Abstract
Background
Hip arthroscopy is a common orthopaedic procedure used as a diagnostic and therapeutic tool with a multitude of surgical indications. The complication rate is reportedly between 1.3% and 23.3%. Major complications are related to traction, fluid extravasation, and iatrogenic chondral injury. Although osteonecrosis is a concern with any surgical procedure about the hip, this complication has been primarily a theoretical concern with hip arthroscopy.
Case Description
We report the case of a 24-year-old man who presented with a 2-year history of left hip pain. He underwent hip arthroscopy to include débridement of a torn labrum and removal of a prominent pincer lesion for femoroacetabular impingement. Traction was initiated by applying manual traction to the traction bar until 10 mm of joint distraction was obtained. Traction was removed at 90 minutes. At the 3-month followup, MRI showed osteonecrosis in the subcapital region of the left femoral head.
Literature Review
It generally is agreed the magnitude and duration of traction during hip arthroscopy increase the risk of traction-related injuries. Only one previous case of femoral head osteonecrosis associated with hip arthroscopy has been reported, and this may have resulted from the initial traumatic event. Based on anatomic studies, the use of standard arthroscopic portals would not put at risk any dominant normal vascular structures supplying the femoral head. In contrast, the literature shows that femoral head osteonecrosis may develop secondary to a combination of increased intraarticular pressure and traction.
Purposes and Clinical Relevance
We suspect this case of femoral head osteonecrosis after hip arthroscopy was caused by traction used in the procedure.
Introduction
First described by Burman [2] in 1931, hip arthroscopy did not become a common orthopaedic procedure until the 1980s. Today, hip arthroscopy is used as a diagnostic and therapeutic tool, sometimes as an adjunct to other procedures, with a multitude of surgical indications. Indications for hip arthroscopy include diagnostic evaluation of the hip, irrigation and débridement of an infected joint, synovectomy, loose body removal, impingement of the ligamentum teres, treatment of femoroacetabular impingement (FAI), débridement for osteoarthritis, biopsy, and intraoperative control of osteotomy or epiphysiolysis [9]. The current complication rates reported in the literature are between 1.3% and 23.3% [3–6, 9, 10, 17–25]. The major complications associated with hip arthroscopy are related to traction, fluid extravasation, and iatrogenic chondral injury.
Osteonecrosis of the femoral head is most commonly seen in patients between the ages of 20 and 50 years, with an incidence of 10,000 to 20,000 per year in the United States [16]. Although osteonecrosis is a concern with any surgical procedure about the hip, this complication has been more of a possible concern with hip arthroscopy. We found only one report in the literature [19], and the subject of that case report had experienced antecedent trauma thought to have placed the patient at risk for development of this condition.
We report a case of osteonecrosis after hip arthroscopy in a previously healthy patient with no evidence of osteonecrosis on preoperative MRI and review the literature on this topic.
Case Report
A 24-year-old active-duty soldier presented to his primary care provider complaining of three months of hip pain. A noncontrast MRI study was obtained that was interpreted as normal by a nonmusculoskeletal radiologist. During the following 6 months, he was prescribed multiple courses of physical therapy and nonsteroidal antiinflammatory drugs by his primary care provider. His pain was refractory to the physiotherapy and drugs, and he was referred to our orthopaedic clinic. He denied any traumatic events or changes in his symptoms between the time when the MRI was performed and our first clinic visit. On presentation to our clinic the pain was worse after sitting for long periods of time and exacerbated by the aerobic and strength training activities required for his job as a soldier. He also reported a history of painful snapping in his left groin. Our patient was a smoker but denied any history of contact sports, deep-sea diving, steroid treatment or abuse, or alcohol abuse. He had a negative HIV serology and no other diagnosed immune disorders. The previously obtained MRI was interpreted by the surgeon as suggesting an anterior superior labral tear (Fig. 1).
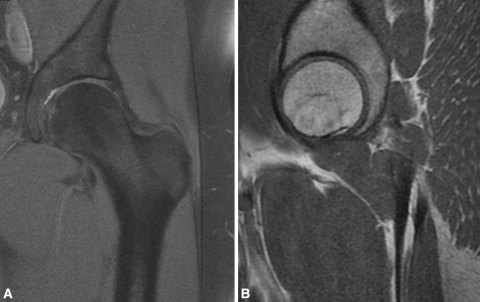
Fig. 1A–B.
Preoperative (A) coronal proton density fat saturation-weighted and (B) sagittal T1-weighted MR images show the femoral head. This noncontrast MRI was performed in March 2008, and shows no evidence of osteonecrosis of the femoral head.
On physical examination, a positive impingement sign was present with limited internal rotation of the left hip. No popping or snapping was elicited on examination. Initial plain radiographs showed a crossover sign suggestive of a pincer-type lesion (Fig. 2). In addition to the labral tear the patient was diagnosed with left hip FAI, pincer-type, and offered hip arthroscopy with decompression of the FAI lesion.
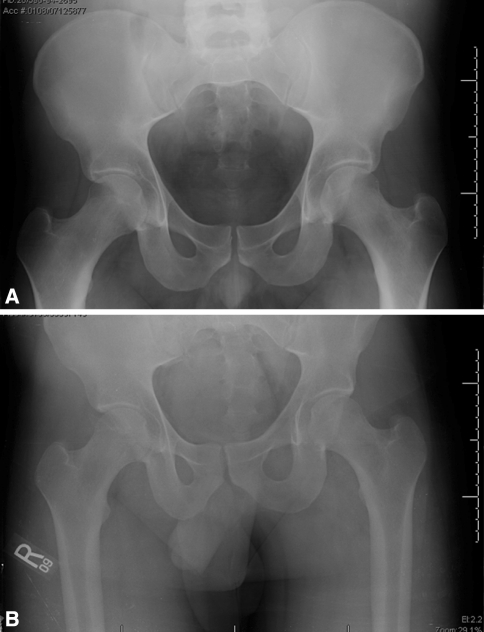
Fig. 2A–B.
(A) A preoperative AP radiograph of the pelvis from September 2008 shows evidence of a cross-over sign bilaterally. (B) The postoperative AP radiograph was taken in the recovery room immediately after surgery.
The procedure was performed with the patient under general anesthesia and pharmacologic paralysis in the supine position on a fracture table for hip distraction. A large, padded perineal post (Philippon KAF; Bledsoe, Grand Prairie, TX) was placed between the patient’s legs and distraction was performed under fluoroscopic guidance by applying manual traction to the traction bar in abduction, followed by adduction over the post until 10 mm of joint distraction was noted. The joint was not aspirated or injected before distraction. The procedure was performed using a pressure- and flow-controlled pump with pressure set at 40 mm Hg. The standard anterolateral portal was created first followed by the midanterior portal created under arthroscopic and fluoroscopic observation. A labral tear in the superolateral aspect of the acetabulum was identified adjacent to the pincer lesion. The torn labrum was débrided as the tissue was extensively degenerated and deemed irreparable. The prominent acetabular pincer lesion then was removed with an arthroscopic burr. Resection of the pincer lesion was performed from the anterior aspect of the rim to the 12 o’clock (straight superior) position. We also made a small transverse anteromedial 1-cm2 capsular window [12] and performed a psoas tenotomy in the central compartment, as our patient had reported painful snapping of his groin. No additional capsulotomy was performed. The peripheral compartment was not observed during the index procedure, and at no point during this procedure was there any abnormal bleeding. The traction was removed at 90 minutes.
At the first postoperative visit at 2 weeks, the patient was walking independently without crutches. Although he reported mild pain with hip ROM, on physical examination, he had no pain with log rolling of the leg. In addition, he had mild tenderness to palpation around his groin and pain with forward flexion past 45°. At 8 weeks he walked without an antalgic gait or substantial pain and stated he had attempted running. He reported he continued to have pain with extremes of motion and running.
At the 3-month followup, the patient had increasing pain with ROM, a mild antalgic gait, and night pain. MRI showed a heterogeneous increased signal in the subcapital region of the left femoral head consistent with femoral head osteonecrosis (Fig. 3). There was no evidence of collapse, and there were no identifiable chondral injuries. The patient was given bisphosphonate therapy, as it reportedly delays the progression of collapse and the need for subsequent surgery [1], and was made nonweightbearing for 6 weeks with continued physical therapy for ROM. Repeat MRI 6 weeks later showed no major changes from the previous study. The region of osteonecrosis was 1.5 × 1.2 × 0.9 cm in the AP, transverse, and craniocaudal dimensions, respectively. The patient was scheduled for a repeat arthroscopy with core decompression and autologous bone marrow graft.
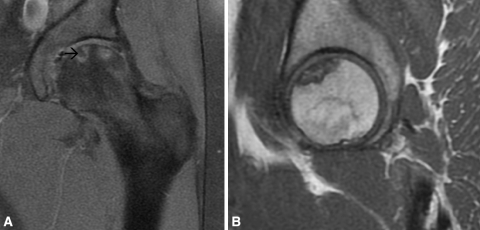
Fig. 3A–B.
Postoperative (A) coronal proton density fat saturation-weighted and (B) sagittal T1-weighted MR images show the region of osteonecrosis of the femoral head. This noncontrast MRI was performed in December 2008 and has a heterogeneous, predominately increased, signal in the subcapital region of the left femoral head involving the 10 o’clock to 2 o’clock position on the coronal image (arrow).
Using the same standard technique as used for the first operation, the femoral head was observed and showed no chondral injury. The lateral vessels were not seen during this second-look arthroscopy. A 7-mm trephine was used to perform the core decompression under biplanar fluoroscopic guidance. Bone marrow aspirate from the iliac crest was injected in the femoral head along with the laterally placed healthy plug of autogenous trephinated bone, which had been removed by the trephine from the femoral neck. The tissue pathology report showed fragments of mature bone with multifocal mild ischemic changes consistent with osteonecrotic bone and no signs of either osteomyelitis or atypia.
Nine months after his core decompression, the patient continues to have pain and decreased ROM but no evidence of articular collapse. The patient was informed data concerning his case would be submitted for publication.
Discussion
Sampson [19] previously reported femoral head osteonecrosis associated with hip arthroscopy in a 36-year-old man treated with partial labrectomy and débridement after sustaining a labral tear secondary to a fall from a ladder. No preoperative MRI was reported in the article to identify whether the patient might already have had findings consistent with femoral head osteonecrosis. Seven months after the initial procedure, MRI revealed femoral head osteonecrosis and a core decompression was performed. Sampson hypothesized the patient was already at an increased risk for femoral head osteonecrosis secondary to the high energy sustained during the injury. Additionally, it was postulated either traction or the partial capsulectomy performed to facilitate instrument mobility might have contributed to development of femoral head osteonecrosis [20]. Although no reports of femoral head osteonecrosis after treatment of FAI exist, Ilizaliturri [11] reports this as a theoretical risk, as the most lateral aspect of the cam deformity is close to the area where the medial circumflex artery enters the hip capsule behind the lateral synovial fold.
In a cadaveric study by Kalhor et al. [12], the medial femoral circumflex artery was confirmed as the dominant blood supply to the femoral head in the majority of adults, although several specimens showed the inferior gluteal artery was predominant. The authors describe the medial femoral circumflex artery as entering the surface of the femoral side of the capsule from the periphery and gives off branches that run from distal to proximal circumferentially around the capsule. The lateral synovial fold, running from the greater trochanter upward along the lateral side of the neck to the lateral margin of the head, is a constant and reliable landmark used in hip arthroscopy to identify the branches of the medial femoral circumflex artery that lie behind it [11]. The most lateral aspect of the cam deformity is close to the lateral synovial fold, which could be disrupted while performing femoral head/neck junction osteoplasty for a cam lesion [11]. The lateral epiphyseal vessels, found behind the lateral synovial fold, arise from the medial femoral circumflex artery after it enters the hip capsule at the level of the superior gemellus [11]. Our case did not involve any débridement extending beyond the central compartment and the lateral epiphyseal vessels were not at risk from the arthroscopic procedure.
The association between these major vascular structures and the standard hip arthroscopy portals was evaluated by Elsaidi et al. [7], who reported the posterolateral portal was located a mean distance of 19 mm from the ascending branch of the lateral femoral circumflex artery. Even with the addition of traction up to 23 kg, there was no change in the distance from the portal sites to their associated neurovascular structures. Neither the anterolateral nor the midanterior portals, which were used in our procedure, have been associated with any dominant vascular structures. In our patient, there is the possibility the lateral femoral circumflex artery was disrupted during portal placement at its location anterior to the femoral attachment of the capsule running laterally toward the greater trochanter, although this vessel reportedly contributes only one or two small branches to the femoral head and neck blood supply [12].
Complications related to traction injuries during hip arthroscopy can be classified as nerve injuries, soft tissue injuries, and the previously mentioned possible concern of femoral head osteonecrosis [11]. The standard hip arthroscope is 5 mm in size and the general consensus is approximately 10 mm of distraction is required for adequate observation of the joint space [4, 8, 9, 15]. We used a 4-mm Karl Storz hip scope (Karl Storz-Endoskope, Tuttlingen, Germany) with a 4-mm cannula. Sufficient joint distraction usually is achieved with a mean distraction force between 15 and 30 kg or 200 to 400 N [6, 8, 10], with some cases using distraction up to 50 kg [9]. If a tensiometer is not available to measure the traction force applied during hip arthroscopy, adequate distraction of the joint is determined radiographically using biplanar fluoroscopy to identify the amount of distraction required to see the vacuum phenomenon. In addition to the magnitude of traction required during hip arthroscopy, it generally is agreed a traction time greater than 2 hours will increase the risk of traction-related injuries [19, 20].
The hip is not a highly distensible joint and increases in intracapsular pressure reportedly lead to pressure increases in the marrow that have been correlated to the development of osteonecrosis of the femoral head [14, 23, 24]. The increase in marrow pressure is presumed secondary to a decrease in local blood flow and venous occlusion [14, 22]. Two in vivo studies suggest changes in marrow pressure do not occur until the intracapsular pressure is at least 200 mm Hg and that osteonecrosis of the trabeculae do not occur until this pressure is maintained for 10 hours or more [14, 23]. Vegter and Lubsen [24] used a rabbit model to cause arterial tamponade by maintaining an increased hydrostatic pressure in the hip. After 2 hours they described a fractional osteonecrosis characterized by necrosis of some trabecular osteocytes, although necrosis of bone-forming marrow tissue and vascular tissue was not observed until 6 hours of tamponade. In relation to hip arthroscopy, the combined effect of traction in the face of increased intraarticular pressure has been described. Two animal models suggest no changes occur in the microcirculation or macrocirculation of the hip with increasing weighted traction [18, 21]. In contrast, Svalastoga et al. [22], reported tamponade of the joint alone reduced the mean oxygen partial pressure to 60% of its initial value, with the application of traction in extension further decreasing the mean oxygen partial pressure to 35% of baseline.
The cause of femoral head osteonecrosis in our patient may have been secondary to disruption of the primary blood supply to the femoral head during portal placement or we believe more likely as a result of a traction injury. Standard arthroscopic portals were used during this particular case, with neither portal having a close association with either the medial femoral circumflex or inferior gluteal arteries, both believed capable of contributing the dominant blood supply to the femoral head [12]. According to Kalhor et al. [12], a transverse capsular window in the proximal anteromedial region can be performed safely without risk to the femoral head vascularity, whereas distal transverse capsulotomies are likely to cause damage to the capsular vessels. As our institution has no tensiometer on our traction tables, we were unable to record the exact amount of force used during our arthroscopic procedure. We do not believe excess traction was used, as our procedure lasted less than 2 hours and the joint space was distracted only approximately 10 mm, which in an anesthetized patient requires approximately 300 to 400 N of force [8]. Our patient’s preoperative MRI showed no evidence of femoral head osteonecrosis. If the patient’s 2 years of pain and functional limitations had been attributable to prearthroscopic osteonecrosis, we would have expected to see this on the original MRI, as this imaging modality has the highest sensitivity and specificity to detect early osteonecrosis [13]. The patient had not sustained antecedent trauma, in contrast to the case reported by Sampson [19], in which the patient sustained a high-energy fall. We believe the femoral head osteonecrosis after hip arthroscopy for FAI in our patient was a result of an injury occurring during the arthroscopic procedure.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of Defense or United States government.
This work was performed at William Beaumont Army Medical Center.
References
- 1.Agarwala S, Shah S, Joshi VR. The use of aldendronate in the treatment of avascular necrosis of the femoral head: follow-up to eight years. J Bone Joint Surg Br. 2009;91:1013–1018. doi: 10.1302/0301-620X.91B8.21518. [DOI] [PubMed] [Google Scholar]
- 2.Burman MS. Arthroscopy or the direct visualization of joints. J Bone Joint Surg Am. 1931;4:669–695. [Google Scholar]
- 3.Byrd J. Complications associated with hip arthroscopy. In: Byrd J, editor. Operative Hip Arthroscopy. New York, NY: Thieme; 1998. pp. 171–176. [Google Scholar]
- 4.Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. doi: 10.1016/S0749-8063(05)80111-2. [DOI] [PubMed] [Google Scholar]
- 5.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 6.Clarke MT, Arora A, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. 2003;406:84–88. doi: 10.1097/00003086-200301000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Elsaidi GA, Ruch DS, Schaefer WD, Kuzma K, Smith BP. Complications associated with traction on the hip during arthroscopy. J Bone Joint Surg Br. 2004;86:793–796. doi: 10.1302/0301-620X.86B6.14426. [DOI] [PubMed] [Google Scholar]
- 8.Eriksson E, Arvidsson I, Arvidsson H. Diagnostic and operative arthroscopy of the hip. Orthopedics. 1986;9:169–176. doi: 10.3928/0147-7447-19860201-07. [DOI] [PubMed] [Google Scholar]
- 9.Funke EL, Munzinger U. Complications in hip arthroscopy. Arthroscopy. 1996;12:156–159. doi: 10.1016/S0749-8063(96)90004-3. [DOI] [PubMed] [Google Scholar]
- 10.Griffin DR, Villar RN. Complications of arthroscopy of the hip. J Bone Joint Surg Br. 1999;81:604–606. doi: 10.1302/0301-620X.81B4.9102. [DOI] [PubMed] [Google Scholar]
- 11.Ilizaliturri VM., Jr Complications of arthroscopic femoroacetabular impingement treatment: a review. Clin Orthop Relat Res. 2009;467:760–768. doi: 10.1007/s11999-008-0618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalhor M, Beck M, Huff TW, Ganz R. Capsular and pericapsular contributions to acetabular and femoral head perfusion. J Bone Joint Surg Am. 2009;91:409–418. doi: 10.2106/JBJS.G.01679. [DOI] [PubMed] [Google Scholar]
- 13.Kamata N, Oshitani N, Sogawa M, Yamagami H, Watanabe K, Fujiwara Y, Arakawa T. Usefulness of magnetic resonance imaging for detection of asymptomatic osteonecrosis of the femoral head in patients with inflammatory bowel disease on long-term corticosteroid treatment. Scand J Gastroenterol. 2008;43:308–313. doi: 10.1080/00365520701676773. [DOI] [PubMed] [Google Scholar]
- 14.Kemp HB. Perthes’ disease: the influence of intracapsular tamponade on the circulation in the hip joint of the dog. Clin Orthop Relat Res. 1981;156:105–114. [PubMed] [Google Scholar]
- 15.Kim SJ, Choi NH, Kim HJ. Operative hip arthroscopy. Clin Orthop Relat Res. 1998;353:156–165. doi: 10.1097/00003086-199808000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7:250–261. doi: 10.5435/00124635-199907000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Lo YP, Chan YS, Lien LC, Lee MS, Hsu KY, Shih CH. Complications of hip arthroscopy: analysis of seventy three cases. Chang Gung Med J. 2006;29:86–92. [PubMed] [Google Scholar]
- 18.Naito M, Schoenecker PL, Owen JH, Sugioka Y. Acute effect of traction, compression, and hip joint tamponade on blood flow of the femoral head: an experimental model. J Orthop Res. 1992;10:800–806. doi: 10.1002/jor.1100100608. [DOI] [PubMed] [Google Scholar]
- 19.Sampson TG. Complications of hip arthroscopy. Clin Sports Med. 2001;20:831–835. doi: 10.1016/S0278-5919(05)70288-X. [DOI] [PubMed] [Google Scholar]
- 20.Sampson TG. Complications of hip arthroscopy. Tech Orthop. 2005;20:63–66. doi: 10.1097/01.bto.0000153634.91198.c8. [DOI] [PubMed] [Google Scholar]
- 21.Stucker R, Huter T, Haberstroh J. [he effect of traction treatment on blood flow in the immature hip: an animal study] [in German] Z Orthop Ihre Grenzgeb. 1996;134:332–336. doi: 10.1055/s-2008-1039770. [DOI] [PubMed] [Google Scholar]
- 22.Svalastoga E, Kiaer T, Jensen PE. The effect of intracapsular pressure and extension of the hip on oxygenation of the juvenile femoral epiphysis: a study in the goat. J Bone Joint Surg Br. 1989;71:222–226. doi: 10.1302/0301-620X.71B2.2494185. [DOI] [PubMed] [Google Scholar]
- 23.Tachdjian MO, Grana L. Response of the hip joint to increased intra-articular hydrostatic pressure. Clin Orthop Relat Res. 1968;61:199–212. doi: 10.1097/00003086-196811000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Vegter J, Lubsen CC. Fractional necrosis of the femoral head epiphysis after transient increase in joint pressure: an experimental study in juvenile rabbits. J Bone Joint Surg Br. 1987;69:530–535. doi: 10.1302/0301-620X.69B4.3611153. [DOI] [PubMed] [Google Scholar]
- 25.Villar RN. Arthroscopic debridement of the hip. J Bone Joint Surg Br. 1991;73(suppl II):170–171. [Google Scholar]