Abstract
This study examined psychosocial factors associated with HIV-risk behavior among Latina women at self-disclosed heterosexual risk for HIV infection. Data were collected via structured interviews for 187 Puerto Rican women, aged 18–35, who attended a health clinic in the Bronx, New York. Over 64% of all participants reported unprotected vaginal sex with primary sexual partners. Higher levels of unprotected vaginal sex were associated with living with the partner, residing with children, current employment, heightened negative mood, and greater social support from the partner. The relationship between increased negative mood and increased unprotected vaginal sex use was mediated by employment, after controlling for educational level, living with the partner, and residing with children. The findings suggest that interventions designed to facilitate HIV-protective behaviors may need to consider that employment may supercede relationship factors among populations of urban women identified at increased heterosexual risk for HIV infection.
Keywords: employment, social support, HIV risk, Latinas
Introduction
Background
Although the total number of annual cases of AIDS has declined over recent years, women continue to represent the fastest growing group of adults infected with HIV (Centers for Disease Control and Prevention [CDC], 1999). AIDS represents the leading cause of death in women of reproductive age, and HIV infection occurs disproportionately in women of color of childbearing age (CDC, 1999). Latina women represented 20% of AIDS cases reported among women through June 1999, and the most common exposure category for Latina women with AIDS was heterosexual contact (63%; CDC, 1999). Among Latinas, the highest rates of reported HIV infection occur among Puerto Rican women who reside in the northeastern United States (CDC, 1999). Although the greater efficiency of male-to-female viral transmission may partially explain the increased vulnerability to risk for heterosexual HIV infection for women in general (Anderson and May, 1988; Friedland and Kline, 1987), Latina women seem less at risk because of their own behavior, but more due to the HIV-risk behavior of their partners, who are more likely to report intravenous drug use (IDU) and having sex with men or multiple partners or both (Carballo-Dieguez and Dolezal, 1996; Choi et al., 1994; Diaz et al., 1994; Dolcini et al., 1995; Marin et al., 1993a,b; Sabogal et al., 1993).
Condom Use
Condom use represents an efficacious means of preventing HIV transmission (Conant et al., 1986; Francis and Chin, 1987; Gielen et al., 1994). However, Latina women, including Puerto Rican women, report low rates or inconsistent condom use (Grella et al., 1995; Harrison et al., 1991; Marin et al., 1993a,b; Moore et al., 1995). In one study, nearly 63% of Puerto Rican women reported never using condoms during vaginal sex with sexual partners (Moore et al., 1995). However, although there exists general acknowledgment about the greater risk of heterosexual infection of HIV among Latina women, very little is known regarding psychosocial correlates of sexual risk taking among Latinas, knowledge which could be targeted for prevention efforts (Carmona-Vargas et al., 1999; Deren et al., 1996; Newcomb et al., 1998; Romero and Arguellas, 1993).
Condom Use and Negative Mood
Research has determined that negative mood correlates with sexual risk behavior in populations other than Latinos, e.g., with demonstrated associations between increased depression and higher concurrent sexual risk practices in gay and bisexual adolescent males (Rotheram-Borus et al., 1995), HIV+ adults, including gay men (Kelly et al., 1993; Robbins et al., 1994), and HIV− women (Morrill et al., 1996; Orr et al., 1994). Heightened psychological distress was associated with more unprotected sex among women of color (Harlow et al., 1998), female sex workers in a syringe exchange program (Paone et al., 1999), and with decreases in adopting and maintaining safer sexual practices among HIV-serodiscordant couples (Skurnick et al., 1998). Also, depression and emotional distress differentiated higher-risk from lower- to moderate-HIV-risk behavior among Black homeless women (Nyamathi, 1992). However, very little research has investigated how negative mood relates to HIV sexual-risk behavior in Latinas, especially Puerto Rican women.
HIV-Risk Behavior and Social Support
Some research suggests that understanding the social context of HIV risk, including gender dynamics that affect common sexual behavior patterns and characteristic correlates of risk taking, remains critical to the development of preventive strategies and interventions (Amaro, 1995; Carmona-Vargas et al., 1999; Miller, 1999; Skurnick et al., 1998). For example, social support networks appear important in maintaining overall psychological and physical health (Broadhead et al., 1983; Cohen, 1988; Cohen and McKay, 1984; Cohen and Syme, 1985; Cohen and Wills, 1985; Dixon et al., 1998, 1999; Leserman et al., 1999; Penninx et al., 1998; Wortman, 1984). In fact, both total and individual components of perceived social support have been associated with lower levels of negative mood, including depression and anxiety (Antoni et al., 1990; Antoni and Schneiderman, 1998; Dixon et al., 2001; Hays et al., 1990, 1992; Kelly et al., 1993; Miller et al., 1997; Namir et al., 1989; Penninx et al., 1998; Turner et al., 1993). However, research investigating social support and HIV sexual-risk behavior reveals inconsistent findings. Although low social support, decreased seeking social support, and dissatisfaction with social support were associated with unprotected anal sex in gay and bisexual men (Dilley et al., 1998; Folkman et al., 1992; Strathdee et al., 1998), and with less condom use in female IDUs in some work (Brown, 1998), other studies have determined that social support was not associated with condom use in female methadone patients (el-Bassel and Schilling, 1994) or unprotected anal sex in gay men (Mayne et al., 1998). With regard to the present study, whereas Latinas are more likely to report family influences on condom use than White or African American women (Grella et al., 1995), the potential impact of social support from family members, husbands or boyfriends, or even friends, remains undetermined.
Marriage and Work
Interestingly, marriage appears to provide paradoxical psychological and physical health effects for women, i.e., by increasing social support and economic advantage, thereby enhancing overall health on the one hand, whereas simultaneously reducing control overpaid versus unpaid work (Ballantyne, 1999; Reviere and Eberstein, 1992). Regarding sexual-risk behavior, among Latino and non-Latino populations, unmarried status has been identified as a correlate of consistent condom use (Harrison et al., 1996; Newcomb et al., 1998), along with higher levels of education (Harrison et al., 1996; Kelly et al., 1995; McCoy and Incardi, 1993; Potter and Anderson, 1993; Strathdee et al., 1998), and being employed (Harrison et al., 1996; McCoy and Incardi, 1993). Regarding current employment, when compared with women who do not work outside of the home, women with external employment appear healthier across numerous physical and psychological health parameters, including fewer sick and hospital days, fewer acute conditions, fewer limitations in activity resulting from chronic conditions, better self-reported health status, and better psychological well-being (Anson and Anson, 1987; Arber, 1991; Elliott and Huppert, 1991; Hibbard and Pope, 1985; Reviere and Eberstein, 1992; Rosenfeld, 1992; Wheeler et al., 1983). However, the relative salience of social support (e.g., from marriage) versus employment remains unknown with regard to HIV sexual-risk behavior, particularly among Latina women.
Conceptual Framework
This study investigated levels of HIV sexual-risk behavior in a sample of Latinas of Puerto Rican ethnicity residing in the northeastern United States. We hypothesized that these women would report relatively high percentages of higher risk-sexual behaviors, such as anal intercourse, as well as relatively low percentages of consistent condom use with their husbands or boyfriends. Moreover, we hypothesized that negative mood would be associated with condom use in this at-risk population. Finally, we investigated the possible associations and specific pathways by which two competing factors—either social support (e.g., from the husband/boyfriend [HBF], family members, or friends) or current employment—may have influenced the association between negative mood and condom use in Puerto Rican women.
Specifically, we tested whether social support or employment represented mediator mechanisms by which either of these influences may have occurred. Because prior work indicates that social support may directly influence mental well-being and health behaviors in general populations (Broadhead et al., 1983; Cohen and Hoberman, 1983; Cohen and McKay, 1984; Cohen and Syme, 1985; Cohen and Wills, 1985), yet reveals inconsistent findings regarding sexual-risk behavior (Brown, 1998; Dilly et al., 1998; el-Balssel and Schilling, 1994; Folkman et al., 1992; Mayne et al., 1998; Strathdee et al., 1998), it is important to evaluate how social support from different sources (family, husbands or boyfriends, friends) may be associated with both negative mood and sexual protective behavior in populations at risk for HIV infection (Grella et al., 1995). Therefore, we hypothesize that social support will mediate the relationship between negative mood and condom use, such that the presence of negative mood may alter perceptions of social support so as to render the individual more vulnerable to failing to engage in self-protective behaviors.
Furthermore, given the health-enhancing benefits of employment for women overall (Anson and Anson, 1987; Arber, 1991; Elliott and Huppert, 1991; Hibbard and Pope,1985; Reviere and Eberstein,1992; Rosenfeld, 1992; Wheeler et al., 1983), we hypothesize that current employment (e.g., via the socioeconomic benefits of working outside the home, an increase in available social support from fellow students, coworkers or supervisors, a sense of self-efficacy, or all of these, LaCroix and Haynes, 1987) will facilitate sexual protective behaviors, such as condom use. Moreover, we propose that employment will mediate the relationship between negative mood and condom use, such that heightened depressed mood may alter whether women access (participate in) current employment, which may then influence condom use.
Thus, the study reported herein tests two different mediator models: hypothesis 3 (social support as a mediator); hypothesis 4 (employment as a mediator); each model proposing different pathways by which either social support or employment may influence the impact of negative mood on condom use in Puerto Rican women identified at heterosexual risk for HIV infection. We propose that the development of an appropriate model would facilitate the identification of potential factors specific to HIV-related sexual health to target for prevention and intervention strategies among at-risk populations.
Methods
Procedure
This study represented a component of a larger investigation funded through a cooperative agreement with the CDC (Atlanta, Georgia), which investigated HIV risk factors related to sexual decision making among Puerto Rican women who resided in the Bronx, New York, from 1994 to 1995. Potential participants were recruited from the waiting room of a primary health care community center located in the Bronx, New York. This public sector facility was chosen due to the comparability with other health care facilities in New York City regarding the provision of services such as annual gynecological exams, pediatric care, treatment for general health concerns, and collection of WIC certificates. The study interviewer determined the eligibility of the potential study participant, briefed the woman about the study intent and details, and then asked the woman to participate. Prior experience within similar settings revealed that disproportionate numbers of potential participants refused to participate in research studies that required written consent (Harrison et al., 1991). Therefore, verbal, rather than signed consent to participate was used so that there would be no record of participants' names. The face-to-face interview required approximately 45–90 min to complete. Interviewers were Puerto Rican women who lived in the Bronx and who were fluent in Spanish. Participants were provided with a choice to conduct the interview in Spanish or English. All except one participant elected to conduct the interview in English. The translation procedures for the study instruments have been described in detail elsewhere (Moore et al., 1995). All study participants received $30.00 cash upon completion of the semi-structured interview. No further contact with respondents occurred following participation in the study.
Participants
Interviewers approached a total of 258 women to participate in a study investigating sexual behavior in young women. Only those women who were Puerto Rican, between the ages of 18 and 35, reported being in a heterosexual relationship for at least 1 year and having vaginal sex with that partner during the 6 months prior to the screening process were recruited. These women could not have been currently pregnant, were more than 6 months postpartum, and were required to have no lifetime history of injecting drug use. This last criterion was used to help focus the investigation on heterosexual risk factors for HIV infection. Twenty-three refused to undergo the screening procedure for the study. Forty-five women failed to meet eligibility for the study, and 8 were unable to complete screens, leaving a total of 187 participants.
Measures
Developing Interview Measures
The Centers for Disease Control and Prevention developed the structured interview measurements used for this research project and used focus groups conducted with Puerto Rican women to determine the appropriateness of the initial research questions (Moore et al., 1995). Study interviewers, who represented part of the local Hispanic community, participated in the finalization of survey items for the current study.
Negative Mood
Negative mood was measured using 7 items each from the Tension–Anxiety and Depression–Dejection subscales of the Profile of Mood States (POMS; McNair et al., 1992), a scale that measures subjective mood or affective states. Participants rated the extent to which they had been experiencing that mood for the past month along a 4-point Likert scale ranging from 0 (Never/Rarely) to 3 (Almost Always). Negative items were reversed and then summed with positive items in order to provide a total negative mood score (possible range of scores = 0–42; α = .70). Both the total scale and subscales of the POMS have demonstrated adequate reliability and validity (McNair et al., 1992).
Social Support
Social support was measured using subscales from the Source-Specific Social Provisions Scale (SS-SPS; Cutrona, 1989), a self-report scale that measures perceived source-specific social support across several areas, and from the Interpersonal Support Evaluation List (ISEL; Cohen and Hoberman, 1983), adapted in style similar to the SS-SPS. Subscales selected for this study assessed participants' perception of guidance (advice, information) and tangible (monetary aid, assistance) social support, with total social support representing the sum of all items (7 total) across these two subscales. These support dimensions have been shown to represent the best predictors of psychological and physical health outcomes in HIV+ gay men (e.g., Cruess et al., 2000; Dixon et al., 1998, 1999; Lutgendorf et al., 1998). Participants evaluated the extent to which each of the provisions of social support was currently available along a 3-point Likert scale (0: No, 1: Sometimes, 2: Yes). For each question, participants were asked to name a maximum of four people who were available to them to provide each type of support, e.g., “Would someone have been available to babysit if you needed to leave your children overnight?” Amount of Source-Specific Social Support was determined by first coding each response as “family,” “husband or boyfriend,” “friend or neighbor,” “religious minister,” or “other (nonspecified)” source of social support. Next, all items were summed within each coded source of support (possible range of scores for “husband or boyfriend” = 0–7; “family,” “friend or neighbor,” “religious minister,” or “other (nonspecified)” = 0–28). As a data reduction strategy, we examined each variable for the assumptions of normality prior to entry into the univariate and multivariate analyses. As a result, we retained only total social support from the “husband or boyfriend,” “family,” and “friends” as source-specific social support variables. Both the total scale and the subscales of the SS-SPS and ISEL have demonstrated adequate reliability and validity (Cohen and Hoberman, 1983; Cutrona, 1989).
Sexual Activities and Condom Use
First, participants rated their frequency of participation in vaginal sex, anal sex, or both with their husbands or boyfriends during the 6 months prior to the interview on a 6-point Likert scale ranging from 0 (Never/None) to 5 (More than once a day, Almost every day). Next, participants rated their frequency of condom use during vaginal and anal intercourse during the same 6-month time-period along the following 5-point scale: 0: Never; 1: Less than half the time; 2: About half the time; 3: More than half the time; and 4: Always. The dimensions of greater unprotected vaginal and anal sex were operationalized with lower scores obtained for these “frequency of condom use” items. Finally, due to the approximately bimodal distribution of the raw data, we collapsed each condom use item into ordinal trichotomous variables (0: Never; 1: Sometimes; 2: Always).
Background and Control Variables
Background variables included age, educational level, religious affiliation, living arrangements (live with husband or boyfriend, reside with children), and marital status. In addition, in order to assess perceived risk for HIV infection as a potential control variable, participants were asked to rate their chance of getting HIV from their husband or boyfriend on a 4-point Likert scale ranging from 0 (No chance) to 3 (Good chance). Finally, because this investigation focused on condom use as a self-protective behavior, we considered that participants who were currently trying to get pregnant would represent a potential serious confound. Therefore, we asked participants if they had been trying to get pregnant (0: No or 1: Yes).
Results
Sample Characteristics
Our sample ranged in demographic and psychosocial characteristics, as indicated in Tables I and II. One hundred eighty-seven participants completed face-to-face structured interviews. The mean age of participants was 27.03 (SD = 5.04). The majority of these women indicated at least a high school education. Thirty-nine reported that they were employed outside of the home. Approximately two thirds of the women reported at least some chance that they would get HIV from their husbands or boyfriends. The majority of women (91.4%) reported that they were not trying to get pregnant. All participants reported vaginal intercourse, with the majority reporting unprotected vaginal sex with their partner during the 6 months prior to the interview. Of the proportion of women reporting anal sex (24.7%), approximately half indicated that they never used condoms with their partner. Finally, although the lack of standardization norms restricted comparisons, the sample fell in the middle range of scores for negative mood, and the low to middle range of scores for total social support from either the husband/boyfriend, friends, or family members.
Table I.
Description of the Sample
| Variable | M | SD | Percent (%) |
|---|---|---|---|
| Age | 27.03 | 5.04 | |
| Trying to get pregnant | 8.6 | ||
| Education | |||
| Less than 8th grade, no GED | 3.7 | ||
| Some high school, no GED | 29.4 | ||
| High school graduate or GED | 35.3 | ||
| Some college | 25.7 | ||
| College degree | 5.9 | ||
| Religious affiliation | |||
| Catholic | 83.8 | ||
| Protestant | 8.4 | ||
| Other | 1.0 | ||
| None | 6.8 | ||
| Living arrangementsa | |||
| Live with husband/boyfriend | 51.9 | ||
| Live with parents (hers, his, or both) | 22.0 | ||
| Children live with | 74.9 | ||
| Live with roommate or friend | 7.3 | ||
| Other | 10.4 | ||
| Marital status | |||
| Married/Living together | 32.1 | ||
| Separated/Divorced | 12.3 | ||
| Single | 55.6 | ||
| Perceived risk variable | |||
| At least some perceived chance will get HIV from husband or boyfriend | 69.7 |
Multiple potential living arrangements cause percentages to total more than 100%.
Table II.
Descriptive Statistics for Predictor and Outcome Variables
| Variable | Percent (%) | M | SD |
|---|---|---|---|
| Negative mood (Range 3–37) | 18.62 | 6.38 | |
| Total social support from… | |||
| Husband or boyfriend (Range 0–7) | 1.97 | 2.36 | |
| Family members (Range 0–19) | 6.24 | 4.02 | |
| Friends (Range 0–6) | 2.16 | 2.56 | |
| Employment | |||
| Regular or occasional full- or part-time work | 61.0 | ||
| Not working outside the home | 39.0 | ||
| Frequency of vaginal sex w/HBF (N = 187) | |||
| Less than 4×/month | 10.8 | ||
| About 1×/week | 29.0 | ||
| 2 to 6×/week | 34.4 | ||
| About 1×/day | 11.3 | ||
| More than 1×/day, almost every day | 14.0 | ||
| Frequency of anal sex w/HBF (N = 46) | |||
| Less than 4×/month | 71.7 | ||
| About 1×/week | 8.7 | ||
| 2 to 6×/week | 4.3 | ||
| About 1×/day | 8.7 | ||
| More than 1×/day, almost every day | 4.3 | ||
| Condom use during vaginal sex past 6 months (N = 187) | |||
| Never | 40.9 | ||
| Sometimes | 23.7 | ||
| Always | 35.5 | ||
| Condom use during anal sex past 6 months (N = 46) | |||
| Never | 48.9 | ||
| Sometimes | 20.0 | ||
| Always | 31.1 |
Relationships Among Control, Predictor, and Outcome Variables
The relationships among the control, predictor, and outcome variables are presented in Table III. Social support from the husband or boyfriend was the only source of social support associated with condom use, and only for vaginal sex. Greater unprotected vaginal sex was associated with lower educational level, residing with the husband or boyfriend, children living with the respondent, a lack of employment, heightened negative mood, and greater social support from the husband or boyfriend. Greater unprotected anal sex was associated with lower educational level and condom use during vaginal sex. Although lack of space prevented the display of all associations, there were no significant relationships between condom use and age, religious affiliation, other living arrangements, marital status, social support from family members or friends, trying to get pregnant, or the perceived risk variable.
Table III.
Correlations Among Control, Predictor, and Outcome Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Level of education | — | .03 | −.18** | −.14 | .40*** | .11 | .06 | .18* | −.24*** | .27*** | .31* |
| 2. Live with HBF | — | .27*** | −.04 | .02 | −.07 | −.03 | .17** | .03 | −.38*** | −.14 | |
| 3. Children live with | — | .07 | −.25*** | −.03 | −.07 | −.04 | .15* | −.19** | −.22 | ||
| 4. Perceived risk | — | −.08 | −.06 | −.01 | −.16* | .26*** | −.03 | .07 | |||
| 5. Employment | — | .01 | −.06 | .05 | −.26*** | .28*** | .01 | ||||
| 6. Soc support-FAM | — | −.01 | .06 | −.02 | .09 | .09 | |||||
| 7. Soc support-FRD | — | .05 | −.02 | −.10 | −.12 | ||||||
| 8. Soc support-HBF | — | −.13 | −.21** | −.06 | |||||||
| 9. Negative mood | — | −.20** | −.11 | ||||||||
| 10. Condom-vaginal | — | .44** | |||||||||
| 11. Condom-anal | — |
Note. Live with HBF = Live with husband or boyfriend; Children live with = Live with children; Perceived risk = perceived chance that will get HIV from HBF; Employment = Regular or occasional full- or part-time work; Soc support-FAM = Social support from family members; Soc support-FRD = Social support from friends; Soc support-HBF = Social support from husband or boyfriend; Condom-vaginal = Condom use during vaginal sex during the past 6 months; Condom-anal= Frequency of condom use during anal sex during the past 6 months (N = 24).
p = .05, 2-tailed.
p = .01, 2-tailed.
p = .001, 2-tailed.
Mediators of Condom Use
Social Support as a Mediator (Hypothesis 3)
We examined whether social support from the husband/boyfriend, friends, or family members mediated the relationship between negative mood (predictor) and condom use (criterion) during vaginal sex. However, each of these variables failed to meet our first criteria, that all three variables (predictor, outcome, and mediator) demonstrate significant correlations with one another. Therefore, social support from the husband or boyfriend, friends, or family members failed to mediate the relationship between negative mood and condom use. Instead, post hoc analyses revealed that there remained significant independent associations when negative mood (β = −.16; p < .05) and social support from the husband or boyfriend (β = −.18; p < .01) were regressed against condom use, after controlling for educational level, residing with the husband or boyfriend, and children living with the respondent (Fchange[2,180] = 5.48; p < .01).
Employment as a Mediator (Hypothesis 4)
Next, we examined whether employment mediated the relationship between negative mood (predictor) and decreased condom use (criterion) during vaginal sex. Employment met our first criteria, that all three variables (predictor, outcome, and mediator) demonstrated significant correlations with one another. While controlling for educational level, residing with the husband or boyfriend, and children living with the respondent, we entered next employment into the equation, followed by negative mood (predictor), all regressed against condom use during vaginal sex (outcome). Employment was considered a mediator if the beta weight of the previously significant negative mood × condom use association became nonsignificant (p > .05) after including the mediator variable into the overall regression equation.
We found that employment mediated the association between increased negative mood and decreased condom use during vaginal sex, after controlling for educational level, residing with the husband or boyfriend, and children living with the participant. The path diagram for this relationship is presented in Fig. 1. As can be seen, the beta weight between negative mood and condom use during vaginal sex was significant (β = −.21; p < .01), but became nonsignificant (β = −.09; ns) when employment was entered into the regression. The beta weight between employment and condom use during vaginal sex was significant before (β = .28; p < .001), and retained significance after negative mood was entered into the regression (β = .18; p < .05). The equation was significant (Fchange[5,175] = 13.38; p < .001), and the incremental variance contributed by employment (sr2 = .03; p < .05) indicated that this employment accounted for a significant proportion of unique variance in condom use during vaginal sex.
Fig. 1.
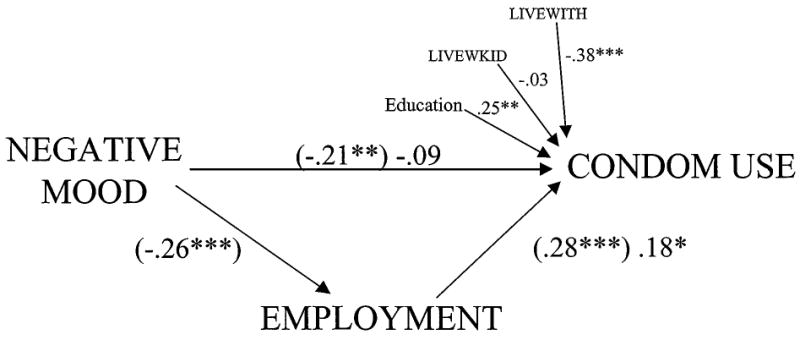
Path diagram for model testing Employment as a mediator of the association between Negative Mood and Condom Use. All equations controlled for Educational Level, Residing with Children, and Residing with Husband or Boyfriend. Standardized β weights for factors entered in model individually are within parentheses, and standardized β weights with all factors in the diagram entered simultaneously are outside parentheses. Significant relationships are indicated by single (p < .05), double (p < .01), or triple (p < .001) asterisks. EMPLOYMENT = Regular or occasional full- or part-time work; LIVEWITH = Reside with Husband or Boyfriend; LIVEWKID = Reside with Children; CONDOM USE = Frequency of condom use during vaginal sex over the past 6 months.
Discussion
This study investigated the impact of psychosocial factors on HIV sexual risk behavior among Puerto Rican women self-identified at heterosexual risk for HIV infection. The finding that 24% of this sample reported anal intercourse, and only one third of those women reported consistent condom use during this higher-risk activity during the past 6 months was striking, and supported our first hypothesis. Taken together, these findings may partially explain the noted increased risk for HIV infection via heterosexual contact among some populations of Latina women (Anderson, 1995; CDC, 1999; Flack et al., 1995; Gwinn et al., 1991; Johnson et al., 1995; Neal et al., 1997), and appear to corroborate past research, which found that Latina women reported low or inconsistent condom use with their primary partners (Dolcini et al., 1995; Galavotti et al., 1995; Marin et al., 1993a,b; McCoy and Inciardi, 1993; Moore et al., 1995; Potter and Anderson, 1993; Wilson et al., 1996). However, we did not find associations between condom use and social support from family members, as has been reported by others (Grella et al., 1995).
Although the finding that the majority of women in this study endorsed at least some level of perceived risk regarding contracting HIV from their husbands or boyfriends, nearly half reported that they never used condoms during vaginal sex appeared consistent with past research in this area (Eversley et al., 1993; Sikkima et al., 1996; Somlai et al., 1998; Woodhouse et al., 1994). Kalichman and Stevenson (1997) have suggested that women who accurately perceived themselves at increased risk for HIV infection, yet reported lower condom use, may have been forced or coerced into unwanted sex. However, we did not find associations between perceived risk and condom use during either vaginal or anal sex, nor was this study designed to investigate the potential impact of coercion on condom use. Alternative potential explanations for this finding may relate to observations by others that the ability of Latinas to protect their sexual health remains challenged by traditional Latina gender role proscriptions that not only emphasize the importance of sustaining relationships while sacrificing personal needs (Wyatt, 1992), but also condone female submissiveness and subservience to partners regarding sexual decision-making (Amaro, 1988).
The findings from our study supported our second hypothesis, that increased negative mood was associated with decreased condom use during vaginal sex. This finding supported prior research investigating associations between psychological distress and HIV sexual risk behavior (Harlow et al., 1998; Kelly et al., 1993; Morrill et al., 1996; Orr et al., 1994; Robbins et al., 1994; Rotheram-Borus et al., 1995), and extended these findings to Puerto Rican women. However, our study failed to support our third hypothesis, because social support from the husband or boyfriend, family members, or friends, failed to mediate the relationship between increased negative mood and decreased condom use. Instead, increased social support from the husband or boyfriend was independently associated, along with negative mood, with decreased condom use, after controlling for educational level, residing with the husband or boyfriend, and children living with the respondent. Although the majority of women reported increased vulnerability to heterosexual HIV infection, and were therefore in great need of maximizing their social and personal resources, they were seemingly adversely affected by relying on their partners for social support in the form of tangible aid and guidance. Thus, the perception of relying on a sexual partner for advice, money, help with child-care, or other forms of assistance may have created a context for the relationship that included some level of dependence on the male partner. Interestingly, these findings appear to corroborate observations that economic disadvantage and strong cultural gender norms seem to exacerbate HIV-risk behavior among Latina women (Amaro, 1995; Gomez et al., 1999; Wyatt, 1994). These authors argue for the importance of addressing broader social and cultural norms toward increasing skills necessary for enhanced HIV protective behavior among women of color.
In our model, employment was predicted to mediate the relationship between negative mood and condom use, transmitting the effect of negative mood onto condom use. In fact, our findings appeared to support our fourth hypothesis, in that current employment mediated the relationship between increased feelings of depression and anxiety and decreased condom use during vaginal sex. In other words, heightened negative mood appeared to influence whether women engaged in employment in a way that then influenced condom use. This finding corroborated previous research in this area, which determined that not being employed was strongly associated with decreased condom use (Harrison et al., 1991; Kelly et al., 1995; McCoy and Inciardi, 1993; Potter and Anderson, 1993), and extended these findings to consider the role that negative mood may play in explaining this association among urban Puerto Rican women.
A few caveats are in order: First, the cross-sectional data available from this study limits the validity of inferences about potential causal directions between the independent and dependent variables. For example, it was quite possible that decreased condom use, within a context of ongoing perception of risk for HIV infection from the sexual partner, created psychological distress, rather than the other way around. The findings could also be interpreted as follows: employed Latina women may have experienced less feelings of psychological distress that would place them at increased risk for more unprotected vaginal sex. This study did not determine complete sexual histories from the respondents, including the number of lifetime primary and nonprimary sexual partners, lifetime experience with condoms, age of initiation into sexual activities, lifetime overall sexual experience, serial monogamous, concurrent multiple sexual partners, or a combination of these. Also, this study derived results from a population of Latina women of Puerto Rican ethnicity who resided in an urban center of the northeastern United States who indicated sexual activity during the past year, who denied any history of injecting drug use, and the majority of whom were not trying to get pregnant. Therefore, these findings should not be generalized to Puerto Rican women in New York, given that this was a small and nonrepresentative sample. Moreover, one cannot generalize these findings to Latinas of non-Puerto Rican ethnicity, non-Hispanic populations, HIV-infected individuals, and other populations, such as elderly persons, homosexuals, drug-involved individuals or individuals who reside in rural or suburban areas outside of the northeastern United States, to name a few examples. Finally, the sexual protective behavior in this study may have been influenced by factors not assessed, such as male partner characteristics, e.g., his willingness (or lack thereof) to use condoms during vaginal sex.
Nonetheless, the results from the current investigation include direct applications for empirically targeted interventions to promote specific AIDS-preventive behaviors in populations self-identified at increased risk for HIV infection. Designed interventions should consider the influence created by an interaction between demographic, social, and relationship factors on sexual risk behavior while considering potential “toxic” effects of social support from the primary sexual partner. For example, Puerto Rican women who are unemployed, poorly educated, and reside with their children, sexual partners, or both, and who rely on their partner for guidance and tangible assistance appear less likely to use condoms, even if they believe that the behavior of their sexual partner places them at increased risk for HIV infection. These women may require a different intervention approach for HIV risk reduction than women who live independently, work outside of their home, and have higher levels of education. For example, clinical interventions may need to introduce the concept of employment outside of the home as a potential risk-reduction factor, as well as to reframe attributions of condom use as demonstrations of feelings of affection, loyalty, concern, and consideration for intimate sexual partners. Future research should use larger sample sizes and longitudinal designs to replicate the findings of this investigation with other populations vulnerable to HIV infection from sexual partners, in order to develop appropriate prevention and intervention strategies.
References
- Amaro H. Considerations for prevention of HIV infection among Hispanic women. Psychology of Women Quarterly. 1988;12:429–443. [Google Scholar]
- Amaro H. Love, sex, and power: Considering women's realities in HIV prevention. American Psychologist. 1995;50:437–447. doi: 10.1037//0003-066x.50.6.437. [DOI] [PubMed] [Google Scholar]
- Anderson NB. Behavioral and sociocultural perspectives on ethnicity and health: Introduction to the special issue. Health Psychology. 1995;14:589–591. [PubMed] [Google Scholar]
- Anderson RM, May RM. Epidemiological parameters of HIV transmission. Nature. 1988;333:514–522. doi: 10.1038/333514a0. [DOI] [PubMed] [Google Scholar]
- Anson O, Anson J. Women's health and labour force status: An enquiry using a multi-point measure of labour force participation. Social Science and Medicine. 1987;25:57–63. doi: 10.1016/0277-9536(87)90207-3. [DOI] [PubMed] [Google Scholar]
- Antoni MH, Schneiderman N. HIV and AIDS. In: Bellack AS, Hersen M, editors. Comprehensive clinical psychology. New York: Pergamon; 1998. pp. 238–275. [Google Scholar]
- Antoni MH, Goodkin K, Goldstein V, LaPerriere A, Ironson G, Fletcher M, Schneiderman N. Coping responses to HIV-1 serostatus notification predict short-term affective distress and one-year immunologic status in HIV-1 seronegative and seropositive gay men. Psychosomatic Medicine. 1990;53:227. [Google Scholar]
- Arber S. Class, paid employment and family roles: Making sense of structural disadvantage, gender and health status. Social Science and Medicine. 1991;32:425–436. doi: 10.1016/0277-9536(91)90344-c. [DOI] [PubMed] [Google Scholar]
- Ballantyne PJ. The social determinants of health: A contribution to the gender differences in health and illness. Scandinavian Journal of Public Health. 1999;27:290–295. [PubMed] [Google Scholar]
- Broadhead WE, Kaplan B, James S, Wagner E, Schoenbach U, Grimson R, Heyden S, Tibblin G, Gehlbach S. The epidemiologic evidence for a relationship between social support and health. American Journal of Epidemiology. 1983;117:521–537. doi: 10.1093/oxfordjournals.aje.a113575. [DOI] [PubMed] [Google Scholar]
- Brown EJ. Female injecting drug users: Human immunodeficiency virus risk behavior and intervention needs. Journal of Professional Nursing. 1998;14:361–369. doi: 10.1016/s8755-7223(98)80078-1. [DOI] [PubMed] [Google Scholar]
- Carballo-Dieguez A, Dolezal C. HIV risk behaviors and obstacles to condom use among Puerto Rican men in New York City who have sex with men. American Journal of Public Health. 1996;86:1619–1622. doi: 10.2105/ajph.86.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmona-Vargas J, Romero GJ, Loeb RB. The impact of HIV status and acculturation on Latinas' sexual risk taking. Cultural Diversity and Ethnic Minority Psychology. 1999;5:209–221. [Google Scholar]
- Centers for Disease Control and Prevention, Department of Health and Human Services, National Center for HIV, STD and TB Prevention. HIV/AIDS Surveillance Report, US HIV and AIDS cases reported through June 1999. Vol. 11. Atlanta, Georgia: 1999. [Google Scholar]
- Choi KH, Catania JA, Dolcini MM. Extramarital sex and HIV risk behavior among US adults: Results from the national AIDS behavioral study. American Journal of Public Health. 1994;84:2003–2007. doi: 10.2105/ajph.84.12.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S, McKay G. Social support, stress, and the buffering hypothesis: A theoretical analysis. In: Baum A, Taylor SE, Singer JE, editors. Handbook of psychology and health. Vol. 4. Hillsdale, NJ: Erlbaum; 1984. pp. 253–267. [Google Scholar]
- Cohen S, Syme S, editors. Social support and health. New York: Academic press; 1985. [Google Scholar]
- Cohen S, Wills T. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Conant M, Hardy D, Sernatinger J, Spicer D, Levy JA. Condoms prevent transmission of AIDS-associated retrovirus. Journal of the American Medical Association. 1986;255:1706. [PubMed] [Google Scholar]
- Cruess S, Antoni MH, Kilbourn K, Ironson G, Klimas N, Fletcher MA, Baum A, Schneiderman N. Optimism, distress and immunologic status in HIV-infected gay men following Hurricane Andrew. International Journal of Behavioral Medicine. 2000;7:160–182. [Google Scholar]
- Cutrona CE. Ratings of social support by adolescents and adult informants: Degree of correspondence and prediction of depressive symptoms. Journal of Personality and Social Psychology. 1989;57:723–730. doi: 10.1037//0022-3514.57.4.723. [DOI] [PubMed] [Google Scholar]
- Deren S, Sanchez J, Shedlin M, Davis WR, Beardsley M, Des Jarlais D, Miller K. HIV risk behaviors among Dominican brothel and street prostitutes in New York City. AIDS Education and Prevention. 1996;8:444–456. [PubMed] [Google Scholar]
- Diaz T, Chu SY, Conti L, Sorvillo F, Caeca PJ, Hermann P. Risk behaviors of persons with heterosexually acquired HIV infection in the United States: Results of a multistate surveillance project. Journal of Acquired Immune Deficiency Syndromes. 1994;7:958–963. [PubMed] [Google Scholar]
- Dilly JW, McFarland W, Sullivan P, Discepola M. Psychosocial correlates of unprotected anal sex in a cohort of gay men attending an HIV-negative support group. AIDS Education and Prevention. 1998;10:317–326. [PubMed] [Google Scholar]
- Dixon D, Antoni M, Kilbourn K, Wagner S, Schneiderman N, Klimas N, Fletcher MA. Social support buffers PTSD symptoms and HHV-6 antibody tiers in HIV+ gay men following Hurricane Andrew. NeuroImmunoModulation. 1998;5:15. [Google Scholar]
- Dixon D, Antoni M, Wagner S, Kilbourn K, Schneiderman N, Klimas N, Fletcher MA. Acute and sustained effects of anxiety on immune status and social support in HIV+ gay men following Hurricane Andrew. NeuroImmunoModulation. 1999;6:214. [Google Scholar]
- Dixon DA, Cruess S, Kilbourn K, Klimas N, Fletcher MA, Ironson G, Baum A, Schneiderman N, Antoni M. Social support mediates the relationship between loneliness and Human Herpsesvirus-6 antibody titers in HIV+ gay men following Hurricane Andrew. Journal of Applied Social Psychology. 2001;31(6):1111–1132. doi: 10.1111/j.1559-1816.2001.tb02665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolcini MM, Coates TJ, Catania JA, Kegeles SM, Hauck WW. Multiple sexual partners and their psychosocial correlates: The population-based AIDS in multiethnic neighborhoods (AMEN) study. Health Psychology. 1995;14:22–31. doi: 10.1037//0278-6133.14.1.22. [DOI] [PubMed] [Google Scholar]
- el-Bassel N, Schilling RF. Social support and sexual risk taking among women on methadone. AIDS Education and Prevention. 1994;6:506–513. [PubMed] [Google Scholar]
- Elliott BJ, Huppert FA. In sickness and in health: Associations between physical and mental well-being, employment and parental status in a British nationwide sample of married women. Psychological Medicine. 1991;21:515–524. doi: 10.1017/s0033291700020626. [DOI] [PubMed] [Google Scholar]
- Eversley RB, Newstetter A, Avins A, Beirnes D, Haynes-Sanstad K, Hearst N. Sexual risk and perception of risk for HIV infection among multiethnic family planning clients. American Journal of Preventive Medicine. 1993;9:92–95. [PubMed] [Google Scholar]
- Flack JM, Amaro H, Jenkins W, Kunitz S, Levy J, Mixon M, Yu E. Behavioral and sociocultural perspectives on ethnicity and health: Panel I: Epidemiology of minority health. Health Psychology. 1995;14:592–600. doi: 10.1037//0278-6133.14.7.592. [DOI] [PubMed] [Google Scholar]
- Folkman S, Chesney MA, Pollack L, Phillips C. Stress, coping, and high-risk sexual behavior. Health Psychology. 1992;11:218–222. doi: 10.1037//0278-6133.11.4.218. [DOI] [PubMed] [Google Scholar]
- Francis DP, Chin J. The prevention of acquired immunodeficiency syndrome in the United States: An objective strategy for medicine, public health, business, and the community. Journal of the American Medical Association. 1987;257:1357–1366. [PubMed] [Google Scholar]
- Friedland GH, Klein RS. Transmission of the human immunodeficiency virus. New England Journal of Medicine. 1987;317:1125–1135. doi: 10.1056/NEJM198710293171806. [DOI] [PubMed] [Google Scholar]
- Galavotti C, Cabral RJ, Lansky A, Grimley DM, Riley GE, Prochaska JO. Validation of measures of condom and other contraceptive use among women at high risk for HIV infection and unintended pregnancy. Health Psychology. 1995;14:570–578. doi: 10.1037//0278-6133.14.6.570. [DOI] [PubMed] [Google Scholar]
- Gielen AC, Faden RR, O'Campo P, Kass N, Anderson J. Women's protective sexual-behaviors: A test of the health belief model. AIDS Education and Prevention. 1994;6:1–11. [PubMed] [Google Scholar]
- Gomez CA, Hernandez M, Faigeles B. Sex in the New World: An empowerment model of HIV prevention in Latina immigrant women. Health, Education and Behavior. 1999;26:200–212. doi: 10.1177/109019819902600204. [DOI] [PubMed] [Google Scholar]
- Grella CE, Annon JJ, Anglin MD. Ethnic differences in HIV risk behaviors, self-perceptions, and treatment outcomes among women in methadone maintenance treatment. Journal of Psychoactive Drugs. 1995;27:421–433. doi: 10.1080/02791072.1995.10471706. [DOI] [PubMed] [Google Scholar]
- Gwinn M, Pappaioanou M, Geeorge J, Hannon W, Wasser S, Redus M, Hoff R, Grady G, Willoughby A, Novello A, Peterson L, Dondero T, Curran J. Prevalence of HIV infection in childbearing women in the United States. Journal of the American Medical Association. 1991;265:1704–1708. [PubMed] [Google Scholar]
- Harlow LL, Rose JS, Morokoff PJ, Quina K, Mayer K, Mitchell K, Schnoll R. Women HIV sexual risk takers: Related behaviors, interpersonal issues, and attitudes. Womens Health. 1998;4:407–439. [PubMed] [Google Scholar]
- Harrison JS, Norris FH, Kay KL, Dixon D, Peters M, Moore J. Heterosexual risk for HIV among Puerto Rican women: Does power influence self-protective behavior?. Paper presented at the Eleventh International Conference on AIDS; Vancouver, British Columbia, Canada. 1996. [Google Scholar]
- Harrison DF, Wambach KG, Byers JB, Imershein AW, Levine P, Maddox K. AIDS knowledge and risk behaviors among culturally diverse women. AIDS Education and Prevention. 1991;3:79–89. [PubMed] [Google Scholar]
- Hays RB, Chauncey S, Tobey L. The social support networks of gay men with AIDS. Journal of Community Psychology. 1990;18:374–385. [Google Scholar]
- Hays RB, Turner H, Coates TJ. Social support, AIDS-related symptoms, and depression among gay men. Journal of Consulting and Clinical Psychology. 1992;60:463–469. doi: 10.1037//0022-006x.60.3.463. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Pope CR. Employment status, employment characteristics and women's health. Women and Health. 1985;10:59–77. doi: 10.1300/J013v10n01_05. [DOI] [PubMed] [Google Scholar]
- Johnson KW, Anderson NB, Bastida E, Kramer BJ, Williams D, Wong M. Behavioral and sociocultural perspectives on ethnicity and health: Panel II: Macrosocial and environmental influences on minority health. Health Psychology. 1995;14:601–612. doi: 10.1037//0278-6133.14.7.601. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Stevenson LY. Psychological and social factors associated with history of risk for human immunodeficiency virus infection among African-American inner-city women. Journal of Women's Health. 1997;6:209–217. doi: 10.1089/jwh.1997.6.209. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Bahr GR, Koob JJ, Morgan MG, Kalichman SC, Stevenson LY, Brasfield TL, Bernstein BM, St Lawrence JS. Factors associated with severity of depression and high-risk sexual behavior among persons diagnosed with human immunodeficiency virus (HIV) infection. Health Psychology. 1993;12:215–219. doi: 10.1037//0278-6133.12.3.215. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Sikkema KJ, Winett RA, Solomon LJ, Roffman RA, Heckman TG, Stevenson LY, Perry MJ, Norman AD, Desiderato LJ. Factors predicting continued high-risk behavior among gay men in small cities: Psychological, behavioral, and demographic characteristics related to unsafe sex. Journal of Consulting and Clinical Psychology. 1995;63:101–107. doi: 10.1037//0022-006x.63.1.101. [DOI] [PubMed] [Google Scholar]
- LaCroix AZ, Haynes SG. Gender differences in the health effects of workplace roles. In: Barnett RC, Biener L, Baruch GK, editors. Gender and stress. New York: The Free Press; 1987. pp. 96–117. [Google Scholar]
- Leserman J, Jackson E, Petitto J, Golden R, Silva S, Perkins D, Cai J, Folds J, Evans DL. Progression to AIDS: The effects of stress, depressive symptoms, and social support. Psychosomatic Medicine. 1999;61:397–406. doi: 10.1097/00006842-199905000-00021. [DOI] [PubMed] [Google Scholar]
- Lutgendorf S, Antoni M, Ironson G, Starr K, Costello N, Zuckerman M, Klimas N, Fletcher MA, Schneiderman N. Changes in cognitive coping skills and social support during cognitive behavioral stress management intervention and distress outcomes in symptomatic human immunodeficiency virus (HIV)-seropositive gay men. Psychosomatic Medicine. 1998;60:204–214. doi: 10.1097/00006842-199803000-00017. [DOI] [PubMed] [Google Scholar]
- Marin BV, Gomez CA, Hearst N. Multiple heterosexual partners and condom use among Hispanics and non-Hispanic Whites. Family Planning Perspectives. 1993a;25:170–174. [PubMed] [Google Scholar]
- Marin BV, Tschann JM, Gomez CA, Kegeles SM. Acculturation and gender differences in sexual attitudes and behaviors: Hispanic vs Non-Hispanic White unmarried adults. American Journal of Public Health. 1993b;83:1759–1761. doi: 10.2105/ajph.83.12.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayne TJ, Acree M, Chesney MA, Folkman S. HIV sexual risk behavior following bereavement in gay men. Health Psychology. 1998;17:403–411. doi: 10.1037//0278-6133.17.5.403. [DOI] [PubMed] [Google Scholar]
- McCoy HV, Inciardi JA. Women and AIDS: Social determinants of sex-related activities. Women and Health. 1993;20:69–86. doi: 10.1300/J013v20n01_05. [DOI] [PubMed] [Google Scholar]
- McNair DH, Lorr M, Droppelman LF. Manual for the profile of mood states. San Diego, CA: Edits Education and Industrial Testing Service; 1992. Revised 1992. [Google Scholar]
- Miller M. A model to explain the relationship between sexual abuse and HIV risk among women. AIDS Care. 1999;11:3–20. doi: 10.1080/09540129948162. [DOI] [PubMed] [Google Scholar]
- Miller GE, Kemeny M, Taylor S, Cole S, Vissher B. Social relationships and immune processes in HIV seropositive gay and bisexual men. Annals of Behavioral Medicine. 1997;19:139–151. doi: 10.1007/BF02883331. [DOI] [PubMed] [Google Scholar]
- Moore J, Harrison JS, Kay KL, Deren S, Doll LS. Factors associated with Hispanic women's HIV-related communication and condom use with male partners. AIDS Care. 1995;7:415–427. doi: 10.1080/09540129550126371. [DOI] [PubMed] [Google Scholar]
- Morrill AC, Ickovis JR, Golubchikov VV, Beren SE, Rodin J. Safer sex: Social and psychological predictors of behavioral maintenance and change among heterosexual women. Journal of Consulting and Clinical Psychology. 1996;64:819–828. doi: 10.1037//0022-006x.64.4.819. [DOI] [PubMed] [Google Scholar]
- Namir S, Alumbaugh M, Fawzy F, Wolcott D. The relationship of social support to physical and psychological aspects of AIDS. Psychology and Health. 1989;3:77–86. [Google Scholar]
- Neal JJ, Fleming PL, Green TA, Ward JW. Trends in heterosexually acquired AIDS in the United States, 1988 through 1995. Journal of Acquired Immune Deficiency Syndrome and Human Retrovirology. 1997;14:465–474. doi: 10.1097/00042560-199704150-00011. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Wyatt GE, Romero GJ, Tucker MB, Wayment HA, Carmona JV, Solis B, Mitchell-Kernan C. Acculturation, sexual risk-taking, and HIV health promotion among Latinas. Journal of Counseling Psychology. 1998;45:454–467. [Google Scholar]
- Nyamathi A. Comparative study of factors relating to HIV risk level of black homeless women. Journal of Acquired Immune Deficiency Syndrome. 1992;5:222–228. [PubMed] [Google Scholar]
- Orr ST, Celentano DD, Santelli J, Burwell L. Depressive symptoms and risk factors for HIV acquisition among black women attending urban health centers in Baltimore. AIDS Education and Prevention. 1994;6:230–236. [PubMed] [Google Scholar]
- Paone D, Cooper H, Alperen J, Shi Q, DesJarlais DC. HIV risk behaviours of current sex workers attending syringe exchange: The experiences of women in five US cities. AIDS Care. 1999;11:269–280. doi: 10.1080/09540129947910. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, van Tilburg T, Boeke A, Deeg D, Kriegsman K, van Eijk J. Effects of social support and personal coping resources on depressive symptoms: Different for various chronic diseases? Health Psychology. 1998;17:551–558. doi: 10.1037//0278-6133.17.6.551. [DOI] [PubMed] [Google Scholar]
- Potter LB, Anderson JE. Patterns of condom use and sexual behavior among never-married women. Sexually Transmitted Diseases. 1993;20:201–208. doi: 10.1097/00007435-199307000-00005. [DOI] [PubMed] [Google Scholar]
- Reviere R, Eberstein IW. Work, marital status, and heart disease. Health Care for Women International. 1992;13:393–399. doi: 10.1080/07399339209516016. [DOI] [PubMed] [Google Scholar]
- Robbins AG, Dew MA, Davidson S, Pendower L, Becker JT, Kingsley L. Psychosocial factors associated with risky sexual behavior among HIV-seropositive gay men. AIDS Education and Prevention. 1994;6:483–492. [PubMed] [Google Scholar]
- Romero GJ, Arguellas L. AIDS knowledge and beliefs of citizen and non-citizen Chicanas/Mexicanas. Latino Studies Journal. 1993;4:79–94. [Google Scholar]
- Rosenfeld JA. Maternal work outside the home and its effect on women and their families. Journal of the American Medical Women's Association. 1992;47:47–53. [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Rosario M, Reid H, Koopman C. Predicting patterns of sexual acts among homosexual and bisexual youths. American Journal of Psychiatry. 1995;152:588–595. doi: 10.1176/ajp.152.4.588. [DOI] [PubMed] [Google Scholar]
- Sabogal F, Faigeles B, Catania JA. Data from the National AIDS Behavioral Surveys: II. Multiple sexual partners among Hispanics in high-risk cities. Family Planning Perspectives. 1993;25:257–262. [PubMed] [Google Scholar]
- Skurnick JH, Abrams J, Kennedy CA, Valentine SN, Cordell JR. Maintenance of safe sex behavior by HIV-serodiscordant heterosexual couples. AIDS Education and Prevention. 1998;10:493–505. [PubMed] [Google Scholar]
- Sikkima EJ, Heckman TG, Kelly JA, Anderson ES, Winett RA, Solomon LJ, Wagstaff DA, Roffman RA, Perry MJ, Cargill V, Crumble DA, Fuqua RW, Norman AD, Mercer MB. HIV risk behaviors among women living in low income, inner city housing developments. American Journal of Public Health. 1996;86:1123–1128. doi: 10.2105/ajph.86.8_pt_1.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somlai AM, Kelly JA, Wagstaff DA, Whitson DP. Patterns, predictors, and situational contexts of HIV risk behaviors of among homeless men and women. Social Work. 1998;43:7–20. doi: 10.1093/sw/43.1.7. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Hogg RS, Martindale SL, Cornelisse PG, Craib KJ, Montaner JS, O'Shaughnessy MV, Schechter MT. Determinants of sexual risk-taking among young HIV-negative gay and bisexual men. Journal of Acquired Immune Deficiency Syndrome and Human Retrovirology. 1998;19:61–66. doi: 10.1097/00042560-199809010-00010. [DOI] [PubMed] [Google Scholar]
- Turner HA, Hays R, Coates T. Determinants of social support among gay men: The context of AIDS. Journal of Health and Social Behavior. 1993;34:37–53. [PubMed] [Google Scholar]
- Wheeler AP, Lee ES, Loe HD. Employment, sense of well-being, and use of professional services among women. American Journal of Public Health. 1983;73:908–911. doi: 10.2105/ajph.73.8.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson TE, Jaccard J, Levinson RA, Minkoff H, Endias R. Testing for HIV and other sexually transmitted diseases: Implications for risk behavior in women. Health Psychology. 1996;15:252–260. doi: 10.1037//0278-6133.15.4.252. [DOI] [PubMed] [Google Scholar]
- Woodhouse DE, Rothenberg RB, Potterat JJ, Darrow WW, Muth SQ, Klovdahl AS, Zimmerman HP, Rogers HL, Maldonado TS, Muth JB. Mapping of social network of heterosexuals at high risk for HIV infection. AIDS. 1994;8:1331–1336. doi: 10.1097/00002030-199409000-00018. [DOI] [PubMed] [Google Scholar]
- Wortman CB. Social support and the cancer patient: Conceptual and methodologic issues. Cancer. 1984;53:2339–2362. doi: 10.1002/cncr.1984.53.s10.2339. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. The sociocultural context of African American and European American women's rape. Journal of Social Issues. 1992;48:77–91. [Google Scholar]
- Wyatt GE. The sociocultural relevance of sex research: Challenges for the 1990s and beyond. American Psychologist. 1994;49:748–754. doi: 10.1037//0003-066x.49.8.748. [DOI] [PubMed] [Google Scholar]


