP model was attributed to decreased production of CXCL10 and failure to recruit the phagocytic neutrophils that are necessary for resistance in this model (Kelly-Scumpia et al., 2010). The differential effect of type I IFN on neutrophil recruitment in the two models of polymicrobial sepsis is difficult to explain and might relate to differences in bacterial load and lethality. In influenza virus–infected mice, decreased neutrophil recruitment to the lungs was attributed to the ability of type I IFN to decrease the production of CXCR2 ligands, such as CXCL1 and 2. This was not observed in either sepsis model, whereas CXCL10 production was decreased in both sepsis models, albeit with opposite effects on neutrophil recruitment and activation (Weighardt et al., 2006; Shahangian et al., 2009; Kelly-Scumpia et al., 2010). Clearly the role of type I IFN in chemokine-induced neutrophil recruitment falls short of explaining the full range of type I IFN’s regulatory effects on toxicity and infection in these complex models. A quite different mechanism should also be invoked to explain how type I IFN drives TNF-induced lethal shock (Huys et al., 2009). TNF induces IFN-β production in vitro, and this may establish an autocrine loop that promotes the sustained production of chemokines and other STAT1-dependent genes (Yarilina et al., 2008).
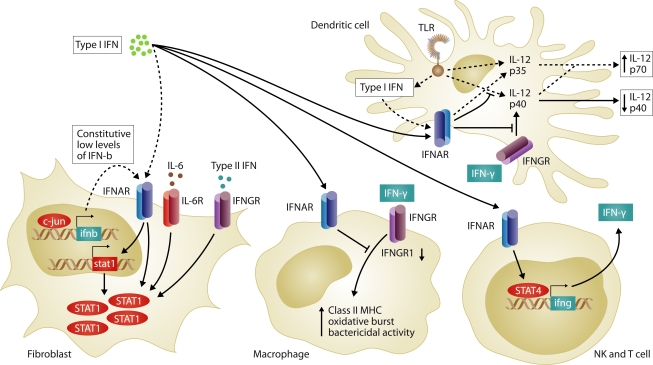
Cross-regulation of type I and II IFNs
Although type I and type II IFN share some common mechanisms in the activation of the immune response, IFN-γ is generally a more potent activator of phagocytic cell and antigen-presenting cell function than type I IFN. The interaction between type I and type II IFN signals is complex and has received relatively little attention. Both types of IFN are often produced during the course of the same immune response, and evidence suggests that cross-regulation exerts physiologically meaningful effects (Fig. 3). For example, exposure of macrophages to type I IFN in vitro inhibits IFN-γ binding to the cells and prevents IFN-γ from enhancing class II MHC expression, Fc receptor expression, and oxidative burst (Ling et al., 1985; Yoshida et al., 1988). L. monocytogenes infection induces type I IFN production, which suppresses macrophage activation by IFN-γ by decreasing IFNGR1 mRNA and IFN-γ receptor surface expression (Rayamajhi et al., 2010).
Figure 3.
Cross-talk between type I IFN and IFN-γ. High levels of type I IFN (solid arrows) decrease the expression of IFNGR1 and inhibit IFN-γ-induced activation of MHC class II expression, oxidative burst, and bactericidal activity in macrophages. However, low constitutive levels of type I IFN (dashed arrows) prime cells for secondary responses to type I and II IFNs and IL-6 by favoring expression and activation of STAT1 (shown in fibroblasts). In DCs, low concentrations of type I IFN are essential for the optimal production of the IFN-γ–inducing cytokine IL-12p70, whereas higher levels of type I IFN suppress TLR- and IFN-γ–induced IL-12p40 expression, thus dampening IL-12p70 production. Type I IFN can also directly induce the production of IFN-γ in NK cell and T cells via the activation of STAT4.
In addition to signaling through the ISGF3 complex, type I IFN can activate STAT1 homodimers, and thus mimic the gene induction pattern of IFN-γ (van Boxel-Dezaire et al., 2006). In addition, cells are continuously exposed to low levels of type I IFN, and the resulting weak signal is required for the cells to produce high levels of IFN in response to inducing stimuli (Taniguchi and Takaoka, 2001). For example, the priming of cells by constitutive sub-threshold type I IFN signaling enhances their response to stimulation with other cytokines, including an at least 10-fold enhancement of the response to IFN-γ, by favoring STAT1 activation. This sensitization has been attributed to the association of the two nonligand binding receptors components, IFNAR1 and IFNGR2, in the caveolar membrane domains (Takaoka et al., 2000). More recently, constitutive expression of c-Jun was shown to induce endocrine or paracrine production of low levels of IFN-β that maintains expression of STAT1 required for optimal cellular responses to type I IFN, as well as to IFN-γ and IL-6 (Gough et al., 2010). Furthermore, the induction of low levels of type I IFN during stimulation of DCs through innate receptors is essential for optimal production of the IL-12 p70 heterodimer (Gautier et al., 2005), thus indirectly contributing to IFN-γ production. In the presence of high concentrations of type I IFN, however, the production of IL-12p40 is suppressed, limiting the amount of IL-12 heterodimer (Byrnes et al., 2001).
By signaling through STAT4, type I IFN has also been reported to directly induce the production of IFN-γ in NK and T cells, particularly in the absence of STAT1, which normally suppresses IFN-γ production (Brinkmann et al., 1993; Freudenberg et al., 2002; Nguyen et al., 2000). Because of the transient nature of STAT4 activation by type I IFN and the regulatory effect of STAT1, the physiological role of type I IFN in controlling IFN-γ production, as compared with classical IFN-γ–inducing cytokines such as IL-2 and IL-12, remains to be evaluated.
Type I IFN and autoimmunity
The connection between viral or other infections and autoimmunity has been known for a long time, although the precise mechanisms and the possible role of type I IFN in pathogenesis has remained difficult to determine (Münz et al., 2009; Rose, 2010). The development of Lyme arthritis after Borrelia burgdorferi infection is associated with an IFN-induced gene expression signature that is independent of T and B cells (Miller et al., 2008). Blocking type I, but not type II, IFN signaling reduced both the IFN signature and the development of arthritis (Miller et al., 2008). Therapeutic treatment with type I IFN for cancer, chronic viral infections, and multiple sclerosis has been associated with significant collateral toxic effects characterized by chronic fatigue because of transient or chronic autoimmune pathology (Malik et al., 2001; Biggioggero et al., 2010). The mechanisms of type I IFN-induced autoimmunity has been attributed in part to increased DC activation and antigen uptake and presentation from apoptotic cells, as well as increased production of autoantibodies (Jego et al., 2003; Rizza et al., 2010).
A prominent feature of systemic lupus erythematosus (SLE) is the increased expression of type I IFN–regulated genes in blood cells, which is often associated with the presence of IFN in the plasma (Bennett et al., 2003; Rönnblom and Alm, 2003). The cells producing type I IFN in SLE appear to be predominantly pDC, which are reduced in number in the blood but are abundant in skin and lymph nodes (Rönnblom et al., 2009). In SLE patients, immune complexes consisting of autoantibodies bound to self-DNA and RNA can stimulate production of type I IFN through TLR7 and TLR9 after being internalized following binding to Fc receptors (Rönnblom et al., 2009). Stimulation of pDCs through TLR7 and TLR9 also renders these cells resistant to the apoptotic effect of glucocorticosteroids, thus decreasing the ability of these drugs to reduce type I IFN production and effectively treat the patients (Guiducci et al., 2010). Several genes that have been associated with susceptibility to SLE are involved either in the regulation of the IFN response or in the ability to clear immune complexes through Fc receptors, and thus to degrade nucleic acid released from dying cells (Morel, 2010). The pathogenic role of type I IFN in SLE is mediated in part by its ability to induce immune activation, including a positive feedback loop that induces plasma cell maturation and increases autoantibody formation (Jego et al., 2003). Pathology in SLE could also be caused by the ability of type I IFN to directly induce pathogenic effects at the tissue level. For example, type I IFN directly induces vasculogenesis and may be responsible for the premature atherosclerosis found in SLE patients (Denny et al., 2007). The role of type I IFN in this disease has now been confirmed in lupus-prone mouse strains (Agrawal et al., 2009; Triantafyllopoulou et al., 2010).
The presence of pDCs in autoimmune target tissues is associated with an IFN-induced gene signature, suggesting the possible involvement of type I IFN in several other autoimmune disorders, including diabetes mellitus, dermatomyositis, and Sjogren’s syndrome (Guiducci et al., 2009). A clear association also exists between type I IFN and cutaneous skin diseases characterized by interface dermatitis, such as lichen planus, dermatomyositis, lichen sclerosus, cutaneous lupus, and cutaneous graft-versus-host disease, in which pDC infiltrates and deposition of nucleic acid–containing immune complexes is observed (Wenzel and Tüting, 2008). A pDC infiltrate linked to an IFN signature is also observed in psoriasis. Although tissue deposition of immune complexes is not observed in psoriasis, the antimicrobial cationic peptide LL-37 accumulates in lesions where it binds to and transports self-DNA and RNA to the early endosomal compartment of pDC, thereby stimulating type I IFN production through TLR9 and TLR7, respectively (Ganguly et al., 2009).
The involvement of type I IFN in the pathogenesis of several autoimmune diseases indicates the possibility to therapeutically target either type I IFN or the mechanisms leading to IFN production in those diseases (Guiducci et al., 2009; Pascual et al., 2010). Paradoxically, however, in several experimental and clinical autoimmune conditions, treatment with type I IFN or its induction has proven beneficial. In most cases, these conditions are tissue-specific autoimmune or inflammatory syndromes characterized by activation of effector Th1 and Th17 responses, including arthritis, inflammatory bowel diseases, and multiple sclerosis (Lee et al., 2006; Yarilina et al., 2007; Prinz et al., 2008). IFN-β is a common and effective treatment for reducing disease recurrence in multiple sclerosis (Noseworthy et al., 2000; Comi, 2009). The mechanisms by which type I IFN affects these pathological conditions are most likely linked to its immunoregulatory effects, including its ability to affect IL-12 production, to activate regulatory T cells, and to constrain Th17 cell–mediated autoimmune inflammation (Byrnes et al., 2001; Levings et al., 2001; Dikopoulos et al., 2005; Guo et al., 2008).
Type I IFN and cancer
Several of the biological functions of type I IFN, including its regulation of innate and adaptive immunity and its antiangiogenic and proapoptotic effects, make it an obvious candidate for anti-cancer therapy. Indeed, type I IFN has been used with some success for the treatment of several types of cancer, including hematological malignancies (hairy cell leukemia, chronic myeloid leukemia, and some B and T cell lymphomas), and solid tumors (melanoma, renal carcinoma, and Kaposi’s sarcoma; Ferrantini et al., 2007; Moschos and Kirkwood, 2007). In some of those indications, type I IFN therapy is still in use; in others it has been superseded by more effective targeted therapies. The antitumor effect of type I IFN therapy is accompanied by severe side effects, including autoimmune and inflammatory symptoms, as well as direct tissue toxicity, that are probably responsible for the hematological and neurological side effects. It was recently shown that endogenous type I IFN, like IFN-γ, prevents the growth of primary carcinogen-induced and transplantable tumors (Dunn et al., 2005). Unexpectedly, unlike IFN-γ, type I IFN does not act directly on tumor cells. Hematopoietic cells, in particular NK cells, are critical IFN-α/β targets during development of protective antitumor responses (Dunn et al., 2005; Swann et al., 2007). Thus, one of the earliest described immunoregulatory functions of type I IFN—its ability to regulate NK cell functions (Trinchieri and Santoli, 1978)—has now been proven to be one of the major mechanisms of the regulation of tumor growth by endogenous type I IFN. However, a possible intrinsic role of type I IFN in regulating tumor cell proliferation, apoptosis, and autophagy, as discussed above for infectious diseases, should not be discounted and has only recently begun to be investigated in depth (Goldszmid et al., 2009). The ability of oncogenes such as Ras and HPV16 E6E7 to down-regulate IFN-inducing innate receptors, RIG-I and TLR9, respectively, is suggestive of a role of type I IFN in modulating not only the infectiveness of oncogenic viruses but also their cell transforming ability (Hasan et al., 2007; Shmulevitz et al., 2010).
Conclusions
In these last few years, our understanding of the mechanisms controlling the production and the function of type I IFN in infection, immunity, autoimmunity, and oncology has been progressing at a very fast pace, and the role of this family of cytokines in physiology and pathology is finally starting to be fully appreciated. Type I IFN are essential for organisms to survive acute viral infection, even if many viruses have developed mechanisms to escape their effects. However, the organism pays a price for this effective innate resistance, as the toxicity of IFN causes acute and chronic morbidity and alters innate and adaptive defenses against other opportunistic infections. This fact was recognized very early, as Dr. Louis Cruveilhier wrote during the Spanish flu epidemic of 1918–1919: “Si la grippe tue, c’est parce qu’elle frappe au thorax” or (to paraphrase), “Flu condemns, and additional infection executes” (Cruveilhier, 1919). However, as the mechanisms underlying the actions of type I IFN are becoming better understood, there is hope of a more rationale therapeutic targeting.
Acknowledgments
I thank Alan Sher and Anne O’Garra for critically reading the manuscript.
Footnotes
Abbreviations used:
- CLP
- cecal ligation and puncture
- DAI
- DNA-dependent activator of IRFs
- dsRNA
- double-stranded RNA
- IRF
- IFN regulatory factor
- ISGF3
- IFN-stimulated gene factor 3
- NOD
- nucleotide-binding oligomerization domain–containing protein
- pDC
- plasmacytoid DC
- RIG-I
- retinoic acid–inducible gene I
- SLE
- systemic lupus erythematosus
- TLR
- Toll-like receptor
References
- Agrawal H., Jacob N., Carreras E., Bajana S., Putterman C., Turner S., Neas B., Mathian A., Koss M.N., Stohl W., et al. 2009. Deficiency of type I IFN receptor in lupus-prone New Zealand mixed 2328 mice decreases dendritic cell numbers and activation and protects from disease. J. Immunol. 183:6021–6029 10.4049/jimmunol.0803872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonelli L.R., Gigliotti Rothfuchs A., Goncalves R., Roffe E., Cheever A.W., Bafica A., Salazar A.M., Feng C.G., Sher A. 2010. Intranasal Poly-IC treatment exacerbates tuberculosis in mice through the pulmonary recruitment of a pathogen-permissive monocyte/macrophage population. J. Clin. Invest. 120:2674–2682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asselin-Paturel C., Boonstra A., Dalod M., Durand I., Yessaad N., Dezutter-Dambuyant C., Vicari A., O’Garra A., Biron C., Brière F., Trinchieri G. 2001. Mouse type I IFN-producing cells are immature APCs with plasmacytoid morphology. Nat. Immunol. 2:1144–1150 10.1038/ni736 [DOI] [PubMed] [Google Scholar]
- Auerbuch V., Brockstedt D.G., Meyer-Morse N., O’Riordan M., Portnoy D.A. 2004. Mice lacking the type I interferon receptor are resistant to Listeria monocytogenes. J. Exp. Med. 200:527–533 10.1084/jem.20040976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekisz J., Baron S., Balinsky C., Morrow A., Zoon K.C. 2010. Antiproliferative properties of type I and type II interferon. Pharmaceuticals (Basel). 3:994–1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett L., Palucka A.K., Arce E., Cantrell V., Borvak J., Banchereau J., Pascual V. 2003. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J. Exp. Med. 197:711–723 10.1084/jem.20021553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry M.P.R., Graham C.M., McNab F.W., Xu Z., Bloch S.A.A., Oni T., Wilkinson K.A., Banchereau R., Skinner J., Wilkinson R.J., et al. 2010. An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature. 466:973–977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besch R., Poeck H., Hohenauer T., Senft D., Hacker G., Berking C., Hornung V., Endres S., Ruzicka T., Rothenfusser S., Hartmann G. 2009. Proapoptotic signaling induced by RIG-I and MDA-5 results in type I interferon-independent apoptosis in human melanoma cells. J. Clin. Invest. 119:2399–2411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggioggero M., Gabbriellini L., Meroni P.L. 2010. Type I interferon therapy and its role in autoimmunity. Autoimmunity. 43:248–254 10.3109/08916930903510971 [DOI] [PubMed] [Google Scholar]
- Boasso A., Hardy A.W., Anderson S.A., Dolan M.J., Shearer G.M. 2008. HIV-induced type I interferon and tryptophan catabolism drive T cell dysfunction despite phenotypic activation. PLoS One. 3:e2961 10.1371/journal.pone.0002961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie A.G., Unterholzner L. 2008. Viral evasion and subversion of pattern-recognition receptor signalling. Nat. Rev. Immunol. 8:911–922 10.1038/nri2436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkmann V., Geiger T., Alkan S., Heusser C.H. 1993. Interferon alpha increases the frequency of interferon-γ–producing human CD4+ T cells. J. Exp. Med. 178:1655–1663 10.1084/jem.178.5.1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss C., Opitz B., Hocke A.C., Lippmann J., van Laak V., Hippenstiel S., Krüll M., Suttorp N., Eitel J. 2010. Essential role of mitochondrial antiviral signaling, IFN regulatory factor (IRF)3, and IRF7 in Chlamydophila pneumoniae-mediated IFN-beta response and control of bacterial replication in human endothelial cells. J. Immunol. 184:3072–3078 10.4049/jimmunol.0902947 [DOI] [PubMed] [Google Scholar]
- Byrnes A.A., Ma X., Cuomo P., Park K., Wahl L., Wolf S.F., Zhou H., Trinchieri G., Karp C.L. 2001. Type I interferons and IL-12: convergence and cross-regulation among mediators of cellular immunity. Eur. J. Immunol. 31:2026–2034 [DOI] [PubMed] [Google Scholar]
- Carrero J.A., Calderon B., Unanue E.R. 2004. Type I interferon sensitizes lymphocytes to apoptosis and reduces resistance to Listeria infection. J. Exp. Med. 200:535–540 10.1084/jem.20040769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrero J.A., Calderon B., Unanue E.R. 2006. Lymphocytes are detrimental during the early innate immune response against Listeria monocytogenes. J. Exp. Med. 203:933–940 10.1084/jem.20060045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu Y.H., Macmillan J.B., Chen Z.J. 2009. RNA polymerase III detects cytosolic DNA and induces type I interferons through the RIG-I pathway. Cell. 138:576–591 10.1016/j.cell.2009.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choubey D., Duan X., Dickerson E., Ponomareva L., Panchanathan R., Shen H., Srivastava R. 2010. Interferon-inducible p200-family proteins as novel sensors of cytoplasmic DNA: role in inflammation and autoimmunity. J. Interferon Cytokine Res. 30:371–380 10.1089/jir.2009.0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colonna M., Trinchieri G., Liu Y.J. 2004. Plasmacytoid dendritic cells in immunity. Nat. Immunol. 5:1219–1226 10.1038/ni1141 [DOI] [PubMed] [Google Scholar]
- Comi G. 2009. Shifting the paradigm toward earlier treatment of multiple sclerosis with interferon beta. Clin. Ther. 31:1142–1157 10.1016/j.clinthera.2009.06.007 [DOI] [PubMed] [Google Scholar]
- Cooper A.M., Pearl J.E., Brooks J.V., Ehlers S., Orme I.M. 2000. Expression of the nitric oxide synthase 2 gene is not essential for early control of Mycobacterium tuberculosis in the murine lung. Infect. Immun. 68:6879–6882 10.1128/IAI.68.12.6879-6882.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruveilhier L. 1919. La grippe à Paris en 1919. Le Journal Médical Français. 448 [Google Scholar]
- de la Maza L.M., Peterson E.M., Goebel J.M., Fennie C.W., Czarniecki C.W. 1985. Interferon-induced inhibition of Chlamydia trachomatis: dissociation from antiviral and antiproliferative effects. Infect. Immun. 47:719–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker T., Müller M., Stockinger S. 2005. The yin and yang of type I interferon activity in bacterial infection. Nat. Rev. Immunol. 5:675–687 10.1038/nri1684 [DOI] [PubMed] [Google Scholar]
- Denny M.F., Thacker S., Mehta H., Somers E.C., Dodick T., Barrat F.J., McCune W.J., Kaplan M.J. 2007. Interferon-alpha promotes abnormal vasculogenesis in lupus: a potential pathway for premature atherosclerosis. Blood. 110:2907–2915 10.1182/blood-2007-05-089086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dikopoulos N., Bertoletti A., Kröger A., Hauser H., Schirmbeck R., Reimann J. 2005. Type I IFN negatively regulates CD8+ T cell responses through IL-10-producing CD4+ T regulatory 1 cells. J. Immunol. 174:99–109 [DOI] [PubMed] [Google Scholar]
- Dunn G.P., Bruce A.T., Sheehan K.C., Shankaran V., Uppaluri R., Bui J.D., Diamond M.S., Koebel C.M., Arthur C., White J.M., Schreiber R.D. 2005. A critical function for type I interferons in cancer immunoediting. Nat. Immunol. 6:722–729 10.1038/ni1213 [DOI] [PubMed] [Google Scholar]
- Fehr T., Schoedon G., Odermatt B., Holtschke T., Schneemann M., Bachmann M.F., Mak T.W., Horak I., Zinkernagel R.M. 1997. Crucial role of interferon consensus sequence binding protein, but neither of interferon regulatory factor 1 nor of nitric oxide synthesis for protection against murine listeriosis. J. Exp. Med. 185:921–931 10.1084/jem.185.5.921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes-Alnemri T., Yu J.W., Juliana C., Solorzano L., Kang S., Wu J., Datta P., McCormick M., Huang L., McDermott E., et al. 2010. The AIM2 inflammasome is critical for innate immunity to Francisella tularensis. Nat. Immunol. 11:385–393 10.1038/ni.1859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrantini M., Capone I., Belardelli F. 2007. Interferon-alpha and cancer: mechanisms of action and new perspectives of clinical use. Biochimie. 89:884–893 10.1016/j.biochi.2007.04.006 [DOI] [PubMed] [Google Scholar]
- Freudenberg M.A., Merlin T., Kalis C., Chvatchko Y., Stübig H., Galanos C. 2002. Cutting edge: a murine, IL-12-independent pathway of IFN-gamma induction by gram-negative bacteria based on STAT4 activation by Type I IFN and IL-18 signaling. J. Immunol. 169:1665–1668 [DOI] [PubMed] [Google Scholar]
- Ganguly D., Chamilos G., Lande R., Gregorio J., Meller S., Facchinetti V., Homey B., Barrat F.J., Zal T., Gilliet M. 2009. Self-RNA–antimicrobial peptide complexes activate human dendritic cells through TLR7 and TLR8. J. Exp. Med. 206:1983–1994 10.1084/jem.20090480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautier G., Humbert M., Deauvieau F., Scuiller M., Hiscott J., Bates E.E., Trinchieri G., Caux C., Garrone P. 2005. A type I interferon autocrine-paracrine loop is involved in Toll-like receptor–induced interleukin-12p70 secretion by dendritic cells. J. Exp. Med. 201:1435–1446 10.1084/jem.20041964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold J.A., Hoshino Y., Hoshino S., Jones M.B., Nolan A., Weiden M.D. 2004. Exogenous gamma and alpha/beta interferon rescues human macrophages from cell death induced by Bacillus anthracis. Infect. Immun. 72:1291–1297 10.1128/IAI.72.3.1291-1297.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldszmid R.S., Hasan U.A., Trinchieri G. 2009. Double stranded RNA tricks melanoma cells into committing suicide. Pigment Cell Melanoma Res. 22:705–706 10.1111/j.1755-148X.2009.00631.x [DOI] [PubMed] [Google Scholar]
- Gough D.J., Messina N.L., Hii L., Gould J.A., Sabapathy K., Robertson A.P., Trapani J.A., Levy D.E., Hertzog P.J., Clarke C.J., Johnstone R.W. 2010. Functional crosstalk between type I and II interferon through the regulated expression of STAT1. PLoS Biol. 8:e1000361 10.1371/journal.pbio.1000361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guiducci C., Coffman R.L., Barrat F.J. 2009. Signalling pathways leading to IFN-alpha production in human plasmacytoid dendritic cell and the possible use of agonists or antagonists of TLR7 and TLR9 in clinical indications. J. Intern. Med. 265:43–57 10.1111/j.1365-2796.2008.02050.x [DOI] [PubMed] [Google Scholar]
- Guiducci C., Gong M., Xu Z., Gill M., Chaussabel D., Meeker T., Chan J.H., Wright T., Punaro M., Bolland S., et al. 2010. TLR recognition of self nucleic acids hampers glucocorticoid activity in lupus. Nature. 465:937–941 10.1038/nature09102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo B., Chang E.Y., Cheng G. 2008. The type I IFN induction pathway constrains Th17-mediated autoimmune inflammation in mice. J. Clin. Invest. 118:1680–1690 10.1172/JCI33342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häcker H., Redecke V., Blagoev B., Kratchmarova I., Hsu L.C., Wang G.G., Kamps M.P., Raz E., Wagner H., Häcker G., et al. 2006. Specificity in Toll-like receptor signalling through distinct effector functions of TRAF3 and TRAF6. Nature. 439:204–207 10.1038/nature04369 [DOI] [PubMed] [Google Scholar]
- Haller O., Kochs G., Weber F. 2006. The interferon response circuit: induction and suppression by pathogenic viruses. Virology. 344:119–130 10.1016/j.virol.2005.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan U.A., Caux C., Perrot I., Doffin A.C., Menetrier-Caux C., Trinchieri G., Tommasino M., Vlach J. 2007. Cell proliferation and survival induced by Toll-like receptors is antagonized by type I IFNs. Proc. Natl. Acad. Sci. USA. 104:8047–8052 10.1073/pnas.0700664104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry T., Kirimanjeswara G.S., Ruby T., Jones J.W., Peng K., Perret M., Ho L., Sauer J.D., Iwakura Y., Metzger D.W., Monack D.M. 2010. Type I IFN signaling constrains IL-17A/F secretion by gammadelta T cells during bacterial infections. J. Immunol. 184:3755–3767 10.4049/jimmunol.0902065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huys L., Van Hauwermeiren F., Dejager L., Dejonckheere E., Lienenklaus S., Weiss S., Leclercq G., Libert C. 2009. Type I interferon drives tumor necrosis factor–induced lethal shock. J. Exp. Med. 206:1873–1882 10.1084/jem.20090213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs A., Lindenmann J. 1957. Virus interference. I. The interferon. Proc. R. Soc. Lond. B Biol. Sci. 147:258–267 10.1098/rspb.1957.0048 [DOI] [PubMed] [Google Scholar]
- Ishihara T., Aga M., Hino K., Ushio C., Taniguchi M., Iwaki K., Ikeda M., Kurimoto M. 2005. Inhibition of Chlamydia trachomatis growth by human interferon-alpha: mechanisms and synergistic effect with interferon-gamma and tumor necrosis factor-alpha. Biomed. Res. 26:179–185 10.2220/biomedres.26.179 [DOI] [PubMed] [Google Scholar]
- Jaitin D.A., Schreiber G. 2007. Upregulation of a small subset of genes drives type I interferon-induced antiviral memory. J. Interferon Cytokine Res. 27:653–664 10.1089/jir.2006.0162 [DOI] [PubMed] [Google Scholar]
- Jego G., Palucka A.K., Blanck J.P., Chalouni C., Pascual V., Banchereau J. 2003. Plasmacytoid dendritic cells induce plasma cell differentiation through type I interferon and interleukin 6. Immunity. 19:225–234 10.1016/S1074-7613(03)00208-5 [DOI] [PubMed] [Google Scholar]
- Jia T., Leiner I., Dorothee G., Brandl K., Pamer E.G. 2009. MyD88 and Type I interferon receptor-mediated chemokine induction and monocyte recruitment during Listeria monocytogenes infection. J. Immunol. 183:1271–1278 10.4049/jimmunol.0900460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaghiosoff M., Steinborn R., Kovarik P., Kriegshäuser G., Baccarini M., Donabauer B., Reichart U., Kolbe T., Bogdan C., Leanderson T., et al. 2003. Central role for type I interferons and Tyk2 in lipopolysaccharide-induced endotoxin shock. Nat. Immunol. 4:471–477 10.1038/ni910 [DOI] [PubMed] [Google Scholar]
- Kawai T., Akira S. 2010. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat. Immunol. 11:373–384 10.1038/ni.1863 [DOI] [PubMed] [Google Scholar]
- Kelly-Scumpia K.M., Scumpia P.O., Delano M.J., Weinstein J.S., Cuenca A.G., Wynn J.L., Moldawer L.L. 2010. Type I interferon signaling in hematopoietic cells is required for survival in mouse polymicrobial sepsis by regulating CXCL10. J. Exp. Med. 207:319–326 10.1084/jem.20091959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Rachmilewitz D., Raz E. 2006. Homeostatic effects of TLR9 signaling in experimental colitis. Ann. N. Y. Acad. Sci. 1072:351–355 10.1196/annals.1326.022 [DOI] [PubMed] [Google Scholar]
- Levings M.K., Sangregorio R., Galbiati F., Squadrone S., de Waal Malefyt R., Roncarolo M.G. 2001. IFN-alpha and IL-10 induce the differentiation of human type 1 T regulatory cells. J. Immunol. 166:5530–5539 [DOI] [PubMed] [Google Scholar]
- Li X., Leung S., Qureshi S., Darnell J.E., Jr., Stark G.R. 1996. Formation of STAT1-STAT2 heterodimers and their role in the activation of IRF-1 gene transcription by interferon-alpha. J. Biol. Chem. 271:5790–5794 10.1074/jbc.271.10.5790 [DOI] [PubMed] [Google Scholar]
- Li X., Leung S., Kerr I.M., Stark G.R. 1997. Functional subdomains of STAT2 required for preassociation with the alpha interferon receptor and for signaling. Mol. Cell. Biol. 17:2048–2056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin K.L., Suzuki Y., Nakano H., Ramsburg E., Gunn M.D. 2008. CCR2+ monocyte-derived dendritic cells and exudate macrophages produce influenza-induced pulmonary immune pathology and mortality. J. Immunol. 180:2562–2572 [DOI] [PubMed] [Google Scholar]
- Ling P.D., Warren M.K., Vogel S.N. 1985. Antagonistic effect of interferon-beta on the interferon-gamma-induced expression of Ia antigen in murine macrophages. J. Immunol. 135:1857–1863 [PubMed] [Google Scholar]
- Malik U.R., Makower D.F., Wadler S. 2001. Interferon-mediated fatigue. Cancer. 92:1664–1668 [DOI] [PubMed] [Google Scholar]
- Manca C., Tsenova L., Bergtold A., Freeman S., Tovey M., Musser J.M., Barry C.E., III, Freedman V.H., Kaplan G. 2001. Virulence of a Mycobacterium tuberculosis clinical isolate in mice is determined by failure to induce Th1 type immunity and is associated with induction of IFN-alpha /beta. Proc. Natl. Acad. Sci. USA. 98:5752–5757 10.1073/pnas.091096998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manca C., Tsenova L., Freeman S., Barczak A.K., Tovey M., Murray P.J., Barry C., Kaplan G. 2005. Hypervirulent M. tuberculosis W/Beijing strains upregulate type I IFNs and increase expression of negative regulators of the Jak-Stat pathway. J. Interferon Cytokine Res. 25:694–701 10.1089/jir.2005.25.694 [DOI] [PubMed] [Google Scholar]
- Mancuso G., Midiri A., Biondo C., Beninati C., Zummo S., Galbo R., Tomasello F., Gambuzza M., Macrì G., Ruggeri A., et al. 2007. Type I IFN signaling is crucial for host resistance against different species of pathogenic bacteria. J. Immunol. 178:3126–3133 [DOI] [PubMed] [Google Scholar]
- Mancuso G., Gambuzza M., Midiri A., Biondo C., Papasergi S., Akira S., Teti G., Beninati C. 2009. Bacterial recognition by TLR7 in the lysosomes of conventional dendritic cells. Nat. Immunol. 10:587–594 10.1038/ni.1733 [DOI] [PubMed] [Google Scholar]
- Marié I., Durbin J.E., Levy D.E. 1998. Differential viral induction of distinct interferon-alpha genes by positive feedback through interferon regulatory factor-7. EMBO J. 17:6660–6669 10.1093/emboj/17.22.6660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei F., Schiavoni G., Tough D.F. 2010. Regulation of immune cell homeostasis by type I interferons. Cytokine Growth Factor Rev. 10.1016/j.cytogfr.2010.05.002 [DOI] [PubMed] [Google Scholar]
- McWhirter S.M., Barbalat R., Monroe K.M., Fontana M.F., Hyodo M., Joncker N.T., Ishii K.J., Akira S., Colonna M., Chen Z.J., et al. 2009. A host type I interferon response is induced by cytosolic sensing of the bacterial second messenger cyclic-di-GMP. J. Exp. Med. 206:1899–1911 10.1084/jem.20082874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J.C., Ma Y., Bian J., Sheehan K.C., Zachary J.F., Weis J.H., Schreiber R.D., Weis J.J. 2008. A critical role for type I IFN in arthritis development following Borrelia burgdorferi infection of mice. J. Immunol. 181:8492–8503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morel L. 2010. Genetics of SLE: evidence from mouse models. Nat Rev Rheumatol. 6:348–357 10.1038/nrrheum.2010.63 [DOI] [PubMed] [Google Scholar]
- Moschos S., Kirkwood J.M. 2007. Present role and future potential of type I interferons in adjuvant therapy of high-risk operable melanoma. Cytokine Growth Factor Rev. 18:451–458 10.1016/j.cytogfr.2007.06.020 [DOI] [PubMed] [Google Scholar]
- Münz C., Lünemann J.D., Getts M.T., Miller S.D. 2009. Antiviral immune responses: triggers of or triggered by autoimmunity? Nat. Rev. Immunol. 9:246–258 10.1038/nri2527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagano Y., Kojima Y. 1958. Inhibition de l’infection vaccinale par un facteur liquide dans le tissu infecte par le virus homologue. C. R. Seances Soc. Biol. Fil. 152:1627–1629 [PubMed] [Google Scholar]
- Navarini A.A., Recher M., Lang K.S., Georgiev P., Meury S., Bergthaler A., Flatz L., Bille J., Landmann R., Odermatt B., et al. 2006. Increased susceptibility to bacterial superinfection as a consequence of innate antiviral responses. Proc. Natl. Acad. Sci. USA. 103:15535–15539 10.1073/pnas.0607325103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen K.B., Cousens L.P., Doughty L.A., Pien G.C., Durbin J.E., Biron C.A. 2000. Interferon alpha/beta-mediated inhibition and promotion of interferon gamma: STAT1 resolves a paradox. Nat. Immunol. 1:70–76 [DOI] [PubMed] [Google Scholar]
- Noseworthy J.H., Lucchinetti C., Rodriguez M., Weinshenker B.G. 2000. Multiple sclerosis. N. Engl. J. Med. 343:938–952 10.1056/NEJM200009283431307 [DOI] [PubMed] [Google Scholar]
- O’Connell R.M., Saha S.K., Vaidya S.A., Bruhn K.W., Miranda G.A., Zarnegar B., Perry A.K., Nguyen B.O., Lane T.F., Taniguchi T., et al. 2004. Type I interferon production enhances susceptibility to Listeria monocytogenes infection. J. Exp. Med. 200:437–445 10.1084/jem.20040712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor W., Jr., Kamanaka M., Booth C.J., Town T., Nakae S., Iwakura Y., Kolls J.K., Flavell R.A. 2009. A protective function for interleukin 17A in T cell-mediated intestinal inflammation. Nat. Immunol. 10:603–609 10.1038/ni.1736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oganesyan G., Saha S.K., Guo B., He J.Q., Shahangian A., Zarnegar B., Perry A., Cheng G. 2006. Critical role of TRAF3 in the Toll-like receptor-dependent and -independent antiviral response. Nature. 439:208–211 10.1038/nature04374 [DOI] [PubMed] [Google Scholar]
- Pandey A.K., Yang Y., Jiang Z., Fortune S.M., Coulombe F., Behr M.A., Fitzgerald K.A., Sassetti C.M., Kelliher M.A. 2009. NOD2, RIP2 and IRF5 play a critical role in the type I interferon response to Mycobacterium tuberculosis. PLoS Pathog. 5:e1000500 10.1371/journal.ppat.1000500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascual V., Chaussabel D., Banchereau J. 2010. A genomic approach to human autoimmune diseases. Annu. Rev. Immunol. 28:535–571 10.1146/annurev-immunol-030409-101221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plumlee C.R., Lee C., Beg A.A., Decker T., Shuman H.A., Schindler C. 2009. Interferons direct an effective innate response to Legionella pneumophila infection. J. Biol. Chem. 284:30058–30066 10.1074/jbc.M109.018283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prchal M., Pilz A., Simma O., Lingnau K., von Gabain A., Strobl B., Müller M., Decker T. 2009. Type I interferons as mediators of immune adjuvants for T- and B cell-dependent acquired immunity. Vaccine. 27:G17–G20 10.1016/j.vaccine.2009.10.016 [DOI] [PubMed] [Google Scholar]
- Prinz M., Schmidt H., Mildner A., Knobeloch K.P., Hanisch U.K., Raasch J., Merkler D., Detje C., Gutcher I., Mages J., et al. 2008. Distinct and nonredundant in vivo functions of IFNAR on myeloid cells limit autoimmunity in the central nervous system. Immunity. 28:675–686 10.1016/j.immuni.2008.03.011 [DOI] [PubMed] [Google Scholar]
- Puccetti P. 2007. On watching the watchers: IDO and type I/II IFN. Eur. J. Immunol. 37:876–879 10.1002/eji.200737184 [DOI] [PubMed] [Google Scholar]
- Qiu H., Fan Y., Joyee A.G., Wang S., Han X., Bai H., Jiao L., Van Rooijen N., Yang X. 2008. Type I IFNs enhance susceptibility to Chlamydia muridarum lung infection by enhancing apoptosis of local macrophages. J. Immunol. 181:2092–2102 [DOI] [PubMed] [Google Scholar]
- Rayamajhi M., Humann J., Penheiter K., Andreasen K., Lenz L.L. 2010. Induction of IFN-alphabeta enables Listeria monocytogenes to suppress macrophage activation by IFN-gamma. J. Exp. Med. 207:327–337 10.1084/jem.20091746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reutterer B., Stockinger S., Pilz A., Soulat D., Kastner R., Westermayer S., Rülicke T., Müller M., Decker T. 2008. Type I IFN are host modulators of strain-specific Listeria monocytogenes virulence. Cell. Microbiol. 10:1116–1129 10.1111/j.1462-5822.2007.01114.x [DOI] [PubMed] [Google Scholar]
- Rizza P., Moretti F., Belardelli F. 2010. Recent advances on the immunomodulatory effects of IFN-alpha: implications for cancer immunotherapy and autoimmunity. Autoimmunity. 43:204–209 10.3109/08916930903510880 [DOI] [PubMed] [Google Scholar]
- Rönnblom L., Alm G.V. 2003. Systemic lupus erythematosus and the type I interferon system. Arthritis Res. Ther. 5:68–75 10.1186/ar625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rönnblom L., Alm G.V., Eloranta M.L. 2009. Type I interferon and lupus. Curr. Opin. Rheumatol. 21:471–477 10.1097/BOR.0b013e32832e089e [DOI] [PubMed] [Google Scholar]
- Rose N.R. 2010. Autoimmunity, infection and adjuvants. Lupus. 19:354–358 10.1177/0961203309360670 [DOI] [PubMed] [Google Scholar]
- Salaun B., Romero P., Lebecque S. 2007. Toll-like receptors’ two-edged sword: when immunity meets apoptosis. Eur. J. Immunol. 37:3311–3318 10.1002/eji.200737744 [DOI] [PubMed] [Google Scholar]
- Shahangian A., Chow E.K., Tian X., Kang J.R., Ghaffari A., Liu S.Y., Belperio J.A., Cheng G., Deng J.C. 2009. Type I IFNs mediate development of postinfluenza bacterial pneumonia in mice. J. Clin. Invest. 119:1910–1920 10.1172/JCI35412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmulevitz M., Pan L.Z., Garant K., Pan D., Lee P.W. 2010. Oncogenic Ras promotes reovirus spread by suppressing IFN-beta production through negative regulation of RIG-I signaling. Cancer Res. 70:4912–4921 10.1158/0008-5472.CAN-09-4676 [DOI] [PubMed] [Google Scholar]
- Stanley S.A., Johndrow J.E., Manzanillo P., Cox J.S. 2007. The Type I IFN response to infection with Mycobacterium tuberculosis requires ESX-1-mediated secretion and contributes to pathogenesis. J. Immunol. 178:3143–3152 [DOI] [PubMed] [Google Scholar]
- Stockinger S., Decker T. 2008. Novel functions of type I interferons revealed by infection studies with Listeria monocytogenes. Immunobiology. 213:889–897 10.1016/j.imbio.2008.07.020 [DOI] [PubMed] [Google Scholar]
- Swann J.B., Hayakawa Y., Zerafa N., Sheehan K.C., Scott B., Schreiber R.D., Hertzog P., Smyth M.J. 2007. Type I IFN contributes to NK cell homeostasis, activation, and antitumor function. J. Immunol. 178:7540–7549 [DOI] [PubMed] [Google Scholar]
- Tailor P., Tamura T., Kong H.J., Kubota T., Kubota M., Borghi P., Gabriele L., Ozato K. 2007. The feedback phase of type I interferon induction in dendritic cells requires interferon regulatory factor 8. Immunity. 27:228–239 10.1016/j.immuni.2007.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takaoka A., Mitani Y., Suemori H., Sato M., Yokochi T., Noguchi S., Tanaka N., Taniguchi T. 2000. Cross talk between interferon-gamma and -alpha/beta signaling components in caveolar membrane domains. Science. 288:2357–2360 10.1126/science.288.5475.2357 [DOI] [PubMed] [Google Scholar]
- Taniguchi T., Takaoka A. 2001. A weak signal for strong responses: interferon-alpha/beta revisited. Nat. Rev. Mol. Cell Biol. 2:378–386 10.1038/35073080 [DOI] [PubMed] [Google Scholar]
- Triantafyllopoulou A., Franzke C.W., Seshan S.V., Perino G., Kalliolias G.D., Ramanujam M., van Rooijen N., Davidson A., Ivashkiv L.B. 2010. Proliferative lesions and metalloproteinase activity in murine lupus nephritis mediated by type I interferons and macrophages. Proc. Natl. Acad. Sci. USA. 107:3012–3017 10.1073/pnas.0914902107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinchieri G., Santoli D. 1978. Anti-viral activity induced by culturing lymphocytes with tumor-derived or virus-transformed cells. Enhancement of human natural killer cell activity by interferon and antagonistic inhibition of susceptibility of target cells to lysis. J. Exp. Med. 147:1314–1333 10.1084/jem.147.5.1314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinchieri G., Santoli D., Dee R.R., Knowles B.B. 1978. Anti-viral activity induced by culturing lymphocytes with tumor-derived or virus-transformed cells. Identification of the anti-viral activity as interferon and characterization of the human effector lymphocyte subpopulation. J. Exp. Med. 147:1299–1313 10.1084/jem.147.5.1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzé G., Monneron D. 2007. IL-28 and IL-29: newcomers to the interferon family. Biochimie. 89:729–734 10.1016/j.biochi.2007.01.008 [DOI] [PubMed] [Google Scholar]
- van Boxel-Dezaire A.H., Rani M.R., Stark G.R. 2006. Complex modulation of cell type-specific signaling in response to type I interferons. Immunity. 25:361–372 10.1016/j.immuni.2006.08.014 [DOI] [PubMed] [Google Scholar]
- Watanabe T., Asano N., Fichtner-Feigl S., Gorelick P.L., Tsuji Y., Matsumoto Y., Chiba T., Fuss I.J., Kitani A., Strober W. 2010. NOD1 contributes to mouse host defense against Helicobacter pylori via induction of type I IFN and activation of the ISGF3 signaling pathway. J. Clin. Invest. 120:1645–1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weighardt H., Kaiser-Moore S., Schlautkötter S., Rossmann-Bloeck T., Schleicher U., Bogdan C., Holzmann B. 2006. Type I IFN modulates host defense and late hyperinflammation in septic peritonitis. J. Immunol. 177:5623–5630 [DOI] [PubMed] [Google Scholar]
- Wenzel J., Tüting T. 2008. An IFN-associated cytotoxic cellular immune response against viral, self-, or tumor antigens is a common pathogenetic feature in “interface dermatitis”. J. Invest. Dermatol. 128:2392–2402 10.1038/jid.2008.96 [DOI] [PubMed] [Google Scholar]
- Yarilina A., DiCarlo E., Ivashkiv L.B. 2007. Suppression of the effector phase of inflammatory arthritis by double-stranded RNA is mediated by type I IFNs. J. Immunol. 178:2204–2211 [DOI] [PubMed] [Google Scholar]
- Yarilina A., Park-Min K.H., Antoniv T., Hu X., Ivashkiv L.B. 2008. TNF activates an IRF1-dependent autocrine loop leading to sustained expression of chemokines and STAT1-dependent type I interferon-response genes. Nat. Immunol. 9:378–387 10.1038/ni1576 [DOI] [PubMed] [Google Scholar]
- Yoshida R., Murray H.W., Nathan C.F. 1988. Agonist and antagonist effects of interferon α and β on activation of human macrophages. Two classes of interferon γ receptors and blockade of the high-affinity sites by interferon α or β. J. Exp. Med. 167:1171–1185 10.1084/jem.167.3.1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young H.A., Bream J.H. 2007. IFN-gamma: recent advances in understanding regulation of expression, biological functions, and clinical applications. Curr. Top. Microbiol. Immunol. 316:97–117 10.1007/978-3-540-71329-6_6 [DOI] [PubMed] [Google Scholar]
- Zhai Y., Qiao B., Gao F., Shen X., Vardanian A., Busuttil R.W., Kupiec-Weglinski J.W. 2008. Type I, but not type II, interferon is critical in liver injury induced after ischemia and reperfusion. Hepatology. 47:199–206 10.1002/hep.21970 [DOI] [PubMed] [Google Scholar]