Abstract
Patients with acute myeloid leukemia (AML) frequently fail chemotherapy due to refractory disease, relapse, or toxicity. Among older AML patients (age > 60 years), there are few long-term survivors. Lenalidomide is a candidate for study in AML based on its clinical activity in a related disorder, myelodysplastic syndrome (MDS), with the 5q− chromosomal abnormality. We report induction of sustained morphologic and cytogenetic complete remission in 2 older AML patients treated with high-dose, single-agent lenalidomide; each patient had trisomy 13 as the sole cytogenetic abnormality. We show for the first time that lenalidomide has clinical activity in this poor-risk cytogenetic subset of AML. The clinical trials described in this paper have been registered with www.clinicaltrials.gov under identifiers NCT00466895 and NCT00546897.
Introduction
Advances in the treatment of AML, including cytogenetic and molecular risk stratification, have improved clinical outcomes for patients younger than 60 years of age.1–3 In contrast, older AML patients given standard cytotoxic treatments have a dismal prognosis with a median survival of less than 1 year.4,5 Poor outcomes in older patients, who constitute the bulk of AML cases, are related to the combination of unfavorable leukemia biology and comorbidities that limit treatment options.5,6 Thus, successful development of novel AML therapy requires not only improved understanding of leukemogenesis but also tolerability of the drug in older patients. Novel drug development strategies are assisted by identification of molecular markers or biologic features of disease associated with increased likelihood of clinical response to the treatment.
Lenalidomide is active against several hematologic malignancies and Food and Drug Administration–approved for both relapsed multiple myeloma and low-risk MDS with the 5q− cytogenetic abnormality. Cytogenetic responses observed in previous clinical trials of lenalidomide in MDS suggest that lenalidomide eliminated the abnormal MDS clone.7–9 The lenalidomide dose in these trials was limited to 10 mg per day by drug-related myelosuppression; this dose results in substantially lower plasma concentrations compared with higher dosing strategies.10,11 Because therapy-related myelosuppression is routine in AML treatment and may be necessary to obtain complete remissions, we explored the activity of higher doses of lenalidomide in AML in 2 independent clinical trials. We report here sustained morphologic and cytogenetic complete remission (CRc) achieved with high-dose lenalidomide in 2 older AML patients harboring trisomy 13 as the sole cytogenetic abnormality.
Case reports
At both institutions involved, protocols were approved by scientific review committees and then at local institutional review boards, and informed consent was obtained in accordance with the Declaration of Helsinki.
Case 1
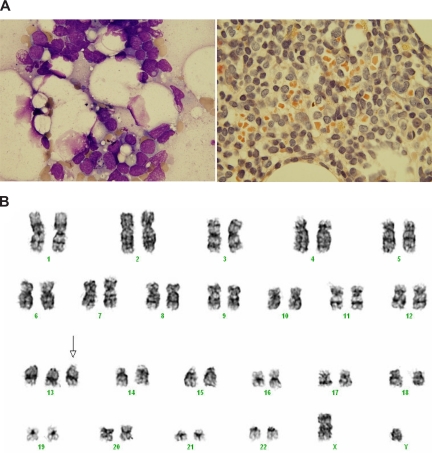
A 71-year-old man with no prior history of MDS presented with dyspnea and pancytopenia. Bone marrow (BM) biopsy showed 90% myeloblasts and undifferentiated (French-American-British [FAB] M0) AML (Figure 1A). Flow cytometry revealed that the blasts expressed CD34, CD33, CD13, and CD117. Metaphase cytogenetics showed trisomy 13 in 5 of 20 metaphase cells but no other abnormalities (Figure 1B). Fluorescent in situ hybridization (FISH) studies excluded abnormalities of chromosomes 5, 7, 8, and 11q23. Patient characteristics are summarized in Table 1.
Figure 1.
Bone marrow morphology and karyotype of case 1 at AML diagnosis. (A) Bone marrow aspirate blast morphology (left, Wright-Giemsa, ×100) and biopsy (right, Leder stain, ×100) demonstrating AML at diagnosis (stains were obtained from Richard-Allan Scientific, Kalamazoo, MI). The blast cells are medium-sized and have a high nuclear:cytoplasmic ratio, agranular Leder-negative cytoplasm, and visible nucleoli. Slides were viewed with an Olympus BX41 microscope (Olympus, Tokyo, Japan) at a 100×/1.30 NA oil objective with Resolve high-viscosity microscope immersion oil (Richard-Allan Scientific). Images were acquired using an Olympus DP70 camera and were processed with DP Controller 1.2.1.108 software (Olympus). Individual image files were assembled in Microsoft PowerPoint 2007. (B) AML karyotype showing trisomy 13 (arrow) at time of AML diagnosis (47,XY, + 13[5]/46,XY[15]).
Table 1.
Summary of AML cases
| Characteristic | Case 1 | Case 2 |
|---|---|---|
| Age, y | 71 | 68 |
| Performance status (ECOG) | 1 | 2 |
| WHO/FAB Dx | AML M0 | AML M2 |
| Prior AML therapy | No | FLAG chemotherapy at original presentation |
| Duration of prior remission | N/A | 3.5 y |
| Lenalidomide treatment | ||
| Cycle 1 | 50 mg/d, days 1-14; no therapy × 30 d | 35 mg/d, days 1-21 |
| Cycle 2 | 50 mg/d × 21 d; no therapy × 30 d | 35 mg days 1-4 (therapy halted due to pneumonia) |
| Cycle 3 | 35 mg days 1-21 | |
| Cycle 4 | (start of cycle delayed 3 wk until resolution of grade 2* neutropenia and thrombocytopenia) 35 mg days 1-21 | |
| Low-dose cycles | 10 mg/d, days 1-28, × 5; then low-dose therapy 10 mg/d, ongoing | |
| Prelenalidomide data | ||
| White blood cells | 1900/μL | 1700/μL |
| Hemoglobin | 6.7 g/dL | 9.3 g/dL |
| Platelets | 74 000/μL | 45 000/μL |
| ANC | 190/μL | 530/μL |
| PB blast | 363/μL (33%) | 0/μL |
| BM cellularity | 30% | 40% |
| BM blasts | 90% | 40% |
| Karyotype | 47,XY,+13[5]/46,XY[15] | 94<4n>,XXYY,+13,+13(cp15)/46,XY(3)/nonclonal(2) |
| Data at CR | ||
| Days to CR | 124 (35 d of high-dose therapy, 28 d of low-dose therapy) | 78 (25 d of treatment) |
| White blood cells | 6100/μL | 7500/μL |
| Hemoglobin | 10.1 g/dL | 8.6 g/dL |
| Platelets | 231 000/μL | 210 000/μL |
| ANC | 4148/μL | 4275/μL |
| BM cellularity | 60% | 40% |
| BM blast | < 5% | <5% |
| Duration of CR | 9 mo | 9 mo |
| CR confirmation | Yes (6 wk, 16 wk) | Yes (5 wk) |
WHO indicates World Heath Organization; ECOG, Eastern Cooperative Oncology Group; Dx, diagnosis; ANC, absolute neutrophil count; PB, peripheral blood; BM, bone marrow; and CR, complete remission.
Toxicity graded by National Cancer Institute Common Toxicity Criteria for Adverse Events, version 3.0.
After providing informed consent, the patient was treated on a Human Research Protection Office (HRPO)–approved clinical trial evaluating lenalidomide in untreated AML for patients older than 60 years of age at Washington University (clinicaltrials.gov: NCT00546897). Study therapy consisted of high-dose lenalidomide at 50 mg per day for 14 days, followed by 30 days off therapy, and then a second course of 50 mg per day for 21 days. Peripheral blood AML blasts cleared after the initial 14-day course of lenalidomide. At day 30, the BM biopsy showed 25% cellularity with 72% blasts and was FLT3-ITD–positive. After cycle 2 of high-dose lenalidomide, BM biopsy showed aplasia with less than 10% cellularity, though blasts were present, and he remained transfusion dependent. Cycle 2 was complicated by 2 episodes of neutropenic fever requiring hospitalization, for which he received G-CSF. Thirty days after completing the 2 high-dose cycles, he began low-dose lenalidomide (10 mg daily in 4-week cycles), as per the clinical protocol. After 21 days of low-dose lenalidomide, his blood cell counts normalized without transfusion or growth factors. At the completion of his first low-dose cycle (124 days from initiation of lenalidomide) BM showed 60% cellularity with less than 5% blasts. Cytogenetics showed no clonal abnormalities, and FLT3-ITD was negative. This CRc was confirmed on 2 subsequent BM biopsies at 6 and 16 weeks after the initial CRc. The patient continued on low-dose lenalidomide for 10 months, but subsequently relapsed (duration of CRc was 9 months).
Notably, 0/13 non–trisomy 13 abnormality AML patients treated on the Washington University clinical trial achieved CR, although 2 PRs were observed. There was one additional patient with trisomy 13 on the study, though the patient also had additional cytogenetic abnormalities as 48,XY + der(1)t(1,1)(p11;q25), + 13. This patient received only 6 days of lenalidomide before going off study due to infection.
Case 2
A 68-year-old man presented with marked pancytopenia and was found to have relapsed AML. Approximately 3.5 years earlier, he had been diagnosed with AML arising from MDS; at that time, he had normal karyotype. Due to medical comorbidities including ischemic cardiomyopathy at the original presentation, he received induction with fludarabine, cytarabine, and G-CSF (FLAG), and achieved CR1. He then received one cycle of cytarabine (1.5 g/m2 × 6 doses) consolidation, completing all therapy 3 years before the current relapse. At relapse, BM biopsy showed 40% myeloblasts and FAB M2 AML (see Table 1), and flow cytometry revealed myeloid blasts expressing CD13, HLA-DR, CD33, and CD34, with subpopulations expressing CD15, CD11b, and CD7. Metaphase cytogenetics demonstrated doubling of a clone with trisomy for chromosome 13.
After providing informed consent, he was treated on a HRPO-approved, phase 1 dose-escalation study of lenalidomide for relapsed AML at The Ohio State University (clinicaltrials.gov: NCT00466895). Study therapy consisted of lenalidomide 35 mg/day on days 1 through 21 of repeated 28-day cycles. At the completion of cycle 1, the CBC showed WBC 1200/μL with ANC 10/μL, and the patient remained red blood cell and platelet transfusion–dependent. BM biopsy showed 16% blasts. Cytogenetic analysis showed persistent disease in 8/20 metaphase cells. Four days after starting cycle 2, lenalidomide was held for fever, hypoxemia, and pneumonia, which resolved after intravenous antibiotics and supportive measures. Four weeks later (lenalidomide still on hold) the patient recovered his blood counts without G-CSF support. BM biopsy showed CR; cytogenetic analysis demonstrated a normal male karyotype in 20 of 20 metaphase cells, and FISH was negative. CRc was confirmed with a repeat BM biopsy 5 weeks later. After achieving CRc, the patient received 2 additional cycles of lenalidomide at 35 mg per day and the dose was then reduced to 10 mg per day (days 1-21 of 28-day cycles) due to drug-related myelosuppression. He subsequently relapsed after a 9-month CRc.
In the Ohio State University trial, 2 of 18 non–trisomy 13 AML patients have responded to lenalidomide. A 74-year-old man with isolated extramedullary relapse (skin only, no blood or marrow involvement) achieved CR on lenalidomide lasting 8 months. Originally, the patient had normal karyotype AML and achieved CR1 with cytarabine, daunorubicin, and etoposide; CR1 lasted 4 years. At first relapse (marrow and extramedullary relapse), he was reinduced with daunorubicin and cytarabine; CR2 lasted 9 months. At second relapse, he was treated with lenalidomide as noted above. Another patient, a 61-year-old male with AML and monosomy 7 who had relapsed after allogeneic transplantation, achieved CRc after 3 cycles of lenalidomide treatment and continues on therapy. He had been transplanted in CR2 with stem cells from an unrelated donor after a nonmyeloablative conditioning regimen and relapsed 9 months after transplantation.
Discussion
We report induction of sustained CRc in 2 older AML patients with trisomy 13 treated with single-agent lenalidomide. In AML, cytogenetic abnormalities remain the most important disease-related prognostic factor.12–15 Occurring in about 3% of AML cases, AML with trisomy 13 is rare and is associated with a very poor prognosis.13,16 Each of the 2 patients achieved morphologic and cytogenetic CR after a prolonged delay (78 and 124 days, respectively) from initiation of intermittent, high-dose lenalidomide. No other antileukemic agent was administered; the remissions were a direct result of lenalidomide therapy. To our knowledge, this is the first report of high-dose lenalidomide inducing morphologic and cytogenetic CRs in AML or any other myeloid disorder with trisomy 13 as the sole chromosomal abnormality.
The biologic mechanism of lenalidomide clinical activity in hematologic malignancies remains unclear. Clinical and cytogenetic responses to lenalidomide in MDS patients have been strongly associated with the 5q− chromosomal abnormality,7–9 providing a genetic starting point for studies to define lenalidomide's mechanism of action in this disease. Indeed, potential genes of interest in 5q− MDS have been identified, including SPARC17 and RPS14.18 Alternatively, extrinsic effects such as NK- or T-cell activation, antiangiogenesis, or cytokine modulation may contribute to its clinical activity. The clinical responses observed here, in the rare subset of AML with trisomy 13, again provide a narrow genetic framework to investigate potential targets of the drug in AML. Interestingly, retrospective analyses of AML patients have identified a strong association of trisomy 13 with mutations of the AML1 (RUNX1) gene and with increased expression of the FLT3 tyrosine kinase (located on chromosome 13),19,20 suggesting potential targets that may be relevant to the lenalidomide activity observed in this report. Further analysis of lenalidomide activity in additional trisomy 13 AML patients may ultimately lead to better understanding of myeloid leukemogenesis and aid in the development of new targeted therapeutic approaches for AML.
Acknowledgments
We thank Dr Sashikant Kulkarni for case 1 cytogenetic analysis and for providing the karyotype image.
The clinical trials of lenalidomide in AML were supported by Celgene (R.V., W.B.). This work was supported in part by an American Society of Clinical Oncology Young Investigator Award (T.A.F.), National Institutes of Health/National Cancer Institute K23CA120708 (W.B.), and the D. Warren Brown Foundation (J.C.B.).
Footnotes
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: T.A.F. designed the Washington University study, interpreted data, and wrote the paper; J.C.B. designed the study, interpreted data, and contributed to the paper; G.M. interpreted data and contributed to the paper; C.N.A. collected clinical data and contributed to the paper; C.K. provided research support to the Ohio State study; J.E.P. reviewed pathology, analyzed data, and contributed to the paper; R.V. designed the study, interpreted data, and contributed to the paper; and W.B. designed the Ohio State study, interpreted data, and wrote the paper.
Conflict-of-interest disclosure: T.A.F., R.V., and W.B. received research support from Celgene for the clinical studies. The remaining authors declare no competing financial interests.
Correspondence: William Blum, MD, B310 Starling Loving Hall, 320 West 10th Avenue, Columbus, OH 43210; e-mail: william.blum@osumc.edu.
References
- 1.Ravandi F, Burnett AK, Agura ED, Kantarjian HM. Progress in the treatment of acute myeloid leukemia. Cancer. 2007;110:1900–1910. doi: 10.1002/cncr.23000. [DOI] [PubMed] [Google Scholar]
- 2.Stone RM. Treatment of acute myeloid leukemia: state-of-the-art and future directions. Semin Hematol. 2002;39:4–10. doi: 10.1053/shem.2002.35977. [DOI] [PubMed] [Google Scholar]
- 3.Tallman MS, Gilliland DG, Rowe JM. Drug therapy for acute myeloid leukemia. Blood. 2005;106:1154–1163. doi: 10.1182/blood-2005-01-0178. [DOI] [PubMed] [Google Scholar]
- 4.Stone RM. The difficult problem of acute myeloid leukemia in the older adult. CA Cancer J Clin. 2002;52:363–371. doi: 10.3322/canjclin.52.6.363. [DOI] [PubMed] [Google Scholar]
- 5.Estey E. Acute myeloid leukemia and myelodysplastic syndromes in older patients. J Clin Oncol. 2007;25:1908–1915. doi: 10.1200/JCO.2006.10.2731. [DOI] [PubMed] [Google Scholar]
- 6.Estey EH. General approach to, and perspectives on clinical research in, older patients with newly diagnosed acute myeloid leukemia. Semin Hematol. 2006;43:89–95. doi: 10.1053/j.seminhematol.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 7.List A, Kurtin S, Roe DJ, et al. Efficacy of lenalidomide in myelodysplastic syndromes. N Engl J Med. 2005;352:549–557. doi: 10.1056/NEJMoa041668. [DOI] [PubMed] [Google Scholar]
- 8.List A, Dewald G, Bennett J, et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med. 2006;355:1456–1465. doi: 10.1056/NEJMoa061292. [DOI] [PubMed] [Google Scholar]
- 9.Raza A, Reeves JA, Feldman EJ, et al. Phase 2 study of lenalidomide in transfusion-dependent, low-risk, and intermediate-1 risk myelodysplastic syndromes with karyotypes other than deletion 5q. Blood. 2008;111:86–93. doi: 10.1182/blood-2007-01-068833. [DOI] [PubMed] [Google Scholar]
- 10.Richardson PG, Blood E, Mitsiades CS, et al. A randomized phase 2 study of lenalidomide therapy for patients with relapsed or relapsed and refractory multiple myeloma. Blood. 2006;108:3458–3464. doi: 10.1182/blood-2006-04-015909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richardson PG, Schlossman RL, Weller E, et al. Immunomodulatory drug CC-5013 overcomes drug resistance and is well tolerated in patients with relapsed multiple myeloma. Blood. 2002;100:3063–3067. doi: 10.1182/blood-2002-03-0996. [DOI] [PubMed] [Google Scholar]
- 12.Byrd JC, Mrozek K, Dodge RK, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100:4325–4336. doi: 10.1182/blood-2002-03-0772. [DOI] [PubMed] [Google Scholar]
- 13.Farag SS, Archer KJ, Mrozek K, et al. Pretreatment cytogenetics add to other prognostic factors predicting complete remission and long-term outcome in patients 60 years of age or older with acute myeloid leukemia: results from Cancer and Leukemia Group B 8461. Blood. 2006;108:63–73. doi: 10.1182/blood-2005-11-4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grimwade D, Walker H, Oliver F, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998;92:2322–2333. [PubMed] [Google Scholar]
- 15.Slovak ML, Kopecky KJ, Cassileth PA, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075–4083. [PubMed] [Google Scholar]
- 16.Dohner H, Arthur DC, Ball ED, et al. Trisomy 13: a new recurring chromosome abnormality in acute leukemia. Blood. 1990;76:1614–1621. [PubMed] [Google Scholar]
- 17.DiMartino JF, Lacayo NJ, Varadi M, et al. Low or absent SPARC expression in acute myeloid leukemia with MLL rearrangements is associated with sensitivity to growth inhibition by exogenous SPARC protein. Leukemia. 2006;20:426–432. doi: 10.1038/sj.leu.2404102. [DOI] [PubMed] [Google Scholar]
- 18.Ebert BL, Pretz J, Bosco J, et al. Identification of RPS14 as a 5q− syndrome gene by RNA interference screen. Nature. 2008;451:335–339. doi: 10.1038/nature06494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dicker F, Haferlach C, Kern W, Haferlach T, Schnittger S. Trisomy 13 is strongly associated with AML1/RUNX1 mutations and increased FLT3 expression in acute myeloid leukemia. Blood. 2007;110:1308–1316. doi: 10.1182/blood-2007-02-072595. [DOI] [PubMed] [Google Scholar]
- 20.Silva FP, Lind A, Brouwer-Mandema G, Valk PJ, Giphart-Gassler M. Trisomy 13 correlates with RUNX1 mutation and increased FLT3 expression in AML-M0 patients. Haematologica. 2007;92:1123–1126. doi: 10.3324/haematol.11296. [DOI] [PubMed] [Google Scholar]