Abstract
It is unclear how Th2 immunity is induced in response to allergens like house dust mite (HDM). Here, we show that HDM inhalation leads to the TLR4/MyD88-dependent recruitment of IL-4 competent basophils and eosinophils, and of inflammatory DCs to the draining mediastinal nodes. Depletion of basophils only partially reduced Th2 immunity, and depletion of eosinophils had no effect on the Th2 response. Basophils did not take up inhaled antigen, present it to T cells, or express antigen presentation machinery, whereas a population of FceRI+ DCs readily did. Inflammatory DCs were necessary and sufficient for induction of Th2 immunity and features of asthma, whereas basophils were not required. We favor a model whereby DCs initiate and basophils amplify Th2 immunity to HDM allergen.
The induction of adaptive cellular immunity is a function of professional APCs such as DCs, that provide signal 1 (peptide-MHC), signal 2 (costimulatory molecules), and signal 3 (instructive cytokines) to naive T lymphocytes upon antigen encounter (Banchereau and Steinman, 1998). Different subsets of CD4+ T helper cells are then generated to control different types of protective immunity. Th1 cells mediate protection to viruses and intracellular bacteria, whereas Th17 cells help protect against extracellular bacteria and fungi. Th2 cells are crucial for the clearance of parasites, such as helminths, via expansion and activation of innate immune system effector cells like eosinophils and basophils. Although the signals required to drive Th1 and Th17 cell differentiation by DCs are now well characterized, the mechanisms leading to Th2 cell differentiation in vivo are still poorly understood, but in most instances require a source of IL-4 to activate the transcription factors STAT6 and GATA-3, and a source of IL-2, IL-7, or TSLP to activate the transcription factor STAT-5 (Le Gros et al., 1990; Seder et al., 1992; Kopf et al., 1993; Zheng and Flavell, 1997; Paul and Zhu, 2010). Despite the overwhelming evidence that IL-4 is necessary for most Th2 responses, DCs were never found to produce IL-4, and it was therefore assumed that Th2 responses would occur by default, in the absence of strong Th1 or Th17 instructive cytokines in the immunological DC–T cell synapse, or when the strength of the MHCII–TCR interaction or the degree of costimulation offered to naive T cells is weak (Constant et al., 1995; Stumbles et al., 1998; Lambrecht et al., 2000; Jankovic et al., 2004). In this model, naive CD4 T cells were the source of instructive IL-4. In an alternative view, IL-4 is secreted by an accessory innate immune cell type, like NKT cells, eosinophils, mast cells, or basophils, which provide IL-4 in trans to activate the Th2-differentiation program (Ben-Sasson et al., 1990). In the latter model, it was hard to foresee a scenario whereby exceedingly rare antigen-specific naive T cells, DCs, and the innate cell–producing IL-4 could find each other in right the anatomical context of lymphoid organs draining the site of helminth infection. Recently, three groups suggested a solution to this problem, by showing that CD49b+FcεRI+ cKit− basophils can migrate into the LNs draining the site of helminth infection or papain injection, and at the same time act as bona fide APCs by taking up and processing antigen, expressing costimulatory molecules, and secreting IL-4 and/or TSLP for Th2 development (Sokol et al., 2008, 2009; Perrigoue et al., 2009; Yoshimoto et al., 2009). Depletion of basophils using an antibody directed to the high-affinity receptor for IgE (FcεRI) led to strongly reduced Th2 immunity in these models, whereas adoptive transfer of only basophils could induce Th2 polarization in naive antigen-specific T cells, without the necessity of DCs. Strikingly, two of these studies also reported that expression of MHCII molecules exclusively on DCs was not sufficient for induction of Th2 immunity to either papain injection or Trichiurus muris infection, yet Th1 responses were intact (Perrigoue et al., 2009; Sokol et al., 2009).
Th2 lymphocytes are not just important for defense against helminth infection; they are also the predominant cell type responsible for controlling eosinophil-rich inflammation typical of allergic diseases like asthma, allergic rhinitis, and atopic dermatitis. The allergens that are responsible for these diseases are very diverse, yet, like helminth-derived secreted products, often contain protease activity. As only one example, house dust mite (HDM) extract contains cysteine protease allergens (Der p 1 and Der p 9), yet is also “contaminated” by small amounts of endotoxin and fungal products (Chua et al., 1988; Hammad et al., 2009; Nathan et al., 2009; Trompette et al., 2009). Not surprisingly, development of Th2 immunity to inhaled HDM allergen was recently shown to depend in varying degrees on its protease activity, and its potential to induce TLR4 signaling and triggering of C-type lectin receptors on DCs and/or bronchial epithelial cells (Hammad et al., 2001, 2009; Barrett et al., 2009; Nathan et al., 2009; Trompette et al., 2009). From these studies, a model emerged by which bronchial epithelial cells instruct DCs to induce Th2 immunity to inhaled allergens, via the release of innate pro-Th2 cytokines like GM-CSF, TSLP, IL-25, and IL-33 (Hammad and Lambrecht, 2008; Barrett et al., 2009; Lambrecht and Hammad, 2009). Strikingly however, basophils have been largely ignored in the model of Th2 sensitization to inhaled allergens in the lungs, and it is currently unknown if these cells could be equally important for inducing immunity and the pathology of asthma.
Here, we sought to identify the role of basophils in a model of HDM-driven asthma. In view of the recent work identifying basophils as APCs in the skin and gut, we also tested their capabilities to present inhaled antigens in the lung. We found that IL-4–producing basophils were recruited to the mediastinal LN (MLN) upon first HDM exposure in a TLR4, MyD88, and T cell dependent way and contributed to the strength of the Th2 response, yet could not demonstrate antigen presenting capacities or expression of chaperones involved in antigen presentation. Contrary to helminth or papain induced Th2 immunity in the gut or skin (Perrigoue et al., 2009; Sokol et al., 2009; Yoshimoto et al., 2009; Tang et al., 2010), inflammatory dendritic cells were both necessary and sufficient for inducing Th2 immunity to HDM in the lung and for causing the immunopathology of asthma, whereas basophils were not. During the course of our studies, we discovered that depleting antibodies to FcεR1 that were used for depleting basophils (Denzel et al., 2008; Sokol et al., 2008, 2009; Perrigoue et al., 2009; Yoshimoto et al., 2009) also depleted a subset of antigen-presenting inflammatory DCs, whereas the protocols used to generate BM basophils in the presence of IL-3 also promoted expansion of CD11b+ DCs expressing FcεR1 (Yoshimoto et al., 2009). Our studies highlight that conclusions on the relative in vivo contribution of basophils versus dendritic cells as APCs and inducers of Th2 immunity differs from model to model, influenced not only by the route of injection and the type of antigen used, but could also be dependent on the way in which cells are depleted and purified for functional studies.
RESULTS
HDM exposure induces the recruitment of IL-4–competent basophils and eosinophils to the draining LNs
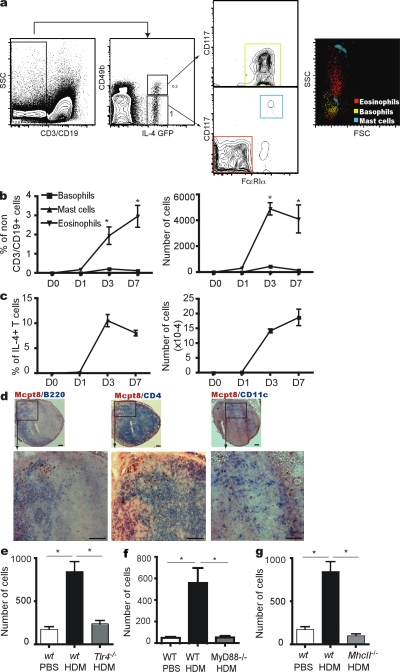
The use of sensitive transgenic IL-4 reporter mice has greatly advanced our understanding of innate type 2 immunity, as eosinophils, mast cells, and basophils were found to have an accessible IL-4 gene locus, thus providing a surrogate marker for identification of these cells in vivo when IL4-enhanced GFP (eGFP) is combined with lineage defining specific antibodies (Mohrs et al., 2001; Min et al., 2004). We therefore examined the appearance of eGFP+ cells in the lung draining MLNs of BALB/c 4get mice (IL-4 GFP-enhanced transcript) that received a single intranasal (i.n.) administration of an extract of the clinically relevant allergen HDM. At 3 d after injection, a population of non-T, non-B (CD3−CD19−) eGFP+ cells was observed in the MLNs of mice injected with HDM, whereas this population was not seen when PBS was injected. When we examined MLN eGFP+ cells more closely, they could be divided further into different populations: DX5(CD49b)+FcεRI+CD117− basophils, DX5−CD117+FcεRI+ mast cells, and DX5+FcεRIloCD117− cells with a FSC and SSC characteristic of eosinophils (Fig. 1 a). Staining with CCR3 antibody or Siglec F antibody confirmed that these cells were indeed eosinophils (unpublished data). We next investigated the kinetics of appearance of these IL-4-eGFP+ cells in the MLN of mice administered i.n. HDM extract. As shown in Fig. 1 b, eosinophils were recruited to the MLNs as early as 1 d after HDM exposure, and this recruitment further increased until 7 d after HDM administration (Fig. 1 b). Very few mast cells were detected in the MLN of mice receiving HDM. Basophil recruitment to the MLN was very transient and peaked at 3 d after allergen administration. However, basophils were no longer detectable in MLNs by day 5 after HDM (Fig. 1 b; see also Fig. 3 b). Interestingly, using the same immunization protocol and same mice for analysis, but gating on CD3+ lymphocytes within the mixed MLN cellular population, Th2 cell differentiation in MLN occurred at day 2 after HDM (unpublished data), and peaked at day 3 (Fig. 1 c). Immunohistochemical analysis of MLNs using an antibody specific for mast cell protease 8 (MCPT8) demonstrated that basophils were recruited to the T cell paracortex of the nodes (Fig. 1 d), excluded from the B cell follicles, and found in close proximity to CD11c+ DCs. Similarly, Siglec F+ eosinophils accumulated in the T cell paracortex (Fig. S1). Recently, we and others have demonstrated that signaling through the TLR4 receptor is crucial for development of Th2 responses to inhaled HDM allergen (Hammad et al., 2009; Phipps et al., 2009; Trompette et al., 2009). To address if TLR4 signaling is also required to recruit basophils to the MLN, we administered HDM to C57BL/6 wt or Tlr4−/− mice. Also in these mice on a C57BL/6 background, lineage−DX5+FcεR1+ basophils were recruited to the MLN 3 d after HDM injection, yet absence of TLR4 profoundly reduced this basophil recruitment (Fig. 1 e). Tang et al. (2010) recently demonstrated that basophil recruitment and Th2 development induced by skin injection of papain relied on generation of reactive oxygen species and oxidized phospholipids that triggered TLR4 and induced a signaling cascade requiring the adaptor molecule TRIF, but not MyD88. However, HDM-driven basophil recruitment to the MLN was dependent on MyD88 signaling (Fig. 1 f).
Figure 1.
HDM exposure induces the recruitment of IL-4-competent basophils and eosinophils to the lung draining LNs. (a) Staining used to identify IL-4–competent cells in MLNs of HDM-administered animals. (b) Kinetics of recruitment of IL-4-EGFP+ basophils, mast cells, and eosinophils to the LNs after HDM administration. (c) IL-4-EGFP+ T cells at different time points after HDM administration. (d) Immunohistological staining of Mcpt8+ basophils (red) and CD4+ T cells, CD11c+ DCs, or B220+ cells (blue) in LNs at D3 after HDM administration. (e) Number of basophils recruited to the LNs of WT or Tlr4−/− mice 3 d after the administration of PBS or HDM. (f) Number of basophils recruited to the LNs of WT or Myd88−/− mice 3 d after the administration of PBS or HDM. (g) Number of basophils recruited to the LNs of WT or MhcII−/− mice 3 d after the administration of PBS or HDM. Data are representative of at least four independent experiments from four to six mice/group. Error bars represent the SEM. *, P < 0.05.
Figure 3.
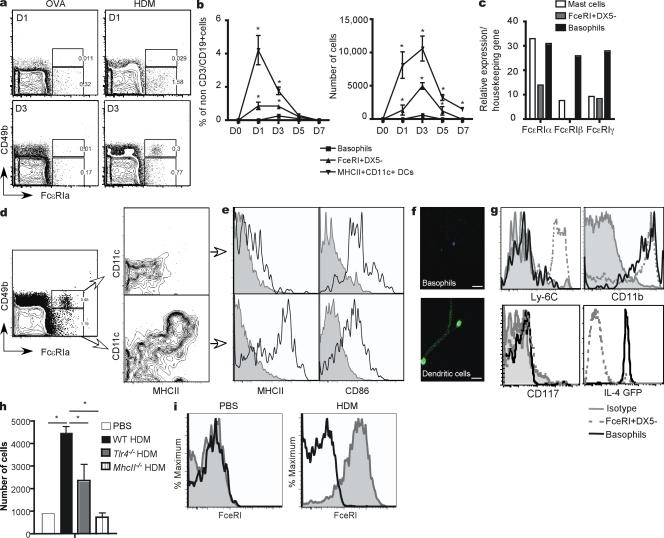
HDM exposure induces the recruitment of FcεRI-expressing monocyte-derived dendritic cells to MLNs. (a) Recruitment of FcεRI+DX5+ basophils and FcεRI+DX5− cells to the lung draining LNs 1 and 3 d after adminstration of OVA or OVA+HDM. (b) Kinetics of recruitment of FcεRI+DX5+ basophils, FcεRI+DX5− cells, and MHCII+CD11c+ DCs to the lung draining LNs after adminstration of HDM. (c) RT-PCR analysis of FcεRIα, β, and γ chain expression in FcεRI+DX5+ basophils and FcεRI+DX5− cells sorted from LNs 3 d after HDM administration, and of peritoneal mast cells of a naive mouse. (d) MHCII and CD11c expression by FcεRI+DX5+ basophils and FcεRI+DX5− cells in the LNs 3 d after the administration of HDM. (e) MHCII and CD86 expression by FcεRI+DX5+ basophils and FcεRI+DX5− cells in the LNs 3 d after the administration of HDM. (f) Immunofluorescence analysis of MHCII expression (green) on FcεRI+DX5+ basophils and FcεRI+DX5− cells sorted from the LNs of HDM-administered animals. Bars, 25 μm. DAPI (blue) was used to counterstain nuclei. Bars, 100 μm. (g) Ly-6C, CD11b, CD117 (c-Kit) and IL-4GFP expression by FcεRI+DX5+ basophils and FcεRI+DX5− cells in the LNs 3 d after the administration of HDM. (h) Number of FcεRI+DX5− cells recruited to the LNs of HDM- or PBS-administered animals. (i) FcεRI expression on lung MHCII+CD11c+ DCs 3 d after the administration of PBS (Left) or HDM (right). Solid black line, isotype-matched control antibody. Data are representative of at least three independent experiments from four to six mice/group. Error bars represent the SEM. *, P < 0.05.
The accumulation of innate type 2 cells during helminth infection has been shown to depend on CD4 T cells that provide a poorly defined signal (not IL-4 or IL-13) for basophil expansion and/or survival (Voehringer et al., 2004; Shen et al., 2008). To address the requirements for CD4 T cells in HDM-mediated basophil recruitment in the lung draining LNs, MhcII−/− mice lacking CD4 T cells were studied (Fig. 1 g). In these mice, there was a severe reduction in the total number of basophils recruited to the MLN compared with wt mice, although on a percentage basis, basophils were still recruited to the node. LNs were however very small in MhcII−/− mice, potentially contributing to reduced basophil recruitment from the bloodstream. Together, these data show that basophils and eosinophils enter the paracortex of lung draining LNs early after inhalation of HDM allergen extract, in a manner requiring TLR4–MyD88 signaling while their numbers are amplified by the presence of CD4 T cells in the nodes.
Contribution of basophils and eosinophils to Th2 immunity to inhaled HDM allergen
IL-4+ basophils were shown to be critical for the initiation of Th2 immunity to papain injected in the footpad of mice (Sokol et al., 2009; Tang et al., 2010). Likewise, eosinophils have been suggested to act as APCs for Th2 immunity in the airways (Shi et al., 2000), and they can produce IL-4 (Mohrs et al., 2001). As inhalation of HDM also induces a strong adaptive Th2 response in the airways (Hammad et al., 2009), and basophils and eosinophils were recruited to the T cell paracortex of the MLN, we next sought to investigate the precise role of these cells in initiating HDM-driven allergic airway inflammation. Basophils were depleted by injecting mice i.v. on day −1 with either depleting moAbs directed against FcεRIα (clone MAR-1; Denzel et al., 2008; Sokol et al., 2009; Tang et al., 2010) or with the basophil-specific depleting Ba103 moAb directed against CD200R3 (Obata et al., 2007). Groups of control mice received matched isotype antibodies. The efficiency of MAR-1 and Ba103 to deplete basophils from MLNs of mice was evaluated at D3 after the i.n. administration of HDM as this was the optimal time point in the recruitment of these cells to the LNs (Fig. 1 b). As cold MAR-1 antibody was used to deplete basophils, we could not use the same fluorochrome-labeled clone for identification of FcεRI+ basophils, and therefore relied on IL-4-eGFP combined with DX5 (CD49b) to check efficiency of depletion in 4-get mice. Compared with mice injected with the isotype control antibodies, the injection of Ba103 or MAR-1 antibodies efficiently depleted IL-4-eGFP+DX5+ basophils from MLNs (94 and 92%, respectively; Fig. 2 a). As this experiment was performed in 4-get mice, we could also study the effect of basophil depletion on CD4 Th2 polarization induced by HDM, by gating on T cells. In mice receiving isotype antibodies, HDM administration increased the percentage of IL-4-eGFP+ T cells to 12.2 ± 2.06–14.7 ± 1.1%, whereas only 0.28 ± 0.09% of T cells had an accessible IL-4 locus in mice administered PBS (Fig. 2 b). Treatment with antibodies to CD200R3 or FcεRI reduced this percentage to 5.44 ± 1.01% and 2.1 ± 0.39%, respectively, in HDM-immunized mice. Treatment with MAR-1 antibody also led to reduced recruitment of IL-4-GFP+ CD49b− eosinophils in the mediastinal nodes at day 3 after HDM (Fig. 2 a).
Figure 2.
Contribution of basophils and eosinophils to Th2 immunity to inhaled HDM allergen. (a) Percentage of basophils in lung draining LNs of HDM-administered animals 3 d after the intravenous injection of anti-CD200R3 antibodies, anti-FcεRI antibodies, or control isotype-matched antibodies. Dot plots (IL4GFP vs CD49b) of lung draining LN cells gated on non– and -B cells. (b) Percentage of IL-4-EGFP+ Th2 cells in lung draining LNs of HDM- or PBS-administered animals 3 d after the intravenous injection of anti-FcεRI antibodies, anti-CD200R3 antibodies, or control isotype-matched antibodies. Dot plots (IL4GFP vs. CD3) of lung draining LN cells gated on CD3+ and lymphocyte scatter characteristics. Number of inflammatory cells in the BAL (c), presence of Siglec F+ eosinophils in the lungs (d), and cytokine production by LN cells of animals sensitized and challenged with HDM, and treated with anti- FcεRI or isotype-matched antibodies (e). (f) Number of inflammatory cells in the BAL, (g) presence of Siglec F+ eosinophils in the lungs, and (h) cytokine production by LN cells of animals sensitized and challenged with HDM, and treated with anti-CD200R3 or isotype-matched antibodies. Number of inflammatory cells in the BAL (i), presence of Siglec F+ eosinophils in the lungs (j), and cytokine production by LN cells of WT or eosinophil-deficient animals sensitized and challenged with HDM (k). Data are representative of at least three independent experiments from six to eight mice/group. Error bars represent the SEM. *, P < 0.05. Bars, 100 μm.
To study if basophil depletion during HDM priming also affected development of allergic eosinophilic lung inflammation upon renewed encounter with allergens, mice were rechallenged with HDM on days 7–11. As reported previously, mice injected with isotype antibodies developed marked eosinophilia and lymphocytosis in the bronchoalveolar lavage (BAL) fluid (Fig. 2, c and f) upon HDM rechallenge and developed inflammatory, eosinophil-rich lesions around the bronchi and the blood vessels in the lung, which is typical of asthma (Fig. 2, d and g). Eosinophilic airway inflammation was associated with substantial Th2 cytokine production by MLN cells restimulated in vitro with HDM (Fig. 2, e and h). Compared with hamster isotype–injected mice, the administration of anti-FcεRI antibodies strongly suppressed airway inflammation as assessed by BAL fluid analysis, tissue infiltration of eosinophils, and levels of Th2 cytokines (Fig. 2, c-e). However, the injection of the CD200R3 basophil-specific antibody Ba103 at the time of sensitization only partially reduced the number of eosinophils in the BAL fluids and in the lungs compared with mice that received isotype rat antibodies (Figs. 2, f and g). Moreover, the administration of CD200R3 antibodies did not induce a significant decrease in the levels of Th2 cytokines, whereas the Th1 cytokine IFN-γ was severely reduced (Fig. 2 H). The precise explanation for this specific reduction in IFN-γ is unclear at present, but could be caused by higher remaining levels of counter-regulatory IL-4 in these mice compared with MAR-1–treated mice. The contribution of eosinophils was studied by immunizing and challenging wt or eosinophil-deficient Gata1ΔDbl (Humbles et al., 2004) mice with HDM. As these mice lack eosinophils altogether (Fig. 2, i and j), we could only assess the degree of Th2 cytokine production in the MLNs after HDM challenge, and found that absence of eosinophils did not affect the strength of the Th2 response, at least in the LN (Fig. 2 k). Strikingly, mice lacking eosinophils also lacked recruitment of lymphocytes to BAL fluid (Fig. 2 i), as previously reported (Lee et al., 2001). Together, these data indicate that FcεRI+ cells contribute to the strength of the initial Th2 response to inhaled HDM, but that Th2 responses are only partially reduced in the absence of basophils, varying considerably depending on the strategy used to deplete basophils.
HDM exposure induces the recruitment of FcεRI-expressing monocyte-derived dendritic cells to MLNs
Although both FcεRI and CD200R3 antibodies depleted basophils equally well (Fig. 2 a), we sought to understand why the effects of FcεRI+ cell depletion on Th2 differentiation and HDM-driven airway inflammation were more pronounced compared with depleting CD200R3 antibody injection. We therefore investigated which cell populations, other than mast cells and basophils, expressed FcεRI in MLNs. Within non–T and –B cells, an additional population of cells expressing FcεRI was found, particularly when HDM, but not the harmless OVA antigen, was administered. This population lacked expression of CD49b (DX5; Fig. 3 A) and was absent from the MLN of mice injected with OVA (or PBS; not depicted). Recruitment of these FcεRI+DX5− cells to the MLN was found to peak between day 1 and 3, and persisted up to 5 d after sensitization with HDM, unlike the kinetics of basophils (Fig. 3 b), which were virtually absent from MLNs by day 5 after HDM administration (Fig. 1 b and Fig. 3 b). Basophils were not detectable at any time point in MLNs of mice injected with OVA alone. Strikingly, eight times more FcεRI+DX5− cells than basophils were recruited to the MLN on day 3 after HDM administration (Fig. 3 b). This difference was even more important when looking at day 1 or 5 after HDM exposure, where the number of basophils in MLNs was 42 times and 38 times less than the number of FcεRI+DX5− cells, respectively. Because DCs (CD11c+MHCIIhi) are known to migrate from the lungs to the MLNs after i.n. HDM exposure (Hammad et al., 2009), we also studied their kinetics of entry into the MLN. As shown in Fig. 3 b, DCs were recruited to the MLNs with a kinetics that was similar to FcεRI+DX5− cells, and the number of DCs recruited to the MLN over time was higher than the number of basophils and FcεRI+DX5− cells. Together, these data clearly show that FcεRI+DX5− cells are specifically recruited in high numbers to the MLNs upon HDM exposure, with a kinetic resembling that of DC recruitment.
In humans, the high-affinity IgE receptor can be expressed as a heterotrimer consisting of the FcεRIα, FcεRIβ, and FcεRIγ chain on basophils and mast cells, but can also consist of a heterodimer consisting of FcεRIα and FcεRIγ, particularly on monocytes and DCs (Maurer et al., 1996, 1998). To identify the type of receptor expressed and test the specificity of FcεRIα antibody for FcεRI+DX5+ cells, the latter population was sorted from MLNs 3 d after HDM sensitization and was analyzed for the expression of the FcεRI α, β and γ chains by RT-PCR. Basophils sorted from MLNs of mice immunized using the same protocol and mast cells sorted from the peritoneal cavity of naive mice were used as a positive control because they express the α, β, and γ chains of the FcεRI receptor (Fig. 3 c). FcεRI+DX5− cells expressed the α and the γ chains of the FcεRI receptor, but did not express the β chain (Fig. 3 c). We wanted to further characterize FcεRI+DX5− cells phenotypically, thus we compared them to FcεRI+DX5+ basophils, as both cell types were recruited to MLNs upon HDM administration (Fig. 3 d). Using nine-color flow cytometry, we first analyzed the expression of MHCII and CD11c on both populations at day 3 after HDM administration. We found that basophils and FcεRI+DX5− cells both expressed MHCII (Fig. 3, d and e), yet the level of expression of MHCII on basophils was much lower than on FcεRI+DX5− cells. Strikingly, at least 75% of FcεRI+DX5− cells highly expressed CD11c and MHCII, which is characteristic of dendritic cells. This high expression of MHCII was confirmed on FcεRI+DX5− cells, but not on basophils, using confocal microscopy (Fig. 3 f). Interestingly, FcεRI+DX5− cells showed a highly dendritic morphology, with a typical nucleus and formed tunneling nanotubules, which are characteristic of DCs. Although basophils only expressed very low levels of MHCII, they were found to express CD86 at levels that were similar to FcεRI+DX5− cells (Fig. 3 e). These data indicate that FcεRI+DX5− cells recruited to the LNs in response to HDM are enriched for MHCII+CD11+ DCs. We have previously shown that HDM allergen challenge leads to rapid recruitment of monocyte-derived CD11b+ DCs to the lungs of mice (Hammad et al., 2009). We analyzed the expression of CD11b and the monocytic marker Ly-6C by FcεRI+DX5− cells and found that they expressed high levels of CD11b and Ly-6C (Fig. 3 g). Basophils were found to express CD11b, but they did not express Ly-6C. FcεRI+DX5− cells lacked expression of CD117 (c-Kit), and only 3% expressed the IL-4GFP reporter. The latter cells could represent basophils that had down-regulated expression of CD49b (DX5). The remaining 20% of non-CD11chi cells within the non–T and –B cell FcεRI+DX5− gate, therefore they consisted primarily of monocytes. These data support the belief that FcεRI+DX5− cells likely differentiate from Ly6C+ monocytes that give rise to inflammatory-type FcεRI+ DCs. Like basophils (Fig. 1, e–g), recruitment of FcεRI+ DCs to the MLN was dependent on TLR4 signaling and grossly reduced in MhcII−/− mice (Fig. 3 h). By gating on MHCIIhiCD11chi nonautofluorescent lung cells, we also observed that lung DCs were universally FcεRI+ in mice exposed to HDM 3 d before, but not those exposed to PBS (Fig. 3 i). Our studies also showed that MAR-1 depletion reduced this population of FcεRI+ DCs significantly (Fig. S2).
FcεRI+ DCs, but not basophils, present antigens to T cells after exposure to HDM and induce Th2 immune responses
We next wanted to characterize FcεRI+ DCs functionally, as it might explain why FcεRI (MAR1) depletion was more effective compared with CD200R3 antibody depletion in reducing type 2 immunity to HDM. First, the antigen uptake capacity of FcεRI+DX5− cells was analyzed and compared with basophils. Mice were injected i.n. on day 0 with fluorescent OVA (OVA-Alexa Fluor 647 [AF647]) mixed with HDM to induce the recruitment of basophils and FcεRI+DX5− cells to the MLN. At day 3, the presence of OVA-AF647 was investigated in basophils and FcεRI+DX5− cells. As shown in Fig. 4 a, 3% of the basophils had signs of OVA uptake, whereas 10% of FcεRI+ DCs had taken up OVA antigen while at the same time expressing MHCII and CD11c. These data indicate that, in the MLNs, FcεRI+DX5− cells are much better than basophils at taking up fluorescent soluble antigen administered via the airways.
Figure 4.
FcεRI+ DCs, but not basophils, present antigens to T cells after exposure to HDM and induce Th2 immune responses. (a) OVA-AF647 uptake by FcεRI+DX5+ basophils (top) and FcεRI+DX5− cells (bottom) in the LNs 3 d after the administration of OVA-AF647 alone or in combination with HDM. (b) OVA-specific naive CD4+ T cell proliferation induced by FcεRI+DX5+ basophils, FcεRI+DX5 cells, or MHCII+CD11c+ DCs sorted from the LNs of OVA+HDM-administered animals 1 or 3 d after antigen exposure. (c) Cytokine production by OVA-specific naive CD4+ T cell restimulated for 4 d with FcεRI+DX5+ basophils, FcεRI+DX5− cells, or MHCII+CD11c+ DCs sorted from the LNs of OVA+HDM-administered animals 3 d after antigen exposure. (d) RT-PCR analysis of MHCII-associated chaperone proteins in FcεRI+DX5+ basophils, FcεRI+DX5− cells, or MHCII+CD11c+ DCs sorted from the LNs 3 d after HDM administration. Data are representative of at least three independent experiments from four to six mice/group.
We compared the capacity of FcεRI+DX5− cells and basophils sorted from MLNs to present antigen to highly purified naive CD4+ T cells ex vivo. Mice were injected i.n with OVA mixed with HDM on day 0. At day 3, FcεRI+DX5− cells and basophils were sorted from MLNs (Fig. 4 b) and were co-cultured for 4 d with highly purified CFSE-labeled OVA-specific CD4+ T cells, obtained from naive DO11.10 T cells. In these experiments, the total fraction of MLN MHCII+CD11c+ DCs (excluding the FcεRI+ cells from the gate) was sorted from the same MLNs and used as a positive control for antigen presentation. T cells stimulated by MHCII+CD11c+ DCs proliferated strongly, as indicated by the strong dilution of CFSE dye (Fig. 4 b). Sorted FcεRI+DX5− cells induced a similarly strong proliferation of T cells that was almost similar to the T cell proliferation induced by MHCII+CD11c+ DCs. Basophils, however, failed to induce any T cell proliferation (Fig. 4 b). When analyzing cytokines present in the co-cultures, T cells co-cultured with FcεRI+DX5− cells produced high levels of the Th2 cytokines IL-13 and IL-10, but also produced some IL-17 and IFN-γ (Fig. 4 c). T cells co-cultured with cDCs produced all of these cytokines, but in a lower amount compared with T cells stimulated by FcεRI+ DCs cells. Basophils did not induce any cytokine production by T cells (Fig. 4 c).
We wanted to understand why basophils were poor APCs in response to HDM allergen. To answer this question, basophils, FcεRI+DX5− cells, and cDCs were sorted from MLNs 3 d after HDM administration and analyzed for the expression of proteins regulating MHCII-restricted antigen presentation (cathepsin S, HLA-DM, and the invariant chain Ii) using RT-PCR. As expected, cDCs expressed high levels of cathepsin S, HLA-DM, and the invariant chain Ii (Fig. 4 d). FcεRI+DX5− also expressed all of these molecules at high levels. However, sorted basophils expressed some mRNA for cathepsin S, but their expression of HLA-DM and of the invariant chain was very low compared with cDCs and FcεRI+DX5− cells.
Dendritic cells are necessary and sufficient for Th2 responses to HDM allergen
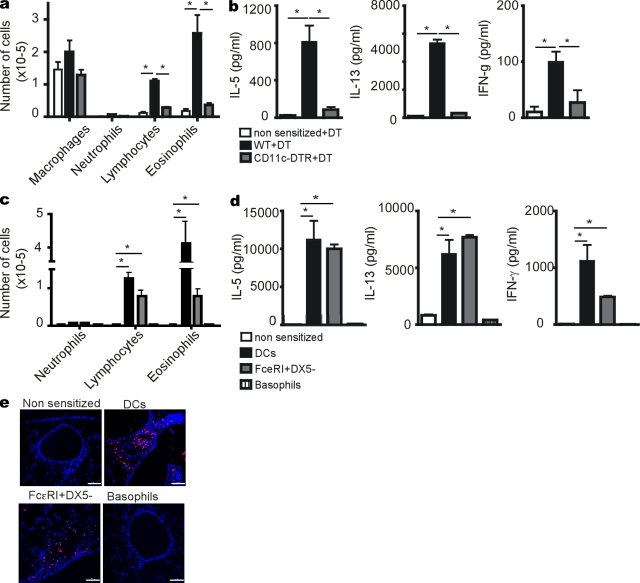
It has been previously reported that the Th2 response to papain injected into the skin was mediated by basophils only, although recent work from another group suggested collaboration between DCs and basophils in a similar model (Sokol et al., 2009; Tang et al., 2010). We next sought to investigate the contribution of DCs to the initiation of inhaled HDM-induced Th2 responses. To achieve this goal, we made use of CD11c-DTR Tg mice in which depletion of CD11chi DCs can be achieved by the administration of diphteria toxin (DT; Jung et al., 2002). CD11c-DTR and WT littermate mice received an i.p. injection of DT and were sensitized i.n. with HDM on day 0. All mice were reexposed to HDM i.n. on days 7–11. On day 14, the degree of eosinophilia and Th2 cytokine production by MLN cells were evaluated. As expected, WT littermates injected with DT and sensitized to HDM developed a strong eosinophilia and lymphocytosis in the BAL fluids (Fig. 5 a), a strong Th2 cytokine production (IL-5 and IL-13), and a low production of the Th1 cytokine IFN-γ by MLN cells restimulated with HDM (Fig. 5 B). This response was not seen in nonsensitized mice challenged with HDM. Injection of CD11c-DTR mice with DT at the time of HDM sensitization prevented the development of eosinophilia and lymphocytosis in the BAL fluids, and this was associated with a substantial decrease in the levels of Th1 and Th2 cytokines by MLN cells. Together, these data indicate that CD11c+ DCs are necessary for the initiation of Th2 responses to HDM allergen.
Figure 5.
Dendritic cells are necessary and sufficient for Th2 responses to HDM allergen. (a) Number of inflammatory cells in the BAL and (b) cytokine production by LN cells of WT or CD11c-DTR animals sensitized and challenged with HDM and treated with DT on day 0. (c) Number of inflammatory cells in the BAL, and (d) Cytokine production by LN cells of animals injected on day 0 i.p with basophils, FcεRI+DX5− cells or MHCII+CD11c+ DCs sorted from the lung draining LNs 1 d after HDM administration. Mice were then challenged with HDM on days 7–11. (e) Immunofluorescence staining of Siglec F+ eosinophils (red) in the lungs. DAPI (blue) was used to counterstain nuclei. Data are representative of at least two independent experiments from four to six mice/group. Error bars represent the SEM. *, P < 0.05. Bars, 100 μm.
We next wanted to address whether lung DCs were sufficient to induce Th2 sensitization to HDM, and if FcεRI+ DCs in particular would be able to induce Th2 immunity. Naive mice were injected i.p. on day 0 with either FcεRI+DX5− cells or cDCs sorted from MLNs of animals that received HDM 3 d earlier. Control mice were not sensitized, but just received a PBS injection. On days 7–11, all mice were challenged with HDM. Mice injected with as few as 3 × 104 MLN DCs obtained form HDM-exposed mice developed a strong eosinophilia and lymphocytosis in the BAL fluids and in the lungs (Fig. 5, c and e), and showed elevated levels of Th2 cytokines by MLN cells (Fig. 5 d) compared with nonsensitized animals. Mice injected with 3 × 104 FcεRI+DX5− cells (containing ∼75% CD11chi DCs) also had an increased number of eosinophils and lymphocytes in BAL fluids and lung tissue (Fig. 5, c and e) compared with control mice. In as similar setup, transfer of 3 × 104 basophils did not induce Th2 immunity to HDM allergen. These data show that MHCIICD11c+ DCs and FcεRI+DX5− cells are sufficient to induce Th2 sensitization to HDM allergen.
Induction of Th2 immunity is a feature of FcεRI+ inflammatory type DCs, not conventional steady-state DCs
Recent work has suggested that DCs cannot induce Th2 immune responses to simple protein or protease antigens or the complex helminth Trichuris (Perrigoue et al., 2009; Sokol et al., 2009; Yoshimoto et al., 2009). Yet our current work and many previously published studies have shown induction of Th2 immunity by DCs in vitro and in vivo (Lambrecht et al., 2000; Eisenbarth et al., 2002; MacDonald et al., 2002; van Rijt et al., 2005). After careful analysis of the papers, we noticed that all groups disputing Th2 induction by DCs were using conventional resident DCs obtained from the LNs or spleen of animals in steady state, which are not the same as migratory inflammatory type DCs (Perrigoue et al., 2009; Sokol et al., 2009; Yoshimoto et al., 2009). To address the relative potential of inflammatory versus conventional steady-state DCs, we used a BM culture system using GM-CSF to generate inflammatory DCs or Fms-like tyrosine kinase (Flt3L) to generate steady-state cDCs (Shortman and Naik, 2007; Xu et al., 2007). These cells were pulsed with OVA antigen and instilled intratracheally, followed by OVA aerosol challenge on days 10–12, as previously described (Lambrecht et al., 2000). Only GM-CSF–cultured DCs, but not Flt3L-cultured cDCs, were able to induce airway eosinophilia, which is typical of a Th2 response (Fig. 6 a) supported by induction of Th2 cytokines in the MLNs (not depicted). Strikingly, only GM-CSF–cultured inflammatory DCs, but not Flt3L-cultured cDCs, expressed FcεRI (Fig. 6 b). When Flt3L cultures were studied more carefully, FcεRI expression was not detected on CD24+ (CD8α+ equivalent) cDCs, CD24− cDCs (CD8α− equivalent), or 120G8+ pDCs (Naik et al., 2005). Long-term culture of BM cells to generate basophils and mast cells in IL-3 also generated MHCII+CD11c+ DCs that expressed levels of FcεRI comparable to mast cells and basophils (Fig. 6 c). We finally studied if FcεRI was also induced on monocytes, as these cells are recruited to the lungs upon HDM challenge and rapidly differentiate to become DCs (Hammad et al., 2009). Therefore, we incubated Ly6Chi CD11b+ sorted BM monocytes with cytokines known to affect DC differentiation and/or FcεRI expression on other cell types. When grown in GM-CSF or IL-3, monocytes rapidly up-regulated the FcεRI receptor and up-regulated expression of MHCII and CD11c, illustrating differentiation to monocyte-derived inflammatory DCs (Fig. 6 d). IL-3 was particularly strong in inducing FcεRI on monocytes without inducing DC differentiation. TSLP, stem cell factor), IL-1, or combinations thereof with GM-CSF, and IL-3 did not further enhance FcεRI expression (unpublished data).
Figure 6.
Induction of Th2 immunity is a feature of FcεRI+ inflammatory type DCs. (a) Number of inflammatory cells in the BAL of mice sensitized by an intratracheal administration of DCs generated from BM cultured in the presence of GM-CSF or Flt3-liter. (b) FcεRI expression on DC subsets generated from BM cultured in the presence of GM-CSF or Flt3-liter. (c) Staining of FcεRI, CD49b, MHCII, and CD11c on BM cells cultured for 10 d with 30 ng/ml IL-3. (d) FcεRI expression on sorted monocytes after 1 or 3 d of culture with GM-CSF or IL-3. Data are representative of at least four independent experiments from four to eight mice/group. Error bars represent the SEM. *, P < 0.05.
DISCUSSION
Basophils have gained renewed interest as inducers and amplifiers of Th2 immunity through their potential to migrate to LNs, provide an early source of IL-4, and at the same time act as APCs in models of helminth infection and injection of the model protease papain, but have been largely ignored in the field of pulmonary mucosal immunity and development of allergic asthma to inhaled allergens (Sokol et al., 2008, 2009). Here, we found that basophils are recruited to the MLNs draining the site of i.n. administration of HDM allergen within 3 d of HDM injection. Several mechanisms could explain this increase. Like basophil expansion and recruitment to sites of helminth infection (Voehringer et al., 2006), we found that this process required adaptive immunity and CD4 T cells, as MHCII-deficient mice had severely reduced recruitment of basophils. The most likely explanation is T cell–derived production of IL-3 (Shen et al., 2008; Kim et al., 2010), which we found to be induced in CD4 T cells upon intranasal HDM administration (unpublished data). Strikingly, accumulation of basophils in the MLN also required innate immunity and triggering of the TLR4 receptor via the MyD88 pathway. Tang et al. (2010) recently suggested that protease allergens like papain injected into the skin of mice leads to basophil recruitment in a process requiring production of reactive oxygen species that lead to formation of oxidized lipids that then trigger the TLR4 pathway. Although we did not measure the induction of these oxidized lipids, we do not believe that HDM triggering of this pathway is essential, as we observed a dependence on the MyD88 adaptor. The pathway of oxidized phospholipid triggering of TLR4 was found to be TRIF dependent, but not MyD88 dependent yet (Imai et al., 2008; Tang et al., 2010). We and others have recently shown that TLR4 triggering and C-type lectin triggering on epithelial cells is crucial for mounting an innate cytokine response to HDM, consisting of production of GM-CSF, TSLP, IL-25, and IL-33 and production of chemokines like CCL2 and CCL20 (Hammad et al., 2009; Nathan et al., 2009; Trompette et al., 2009). Although we did not elucidate the effect of each individual cytokine on the recruitment or expansion of basophils in the MLN, the effects of Myd88 deficiency on basophil recruitment were more pronounced than those in TLR4-deficient mice. This could be explained by the fact that Myd88 is also involved in signaling via the IL-33R (T1/ST2) and that IL-33 is a known expansion factor for basophils in vivo (Schneider et al., 2009). Along the same lines, GM-CSF can greatly facilitate basophil expansion initiated by IL-3 (Schneider et al., 2009).
The precise source for IL-4 driving adaptive Th2 responses has been a matter of great debate (Paul and Zhu, 2010). In one line of thought, innate cells like basophils, mast cells, eosinophils or NKT cells provide a source of IL-4 in trans to activate the Th2 polarization driven by DCs in draining LNs, whereas in another view, naive T cells can themselves provide the source of IL-4 for further enforcement of their lineage. We found that after HDM exposure, IL-4–competent eosinophils outnumbered IL-4 competent basophils in the T cell area of the MLN, and reached that node with faster kinetics. Mast cells did not accumulate in the MLN. When basophils were depleted during HDM sensitization using antibodies to FcεRI or CD200R3, we observed a reduction in the strength of naive CD4 T cell polarization, as well as an abolition of development of allergic airway inflammation and Th2 cytokines upon rechallenge of the mice, particularly when antibodies to FcεRI were used. Genetic elimination of eosinophils using gata1Δdbl mice did not affect the strength of the Th2 response, despite the fact that eosinophils were found in close proximity to DCs in the T cell area of the MLN. One explanation would be that the eosinophils only have a competent open IL-4 locus, but do not secrete IL-4 in the T cell paracortex (Mohrs et al., 2005).
Despite recent reports that basophils can act as APCs for helminth antigens or skin-injected papain, we did not find a role for these cells as APCs for inhaled HDM allergen. First, basophils that accumulated in the MLN were barely positive for a coadministered fluorescent OVA protein, suggesting they were poor in taking up inhaled antigen. Second, when put into culture with naive OVA-specific T cells, basophils did not induce T cell divisions or induce generation of effector cytokines, Third, when administered intratracheally, they did not induce sensitization to HDM allergen. Finally, although basophils expressed levels of CD86 comparable to DCs, they did not express high levels of MHCII or of the HLA-DM chaperone molecule that is crucial for exchange of immunogenic peptides in nascent MHCII complexes (Roche, 1995), nor did they express high levels of the invariant chain that is crucial for routing and transport of MHCII molecules inside APCs (Elliott et al., 1994). Although poor survival of transferred basophils might be an explanation for part of these findings, the total dataset does not support a role for basophils as APCs in HDM-driven Th2 development. Why then, did others find antigen-presenting capacities in these cell types? One possibility is that the experimental models are fundamentally different, with different forms of antigen involved, and a different route of administration. Papain is a pure antigen with cysteine protease activity that could lead to up-regulation of MHCII on basophils, and is mainly reaching the LNs via afferent lymph in the absence of DC-mediated presentation (Sokol et al., 2009). Others have used IgE antibodies to target OVA antigen to basophils, a model that is more appropriate to study the role of these cells in secondary immune responses (Yoshimoto et al., 2009). Although HDM also contains cysteine protease activity, it is a much more complex antigen that can trigger activation of innate immune cells and epithelial cells in many different ways, including triggering of TLR and C-type lectin receptors.
Another explanation for the discrepancies between the models reported is in the way that basophils were purified or depleted for functional studies on antigen presentation. During the course of our studies, we found that FcεRI is also expressed on monocyte-derived, inflammatory-type DCs induced by GM-CSF and/or IL-3, and was depleted by treatment with the MAR-1 antibody. In our functional studies, we took great care to avoid including these cells in the antigen presentation assays, as they were able to induce Th2-type immunity in vitro in the absence of help from basophils. Although we did not check whether a similar population of FcεRI+ DCs exists in models of helminth infection or after papain injection, a note of caution is in place. Protocols using IL-3 to grow basophils from the BM followed by purification of FcεRI+ cells (Yoshimoto et al., 2009) or using DX5 beads (Sokol et al., 2009) still lead to contaminating FcεRI+CD11c+MHCII+DCs (sometimes as much as 10% of the cells). It has long been known that IL-3 can be used almost as efficiently as GM-CSF to generate DCs from BM cultures in mouse or from monocytes in humans (Ebner et al., 2002; Baumeister et al., 2003). If cells purified in this way are used in antigen-presenting assays, or used for adoptive transfer studies in vivo, then presentation might be caused by even a small percentage of contaminating DCs within the range of acceptable purity for bead-purified cells, particularly if 20 × 107 basophils are injected in vivo, given the strength of DCs as APCs (Sokol et al., 2009). We believe that this is also why, in our experiments, a strategy using basophil depletion using MAR1 to deplete FcεRI+ basophils is more potent in suppressing Th2 induction by HDM than use of the basophil-specific antibody Ba103 against CD200R3, as a subset of DCs potently inducing Th2 responses is additionally depleted.
In searching for an explanation of why other groups have failed to demonstrate MAR-1 staining on DCs, we observed that expression was measured on conventional DCs obtained from the central lymphoid organs of animals in steady-state (Denzel et al., 2008). There is, however, precedent for MAR-1 reactivity on DCs in the mouse, when staining was measured on DCs obtained from the lungs of Sendai virus–infected mice but not healthy control mice (Grayson et al., 2007). In this study, type I IFN was shown to induce the receptor on lung cDCs. In our study, only DCs grown in GM-CSF, a model to generate inflammatory DCs (Xu et al., 2007) expressed MAR-1, whereas the CD24+ and CD24− equivalents of CD8α+ and CD8α− steady-state conventional DCs or pDCs grown in Flt3L (Naik et al., 2007) did not express FcεRI. Strikingly, we found that GM-CSF or IL-3 lead to rapid up-regulation of MAR-1 staining on sorted Ly6Chi monocytes, which can rapidly become inflammatory DCs in the mouse (Kool et al., 2008).
The recent papers that highlighted the importance of basophils as APCs also demonstrated that in the systems used, DCs were neither necessary nor sufficient for induction of Th2 immunity, although this has recently been slightly modified (Perrigoue et al., 2009; Sokol et al., 2009; Tang et al., 2010). In the model of HDM sensitization however, depletion of CD11c+ DCs using the same type of CD11cDTR mice lead to strongly reduced Th2 responses to HDM and to reduced eosinophil airway inflammation upon rechallenge of the mice. In addition, adoptive transfer of as few as 3 × 104 lung-derived FcεRI+ DCs or MHCII+CD11c+ DCs obtained from HDM exposed mice to naive mice induced Th2 immunity to HDM and to features of asthma upon rechallenge. This adoptive intratracheal transfer model relies only on antigen presentation of injected cells, and not on carry-over and presentation by endogenous APCs that could bias conclusions (Kuipers et al., 2009). Again, many explanations exist as to why we find a crucial dependence on DCs, whereas others have not. The inhalation of HDM antigen is fundamentally different from skin injection of papain or the gastrointestinal tract infection of a large parasite, as the HDM antigen needs to cross the natural mucosal barrier formed by epithelial tight junctions, possibly relying more on antigen uptake by airway DCs (Vermaelen et al., 2001; Jakubzick et al., 2008). Although this report is the first one demonstrating that depletion of DCs abolishes Th2 priming to inhaled HDM antigen, we have previously demonstrated that DCs are also crucial for mounting a secondary Th2 immune response to inhaled OVA antigen (Lambrecht et al., 1998; van Rijt et al., 2005). It is also in line with many published papers that posit that intratracheal injection of inflammatory type DCs, but not steady-state conventional DCs (Fig. 6) or pDCs, leads to Th2 immunity to inhaled OVA antigen (Lambrecht et al., 2000; Sung et al., 2001; de Heer et al., 2004; Piggott et al., 2005; Matsubara et al., 2006; Krishnamoorthy et al., 2008). We did not use the mice in which MHCII expression is restricted to CD11chi cells (Perrigoue et al., 2009; Sokol et al., 2009), because MHCII expression is not fully restored on migratory DCs (Allenspach et al., 2008), as this might bias our readout of antigen presentation that is strictly dependent on migratory DCs of the lung (Vermaelen et al., 2001).
In conclusion, our data demonstrate that inflammatory DCs, but not basophils, are necessary and sufficient APCs for development of Th2 immunity to HDM allergen when it is first introduced via the natural inhaled route. We favor a model in which basophils amplify Th2 immunity to HDM, initiated by DCs and instructed by innate signaling through TLR4 and Myd88 signaling and C-type lectin signaling on epithelial cells and dendritic cells (Hammad et al., 2009; Nathan et al., 2009; Trompette et al., 2009). Putting basophils in this equation will likely help to better understand the origins of allergic sensitization.
MATERIALS AND METHODS
Mice.
4-get mice (Mohrs et al., 2001) were obtained from Jackson ImmunoResearch Laboratories and bred at the animal facility of the University of Ghent. BALB/c mice were obtained from Harlan. Cd11c-DTR (Jung et al., 2002) and DO11.10 OVA-TCR Tg mice (Murphy et al., 1990; BALB/c background), and Tlr4−/−, Myd88−/−, and MHCII−/− (C57BL/6 background) were bred and maintained at the animal facility of the University of Ghent, and mice were provided by S. Akira (Osaka University, Osaka, Japan). Experiments were approved by the animal ethical committee of the University of Ghent.
Immunization and depletion.
Mice were anaesthetized with isoflurane and immunized i.n. with 100 µg HDM extracts (Greer Laboratories) contained in 40 µl of PBS. In some experiments, HDM was admixed or not to 100 µg OVA (Worthington).
To induce allergic airway inflammation, mice were sensitized i.n. with 100 µg HDM extracts (Greer Laboratories) on day 0, were subsequently challenged with 10 µg HDM i.n. on days 7–11. On day 14, lungs were collected and frozen at −80°C for immunofluorescence staining. BAL was performed with 3× 1 ml of PBS containing EDTA. MLNs were homogenized and cells were plated at a density of 200,000 cells/well. Cells were restimulated for 4 d with 30 µg HDM extracts. Cytokine production was measured by specific ELISA (Invitrogen).
To test the capacities of cDCs and FcεRI+DX5− cells to induce Th2 sensitization, these cells were sorted from MLNs of BALB/c mice 3 d after the i.n. administration of 100 µg HDM extracts. 30,000 cells were administered i.p into BALB/c mice on day 0, and all mice were challenged with 10 µg HDM on days 7–11. On day 14, features of allergic airway inflammation were analyzed.
To deplete DCs, CD11c-DTR transgenic mice were injected i.p on day 0 with 200 ng of DT (Sigma-Aldrich). To deplete FcεRI+ cells, mice were injected i.v with 100 µg anti-FcεRIα (MAR-1) on day 0. To specifically deplete basophils, mice were injected i.v with 30 µg CD200R3 (Ba103) antibody on Day 0 (HyCult)
Flow cytometry and cell sorting.
Cells were incubated for 20 min on ice with the appropriate antibodies. To stain and/or sort FcεRI+ cells, basophils, and cDCs, MLN cells were stained with Alexa Fluor 700–labeled anti-CD3 and anti-CD19 (eBioscience) and biotinylated anti-FcεRIa (MAR-1; eBioscience), followed by streptavidin Pe-Cy5, PE-Cy7-labeled CD49b (eBioscience), APC-AF750–labeled CD117 (eBioscience), Vhorizon450-labeled anti-CD11b (BD), PE-texas red–labeled anti-CD11c (Invitrogen), APC-labeled anti-MHCII (eBioscience), and PE-labeled anti-CD86 antibodies (BD). Dead cells were excluded using Aqua live/dead fixable dye (Invitrogen).
To determine the cellular composition of BAL fluids, cells were stained with MHCII-FITC (2G9; for DC and macrophage staining), CD11c-APC (HL3; for DC staining), CD19-CyChr (RA3-6B2) and CD3-CyChr (145-2C11; BD), and Siglec F-PE (R&D Systems; for eosinophil staining). 2.4.G2 was used to prevent nonspecific binding. The cellular composition of BALF cells was determined using flow cytometry, as described previously (van Rijt et al., 2004).
Cells were acquired on a LSRII flow cytometer (BD) and FlowJo software (Tree Star, Inc.). Cells were sorted on a FACSAria II flow cytometer (BD).
Culture of BM DCs and basophils.
To generate inflammatory DCs, BM cells were obtained from femurs of mice, red blood cells were lysed, and cells were incubated in cell culture medium containing 20 ng/ml GM-CSF, and then harvested 10 d later, essentially as previously described (Lambrecht et al., 2000). To generate conventional DCs, BM cells were incubated with Flt3L, and cells were harvested at day 10, as previously described (Naik et al., 2005). In experiments where DCs were transferred in vivo, they were first pulsed overnight with 100 µg/ml OVA protein (Worthington)
To generate basophils, BM cells were grown in 30 ng/ml IL-3 for 10 d (Lantz et al., 1998). In separate experiments, BM monocytes were sorted from the BM of naive mice, based on expression of Ly6C and CD11b, and cultured for 1–3 d in 20 ng/ml GM-CSF, 30 ng/mlIL-3 g/ml, 30 ng/ml TSLP, or 20 ng/ml IL-1β.
Antigen presentation to T cells in vitro.
CD4+ T cells were isolated from spleen by magnetic-activated cell sorting (purity >98%), labeled with CFSE (Invitrogen), and plated at a density of 300,000 cells/ml in the presence of basophils, FcεRI+DX5− cells, or cDCs sorted from MLNs of mice injected with OVA and HDM (5 T cells:1 DC ratio). After 4 d, cells were harvested and OVA-specific T cell proliferation was determined by staining cells with PE-labeled KJ1-26, APC-labeled anti-CD4, and APC-Cy7–labeled anti-CD3 antibodies.
Immunofluorescence.
Cytospins of sorted basophils and FcεRI+DX5− cells were prepared. Slides were fixed in 4% PFA for 10 min at room temperature and stained with FITC-labeled anti-MHCII antibodies for 30 min at room temperature. To stain eosinophils, lung sections were incubated for 1 h at room temperature with anti–Siglec F antibodies, followed by Cy-3–labeled donkey anti–rat antibodies (Jackson ImmunoResearch Laboratories). Nuclei were counterstained with DAPI. Slides were analyzed on a LSM710 microscope (Carl Zeiss, Inc.) equipped with a 488-nm laser and a tunable Mai-Tai DeepSee multiphoton laser (Coherent). MCPT8 antibodies were provided by H. Karasyama (Tokyo Medical and Dental University Graduate School, Tokyo, Japan).
RT-PCR.
Frozen pellets of sorted cells were frozen and RNA was isolated using RNeasy miniprep (QIAGEN) with on column DNase treatment according to the manufacturer’s protocol. 100 ng RNA was reverse transcribed using random hexamers and superscript II (Invitrogen) for 50 min at 42°C. Quantitative PCR was performed using Taqman Universal PCR Master Mix (Applied Biosystems) and predesigned primers and probe mixes (Assay on Demand; Applied Biosystems). PCR conditions were 2 min at 50°C and 10 min at 95°C, followed by 40 cycles of 15 s at 95°C and 60°C for 1 min using ABI PRISM 7000 (Applied Biosystems). PCR amplification of the housekeeping gene ubiquitin C was performed during each run for each sample to allow normalization between samples.
Online supplemental material.
Fig. S1 depicts a staining for eosinophils in the MLNs of mice that received an i.n. injection of HDM 3 d earlier. Fig. S2 depicts the effect of treatment with antibodies on the percentage of FcεRI+DX5− cells in the MLN. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20101563/DC1.
Acknowledgments
Bart N. Lambrecht and Hamida Hammad were supported by an Odysseus Grant of the Flemish government and by a concerted research initiative grant (GOA 01G01009), a 4 year project grant, and a Multidisciplinary Research Initiative Grant of University of Ghent and a National Institutes of Health R21 grant. Maud Plantinga was supported by a grant of Ghent University. Mirjam Kool was supported by an EU Marie Curie Intra-european Fellowship and Philippe Pouliot was supported by a EU Marie Curie International Incoming Fellowship.
The authors have no conflicting financial interests.
Footnotes
Abbreviations used:
- AF647
- Alexa Fluor 647
- BAL
- bronchoalveolar lavage
- DT
- diphteria toxin
- Flt3L
- Fms-like tyrosine kinase
- eGFP
- enhanced GFP
- HDM
- house dust mite
- i.n.
- intranasal
- MLN
- mediastinal LN
References
- Allenspach E.J., Lemos M.P., Porrett P.M., Turka L.A., Laufer T.M. 2008. Migratory and lymphoid-resident dendritic cells cooperate to efficiently prime naive CD4 T cells. Immunity. 29:795–806 10.1016/j.immuni.2008.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banchereau J., Steinman R.M. 1998. Dendritic cells and the control of immunity. Nature. 392:245–252 10.1038/32588 [DOI] [PubMed] [Google Scholar]
- Barrett N.A., Austen K.F. 2009. Innate cells and T helper 2 cell immunity in airway inflammation. Immunity. 31:425–437 10.1016/j.immuni.2009.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett N.A., Maekawa A., Rahman O.M., Austen K.F., Kanaoka Y. 2009. Dectin-2 recognition of house dust mite triggers cysteinyl leukotriene generation by dendritic cells. J. Immunol. 182:1119–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister T., Rössner S., Pech G., de Bruijn M.F., Leenen P.J., Schuler G., Lutz M.B. 2003. Interleukin-3Ralpha+ myeloid dendritic cells and mast cells develop simultaneously from different bone marrow precursors in cultures with interleukin-3. J. Invest. Dermatol. 121:280–288 10.1046/j.1523-1747.2003.12380.x [DOI] [PubMed] [Google Scholar]
- Ben-Sasson S.Z., Le Gros G., Conrad D.H., Finkelman F.D., Paul W.E. 1990. Cross-linking Fc receptors stimulate splenic non-B, non-T cells to secrete interleukin 4 and other lymphokines. Proc. Natl. Acad. Sci. USA. 87:1421–1425 10.1073/pnas.87.4.1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua K.Y., Stewart G.A., Thomas W.R., Simpson R.J., Dilworth R.J., Plozza T.M., Turner K.J. 1988. Sequence analysis of cDNA coding for a major house dust mite allergen, Der p 1. Homology with cysteine proteases. J. Exp. Med. 167:175–182 10.1084/jem.167.1.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constant S., Pfeiffer C., Woodard A., Pasqualini T., Bottomly K. 1995. Extent of T cell receptor ligation can determine the functional differentiation of naive CD4+ T cells. J. Exp. Med. 182:1591–1596 10.1084/jem.182.5.1591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Heer H.J., Hammad H., Soullié T., Hijdra D., Vos N., Willart M.A., Hoogsteden H.C., Lambrecht B.N. 2004. Essential role of lung plasmacytoid dendritic cells in preventing asthmatic reactions to harmless inhaled antigen. J. Exp. Med. 200:89–98 10.1084/jem.20040035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denzel A., Maus U.A., Rodriguez Gomez M., Moll C., Niedermeier M., Winter C., Maus R., Hollingshead S., Briles D.E., Kunz-Schughart L.A., et al. 2008. Basophils enhance immunological memory responses. Nat. Immunol. 9:733–742 10.1038/ni.1621 [DOI] [PubMed] [Google Scholar]
- Ebner S., Hofer S., Nguyen V.A., Fürhapter C., Herold M., Fritsch P., Heufler C., Romani N. 2002. A novel role for IL-3: human monocytes cultured in the presence of IL-3 and IL-4 differentiate into dendritic cells that produce less IL-12 and shift Th cell responses toward a Th2 cytokine pattern. J. Immunol. 168:6199–6207 [DOI] [PubMed] [Google Scholar]
- Eisenbarth S.C., Piggott D.A., Huleatt J.W., Visintin I., Herrick C.A., Bottomly K. 2002. Lipopolysaccharide-enhanced, toll-like receptor 4-dependent T helper cell type 2 responses to inhaled antigen. J. Exp. Med. 196:1645–1651 10.1084/jem.20021340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott E.A., Drake J.R., Amigorena S., Elsemore J., Webster P., Mellman I., Flavell R.A. 1994. The invariant chain is required for intracellular transport and function of major histocompatibility complex class II molecules. J. Exp. Med. 179:681–694 10.1084/jem.179.2.681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grayson M.H., Cheung D., Rohlfing M.M., Kitchens R., Spiegel D.E., Tucker J., Battaile J.T., Alevy Y., Yan L., Agapov E., et al. 2007. Induction of high-affinity IgE receptor on lung dendritic cells during viral infection leads to mucous cell metaplasia. J. Exp. Med. 204:2759–2769 10.1084/jem.20070360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammad H., Lambrecht B.N. 2008. Dendritic cells and epithelial cells: linking innate and adaptive immunity in asthma. Nat. Rev. Immunol. 8:193–204 10.1038/nri2275 [DOI] [PubMed] [Google Scholar]
- Hammad H., Charbonnier A.S., Duez C., Jacquet A., Stewart G.A., Tonnel A.B., Pestel J. 2001. Th2 polarization by Der p 1—pulsed monocyte-derived dendritic cells is due to the allergic status of the donors. Blood. 98:1135–1141 10.1182/blood.V98.4.1135 [DOI] [PubMed] [Google Scholar]
- Hammad H., Chieppa M., Perros F., Willart M.A., Germain R.N., Lambrecht B.N. 2009. House dust mite allergen induces asthma via Toll-like receptor 4 triggering of airway structural cells. Nat. Med. 15:410–416 10.1038/nm.1946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humbles A.A., Lloyd C.M., McMillan S.J., Friend D.S., Xanthou G., McKenna E.E., Ghiran S., Gerard N.P., Yu C., Orkin S.H., Gerard C. 2004. A critical role for eosinophils in allergic airways remodeling. Science. 305:1776–1779 10.1126/science.1100283 [DOI] [PubMed] [Google Scholar]
- Imai Y., Kuba K., Neely G.G., Yaghubian-Malhami R., Perkmann T., van Loo G., Ermolaeva M., Veldhuizen R., Leung Y.H., Wang H., et al. 2008. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 133:235–249 10.1016/j.cell.2008.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubzick C., Bogunovic M., Bonito A.J., Kuan E.L., Merad M., Randolph G.J. 2008. Lymph-migrating, tissue-derived dendritic cells are minor constituents within steady-state lymph nodes. J. Exp. Med. 205:2839–2850 10.1084/jem.20081430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankovic D., Kullberg M.C., Caspar P., Sher A. 2004. Parasite-induced Th2 polarization is associated with down-regulated dendritic cell responsiveness to Th1 stimuli and a transient delay in T lymphocyte cycling. J. Immunol. 173:2419–2427 [DOI] [PubMed] [Google Scholar]
- Jung S., Unutmaz D., Wong P., Sano G., De los Santos K., Sparwasser T., Wu S., Vuthoori S., Ko K., Zavala F., et al. 2002. In vivo depletion of CD11c+ dendritic cells abrogates priming of CD8+ T cells by exogenous cell-associated antigens. Immunity. 17:211–220 10.1016/S1074-7613(02)00365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S., Prout M., Ramshaw H., Lopez A.F., LeGros G., Min B. 2010. Cutting edge: basophils are transiently recruited into the draining lymph nodes during helminth infection via IL-3, but infection-induced Th2 immunity can develop without basophil lymph node recruitment or IL-3. J. Immunol. 184:1143–1147 10.4049/jimmunol.0902447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kool M., Soullié T., van Nimwegen M., Willart M.A., Muskens F., Jung S., Hoogsteden H.C., Hammad H., Lambrecht B.N. 2008. Alum adjuvant boosts adaptive immunity by inducing uric acid and activating inflammatory dendritic cells. J. Exp. Med. 205:869–882 10.1084/jem.20071087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopf M., Le Gros G., Bachmann M., Lamers M.C., Bluethmann H., Köhler G. 1993. Disruption of the murine IL-4 gene blocks Th2 cytokine responses. Nature. 362:245–248 10.1038/362245a0 [DOI] [PubMed] [Google Scholar]
- Krishnamoorthy N., Oriss T.B., Paglia M., Fei M., Yarlagadda M., Vanhaesebroeck B., Ray A., Ray P. 2008. Activation of c-Kit in dendritic cells regulates T helper cell differentiation and allergic asthma. Nat. Med. 14:565–573 10.1038/nm1766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuipers H., Soullié T., Hammad H., Willart M., Kool M., Hijdra D., Hoogsteden H.C., Lambrecht B.N. 2009. Sensitization by intratracheally injected dendritic cells is independent of antigen presentation by host antigen-presenting cells. J. Leukoc. Biol. 85:64–70 10.1189/jlb.0807519 [DOI] [PubMed] [Google Scholar]
- Lambrecht B.N., Hammad H. 2009. Biology of lung dendritic cells at the origin of asthma. Immunity. 31:412–424 10.1016/j.immuni.2009.08.008 [DOI] [PubMed] [Google Scholar]
- Lambrecht B.N., Salomon B., Klatzmann D., Pauwels R.A. 1998. Dendritic cells are required for the development of chronic eosinophilic airway inflammation in response to inhaled antigen in sensitized mice. J. Immunol. 160:4090–4097 [PubMed] [Google Scholar]
- Lambrecht B.N., De Veerman M., Coyle A.J., Gutierrez-Ramos J.C., Thielemans K., Pauwels R.A. 2000. Myeloid dendritic cells induce Th2 responses to inhaled antigen, leading to eosinophilic airway inflammation. J. Clin. Invest. 106:551–559 10.1172/JCI8107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz C.S., Boesiger J., Song C.H., Mach N., Kobayashi T., Mulligan R.C., Nawa Y., Dranoff G., Galli S.J. 1998. Role for interleukin-3 in mast-cell and basophil development and in immunity to parasites. Nature. 392:90–93 10.1038/32190 [DOI] [PubMed] [Google Scholar]
- Le Gros G., Ben-Sasson S.Z., Seder R., Finkelman F.D., Paul W.E. 1990. Generation of interleukin 4 (IL-4)-producing cells in vivo and in vitro: IL-2 and IL-4 are required for in vitro generation of IL-4-producing cells. J. Exp. Med. 172:921–929 10.1084/jem.172.3.921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee N.A., Gelfand E.W., Lee J.J. 2001. Pulmonary T cells and eosinophils: coconspirators or independent triggers of allergic respiratory pathology? J. Allergy Clin. Immunol. 107:945–957 10.1067/mai.2001.116002 [DOI] [PubMed] [Google Scholar]
- MacDonald A.S., Straw A.D., Dalton N.M., Pearce E.J. 2002. Cutting edge: Th2 response induction by dendritic cells: a role for CD40. J. Immunol. 168:537–540 [DOI] [PubMed] [Google Scholar]
- Matsubara S., Koya T., Takeda K., Joetham A., Miyahara N., Pine P., Masuda E.S., Swasey C.H., Gelfand E.W. 2006. Syk activation in dendritic cells is essential for airway hyperresponsiveness and inflammation. Am. J. Respir. Cell Mol. Biol. 34:426–433 10.1165/rcmb.2005-0298OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer D., Fiebiger S., Ebner C., Reininger B., Fischer G.F., Wichlas S., Jouvin M.H., Schmitt-Egenolf M., Kraft D., Kinet J.P., Stingl G. 1996. Peripheral blood dendritic cells express Fc epsilon RI as a complex composed of Fc epsilon RI alpha- and Fc epsilon RI gamma-chains and can use this receptor for IgE-mediated allergen presentation. J. Immunol. 157:607–616 [PubMed] [Google Scholar]
- Maurer D., Fiebiger E., Reininger B., Ebner C., Petzelbauer P., Shi G.P., Chapman H.A., Stingl G. 1998. Fc ε receptor I on dendritic cells delivers IgE-bound multivalent antigens into a cathepsin S-dependent pathway of MHC class II presentation. J. Immunol. 161:2731–2739 [PubMed] [Google Scholar]
- Min B., Prout M., Hu-Li J., Zhu J., Jankovic D., Morgan E.S., Urban J.F., Jr., Dvorak A.M., Finkelman F.D., LeGros G., Paul W.E. 2004. Basophils produce IL-4 and accumulate in tissues after infection with a Th2-inducing parasite. J. Exp. Med. 200:507–517 10.1084/jem.20040590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohrs M., Shinkai K., Mohrs K., Locksley R.M. 2001. Analysis of type 2 immunity in vivo with a bicistronic IL-4 reporter. Immunity. 15:303–311 10.1016/S1074-7613(01)00186-8 [DOI] [PubMed] [Google Scholar]
- Mohrs K., Wakil A.E., Killeen N., Locksley R.M., Mohrs M. 2005. A two-step process for cytokine production revealed by IL-4 dual-reporter mice. Immunity. 23:419–429 10.1016/j.immuni.2005.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy K.M., Heimberger A.B., Loh D.Y. 1990. Induction by antigen of intrathymic apoptosis of CD4+CD8+ TCRlo thymocytes in vivo. Science. 21:1720–1723 10.1126/science.2125367 [DOI] [PubMed] [Google Scholar]
- Naik S.H., Proietto A.I., Wilson N.S., Dakic A., Schnorrer P., Fuchsberger M., Lahoud M.H., O’Keeffe M., Shao Q.X., Chen W.F., et al. 2005. Cutting edge: generation of splenic CD8+ and CD8- dendritic cell equivalents in Fms-like tyrosine kinase 3 ligand bone marrow cultures. J. Immunol. 174:6592–6597 [DOI] [PubMed] [Google Scholar]
- Naik S.H., Sathe P., Park H.Y., Metcalf D., Proietto A.I., Dakic A., Carotta S., O’Keeffe M., Bahlo M., Papenfuss A., et al. 2007. Development of plasmacytoid and conventional dendritic cell subtypes from single precursor cells derived in vitro and in vivo. Nat. Immunol. 8:1217–1226 10.1038/ni1522 [DOI] [PubMed] [Google Scholar]
- Nathan A.T., Peterson E.A., Chakir J., Wills-Karp M. 2009. Innate immune responses of airway epithelium to house dust mite are mediated through beta-glucan-dependent pathways. J. Allergy Clin. Immunol. 123:612–618 10.1016/j.jaci.2008.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obata K., Mukai K., Tsujimura Y., Ishiwata K., Kawano Y., Minegishi Y., Watanabe N., Karasuyama H. 2007. Basophils are essential initiators of a novel type of chronic allergic inflammation. Blood. 110:913–920 10.1182/blood-2007-01-068718 [DOI] [PubMed] [Google Scholar]
- Paul W.E., Zhu J. 2010. How are T(H)2-type immune responses initiated and amplified? Nat. Rev. Immunol. 10:225–235 10.1038/nri2735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrigoue J.G., Saenz S.A., Siracusa M.C., Allenspach E.J., Taylor B.C., Giacomin P.R., Nair M.G., Du Y., Zaph C., van Rooijen N., et al. 2009. MHC class II-dependent basophil-CD4+ T cell interactions promote T(H)2 cytokine-dependent immunity. Nat. Immunol. 10:697–705 10.1038/ni.1740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S., Lam C.E., Kaiko G.E., Foo S.Y., Collison A., Mattes J., Barry J., Davidson S., Oreo K., Smith L., et al. 2009. Toll/IL-1 signaling is critical for house dust mite-specific Th1 and Th2 responses. Am. J. Respir. Crit. Care Med. 179:883–893 10.1164/rccm.200806-974OC [DOI] [PubMed] [Google Scholar]
- Piggott D.A., Eisenbarth S.C., Xu L., Constant S.L., Huleatt J.W., Herrick C.A., Bottomly K. 2005. MyD88-dependent induction of allergic Th2 responses to intranasal antigen. J. Clin. Invest. 115:459–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche P.A. 1995. HLA-DM: an in vivo facilitator of MHC class II peptide loading. Immunity. 3:259–262 10.1016/1074-7613(95)90111-6 [DOI] [PubMed] [Google Scholar]
- Schneider E., Petit-Bertron A.F., Bricard R., Levasseur M., Ramadan A., Girard J.P., Herbelin A., Dy M. 2009. IL-33 activates unprimed murine basophils directly in vitro and induces their in vivo expansion indirectly by promoting hematopoietic growth factor production. J. Immunol. 183:3591–3597 10.4049/jimmunol.0900328 [DOI] [PubMed] [Google Scholar]
- Seder R.A., Paul W.E., Davis M.M., Fazekas de St Groth B. 1992. The presence of interleukin 4 during in vitro priming determines the lymphokine-producing potential of CD4+ T cells from T cell receptor transgenic mice. J. Exp. Med. 176:1091–1098 10.1084/jem.176.4.1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen T., Kim S., Do J.S., Wang L., Lantz C., Urban J.F., Le Gros G., Min B. 2008. T cell-derived IL-3 plays key role in parasite infection-induced basophil production but is dispensable for in vivo basophil survival. Int. Immunol. 20:1201–1209 10.1093/intimm/dxn077 [DOI] [PubMed] [Google Scholar]
- Shi H.Z., Humbles A., Gerard C., Jin Z., Weller P.F. 2000. Lymph node trafficking and antigen presentation by endobronchial eosinophils. J. Clin. Invest. 105:945–953 10.1172/JCI8945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortman K., Naik S.H. 2007. Steady-state and inflammatory dendritic-cell development. Nat. Rev. Immunol. 7:19–30 10.1038/nri1996 [DOI] [PubMed] [Google Scholar]
- Sokol C.L., Barton G.M., Farr A.G., Medzhitov R. 2008. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat. Immunol. 9:310–318 10.1038/ni1558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol C.L., Chu N.Q., Yu S., Nish S.A., Laufer T.M., Medzhitov R. 2009. Basophils function as antigen-presenting cells for an allergen-induced T helper type 2 response. Nat. Immunol. 10:713–720 10.1038/ni.1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stumbles P.A., Thomas J.A., Pimm C.L., Lee P.T., Venaille T.J., Proksch S., Holt P.G. 1998. Resting respiratory tract dendritic cells preferentially stimulate T helper cell type 2 (Th2) responses and require obligatory cytokine signals for induction of Th1 immunity. J. Exp. Med. 188:2019–2031 10.1084/jem.188.11.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung S., Rose C.E., Jr., Fu S.M. 2001. Intratracheal priming with ovalbumin- and ovalbumin 323-339 peptide-pulsed dendritic cells induces airway hyperresponsiveness, lung eosinophilia, goblet cell hyperplasia, and inflammation. J. Immunol. 166:1261–1271 [DOI] [PubMed] [Google Scholar]
- Tang H., Cao W., Kasturi S.P., Ravindran R., Nakaya H.I., Kundu K., Murthy N., Kepler T.B., Malissen B., Pulendran B. 2010. The T helper type 2 response to cysteine proteases requires dendritic cell-basophil cooperation via RAS-mediated signaling. Nat. Immunol. 10.1038/ni.1883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompette A., Divanovic S., Visintin A., Blanchard C., Hegde R.S., Madan R., Thorne P.S., Wills-Karp M., Gioannini T.L., Weiss J.P., Karp C.L. 2009. Allergenicity resulting from functional mimicry of a Toll-like receptor complex protein. Nature. 457:585–588 10.1038/nature07548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rijt L.S., Jung S., Kleinjan A., Vos N., Willart M., Duez C., Hoogsteden H.C., Lambrecht B.N. 2005. In vivo depletion of lung CD11c+ dendritic cells during allergen challenge abrogates the characteristic features of asthma. J. Exp. Med. 201:981–991 10.1084/jem.20042311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermaelen K.Y., Carro-Muino I., Lambrecht B.N., Pauwels R.A. 2001. Specific migratory dendritic cells rapidly transport antigen from the airways to the thoracic lymph nodes. J. Exp. Med. 193:51–60 10.1084/jem.193.1.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voehringer D., Shinkai K., Locksley R.M. 2004. Type 2 immunity reflects orchestrated recruitment of cells committed to IL-4 production. Immunity. 20:267–277 10.1016/S1074-7613(04)00026-3 [DOI] [PubMed] [Google Scholar]
- Voehringer D., Reese T.A., Huang X., Shinkai K., Locksley R.M. 2006. Type 2 immunity is controlled by IL-4/IL-13 expression in hematopoietic non-eosinophil cells of the innate immune system. J. Exp. Med. 203:1435–1446 10.1084/jem.20052448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Zhan Y., Lew A.M., Naik S.H., Kershaw M.H. 2007. Differential development of murine dendritic cells by GM-CSF versus Flt3 ligand has implications for inflammation and trafficking. J. Immunol. 179:7577–7584 [DOI] [PubMed] [Google Scholar]
- Yoshimoto T., Yasuda K., Tanaka H., Nakahira M., Imai Y., Fujimori Y., Nakanishi K. 2009. Basophils contribute to T(H)2-IgE responses in vivo via IL-4 production and presentation of peptide-MHC class II complexes to CD4+ T cells. Nat. Immunol. 10:706–712 10.1038/ni.1737 [DOI] [PubMed] [Google Scholar]
- Zheng W., Flavell R.A. 1997. The transcription factor GATA-3 is necessary and sufficient for Th2 cytokine gene expression in CD4 T cells. Cell. 89:587–596 10.1016/S0092-8674(00)80240-8 [DOI] [PubMed] [Google Scholar]