Abstract
Objective
To describe contemporary cesarean delivery practice in the U.S.
Study Design
Consortium on Safe Labor collected detailed labor and delivery information from 228,668 electronic medical records from 19 hospitals across the U.S., 2002 – 2008.
Results
The overall cesarean delivery rate was 30.5%. 31.2% of nulliparas were delivered by cesarean section. Prelabor repeat cesarean delivery due to a previous uterine scar contributed 30.9% of all cesarean sections. 28.8% of women with a uterine scar had a trial of labor and the success rate was 57.1%. 43.8% women attempting vaginal delivery had induction. Half of cesarean for dystocia in induced labor were performed before 6 cm of cervical dilation.
Conclusion
To decrease cesarean delivery rate in the U.S., reducing primary cesarean delivery is the key. Increasing VBAC rate is urgently needed. Cesarean section for dystocia should be avoided before the active phase is established, particularly in nulliparas and in induced labor.
Keywords: cesarean delivery, induction, labor, VBAC
INTRODUCTION
Cesarean delivery has become the most common major surgical procedure in many parts of the world.1,2 The national rate of cesarean delivery in the U.S. has increased more than 50% since 1996 to 31.8% in 2007.3 This upward trajectory appears likely to continue in the near future.
Reasons for the increase are multi-faceted. Delayed childbearing, increasing maternal body mass, more multi-fetal gestations and low utilization of vaginal birth after previous cesarean (VBAC) are commonly cited causes.4,5 Cesarean delivery on maternal request6 and physicians’ fear of litigation due to a poor obstetrical outcome7 may also be contributing to the escalating rate of cesarean delivery. Despite anecdotal evidence and the common belief that certain cesarean deliveries may be unnecessary, the magnitude of unnecessary cesarean section at the national level is unknown. Reliable, detailed information on labor and delivery is often unavailable in a large population. Consequently, our understanding of the underlying causes of high cesarean rate is incomplete.
To meet this challenge, the Eunice Shriver Kennedy National Institute of Child Health and Human Development, National Institutes of Health, in collaboration with 12 institutions across the country, conducted a retrospective observational study entitled “the Consortium on Safe Labor”. The goal of the study was to collect comprehensive information on contemporary labor and delivery practice in multiple institutions. This paper describes the contemporary cesarean delivery practice in the U.S. population.
MATERIALS AND METHODS
The Consortium on Safe Labor included 12 clinical centers (with 19 hospitals) across 9 American College of Obstetricians and Gynecologists (ACOG) U.S. districts. There were 8 university affiliated teaching hospitals, 9 teaching community hospitals and 2 non-teaching community hospitals. They were chosen because of the availability of electronic medical records at each institution and because their geographic distribution covers all ACOG US districts. A total of 228,668 deliveries with 233,844 newborns between 2002 and 2008 were included in the study. 87% of births occurred between 2005 and 2007. All births at 23 weeks or later in these institutions were included. 9.5% of women contributed more than one delivery to the database. To avoid intra-person correlation, we selected the first delivery from each subject in the study, leaving 206,969 deliveries for analysis. Participating institutions extracted detailed information from their electronic medical records on maternal demographic characteristics, medical history, reproductive and prenatal history, labor and delivery summary, postpartum and newborn information. Information from the neonatal intensive care unit (NICU) was linked to the newborn records. Data on labor progression were extracted from the electronic labor database. Information on hospital and physician characteristics was collected from surveys of the local investigators, and maternal and newborn discharge summaries (in ICD-9 codes) were linked to each delivery. This project was approved by the Institutional Review Boards of all participating institutions.
Data transferred from the clinical centers were mapped to pre-defined common codes for each variable at the data coordinating center. Data inquiries, cleaning, recoding and logic checking were performed. We also conducted validation studies for four key outcome diagnoses including cesarean for non-reassuring fetal heart rate tracing, asphyxia, NICU admission for respiratory conditions, and shoulder dystocia. To validate data, eligible charts were selected, and investigators were asked to recollect data with chart abstraction done by hand. We compared the information hand collected from the medical charts with that downloaded from the electronic medical records. Appendix I indicates that most variables that were reviewed in this study are highly accurate. Although our records were not sampled randomly, the consistency among different records on the same variable (e.g., singleton, gestational age, attempting vaginal birth, live birth, vertex presentation) indicates that the information provided in the validation studies is reliable and likely to be generalizable to the entire database. Thus, the electronic medical records are reasonably accurate representation of the medical charts.
APPENDIX I.
Validity of data from electronic medical records comparing to medical charts in selected variables
| Sample selection criteria | Information from the electronic medical records | Concordant with medical chart (%) | Disagreed with medical chart (%) | Not found in medical chart (%) |
|---|---|---|---|---|
| Nulliparous, singleton, live, vertex fetus at admission, Attempting vaginal delivery and cesarean delivery due to non- reassuring fetal heart rate tracing (N = 5,662) | Nulliparity | 99.1 | 0.9 | 0.0 |
| Live fetus at admission | 99.9 | 0.1 | 0.0 | |
| Attempting vaginal delivery | 96.2 | 3.6 | 0.2 | |
| Singleton | 98.5 | 0.1 | 1.4 | |
| Vertex at admission | 96.7 | 1.1 | 2.2 | |
| Cesarean delivery | 99.9 | 0.1 | 0.0 | |
| Primary indication for cesarean delivery: non-reassuring fetal heart rate tracing/fetal distress | 93.3 | 3.5 | 3.2 | |
| Singleton, gestational age ≥ 34 weeks, attempting vaginal delivery, had an Apgar score at 5 minutes < 4 or umbilical cord pH <7.0 or base deficit ≥ 12 mmol/L (N = 503) | Singleton | 99.8 | 0 | 0.2 |
| Gestational age ≥ 34 weeks | 97.6 | 2.4 | 0 | |
| Attempting vaginal delivery | 95.8 | 3.8 | 0.4 | |
| Apgar score at 5 minutes < 4 or umbilical cord pH <7.0 or base deficit ≥ 12 mmol/L | 94.0 | 5.2 | 0.8 | |
| Liveborn, gestational age ≥ 34 weeks, admitted to NICU or special care nursery for respiratory conditions (N = 4,641) | Livebirth | 99.7 | 0.1 | 0.2 |
| Gestational age ≥ 34 weeks | 97.3 | 2.6 | 0.1 | |
| Admitted to NICU or special care nursery | 97.4 | 2.2 | 0.4 | |
| Singleton, gestational age ≥ 37 weeks, vertex presentation, clinical diagnosis of shoulder dystocia, no antepartum fetal death, no fetal anomaly (N = 2,640) | Singleton | 98.8 | 0.0 | 1.2 |
| Gestational age ≥ 37 weeks | 98.7 | 0.2 | 1.1 | |
| Vertex at admission | 94.4 | 0.5 | 5.1 | |
| Clinical diagnosis of shoulder dystocia | 91.9 | 7.8 | 0.3 | |
| No antepartum fetal death | 95.9 | 0.7 | 3.4 | |
| No fetal anomaly | 96.1 | 0.3 | 3.6 |
Approximately 5.9% of women in our study had missing information on fetal presentation. Given the importance of fetal presentation in our analysis, we performed multiple imputation.8 A logistic regression model imputed the likelihood of vertex/non-vertex presentation in a particular subject multiple times based on other obstetric characteristics, including maternal race, parity, previous uterine scar, number of fetus, external cephalic version, smoking, placenta previa, cephalopelvic disproportion, gestational age, reason for admission to labor/delivery, trial of labor, induction, fetal scalp electrode, operative vaginal delivery and mode of delivery. When the imputed data were analyzed, the uncertainty that was related to imputation was taken into account.
To make our study population reflect the overall U.S. obstetric population and to minimize the impact of the various number of births from different institutions, we assigned a weight to each subject based on ACOG district, maternal race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic and others), parity (nulliparas vs. multiparas) and plurality (singleton vs. multiple gestation). We first calculated the probability of each delivery with these four factors according to the 2004 National Natality data;9 publicly available National Natality data can no longer be separated by state after 2004. Then, based on the number of subjects each hospital contributed to the database, we assigned a weight to each subject. Appendix II indicates that the weighted study population is close to the entire U.S. obstetric population. Therefore, we used the weighted sample throughout our analyses.
APPENDIX II.
Description of the study population in comparison to the 2004 U.S. birth cohort
| Characteristics | CSL cohort (non-weighted) | CSL cohort (weighted) | U.S. Birth Cohort† |
|---|---|---|---|
| No. of women | 206,969 | 3,997,436 | 4,018,091 |
| Race/ethnicity* (%) | |||
| Non-Hispanic white | 49 | 57 | 57 |
| Non-Hispanic black | 22 | 14 | 14 |
| Hispanics | 17 | 23 | 23 |
| Asian/Pacific Islander | 4 | 3 | 5 |
| Other/unknown | 8 | 3 | 1 |
| Nullipara* (%) | 44 | 40 | 40 |
| Multifetal gestation* (%) | 2.3 | 1.7 | 1.7 |
| Maternal age (mean, years) | 27.6 | 28.1 | 27.4 |
| Cesarean delivery (%) | 29.4 | 30.5 | 31.1 |
| Gestational age (mean, weeks) | 38.2 | 38.1 | 38.6 |
| Preterm birth (< 37 weeks, %) | 13.0 | 14.1 | 12.8 |
These factors plus ACOG district were used to create sample weights.
2006 national natality data.18
We defined “attempting vaginal delivery or a trial of labor” as all vaginal deliveries plus cesarean deliveries with at least two vaginal examination data in the labor progression (or labor curve) database. For indications for cesarean delivery, we first listed all major indications and the percent of cesarean deliveries with a specific indication (one woman may have more than one indication). “Elective cesarean delivery” was defined as cesarean for clinical indications of: 1) elective as denoted in the electronic medical record, 2) declining a trial of labor, and 3) a variety of factors that are not considered accepted indications for cesarean delivery such as elderly gravida, multiparity, remote from term, postterm/postdates, diabetes, chorioamnionitis, chronic or gestational hypertension without preeclampsia/eclampsia, premature rupture of the membranes, HPV infection, GBS positive, polyhydramnios, fetal demise, tubal ligation, and social/religion concerns. We then grouped all indications into three hierarchical, mutually exclusive categories: “clinically indicated”, “mixed”, and “truly elective”. The “mixed” group included cesarean deliveries where not enough detailed information (e.g., HIV with an unknown viral load or unknown presentation of twins) was available to judge the necessity or where the clinical indications were not that strong (e.g., preeclampsia).
Duration of labor arrest was calculated as the duration of no appreciable change of cervical dilation in the 1st stage and the time interval between the first 10 cm and delivery in the 2nd stage. “No appreciable change in cervical dilation” was defined as within 1 cm of change in dilation prior to delivery. All statistical analyses were performed using SAS version 9.1. Given that this is a descriptive analysis with a very large sample size, no statistical testing was performed; nor were confidence intervals provided.
RESULTS
The overall rate of cesarean delivery in our cohort was 30.5%, varying from 20% to 44% among the participating hospitals. Table 1 presents the overall and specific categories of cesarean delivery (primary vs. repeat, and prelabor vs. intrapartum) by maternal characteristics. With advancing maternal age, the overall cesarean rate doubled from 21.0% at age < 20 years to 42% in women 35 years or older, mainly due to repeat, prelabor cesarean deliveries. Obesity was associated with substantially higher cesarean rates in all categories. One in three nulliparas was delivered by cesarean section (31.2%). Multiparas had an overall cesarean rate similar to that of nulliparas (30.0%), primarily due to prelabor, repeat cesarean delivery.
Table 1.
Cesarean rate by maternal characteristics and type of cesarean delivery
| Proportion of the population (%) | Overall Cesarean Rate* (%) | Primary Cesarean Delivery* (%) | Repeat Cesarean Delivery* (%) | Prelabor Cesarean Delivery* (%) | Intrapartum Cesarean Delivery* (%) | |
|---|---|---|---|---|---|---|
| N (unweighted) | 206,969 | 60,866 | 38,336 | 22,530 | 32,380 | 28,486 |
| N (weighted) | 3,997,436 | 1,220,877 | 727,941 | 492,935 | 696,583 | 524,294 |
| Maternal age (years) | ||||||
| <20 | 8.6 | 21.0 | 18.8 | 2.2 | 6.6 | 14.5 |
| 20 – 24 | 22.6 | 24.6 | 16.5 | 8.1 | 11.7 | 12.9 |
| 25 – 29 | 27.0 | 28.1 | 16.6 | 11.5 | 15.9 | 12.3 |
| 30 – 34 | 24.7 | 33.6 | 18.9 | 14.9 | 20.6 | 13.2 |
| 35+ | 17.2 | 42.2 | 21.7 | 20.5 | 28.3 | 14.0 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 56.6 | 29.9 | 18.3 | 11.6 | 17.8 | 12.1 |
| Non-Hispanic black | 14.2 | 33.4 | 20.5 | 13.2 | 17.4 | 16.3 |
| Hispanic | 22.9 | 30.3 | 16.5 | 13.8 | 16.9 | 13.4 |
| Asian/Pacific Islanders | 3.2 | 30.6 | 19.6 | 11.1 | 15.5 | 15.2 |
| Other | 3.1 | 29.3 | 17.4 | 11.8 | 17.2 | 12.1 |
| Health insurance | ||||||
| Private | 53.5 | 31.3 | 19.3 | 12.0 | 17.9 | 13.4 |
| Public | 33.3 | 31.6 | 18.1 | 13.6 | 17.9 | 13.8 |
| Other/unknown | 13.2 | 24.6 | 14.0 | 10.6 | 14.2 | 10.3 |
| Body mass index at delivery (km/m2) | ||||||
| <25 | 13.5 | 22.3 | 14.0 | 8.4 | 13.8 | 8.6 |
| 25.0 – 29.9 | 37.7 | 25.6 | 15.8 | 9.8 | 14.5 | 11.1 |
| 30.0 – 34.9 | 27.6 | 32.6 | 19.3 | 13.3 | 18.4 | 14.3 |
| 35.0+ | 21.2 | 43.7 | 24.6 | 19.2 | 25.0 | 18.8 |
| Parity | ||||||
| Nulliparas | 40.4 | 31.2 | 31.2 | 0.1 | 9.7 | 21.5 |
| Multiparas | 59.6 | 30.0 | 9.4 | 20.6 | 22.7 | 7.4 |
| Number of fetuses | ||||||
| Singleton | 98.3 | 29.9 | 17.7 | 12.2 | 16.9 | 13.1 |
| Multiple | 1.7 | 65.9 | 47.0 | 18.9 | 50.6 | 15.3 |
| Labor induction in women attempting vaginal delivery | ||||||
| No | 56.2 | 11.8 | 9.1 | 2.7 | 0 | 11.8 |
| Yes | 43.8 | 21.1 | 19.5 | 1.6 | 0 | 21.1 |
| Previous uterine scar | ||||||
| No | 84.9 | 21.1 | 21.1 | 0 | 7.8 | 13.2 |
| Yes | 15.1 | 83.6 | 2.2 | 81.4 | 71.3 | 12.3 |
| Vertex presentation (Singleton only) | ||||||
| No | 5.1 | 92.8 | 71.1 | 21.6 | 73.8 | 19.0 |
| Yes | 94.9 | 26.6 | 14.9 | 11.7 | 13.8 | 12.8 |
| Hospital type | ||||||
| University affiliated teaching hospital | 60.7 | 32.9 | 19.4 | 13.5 | 19.5 | 13.5 |
| Teaching community hospital | 35.9 | 27.2 | 16.7 | 10.5 | 14.5 | 12.8 |
| Non-teaching community hospital | 3.4 | 23.1 | 12.8 | 10.4 | 12.6 | 10.5 |
Overall cesarean rate = primary + repeat cesarean rates = prelabor + intrapartum cesarean rates. Repeat cesarean section includes cesarean section after previous myomectomy in nulliparas (0.1%).
65.9% of multi-fetal gestations were delivered by cesarean section (in comparison to 29.9% in singleton pregnancies), and a majority of multifetal gestations did not attempt vaginal delivery. The induction rate was 36.2%, using all deliveries as the denominator, or 43.8% among women attempting vaginal delivery. The cesarean rate was twice as high in induced labor than in spontaneous labor in all pregnancies (21.1% vs. 11.8%) and in singleton nulliparas with vertex presentation (31.4% vs. 14.2%). In women with a previous uterine scar, 28.8% had a trial of labor. Among them, the rate of successful VBAC was 57.1%. Overall, 83.6% of women with a uterine scar were delivered by cesarean section. 92.8% of fetuses with non-vertex presentation were delivered by cesarean section.
To further examine the relative contribution of obstetric factors to the cesarean rate, we grouped the women into 7 categories according to the classification scheme proposed by Robson.10 Table 2 indicates that term pregnancies with a vertex, singleton fetus and previous uterine scar contributed the most cesarean deliveries in the U.S. (30.9%), followed by term gestations with a singleton, vertex fetus whose labor was induced (19.2%). Multi-fetal gestations and pregnancies with non-vertex presentation accounted for only 6.7% of all births but contributed to one-fifth of all cesarean deliveries.
Table 2.
Relative contribution of obstetric factors
| Robson Classification* | Obstetric characteristics | Proportion of all deliveries (%) | Rate of prelabor cesarean Delivery (%) | Rate of intrapartum cesarean delivery (%) | Proportion of all cesarean deliveries (%) |
|---|---|---|---|---|---|
| 1 | Nulliparous, singleton, vertex, ≥37 weeks, spontaneous labor | 16.5 | -- | 14.8 | 8.0 |
| 3 | Multiparous, singleton, vertex, ≥37 weeks, no uterine scar, spontaneous labor | 20.9 | -- | 3.1 | 2.1 |
| 2a + 4a | All women, singleton, vertex, ≥37 weeks, no uterine scar, induced labor | 30.9 | -- | 19.0 | 19.2 |
| 2b + 4b | All women, singleton, vertex, ≥37 weeks, no uterine scar, prelabor cesarean delivery | 2.4 | 100 | -- | 7.9 |
| 5 | All women, singleton, vertex, ≥37 weeks, uterine scar | 11.5 | 70.2 | 11.8 | 30.9 |
| 10 | All women, singleton, vertex, <37 weeks, regardless uterine scar | 11.1 | 21.5 | 14.2 | 13.0 |
| 6 + 7 + 8 + 9 | All women, multiple gestation or non-vertex presentation, regardless uterine scar | 6.7 | 67.7 | 17.9 | 18.8 |
| Overall | 100% | 100% |
Based on classification scheme proposed by Robson (2001).
The main indication for prelabor cesarean delivery was previous uterine scar, followed by fetal malpresentation (Table 3). Among intrapartum cesarean deliveries, approximately half of them were performed for “failure to progress” or “cephalopelvic disproportion”, and more than a quarter were performed for indications of non-reassuring fetal testing or fetal distress. “Truly elective” cesarean delivery accounted for 9.6% of prelabor and 2.1% of intrapartum cesarean deliveries. As some prelabor cesarean deliveries in the “mixed” group were eligible for a trial of labor (e.g., single previous low transverse cesarean section and vertex-vertex twin gestation), the “truly elective” cases may be an underestimate in the current study.
Table 3.
Main recorded indications for cesarean delivery
| Indication | Prelabor Cesarean Delivery (%) | Intrapartum Cesarean Delivery (%) |
|---|---|---|
| Individual indications# | ||
| Previous uterine scar | 45.1 | 8.2 |
| Failure to progress/cephalopelvic disproportion | 2.0 | 47.1 |
| Elective* | 26.4 | 11.7 |
| Non-reassuring fetal testing/fetal distress | 6.5 | 27.3 |
| Fetal malpresentation | 17.1 | 7.5 |
| Hypertensive disorders | 3.1 | 1.6 |
| Fetal macrosomia | 3.3 | 1.2 |
| Multiple gestation | 2.8 | 0.8 |
| Grouped indications (hierarchical, mutually exclusive) | ||
| Clinically indicated‡ | 9.7 | 74.9 |
| Mixed§ | 80.7 | 23.0 |
| Truly elective† | 9.6 | 2.1 |
| Total | 100 | 100 |
Women may have more than one indication. The total percentage may exceed 100%.
Indications for elective cesarean delivery include “elective”, declining trial of labor, elder gravid, multiparity, remote from term, postterm/postdates, diabetes, chorioamnionitis, chronic or gestational hypertension without preeclampsia/eclampsia, premature rupture of the membranes, HPV infection, GBS positive, polyhydramnios, fetal demise, tubal ligation, and social/religion concerns.
Clinically indicated includes emergency, non-reassuring fetal heart rate tracing/fetal distress, failure to progress, cephalopelvic disproportion, failed induction, failed forceps, failed VBAC, placenta abruption, placenta previa, shoulder dystocia, and history of shoulder dystocia;
Mixed includes: previous uterine scar, breech/malpresentation, fetal anomalies, fetal macrosomia, HIV infection, multiple gestation, preeclampsia/eclampsia, other;
Truly elective: without any indication in the “clinically indicated” or “mixed” categories.
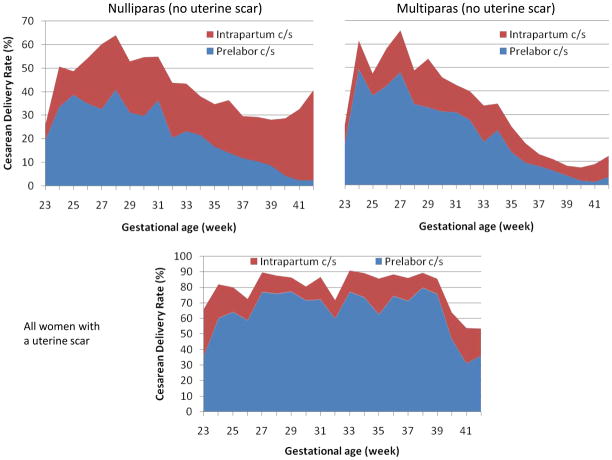
The cesarean rate was higher at the earlier gestational ages of delivery (Figure 1). For example, the cesarean delivery rate was over 60% at 28 weeks gestation and declined gradually with advancing gestation. In nulliparas, intrapartum cesarean deliveries constituted the majority of cesarean sections at term (≥37 weeks). Among multiparas, most cesarean deliveries occurred prior to the onset of labor across all gestational ages. Unlike in most women, the cesarean rate in women with a uterine scar did not decline with advancing gestation until 40 weeks.
Figure 1.
Cesarean delivery rate by type of cesarean (prelabor vs. intrapartum), gestational age and parity (nulliparas, multiparas, women with a uterine scar).
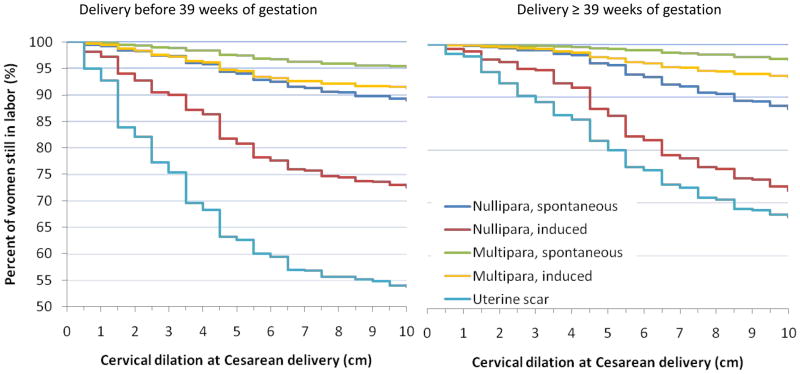
We further examined the timing of cesarean delivery relative to cervical dilation among those women with vertex, singleton gestation attempting vaginal delivery (Figure 2). Induced labor was associated with twice as many cesarean deliveries as spontaneous labor in both nulliparas and multiparas before and after 39 weeks, and the cesarean section was performed earlier in terms of cervical dilation in induced labor than in spontaneous labor. The cesarean rate was substantially higher in women with a uterine scar (47% and 33% before and after 39 weeks, respectively), and the cesarean section was performed at lower cervical dilation before 39 weeks than after 39 weeks.
Figure 2.
Cervical dilation at intrapartum cesarean delivery among women attempting vaginal delivery by parity, onset of labor (induced vs. spontaneous onset), previous uterine scar in singleton gestations
Table 4 presents total duration of labor arrest before intrapartum cesarean delivery for “failure to progress”, “cephalopelvic disproportion” or “failed induction” among singleton, vertex presentation with and without a uterine scar. The duration of labor arrest declined as labor advanced. At 4 cm of cervical dilation, for example, the median duration for nulliparas was 4 hours and less than 3 hours at 6 cm. The duration was similar between spontaneous and induced labors. However, nearly half of cesarean sections were done before 6 cm in induced labor and in women with a previous uterine scar. One-third of cesarean deliveries at the 2nd stage were performed at less than 3 hours in nulliparas while a quarter were performed at less than 2 hours in multiparas.
Table 4.
Total duration of labor arrest (in hours) prior to intrapartum cesarean deliveries for “failure to progress/cephalopelvic disproportion” or “failed induction” among singleton, vertex presentation with and without a previous uterine scar
| Cervical dilation at cesarean section (cm) | Nulliparas | Multiparas | Women with a previous uterine scar having a trial of labor Median (cumulative percentage) |
||
|---|---|---|---|---|---|
| Spontaneous labor Median (cumulative percentage) |
Induced labor Median (cumulative percentage) |
Spontaneous labor Median (cumulative percentage) |
Induced labor Median (cumulative percentage) |
||
| 0 | 13.8 (0.3%) | 14.5 (4%) | -- (0.1%) | 16.0 (2%) | 9.6 (2%) |
| 1 | 10.0 (2%) | 9.4 (10%) | -- (1%) | 11.7 (6%) | 6.3 (6%) |
| 2 | 6.8 (3%) | 5.6 (15%) | -- (3%) | 8.6 (9%) | 6.5 (16%) |
| 3 | 4.0 (7%) | 4.3 (23%) | 6.9 (6%) | 5.5 (16%) | 5.0 (21%) |
| 4 | 4.0 (17%) | 4.0 (40%) | 2.7 (14%) | 3.4 (29%) | 2.5 (36%) |
| 5 | 3.5 (28%) | 3.2 (53%) | 4.0 (19%) | 2.4 (44%) | 2.8 (49%) |
| 6 | 2.9 (38%) | 2.8 (63%) | 3.6 (31%) | 2.5 (54%) | 3.2 (62%) |
| 7 | 2.8 (46%) | 2.2 (69%) | 2.8 (39%) | 2.6 (63%) | 2.4 (69%) |
| 8 | 3.0 (56%) | 2.6 (75%) | 2.8 (53%) | 2.9 (71%) | 2.0 (75%) |
| 9 | 2.2 (65%) | 2.3 (81%) | 2.8 (69%) | 1.7 (83%) | 1.3 (84%) |
| 2nd stage | 3.8 (100%) | 3.5 (100%) | 2.9 (100%) | 2.8 (100%) | 2.3 (100%) |
| Among the 2nd stage cesarean deliveries (cumulative percentage) | |||||
| < 2 hr | 12% | 14% | 24% | 27% | 39% |
| 2 – 3 hr | 33% | 35% | 55% | 63% | 56% |
| 3 – 4 hr | 55% | 63% | 74% | 81% | 76% |
| ≥4 hr | 100% | 100% | 100% | 100% | 100% |
--: The number of subjects is too small to have a meaningful value.
COMMENTS
Our study is a large, contemporary assessment of cesarean delivery practice for the U.S. obstetric population. We found that:
One in three nulliparas was delivered by cesarean section.
Prelabor repeat cesarean delivery due to a previous uterine scar was the most common reason for cesarean section, contributing almost a third of all cesarean deliveries. In contrast, the rate of trial of labor is disappointingly low, and the associated success rate for vaginal birth has declined.
Approximately 44% of women attempting vaginal delivery had induced labor, and that within this group the cesarean rate was twice as high as in women with spontaneous labor.
A high percentage of intrapartum cesarean deliveries were performed before 6 cm of cervical dilation, particularly in nulliparas, induced labor and women attempting VBAC.
VBAC
The VBAC rate experienced precipitous decline since 1996, which coincided with an over 50% increase in cesarean rate during the same period.3 Our study indicates that prelabor repeat cesarean sections currently have a profound impact on the overall cesarean rate. Some experts estimate that two-thirds of women with a uterine scar are eligible for a trial of labor.11 Yet, the rate of trial of labor is quite low in the U.S. In 1999 – 2002, Landon et al.12 reported a rate of 38.9% in a NICHD Maternal-fetal Medicine Unit Research Network study. The rate of trial of labor declined significantly from 48.3% in 1999 to 30.7% in 2002. This is consistent with our finding that the rate was 28.8% in 2005 – 2007, and ours may be an overestimate for the national level because academic institutions are overrepresented in our study. The low rate of trial of labor has been attributed in part to a slight increase in absolute risks of maternal and neonatal morbidity, professional liability concerns and physician and patient’s attitude towards VBAC.5 The recent change in ACOG recommendations also has reduced the availability of VBAC services in many hospitals.13
The success rate of attempted VBAC in our study was markedly lower (57.1%) than that in previous large studies. Lieberman et al.14 noted a VBAC success rate of 87% in 41 birth centers in 1990 – 2000. Macones et al.15 found a success rate of 75.5% in a regional study with 17 hospitals in 1996 – 2000, similar to that found by Landon et al.12 (73.4%). Gregory et al.16, using 2002 California hospital discharge data, reported an overall success rate of 67%. One possible explanation of our finding is that the success rate of attempted VBAC is more recently influenced by other factors. Physicians and patients may be less committed even during a trial of labor.17 For instance, half of the intrapartum cesarean sections for dystocia were performed before 6 cm of cervical dilation in our study. Many women may not be in active phase before that time.18 The frequency of oxytocin use for labor augmentation in the trial of labor was 1/6 of that in multiparous women without a uterine scar.
Another possible reason for the low success rate may be related to our definition of “a trial of labor”. A woman with a uterine scar, minimal dilation and two pelvic exams recorded in the labor database would have been considered a trial of labor. Such cases may have increased the VBAC rate but reduced the success rate. However, findings of vaginal exams that were entered in the labor progression (labor curve) computer system on the labor floor are often an indication for intended vaginal delivery. Thus, the above scenario may not have substantially affected our results.
Induction of labor
In parallel with the increasing cesarean rate, the rate of labor induction also has increased significantly in many developed countries, including a doubling of the U.S. rate between 1990–2000 (from 9.5% in 1990 to 20.2% in 2000, and 22.6% in 2006).19 In comparison, the overall induction rate was 35.2% in our study (around 2006); the induction rate in women attempting vaginal delivery was 43.8%. These findings suggest that the national figures based on birth certificates may have been an underestimate of the true national induction rate.20
For medically-indicated induction of labor, the benefits for the mother and/or the fetus are indisputable. However, controversies arise when labor is induced for women with absent or marginal clinical indications.21–23 Our data show that induced labor was twice as likely to result in cesarean delivery than spontaneous labor. Half of cesarean sections for dystocia in induced labor were performed before 6 cm of dilation, suggesting that clinical impatience may play a role in decision-making. Some studies also suggest that induction of labor increases the risk of postpartum hemorrhage and blood transfusion.22 Therefore, while more research is warranted, caution is needed to perform elective labor induction, as it may result in maternal morbidity and repeat cesarean deliveries in subsequent pregnancies.
Timing of intrapartum cesarean delivery
The high proportion of intrapartum cesarean deliveries done before 6 cm of cervical dilation is concerning, particularly in nulliparas and in induced labor. The active phase of labor is typically considered starting at 4 cm of dilation.24,25 However, a recent study showed that multiparas may not start the active phase until 6 cm while nulliparas may not have a typical active phase of labor.18 In contemporary nulliparous women who had vaginal delivery and normal perinatal outcome, labor may not progress for 6 hours at 4 cm or 3 hours at 5 cm of dilation (results not shown). In the current study, the median duration of labor arrest in nulliparas, including periods before and after any intervention, was 4 hours at 4 cm. Thus, a cesarean section for dystocia before 6 cm in nulliparas appears too soon in some cases.
We also found that one-third of cesarean deliveries at the 2nd stage were performed at less than 3 hours in nulliparas while a quarter were performed at less than 2 hours in multiparas. This is of concern because ACOG guidelines define arrest of descent as greater than 3 hours in nulliparas with epidural analgesia and greater than 2 hours in multiparas with epidural analgesia.26 Given that 90% of the subjects used epidural analgesia and that the median duration in the 2nd stage arrest included “decision-to-incision” time, the true waiting period in the 2nd stage arrest appears shorter than ACOG recommendations in many cesarean cases.
It should be noted that even though we selected 12 institutions across 9 ACOG districts, our study subjects were not a random sample of all births in the U.S. Academic institutions are overrepresented in our cohort. This may in part explain why our weighted preterm birth rate was higher (14.1%) than the national average (12.8% in 2006)19 and why the induction rate in our study was higher than the published national average. Yet, our overall cesarean rate was slightly lower than the corresponding national average (30.5% vs. 31.1% in 2006).19 Nonetheless, for the first time we were able to separate cesarean delivery by prelabor and intrapartum in a large multicenter study. Our study provides detailed information on when cesarean section was performed, allowing us to identify potential areas for optimal management.
In summary, our study shows that one in three nulliparas is delivered by cesarean section, which has a tremendous impact on subsequent prelabor repeat cesarean delivery. Prelabor repeat cesarean delivery now contributes almost a third of all cesarean deliveries. To make a significant impact on the high cesarean delivery rate in the U.S. the focus should be preventing unnecessary primary cesarean deliveries from several aspects. First, we need to decrease the rate of cesarean delivery associated with a high rate of induction of labor. Cesarean section for dystocia should be avoided before active phase of labor is established particularly in nulliparas, induced labor and VBAC attempts. Second, there should be a clinically accepted indication for performing cesarean delivery. Finally, increasing access to, safety of, and patient education on trial of labor in women with a previous uterine scar and improving the success rate are urgently needed.
Acknowledgments
The Consortium on Safe Labor was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through a contract (Contract No. HHSN267200603425C).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Villar J, Valladares E, Wojdyla D, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006 Jun 3;367(9525):1819–29. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 2.Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 2010;375(9713):490–9. doi: 10.1016/S0140-6736(09)61870-5. [DOI] [PubMed] [Google Scholar]
- 3.Hamilton BE, Martin JA, Ventura SJ. National vital statistics reports, Web release. 12. Vol. 57. Hyattsville, MD: National Center for Health Statistics; Births: Preliminary data for 2007. Released March 18, 2009. [Google Scholar]
- 4.Joseph KS, Young DC, Dodds L, O’Connell CM, Allen VM, Chandra S, Allen AC. Changes in maternal characteristics and obstetric practice and recent increases in primary cesarean delivery. Obstet Gynecol. 2003;102:791–800. doi: 10.1016/s0029-7844(03)00620-3. [DOI] [PubMed] [Google Scholar]
- 5.Macones GA. Clinical outcomes in VBAC attempts: what to say to patients? Am J Obstet Gynecol. 2008;199:1–2. doi: 10.1016/j.ajog.2008.03.040. [DOI] [PubMed] [Google Scholar]
- 6.Habiba M, Kaminski M, Da Fré M, Marsal K, Bleler O, Librero J, Grandjean H, Gratia P, Guaschino S, Hel W, Taylor D, Cuttini M. Cesarean section of request: a comparison of obstetricians’ attitudes in eight European countries. BJOG. 2006;113:647–56. doi: 10.1111/j.1471-0528.2006.00933.x. [DOI] [PubMed] [Google Scholar]
- 7.Murthy K, Grobman WA, Lee TA, Holl JL. Association between rising professional liability insurance premiums and primary cesarean delivery rates. Obstet Gynecol. 2007;110:1264–9. doi: 10.1097/01.AOG.0000287294.89148.23. [DOI] [PubMed] [Google Scholar]
- 8.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 9.Martin JA, Hamilton BE, Sutton PD, et al. National vital statistics reports. 1. Vol. 55. Hyattsville, MD: National Center for Health Statistics; 2006. Births: Final data for 2004. [PubMed] [Google Scholar]
- 10.Robson SM. Can we reduce the cesarean section rate? Best Practice Res Clin Obstet Gynaecol. 2001;15:179–94. doi: 10.1053/beog.2000.0156. [DOI] [PubMed] [Google Scholar]
- 11.Landon MB. Vaginal birth after cesarean delivery. Clin Perinatol. 2008;35:491–504. doi: 10.1016/j.clp.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351:2581–9. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 13.Roberts RG, Deutchman M, King VJ, Fryer GE, Miyoshi TJ. Changing policies on vaginal birth after cesarean: impact on access. Birth. 2007;34:316–22. doi: 10.1111/j.1523-536X.2007.00190.x. [DOI] [PubMed] [Google Scholar]
- 14.Lieberman E, Ernst EK, Rooks JP, Stapleton S, Flamm B. Results of the national study of vaginal birth after cesarean in birth centers. Obstet Gynecol. 2008;111:285–91. [Google Scholar]
- 15.Macones GA, Peipert J, Nelson DB, et al. Maternal complications with vaginal birth after cesarean delivery: a multicenter study. Am J Obstet Gynecol. 2005;193:1656–62. doi: 10.1016/j.ajog.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Gregory KD, Korst LM, Fridman M, et al. Vaginal birth after cesarean: clinical risk factors associated with adverse outcome. Am J Obstet Gynecol. 2008;198:452.e1–452.e12. doi: 10.1016/j.ajog.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 17.Kalish RB, McCullough L, Gupta M, Thaler HT, Chervenak FA. Intrapartum elective cesarean delivery: a previously unrecognized clinical entity. Obstet Gynecol. 2004;103:1137–41. doi: 10.1097/01.AOG.0000128118.37737.df. [DOI] [PubMed] [Google Scholar]
- 18.Zhang J, Troendle J, Mikolajczyk R, Sundaram R, Beaver J, Fraser W. The natural history of the normal first stage of labor. Obstet Gynecol. 2010;115:705–10. doi: 10.1097/AOG.0b013e3181d55925. [DOI] [PubMed] [Google Scholar]
- 19.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, et al. National vital statistics reports. 7. Vol. 57. Hyattsville, MD: National Center for Health Statistics; 2009. Births: Final data for 2006. [Google Scholar]
- 20.Roberts CL, Bell JC, Ford JB, Morris JM. Monitoring the quality of maternity care: how well are labour and delivery events reported in population health data? Pediatr Perinatal Epidemiol. 2009;23:144–52. doi: 10.1111/j.1365-3016.2008.00980.x. [DOI] [PubMed] [Google Scholar]
- 21.Vahratian A, Zhang J, Troendle JF, Sciscione AC, Hoffman MK. Labor progression and risk of cesarean delivery in electively induced nulliparas. Obstetrics and Gynecology. 2005;105:698–704. doi: 10.1097/01.AOG.0000157436.68847.3b. [DOI] [PubMed] [Google Scholar]
- 22.Grobman WA. Elective induction: when? Ever? Clin Obstet Gynecol. 2007;50:537–46. doi: 10.1097/GRF.0b013e31804bdec4. [DOI] [PubMed] [Google Scholar]
- 23.Nicholson JM, Parry S, Caughey AB, Rosen S, Keen A, Macones GA. The impact of the active management of risk in pregnancy at term on birth outcomes: a randomized clinical trial. Am J Obstet Gynecol. 2008;198(511):e1–15. doi: 10.1016/j.ajog.2008.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albers LL, Schiff M, Gorwoda JG. The length of active labor in normal pregnancies. Obstet Gynecol. 1996;87:355–9. doi: 10.1016/0029-7844(95)00423-8. [DOI] [PubMed] [Google Scholar]
- 25.Rouse DJ, Owen J, Hauth JC. Active-phase labor arrest: oxytocin augmentation for at least 4 hours. Obstet Gynecol. 1999;93:323–8. doi: 10.1016/s0029-7844(98)00448-7. [DOI] [PubMed] [Google Scholar]
- 26.American College of Obstetricians and Gynecologists. Dystocia and augmentation of labor. ACOG Practice Bulletin No. 49. Obstet Gynecol. 2003;102:1445–54. doi: 10.1016/j.obstetgynecol.2003.10.011. [DOI] [PubMed] [Google Scholar]