Abstract
Objective
A systematic review and meta-analysis to investigate the efficacy of interventions incorporating motivational interviewing for smoking cessation and identify correlates of treatment effects.
Data Sources
MEDLINE/PubMed, PsycInfo, and other sources including grey literature.
Study Selection
Title/abstract search terms were motivational interview* OR motivational enhancement AND smok*, cigarette*, tobacco, OR nicotine. Randomized trials reporting number of smokers abstinent at follow up were eligible.
Data Extraction
Data were independently coded by the first and third authors. We coded for a variety of study, participant, and intervention related variables.
Data Synthesis
A random effects logistic regression with both a random intercept and a random slope for the treatment effect.
Results
Thirty-one smoking cessation research trials were selected for the study: 8 comprised adolescent samples, 8 comprised adults with chronic physical or mental illness, 5 comprised pregnant/postpartum women, and 10 comprised other adult samples. Analysis of the trials (9,485 individual participants) showed an overall odds ratio comparing likelihood of abstinence in the MI versus control condition of OR=1.45, 95% Confidence Interval or CI = 1.14-1.83). Additional potential correlates of treatment effects such as study, sample, and intervention characteristics were examined.
Conclusions
This is the most comprehensive review of MI for smoking cessation conducted to-date. These findings suggest that current MI smoking cessation approaches can be effective for adolescents and adults. However, comparative efficacy trials could be useful.
Keywords: Motivational Interviewing, Smoking Cessation, Systematic Review, Meta-Analysis
INTRODUCTION
Motivational Interviewing[1, 2] is a person-centered, guiding method of counseling to elicit and strengthen motivation for change. The approach guides the individual to explore and attempt to resolve normal ambivalence about changing while increasing ambivalence or perceived discrepancy (similar to cognitive dissonance; see Festinger)[3] between current behavior and overall values. Counselors employ the principles of expressing empathy, avoiding arguing, managing resistance without confrontation, and supporting the individual’s self-efficacy; using counseling techniques such as open-ended questioning, reflective listening, summarizing, affirming, and eliciting client self-motivational statements.[2] Self-motivational statements, or change-talk, are hypothesized to contribute greatly to changes in actual behavior.[4]
The MI approach was originally developed for use in substance abuse settings and stands in direct contrast to traditional addiction interventions that utilized heavy confrontation of denial and resistance and assumed that patients must “hit bottom” before being ready to change.[5] While MI is goal-oriented, it attempts to minimize and/or avoid the phenomenon of psychological reactance, part of what may be occurring when some individuals intentionally ignore health recommendations by using substances.[6] Several studies have found high patient satisfaction with this approach.[7] Additionally, several studies have demonstrated the greatest impact for those who are least ready to change initially.[5, 7]
Several reviews and meta-analyses have supported the efficacy of MI in decreasing substance use and other problem behaviors.[2, 7-13] These effects have been found to diminish little after the end of treatment.[8, 9] Evidence for efficacy has been found even when delivered in a brief format by non-specialists in diverse settings and when compared to either placebo or other active treatment. Clear evidence for the use of MI in the treatment of alcohol-related problems exists, and there is also solid support for the treatment of illicit drug problems. These studies have been performed in a variety of settings (e.g., college campuses and hospitals) using a variety of samples (e.g., men and women). Fewer studies, particularly randomized controlled trials, have been conducted on other health risk behaviors; however, there is evidence for efficacy here as well (e.g., medication adherence, HIV prevention, diet and exercise behaviors; physical health problems; see reviews).[7, 11] Of course, significant positive outcomes have not been universal across all studies. Effectiveness can vary across providers, populations, problems, and settings.[14] For example, one review found that psychologists and physicians obtained significant MI effects 80% of the time, whereas other healthcare providers obtained effects 46% of the time.[15] However, the field is relatively young, and definitive patterns of variability have not yet been established.[16]
Prior reviews and meta-analyses have included trials of MI for smoking cessation. However, several of the reviews included only two early smoking studies using very brief MI interventions (e.g., 15 minutes), finding mixed results.[9, 10, 17] More recent reviews and meta-analyses included 5-12 studies, also finding mixed or negative results.[7, 14, 15] Since there are many more randomized controlled trials evaluating MI and smoking available now, it is worthwhile to conduct a more extensive systematic review and meta-analysis of the MI and smoking literature.
Literature reviews have traditionally taken a narrative approach toward summarizing multiple comparable studies and observations. Meta-analysis offers the ability to critically evaluate and statistically combine the results of these studies and trials. The main advantage of meta-analysis is that it improves statistical power and produces more precise estimates of effect size.[18] Additionally, study results may be combined to examine specific effects in clinically important subgroups outside of the main research question.[18] The aims of the current systematic review and meta-analysis were to determine the efficacy of MI for smoking cessation and identify potential correlates of treatment effects.
METHODS
MEDLINE/PubMed, PsycInfo, and other sources including grey literature or unpublished works (for a summary of grey literature searching, see Rothstein and Hopewell)[19] were searched. Title/abstract search terms were motivational interview* OR motivational enhancement AND smok*, cigarette*, tobacco, OR nicotine. We considered studies for inclusion if they mentioned motivational interviewing or enhancement and referenced at least one of the primary motivational interviewing texts.[1, 2] Limits were English language and human participants. Prior MI reviews were searched, and relevant studies were requested from the Motivational Interviewing Network of Trainers list-serve. Randomized trials that reported the number of smokers who were abstinent at follow up were eligible. Authors were contacted for missing data. Studies that were published through August, 2008 were eligible for inclusion, and the majority was published since 2000. Most articles that were ineligible for inclusion were conceptual pieces or treatment recommendations rather than empirical articles.
Data were independently coded by the first (CH) and third (MH) authors. Disagreements were resolved by consensus. We coded for a variety of 1) study related variables: publication year, whether cluster randomization was used, type of abstinence validation, and duration of follow up; 2) participant related variables: nature of the population, age, percentage of White participants, percentage of female participants, number of cigarettes smoked per day at baseline; and 3) intervention related variables – the nature of the MI provided (whether it was rated as to intervention fidelity and whether it was combined with other treatment approaches), provider specialty and training in MI, treatment duration, and whether pharmacotherapy was used.
Four categories of studies were created by follow up time-point: between 4 and 8 weeks inclusive, between 10 and 12 weeks inclusive, between 22 and 26 weeks inclusive, and 52 weeks. One set of observations for each study was included within each category. For example, if a study reported outcomes at four and eight weeks, only the observation at eight weeks was included. Other time points were not used; when other time periods were included, the models would not converge. This is likely due to high collinearity between outcomes within studies that measured outcomes so closely in time.
Studies also varied as to the duration of abstinence used as the primary outcome. Note that for studies in which outcomes were reported for more than one abstinence duration (for example, both seven and 30 day continuous abstinence assessed at the same follow up time point for the same study), we chose the minimum number of self-reported days for inclusion in the analysis. The reason for choosing the minimum was to increase the uniformity of the definition of abstinence; more studies reported shorter abstinence outcomes (such as one or seven day continuous abstinence) than longer outcomes (such as 30 or 90 day continuous abstinence).
We used a random effects logistic regression to estimate the overall treatment effect, similar to the regression for meta-analysis described by Thompson and Sharp [20]. We included random slopes and intercepts and allowed them to be correlated. Our model differs from that of Thompson and Sharp [20] in that we assume that the intercept is random rather than fixed. As noted by Thompson and Sharp[20], the intercept provides for an analysis stratified by group as per DerSimonian and Laird [21]. We used a random intercept to improve the stability and identifiability of the models; for example, a fixed intercept model would not be identifiable since no one in the Haug et al. [22] study abstained at follow-up.
We used an ecological approach to evaluate the relationship of potential confounders with the MI effect.[23] An ecological approach is one in which group level sample characteristics (such as the percentage of women in each arm of a study) are examined rather than individual level characteristics. We did not have individual level data to assess such relationships directly. We entered the group level characteristics individually into the logistic regression random effects models to investigate whether the MI effect was enhanced or attenuated after controlling for the potential confounder. In all models, we controlled for evaluation time using three time dummy variables.
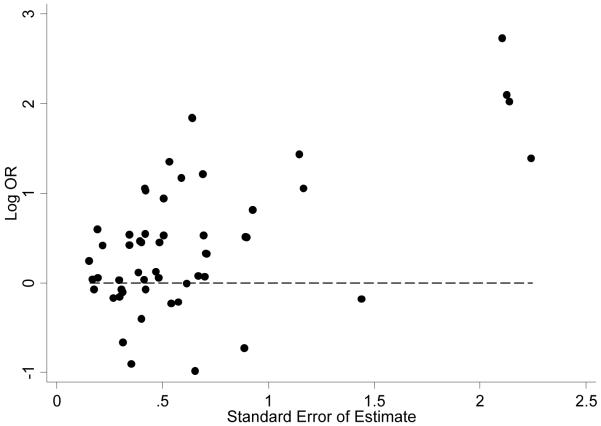
We used a funnel plot and regression analysis to assess publication bias. We used a multiple linear regression of the log odds ratio regressed on the standard error of the estimates and time as a categorical variable to empirically test for bias, similar to the methods of Sterne and colleagues.[24] For the linear regression used to assess bias, we accounted for study level clustering through the use of robust standard errors. All analyses were conducted in STATA version 10 (College Station, Texas).
RESULTS
Study Characteristics
Thirty-five published trials were identified since 1998: 8 comprised adolescent samples, 9 comprised adults with chronic physical or mental illness, 7 comprised pregnant/postpartum women, and 11 comprised other adult samples (see reference list for studies included). We analyzed data from 31 unique papers (9,485 individual participants; see Table 1 for overall study characteristics). We excluded two studies because they compared MI to active treatments with no control conditions.[25, 26] We excluded two other studies from the analysis because they had follow up time points that differed from the other studies.[27, 28] The 31 papers included data on 33 randomized control groups and 34 MI groups (two trials had two randomized substudies,[29, 30] and another trial compared one control condition to two forms of MI).[31]
Table 1. Overall Study Characteristics.
| Control groups reported* (n=33) |
Control Mean (SD) or % (n) |
MI groups reported* (n=34) |
MI Mean (SD) or % (n) |
|
|---|---|---|---|---|
| Total number of participants | 4,694 | 4,791 | ||
| % Females in study sample | 29 | 68% (2 7%) | 30 | 68% (27%) |
| % Whites in study sample | 18 | 61% (3 7%) | 19 | 57% (38%) |
| Baseline age | 29 | 34 (13) | 30 | 35 (13) |
| Baseline cigarettes per day | 28 | 15 (6) | 28 | 16 (6) |
| Baseline sample size | 33 | 142 (147) | 34 | 141 (139) |
| Study included pharmacotherapy |
33 | 45% (n=15) | 34 | 47% (n=16) |
| Biochemical verification of abstinence |
33 | 82% (n=27) |
34 | 82%(n=28) |
| MI combined with other interventions |
34 | 74% (n=25) |
||
| Fidelity check conducted | 34 | 50% (n=17) | ||
| Duration of staff training in MI (in hours) |
11 | 52 (72) |
||
| Duration of MI intervention (in minutes) |
32 | 101 (122) | ||
| Variable |
Papers
reporting |
Mean (SD)/
% (n) |
||
| Publication Year | 30** | 2004 (2.6) | ||
| Study conducted in the USA | 31 | 71% (n=22) | ||
| Cluster RCT | 31 | 16% (n=5) |
Smith and colleagues [30] reported on MI and control intervention effects for both low and high risk smokers. Both Hyman and colleagues [31] and Ahluwalia and colleagues[29] reported intervention effects for two different MI conditions, and Ahluwalia and colleagues [29] also had two control conditions.
31 papers included, but one study consisted of unpublished data (Hannover and colleagues).
MI = Motivational Interviewing intervention, n = number of arms/papers, SD = standard deviation, RCT = randomized controlled trial
In Table 1, we detail the characteristics of the study samples. Not all trials reported all characteristics. Only three studies did not cite abstinence or cessation as a primary outcome. Studies that cited other primary outcomes such as reduction in smoking were Kelly and Lapworth [32], McCambridge and Strang [33], and Tappin and colleagues [34]. In terms of mean baseline study level characteristics within the MI arms (see Table 1), mean participant age was 35 years, and mean cigarettes smoked per day was 16. Sixty-eight percent of the participants in the MI arms were female, and 57% were White. Control arm characteristics were very similar. The individual level characteristics differed from the mean of the study level characteristics; for example, because larger studies were more likely to be all female, 82% of the entire MI arm sample was female. In terms of study design and reporting, the mean publication date was 2004. Seventy-one percent of the studies were conducted in the USA (all others were conducted in Europe and Australia), and sixteen percent of the studies were cluster randomized (e.g., by provider or clinic). Thirty-nine percent of the studies used carbon monoxide for biochemical verification of abstinence, 29% used saliva cotinine, 23% used either urine or serum cotinine, and 19% used self-report alone; the percentages sum to greater than 100% because two studies used carbon monoxide with urine and one study used carbon monoxide with saliva.
In terms of intervention characteristics among those reporting data, the mean duration of the MI interventions was 101 minutes (reported for 32 MI arms), and the mean duration of staff training in MI was 52 hours (reported for 11 MI arms). Of the 33 MI arms in which data were reported, providers were 36% counselors/therapists, 18% staff/interventionists, 12% nurses/midwives, 9% mixed, 6% psychologists, 6% physicians, 6% health educators, and 6% trainees. Most (74%) MI arms combined MI with some additional intervention. These included 12% personalized risk feedback (e.g., carbon monoxide level), 6% educational pamphlets, 12% other types of interventions (e.g., CBT, relapse prevention, videos), and 44% included multiple other interventions (e.g., feedback and pamphlet). Fifty percent of the MI arms included some MI fidelity check (e.g., video-recording or observer rating); however, many of these checks were either minimal or not well-described. Approximately half of the arms also included pharmacotherapy; however, the use of pharmacotherapy was sometimes confounded with behavioral treatment condition or was provided on an optional basis. The typical control condition was brief advice plus some written materials. However, the control conditions varied widely as to how they were delivered (e.g., in person or over the telephone) as well as in terms of what was delivered, including no treatment, treatment as usual, education, referral, brief generic counseling, quit-lines, nicotine replacement therapy, and MI for diet and exercise.
Overall MI Effects
Table 2 reports abstinence rates by treatment condition and follow up time point for each study. Overall, the MI effect compared to control was statistically significant and of clinically relevant magnitude (odds ratio or OR=1.45, 95% Confidence Interval or CI = 1.14-1.83). In other words, participants in MI treatment conditions had 45% greater odds of being abstinent at follow-up evaluation than control participants. Results were similar both in an unadjusted analysis and after adjusting for time of follow-up measurement using time as an ordinal or categorical variable. These were intent-to-treat analyses. When we conducted completer only analyses, the overall MI effect did not substantially change (OR=1.48, CI=1.13-1.94).
Table 2. Treatment Effects by Study.
| Follow up Time point |
Authors | Year | Control % (n) Abstinent |
MI % (n) Abstinent |
Difference | Odds Ratio |
95% CI** |
|---|---|---|---|---|---|---|---|
|
4-8
weeks |
Stotts et al.[35] |
2002 | 21.5% (135) |
20.1% (134) |
−1.4% | 0.92 | (0.51, 1.66) |
| Borrelli et al.[36] |
2005 | 9.0% (144) |
9.3% (129) |
0.3% | 1.03 | (0.45, 2.35) | |
| Brown et al.[37] |
2003 | 10.7% (75) |
11.2% (116) |
0.5% | 1.06 | (0.42, 2.69) | |
| Okuyemi et al.[38] |
2007 | 5.6% (107) |
6.1% (66) | 0.5% | 1.09 | (0.29, 4.00) | |
| Kelly & Lapworth[32] |
2006 | 15.4% (26) |
20.0% (30) |
4.6% | 1.38 | (0.34, 5.53) | |
| Glasgow et al.[39] |
2000 | 6.9% (576) |
10.2% (578) |
3.3% | 1.52 | (1.00, 2.32) | |
| Helstrom et al.[40] |
2007 | 5.6% (36) | 8.9% (45) | 3.3% | 1.66 | (0.29, 9.61) | |
| Colby et al.[41] |
2005 | 0.0% (42) | 2.3% (43) | 2.3% | Infinite* | Undefined | |
|
10-12
weeks |
Ingersoll et al.[42] |
2007 | 55.6% (18) |
31.8% (22) |
−23.8% | 0.37 | (0.10, 1.36) |
| Stein et al.[43] | 2006 | 8.3% (192) |
5.8% (191) |
−2.5% | 0.67 | (0.30, 1.49) | |
| Haug et al.[22] | 2004 | 0.0% (33) | 0.0% (30) | 0.0% | 1* | Undefined | |
| Wakefield et al.[44] |
2004 | 6.3% (63) | 6.8% (74) | 0.5% | 1.07 | (0.27, 4.16) | |
| Kelly & Lapworth[32] |
2006 | 15.4% (26) |
20.0% (30) |
4.6% | 1.38 | (0.34, 5.53) | |
| Colby et al.[45] | 1998 | 10.0% (20) |
20.0% (20) |
10.0% | 2.25 | (0.36, 13.97) | |
| Baker et al.[46] | 2006 | 6.0% (151) |
15.0% (147) |
9.0% | 2.78 | (1.23, 6.25) | |
| Curry et al.[47] | 2003 | 2.7% (147) |
8.3% (156) |
5.6% | 3.25 | (1.03, 10.21) | |
| Hokanson et al.[48] |
2006 | 5.3% (57) | 15.8% (57) |
10.5% | 3.37 | (0.86, 13.19) | |
| McCambridge & Strang[33] |
2004 | 7.9% (63) | 25.0% (76) |
17.1% | 3.87 | (1.35, 11.06) | |
| Colby et al.[41] | 2005 | 0.0% (42) | 4.7% (43) | 4.7% | Infinite* | Undefined | |
|
22-26
weeks |
Ahluwalia et al.[29] (MI + Placebo NRT) |
2006 | 15.4% (188) |
6.9% (189) |
−8.5% | 0.40 | (0.20, 0.81) |
| Tappin et at.[34] |
2000 | 8.0% (50) | 4.0% (50) | −4.0% | 0.48 | (0.08, 2.74) | |
| Ahluwalia et al.[29] (MI + NRT) |
2006 | 18.0% (189) |
10.1% (189) |
−7.9% | 0.51 | (0.28, 0.93) | |
| Ruger et al.[49] | 2008 | 8.0% (100) |
6.4% (110) |
−1.6% | 0.78 | (0.27, 2.24) | |
| Okuyemi et al.[38] |
2007 | 9.3% (107) |
7.6% (66) | −1.7% | 0.80 | (0.26, 2.44) | |
| Horn et al.[50] | 2007 | 2.9% (34) | 2.4% (41) | −0.5% | 0.82 | (0.05, 13.70) | |
| Tappin et al.[51] |
2005 | 8.8% (411) |
7.4% (351) |
−1.4% | 0.83 | (0.49, 1.41) | |
| Smith et al.[30] (Low-risk for relapse) |
2001 | 24.8% (121) |
22.0% (127) |
−2.8% | 0.86 | (0.48, 1.55) | |
| Hokanson et al.[48] |
2006 | 10.5% (57) |
10.5% (57) |
0.0% | 1.00 | (0.30, 3.31) | |
| Hannover et al. | Unpub | 21.2% (433) |
21.9% (438) |
0.7% | 1.04 | (0.75, 1.44) | |
| Stein et al.[43] | 2006 | 4.7% (192) |
5.2% (191) |
0.5% | 1.12 | (0.45, 2.83) | |
| Borrelli et al.[36] |
2005 | 10.4% (144) |
11.6% (129) |
1.2% | 1.13 | (0.53, 2.42) | |
| Glasgow et al.[39] |
2000 | 14.9% (576) |
18.3% (578) |
3.4% | 1.28 | (0.94, 1.75) | |
| Hyman et al.[31] (Sequential tx for several health behaviors) |
2007 | 21.5% (93) |
27.1% (96) |
5.6% | 1.36 | (0.69, 2.65) | |
| Hyman et al.[31] (Simultaneous tx for several health behaviors) |
2007 | 21.5% (93) |
29.3% (92) |
7.8% | 1.52 | (0.78, 2.96) | |
| Smith et al.[30] (High-risk for relapse) |
2001 | 12.7% (102) |
18.8% (101) |
6.1% | 1.59 | (0.74, 3.41) | |
| Helstrom et al.[40] |
2007 | 5.6% (36) | 8.9% (45) | 3.3% | 1.66 | (0.29, 9.61) | |
| Kelly & Lapworth[32] |
2006 | 15.4% (26) |
23.3% (30) |
7.9% | 1.67 | (0.43, 6.52) | |
| Brown et al.[37] |
2003 | 8.0% (75) | 12.9% (116) |
4.9% | 1.71 | (0.63, 4.62) | |
| McClure et al.[52] |
2005 | 12.4% (137) |
19.6% (138) |
7.2% | 1.72 | (0.89, 3.32) | |
| Manfredi et al.[53] |
2004 | 8.6% (547) |
14.7% (517) |
6.1% | 1.83 | (1.25, 2.70) | |
| Baker et al.[46] | 2006 | 4.0% (151) |
9.5% (147) |
5.5% | 2.54 | (0.95, 6.81) | |
| Butler et al.[54] |
1999 | 3.0% (266) |
8.1% (270) |
5.1% | 2.86 | (1.25, 6.55) | |
| Colby et al.[41] |
2005 | 2.4% (42) | 9.3% (43) | 6.9% | 4.21 | (0.45, 39.29) | |
| Soria et al.[55] | 2006 | 3.5% (86) | 18.4% (114) |
14.9% | 6.25 | (1.80, 21.71) | |
| Gariti et al.[56] | 2002 | 0.0% (30) | 5.9% (34) | 5.9% | Infinite* | Undefined | |
| Herman & Fahnlander[57] |
2003 | 0.0% (22) | 15.0% (20) |
15.0% | Infinite* | Undefined | |
|
52
weeks |
McClure et al.[52] |
2005 | 19.7% (137) |
18.1% (138) |
−1.6% | 0.90 | (0.49, 1.65) |
| Hannover et al. |
Unpub | 19.6% (433) |
18.5% (438) |
−1.1% | 0.93 | (0.66, 1.30) | |
| Smith et al.[30] (High-risk for relapse) |
2001 | 13.7% (102) |
12.9% (101) |
−0.8% | 0.93 | (0.41, 2.09) | |
| Smith et al.[30] (Low-risk for relapse) |
2001 | 23.1% (121) |
23.6% (127) |
0.5% | 1.03 | (0.57, 1.85) | |
| Manfredi et al.[53] |
2004 | 10.8% (547) |
11.4% (517) |
0.6% | 1.07 | (0.73, 1.56) | |
| Brown et al.[37] |
2003 | 9.3% (75) |
13.8% (116) |
4.5% | 1.55 | (0.61, 3.98) | |
| Borrelli et al.[36] |
2005 | 8.3% (144) |
12.4% (129) |
4.1% | 1.56 | (0.71, 3.43) | |
| Baker et al.[46] | 2006 | 6.6% (151) |
10.9% (147) |
4.3% | 1.72 | (0.75, 3.93) | |
| Curry et al.[47] | 2003 | 0.7% (147) |
1.9% (156) |
1.2% | 2.86 | (0.29, 27.83) | |
| Soria et al.[55] | 2006 | 3.5% (86) |
18.4% (114) |
14.9% | 6.25 | (1.80, 21.71) |
ORs in which the control abstinence rate is 0 were included in figure 1 by adding 0.25 to the cell; in actuality, they are undefined due to division by zero. The random rather than fixed intercept in the regression models accounted for such low control abstinence rates. ORs calculated before rounding abstinence rates.
95% confidence intervals obtained using Woolf’s method. [58]
MI = motivational interviewing intervention, NRT = nicotine replacement therapy, tx = treatment
Overlapping confidence intervals suggested that the relative MI effect did not differ significantly depending on the timing of the follow-ups (see Table 3). Note that many studies reported multiple follow up assessments. The odds ratio of the MI effect was 1.47 (CI=0.97-2.23) at the 4-8 week evaluations, 1.66 (CI=1.08-2.56) at the 10-12 week evaluations, 1.44 (CI=1.11-1.88) at the 22-26 week evaluations and 1.25 (CI=0.91-1.71) at 52 week evaluations. When we evaluated only studies including more than one follow-up time-point, we found that the superiority of MI over control interventions did not decrease over time.
Table 3. MI Effects by Follow-Up Time Point and Population.
| Control % (n) Abstinent |
MI % (n) Abstinent |
Difference | Adjusted Odds Ratio |
Odds Ratio 95% CI |
Adjusted P-value |
|
|---|---|---|---|---|---|---|
| Time Point * | ||||||
| 4-8 Weeks | 8.9% (1141) |
11.0% (1141) |
2.1% | 1.47 | (0.97, 2.23) |
0.067 |
| 10-12 Weeks | 7.0% (812) |
11.6% (846) |
4.6% | 1.66 | (1.08, 2.56) |
0.022 |
| 22-26 Weeks | 11.6% (4215) |
14.0% (4279) |
2.4% | 1.44 | (1.11, 1.88) |
0.006 |
| 52 Weeks | 12.7% (1943) |
14.1% (1983) |
1.4% | 1.25 | (0.91, 1.71) |
0.177 |
| Population ** | ||||||
| Adolescents | 6.0% (235) |
11.5% (295) |
5.5% | 2.29 | (1.34, 3.89) |
0.002 |
| Adults with Chronic Illnesses |
8.4% (667) |
13.4% (746) |
5.0% | 1.34 | (0.89, 2.01) |
0.157 |
| Adults | 11.9% (2319) |
14.7% (2289) |
2.8% | 1.44 | (1.04, 2.01) |
0.029 |
| Pregnant/Postpartum Women |
14.1% (994) |
13.8% (949) |
−0.3% | 1.00 | (0.61, 1.62) |
0.990 |
The adjusted odds ratio and adjusted p-value describe the effect for each time period from a multiple logistic regression model with a random intercept and a random slope for the treatment effect.
The adjusted odds ratio and adjusted p-value describe the overall effect for each subgroup using data from all time points entered into a multiple logistic regression with a random intercept for study and a random slope for the treatment effect. Dummy variables for time were included in the model. For ease of presentation, we only present % abstinent data from the 22-24 week follow up time point.
MI = Motivational Interviewing intervention, n = sample size, CI = confidence interval
Effects of Sample Characteristics
Using an ecological approach, we did not find significant differences in intervention effects based on whether participants were treatment-seeking or not, the percentage of non-White participants, percentage of females, average number of cigarettes smoked per day, or average age.
With regard to other types of populations, the odds ratio for the MI effect was 2.29 (CI=1.34-3.89) for adolescents, 1.44 (CI=1.04-2.01) for adults, 1.34 (CI=0.89-2.01) for adults with chronic illnesses, and 1.00 (CI=0.61-1.62) for pregnant and post-partum women (see Table 3). However, the pooled-data (MI and control conditions) time one (4-8 week) quit rate was higher among pregnant and post-partum women compared to others (21% quit rate among pregnant and post-partum women compared with 8% among adults, 9% among adults with chronic illnesses, and 9% among adolescents).
Effects of Study and Intervention Characteristics
We also examined whether there was evidence of potential mediation of the MI effect by study or MI intervention characteristics by controlling for potential mediators in models. We did not find that the magnitude of the MI effect differed substantially after controlling for the following study characteristics: publication year, whether the study was a cluster RCT, whether the study included the use of pharmacotherapy. Nor did moderation models find evidence that the method of abstinence verification (carbon monoxide, cotinine, or self-report) significantly altered the MI effect. However, studies that used carbon monoxide verification tended to demonstrate larger MI effects (OR=1.92, 95% CI 1.11-3.34 when examining the effect in the 12 papers that used CO verification). We also examined the effects of MI on quit attempts in the eight studies that reported these data and found the MI effects to be smaller for quit attempts than for actual abstinence (OR=1.27, 95% CI 1.08-1.49, using a fixed effects slope and random intercept model due to inestimability of the random slope in this reduced sample size).
We did not find evidence of mediation based on the following MI intervention characteristics: hours of staff training in MI, total MI duration, and whether MI was combined with another treatment (e.g., CBT). Additionally, there was no apparent overall impact of provider type (e.g., physician, nurse, counselor) after controlling for whether the study included pharmacotherapy. There was no evidence that the studies that assessed MI fidelity had different intervention abstinence effects from those that did not. As noted in Table 1, 74% of the trials were rated as including additional interventions beyond “pure” MI. We examined a regression in which we controlled for additional interventions. This did not change the impact of MI by itself (OR=1.42, 95% CI 1.13-1.79). In examining the eight trials that did not include any additional form of intervention, the OR for the MI effect was 1.84 (95% CI 0.92-3.67). Although not statistically significant, the magnitude of the effect was consistent with what we observed using the full data. We did not find the intervention effects to be altered significantly based on whether the control condition consisted of brief advice only or was delivered in person.
Evaluation of Potential Publication Bias
We also used a funnel plot to assess publication bias. The funnel plot in Figure 1 shows slight evidence of bias in reporting of results. An unbiased plot should look like a horizontal funnel with the smallest variability in ORs around smaller standard errors. The funnel should be centered around the true log OR (not necessarily 0 which is the null effect). Heuristically, less precise studies or those with smaller sample sizes and larger standard errors are more likely to be affected by chance and more widely scattered around the true log OR. The concern is that negative findings might not be reported, and hence the shape of the funnel below log OR=0 would be distorted. When small studies with zero abstinent in control arm are added to the figure by adding 0.25 a person to the zero cell (to avoid division by zero), there is a positive relationship between the standard error and the log odds ratio. This was confirmed by the multiple linear regression in which we regressed the log odds ratio on the standard error and time (slope=0.94, CI 0.59-1.28 for the standard error coefficient in the model).
Figure 1. Funnel Plot to Detect Possible Publication Bias.
DISCUSSION
Summary of the Current Meta-Analysis and Comparison to Prior Meta-Analyses
This is the most comprehensive review of MI for smoking cessation conducted to-date including 31 unique empirical studies (9,485 individual participants). There was a great deal of methodological variability and lack of trial reporting detail in the studies included. There was also a great deal of variability in intervention effect, but the overall MI intervention effect was significant at an OR of 1.45, and MI effects peaked at 10-12 weeks follow up. There appears to be slight publication bias in reporting the MI effects on smoking cessation, indicating that trials demonstrating statistically significant differences in intervention effects are slightly more likely to be reported than trials with null results.
Several other meta-analyses of various smoking cessation treatments including motivational interviewing have been conducted. These meta-analyses have not reported significant differences in outcome for MI versus other approaches (e.g., cognitive behavioral therapy) across studies. Our finding of the overall MI effect (OR = 1.45) across diverse studies is within the range found in other meta-analyses, albeit at the lower end of the range.[59-61] Prior meta-analyses of approaches including MI have found significant treatment effects for adolescents and young adults as well as pregnant smokers.[62-66] Similar to our analyses, Mojica and colleagues performed a meta-analysis of smoking cessation interventions by type of provider and did not find a moderational effect.[67]
Limitations
The quantitative results of meta-analyses should be interpreted with caution due to the influence of inclusion and exclusion criteria and potential publication bias.[69, 70] In the current study, the inclusion/exclusion criteria were fairly straightforward, and only slight publication bias was noted. However, the effects of MI may be overestimated due to this slight bias. Additionally, while the overall findings regarding MI effects compared to control is based on randomized study designs, findings of other analyses are not. For example, we found studies that used carbon monoxide verification to produce stronger effects than studies that did not. However, participants were not randomized to CO versus other biochemical verification and the 95% confidence intervals overlapped, so conclusions regarding this finding are limited. The use of study-level rather than individual-level data in meta-analyses does not permit certain in-depth analyses. For example, we were not able to conduct multi-level analyses to fully investigate the impact of cluster randomization. However, when we performed an analysis only among those trials that did not use cluster randomization (26 trials), the inferences remained the same (OR=1.47, 95% CI 1.10-1.96). Pooling studies can also draw attention away from differences in study results that may provide insights into clinically important differences in effects.[18] Additionally, meta-analyses usually report pooled effects as odds ratios while effectiveness in a clinical setting may differ according to level of baseline risk.[18] On the other hand, we did examine some risk variables such as baseline cigarettes per day, chronic illness status, etc. and reported outcomes for individual studies in Table 2. In addition, the nature of the MI interventions varied across studies, and intervention fidelity was rarely adequately assessed. Even for studies in which satisfactory intervention fidelity is demonstrated, intervention delivery in this same manner in non-research settings is certainly not guaranteed.
Clinical Implications and Directions for Future Research
These results suggest that MI can be efficacious for smoking cessation particularly among adolescents. In the current study, we did not find MI to be better than control for pregnant/postpartum women, who may already possess high levels of motivation to quit for the sake of their baby, as evidenced by quit rates twice those of the other populations at 4-6 weeks. Thus, these women may need interventions more directly supporting other aspects of quitting such as skill-development and self-efficacy in addition to motivational enhancement. While the effects of MI were moderate, the interventions tended to be relatively short (about 1.5 hours) and therefore, may be more cost-effective than some other approaches once staff training is completed. Likewise, the mean number of cigarettes smoked at baseline was less than a pack per day, at 15 cigarettes, so the use of MI with more dependent smokers (perhaps used in part to motivate adherence to pharmacotherapies) may demonstrate different results. While the overall abstinence rates were lower in both the MI and control conditions in studies with longer follow ups, as is common with other behavioral interventions,[61, 63] the relative superiority of MI versus control did not appear to decrease over time in studies that reported multiple follow-up time-points.
Future research could benefit from the use of standardized MI protocols and fidelity assessments. As has been suggested in prior reviews,[9] research reports should provide greater methodological detail in terms of study, intervention, and population characteristics. For example, detailed reporting on quit motivation and quit attempts using standardized measures would allow for more in-depth understanding of the quitting process and intervention effects. Additionally, most of the studies reviewed were conducted in the USA, which limits generalizability somewhat. One of the biggest remaining questions about the efficacy of MI for smoking cessation is how it compares to other cessation approaches. In most cases, MI interventions have been combined with other interventions, so dismantling studies could also be useful. More information about what may enhance the effects of MI in some studies is needed. While the effects of MI varied across studies, we had difficulty identifying intervention or study factors associated with effect size variability. In comparisons across studies, MI’s effects appear comparable to other approaches; however, MI needs to be tested head-to-head with other approaches in RCTs to draw firm conclusions in this regard.
Acknowledgments
The authors would like to thank Sharon Manne, Sara Filseth, Indira Friel, Chelsea Rose, and Jeanne Pomenti for their assistance with literature searching, data management, and manuscript preparation.
Funding: This work was supported by the National Institutes of Health [K07 CA108685 to CH, P30 CA006927 to Fox Chase Cancer Center].
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Tobacco Control and any other BMJPGL products to exploit all subsidiary rights, as set out in our license (http://tobaccocontrol.bmj.com/ifora/licence.pdf).
Footnotes
Competing Interests: The first author (CH) is affiliated with the Motivational Interviewing Network of Trainers and is an author of one of the studies reviewed.[42]
What this paper adds
Prior reviews and meta-analyses have included trials of MI for smoking cessation. However, several of the reviews and meta-analyses included only a few early smoking studies using very brief MI interventions, finding mixed or negative results. Since there are many more randomized controlled trials evaluating MI and smoking available now, it is worthwhile to conduct a more extensive systematic review and meta-analysis of the MI and smoking literature.
Analysis of 31 randomized controlled trials (9,485 individual participants) showed an overall odds ratio comparing likelihood of abstinence in the MI versus control condition of 1.45 (95% Confidence Interval or CI = 1.14-1.83). These findings suggest that current MI smoking cessation approaches can be effective for adolescents and adults. However, comparative efficacy trials could be useful.
References
- [1].Miller WR, Rollnick S. Motivational interviewing:Preparing people to change addictive behavior. Guilford Press; New York, NY: 1991. [Google Scholar]
- [2].Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. Guilford Press; New York, NY: 2002. [Google Scholar]
- [3].Festinger L. A theory of cognitive dissonance. Row, Peterson; Evanston, IL: 1957. [Google Scholar]
- [4].Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Miller WR. Motivational interviewing: research, practice, and puzzles. Addict Behav. 1996;21(6):835–842. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- [6].Brehm S, Brehm J. Psychological reactance. Academic Press; New York: 1981. [Google Scholar]
- [7].Resnicow K, DiIorio C, Soet JE, et al. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol. 2002;21(5):444–451. [PubMed] [Google Scholar]
- [8].Burke BL, Arkowitz H, Dunn C. The efficacy of Motivational Interviewing and its adaptations: What we know so far. In: Miller WR, Rollnick R, editors. Motivational interviewing:preparing people for change. Guilford Press; New York: 2002. [Google Scholar]
- [9].Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- [10].Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- [11].Knight KM, McGowan L, Dickens C, et al. A systematic review of motivational interviewing in physical health care settings. British Journal of Health Psychology. 2006;11(Pt 2):319–332. doi: 10.1348/135910705X52516. [DOI] [PubMed] [Google Scholar]
- [12].Noonan WC, Moyers TB. Motivational interviewing: a review. Journal of Substance Misuse. 1997;2:8–16. [Google Scholar]
- [13].Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- [14].Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- [15].Rubak S, Sandbaek A, Lauritzen T, et al. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- [16].Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings: a review. Arch Pediatr Adolesc Med. 2005;159(12):1173–1180. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- [18].Fletcher RW, Fletcher SW. Clinical Epidemiology: The Essentials. 4th ed Lippincott, Williams, and Wilkins; 2005. [Google Scholar]
- [19].Rothstein HR, Hopewell S. The grey literature. In: Cooper H, Hedges L, Valentine J, editors. The handbook of research synthesis. Russell-Sage; New York: 2007. [Google Scholar]
- [20].Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: A comparison of methods. Stat Med. 1999;18:2693–2708. doi: 10.1002/(sici)1097-0258(19991030)18:20<2693::aid-sim235>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- [21].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- [22].Haug NA, Svikis DS, Diclemente C. Motivational enhancement therapy for nicotine dependence in methadone-maintained pregnant women. Psychol Addict Behav. 2004;18(3):289–292. doi: 10.1037/0893-164X.18.3.289. [DOI] [PubMed] [Google Scholar]
- [23].McMahan B, Trichopoulos D. Epidemiology: principles and methods. 2nd ed. Little, Brown, and Company; New York: 1996. [Google Scholar]
- [24].Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–1129. doi: 10.1016/s0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- [25].George TP, Ziedonis DM, Feingold A, et al. Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. Am J Psychiatry. 2000;157(11):1835–1842. doi: 10.1176/appi.ajp.157.11.1835. [DOI] [PubMed] [Google Scholar]
- [26].Okuyemi KS, Thomas JL, Hall S, et al. Smoking cessation in homeless populations: a pilot clinical trial. Nicotine and Tobacco Research. 2006;8(5):689–699. doi: 10.1080/14622200600789841. [DOI] [PubMed] [Google Scholar]
- [27].Rigotti NA, Park ER, Regan S, et al. Efficacy of telephone counseling for pregnant smokers: a randomized controlled trial. Obstet Gynecol. 2006;108(1):83–92. doi: 10.1097/01.AOG.0000218100.05601.f8. [DOI] [PubMed] [Google Scholar]
- [28].Ershoff DH, Quinn VP, Boyd NR, et al. The Kaiser Permanente prenatal smoking-cessation trial: when more isn’t better, what is enough? Am J Prev Med. 1999;17(3):161–168. doi: 10.1016/s0749-3797(99)00071-9. [DOI] [PubMed] [Google Scholar]
- [29].Ahluwalia JS, Okuyemi K, Nollen N, et al. The effects of nicotine gum and counseling among African American light smokers: a 2 × 2 factorial design. Addiction. 2006;101(6):883–891. doi: 10.1111/j.1360-0443.2006.01461.x. [DOI] [PubMed] [Google Scholar]
- [30].Smith SS, Jorenby DE, Fiore MC, et al. Strike while the iron is hot: can stepped-care treatments resurrect relapsing smokers? J Consult Clin Psychol. 2001;69(3):429–439. doi: 10.1037//0022-006x.69.3.429. [DOI] [PubMed] [Google Scholar]
- [31].Hyman DJ, Pavlik VN, Taylor WC, et al. Simultaneous vs sequential counseling for multiple behavior change. Arch Intern Med. 2007;167(11):1152–1158. doi: 10.1001/archinte.167.11.1152. [DOI] [PubMed] [Google Scholar]
- [32].Kelly AB, Lapworth K. The HYP program-targeted motivational interviewing for adolescent violations of school tobacco policy. Prev Med. 2006;43(6):466–471. doi: 10.1016/j.ypmed.2006.06.018. [DOI] [PubMed] [Google Scholar]
- [33].McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- [34].Tappin DM, Lumsden MA, McIntyre D, et al. A pilot study to establish a randomized trial methodology to test the efficacy of a behavioural intervention. Health Educ Res. 2000;15(4):491–502. doi: 10.1093/her/15.4.491. [DOI] [PubMed] [Google Scholar]
- [35].Stotts AL, Diclemente CC, Dolan-Mullen P. One-to-one: a motivational intervention for resistant pregnant smokers. Addict Behav. 2002;27(2):275–292. doi: 10.1016/s0306-4603(01)00174-5. [DOI] [PubMed] [Google Scholar]
- [36].Borrelli B, Novak S, Hecht J, et al. Home health care nurses as a new channel for smoking cessation treatment: outcomes from project CARES (Community-nurse Assisted Research and Education on Smoking) Prev Med. 2005;41(5-6):815–821. doi: 10.1016/j.ypmed.2005.08.004. [DOI] [PubMed] [Google Scholar]
- [37].Brown RA, Ramsey SE, Strong DR, et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tob Control. 2003;12(Suppl 4):IV3–10. doi: 10.1136/tc.12.suppl_4.iv3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Okuyemi KS, James AS, Mayo MS, et al. Pathways to health: a cluster randomized trial of nicotine gum and motivational interviewing for smoking cessation in low-income housing. Health Educ Behav. 2007;34(1):43–54. doi: 10.1177/1090198106288046. [DOI] [PubMed] [Google Scholar]
- [39].Glasgow RE, Whitlock EP, Eakin EG, et al. A brief smoking cessation intervention for women in low-income planned parenthood clinics. Am J Public Health. 2000;90(5):786–789. doi: 10.2105/ajph.90.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Helstrom A, Hutchison K, Bryan A. Motivational enhancement therapy for high-risk adolescent smokers. Addict Behav. 2007;32(10):2404–2410. doi: 10.1016/j.addbeh.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Colby SM, Monti PM, O’Leary Tevyaw T, et al. Brief motivational intervention for adolescent smokers in medical settings. Addict Behav. 2005;30(5):865–874. doi: 10.1016/j.addbeh.2004.10.001. [DOI] [PubMed] [Google Scholar]
- [42].Ingersoll KS, Cropsey KL, Heckman CJ. A test of motivational plus nicotine replacement interventions for HIV positive smokers. AIDS and Behavior. 2007 doi: 10.1007/s10461-007-9334-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Stein MD, Weinstock MC, Herman DS, et al. A smoking cessation intervention for the methadone-maintained. Addiction. 2006;101(4):599–607. doi: 10.1111/j.1360-0443.2006.01406.x. [DOI] [PubMed] [Google Scholar]
- [44].Wakefield M, Olver I, Whitford H, et al. Motivational interviewing as a smoking cessation intervention for patients with cancer: randomized controlled trial. Nurs Res. 2004;53(6):396–405. doi: 10.1097/00006199-200411000-00008. [DOI] [PubMed] [Google Scholar]
- [45].Colby SM, Monti PM, Barnett NP, et al. Brief motivational interviewing in a hospital setting for adolescent smoking: a preliminary study. J Consult Clin Psychol. 1998;66(3):574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- [46].Baker A, Richmond R, Haile M, et al. A randomized controlled trial of a smoking cessation intervention among people with a psychotic disorder. Am J Psychiatry. 2006;163(11):1934–1942. doi: 10.1176/ajp.2006.163.11.1934. [DOI] [PubMed] [Google Scholar]
- [47].Curry SJ, Ludman EJ, Graham E, et al. Pediatric-based smoking cessation intervention for low-income women: a randomized trial. Arch Pediatr Adolesc Med. 2003;157(3):295–302. doi: 10.1001/archpedi.157.3.295. [DOI] [PubMed] [Google Scholar]
- [48].Hokanson JM, Anderson RL, Hennrikus DJ, et al. Integrated tobacco cessation counseling in a diabetes self-management training program: a randomized trial of diabetes and reduction of tobacco. Diabetes Educ. 2006;32(4):562–570. doi: 10.1177/0145721706289914. [DOI] [PubMed] [Google Scholar]
- [49].Ruger JP, Weinstein MC, Hammond SK, et al. Cost-effectiveness of motivational interviewing for smoking cessation and relapse prevention among low-income pregnant women: a randomized controlled trial. Value Health. 2008;11(2):191–198. doi: 10.1111/j.1524-4733.2007.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Horn K, Dino G, Hamilton C, et al. Efficacy of an emergency department-based motivational teenage smoking intervention. Prev Chronic Dis. 2007;4(1):A08. [PMC free article] [PubMed] [Google Scholar]
- [51].Tappin DM, Lumsden MA, Gilmour WH, et al. Randomised controlled trial of home based motivational interviewing by midwives to help pregnant smokers quit or cut down. BMJ. 2005;331(7513):373–377. doi: 10.1136/bmj.331.7513.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].McClure JB, Westbrook E, Curry SJ, et al. Proactive, motivationally enhanced smoking cessation counseling among women with elevated cervical cancer risk. Nic & Tob Res. 2005;7(6):881–889. doi: 10.1080/14622200500266080. [DOI] [PubMed] [Google Scholar]
- [53].Manfredi C, Crittenden KS, Cho YI, et al. Long-term effects (up to 18 months) of a smoking cessation program among women smokers in public health clinics. Prev Med. 2004;38(1):10–19. doi: 10.1016/j.ypmed.2003.09.022. [DOI] [PubMed] [Google Scholar]
- [54].Butler CC, Rollnick S, Bachman M, et al. Motivational consulting versus brief advice for smokers in general practice: a randomized trial. BrJ Gen Pract. 1999;49:611–616. [Google Scholar]
- [55].Soria R, Legido A, Escolano C, et al. A randomised controlled trial of motivational interviewing for smoking cessation. Br J Gen Pract. 2006;56(531):768–774. [PMC free article] [PubMed] [Google Scholar]
- [56].Gariti P, Alterman A, Mulvaney F, et al. Nicotine intervention during detoxification and treatment for other substance use. Am J Drug Alcohol Abuse. 2002;28(4):671–679. doi: 10.1081/ada-120015875. [DOI] [PubMed] [Google Scholar]
- [57].Herman KC, Fahnlander B. A motivational intervention to reduce cigarette smoking among college students: overview and exploratory investigation. J College Counseling. 2003;6(1):10. [Google Scholar]
- [58].Woolf B. On estimating the relationship between blood group and disease. Ann Hum Genet. 1955;19:251–253. doi: 10.1111/j.1469-1809.1955.tb01348.x. [DOI] [PubMed] [Google Scholar]
- [59].Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation (Review) Cochrane Database of Systematic Reviews 2005. 2005;(2):1–23. doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]
- [60].Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database Syst Rev. 2008;(1) doi: 10.1002/14651858.CD001188.pub3. CD001188. [DOI] [PubMed] [Google Scholar]
- [61].Smedslund G, Fisher KJ, Boles SM, et al. The effectiveness of workplace smoking cessation programmes: a meta-analysis of recent studies. Tob Control. 2004;13(2):197–204. doi: 10.1136/tc.2002.002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Baer JS, Peterson PL, Wells EA. Rationale and design of a brief substance use intervention for homeless adolescents. Addiction Research and Theory. 2004;12(4):317–334. [Google Scholar]
- [63].Grimshaw GM, Stanton A. Tobacco cessation interventions for young people. Cochrane Database Syst Rev. 2006;(4) doi: 10.1002/14651858.CD003289.pub4. CD003289. [DOI] [PubMed] [Google Scholar]
- [64].Lumley J, Chamberlain C, Dowswell T, et al. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev. 2009;(3) doi: 10.1002/14651858.CD001055.pub3. CD001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. J Consult Clin Psychol. 2004;72(6):1144–1156. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- [66].Sussman S, Sun P, Dent CW. A meta-analysis of teen cigarette smoking cessation. Health Psychol. 2006;25(5):549–557. doi: 10.1037/0278-6133.25.5.549. [DOI] [PubMed] [Google Scholar]
- [67].Mojica WA, Suttorp MJ, Sherman SE, et al. Smoking-cessation interventions by type of provider: a meta-analysis. Am J Prev Med. 2004;26(5):391–401. doi: 10.1016/j.amepre.2004.02.014. [DOI] [PubMed] [Google Scholar]
- [68].Prochaska JO, DiClimente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy: Theory Research, and Practice. 1982;19:276–288. [Google Scholar]
- [69].Pai M, McCulloch M, Gorman JD, et al. Systematic reviews and meta-analyses: an illustrated, step-by-step guide. Natl Med J India. 2004;17(2):86–95. [PubMed] [Google Scholar]
- [70].Fagard RH, Staessen JA, Thijs L. Advantages and disadvantages of the meta-analysis approach. J Hypertens Suppl. 1996;14(2):S9–12. doi: 10.1097/00004872-199609002-00004. discussion S13. [DOI] [PubMed] [Google Scholar]