Abstract
Objective
The aim of the current study was to evaluate family functioning, social support, and functional impairment as predictors of mood symptoms one year following acute phase treatment for bipolar I disorder. This study builds upon the extant literature by evaluating these putative psychosocial risk factors simultaneously to determine whether they account for unique variance in clinical outcomes.
Method
Patients (N = 92) were recruited from hospital settings during an acute mood episode to participate in pharmacological or combined family and pharmacological interventions. The Modified Hamilton Rating Scale for Depression, Bech-Rafaelson Mania Scale, Family Assessment Device, Interpersonal Support Evaluation List, and UCLA Social Attainment Survey were administered at acute phase treatment completion and again at 1 year follow-up. Controlling for mood symptom severity at acute phase treatment completion, multiple regression analyses were used to examine longitudinal associations between the psychosocial variables and subsequent depressive and manic symptoms.
Results
None of the aforementioned psychosocial variables predicted manic symptomatology, and social support alone emerged as a unique predictor of depression at the 1 year follow-up. Effects of social support were moderated by recovery status, such that the strength of association between social support and subsequent depression was stronger for those who had not fully recovered during the acute phase of treatment than for those who had.
Conclusions
Low levels of social support at acute phase treatment completion, especially in concert with residual symptomatology, may place individuals with bipolar I disorder at risk for subsequent depressive symptoms. These data suggest that maintenance therapies focused on improving level of social support might be especially important to consider in the management of bipolar depression, and add to a growing literature focused on unique versus shared effects of psychosocial risk factors for poor illness course in bipolar disorder.
1. Introduction
Bipolar disorder is a highly recurrent illness with significant morbidity. Indeed, over 90% of patients report multiple affective episodes across their lifetimes [1], and extended periods of subthreshold symptomatology represent the norm, rather than the exception, for people suffering from the illness. Results from recent large-scale, prospective studies have revealed that patients remain symptomatically ill for roughly 50% of their lives, with depressive symptoms outnumbering manic symptoms three-fold [2, 3]. The predominance of depression over the long-term course of bipolar disorder is particularly alarming, as it has been shown to confer significant mortality risk due to suicide [4].
The significant morbidity and mortality associated with bipolar disorder is particularly notable in light of the emergence of several promising pharmacological and psychosocial treatments for bipolar disorder [5]. Given the availability of interventions that have demonstrated efficacy for the acute treatment of bipolar illness, it is important to turn attention to the question of who does, and who does not, maintain treatment gains over time. Identification of immediate post-treatment risk factors for subsequent mood symptoms would advance an understanding of who is at increased risk for poor illness course following acute phase treatment, and might also illuminate potential targets for treatment in maintenance therapies.
Although there are several demographic (e.g., socioeconomic status), clinical course (e.g., age of onset), and biological (e.g., genetic loading) variables that one could evaluate as immediate post-treatment risk factors for subsequent mood symptoms in bipolar disorder, it is notable that the majority of such risk factors are fixed and unalterable. As an alternative, the current study focused specifically on psychosocial risk factors, as they are malleable and potentially amenable to change. In particular, we evaluated three putative risk factors that have received considerable attention in the research literature; family functioning, social support, and functional impairment. Poor family functioning and low social support have each been shown to be predictive of subsequent mood symptom levels [6-9] and of episode recurrence [10-12] in naturalistic studies of bipolar samples. Although functional impairment has been evaluated primarily as an outcome of bipolar disorder [13], there is emerging data that functional impairment may also be predictive of subsequent symptomatology [14] and onset of new episodes [15].
When symptom based outcomes have been evaluated, there is mounting evidence that the effects of social support and functional impairment on course of bipolar disorder may be polarity-specific, with effects for depression but not for mania [11, 14, 16]. Results from studies of family functioning suggest that family difficulties may be predictive of both depressive [8, 9] and manic [8, 12] symptoms. Thus, additional research investigating these variables in bipolar disorder would benefit from the evaluation of continuous, symptom-based outcomes (versus presence or absence of any mood episode), especially in light of evidence that patients spend a significant portion of their lives experiencing some level of residual symptomatology [2]. In addition, with few exceptions [9, 11, 15], the majority of studies that have evaluated the impact of family functioning, social support, and functional impairment on the course of bipolar illness have evaluated these variables independently of one another. Thus, it is unclear whether these variables each account for unique variance in bipolar outcomes, or whether they represent more global psychosocial risk.
In an effort to advance an understanding of psychosocial risk factors for poor illness course following treatment completion, the aim of the current study was to evaluate immediate post-treatment measures of family functioning, social support, and functional impairment as predictors of mood symptoms one year following acute phase treatment for bipolar I disorder. Although prior research from our group has used subsets of data from the same clinical trial to evaluate longitudinal associations between social support [7], family functioning [17], and functional impairment [14] and mood symptoms, these studies have evaluated such risk factors independently of one another, and have not specifically evaluated such variables as predictors of mood symptoms during the period between the end of acute phase treatment and one year follow-up. The current study builds upon prior research by focusing on this critical time period for patients, and by simultaneously evaluating psychosocial risk factors to determine whether they account for unique variance in clinical outcomes. One additional strength of the current study is that it focused on continuous, symptom-based outcomes in order to evaluate polarity-specific effects.
2. Method
2.1. Participants
Participants were patients with bipolar I disorder (N = 92) who were recruited from inpatient and partial hospitalization programs at a university-affiliated hospital to participate in a clinical trial of pharmacological and family interventions [18]. At the time of study entry, participants were required to meet criteria for a diagnosis of bipolar I disorder (current episode manic, depressed, or mixed) according to the Structured Clinical Interview for DSM-III-R Axis I disorders (SCID-I) [19]. Relevant to the current study, participants were also required to be living with or in regular contact with a significant other (e.g., partner, parent, child). Additional inclusion and exclusion criteria are described in greater detail elsewhere [18]. Sociodemographic and clinical characteristics of study participants are summarized in Table 1.
Table 1.
Sociodemographic and clinical characteristics of study participants
| n | % | Mean | SD | |
|---|---|---|---|---|
| Female | 52 | 57 | ||
| Caucasian | 86 | 94 | ||
| Age (years) | 39 | 11.5 | ||
| Marital status | ||||
| Married/cohabiting | 62 | 68 | ||
| Divorced, separated, widowed | 16 | 17 | ||
| Single, never married | 14 | 15 | ||
| Episode at study entry | ||||
| Manic | 69 | 75 | ||
| Depressed | 18 | 20 | ||
| Mixed | 5 | 5 | ||
| Age of first episode (years) | ||||
| Manic | 28 | 10.6 | ||
| Depressive | 22 | 9.5 | ||
2.2. Measures
All assessments were conducted by bachelor’s and master’s level clinical raters. Raters were blind to treatment assignment for purposes of follow-up assessment. The 17-item Modified Hamilton Rating Scale for Depression (MHRSD) [20] and the 11-item Bech-Rafaelson Mania Scale (BRMS) [21] were used to assess depressive and manic symptom severity, respectively. Both the MHRSD and the BRMS are widely used interview-based instruments that have established psychometric properties [20-22], and the MHRSD has been shown to correlate significantly with the original Hamilton Rating Scale [20].
The 12-item General Functioning subscale of the Family Assessment Device (FAD-GF) [23] was used as a self-report measure of family functioning1. Subscale scores on the FAD range from 1 to 4, with higher scores representing poorer family functioning. A clinical cutoff score of 2.0 has been specified to identify families that fall within the range of unhealthy functioning on the FAD-GF subscale [24]. The FAD-GF has been widely used and has demonstrated strong psychometric performance [24]. Internal consistency reliability was high in the current study (Cronbach’s α = 0.91).
Social support was assessed using the 40-item self-report Interpersonal Support Evaluation List (ISEL) [25]. The ISEL has been widely used to measure social support in nonclinical [e.g., 26-30] and clinical samples [e.g., 31-33], including those comprised of individuals with bipolar disorder [6, 7, 34]. ISEL total scores are comprised of 4 subscales: tangible assistance (material aid), appraisal (availability of someone to talk about one’s problems), self-esteem (positive appraisal of self from others and positive comparison of oneself to others), and belonging (availability of people with whom one can do things). Responses are coded such that higher scores reflect greater levels of social support. Extensive data on the psychometric properties of the ISEL have been published elsewhere [35]. Internal consistency reliability of the ISEL was high in the current study (Cronbach’s α = 0.94).
The interview-based UCLA Social Attainment Survey (SAS) [36] was used to measure functional impairment. It includes 7 items that assess peer functioning (SAS-P), romantic relationship functioning (SAS-R), and involvement in activities (SAS-A). For purposes of the current analysis, we utilized the SAS-A subscale as it is not confounded by family/interpersonal functioning (which were assessed by the FAD-GF and ISEL) and focuses instead on involvement in activities outside the home. The SAS and its subscales have been used in several studies to evaluate functional impairment in bipolar disorder [37-40], as well as other severe mental illnesses [41, 42]. In the current study, the SAS demonstrated acceptable internal consistency reliability (Cronbach’s α = .66).
2.3 Procedures
Patients were approached during an acute mood episode to determine their willingness to participate in an institutional review board-approved clinical trial. After a complete description of the study, patients and their family members provided written informed consent if they agreed to participate. As described in greater detail elsewhere [18], patients were randomly assigned to receive 4 months of acute outpatient treatment consisting of pharmacotherapy alone, pharmacotherapy plus multifamily psychoeducation group therapy, or pharmacotherapy plus family therapy. Following completion of the acute phase of treatment, all study patients, regardless of treatment assignment, were treated with maintenance pharmacotherapy on an outpatient basis for up to 24 months. For those participants who were randomized to receive pharmacotherapy plus family therapy, additional family therapy sessions were offered over the maintenance phase of treatment, on an as-needed basis. Symptom severity and psychosocial functioning assessments collected immediately following the acute phase of treatment and symptom severity assessments collected at 1 year post-treatment were used in the current study analyses.
3. Results
3.1 Descriptive data
Data were available for 72% (n = 66) of the total sample at acute phase treatment completion, and for 49% (n = 45) of the total sample at 1 year post-treatment. Results from preliminary analyses using independent samples t-tests revealed no significant differences on demographic characteristics (all ps ≥ 0.46) or baseline mood symptom levels (all ps ≥ 0.40) between those included in the analyses versus those excluded from analysis due to missing data. Of the participants for whom there were data available, 42% (n = 28) met criteria for episode recovery, 32% (n = 21) were partially symptomatic, and 26% (n = 17) were symptomatic following acute phase treatment, as defined using published clinical cutoffs for the BRMS (BRMS ≤ 5) and MHRSD (MHRSD ≤ 7). Means, standard deviations, and intercorrelations between study variables are presented in Table 2.
Table 2.
Means, Standard Deviations, and Intercorrelations Between All Study Variables
| Mean | SD | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. MHRSD | 8.62 | 6.89 | .15 | .11 | -.22 | -.26* | .54** | .37** |
| 2. BRMS | 3.41 | 5.12 | _ | .39** | -.25 | .08 | -.03 | .05 |
| 3. FAD-GF | 2.10 | 0.55 | _ | -.44** | -.22 | .22 | -.08 | |
| 4. ISEL | 81.42 | 21.49 | _ | .34** | -.48** | -.13 | ||
| 5. SAS-A | 2.99 | 1.04 | _ | -.21 | -.03 | |||
| 6. T2 MHRSD | 6.85 | 5.69 | _ | .40** | ||||
| 7. T2 BRMS | 2.49 | 4.10 | _ |
Note. MHRSD = Modified Hamilton Rating Scale for Depression at acute phase treatment completion; BRMS = Bech-Rafaelson Mania scale at acute phase treatment completion; FAD-GF = Family Assessment Device – General Functioning at acute phase treatment completion; ISEL = Interpersonal Support Evaluation List at acute phase treatment completion; SAS-A = UCLA Social Attainment Survey – Involvement in Activities at acute phase treatment completion; T2 MHRSD = MHRSD at 1 year post-treatment; T2 BRMS = BRMS at 1 year post-treatment.
p ≤ .05.
p ≤ .01.
3.2 Psychosocial predictors of mania 1 year following acute phase treatment
Results from multiple regression analysis revealed that, controlling for immediate post-treatment BRMS score, neither general family functioning (F(1,44) = 0.63, p = .43, sr = -0.13), social support (F(1,44) = 0.70, p = .41, sr = -0.14), nor functional impairment (F(1,44) = 0.07, p = .80, sr = -0.04) were predictive of manic symptom levels at the 1 year follow-up. In fact, the omnibus test revealed that, together as a set, these variables accounted for only 3% of the variance in mania outcomes (R2 = 0.03, F(4,41) = 0.30, p = 0.87).
3.3 Psychosocial predictors of depression 1 year following acute phase treatment
Results from multiple regression analysis revealed that, controlling for immediate post-treatment MHRSD score, social support emerged as a unique predictor of depressive symptomatology at the 1 year follow-up (F(1,44) = 10.41, p = .003, sr = -0.37). However, neither general family functioning (F(1,44) = 0.17, p = .68, sr = 0.05) nor functional impairment (F(1,44) = 0.40, p = .53, sr = 0.07) were uniquely predictive of subsequent depression symptoms. The omnibus test revealed that, together as a set, these variables accounted for 53% of the variance in depression outcomes (R2 = 0.53, F(4,41) = 10.24, p = .00), although this effect was primarily explained by the large percentage in variance accounted for by MHRSD at immediate post-treatment (F(1,44) = 19.57, p = .00, sr = 0.50).
When ISEL subscales were evaluated simultaneously in the model, to examine whether particular aspects of social support were more strongly associated with outcome than others, none of the specific ISEL subscales accounted for unique variance in depression symptom outcomes (ps = .17 - .97). Given the rather high internal consistency reliability of the full ISEL, this finding was most likely due to the strong intercorrelation between ISEL items, and suggests that current study data are best interpreted within the context of an overall level of social support.
3.4 Influence of maintenance treatment on associations between psychosocial risk factors and depression symptom outcome
Of the 45 participants for whom follow-up data were available, 76% (n = 34) received maintenance pharmacotherapy alone and 13% (n = 6) received maintenance pharmacotherapy plus family therapy (with a mean of 6.7(SD = 6.5) sessions). The remaining 11% (n = 5) dropped out of randomized treatment following the acute phase, and therefore did not receive study maintenance treatment. However, these individuals continued to be assessed over the follow-up period. In order to rule out maintenance treatment received as one potential explanation for the association between psychosocial risk factors and depression symptom outcome, study analyses were repeated using an orthogonal set of Helmert contrast codes [43] evaluating the impact of receiving any versus no maintenance study treatment, as well as the impact of receiving any versus no additional family therapy.
Multiple regression analysis revealed that, over and above immediate post-treatment MHRSD and maintenance treatment received, social support remained a unique predictor of depressive symptoms at the one year follow-up, (F(1,44) = 11.53, p = .002, sr = -0.38), whereas general family functioning (F(1,44) = 0.07, p = .79, sr = 0.03) and functional impairment (F(1,44) = 0.29, p = .59, sr = 0.06) failed to account for unique variance in depression symptom outcome.
3.5 Recovery status as a moderator of depression symptom outcome
Finally, given the varying degree of response to treatment, effects of social support on depression were reexamined to determine if and how recovery status of patients following acute phase treatment might have influenced study findings. To do so, MHRSD scores at 1 year post-treatment were regressed onto immediate post-treatment ISEL, a contrast-coded predictor of recovery status (-1 = not recovered, 1 = recovered), and the interaction between ISEL and recovery status.2 Over and above the simple effects of social support (F(1,44) = 9.97, p = .003) and recovery status (F(1,44) = 12.10, p = .001), results revealed a significant ISEL × Recovery interaction (B = .066, SE(B) = .028, F(1,44) = 5.47, p = 0.02) such that the strength of association between immediate post-treatment social support and depression at 1 year follow-up was stronger for those who had not recovered from a mood episode than for those who had. A depiction of this finding is presented in Figure 1.
Figure 1.
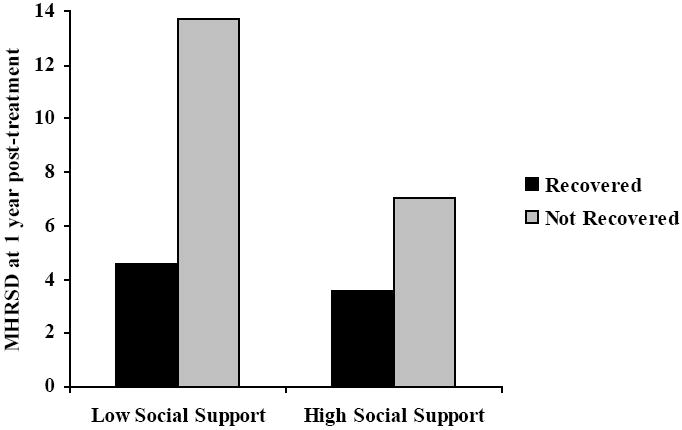
Recovery Status Moderates the Association Between Immediate Post-Treatment Social Support and Depression at 1 Year Follow-Up
4. Discussion
The aim of this study was to investigate psychosocial predictors of mood symptoms one year following acute phase treatment for bipolar I disorder, with a specific focus on evaluating the unique effects of family functioning, social support, and functional impairment. Study results indicated that none of the aforementioned psychosocial variables predicted subsequent manic symptomatology, and social support alone emerged as a unique predictor of depression one year following acute phase treatment. These data are consistent with prior studies of social support as a predictor of depression in naturalistic follow-up samples [6, 7, 11], and extend the research literature by suggesting that low levels of social support following the completion of acute phase treatment may place individuals with bipolar disorder at risk for subsequent depressive symptoms.
Additional analysis further revealed that the combination of low social support and residual symptomatology following the acute phase of treatment may confer particularly high risk for depression symptoms over time. Thus, these individuals might especially benefit from adjunctive maintenance psychotherapy treatments that aim to improve perceived or actual social supports [e.g., 44, 45]. Although social support predicted depression over and above maintenance treatment received in the current study, it is notable that only a small percentage of patients received additional family intervention over the maintenance phase, and average number of sessions was limited (i.e., 6.7 sessions over 12 months). Further, family therapy may address only one (albeit important) component of social support, which has been theorized to extend beyond the family into other social realms [46].
It should also be noted that the simple effect for social support remained a significant predictor of subsequent depression in the moderator analysis. Consequently, although the strength of effect was stronger for those who had not recovered following acute phase treatment, there nevertheless remained an increased risk for depressive symptoms among all patients who reported low levels of social support upon treatment completion. Given this documented risk, further research is necessary in order to evaluate whether social support is an important intervention target for maintenance psychotherapies for bipolar disorder, and whether such interventions will be more efficacious for those who report lower levels of social support upon completion of acute phase treatment. Conversely, this research may also be used to investigate whether maintenance pharmacotherapy alone is sufficient for those individuals who experience recovery and report higher levels of social support following acute phase treatment for an index mood episode.
Notably, when all three study variables were evaluated together, neither general family functioning nor functional impairment predicted subsequent depressive symptomatology. Moreover, results were unchanged when specific dimensions of family functioning were evaluated. This finding was surprising in light of evidence from prior research that each of these variables, when evaluated independently, have been shown to confer risk for mood symptoms in patients with bipolar disorder [8, 12, 14, 15]. One possible explanation for this finding is that the effects of family functioning and functional impairment are better accounted for by their shared variance with social support. Indeed, measures of functional impairment used in prior research have been typically multidimensional, and include a social/interpersonal component [13-15]. Further, family functioning, by definition, is an interpersonal construct. However, we cannot conclude whether other specific realms of family functioning, such as those defined in the expressed emotion (EE) construct [8, 9], would predict bipolar mood symptoms over and above social support. Future research that employs specific measures of family functioning that are not assessed by the FAD would help clarify this question.
On a final note, current study data are also consistent with polarity-specific models linking many psychosocial constructs, especially those interpersonal in nature, to depression versus mania in bipolar samples [16]. Indeed, even when evaluated together as a set, family functioning, social support, and functional impairment explained only 3% of the variance in manic symptom outcomes. Nevertheless, it is important to note that psychosocial variables are not irrelevant toward an understanding of the long-term course of mania. It has been argued that mania may be linked to specific psychosocial variables related to sleep and behavioral activation [6, 47], and future research that incorporates psychosocial variables associated with both depressive and manic symptom outcomes would add to an understanding of what predicts better or poorer illness course following completion of acute phase treatment for bipolar I disorder.
Study limitations should be considered when interpreting the above data. Given the predominantly Caucasian sample, inclusion of bipolar I disorder only, and the modest rates of retention at follow-up, generalizability to larger, more diverse patients, and to those with bipolar II disorder, is limited. Larger samples would also allow for the examination of potential bidirectional associations between psychosocial risk factors and mood symptoms in bipolar illness. The focus on family interventions in the larger treatment trial, with a requirement that a significant other participate in the study, may have influenced levels of psychosocial functioning. As such, it is unclear how study results might generalize to individuals with bipolar disorder who cannot readily identify a significant family relationship, and future research is needed to determine if study findings will extend to periods following different types of acute phase treatment (e.g., individual CBT) [48]. Finally, it should be noted that all assessments of psychosocial functioning were self-report in nature, and therefore reflect patient perceptions of family functioning, social support, and functional impairment. Future research that employs objective ratings of psychosocial functioning would further enhance this growing area of study.
In conclusion, current study data indicated that, after controlling for the effects of family functioning and functional impairment, social support emerged as a unique predictor of depression severity one year following acute phase treatment for bipolar I disorder. Further, the combination of low social support and residual symptomatology may confer especially high risk for depression in bipolar illness. These data suggest that maintenance therapies focused on improving level of social support might be especially important to consider in the management of bipolar depression, and add to a growing literature focused on unique versus shared effects of psychosocial risk factors for poor illness course in bipolar disorder.
Acknowledgments
This research was supported by grant R01MH048171 from the National Institute of Mental Health. Preparation of this manuscript was supported by grant K23MH079907 from the National Institute of Mental Health and a Young Investigator Award from the American Foundation for Suicide Prevention, both awarded to Dr. Weinstock.
Footnotes
It is of note that the full FAD contains 6 additional subscales that assess the following specific dimensions of family functioning: problem solving, communication, roles, affective responsiveness, affective involvement, and behavior control. When study analyses were repeated using the specific dimensions of family functioning from the FAD, the direction and strength of study effects were similar to those reported using FAD-GF subscale only. For ease of interpretation, only results using the FAD-GF are presented in the text.
The analysis of the ISEL × Recovery interaction as a predictor of depression at 1 year post-treatment did not include immediate post-treatment MHRSD scores as a covariate. This decision was made because MHRSD scores at immediate post-treatment were used, in part, to calculate recovery status, and are therefore redundant with the contrast-coded Recovery Status variable. However, when the analysis was repeated, regressing MHRSD scores at 1 year post-treatment onto immediate post-treatment MHRSD, ISEL, and the interaction between ISEL and MHRSD, results were similar to those found for the original moderator analysis. Specifically, there was a significant effect for the ISEL × MHRSD interaction such that the association between social support and depression at 1 year post-treatment was stronger for those who had higher (vs. lower) depression scores at immediate post-treatment (B = -.015, SE(B) = .004, F(1,44) = 13.65, p = .001).
Study findings were presented in part at the annual meeting of the Association for Behavioral and Cognitive Therapies, Orlando, FL, 2008.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Solomon DA, Keitner GI, Miller IW, Shea MT, Keller MB. Course of illness and maintenance treatments for patients with bipolar disorder. J Clin Psychiatry. 1995;56:5–13. [PubMed] [Google Scholar]
- 2.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 3.Post RM, Denicoff KD, Leverich GS, Altshuler LL, Frye MA, Suppes TM, et al. Morbidity in 258 bipolar outpatients followed for 1 year with daily prospective ratings on the NIMH life chart method. J Clin Psychiatry. 2003;64:680–690. doi: 10.4088/jcp.v64n0610. [DOI] [PubMed] [Google Scholar]
- 4.Tondo L, Isacsson G, Baldessarini R. Suicidal behaviour in bipolar disorder: risk and prevention. CNS Drugs. 2003;17:491–511. doi: 10.2165/00023210-200317070-00003. [DOI] [PubMed] [Google Scholar]
- 5.Fountoulakis KN, Vieta E. Treatment of bipolar disorder: a systematic review of available data and clinical perspectives. Int J Neuropsychopharmacol. 2008;11:999–1029. doi: 10.1017/S1461145708009231. [DOI] [PubMed] [Google Scholar]
- 6.Johnson SL, Meyer B, Winett C, Small J. Social support and self-esteem predict changes in bipolar depression but not mania. J Affect Disord. 2000;58:79–86. doi: 10.1016/s0165-0327(99)00133-0. [DOI] [PubMed] [Google Scholar]
- 7.Johnson SL, Winett CA, Meyer B, Greenhouse WJ, Miller I. Social support and the course of bipolar disorder. J Abnorm Psychol. 1999;108:558–566. doi: 10.1037//0021-843x.108.4.558. [DOI] [PubMed] [Google Scholar]
- 8.Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. J Affect Disord. 2004;82:343–352. doi: 10.1016/j.jad.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Yan LJ, Hammen C, Cohen AN, Daley SE, Henry RM. Expressed emotion versus relationship quality variables in the prediction of recurrence in bipolar patients. J Affect Disord. 2004;83:199–206. doi: 10.1016/j.jad.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Bauwens F, Tracy A, Pardoen D, Vander Elst M, Mendlewicz J. Social adjustment of remitted bipolar and unipolar out-patients. A comparison with age- and sex-matched controls. Br J Psychiatry. 1991;159:239–244. doi: 10.1192/bjp.159.2.239. [DOI] [PubMed] [Google Scholar]
- 11.Cohen AN, Hammen C, Henry RM, Daley SE. Effects of stress and social support on recurrence in bipolar disorder. J Affect Disord. 2004;82:143–147. doi: 10.1016/j.jad.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Arch Gen Psychiatry. 1988;45:225–231. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- 13.Calabrese JR, Hirschfeld RM, Reed M, Davies MA, Frye MA, Keck PE, et al. Impact of bipolar disorder on a U.S. community sample. J Clin Psychiatry. 2003;64:425–432. doi: 10.4088/jcp.v64n0412. [DOI] [PubMed] [Google Scholar]
- 14.Weinstock LM, Miller IW. Functional impairment as a predictor of short-term symptom course in bipolar I disorder. Bipolar Disord. 2008;10:437–442. doi: 10.1111/j.1399-5618.2007.00551.x. [DOI] [PubMed] [Google Scholar]
- 15.Gitlin MJ, Swendsen J, Heller TL, Hammen C. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995;152:1635–1640. doi: 10.1176/ajp.152.11.1635. [DOI] [PubMed] [Google Scholar]
- 16.Johnson SL, Winters R, Meyer B. A polarity-specific model of bipolar disorder. In: Joiner TE, Brown JS, Kistner J, editors. The interpersonal, cognitive, and social nature of depression. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2006. pp. 153–171. [Google Scholar]
- 17.Uebelacker LA, Beevers CG, Battle C, Strong D, Keitner G, Solomon D, et al. Family functioning in bipolar disorder. J Fam Psychol. 2006;4:701–704. doi: 10.1037/0893-3200.20.4.701. [DOI] [PubMed] [Google Scholar]
- 18.Miller IW, Solomon DA, Ryan CE, Keitner GI. Does adjunctive family therapy enhance recovery from bipolar I mood episodes? J Affect Disord. 2004;82:431–436. doi: 10.1016/j.jad.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-III-R, Patient Version. New York: Biometrics Research Department, New York State Psychiatric Institute; 1987. [Google Scholar]
- 20.Miller IW, Bishop S, Norman WH, Maddever H. The Modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Res. 1985;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- 21.Bech P, Rafaelsen OJ, Kramp P, Bolwig TG. The mania rating scale: scale construction and inter-observer agreement. Neuropharmacology. 1978;17:430–431. doi: 10.1016/0028-3908(78)90022-9. [DOI] [PubMed] [Google Scholar]
- 22.Bech P. The Bech-Rafaelsen Mania Scale in clinical trials of therapies for bipolar disorder: a 20-year review of its use as an outcome measure. CNS Drugs. 2002;16:47–63. doi: 10.2165/00023210-200216010-00004. [DOI] [PubMed] [Google Scholar]
- 23.Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. J Marital Fam Ther. 1983;9:171–180. [Google Scholar]
- 24.Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. J Marital Fam Ther. 1985;11:345–356. [Google Scholar]
- 25.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 26.Bates DS, Toro PA. Developing measures to assess social support among homeless and poor people. J Community Psychology. 1999;27:137–156. [Google Scholar]
- 27.Brookings JB, Bolton B. Confirmatory factor analysis of the Interpersonal Support Evaluation List. Am J Community Psychology. 1988;16:137–147. doi: 10.1007/BF00906076. [DOI] [PubMed] [Google Scholar]
- 28.Delistamati E, Samakouri MA, Davis EA, Vorvolakos T, Xenitidis K, Livaditis M. Interpersonal Support Evaluation List (ISEL)--college version: validation and application in a Greek sample. Int J Soc Psychiatry. 2006;52:552–560. doi: 10.1177/0020764006074184. [DOI] [PubMed] [Google Scholar]
- 29.Sarkadi A, Bremberg S. Socially unbiased parenting support on the Internet: a cross-sectional study of users of a large Swedish parenting website. Child Care Health Dev. 2005;31:43–52. doi: 10.1111/j.1365-2214.2005.00475.x. [DOI] [PubMed] [Google Scholar]
- 30.Schonfeld IS. Dimensions of functional social support and psychological symptoms. Psychol Med. 1991;21:1051–1060. doi: 10.1017/s003329170003004x. [DOI] [PubMed] [Google Scholar]
- 31.Chen CH, Tseng YF, Chou FH, Wang SY. Effects of support group intervention in postnatally distressed women. A controlled study in Taiwan. J Psychosom Res. 2000;49:395–399. doi: 10.1016/s0022-3999(00)00180-x. [DOI] [PubMed] [Google Scholar]
- 32.Degen HM, Myers BJ, Williams-Petersen MG, Knisely JS, Schnoll SS. Social support and anxiety in pregnant drug abusers and nonusers: unexpected findings of few differences. Drug Alcohol Depend. 1993;32:37–44. doi: 10.1016/0376-8716(93)90020-q. [DOI] [PubMed] [Google Scholar]
- 33.Thomas JL, Jones GN, Scarinci IC, Brantley PJ. Social support and the association of type 2 diabetes and depressive and anxiety disorders among low-income adults seen in primary care clinicis. J Clin Psychol Med Settings. 2007;14:351–359. [Google Scholar]
- 34.Johnson L, Lundstrom O, Aberg-Wistedt A, Mathe AA. Social support in bipolar disorder: its relevance to remission and relapse. Bipolar Disord. 2003;5:129–137. doi: 10.1034/j.1399-5618.2003.00021.x. [DOI] [PubMed] [Google Scholar]
- 35.Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IB, Sarason BR, editors. Social support: Theory, research, and applications. The Hague, the Netherlands: Martinus Nojhof; 1985. pp. 73–94. [Google Scholar]
- 36.Goldstein MJ. Further data concerning the relation between premorbid adjustment and paranoid symptomatology. Schizophr Bull. 1978;4:236–243. doi: 10.1093/schbul/4.2.236. [DOI] [PubMed] [Google Scholar]
- 37.Feske U, Frank E, Mallinger AG, Houck PR, Fagiolini A, Shear MK, et al. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry. 2000;157:956–962. doi: 10.1176/appi.ajp.157.6.956. [DOI] [PubMed] [Google Scholar]
- 38.George EL, Miklowitz DJ, Richards JA, Simoneau TL, Taylor DO. The comorbidity of bipolar disorder and axis II personality disorders: prevalence and clinical correlates. Bipolar Disord. 2003;5:115–122. doi: 10.1034/j.1399-5618.2003.00028.x. [DOI] [PubMed] [Google Scholar]
- 39.Meyer B. Coping with severe mental illness: Relations of the brief COPE with symptoms, functioning, and well-being. J Psychopathol Behav Assess. 2001;23:265–277. [Google Scholar]
- 40.Rea MM, Tompson MC, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. J Consult Clin Psychol. 2003;71:482–492. doi: 10.1037/0022-006x.71.3.482. [DOI] [PubMed] [Google Scholar]
- 41.Subotnik KL, Nuechterlein KH, Ventura J. MMPI discriminators of deficit vs. non-deficit recent-onset schizophrenia patients. Psychiatry Res. 2000;93:111–123. doi: 10.1016/s0165-1781(00)00102-5. [DOI] [PubMed] [Google Scholar]
- 42.Torgalsboen AK. Consumer satisfaction and attributions of improvement among fully recovered schizophrenics. Scand J Psychol. 2001;42:33–40. doi: 10.1111/1467-9450.00212. [DOI] [PubMed] [Google Scholar]
- 43.Judd CM, McClelland GH. Data Analysis: A Model Comparison Approach. San Diego, CA: Harcourt, Brace, Jovanovich; 1989. [Google Scholar]
- 44.Bauer MS. Supporting collaborative practice management: The Life Goals Program. In: Johnson SL, Leahy RL, editors. Psychological Treatment of Bipolar Disorder. New York: Guilford; 2004. pp. 203–225. [Google Scholar]
- 45.Frank E, Swartz HA. Interpersonal and social rhythm therapy. In: Johnson SL, Leahy RL, editors. Psychological Treatment of Bipolar Disorder. New York: Guilford; 2004. pp. 162–183. [Google Scholar]
- 46.Barrera MJ. Distinctions between social support concepts, measures, and models. Am J Community Psychology. 1986;14:413–445. [Google Scholar]
- 47.Johnson SL, Sandrow D, Meyer B, Winters R, Miller I, Solomon D, et al. Increases in manic symptoms after life events involving goal attainment. J Abnorm Psychol. 2000;109:721–727. doi: 10.1037//0021-843x.109.4.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Basco MR, Rush AJ. Cognitive-behavioral therapy for bipolar disorder. New York: Guilford; 1996. [Google Scholar]


