Abstract
Objectives
Family members of patients with bipolar disorder experience high rates of subjective and objective burden which place them at risk for adverse physical health and mental health outcomes. We present preliminary efficacy data from a novel variation of Family Focused Treatment [Miklowitz DJ. Bipolar Disorder: A Family-Focused Treatment Approach (2nd ed.). New York: The Guilford Press, 2008] that aimed to reduce symptoms of bipolar disorder by working with caregivers to enhance illness management skills and self-care.
Methods
The primary family caregivers of 46 patients with bipolar I (n = 40) or II (n = 6) disorder, diagnosed by the Structured Clinical Interview for DSM-IV Axis I Disorders, were assigned randomly to receive either: (i) a 12–15-session family-focused, cognitive-behavioral intervention designed to provide the caregiver with skills for managing the relative’s illness, attaining self-care goals, and reducing strain, depression, and health risk behavior [Family-Focused Treatment-Health Promoting Intervention (FFT-HPI)]; or (ii) an 8–12-session health education (HE) intervention delivered via videotapes. We assessed patients pre- and post-treatment on levels of depression and mania and caregivers on levels of burden, health behavior, and coping.
Results
Randomization to FFT-HPI was associated with significant decreases in caregiver depressive symptoms and health risk behavior. Greater reductions in depressive symptoms among patients were also observed in the FFT-HPI group. Reduction in patients’ depression was partially mediated by reductions in caregivers’ depression levels. Decreases in caregivers’ depression were partially mediated by reductions in caregivers’ levels of avoidance coping.
Conclusions
Families coping with bipolar disorder may benefit from family interventions as a result of changes in the caregivers’ ability to manage stress and regulate their moods, even when the patient is not available for treatment.
Keywords: depression, health burden, illness management, psychoeducation, stress
Bipolar disorder affects the family members of a patient and is affected by the family environments associated with caregiving. From 89% to 91% of family members report feelings of emotional distress (i.e., ‘subjective burden’) in relation to the severity of the patient’s illness symptoms (1, 2); between 24% and 38% score above the standard cutoffs on self-report measures of depressive symptoms (2). Patient suicidal ideation and behavior in particular have been associated with increased symptoms of caregiver depression (3). For family members with their own history of mood disorders, caregiving more than doubles the risk of recurrence of an episode of major depression in the caregiver compared to the risk of recurrence among persons with a history of mood disorder but without caregiving responsibilities (4).
Recent studies suggest that subjective burden and/or depression also compromise caregivers’ ability to effectively manage the demands associated with caregiving, which in turn leads to less favorable patient outcomes. Higher levels of caregiver burden are associated with more emotion-focused coping and/or lower mastery among caregivers (5–7) and with poorer patient medication adherence and clinical outcomes among patients (8, 9). Highly burdened family members are also less likely to practice adequate self-care and to suffer adverse effects on their physical health (2, 10, 11), further compromising their resilience and readiness to manage acute or subacute problems with the relative with bipolar disorder.
The widespread dissemination of education and support groups for family members alone (i.e., without the patient), such as the Family to Family Program developed by the National Alliance on Mental Illness (NAMI) (12) and the Support and Family Education Program (SAFE) (13), attests to the family’s interest in psychosocial interventions for bipolar disorder and other major mental disorders. However, programs developed for family members have seldom evaluated the impact of such programs on patient as well as family outcomes, leaving unanswered the important question of whether interventions with family members alone can benefit the patient as well. We developed a Family-Focused Treatment-Health Promoting Intervention (FFT-HPI), a brief (12–15 session), manualized, psychoeducational intervention for family members of patients with bipolar disorder which aims to provide the caregiver with enhanced skills for managing the relative’s illness, defining self-care goals and resolving barriers to patient care and self-care through education, examination of core beliefs that maintain dysfunctional interaction patterns, and problem solving. FFT-HPI targets both patient symptoms and caregiver health behavior (e.g., seeking appropriate medical care and following recommendations) and mental health outcomes. The main purpose of this study was to evaluate the efficacy of FFT-HPI in an initial clinical trial where family members were randomized to receive either FFT-HPI or education about bipolar disorder and health problems that are common among caregivers. Primary outcome variables for caregivers were depressive symptoms and health behavior. Primary outcome measures for the patient were symptoms of bipolar depression and mania.
First, we hypothesized that caregivers treated with FFT-HPI would demonstrate decreased depressive symptoms and subjective burden and improved health behavior from pre- to post-treatment compared to caregivers treated with a health education intervention (HE). Second, we hypothesized that the patients with bipolar disorder associated with caregivers treated with FFT-HPI would report reduced symptoms of bipolar disorder post-treatment relative to the patients of caregiver treated with HE.
Recently, Miklowitz and Scott (14) identified “the lack of clarity about the mediators of outcome” as a key weakness in the psychotherapy literature on change. Therefore, a secondary aim was to identify potential mediators of patient and caregiver outcomes. We predicted that the hypothesized differential reduction in patient symptoms between treatment groups would be mediated by changes in caregivers’ levels of depression. Secondarily, based on prior studies of caregiving and depression, we predicted that clinical improvement in the caregiver would be mediated by reductions in avoidance coping, a form of emotion-focused coping characterized by denial, wishful thinking, and displays of emotion (5).
Patients and methods
Participants
Caregiver participants were recruited from the Mount Sinai Outpatient Mental Health Clinic, New York, NY (n = 5), from the Bronx Veterans Affairs Medical Center, Bronx, NY (n = 2), and from the Mood Disorders Support Group of New York (MDSG), New York, NY (n = 36). At the mental health facilities clinicians referred the bipolar disorder relatives of eligible caregivers to the study team. Caregivers were recruited at the MDSG directly via fliers, referral from group leaders, or through a brief presentation by study staff at weekly “Family and Friends” support group meetings. Interested caregivers from all sources were consented and screened for eligibility. To be eligible, caregivers had to be age 18 or older and to be the primary caregiver of a relative diagnosed with bipolar I or II disorder based on the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (15) who consented to the study. The primary caregiver met at least three (two for nonrelatives) of five criteria established by Pollak and Perlick (16): (i) is a spouse or parent; (ii) has more frequent contact than any other caregiver; (iii) helps to support the patient financially; (iv) is contacted by treatment staff for emergencies; (v) has been involved in the patient’s treatment.
Caregivers also had to demonstrate current physical and mental health problems, defined as scoring positive for at least one health risk behavior on the Health Risk Behavior Scale (HRB) (17) and either scoring ≥ 10 on the Center for Epidemiological Studies for Depression Scale (18) or scoring positive on ≥ 4 burden areas on the Social Behavior Assessment Schedule (SBAS) (19). Of 50 caregivers referred, 40 (80%) of 50 caregivers referred from the MDSG and 10 (38.4%) of 26 caregivers referred from the mental health facilities (71.4% of the caregivers of consenting patients) agreed to participate. Of these, four were determined to be ineligible: three did not meet criteria for health risk behavior, and one caregiver’s relative did not meet diagnostic criteria on the SCID. Twelve (46%) patients from the mental health facilities and none from the MDSG refused participation.
A total of 46 caregivers met inclusion criteria, gave consent, and were randomized to receive 12–15 sessions of FFT-HPI or 8–12 sessions of HE using a random numbers table where all even numbers were assigned to FFT-HPI and odd numbers were assigned to HE. The randomization was performed by a research assistant not connected to the present study who put treatment assignments into sealed envelopes numbered sequentially. The envelopes were then opened by the project director in the weekly research meeting immediately following completion of each pretreatment assessment. The small number of subjects did not allow for a blocking/stratification procedure. Parents of young adults who were equally involved in caregiving were randomized as one unit. Three parental couples were randomized to HPI and one to HE; 25 caregivers were assigned to FFT-HPI and 21 were assigned to HE.
Patient and caregiver measures
Patients and caregivers were assessed by trained research assistants prior to randomization so that both the assessor and the participants were blind to treatment assignment during administration of the initial assessment. All patient assessments were performed by master’s-level clinical doctoral students. Participants were reassessed immediately post-treatment and six months post-treatment on all measures described below. Post-test assessments were performed by an independent evaluator from a separate location who was kept blind to treatment condition. This initial report focuses on change observed over the course of treatment; data on maintenance of treatment effects will be reported separately.
Assessment instruments
The patient’s lifetime diagnosis of bipolar disorder and current episode status were confirmed using the mood and psychosis modules from the SCID (15). Current symptom level was assessed using the Hamilton Rating Scale for Depression (HAM-D) (20) and the Young Mania Rating Scale (YMRS) (21). Internal consistency reliability in the present study was 0.849 for the HAM-D and 0.852 for the YMRS.
The caregiver’s lifetime diagnosis and current episode status were evaluated by the Mini International Neuropsychiatric Interview version (MINI Plus version 5.0) (22), a semistructured interview designed to identify current major Axis I disorders. The Center for Epidemiological Studies of Depression Scale (CES-D) (18), a self-report measure of depressive symptoms, was used to screen caregivers for symptomatic distress for inclusion. Caregiver depression was evaluated pre- and post-treatment by the Quick Inventory of Depressive Symptomatology (QIDS-C) (23). The QIDS is a 16-item index of severity of depressive symptoms which has high internal consistency (Cronbach’s alpha = 0.86) and correlates highly with the 30-item Inventory of Depressive Symptoms (0.96) and the 24-item HAM-D (0.84). Each of the two master’s-level clinicians administered the first three diagnostic and clinical symptom scales together with the first author (DAP): both clinicians’ diagnostic interview ratings corresponded 100% with DAP’s, and clinical symptom scales differed from DAP’s by no more than one point.
The HRB, a nine-item assessment of behavioral health risks of caregiving, (e.g., eating less than three meals a day, not getting enough rest, forgetting to take medications, missing doctor’s appointments), was used to evaluate caregiver health behavior. The HRB correlates with perceptions of general health (24) and demonstrated adequate internal consistency reliability in the present study (Cronbach’s alpha = 0.78).
The SBAS, a semistructured interview, was used to assess caregivers’ experience of objective and subjective burden over the six months prior to study (pretreatment assessment) and during the course of treatment (post-treatment assessment) in three domains: patient problem behaviors (e.g., violence, unpredictability); patient role dysfunction at work and at home; and adverse effects on others (the impact of the illness on the caregiver’s work, social, and leisure time). In judging objective burden, caregivers were asked to rate the degree to which each problem was present on a scale of 0 (none), 1 (moderate), or 2 (severe). In judging subjective burden, they rated the degree of distress they experienced as a result of each item previously rated as objectively present, using the same scale. When objective burden was coded as 0, the corresponding item on the subjective scale was also coded as 0. The total subjective burden score across 56 items (Cronbach’s alpha = 0.88) was used to evaluate the study hypotheses as this represented the purer measure of perceived strain.
Avoidance coping was measured using six items from the Ways of Coping Questionnaire (25) as adapted by Scazufca and Kuipers (5) and MacCarthy and Brown (26). Examples of avoidance coping are “avoided other people” and “tried to take my mind off things by smoking, drinking, or taking pills.” Caregivers rated the degree to which they employed each strategy in response to the most stressful situation with the patient in the last month on a scale of 1 (never) to 5 (all the time). Responses were summed across items to generate an overall index ranging from 6 to 36.
FFT treatment
FFT-HPI combined education about optimal management of bipolar disorder (27) with examination of the caregiver’s automatic thoughts, feelings, and core beliefs about caregiving that sustain symptoms of depression and anxiety and interfere with efforts to seek social support, engage in pleasurable activities outside the home, and practice adequate medical and self-care. By helping family members define appropriate levels of support and monitoring relative to the patient’s mental status, the intervention not only honed management skills but helped the caregiver to define realistic expectations for the patient and accept the limitations imposed by his/her illness, while simultaneously supporting more autonomous functioning for the caregiver.
The intervention consisted of two phases. In Phase I: Psychoeducation and Goal Setting (Sessions 1– 4), the therapist covered basic material on the etiology of bipolar disorder, treatment and medication adherence, relapse prevention, sleep and daily routines, stress and emotion regulation, and effective communication strategies, as described by Miklowitz (27). Caregivers were provided with an educational video and reading materials to facilitate education. In addition, the therapist reviewed the caregiver’s assessment with him/her collaboratively and used it to help generate self-care goals. Four goals were set for each caregiver: (i) an interpersonal goal that aimed to improve one or more problematic aspect of the caregiver’s relationship with the patient (e.g., checking on or doing things for the patient to excess), (ii) an emotional/symptoms goal which aimed to reduce the caregiver’s distress, experienced in symptoms of depression, anxiety, and/or subjective burden; and (iii) and (iv) two self-care goals aimed at promoting greater physical and emotional health and well-being (e.g., weight control, exercise, expanding support network, routine medical tests).
In Phase II: Behavioral Analysis of Self-care Barriers (Sessions 5–15), the therapist used cognitive-behavioral therapy (CBT) and problem-solving strategies to identify situations where objective caregiving demands and/or subjective strain and associated cognitions (i.e., self-care barriers) interfered with the practice of illness management and self-care goals and to facilitate adoption of alternate, health-promoting responses. Based on a collaborative discussion that integrated salient findings from the assessment (e.g., depression score) with the caregivers’ perceptions of what might make it difficult to achieve their goals, each caregiver was assigned to one of four modules designed to address common barriers to self-care: (i) support diversification, which focused on broadening the patient and caregiver support networks and increasing patient self-reliance; (ii) conflict resolution, which utilized problem-solving and communication skills training and included an optional 1– 3 sessions with the relative with bipolar disorder; (iii) efficacy and expectations, which challenged depressogenic cognitions and used positive self-statements, exercise, and sleep hygiene to reduce depressive symptoms and increase caregiver self-efficacy; and (iv) a blend of 1–3. A summary of the major therapeutic tasks and strategies throughout the treatment is provided in Table 1 (treatment manual available upon request). The treatment was delivered by two experienced clinicians trained in FFT and CBT (DAP and NL) and was supported by weekly peer supervision and monthly supervision with DJM. Sessions were delivered on a weekly basis and were 45 minutes in duration. Randomly selected treatment tapes were rated by two independent raters using an adaptation of Weisman et al.’s Treatment Competence and Adherence Scales (28). Of 10 sessions rated by two raters, 90% (18/20) were rated at or above a preselected adherence threshold. Agreement between the two raters was good (kappa = 0.91).
Table 1.
Therapeutic tasks for Family-Focused Treatment-Health Promoting Intervention sessions
| Phase I: Psychoeducation and goal setting |
| Session 1 |
|
| Session 2 |
|
| Session 3 |
|
| Session 4 |
|
| Phase II: Behavioral analysis of barriers to patient illness management, self-care |
| Session 5 |
|
| Sessions 6–15 |
|
Health education intervention
The HE comparison treatment adopted a didactic approach to informing family members about health problems and concerns that have been identified in the literature as common among and/or relevant to caregivers. Information was delivered via professionally produced DVDs on topics ranging from depression to heart disease to chronic pain. Initially, participants viewed a DVD that provided education about bipolar disorder. Next, they viewed a core set of eight 20–25-minute tapes (one per session) describing the most common health problems experienced by caregivers (based on prior studies), and then selected up to four additional tapes of their own choice. All tapes were facilitated by a clinical research associate, who stopped each tape at standardized, logical break points to review and ensure that the caregiver understood the information, but refrained from discussion of the material or the caregiver’s own situation.
Data analysis
All 43 participants who began Phase II of the treatment completed the treatment and the post-treatment assessment. All principal analyses were conducted based on the intention-to-treat principle using all available data for analysis. First, the treatment and control groups were compared on pretreatment sociodemographic and clinical characteristics using t-tests and Χ2 or Fisher’s exact tests. Next, mixed effects linear regression models with random subject effects were used to evaluate the effect of treatment group on each of the four outcome variables (caregiver depressive symptoms and health risk behaviors and patient depressive and manic/hypomanic symptoms), and on hypothesized mediating variables (subjective burden and avoidance coping). Each variable measured at post-treatment was regressed onto treatment group assignment, followed by the respective pretreatment value for that variable. In an additional analysis, the model described above for patient depression scores was computed again, adding the interaction between treatment group and change in caregiver depression (pre- to post-treatment) scores as the final entry, in order to evaluate the hypothesis that a differential reduction in patient depression between treatment groups was greatest in the subgroup who showed more treatment-related changes in caregiver depression (29).
We also conducted exploratory models evaluating level of caregiver avoidance coping as a mediator of treatment-related changes in caregiver depression and health risk behavior, in each case adding the interaction between group and the pre- to post-treatment change in the hypothesized mediating variable after the baseline value of the dependent variable and group variable had been entered. Since caregiver subjective burden was conceptualized as a secondary outcome, it was not included in these analyses.
Results
Sample characteristics
Of the 46 participants randomized to treatment, 1 FFT-HPI participant and 2 HE participants dropped out after only 1–2 sessions (i.e., prior to Phase II) and were not able to be followed. However, all participants who began Phase II of the treatment completed the treatment and the post-treatment assessment and were included in all analyses, bringing the final sample to 24 FFT-HPI and 19 HE participants (N = 43). Participants in both conditions were seen weekly for an average of 14.3 ± 1.6 sessions over 4.7 ± 1.1 months in FFT-HPI and 8.1 ± 2.4 sessions in HE. All patients completed the minimum number of sessions (12 in FFT-HPI and 8 in HE) except 1 FFT-HPI patient who completed 7 sessions and 1 HE patient who completed 4. Table 2 displays the pretreatment sociodemographic and clinical characteristics of the study sample. No significant differences between treatment groups were observed prior to the onset of treatment on any of 14 caregiver and patient sociodemographic variables or on 8 clinical characteristics.
Table 2.
Sociodemographic and clinical characteristics of patients with bipolar disorder and their family caregiversa
| Caregiver | Patient | |||||
|---|---|---|---|---|---|---|
| FFT-HPI (n = 24) | HE (n = 19) | t or (Χ²)b | FFT-HPI (n = 22)c | HE (n = 18)c | t or (Χ²)b | |
| Female | 20 (83.3) | 16 (84.2) | 14 (63.6) | 11 (61.1) | ||
| Age, mean ± SD | 51.8 ± 12.8 | 54.0 ± 11.9 | 1.98 | 39.4 ± 16.7 | 29.0 ± 12.9 | 2.15 |
| Ethnicity | 0.73 | 0.23 | ||||
| Caucasian | 19 (79.2) | 14 (73.7) | 16 (72.7) | 14 (77.8) | ||
| African American | 0 (0) | 2 (10.5) | 1 (4.5) | 2 (11.1) | ||
| Hispanic | 5 (20.8) | 2 (10.5) | 5 (22.7) | 2 (11.1) | ||
| Other | 0 (0) | 1 (5.3) | 0 (0) | 0 (0) | ||
| Marital status | 0.23 | 0.06 | ||||
| Married/cohabitating | 14 (58.3) | 5 (26.3) | 3 (13.6) | 3 (16.7) | ||
| Widowed/divorced/separated | 6 (25.0) | 8 (42.1) | 7 (31.8) | 5 (27.9) | ||
| Never married | 4 (16.7) | 6 (31.6) | 12 (54.5) | 10 (55.6) | ||
| Employment status | 0.47 | 1.10 | ||||
| Full time | 12 (50.0) | 10 (52.6) | 3 (13.6) | 4 (22.2) | ||
| Part time | 5 (20.8) | 6 (31.6) | 6 (27.3) | 1 (5.6) | ||
| Retired | 6 (25.0) | 3 (15.8) | 0 (0) | 0 (0) | ||
| Unemployed | 1 (4.2) | 0 (0) | 11 (50.0) | 5 (27.8) | ||
| Student | 0 (0) | 0 (0) | 2 (9.1) | 8 (44.4) | ||
| Relationship of caregiver to patient | 1.50 | |||||
| Parent | 15 (62.5) | 15 (79.0) | ||||
| Spouse/significant other | 4 (16.7) | 2 (10.6) | ||||
| Adult child | 5 (20.8) | 1 (5.3) | ||||
| Friend or neighbor | 0 (0) | 1 (5.3) | ||||
| Living with patient | 14 (58.3) | 14 (73.7) | 1.10 | |||
| Socioeconomic status | ||||||
| I or II | 13 (54.2) | 10 (52.7) | 3 (13.6) | 2 (11.1) | ||
| III | 8 (33.3) | 6 (31.6) | 7 (31.8) | 4 (22.2) | ||
| IV or V | 3 (12.5) | 3 (15.8) | 12 (54.5) | 12 (66.6) | ||
| Age of onset, mean ± SD | 21.3 ± 12.0 | 18.1 ± 7.3 | 0.98 | |||
| Total psychiatric admissions, mean ± SD | 4.4 ± 5.3 | 4.3 ± 3.8 | 0.04 | |||
| Lifetime diagnosis | ||||||
| Bipolar I disorder | 0 (0) | 0 (0) | 19 (86.4) | 15 (83.3) | ||
| Bipolar II disorder | 0 (0) | 0 (0) | 3 (13.6) | 3 (16.7) | ||
| Major depressive disorder | 8 (33.3) | 6 (31.6) | 0 (0) | 0 (0) | ||
| Current episode | 0.42 | |||||
| Major depressive episode | 0 (0) | 2 (10.5) | 10 (45.5) | 8 (44.4) | ||
| Manic episode | 0 (0) | 0 (0) | 3 (13.6) | 3 (16.7) | ||
| Hypomanic episode | 0 (0) | 0 (0) | 0 (0) | 2 (11.1) | ||
| No episode | 24 (100) | 17 (89.5) | 9 (40.9) | 5 (27.8) | ||
| HAM-D score, mean ± SD | 15.6 ± 10.3 | 14.9 ± 5.7 | 0.26 | |||
| YMRS score, mean ± SD | 8.8 ± 9.7 | 9.2 ± 9.2 | 0.15 | |||
All values are n (%) unless otherwise noted.
Due to low expected cell frequencies, Χ2 or Fisher's exact tests were calculated combining across categories for the following variables: ethnicity (white versus nonwhite), marital status (ever versus never married), employment (working versus not working), relationship to caregiver (parent versus other), current episode (any episode versus none). Tests could not be performed for gender, lifetime diagnosis, and socioeconomic status (SES), but groups did not differ by more than 3% on these variables except for patient SES, where the values in the HE group were weighted toward the lower end of the distribution. No comparisons performed were significant at p < 0.05.
The lower n for patients relative to caregivers reflects the participation of two couples in FFT-HPI and one couple in HE.
FFT-HPI = Family-Focused Treatment-Health Promoting Intervention; HE = health education intervention; HAM-D = Hamilton Rating Scale for Depression; YMRS = Young Mania Rating Scale.
Patient and caregiver treatment outcomes
Table 3 summarizes the results of the analyses regressing the caregiver and patient outcome variables [caregiver: QIDS, HRB, burden (SBAS); patient: HAM-D, YMRS] onto treatment group assignment (FFT-HPI versus HE), controlling for pretreatment values. As hypothesized, caregivers in the FFT-HPI intervention arm showed significant reductions in depressive symptoms on the QIDS [F(1,41) = 4.64, p = 0.037] and in health risk behaviors [F(1,41) = 5.11, p = 0.029] relative to caregivers in the health education arm. The effect sizes (ES) (Cohen’s d) for QIDS and HRB were 0.50 and 0.99, respectively. The group effect for caregiver burden was also significant [F(1,41) = 7.51, p = 0.009], ES = 1.23.
Table 3.
Relationship of treatment assignment to family and patient physical and mental health outcomes
| Family-Focused Therapy-Health Promoting Intervention (n = 24) |
Health education intervention (n = 19) |
Group | ||||
|---|---|---|---|---|---|---|
| Variable | Pretreatment Mean (SD) |
Post-treatment Mean (SD) |
Pretreatment Mean (SD) |
Post-treatment Mean (SD) |
F | p-value |
| Caregiver QIDS | 8.2 (3.8) | 4.6 (2.9) | 9.0 (5.6) | 8.5 (8.4) | 4.64 | 0.037 |
| Caregiver HRB | 4.7 (2.2) | 2.0 (2.3) | 3.8 (2.3) | 3.7 (2.6) | 5.11 | 0.029 |
| Caregiver burden (SBAS) | 0.8 (0.2) | 0.4 (0.2) | 0.7 (0.3) | 0.6 (0.4) | 7.51 | 0.009 |
| Patient HAM-D | 15.2 (10.1) | 5.6 (6.1) | 14.5 (5.9) | 11.2 (9.1) | 5.44 | 0.025 |
| Patient YMRS | 8.1 (9.7) | 1.6 (2.4) | 9.3 (8.8) | 5.8 (9.0) | 4.66 | 0.037 |
For economy of space, the coefficients and significance levels only for treatment group assignment are shown. QIDS = Quick Inventory of Depressive Symptomatology; HRB = Health Risk Behavior Scale; HAM-D = Hamilton Rating Scale for Depression-21 items; YMRS = Young Mania Rating Scale; SBAS = Social Behavior Assessment.
When caregivers participated in FFT-HPI, the patients with bipolar disorder showed significant decreases in depressive symptoms on the HAM-D relative to patients whose caregivers participated in HE [F(1,39) = 5.44, p = 0.025], ES = 0.67. Patients whose caregivers were treated with FFT-HPI also showed a significant reduction on the YMRS relative to patients whose caregivers were treated with HE [F(1,39) = 4.66, p = 0.037], though the ES (0.34) was not as large as that observed for the HAM-D.
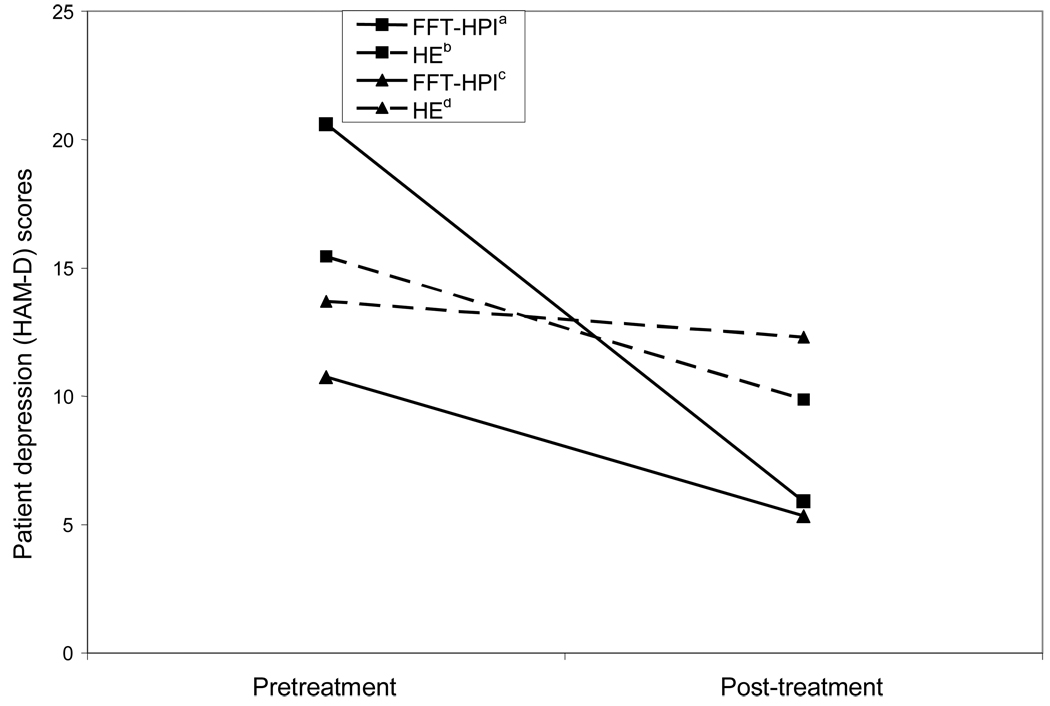
Exploratory tests of mediational hypotheses
The interaction of group and change in caregiver QIDS score over the pre-/post-treatment interval was significant in predicting changes in patients’ HAM-D scores [F(1,37) = 4.25, p = 0.011], and the increase in explanatory power with the inclusion of the interaction term was also significant, increasing the amount of variance explained (R2) from 0.16 to 0.27 [FΔ (1,37) = 4.72, p = 0.036]. Figure 1 depicts the interaction between treatment group and change in caregiver QIDS over the course of treatment. Examining this figure we see that in the FFT-HPI condition, large reductions in caregiver depressive symptoms were associated with large reductions in patient depression, whereas in the HE condition, there were little or no reductions in HAM-D scores associated with higher changes in caregiver depression. This finding indicates that the greater decrease in patient depressive symptoms observed in FFT-HPI was mediated in part by changes in caregiver depression observed over the course of treatment with FFT-HPI. More specifically, it indicates that participation in FFT-HPI was associated with a greater decrease in depressive symptoms for those patients whose caregivers experienced the greatest decreases in depressive symptoms. By contrast, the interaction term for caregiver depression in the parallel model predicting patient YMRS scores was not significant.
Fig. 1.
Changes in patients’ depressive symptoms (HAM-D) over the course of the caregivers’ treatment with Family-Focused Treatment-Health Promoting Intervention (FFT-HPI) or health education (HE) as a function of the reduction in caregivers’ depression scores. Caregivers are grouped according to whether they showed reductions in depression scores above or below the sample median of 3.0. The interaction of treatment group with change in caregiver depression score (QIDS) from pre- to post-treatment was a significant predictor of patient HAM-D post-treatment [F(1,37) = 4.82, p = 0.011] after controlling for level of patients’ depression scores (HAM-D) during the pretreatment period.
aCaregiver depression reduction score > median (n = 12).
bCaregiver depression reduction score > median (n = 9).
cCaregiver depression reduction score < median (n = 12).
dCaregiver depression reduction score < median (n = 10).
The interaction of group and change in caregivers’ avoidance coping over the course of treatment was significant in predicting changes in caregivers’ QIDS scores [F = 4.01, p = 0.014], and the change in R2, from 0.12 to 0.24, was also significant [FΔ(1,37) = 5.82, p = 0.021], indicating that the greater decrease in depressive symptoms observed for caregivers in the FFT-HPI arm was partially mediated by a decrease in caregivers’ avoidance coping. Additionally, participation in FFT-HPI resulted in a greater decrease in depressive symptoms for those caregivers who reported a greater decrease in avoidance coping. The interaction term for change in avoidance coping in the parallel analysis conducted for health risk behavior was not significant.
Discussion
This study examined the preliminary efficacy of an intervention for caregivers of patients with bipolar disorder designed to improve both patient and caregiver mental health outcomes and caregiver self-care compared to a standard health education intervention. As hypothesized, caregivers treated with a psychoeducational and cognitive-behavioral approach in the FFT-HPI condition experienced a significant reduction in depressive symptoms and improvement in health behaviors relative to caregivers who received education alone. They also reported significant reductions in subjective burden associated with the patients’ symptoms and role dysfunction over the course of treatment.
Importantly, the treatment gains in FFT-HPI were not limited to caregivers. As hypothesized, the patients associated with caregivers in FFT-HPI showed a decrease in symptoms of depression and mania relative to patients associated with caregivers receiving health education. Moreover, the greater reduction in patients’ depressive symptoms observed in the FFT-HPI condition was mediated in part by caregiver depressive symptoms. These findings demonstrate that psychoeducation and focused cognitive work with caregivers can also impact patients’ symptoms, even without the direct participation of the patient in the intervention. Our findings are consistent with those of Reinares et al. (30), who reported that a randomized trial of group psychoeducation for caregivers of patients with bipolar disorder was associated with a significant reduction in the percentage of patients with a recurrence of mania/hypomania as well as increased time to such an episode.
Prior studies have demonstrated that higher levels of caregiver burden are associated with an increased likelihood that patients will have an earlier recurrence of bipolar illness (31, 32). Caregivers who are highly burdened and/or distressed may have diminished coping resources and exercise less resilience in dealing with crises or exacerbations of the patient’s illness. Caregivers with high levels of burden, psychological distress, and depression are more likely to use avoidance or emotion-focused coping strategies, which are thought to reflect the perception that the situation is unchangeable (6, 10, 33, 34). In the present study, the greater reduction in caregiver depression in the FFT-HPI group was mediated in part by decreases in their avoidance coping. By equipping caregivers with practical advice on illness management and challenging depressogenic cognitions, FFT-HPI may alter appraisal of the potential for change in both the caregiver and the patient with bipolar disorder.
This study has certain limitations. First, because caregivers in FFT- HPI had roughly twice the number of sessions as those in the HE condition, we cannot rule out the possibility that the differences observed between treatment conditions may have been attributable to the treatment dose, rather than to the different therapeutic strategies employed. However, our findings that the greater reduction in patient depressive symptoms observed in FFT-HPI was mediated by a greater decrease in caregiver depressive symptoms, which was in turn mediated by a reduction in avoidance coping, coupled with the exclusive provision of customized illness management strategies in FFT-HPI suggest that the caregiver and patient symptom reduction observed was related to specific strategies employed in FFT-HPI targeting caregiver depression, coping, and illness management skills. Future studies should equalize the dose between treatment conditions, however, to rule out this alternate interpretation of the findings. We did not systematically record data on medication prescriptions. While changes in medication regimen during the course of treatment might account for decreases in patients’ symptoms, physicians referring patients to the study were blind to their caregivers’ treatment assignment and caregivers and patients recruited through the support group were asked not to discuss their participation with the patients’ providers. It therefore seems unlikely that changes in physician prescribing patterns account for the study’s findings.
Another limitation is the relative lack of ethnic diversity among participants: roughly three-quarters of both caregivers and patients were Caucasian. In addition, the sample was skewed towards the upper end of the socioeconomic distribution, limiting our ability to generalize the study’s findings to people of lower socioeconomic classes and more diverse ethnic backgrounds. Although one of the study therapists (NL) was fluent in Spanish, our ability to recruit more Hispanic and socioeconomically disadvantaged caregivers was impacted by the relatively high refusal rate of patients from the mental health (versus support group) settings. Difficulties in engaging families in educational programs in mental health settings have been well documented (e.g., 35). Our relatively high success rate in recruiting participants through the support group, where the initial contact was with the family member, suggests that participation in family programs in mental health settings may be enhanced by incorporating programs from support and advocacy groups such as the Depression and Bipolar Support Alliance and NAMI into the roster of services offered in mental health settings.
The study was designed as a pilot randomized clinical trial and as such is limited in sample size. This in turn limited the range of outcome variables that could be evaluated. A key question in evaluating the effectiveness of a psychosocial intervention is whether improvement in symptoms translates into improvement in functional status. Miklowitz et al. (36) found that intensive psychosocial intervention with patients with bipolar disorder, seen alone or with family members, plus pharmacotherapy resulted in improved patient functional outcomes relative to brief psychoeducation. The potential to achieve comparable results working with the caregiver alone is an important research question with direct relevance to clinical care that must await future studies. Other questions of interest for future studies include identification of potential moderators of treatment response that could be used to personalize treatment. For example, studies have demonstrated differences between parents and spousal caregivers in their emotional behavior toward their relative with mental illness; i.e., parents of patients with bipolar disorder exhibit higher levels of emotional overinvolvement than do spouses (e.g., 37). Emotional overinvolvement has been associated with avoidance coping (5) but also with high levels of warmth (38), and a lower risk of Axis I psychopathology among caregivers of patients with bipolar disorder (37), suggesting that parents may be better equipped than spouses to benefit from FFT-HPI, which emphasizes the caregiver defining separate self-care goals as well as illness management goals for the patient. However, this study was not statistically powered to examine treatment moderators such as whether parental caregivers and/or caregivers of more chronically ill patients responded better to FFT-HPI than spousal caregivers or caregivers of first- or second-episode patients. Future research should examine focused hypotheses about treatment moderators in larger samples. Future studies might also help further elucidate mediators of the treatment effect for patients by incorporating measures of medication adherence and/or of the emotional relationship between patient and caregiver.
The potential public health significance of an intervention that improves clinical symptoms of patients with bipolar disorder through working with their caregivers can be evaluated by examining statistics on service use of these patients. Data from the National Comorbidity Study Replication (39) indicate that only one-third (33.8%) of patients with bipolar disorder utilized any outpatient mental health service in a 12-month period, and of these, only half (47.7–49.8%) attended often or systematically enough to receive “minimally adequate treatment” according to official treatment guidelines for bipolar disorder (40). Similarly, despite the availability of effective family interventions for bipolar disorder (12, 13), studies have shown that such family psychoeducation is rarely practiced in the public sector (41). Even when patients seek treatment, they are frequently nonadherent with the prescribed medication regimens (42), with adherence rates ranging from 23% to 68% (9).
From this perspective, FFT-HPI offers a viable alternative for treating patients with bipolar disorder when concerned family members are available for treatment but the patient is not. Further, as the patient’s symptoms stabilize with caregiver intervention, he/she may become available for family and/or individual psychosocial treatment at a later date.
Acknowledgements
This study was supported by grant R34 MH071396 from the National Institute of Mental Health. The authors are indebted to Bruce Rounsaville, M.D., and Carolyn Mazure, Ph.D., for guidance on issues pertaining to treatment development and women’s health, and to the Mood Disorders Support Group of New York “Family and Friends” facilitators who helped adapt the model to better meet the needs of family members. Finally, we offer a special thanks to the family members and relatives with bipolar disorder who participated in this initial study.
Footnotes
The authors of this paper do not have any commercial associations that might pose a conflict of interest in connection with this manuscript.
References
- 1.Perlick DA, Clarkin JF, Sirey J, et al. Burden experienced by caregivers of persons with bipolar affective disorder. Br J Psychiatry. 1999;174:56–62. doi: 10.1192/bjp.175.1.56. [DOI] [PubMed] [Google Scholar]
- 2.Perlick DA, Rosenheck RA, Miklowitz DJ, et al. Prevalence and correlates of burden among caregivers of patients with bipolar disorder enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder. Bipolar Disord. 2007;9:262–273. doi: 10.1111/j.1399-5618.2007.00365.x. [DOI] [PubMed] [Google Scholar]
- 3.Chessick CA, Perlick DA, Miklowitz DJ, et al. Current suicide ideation and prior suicide attempts of bipolar patients as influences on caregiver burden. Suicide Life Threat Behav. 2007;37:482–491. doi: 10.1521/suli.2007.37.4.482. [DOI] [PubMed] [Google Scholar]
- 4.Russo J, Vitaliano PP, Brewer DD, Katon W, Becker J. Psychiatric disorders in spouse caregivers of care recipients with Alzheimer’s disease and matched controls: A diathesis-stress model of psychopathology. J Abnorm Psychology. 1995;104:197–204. doi: 10.1037//0021-843x.104.1.197. [DOI] [PubMed] [Google Scholar]
- 5.Scazufca M, Kuipers E. Coping strategies in relatives of people with schizophrenia before and after psychiatric admission. Br J Psychiatry. 1999;174:154–158. doi: 10.1192/bjp.174.2.154. [DOI] [PubMed] [Google Scholar]
- 6.Noh S, Avison WH. Spouses of discharged psychiatric patients: Factors associated with their experience of burden. J Marriage Fam. 1988;1:377–389. [Google Scholar]
- 7.Perlick DA, Rosenheck RA, Miklowitz DJ, et al. Caregiver burden and health in bipolar disorder: A cluster analytic approach. J Nerv Ment Dis. 2008;196:484–491. doi: 10.1097/NMD.0b013e3181773927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cochran SD, Gitlin MJ. Attitudinal correlates of lithium compliance in bipolar affective disorders. J Nerv Ment Dis. 1988;176:457–464. doi: 10.1097/00005053-198808000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Perlick DA, Rosenheck RA, Kaczynski R, Kozma L. Medication non-adherence in bipolar disorder: a patient-centered review of research findings. Clin Approach Bipolar Disord. 2004;3:59–70. [Google Scholar]
- 10.Li LW, Seltzer MM, Greenberg JS. Change in depressive symptoms among daughter caregivers: An 18-month longitudinal study. Psychol Aging. 1999;41:206–219. doi: 10.1037//0882-7974.14.2.206. [DOI] [PubMed] [Google Scholar]
- 11.Coyne JC, Kessler RC, Tal M, Turnbull J, Wortman CB, Greden JF. Living with a depressed person. J Consult Clin Psychol. 1987;55:347–352. doi: 10.1037//0022-006x.55.3.347. [DOI] [PubMed] [Google Scholar]
- 12.Dixon L, Stewart B, Burland J, Delahanty J, Lucksted A, Joffman M. Pilot study of the effectiveness of the Family-to-Family Education Program. Psychiatr Serv. 2001;52:965–967. doi: 10.1176/appi.ps.52.7.965. [DOI] [PubMed] [Google Scholar]
- 13.Sherman M. The Support and Family Education (SAFE) Program: mental health facts for families. Psychiatr Serv. 2003;54:35–37. doi: 10.1176/appi.ps.54.1.35. [DOI] [PubMed] [Google Scholar]
- 14.Miklowitz DJ, Scott J. Psychosocial treatments for bipolar disorder: cost-effectiveness, mediating mechanisms, and future directions. Bipolar Disord. 2009;11:110–122. doi: 10.1111/j.1399-5618.2009.00715.x. [DOI] [PubMed] [Google Scholar]
- 15.First MB, Spitzer RL, Gibbon M, et al. New York: Biometrics Research Department; 1997. Structured clinical interview for DSM-IV Axis I disorders-non-patient edition (SCID-I/NP, version 2.0, 4/97 revisions) [Google Scholar]
- 16.Pollak CP, Perlick D. Sleep problems and institutionalization of the elderly. J Geriatr Psychiatry Neurol. 1991;4:204–210. doi: 10.1177/089198879100400405. [DOI] [PubMed] [Google Scholar]
- 17.Burton LC, Newsom JT, Schulz R, Hirsch CH, German PS. Preventative health behaviors among spousal caregivers. Prev Med. 1997;26:162–169. doi: 10.1006/pmed.1996.0129. [DOI] [PubMed] [Google Scholar]
- 18.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 19.Platt S, Weyman A, Hirsch S, Hewett S. The Social Behavior Assessment Schedule (SBAS): rationale, contents, scoring and reliability of a new interview schedule. Soc Psychiatry Psychiatr Epidemiol. 1980;15:43–55. [Google Scholar]
- 20.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity, and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 22.Sheehan DV, Lecrubier Y. English version 5.0.0. Tampa: University of South Florida; 1998. M.I.N.I Plus. Mini international neuropsychiatric interview. [Google Scholar]
- 23.Rush AJ, Trivdei MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinical Rating (QIDS-C), and Self-Report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 25.Folkman S, Lazarus RS. Coping as a mediator of emotion. J Pers Soc Psychol. 1988;54:466–475. [PubMed] [Google Scholar]
- 26.MacCarthy B, Brown R. Psychosocial factors in Parkinson's disease. Br J Clin Psychol. 1989;28:41–52. doi: 10.1111/j.2044-8260.1989.tb00810.x. [DOI] [PubMed] [Google Scholar]
- 27.Miklowitz DJ. Bipolar Disorder: A Family-Focused Treatment Approach. 2nd ed. New York: The Guilford Press; 2008. [Google Scholar]
- 28.Weisman AG, Okazaki S, Gregory J, et al. Evaluating therapist competency and adherence to behavioral family management with bipolar patients. Fam Proc. 1998;37:107–121. doi: 10.1111/j.1545-5300.1998.00107.x. [DOI] [PubMed] [Google Scholar]
- 29.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;9:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 30.Reinares M, Colom F, Sanchez-Moreno J, et al. Impact of caregiver group psychoeducation on the course and outcome of bipolar patients in remission: a randomized controlled trial. Bipolar Disord. 2008;10:511–519. doi: 10.1111/j.1399-5618.2008.00588.x. [DOI] [PubMed] [Google Scholar]
- 31.Perlick DA, Rosenheck RR, Clarkin JF, Raue P, Sirey J. Impact of family burden and patient symptom status on clinical outcome in bipolar affective disorder. J Nerv Ment Dis. 2001;189:31–37. doi: 10.1097/00005053-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Perlick DA, Rosenheck RA, Clarkin JF, et al. Impact of family burden and affective response on clinical outcome among patients with bipolar disorder. Psychiatr Serv. 2004;55:1029–1035. doi: 10.1176/appi.ps.55.9.1029. [DOI] [PubMed] [Google Scholar]
- 33.Stephens MAP, Norris VK, Kinney JM, Ritchie SW, Grotz RC. Stressful situations in caregiving: relations between caregiver coping and well-being. Psychol Aging. 1988;3:208–209. doi: 10.1037//0882-7974.3.2.208. [DOI] [PubMed] [Google Scholar]
- 34.Wallhagen MI. Perceived control and adaptation in elder caregivers: development of an explanatory model. Interna J Ag Hum Devel. 1993;36:219–237. doi: 10.2190/ba90-aqx3-t6ce-abek. [DOI] [PubMed] [Google Scholar]
- 35.Sherman MD, Carothers R. Applying the readiness to change model to implemention of family intervention for serious mental illness. Comm Ment Health J. 2005;41:115–127. doi: 10.1007/s10597-005-2647-8. [DOI] [PubMed] [Google Scholar]
- 36.Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: a 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419–426. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldstein T, Miklowitz DJ, Richards JA. Expressed emotion attitudes and individual psychopathology among the relatives of bipolar patients. Fam Proc. 2002;41:645–657. doi: 10.1111/j.1545-5300.2002.00645.x. [DOI] [PubMed] [Google Scholar]
- 38.Brown GW, Birley LT, Wing JK. Influence of family life on the course of schizophrenic disorders: a replication. Br J Psychiatry. 1972;121:241–258. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- 39.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 40.American Psychiatric Association. Practice Guidelines for Treatment of Patients with Bipolar Disorder. 2nd ed. Washington, DC: American Psychiatric Association Press; 2002. [Google Scholar]
- 41.Dixon L. Providing services to families of persons with schizophrenia: present and future. J Ment Health Policy Econ. 1999;2:3–8. doi: 10.1002/(sici)1099-176x(199903)2:1<3::aid-mhp31>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 42.Greenhouse WJ, Meyer B, Johnson SL. Coping and medication adherence in bipolar disorder. J Affect Disord. 2000;59:237–241. doi: 10.1016/s0165-0327(99)00152-4. [DOI] [PubMed] [Google Scholar]