Abstract
The paradoxical coexistence of spontaneous tumor antigen–specific immune responses with progressive disease in cancer patients furthers the need to dissect the molecular pathways involved in tumor-induced T cell dysfunction. In patients with advanced melanoma, we have previously shown that the cancer-germline antigen NY-ESO-1 stimulates spontaneous NY-ESO-1–specific CD8+ T cells that up-regulate PD-1 expression. We also observed that PD-1 regulates NY-ESO-1–specific CD8+ T cell expansion upon chronic antigen stimulation. In the present study, we show that a fraction of PD-1+ NY-ESO-1–specific CD8+ T cells in patients with advanced melanoma up-regulates Tim-3 expression and that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells are more dysfunctional than Tim-3−PD-1+ and Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells, producing less IFN-γ, TNF, and IL-2. Tim-3–Tim-3L blockade enhanced cytokine production by NY-ESO-1–specific CD8+ T cells upon short ex vivo stimulation with cognate peptide, thus enhancing their functional capacity. In addition, Tim-3–Tim-3L blockade enhanced cytokine production and proliferation of NY-ESO-1–specific CD8+ T cells upon prolonged antigen stimulation and acted in synergy with PD-1–PD-L1 blockade. Collectively, our findings support the use of Tim-3–Tim-3L blockade together with PD-1–PD-L1 blockade to reverse tumor-induced T cell exhaustion/dysfunction in patients with advanced melanoma.
There is ample evidence that patients with melanoma can develop immune responses directed against antigens expressed by their own tumor (Boon et al., 2006). Among these antigens, cancer-germline antigens (CGAs) are expressed by tumors of many different histological types, including melanoma, but not by normal tissues, except testis. Because germ cells in testis do not express HLA molecules on their surface (Haas et al., 1988), CGAs represent strictly tumor-specific T cell targets (Boon et al., 2006). Among CGAs, NY-ESO-1 has been shown to stimulate spontaneous cellular and humoral responses that are detectable only in patients with advanced NY-ESO-1–expressing cancer (Stockert et al., 1998; Jäger et al., 2000; Mandic et al., 2005; Fourcade et al., 2008). Understanding the failure of spontaneous NY-ESO-1–specific T cell responses to promote regression of NY-ESO-1+ tumors is therefore critical for the design of novel therapeutic interventions aimed at overcoming tumor-induced immune escape.
We have previously shown that the large majority of spontaneous NY-ESO-1–specific CD8+ T cells up-regulates programmed death 1 (PD-1) expression (Fourcade et al., 2009), which appears to be associated with T cell exhaustion/dysfunction in chronic viral infections in animals and humans (Barber et al., 2006; Day et al., 2006; Petrovas et al., 2006; Trautmann et al., 2006). We observed that PD-1 up-regulation on spontaneous NY-ESO-1–specific CD8+ T cells occurs along with T cell activation and is not directly associated with an inability to produce cytokines ex vivo upon stimulation with cognate antigen. Blockade of the PD-1–programmed death ligand 1 (PD-L1) pathway in combination with prolonged antigen stimulation with PD-L1+ APCs or melanoma cells augmented the frequencies of cytokine-producing, proliferating, and total NY-ESO-1–specific CD8+ T cells. Our findings are in line with previous studies of PD-1 expression by HIV- and SIV-specific CD8+ T cells, demonstrating that PD-1 is a regulator of antigen-specific CD8+ T cell expansion in the context of chronic antigen exposure, although it does not exhibit a major impact upon their functionality on a cell-per-cell basis (Petrovas et al., 2006, 2007). To further determine whether other molecular pathways are involved in tumor antigen–specific T cell dysfunction, we studied T cell immunoglobulin and mucin-domain–containing molecule 3 (Tim-3) expression on spontaneous NY-ESO-1–specific CD8+ T cells from patients with advanced melanoma and investigated whether Tim-3 up-regulation defines a subgroup of dysfunctional tumor antigen–specific CD8+ T cells. Tim-3 is a transmembrane protein constitutively expressed on Th1/Tc1 cells in mice and humans (Monney et al., 2002). Several lines of evidence support the role of Tim-3 as an inhibitory molecule that down-regulates effector Th1/Tc1 cell responses. In mice, blocking the Tim-3–Tim-3L pathway resulted in hyperproliferation of Th1-type cells and abrogated the induction of peripheral and transplantation tolerance (Sabatos et al., 2003; Sánchez-Fueyo et al., 2003). Tim-3 interacts with its ligand galectin-9 to induce cell death in Th1 cells (Zhu et al., 2005). In humans, Tim-3 expression is defective in CD4+ T cells producing high levels of IFN-γ, as well as those isolated from cerebrospinal fluid of patients with multiple sclerosis (Koguchi et al., 2006). Recently, Tim-3 up-regulation has been reported in HIV-specific and HCV-specific CD8+ T cells in patients with progressive HIV infection and chronic hepatitis C, respectively (Jones et al., 2008; Golden-Mason et al., 2009). Tim-3+ HIV- and HCV-specific CD8+ T cells were distinct from the PD-1+ CD8+ T cells and exhibited T cell dysfunction. However, it is unknown whether tumor antigen–specific CD8+ T cells in patients with advanced cancers express Tim-3.
In this study, we show that a fraction of PD-1+ NY-ESO-1–specific CD8+ T cells, which represents the large majority of circulating NY-ESO-1–specific CD8+ T cells in patients with advanced melanoma, up-regulates Tim-3 expression. Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells are highly dysfunctional compared with Tim-3−PD-1+ and Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells. Tim-3–Tim-3L pathway blockade alone or in combination with PD-1–PD-L1 pathway blockade enhanced NY-ESO-1–specific CD8+ T cell numbers and functions. Collectively, our findings support the use of Tim-3–Tim-3L blockade in association with PD-1–PD-L1 blockade to reverse tumor-induced T cell exhaustion/dysfunction in patients with advanced melanoma.
RESULTS
Tim-3 expression is up-regulated on NY-ESO-1–specific CD8+ T cells
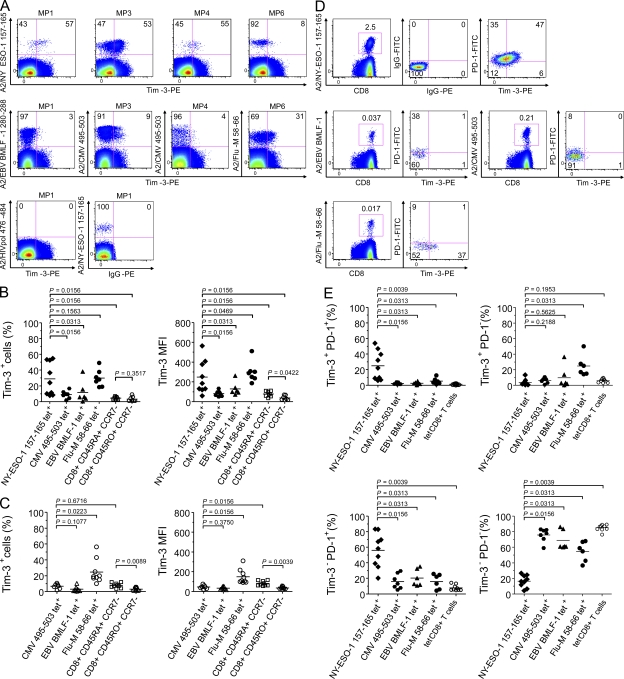
Using HLA-A2 (A2) tetramers, we assessed Tim-3 expression by flow cytometry on the surface of spontaneous ex vivo detectable NY-ESO-1–specific CD8+ T cells and CMV-, EBV-, and influenza (Flu)-specific CD8+ T cells isolated from PBMCs of nine HLA-A*0201+ (HLA-A2+) stage IV melanoma patients and nine HLA-A2+ healthy donors. In melanoma patients, frequencies of Tim-3+ cells among NY-ESO-1–specific CD8+ T cells (mean 28.8% ± SD 20.7%) were significantly higher than those of CMV-specific CD8+ T cells (8.8 ± 4.9%; P = 0.0156) and EBV-specific CD8+ T cells (11.6 ± 13.8%; P = 0.0313; Fig. 1, A and B). The mean percentage of Tim-3 expression on NY-ESO-1–specific CD8+ T cells was similar to the one observed on Flu-specific CD8+ T cells, although Tim-3 expression on Flu-specific CD8+ T cells was more homogenous among patients than on NY-ESO-1–specific CD8+ T cells (29.8 ± 10.8%; P = 0.1563). The percentages of Tim-3+ NY-ESO-1–specific CD8+ T cells in melanoma patients were consistently higher than those of Tim-3+ effector (CD45RA+CCR7−) and effector memory (CD45RO+CCR7−) CD8+ T cells (4.6% ± 1.6% and 3.3% ± 3.2%, respectively; P = 0.0156). Similar observations were made when analyzing Tim-3 expression as mean fluorescence intensity (MFI), with the exception that Tim-3 MFI was higher on total effector than on total effector memory CD8+ T cells (77.7 ± 29.5 versus 38 ± 23.7, respectively; P = 0.0422; Fig. 1 B, right).
Figure 1.
Tim-3 is up-regulated and coexpressed with PD-1 on NY-ESO-1–specific CD8+ T cells. (A) Representative dot plots from melanoma patients (MP) showing ex vivo Tim-3 expression on A2/NY-ESO-1 157–165, A2/EBV BMLF-1 280–288, A2/CMV 495–503, and A2/Flu-M 58–66 tet+ CD8+ T cells. As shown for one melanoma patient (MP1), CD8+ T cells stained with A2/HIVpol 476–484 tetramers or PE-labeled IgG control Ab were used to establish the threshold for identifying tet+ cells and Tim-3+ cells, respectively. (B and C) Pooled data showing the percentage (%) and MFI of Tim-3 expression on NY-ESO-1–, CMV-, EBV-, and Flu-specific CD8+ T cells, as well as total effector (CD45RA+ CCR7−) and effector/memory (CD45RO+ CCR7−) CD8+ T cells from nine melanoma patients (B) and nine healthy donors (C). (D) Dot plots from one representative melanoma patient showing ex vivo Tim-3 and PD-1 expression on A2/NY-ESO-1 157–165, A2/EBV BMLF-1 280–288, A2/CMV 495–503 and A2/Flu-M 58–66 tet+ CD8+ T cells. As control, A2/NY-ESO-1 157–165 tet+ CD8+ T cells stained with PE-labeled and FITC-labeled IgG control antibodies are shown. (E) Pooled data showing the distribution of NY-ESO-1–, CMV-, EBV-, and Flu-specific CD8+ T cells, as well as total tet− CD8+ T cells according to Tim-3 and PD-1 expression. Horizontal bars depict the mean percentage or MFI of Tim-3 and/or PD-1 expression on tet+ CD8+ T cells. The p- values were calculated using the Wilcoxon signed rank test. Data shown are representative of at least three independent experiments.
In healthy donors, frequencies of Tim-3+ cells were also significantly higher among Flu-specific CD8+ T cells (24.8 ± 15%) than among CMV- and EBV-specific CD8+ T cells (6.8 ± 3.2% and 3.1 ± 3.3%, respectively; P = 0.0223; Fig. 1 C). As expected, no spontaneous NY-ESO-1–specific CD8+ T cells were detectable in PBMCs from healthy donors. The mean percentage of Tim-3+ cells and the mean Tim-3 MFI were significantly higher for total effector (CD45RA+CCR7−) than for total effector memory (CD45RO+CCR7−) CD8+ T cells (9.8 ± 5.9% versus 3.1 ± 2.1% and 81.3 ± 24.9 versus 35.6 ± 13.4, respectively; P = 0.0089 and P = 0.0039).
We have assessed Tim-3 expression on different subsets of mononuclear cells, including CD4+ T cells, CD8+ T cells, NK cells (CD56+), B cells (CD19+), monocytes (CD14+), and myeloid DCs (mDCs; CD11c+) isolated from PBMCs of six melanoma patients and six healthy donors. We found that Tim-3 expression is up-regulated on the surface of NK cells, monocytes, and mDCs in melanoma patients and healthy donors. However, within these cell subsets, no significant difference was observed for Tim-3 expression between melanoma patients and healthy donors (Fig. S1).
As the majority of spontaneous NY-ESO-1–specific CD8+ T cells in melanoma patients up-regulates PD-1 expression (Fourcade et al., 2009), we next determined whether Tim-3 and PD-1 are expressed on identical or distinct T cell subsets. Using HLA-A2 tetramers, NY-ESO-1–, CMV-, EBV-, and Flu-specific CD8+ T cells present in PBMCs of nine melanoma patients were costained ex vivo for Tim-3 and PD-1 and analyzed by flow cytometry. We observed that Tim-3 expression on NY-ESO-1–specific CD8+ T cells (mean of Tim-3+ NY-ESO-1–specific CD8+ T cells: 28.8 ± 20.7% of total NY-ESO-1–specific CD8+ T cells; Fig.1 B) was associated with PD-1 expression, as the mean percentage of Tim-3+PD-1+ cells among total NY-ESO-1–specific CD8+ T cells was significantly higher than the mean percentage of Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells (24.8 ± 18.7% versus 4 ± 3.9%, respectively; P = 0.0039; Fig. 1, D and E). Among total NY-ESO-1–specific CD8+ T cells, Tim-3− NY-ESO-1–specific CD8+ T cells (mean 71.2 ± 20.7% of total NY-ESO-1–specific CD8+ T cells; Fig. 1 B) were predominantly PD-1+ (mean 54.2 ± 20.1%) and Tim-3−PD-1− represented a smaller subset (mean 17 ± 8%; Fig. 1, D and E). In sharp contrast with our findings of Tim-3 and PD-1 expression on NY-ESO-1–specific CD8+ T cells, CMV-, EBV-, and Flu-specific CD8+ T cells in the same melanoma patients were in their large majority Tim-3−PD-1− (means 75.7 ± 8.5%, 65.4 ± 10.2%, and 52.2 ± 12.6% of total virus-specific CD8+ T cells, respectively) and displayed very low frequencies of Tim-3+PD-1+ cells (means 2.1 ± 1.2%, 2.9 ± 1.4%, and 6.1 ± 4.1% of total virus-specific CD8+ T cells, respectively). In addition, and in contrast to NY-ESO-1–specific CD8+ T cells, Tim-3 and PD-1 were mainly expressed by distinct populations among CMV-, EBV-, and Flu-specific CD8+ T cells (Fig. 1, D and E). Strikingly, although the levels of Tim-3 expression on Flu-specific CD8+ T cells were similar to those of NY-ESO-1–specific CD8+ T cells (mean of Tim-3+ Flu-specific CD8+ T cells, 29.8 ± 10.8% of total Flu-specific CD8+ T cells; Fig. 1 B), Tim-3+ Flu-specific CD8+ T cells were predominantly PD-1− (mean 24.3 ± 15%) and PD-1+ cells represented a much smaller fraction (mean 5.5 ± 3.1%; Fig. 1 E). Among total CD8+ T cells, frequencies of Tim-3+ PD-1+ CD8+ T cells were lower than those of Tim-3−PD-1−, Tim-3−PD-1+ and Tim-3+PD-1−CD8+ T cells in melanoma patients and healthy donors. Notably, Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells represented up to 33% of total Tim-3+PD-1+ CD8+ T cells in melanoma patients (unpublished data).
Collectively, our results demonstrate that Tim-3 expression is up-regulated on tumor-induced NY-ESO-1–specific CD8+ T cells and on Flu-specific CD8+ T cells in advanced-stage melanoma patients with a heterogeneous expression observed on NY-ESO-1–specific CD8+ T cells. In addition, the vast majority of Tim-3+ NY-ESO-1–specific, but not Flu-, EBV-, and CMV-specific CD8+ T cells, up-regulates PD-1 expression.
Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells represent a dysfunctional T cell population
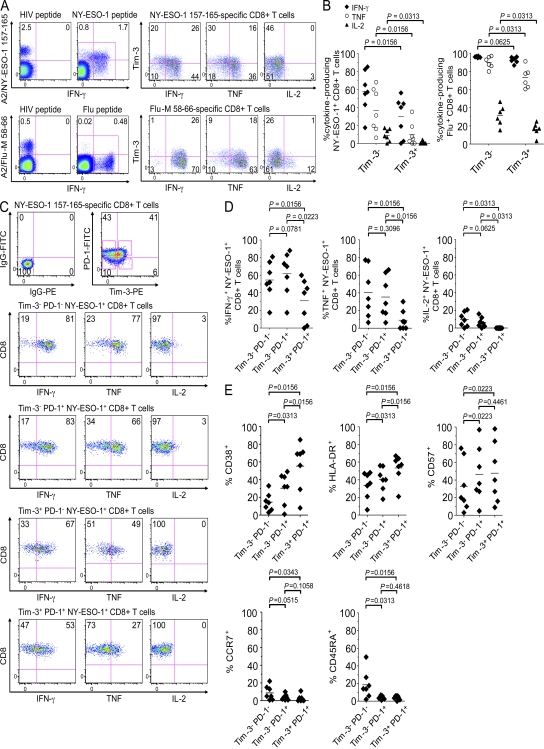
We next compared the ability of Tim-3+ and Tim-3− NY-ESO-1–specific CD8+ T cells to produce cytokines ex vivo upon short stimulation (6 h) with cognate peptide–pulsed APCs (autologous CD3− cells). Percentages of IFN-γ–, TNF-, and IL-2–producing cells within Tim-3+ and Tim-3− fractions of NY-ESO-1–specific CD8+ T cells were assessed after gating on NY-ESO-1–specific CD8+ T cells, including A2/NY-ESO-1 157–165 tetramer+ (tet+) and cytokine-producing CD8+ T cells (Fig. 2 A, left). Cytokine production was restricted to NY-ESO-1–specific CD8+ T cells, as no cytokine was produced by A2/NY-ESO-1 157–165 tet+ CD8+ T cells after incubation with HIV peptide. As shown for one melanoma patient in Fig. 2 A (right) and for seven melanoma patients in Fig. 2 B (left), Tim-3+ NY-ESO-1–specific CD8+ T cells produced significantly less IFN-γ (P = 0.0156), TNF (P = 0.0156), and IL-2 (P = 0.0313) than Tim-3− NY-ESO-1–specific CD8+ T cells. In six out of seven melanoma patients tested, we also investigated the capacity of Tim-3+ and Tim-3− Flu-specific CD8+ T cells to produce cytokines ex vivo upon short stimulation with cognate peptide–pulsed APCs. Tim-3+ Flu-specific CD8+ T cells produced significantly less IL-2 and TNF than Tim-3− Flu-specific CD8+ T cells (P = 0.0313). However, the difference in the percentages of TNF-producing cells between Tim-3+ and Tim-3− subsets was much lower for the Flu-specific CD8+ T cells (mean 73 ± 11.6% versus 89.9 ± 6.5%, respectively) than for the NY-ESO-1–specific CD8+ T cells (mean 9.8 ± 12.8% versus 38 ± 24.3%; Fig. 2 B, right). In addition, we measured no difference in IFN-γ production between Tim-3+ and Tim-3− Flu-specific CD8+ T cells (P = 0.0625). To better understand the major differences in cytokine production between Tim-3+ and Tim-3− NY-ESO-1– and Flu-specific CD8+ T cells, we next investigated whether Tim-3+ NY-ESO-1–specific CD8+ T cells, which also coexpress PD-1 in their large majority (mean 86.1% of total Tim-3+ NY-ESO-1–specific CD8+ T cells) represent a more dysfunctional population than Tim-3+ Flu-specific CD8+ T cells, which coexpress PD-1 only in their minority (mean 19.5% of total Tim-3+ Flu-specific CD8+ T cells). To this end, we costained NY-ESO-1–specific CD8+ T cells from patients for Tim-3 and PD-1 and analyzed cytokine production after 6hr-stimulation with cognate peptide. As shown for one melanoma patient in Fig. 2C and for seven melanoma patients in Fig. 2 D, Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells produced significantly less IFN-γ (P = 0.0156), TNF (P = 0.0156), and IL-2 (P = 0.0313) than Tim-3−PD-1− cells. We did not observe significant differences in cytokine production between Tim-3−PD-1+ and Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells, confirming our previous findings that PD-1 up-regulation is not directly associated with an inability to produce cytokines upon ex vivo stimulation (Fourcade et al., 2009). Strikingly, in one melanoma patient with very high levels of spontaneous NY-ESO-1–specific CD8+ T cells (Fig. 2 C), we observed that Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells produced less IFN-γ and TNF than Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells (67 versus 81% and 49 versus 77%, respectively), suggesting that Tim-3 expression alone defines a population of dysfunctional T cells, as previously reported for HIV-specific CD8+ T cells (Jones et al., 2008). Furthermore, we observed in the same patient that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells produced less IFN-γ and TNF than Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells (53% versus 67% and 27% versus 49%, respectively), suggesting that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells represent a highly dysfunctional T cell population. Notably, the low frequencies of Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells did not allow us to evaluate their function in six out of the seven melanoma patients tested. Collectively, our findings demonstrate that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells are highly dysfunctional in terms of cytokine production.
Figure 2.
Co-expression of Tim-3 and PD-1 by NY-ESO-1–specific CD8+ T cells defines a population of dysfunctional T cells that up-regulate activation markers. (A and B) Representative dot plots from one melanoma patient (A) and summary data for melanoma patients (n = 7; B) showing the percentage of cytokine-producing A2/NY-ESO-1 157–165 tet+ and A2/Flu-M 58–66 tet+ CD8+ T cells among Tim-3+ and Tim-3− fractions after short ex vivo stimulation (6 h) with cognate peptide or irrelevant peptide (HIV peptide). (C and D) Dot plots from one patient (C) and summary data for all melanoma patients (n = 7; D) showing the percentages of cytokine-producing A2/NY-ESO-1 157–165 tet+ CD8+ T cells according to Tim-3 and PD-1 expression. (E) Pooled data from melanoma patients (n = 7) showing expression of CD38, HLA-DR, CD57, CCR7, and CD45RA on A2/NY-ESO-1 157–165 tet+ CD8+ T cells according to Tim-3 and PD-1 expression. The p-values were calculated using the Wilcoxon signed rank test. Data shown are representative of at least three independent experiments.
Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells exhibit high levels of T cell activation
We next assessed the differentiation/activation status of NY-ESO-1–specific CD8+ T cells according to the expression of Tim-3 and/or PD-1. We have compared the percentages of CD8+ T cells from PBMCs of seven stage IV melanoma patients that express the following markers ex vivo: CD38, HLA-DR, CD57, CCR7, CD45RA, CD27, and CD28 among Tim-3−PD-1−, Tim-3−PD-1+, and Tim-3+PD-1+ A2/NY-ESO-1 157–165 tet+ CD8+ T cells. The expression of the activation markers CD38, HLA-DR, and CD57 was higher on Tim-3−PD-1+ than on Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells (P = 0.0313, 0.0313, and 0.0223, respectively; Fig. 2 E). CD38 and HLA-DR were further up-regulated on Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells than on Tim-3−PD-1+ cells (P = 0.0156), whereas both populations expressed similar levels of CD57 (P = 0.4461; Fig. 2 E). The percentages of CCR7+ or CD45RA+ Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells were similar to Tim-3−PD-1+ NY-ESO-1–specific CD8+ T cells (P = 0.1058 and P = 0.4618, respectively), but lower than Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells (P = 0.0343 and P = 0.0156, respectively). In addition, the large majority (>80%) of Tim-3+PD-1+, Tim-3−PD-1+, and Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells were CD27+ and CD28− (unpublished data).
In six melanoma patients, we assessed the expression of CD38, HLA-DR, CD57, CCR7, CD45RA, CD27, and CD28 on A2/Flu-M 58–66 tet+ CD8+ T cells, which do not coexpress Tim-3 and PD-1 in their large majority. We observed that Flu-specific CD8+ T cells displayed a less activated phenotype than NY-ESO-1–specific CD8+ T cells, expressing lower levels of CD38, HLA-DR, and CD57. As compared with NY-ESO-1–specific CD8+ T cells, Flu-specific CD8+ T cells expressed higher levels of CD45RA, whereas no significant differences in terms of CCR7, CD27, and CD28 expression were observed. Therefore, Flu-specific CD8+ T cells include a higher proportion of effector cells (CCR7−CD45RA+) than NY-ESO-1–specific CD8+ T cells that, by their large majority, are effector/memory CD8+ T cells (CCR7−CD45RA−; Fig. S2).
Altogether, our findings show that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells represent a highly activated T cell subset that exhibit a maturation/differentiation status similar to that of Tim-3−PD-1+ NY-ESO-1–specific CD8+ T cells.
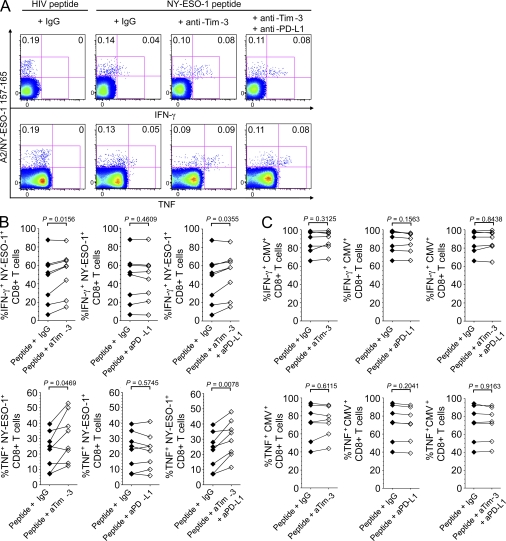
Ex vivo blockade of the Tim-3–Tim-3L pathway enhances NY-ESO-1–specific CD8+ T cell cytokine production
We next tested whether Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cell function augmented by blocking the interaction of Tim-3 with its ligands during a short ex vivo stimulation (6 h). Purified CD8+ T cells isolated from PBMCs of eight melanoma patients with spontaneous NY-ESO-1–specific CD8+ T cells were incubated with APCs (autologous CD3− cells) pulsed with peptide NY-ESO-1 157–165 or peptide HIVpol 476–484 as control, in the presence of blocking mAbs against Tim-3 (clone 2E2) and/or anti–PD-L1 or IgG control antibodies. After stimulation with cognate peptide and anti–Tim-3 mAbs, we observed an increase in total NY-ESO-1–specific CD8+ T cells that produced IFN-γ (P = 0.0156) and TNF (P = 0.0469; Fig. 3, A and B). In contrast, no significant increase in IL-2–producing NY-ESO-1–specific CD8+ T cells was observed (P = 0.5469; unpublished data). PD-1–PD-L1 blockade in combination with Tim3–Tim-3L blockade did not further enhance the capacity of NY-ESO-1–specific CD8+ T cells to produce IFN-γ (P = 0.0680), TNF (P = 0.8438), and IL-2 (P = 0.2188; unpublished data) as compared with incubation with anti–Tim-3 mAbs alone. In agreement with our previous findings, PD-1–PD-L1 blockade alone did not increase cytokine production by NY-ESO-1–specific CD8+ T cells upon short ex vivo stimulation with cognate peptide (Fourcade et al., 2009). We observed no cytokine production by NY-ESO-1 157–165–specific CD8+ T cells after short ex vivo stimulation (6 h) with an irrelevant peptide with or without Tim-3 and/or PD-1 blockade (Fig. S3 A). We also observed that Tim-3 pathway blockade did not significantly enhance cytokine production by CMV-specific CD8+ T cells, which express low levels of Tim-3 ex vivo (Fig. 3 C).
Figure 3.
Ex vivo blockade of the Tim-3–Tim-3L pathway enhances cytokine production by NY-ESO-1–specific CD8+ T cells. (A and B) Representative dot plots from one melanoma patient (A) and summary data for all melanoma patients (n = 8; B) showing the percentages of A2/NY-ESO-1 157–165 tet+ CD8+ T cells that produce IFN-γ and TNF among total NY-ESO-1–specific CD8+ T cells after short ex vivo stimulation with cognate peptide in the presence of blocking anti–Tim-3 and/or anti–PD-L1 mAbs or an isotype control antibody (IgG). (C) Summary data for melanoma patients (n = 6) showing the percentages of A2/CMV 495–503 tet+ CD8+ T cells that produce IFN-γ and TNF among total CMV-specific CD8+ T cells after short ex vivo stimulation with cognate peptide in the presence of blocking anti–Tim-3 and/or anti–PD-L1 mAbs or an isotype control antibody (IgG). The p-values were calculated using the Wilcoxon signed rank test. Data shown are representative of two independent experiments performed in duplicate.
Tim-3–Tim-3L blockade alone or in combination with PD-1–PD-L1 blockade increases the frequency of cytokine-producing NY-ESO-1–specific CD8+ T cells upon prolonged antigen stimulation
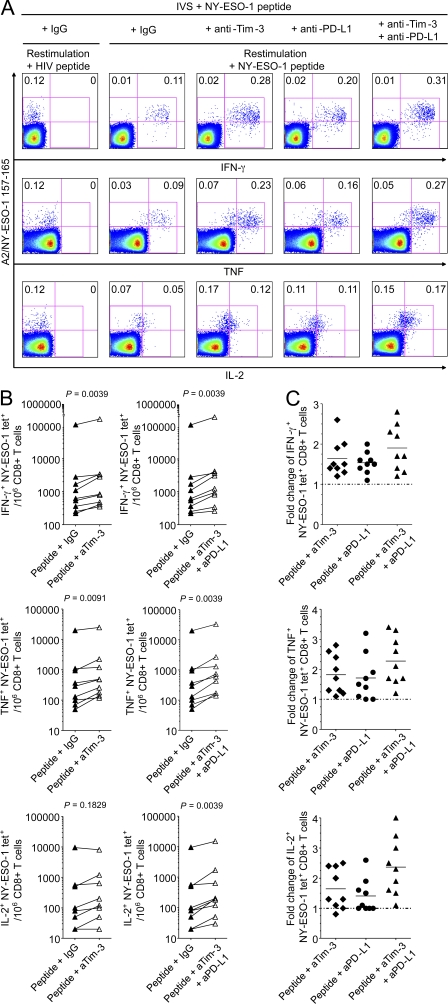
We next assessed the impact of Tim-3 expression on cytokine production by NY-ESO-1–specific CD8+ T cells after a multiday in vitro stimulation (IVS) with peptide-pulsed APCs. PBMCs from nine melanoma patients with spontaneous NY-ESO-1–specific CD8+ T cell response were incubated for 6 d with NY-ESO-1 157–165 peptide in the presence of mAbs against Tim-3 and/or PD-L1 or IgG control antibodies. After 6 d, cells were shortly restimulated (6 h) with NY-ESO-1 peptide or HIV peptide as control before evaluating cytokine production by A2/NY-ESO-1 157–165 tet+ CD8+ T cells. We observed a significant increase in the frequencies of NY-ESO-1–specific CD8+ T cells that produced IFN-γ and TNF (P = 0.0039 and P = 0.0091, respectively) after incubation in the presence of cognate peptide and anti–Tim-3 mAbs, as compared with cognate peptide and IgG control (Fig. 4, A and B), resulting in a 1.6- and 1.8-fold change in the frequencies of IFN-γ– and TNF-producing NY-ESO-1–specific CD8+ T cells, respectively (Fig. 4 C). The frequency of IL-2–producing NY-ESO-1–specific CD8+ T cells increased in a majority of patients in the presence of cognate peptide and anti–Tim-3 mAbs alone, albeit the difference was not statistically significant when compared with IgG control (P = 0.1829). We further observed a significant increase in the frequencies of not only IFN-γ– and TNF- but also IL-2–producing NY-ESO-1–specific CD8+ T cells in the presence of both anti–Tim-3 and anti–PD-L1 mAbs when compared with IgG control antibodies (P = 0.0039), anti–Tim-3 mAbs alone (P = 0.0283, P = 0.0117, and P = 0.0418, respectively), and anti–PD-L1 mAbs alone (P = 0.0177, P = 0.0091, and P = 0.0128, respectively; Fig. 4, A and B and not depicted), suggesting a synergistic effect of Tim-3–Tim-3L and PD-1–PD-L1 blockades on NY-ESO-1–specific CD8+ T cell expansion. This increase resulted in a 1.9-, 2.3-, and 2.4-fold change in the frequencies of IFN-γ-, TNF-, and IL-2–producing NY-ESO-1–specific CD8+ T cells, respectively, when compared with IgG control antibody (Fig. 4 C). As control, PBMCs were incubated with an irrelevant peptide for 6 d in the presence of anti–Tim-3 or anti–PD-L1 mAbs. We did not observe a significant effect of Tim-3 or PD-1 pathway blockade on the frequency of cytokine-producing NY-ESO-1–specific CD8+ T cells after restimulation with cognate peptide (Fig. S3 B). Notably, we observed that Tim-3–Tim-3L blockade increased the percentages of NY-ESO-1–specific CD8+ T cells that produced TNF and IL-2, but not IFN-γ, among total NY-ESO-1–specific CD8+ T cells compared with incubation with IgG control antibody (P = 0.0090, P = 0.0128, and P = 0.1094, respectively; Fig. S4). This observation is in line with our data showing that Tim-3–Tim-3L blockade ex vivo enhances the functionality of NY-ESO-1–specific CD8+ T cells. Although PD-1–PD-L1 blockade alone did not significantly change the capacity of NY-ESO-1–specific CD8+ T cells to produce cytokines (i.e., no increase in the percentages of cytokine-producing cells among total NY-ESO-1–specific CD8+ T cells; Fig. S4), we observed that Tim-3–Tim-3L blockade in combination with PD-1–PD-L1 blockade augmented the percentages of NY-ESO-1–specific CD8+ T cells that produced TNF and IL-2 compared with incubation with IgG control antibody (P = 0.0078 and P = 0.0039, respectively) or Tim-3–Tim-3L blockade alone (P = 0.0433 and P = 0.0117, respectively; Fig. S4). This increase resulted in a 1.3- and 2.2-fold change in the percentages of TNF- and IL-2–producing NY-ESO-1–specific CD8+ T cells among total NY-ESO-1–specific CD8+ T cells, respectively, when compared with IgG control antibody (Fig. S4), indicating a synergistic effect of Tim-3–Tim-3L and PD-1–PD-L1 blockades. Notably, we observed a significant increase in the expression of PD-1 and Tim-3 by NY-ESO-1–specific CD8+ T cells after a 6-d IVS in the presence of cognate peptide and IgG control antibodies as compared with incubation with an irrelevant peptide (Fig. S5). These findings are in line with our previous observation of Tim-3 and PD-1 up-regulation by activated NY-ESO-1–specific CD8+ T cells. Interestingly, Tim-3 or PD-1 blockade in the presence of cognate peptide induced a modest but significant increase in PD-1 and Tim-3 expression, respectively, by NY-ESO-1–specific CD8+ T cells, but not by NY-ESO-1 tet− CD8+ T cells, compared with incubation with cognate peptide and IgG control antibodies (Fig. S5). The up-regulation of Tim-3 and PD-1 expression by NY-ESO-1–specific CD8+ T cells after PD-1 or Tim-3 blockade in the presence of cognate peptide is likely caused by higher levels of T cell activation and may possibly contribute to the synergistic effects of Tim-3 and PD-1 blockades.
Figure 4.
Blockade of the Tim-3–Tim-3L pathway alone or in combination with PD-1–PD-L1 blockade with prolonged antigen stimulation increases the frequency of cytokine-producing NY-ESO-1–specific CD8+ T cells. (A and B) Representative flow cytometry analysis from one melanoma patient showing percentages of IFN-γ-, TNF-, and IL-2–producing A2/NY-ESO-1 157–165 tet+ CD8+ T cells among total CD8+ T cells (A) and pooled data from melanoma patients (n = 9) showing the variation in the frequencies of IFN-γ–, TNF-, and IL-2–producing NY-ESO-1 tet+ cells for 106 CD8+ T cells (B). PBMCs were incubated for 6 d with NY-ESO-1 157–165 peptide or with HIVpol 476–484 peptide and blocking anti–Tim-3 (aTim-3) and/or anti–PD-L1 (aPD-L1) mAbs or an isotype control antibody (IgG) before evaluating intracellular cytokine production of A2/NY-ESO-1 157–165 tet+ CD8+ T cells in response to cognate peptide. (C) Fold change of the frequency of IFN-γ–, TNF-, and IL-2–producing A2/NY-ESO-1 157–165 tet+ CD8+ T cells after 6-d IVS with cognate peptide and blocking anti–Tim-3 and/or anti–PD-L1 mAbs. The ratio of the frequency of cytokine-producing tet+ CD8+ T cells from melanoma patients (n = 9) in the presence of indicated antibody treatment and isotype control antibody is shown. The p-values were calculated using the Wilcoxon signed rank test. Data shown are representative of two independent experiments performed in duplicate.
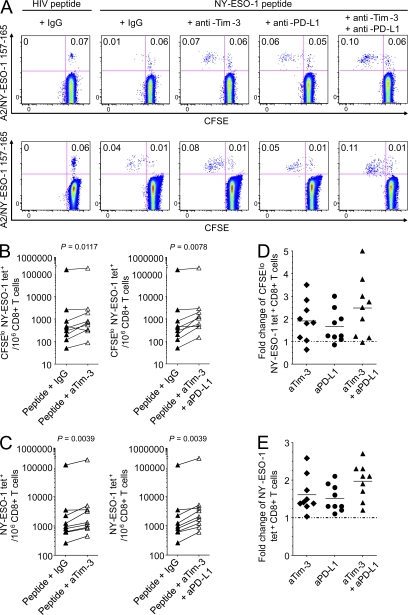
Tim-3–Tim-3L blockade alone or in combination with PD-1–PD-L1 blockade increases proliferation of NY-ESO-1–specific CD8+ T cells
Next, we evaluated whether Tim-3–Tim-3L blockade alone or in combination with PD-1–PD-L1 blockade increased proliferation of NY-ESO-1–specific CD8+ T cells in response to the cognate antigen in a multiday IVS. CFSE-labeled PBMCs from nine melanoma patients with spontaneous NY-ESO-1–specific CD8+ T cell response were stimulated for 6 d with NY-ESO-1 157–165 peptide in the presence of mAbs against Tim-3 and/or PD-L1 or IgG control antibodies. As control, PBMCs were incubated for 6 d with HIVpol 476–484 peptide. As shown in Fig. 5 A for two melanoma patients and in Fig. 5 (B and C) for nine patients, the addition of anti–Tim-3 mAbs augmented the frequencies of CFSElo and total A2/NY-ESO-1 157–165 tet+ CD8+ T cells stimulated in the presence of cognate peptide as compared with peptide and IgG control antibody (P = 0.0117 and P = 0.0039, respectively), resulting in a 1.9- and a 1.6-fold change in the frequencies of CFSElo and total A2/NY-ESO-1 157–165 tet+ CD8+ T cells, respectively (Fig. 5, D and E). In line with previous findings (Fourcade et al., 2009), PD-1–PD-L1 blockade in the presence of cognate peptide enhanced proliferating and total NY-ESO-1–specific CD8+ T cells (P = 0.0117 and P = 0.0039, respectively; Fig. 5 A and not depicted), resulting in a 1.7- and a 1.5-fold change in the frequencies of CFSElo and total A2/NY-ESO-1 157–165 tet+ CD8+ T cells, respectively (Fig. 5, D and E). Importantly, blockade of both Tim-3–Tim-3L and PD-1–PD-L1 pathways further increased the frequencies of CFSElo and total A2/NY-ESO-1 157–165 tet+ CD8+ T cells as compared with stimulation with IgG control antibodies (P = 0.0078 and P = 0.0039, respectively; Fig. 5, A–C), Tim-3 blockade alone (P = 0.0078 and P = 0.0039, respectively), or PD-L1 blockade alone (P = 0.0324 and P = 0.0078, respectively). This synergistic effect resulted in the highest increases in the frequencies of CFSElo and total A2/NY-ESO-1 157–165 tet+ CD8+ T cells (2.6- and 2.0-fold, respectively) as compared with stimulation with IgG control antibody (Fig. 5, D and E). No proliferation of NY-ESO-1 157–165-specific CD8+ T cells was observed after a 6-d IVS with an irrelevant peptide with or without Tim-3 and/or PD-1 blockade (Fig. S3 C).
Figure 5.
Blockade of the Tim-3–Tim-3L pathway alone or in combination PD-1–PD-L1 blockade with prolonged antigen stimulation increases the frequency of proliferating and total NY-ESO-1–specific CD8+ T cells. Representative flow cytometry analysis from two melanoma patients showing percentages of CFSElo A2/NY-ESO-1 157–165 tet+ CD8+ T cells among total CD8+ T cells (A) and pooled data from melanoma patients (n = 9) showing the variation in the numbers of CFSElo (B) and total (C) A2/NY-ESO-1 157–165 tet+ cells for 106 CD8+ T cells. CFSE-labeled PBMCs were incubated for 6 d with NY-ESO-1 157–165 peptide or HIVpol 476–484 peptide and blocking anti–Tim-3 (aTim-3), and/or anti–PD-L1 (aPD-L1) mAbs or an isotype control antibody (IgG). (D and E) Fold change of the frequencies of CFSElo (D) and total (E) A2/NY-ESO-1 157–165 tet+ CD8+ T cells after 6-d IVS with cognate peptide and blocking anti–Tim-3 (aTim-3) and/or anti–PD-L1 (aPD-L1) mAbs (n = 9). The ratio of the percentages of CFSElo and total A2/NY-ESO-1 157–165 tet+ CD8+ T cells in the presence of indicated antibody treatment and isotype control antibody is shown. The p-values were calculated using the Wilcoxon signed rank test. Data shown are representative of two independent experiments performed in duplicate.
DISCUSSION
In this study, we show that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells represent a highly dysfunctional population of tumor-induced T cells in patients with advanced melanoma. We first observed that Tim-3 expression is up-regulated on tumor-induced NY-ESO-1–specific CD8+ T cells and on Flu-specific CD8+ T cells in advanced stage melanoma patients as compared with CMV-specific and EBV-specific effector and effector/memory CD8+ T cells. Strikingly, and in contrast not only to total EBV- and CMV-specific CD8+ T cells but also to Flu-specific CD8+ T cells, the majority of Tim-3+ NY-ESO-1–specific CD8+ T cells up-regulates PD-1 expression. Therefore, unlike virus-specific CD8+ T cells evaluated in our study and HIV-specific CD8+ T cells (Jones et al., 2008), spontaneous Tim-3+ NY-ESO-1–specific CD8+ T cells coexpress PD-1 in patients with advanced melanoma.
One critical finding is that Tim-3+PD1+ NY-ESO-1–specific CD8+ T cells are more dysfunctional than Tim3−PD-1+ and Tim3−PD-1− CD8+ T cells, as they produced significantly less IFN-γ, TNF, and IL-2 ex vivo. We found no significant difference in terms of cytokine production between Tim3−PD-1− and Tim-3−PD-1+ NY-ESO-1–specific CD8+ T cells, suggesting that PD-1 up-regulation alone without Tim-3 up-regulation is not directly associated with T cell dysfunction (i.e., cytokine secretion). This observation is in line with our previous demonstration that PD-1 acts as a regulator of NY-ESO-1–specific CD8+ T cell expansion upon chronic antigen exposure and has no major impact on their functionality on a cell-per-cell basis (Fourcade et al., 2009). In one melanoma patient with very high levels of spontaneous NY-ESO-1–specific CD8+ T cells, we found that Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells produced less cytokines than Tim-3−PD-1− NY-ESO-1–specific CD8+ T cells, suggesting that Tim-3 up-regulation alone by tumor antigen–specific CD8+ T cells defines a group of dysfunctional T cells independently of PD-1 up-regulation. Importantly, Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells produced significantly less cytokines than Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells, supporting Tim-3+PD-1+ CD8+ T cells, as a more dysfunctional population than Tim-3+PD-1− CD8+ T cells. The low frequencies of Tim-3+PD-1− NY-ESO-1–specific CD8+ T cells did not allow us to extend this observation to the other melanoma patients included in our study. Interestingly, one study in mice with chronic persistent infections has shown that coexpression of multiple inhibitory receptors, including PD-1, LAG-3, 2B4, and CD160 by the same virus-specific CD8+ T cells was associated with lower T cell functions (Blackburn et al., 2009). Our findings further add to this observation and support that coexpression of Tim-3 and PD-1 is a marker of tumor-induced T cell dysfunction in patients with advanced melanoma.
We observed that blockade of the Tim-3–Tim-3L pathway ex vivo increased the percentages of NY-ESO-1-specific CD8+ T cells that produced cytokines, supporting the role of the Tim-3 pathway in tumor antigen–specific T cell exhaustion/dysfunction. These findings are in line with one study demonstrating the role of Tim-3 blockade in improving Tim-3+ HIV-specific CD8+ T cell functions (Jones et al., 2008). Although we could not measure the percentages of cytokine-producing Tim-3+ NY-ESO-1–specific CD8+ T cells in wells containing the blocking anti–Tim-3 mAbs, it is tempting to speculate that the increased frequencies of cytokine-producing NY-ESO-1–specific CD8+ T cells occurred only within the Tim-3+ NY-ESO-1–specific CD8+ T cell compartment, which represents a fraction of total NY-ESO-1–specific CD8+ T cells (mean 28.8%) and includes a minority of cytokine-producing cells (mean 8.7 and 4.6% of IFN-γ– and TNF-producing Tim-3+ NY-ESO-1–specific CD8+ T cells among total NY-ESO-1–specific CD8+ T cells, respectively). Several lines of evidence support this assumption. First, the increase of cytokine-producing NY-ESO-1–specific CD8+ T cells was observed only in the presence of blocking anti–Tim-3 mAbs, but not blocking anti–PD-L1 mAbs, suggesting the critical role of the Tim-3–Tim3L pathway. Second, Tim-3 blockade in the presence of cognate peptide did not increase the frequency of cytokine-producing, CMV-specific CD8+ T cells, which express low levels of Tim-3, suggesting that the blockade’s effect requires Tim-3 up-regulation by antigen-specific T cells.
In addition, Tim-3 blockade in combination with prolonged antigen stimulation with cognate peptide increased the frequencies of cytokine-producing, proliferating, and total NY-ESO-1–specific CD8+ T cells, confirming the impact of the Tim-3–Tim-3L pathway on NY-ESO-1–specific T cell dysfunction. Strikingly, we also observed increased percentages of TNF- and IL-2–producing CD8+ T cells among total NY-ESO-1–specific CD8+ T cells, supporting the role of Tim-3 blockade in enhancing NY-ESO-1–specific CD8+ T cell functions on a cell-per-cell basis.
One novel finding is that Tim-3–Tim-3L blockade in combination with PD-1–PD-L1 blockade further increased the frequencies of not only IFN-γ– and TNF- but also IL-2–producing NY-ESO-1–specific CD8+ T cells, as well as the frequencies of proliferating and total NY-ESO-1–specific CD8+ T cells, upon prolonged stimulation with cognate antigen. It is likely that the enhanced capacity of NY-ESO-1–specific CD8+ T cells to produce IL-2 after Tim-3–Tim-3L blockade alone and, to a larger extent, after both Tim-3–Tim-3L and PD-1–PD-L1 blockades contributed to the increased frequencies of proliferating NY-ESO-1–specific CD8+ T cells. Collectively, our data demonstrate a synergistic effect of Tim-3–Tim-3L and PD-1–PD-L1 blockades on NY-ESO-1–specific CD8+ T cell functions.
In summary, our data demonstrate that Tim-3+PD-1+ NY-ESO-1–specific CD8+ T cells represent a highly dysfunctional population of tumor-induced T cells in patients with advanced melanoma. They show that Tim-3–Tim-3L blockade can partially restore NY-ESO-1–specific CD8+ T cell numbers and functions and acts in synergy with PD-1–PD-L1 blockade. Therefore, our data support the use of Tim-3–Tim-3L blockade in association with PD-1–PD-L1 blockade in immunotherapeutic interventions to reverse tumor-induced T cell exhaustion/dysfunction in patients with advanced melanoma. One caveat is the disruption of the Tim-3–Tim-3L pathway appears to contribute to autoimmunity (Koguchi et al., 2006). Therefore, it will be critical to carefully monitor the occurrence of serious autoimmune side effects in vivo.
MATERIALS AND METHODS
Study subjects.
Blood samples were obtained under the University of Pittsburgh Cancer Institute Internal Revue Board–approved protocols 00–079 and 05–140 from 19 HLA-A2+ patients with NY-ESO-1–expressing stage IV melanoma. NY-ESO-1 expression by patients’ tumors was assessed by RT-PCR and immunohistochemistry. All patients had serum NY-ESO-1–specific antibodies detected by ELISA assays. Frequencies of NY-ESO-1–specific CD8+ T cells were assessed ex vivo by flow cytometry using PE-labeled HLA-A2/NY-ESO-1 157–165 tetramers. Nine patients who exhibited spontaneous NY-ESO-1–specific CD8+ T cell responses were included in the study. The percentages of ex vivo detectable NY-ESO-1 157–165–specific CD8+ T cells isolated from patients’ PBMCs ranged from 0.012% to 2.5% of total CD8+ T cells (median 0.03%). PBMCs used in this study were obtained from patients with no prior immunotherapy.
Phenotypic analysis.
CD8+ T lymphocytes were purified from PBMCs of patients and healthy donors using MACS Column Technology (Miltenyi Biotec) and incubated with APC-labeled HLA-A2/NY-ESO-1 157–165, HLA-A2/CMV 495–503, HLA-A2/EBV-BMLF-1 280–288, or HLA-A2/Flu-M 58–66 tetramers. The purity of CD8+ T cells was always >95%. Tetramers were provided by the Ludwig Cancer Institute for Cancer Research, Lausanne branch. As a control for specificity of tetramer staining, we did not observe any positive staining of CD8+ T cells from patients when using an HLA-A2/HIVpol 476–484 tetramer (all patients were HIV sero-negative). The minimum percentage of antigen-specific CD8+ T cells detected ex vivo in patients using these tetramers was 0.010% of total CD8+ T cells. Next, cells were stained with PD-1-FITC or IgG1-FITC (BD), Tim-3-PE (R&D Systems), or IgG2a-PE (BD)–, CD3-ECD–, and CD8-PE-Cy7 (Beckman Coulter)–conjugated antibodies. A violet amine–reactive dye (Invitrogen) was used to assess the viability of the cells. Alternatively, after tetramer labeling, cells were stained with the following conjugated antibodies and reagents: PD-1-FITC, CD8-ECD or CD8-PE-Cy7, HLA-DR-ECD, CD45RO-ECD (Beckman Coulter), CD38-PerCp-Cy5.5, CCR7-biotin (BD), CD28-PerCp-Cy5.5, CD57-biotin (BD), CD45RA-PerCp-Cy5.5, CD27-Alexa750 (eBioscience), and streptavidin-Alexa Fluor 750 (Invitrogen). 2.5 million events were collected during flow cytometric analysis on a FACSAria machine (BD) and analyzed using FlowJo software (Tree Star, Inc.).
Intracellular cytokine staining assay.
For ex vivo cytokine production assays, 2 million purified CD8+ T cells were incubated for 6 h in 10% human serum DME Iscove medium with non-CD3 autologous cells pulsed with HLA-A2–restricted peptides NY-ESO-1 157–165, Flu-M 58–66, CMV 495–503, or HIVpol 476–484 (10 µg/ml) in the presence of 10 µg/ml anti–Tim-3 (clone 2E2) or anti–PD-L1 (16–5983; eBioscience) blocking mAbs or isotype control antibodies (BioLegend). For IVS assays, 5 million PBMCs were incubated for 6 d in culture medium containing 50 IU/ml rhIL-2 (PeproTech) with peptide NY-ESO-1 157–165 or peptide HIVpol 476–484 (10 µg/ml) in the presence of 10 µg/ml anti–Tim-3 and/or anti–PD-L1 blocking mAbs or isotype control antibodies. On day 6, cells were restimulated for 6 h with peptide NY-ESO-1 157–165 or HIVpol 476–484 as control (10 µg/ml). After 1 h of incubation, Brefeldin A (Sigma-Aldrich) was added to the culture medium (10 µg/ml). Cells were then stained with APC-labeled HLA-A2/NY-ESO-1 157–165, HLA-A2/Flu-M 58–66, or HLA-A2 CMV 495–503 tetramers, PD-1-FITC, Tim-3-PE, CD8-Pacific Blue (Invitrogen), CD14-ECD, CD19-ECD, CD56-biotin, and streptavidin-ECD (Beckman Coulter) conjugated antibodies. Intracellular staining was performed with IFN-γ-PE-Cy7, TNF-Alexa Fluor 700 (BD), and IL-2-PerCp-Cy5.5 (BioLegend) antibodies. 2.5 million events were collected during flow cytometric analysis.
CFSE proliferation assay.
5 million CFSE-labeled PBMCs were incubated for 6 d in culture medium containing 50 IU/ml rhIL-2 with peptide NY-ESO-1 157–165 or HIVpol 476–484 (10 µg/ml), in the presence of 10 µg/ml anti–Tim-3 and/or anti–PD-L1 blocking mAbs or isotype control antibodies. On day 6, cells were stained with PE-labeled HLA-A2/NY-ESO-1 157–165 tetramers, CD14-ECD, CD19-ECD, CD56-biotin, streptavidin-ECD, CD8-PE-Cy7, and CD3-PE-Cy5.5 (Invitrogen) conjugated antibodies. 2.5 million events were collected during flow cytometric analysis.
Statistics.
Statistical hypotheses were tested with the Wilcoxon signed rank test (for paired results from the same patient) using SAS v. 9.1. Tests were two-sided, and P ≤ 0.05 was considered significant. Because rank tests are not sensitive to the actual values in a comparison, only to their ranks, differing sets of values can produce identical p-values.
Online supplemental material.
Fig. S1 shows Tim-3 expression on different subsets of mononuclear cells isolated from PBMCs of six melanoma patients and six healthy donors. Fig. S2 depicts the activation and maturational status of Flu-M 58–66–specific CD8+ T cells isolated from PBMCs of melanoma patients. Fig. S3 shows that Tim-3 and PD-1 pathway blockades in the absence of cognate peptide stimulation have no effect on NY-ESO-1–specific CD8+ T cell cytokine production and proliferation. Fig. S4 demonstrates that blockade of the Tim-3/Tim-3L pathway alone or in combination with PD-1/PD-L1 blockade with prolonged antigen stimulation enhances NY-ESO-1–specific CD8+ T cell functionality. Fig. S5 depicts the effect of Tim-3 and PD-1 pathway blockades on PD-1 and Tim-3 expression by NY-ESO-1–specific CD8+ T cells. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20100637/DC1.
Acknowledgments
We thank Dr. Lisa Borghesi and Mr. Dewayne Falkner of the Flow Facility of the University of Pittsburgh, Department of Immunology for their technical support. We thank Drs. Ana Anderson, Lawrence P. Kane, and Daniel Olive for their critical reading of the manuscript. We also thank Ms. Lisa Spano for editorial assistance.
This work was supported by the National Institutes of Health/National Cancer Institute grants RO1CA90360 and RO1CA112198 (to H.M. Zarour) and a grant from the Cancer Research Institute (to H.M. Zarour).
The authors have no conflicting financial interests.
Footnotes
Abbreviations used:
- CGA
- cancer-germline antigen
- Flu
- influenza
- IVS
- in vitro stimulation
- mDC
- myeloid DC
- MFI
- mean fluorescence intensity
- PD-1
- programmed death 1
- PD-L1
- programmed death ligand 1
- Tim-3
- T cell immunoglobulin and mucin-domain–containing molecule 3
References
- Barber D.L., Wherry E.J., Masopust D., Zhu B., Allison J.P., Sharpe A.H., Freeman G.J., Ahmed R. 2006. Restoring function in exhausted CD8 T cells during chronic viral infection. Nature. 439:682–687 10.1038/nature04444 [DOI] [PubMed] [Google Scholar]
- Blackburn S.D., Shin H., Haining W.N., Zou T., Workman C.J., Polley A., Betts M.R., Freeman G.J., Vignali D.A., Wherry E.J. 2009. Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors during chronic viral infection. Nat. Immunol. 10:29–37 10.1038/ni.1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boon T., Coulie P.G., Van den Eynde B.J., van der Bruggen P. 2006. Human T cell responses against melanoma. Annu. Rev. Immunol. 24:175–208 10.1146/annurev.immunol.24.021605.090733 [DOI] [PubMed] [Google Scholar]
- Day C.L., Kaufmann D.E., Kiepiela P., Brown J.A., Moodley E.S., Reddy S., Mackey E.W., Miller J.D., Leslie A.J., DePierres C., et al. 2006. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 443:350–354 10.1038/nature05115 [DOI] [PubMed] [Google Scholar]
- Fourcade J., Kudela P., Andrade Filho P.A., Janjic B., Land S.R., Sander C., Krieg A., Donnenberg A., Shen H., Kirkwood J.M., Zarour H.M. 2008. Immunization with analog peptide in combination with CpG and montanide expands tumor antigen-specific CD8+ T cells in melanoma patients. J. Immunother. 31:781–791 10.1097/CJI.0b013e318183af0b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fourcade J., Kudela P., Sun Z., Shen H., Land S.R., Lenzner D., Guillaume P., Luescher I.F., Sander C., Ferrone S., et al. 2009. PD-1 is a regulator of NY-ESO-1-specific CD8+ T cell expansion in melanoma patients. J. Immunol. 182:5240–5249 10.4049/jimmunol.0803245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden-Mason L., Palmer B.E., Kassam N., Townshend-Bulson L., Livingston S., McMahon B.J., Castelblanco N., Kuchroo V., Gretch D.R., Rosen H.R. 2009. Negative immune regulator Tim-3 is overexpressed on T cells in hepatitis C virus infection and its blockade rescues dysfunctional CD4+ and CD8+ T cells. J. Virol. 83:9122–9130 10.1128/JVI.00639-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas G.G., Jr., D’Cruz O.J., De Bault L.E. 1988. Distribution of human leukocyte antigen-ABC and -D/DR antigens in the unfixed human testis. Am. J. Reprod. Immunol. Microbiol. 18:47–51 [DOI] [PubMed] [Google Scholar]
- Jäger E., Nagata Y., Gnjatic S., Wada H., Stockert E., Karbach J., Dunbar P.R., Lee S.Y., Jungbluth A., Jäger D., et al. 2000. Monitoring CD8 T cell responses to NY-ESO-1: correlation of humoral and cellular immune responses. Proc. Natl. Acad. Sci. USA. 97:4760–4765 10.1073/pnas.97.9.4760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R.B., Ndhlovu L.C., Barbour J.D., Sheth P.M., Jha A.R., Long B.R., Wong J.C., Satkunarajah M., Schweneker M., Chapman J.M., et al. 2008. Tim-3 expression defines a novel population of dysfunctional T cells with highly elevated frequencies in progressive HIV-1 infection. J. Exp. Med. 205:2763–2779 10.1084/jem.20081398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koguchi K., Anderson D.E., Yang L., O’Connor K.C., Kuchroo V.K., Hafler D.A. 2006. Dysregulated T cell expression of TIM3 in multiple sclerosis. J. Exp. Med. 203:1413–1418 10.1084/jem.20060210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandic M., Castelli F., Janjic B., Almunia C., Andrade P., Gillet D., Brusic V., Kirkwood J.M., Maillere B., Zarour H.M. 2005. One NY-ESO-1-derived epitope that promiscuously binds to multiple HLA-DR and HLA-DP4 molecules and stimulates autologous CD4+ T cells from patients with NY-ESO-1-expressing melanoma. J. Immunol. 174:1751–1759 [DOI] [PubMed] [Google Scholar]
- Monney L., Sabatos C.A., Gaglia J.L., Ryu A., Waldner H., Chernova T., Manning S., Greenfield E.A., Coyle A.J., Sobel R.A., et al. 2002. Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature. 415:536–541 10.1038/415536a [DOI] [PubMed] [Google Scholar]
- Petrovas C., Casazza J.P., Brenchley J.M., Price D.A., Gostick E., Adams W.C., Precopio M.L., Schacker T., Roederer M., Douek D.C., Koup R.A. 2006. PD-1 is a regulator of virus-specific CD8+ T cell survival in HIV infection. J. Exp. Med. 203:2281–2292 10.1084/jem.20061496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrovas C., Price D.A., Mattapallil J., Ambrozak D.R., Geldmacher C., Cecchinato V., Vaccari M., Tryniszewska E., Gostick E., Roederer M., et al. 2007. SIV-specific CD8+ T cells express high levels of PD1 and cytokines but have impaired proliferative capacity in acute and chronic SIVmac251 infection. Blood. 110:928–936 10.1182/blood-2007-01-069112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatos C.A., Chakravarti S., Cha E., Schubart A., Sánchez-Fueyo A., Zheng X.X., Coyle A.J., Strom T.B., Freeman G.J., Kuchroo V.K. 2003. Interaction of Tim-3 and Tim-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat. Immunol. 4:1102–1110 10.1038/ni988 [DOI] [PubMed] [Google Scholar]
- Sánchez-Fueyo A., Tian J., Picarella D., Domenig C., Zheng X.X., Sabatos C.A., Manlongat N., Bender O., Kamradt T., Kuchroo V.K., et al. 2003. Tim-3 inhibits T helper type 1-mediated auto- and alloimmune responses and promotes immunological tolerance. Nat. Immunol. 4:1093–1101 10.1038/ni987 [DOI] [PubMed] [Google Scholar]
- Stockert E., Jäger E., Chen Y.T., Scanlan M.J., Gout I., Karbach J., Arand M., Knuth A., Old L.J. 1998. A survey of the humoral immune response of cancer patients to a panel of human tumor antigens. J. Exp. Med. 187:1349–1354 10.1084/jem.187.8.1349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trautmann L., Janbazian L., Chomont N., Said E.A., Gimmig S., Bessette B., Boulassel M.R., Delwart E., Sepulveda H., Balderas R.S., et al. 2006. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nat. Med. 12:1198–1202 10.1038/nm1482 [DOI] [PubMed] [Google Scholar]
- Zhu C., Anderson A.C., Schubart A., Xiong H., Imitola J., Khoury S.J., Zheng X.X., Strom T.B., Kuchroo V.K. 2005. The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat. Immunol. 6:1245–1252 10.1038/ni1271 [DOI] [PubMed] [Google Scholar]