Abstract
Background
Revision is technically more demanding than primary total joint arthroplasty (TJA) and requires more extensive use of resources. Understanding the relative risk of rerevision and risk factors can help identify patients at high risk who may require closer postsurgical care.
Objectives/purposes
We therefore evaluated the risk of subsequent revision after primary and revision TJA in the elderly (65 years or older) patient population and identified corresponding patient risk factors.
Patients and Methods
Using the 5% Medicare claims data set (1997–2006), we identified a total of 35,746 patients undergoing primary THA and 72,913 undergoing primary TKA; of these, 1205 who had THAs and 1599 who had TKAs underwent initial revision surgery. The rerevision rate after primary and revision TJAs was analyzed by the Kaplan-Meier method. The relative risk of revision surgery for primary and revision TJAs was compared using hazard ratio analysis.
Results
The 5-year survival probabilities were 95.9%, 97.2%, 81.0%, and 87.4% for primary THA and TKA and revision THA and TKA, respectively. Patients with revision arthroplasty were five to six times more likely to undergo rerevision (adjusted relative risk, 4.89 for THA; 5.71 for TKA) compared with patients with primary arthroplasty. Age and comorbidities were associated with initial revision after primary THA and TKA.
Conclusions
Patients should undergo stringent preoperative screening for preexisting health conditions and careful patient management and followup postoperatively so as to minimize the risk of an initial revision, which otherwise could lead to a significantly greater likelihood of subsequent rerevisions.
Level of Evidence
Level II, prognostic study. See Guideline for Authors for a complete description of levels of evidence.
Introduction
Despite the ability of TJA to improve the functional status and quality of life for many patients [17, 23], 18% of THAs and 8% of TKAs performed annually in the United States are revision procedures [15]. Compared with primary TJA, revision TJA is technically challenging and may require extensive surgical exposure and careful management of periprosthetic bone loss [6]. The complexity of revision TJA also is reflected by the higher hospital cost, longer length of stay, and longer operative time compared with primary procedures [3, 4]. With revision procedures accounting for approximately 19% and 8% of Medicare reimbursements for all THAs and TKAs [22] in the United States, respectively, revision procedures place a tremendous economic burden on the Medicare system. Medicare reimbursements for revision TJA have been projected to exceed $8.5 billion by 2015 [16].
Revision TJAs are associated with elevated risks of complications such as dislocations, infections, venous thromboembolism [9, 14, 19, 24, 26], and mortality [19, 26]. Improvement in quality of life after revision surgery also may be more limited in comparison to primary TJA [18, 23]. Furthermore, previous studies have reported the risk of rerevision for patients undergoing TKA to range from 11% to 19.8% at 5 years and those for patients undergoing THA to be as much as 16.1% at 3 years and 19.4% at 5 years [1, 11, 30–33]. However, these data were obtained from patient cohorts at single institutions [31–33] or by international registries [1, 11, 30], but not for a large, nationally representative patient sample in the United States in which the patient profile or experience of the surgeon/hospital may differ [12, 13]. In the absence of a national joint replacement registry in the United States, national administrative claims databases such as the Medicare claims data set offer very large population-based samples for evaluating the epidemiology and outcomes of TJA [16, 19].
Therefore, the objectives of this study were to (1) determine the relative risk of subsequent revision after primary and revision TJAs; and (2) identify predisposing patient risk factors for revision or rerevision in the elderly (65 years and older) Medicare patient population.
Methods and Materials
The 5% national sample of the Medicare claims database between 1997 and 2006 was used for retrospective review of the outcomes of patients undergoing primary THA and TKA in the elderly patient population. Using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code 81.51 and Current Procedural Terminology (CPT-4) code 27130, patients undergoing primary THA were identified. Similarly, patients undergoing primary TKA were identified using ICD-9-CM code 81.54 and CPT-4 code 27447. To limit the study to the elderly Medicare patient population, we excluded patients younger than 65 years. These patients also were excluded because patients younger than 65 years who enroll in Medicare typically qualify for benefits as a result of their unique health condition in terms of disability or end-stage renal disease. To limit the study to patients undergoing elective TJA, those diagnosed with bone cancer, metastatic cancer, fractures, or joint infection also were excluded. With these exclusions we identified a total of 35,746 patients undergoing primary THAs and 72,913 patients undergoing primary TKAs between 1997 and 2006.
Unique, encrypted Medicare beneficiary identifiers were used to follow these patients longitudinally throughout the 10-year study period. The patients (primary cohort) were tracked longitudinally after their primary procedure to identify subsequent admissions for an initial revision surgery. THA revisions were identified by the ICD-9-CM codes 81.53 and 00.70 to 00.73 and CPT-4 codes 27134, 27137, and 27138, whereas TKA revisions were identified by ICD-9-CM codes 81.55 and 00.80 to 00.84 and CPT-4 codes 27486 and 27487. This subset of patients having revision surgery (revision cohort) then was followed again to identify subsequent admissions for rerevision surgery. Patients who died without undergoing revision or rerevision surgery were considered censored and the longevity of their respective TJA was calculated up to the date of death. Each beneficiary’s enrollment status and date of death were identified in the annual Medicare denominator files. The overall revision probability for each primary and revision cohort at 5 years followup was analyzed by the Kaplan-Meier method.
Hazard ratio analysis (Cox regression) was used to determine the relative risk of revision surgery at 5 years followup for the revision cohort compared with at 5 years followup for the primary cohort. This analysis was adjusted for age, gender, race, and comorbidity. The preexisting health status of each patient was determined using the Charlson comorbidity index [7] and categorized according to their overall degree of comorbidity. The Charlson comorbidity algorithm uses 19 categories of diseases based on diagnosis and surgeries indicated in a patient. A weight with values of 1, 2, 3, or 6 is assigned to each category and the final index is a composite value representing the overall degree of comorbidity. For this analysis, the Charlson index values were grouped into previously established categories [21]: 0 (none), 1–2 (low), 3–4 (moderate), and ≥ 5 (high).
Results
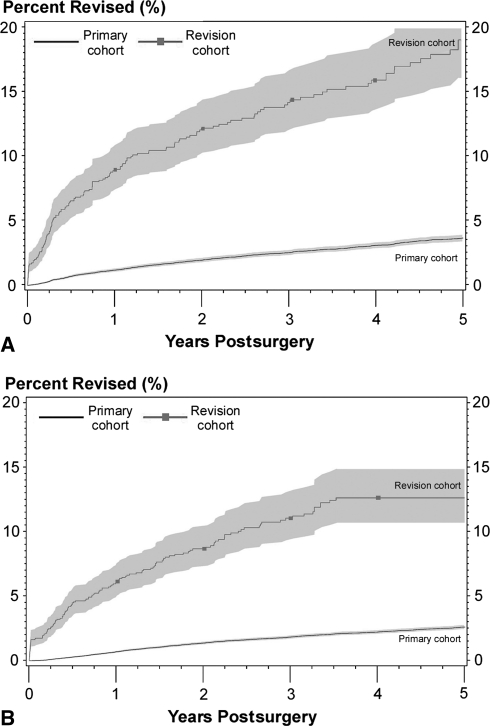
During the study period, 1205 of the 35,746 patients undergoing primary THAs and 1599 of the 72,913 patients undergoing primary TKAs underwent an initial revision surgery, providing patients for the revision cohorts (Table 1). The median (interquartile range) followup durations were 3.33 years (1.49–5.82 years), 3.28 years (1.50–5.88 years), 2.15 years (0.75–4.25 years), and 1.94 years (0.84–3.99 years) for patients undergoing primary THA, primary TKA, revision THA, and revision TKA, respectively. During the study period, patients (10.6%) who had 6619 primary THAs (18.5%), 9396 primary TKAs (12.9%), 221 revision THAs (18.3%), and 170 revision TKAs died. At 5-year followup, the overall survival (revision end point) probabilities were 95.9% and 97.2% for patients undergoing primary THAs and primary TKAs, respectively (Fig. 1). The corresponding overall survival probabilities were 81.0% and 87.4% for patients undergoing revision THAs and revision TKAs, respectively. Patients undergoing revision THAs were approximately five times more likely (p < 0.001) to undergo a rerevision (adjusted relative risk [ARR] = 4.89; 95% confidence interval [CI]: 4.13–5.79) compared with patients undergoing an initial revision. Patients undergoing revision TKAs were six times more likely (p < 0.001) to have a rerevision (ARR = 5.71; 95% CI: 4.81–6.78) than patients undergoing primary surgery.
Table 1.
Demographic characteristics
| Characteristics | Primary THA | Primary TKA | Revision THA | Revision TKA |
|---|---|---|---|---|
| Number of patients | 35,746 | 72,913 | 1205 | 1599 |
| Percent female | 64.7% | 65.2% | 63.3% | 62.5% |
| Percent white | 94.3% | 92.3% | 94.4% | 91.2% |
| Average age ± SD (years) | 74.8 ± 6.5 | 73.6 ± 5.8 | 73.8 ± 6.1 | 72.1 ± 5.3 |
Fig. 1A–B.
The percent of patients undergoing revision (A) THA and (B) TKA are shown (square symbols = revision cohort; no symbols = primary cohort). At 5-year followup, the overall survival probabilities were 95.9% and 97.2% for patients undergoing primary THA and patients undergoing TKA, respectively. The corresponding overall survival probabilities were 81.0% and 87.4% for patients undergoing revision THA and patients undergoing TKA, respectively.
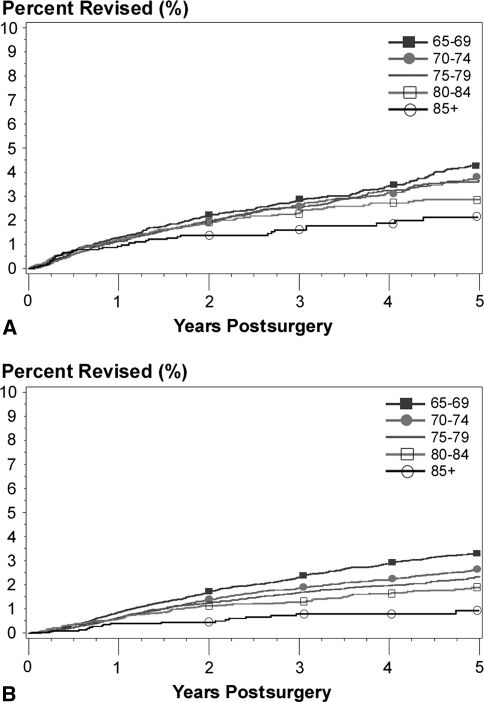
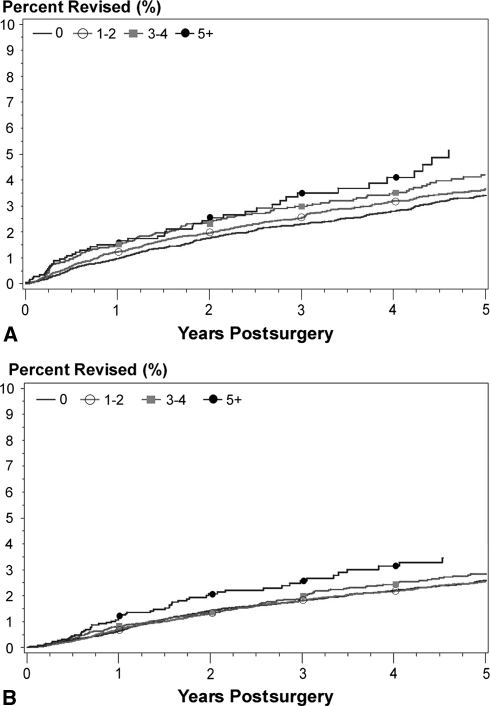
Age (p = 0.002 for THA; p < 0.001 for TKA) and comorbidities (p < 0.001 for THA; p = 0.027 for TKA) were associated with the risk of initial revision for the primary THA and TKA cohort at 5 years followup (Table 2). In general, younger patients undergoing primary surgery (Fig. 2) and patients with more comorbidities undergoing primary surgery (Fig. 3) had a higher risk of revision. For example, at 5 years followup, patients undergoing primary THA aged 70–74, 75–79, 80–84, and 85 + years had 15%, 20%, 26%, and 34% less likelihood (adjusted) of undergoing revision surgery than patients aged 65–69 years, respectively (Table 2). Patients with a Charlson index score of ≥ 5 undergoing primary surgery also had 68% and 40% greater risks of revision (adjusted) after THA and TKA, respectively, compared with those with a Charlson index score of zero (Table 2). Black patients (p = 0.029) and male patients (p = 0.013) also had higher revision risk after primary TKA. The risk of a rerevision also was 49% greater (p = 0.023) for males after revision TKA (Table 3). The remaining factors were not associated with revision risk for patients undergoing primary THA or rerevision risk for patients undergoing revision THA or TKA.
Table 2.
Association between covariates and revision for primary THA and TKA
| Covariate | Group | Primary THA | Primary TKA | ||||
|---|---|---|---|---|---|---|---|
| p value for effect | Adjusted hazards ratio (95% confidence interval) | p Value | p value for effect | Adjusted hazards ratio (95% confidence interval) | p Value | ||
| Age (years) (65–69 reference group) | 70–74 | 0.002 | 0.85 (0.74–0.99) | 0.039 | < 0.001 | 0.75 (0.66–0.84) | < 0.001 |
| 75–79 | 0.80 (0.68–0.93) | 0.004 | 0.67 (0.58–0.76) | < 0.001 | |||
| 80–84 | 0.74 (0.61–0.89) | 0.002 | 0.55 (0.46–0.66) | < 0.001 | |||
| ≥ 85 | 0.66 (0.51–0.86) | 0.002 | 0.31 (0.20–0.46) | < 0.001 | |||
| Gender (female reference group) | Male | 0.447 | 1.05 (0.93–1.18) | 0.447 | 0.013 | 1.14 (1.03–1.26) | 0.013 |
| Race (black reference group) | White | 0.554 | 1.13 (0.84–1.52) | 0.410 | 0.028 | 0.66 (0.45–0.96) | 0.029 |
| Others | 1.31 (0.79–2.20) | 0.297 | 0.78 (0.64–0.95) | 0.015 | |||
| Charlson index score (0 reference group) | 1–2 | < 0.001 | 1.15 (1.02–1.31) | 0.028 | 0.027 | 1.04 (0.94–1.16) | 0.434 |
| 3–4 | 1.37 (1.15–1.63) | < 0.001 | 1.18 (1.01–1.38) | 0.043 | |||
| ≥ 5 | 1.68 (1.30–2.17) | < 0.001 | 1.40 (1.08–1.82) | 0.012 | |||
Fig. 2A–B.
The percent of patients undergoing (A) primary THA (A) and (B) primary TKA stratified by age who had revision surgery is shown (closed squares = 65–69 years old; closed circles = 70–74 years old; no symbol = 75–79 years old; open squares = 80–84 years old; open circles = 85+ years old). Younger patients had a higher risk of revision.
Fig. 3A–B.
The percent of patients undergoing (A) primary THA and (B) primary TKA who underwent revision surgery stratified by comorbidities is shown (Charlson index) (no symbols = 0; open circles = 1–2; closed squares = 3–4; closed circles: 5+). Patients with more comorbidities had a greater risk of undergoing revision surgery.
Table 3.
Association between covariates and rerevision for revision THA and TKA
| Covariate | Group | Revision THA | Revision TKA | ||||
|---|---|---|---|---|---|---|---|
| p value for effect | Adjusted hazards ratio (95% confidence interval) | p value | p value for effect | Adjusted hazards ratio (95% confidence interval) | p value | ||
| Age (years) (65–69 reference group) | 70–74 | 0.818 | 1.25 (0.82–1.90) | 0.306 | 0.197 | 0.79 (0.54–1.17) | 0.246 |
| 75–79 | 1.11 (0.71–1.76) | 0.639 | 0.58 (0.36–0.94) | 0.026 | |||
| 80–84 | 1.02 (0.58–1.79) | 0.935 | 1.03 (0.59–1.80) | 0.926 | |||
| ≥ 85 | 1.35 (0.67–2.74) | 0.405 | 1.17 (0.37–3.77) | 0.788 | |||
| Gender (female reference group) | Male | 0.701 | 0.94 (0.67–1.31) | 0.701 | 0.023 | 1.49 (1.06–2.09) | 0.023 |
| Race (black reference group) | White | 0.413 | 2.17 (0.69–6.84) | 0.186 | 0.076 | 0.53 (0.31–0.92) | 0.025 |
| Others | 2.31 (0.46–11.6) | 0.308 | 0.67 (0.22–2.05) | 0.483 | |||
| Charlson index score (0 reference group) | 1–2 | 0.093 | 0.97 (0.67–1.40) | 0.852 | 0.785 | 1.10 (0.77–1.59) | 0.601 |
| 3–4 | 1.65 (1.05–2.60) | 0.029 | 1.21 (0.73–2.03) | 0.461 | |||
| ≥ 5 | 1.23 (0.57–2.65) | 0.590 | 1.42 (0.63–3.20) | 0.395 | |||
Discussion
Revision TJA is more costly and surgically demanding than primary TJA, which places tremendous economic burden on the healthcare system [3, 4, 16, 22] and provides challenges during patient management and care [6, 8]. Although patients undergoing revision surgery may have a greater risk of complications and mortality [9, 14, 19, 24, 26], the risk of subsequent revision and the relative importance of various risk factors are unclear. Therefore, we sought to characterize the relative risk of subsequent revision after primary and revision TJAs and evaluate predisposing patient risk factors for revision in the elderly US Medicare patient population.
We acknowledge limitations to our study. First, owing to the administrative nature of the Medicare claims database, factors such as implant design, surgical technique, and obesity level are not recorded, thus preventing the analysis of these possible confounding factors [25, 29]. Second, the revision cohort included patients undergoing primary surgery who encountered their first revision surgery at any point during the 10-year study period, including those who underwent short-term and those who underwent longer-term revisions. Third, only patients undergoing revision surgery who had a primary arthroplasty during the study period were included, which provided a shorter followup time for the revision cohort and may have affected the ability to detect risk factors associated with rerevision. Fourth, we did not know the reasons for the revisions. An understanding of the specific reason leading to short-term and longer-term revisions may provide additional insight into the risk of rerevision surgery. However, evaluation of reasons for revision was not possible using the claims database until October 2005, when detailed ICD-9-CM diagnosis codes were introduced [2]. Fifth, information regarding the surgically treated side (laterality) is not provided for approximately 40% of the procedures in recent years. However, we previously found no difference in revision rates between beneficiaries regardless whether the surgically treated side was known [16]. Sixth, unmeasured patient characteristics may account for a large part in the hazard of revision or rerevision. Although our study incorporated various demographic factors, additional analyses using frailty models, which include the potential correlation between the time to the first revision and the time to the second revision, may provide additional insight. Seventh, our findings were based on the Medicare population aged 65 years and older; therefore, it is unclear if rerevision risk in the younger or nonMedicare TJA population is comparable. Despite these limitations, the Medicare claims database provides a large, nationally representative sample of the elderly patient population in the United States and provides a resource for longitudinal followup of outcomes after TJA.
We found Medicare patients who underwent a first revision procedure (revision cohort) were approximately five to six times more likely to undergo a second revision compared with patients who underwent a primary procedure undergoing their first revision (primary cohort). The Swedish National Hip Arthroplasty Register [11] also showed a comparable relative risk of revision for primary and revision cohorts, whereby a 65-year-old man with osteoarthritis is 4.8 times more likely to undergo rerevision compared with the risk of a first revision when the primary implant is revised within the first year after surgery. The overall rates of revision in our study also compare favorably with previous population-based registry studies [1, 30–33] (Table 4). The poorer outcomes after revision surgery could be explained by the more technically demanding procedure, the additional loss of bone stock, or the prolonged operative time during revision procedures [3, 24]. The rerevisions also could be a consequence of the less-than-optimal outcome and the associated complications of the primary joint that preceded the revision procedure or a consequence of the original diseased joint.
Table 4.
Comparisons of revision and rerevision rates with published rates
| Study | Primary THA | Revision THA | Primary TKA | Revision TKA |
|---|---|---|---|---|
| Australian Orthopaedic Association National Joint Replacement Registry [1] | 2.0% (3 years); 2.7% (5 years) | *16.1% (3 years); 19.4% (5 years) | 2.8% (3 years); 3.6% (5 years) | †15.8% (3 years); 19.8% (5 years) |
| Sheng et al. [30] | – | – | – | 11% (5 years) |
| Sierra et al. [31] | – | – | – | 16.1% (5 years); 26.0% (10 years); 31.4% (15 years) |
| Springer et al. [32] | – | 18% (10 years) | – | – |
| Suarez et al. [33] | – | – | – | 18% (12 years) |
| Current study | 4.1% (5 years) | 19.0% (5 years) | 2.8% (5 years) | 12.6% (5 years) |
* These rates reflect minor revision: head and/or insert exchange; the rate for major THA involving replacement of the replacement of the stem and cup was 8.2% at 3 years; †reflect minor revision: patellar replacement and/or tibial insert exchange; the rate for major TKA involving the replacement of tibial and femoral components was 12.5% at 3 years.
We found patients with more comorbidities are more likely to need an initial revision. However, once a revision procedure is done, these patients have a similar likelihood of undergoing a subsequent revision, regardless of their preexisting health condition. In addition to revision surgery, comorbidities have been implicated in the risk of perioperative complications [10, 14, 25] and the overall functional status [28]. A possible implication is that patients should undergo stringent preoperative screening for preexisting health conditions and careful patient management and followup postoperatively so as to minimize the risk of an initial revision, which could progress to subsequent rerevisions. We also found younger patients in the Medicare population were at greater risk of having revision surgery after primary TJA, which may be attributed to their greater activity levels compared with older patients. However, the effects of patient age on revision risk appear variable in differing patient populations [1, 20]. Although higher rates of revision have been reported for younger Swedish patients undergoing primary THA [20], the Australian National Joint Replacement Registry data suggest there were no age-related differences for patients undergoing primary THA [1]. However, increased revision rates were observed for younger patients in the Swedish [27] and Australian primary TKA populations [1]. Regarding outcomes after revision TJA, previous research shows rerevisions are more likely for younger patients [30, 33] in contrast to the lack of association between age and rerevision risk in our data. This lack of agreement may be the result of differences in patient profiles or case mix, although this could not be ascertained because patient comorbidities were not considered in the prior studies [30, 33].
These data provide an understanding of the risk of revision after primary and revision TJAs in the Medicare population. The greater risk of revision after a previous revision procedure could be the consequence of the technically demanding nature of revision surgery and/or of the suboptimal results from the initial primary procedure. Despite the surgical complexities, revision TJA is still a cost-effective means to improve function and relieve pain for patients with a failed primary implant [5], although the reliability may not be as great compared with that of the original primary procedure [18, 23]. More stringent preoperative screening for preexisting health conditions or more attention to patient management and followup postoperatively for patients at high risk may help minimize the risk of an initial revision, which otherwise could lead to a significantly greater risk of rerevisions.
Footnotes
One or more of the authors (KLO, EL, JS, SMK) received research funding from the Homer Stryker Center for Orthopaedic Education and Research.
This work was performed at Exponent, Inc, Philadelphia, PA, USA.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. Hip and Knee Arthroplasty Annual Report 2008. http://www.dmac.adelaide.edu.au/aoanjrr/documents/aoanjrrreport_2008.pdf. Accessed April 28, 2009.
- 2.Bozic KJ. CMS changes ICD-9 and DRG codes for revision TJA. Available at: http://www2.aaos.org/aaos/archives/bulletin/jun05/fline1.asp. Accessed May 5, 2009.
- 3.Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am. 2005;87:570–576. doi: 10.2106/JBJS.D.02121. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am. 2005;87:1746–1751. doi: 10.2106/JBJS.D.02937. [DOI] [PubMed] [Google Scholar]
- 5.Burns AW, Bourne RB, Chesworth BM, MacDonald SJ, Rorabeck CH. Cost effectiveness of revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:29–33. doi: 10.1097/01.blo.0000214420.14088.76. [DOI] [PubMed] [Google Scholar]
- 6.Dennis DA, Berry DJ, Engh G, Fehring T, MacDonald SJ, Rosenberg AG, Scuderi G. Revision total knee arthroplasty. J Am Acad Orthop Surg. 2008;16:442–454. doi: 10.5435/00124635-200808000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 8.Fehring TK, Christie MJ, Lavernia C, Mason JB, McAuley JP, MacDonald SJ, Springer BD. Revision total knee arthroplasty: planning, management, and controversies. Instr Course Lect. 2008;57:341–363. [PubMed] [Google Scholar]
- 9.Jaffer AK, Barsoum WK, Krebs V, Hurbanek JG, Morra N, Brotman DJ. Duration of anesthesia and venous thromboembolism after hip and knee arthroplasty. Mayo Clin Proc. 2005;80:732–738. doi: 10.4065/80.6.732. [DOI] [PubMed] [Google Scholar]
- 10.Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005;435:232–238. doi: 10.1097/01.blo.0000156479.97488.a2. [DOI] [PubMed] [Google Scholar]
- 11.Joint Replacement Unit. The Swedish Hip Arthroplasty Register Annual Report 2005. http://www.jru.orthop.gu.se. Accessed February 26, 2007.
- 12.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909–1916. doi: 10.1302/0301-620X.86B7.14358. [DOI] [PubMed] [Google Scholar]
- 13.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83:1622–1629. doi: 10.1302/0301-620X.83B3.10487. [DOI] [PubMed] [Google Scholar]
- 14.Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 15.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 16.Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, Karrholm J, Garellick G, Havelin LI, Furnes O, Malchau H, Lau E. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(3):144–151. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 17.Loughead JM, Malhan K, Mitchell SY, Pinder IM, McCaskie AW, Deehan DJ, Lingard EA. Outcome following knee arthroplasty beyond 15 years. Knee. 2008;15:85–90. doi: 10.1016/j.knee.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Lubbeke A, Katz JN, Perneger TV, Hoffmeyer P. Primary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidity. J Rheumatol. 2007;34:394–400. [PubMed] [Google Scholar]
- 19.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85:27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84(2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 21.Murray SB, Bates DW, Ngo L, Ufberg JW, Shapiro NI. Charlson Index is associated with one-year mortality in emergency department patients with suspected infection. Acad Emerg Med. 2006;13:530–536. doi: 10.1111/j.1553-2712.2006.tb01004.x. [DOI] [PubMed] [Google Scholar]
- 22.Ong KL, Mowat FS, Chan N, Lau E, Halpern MT, Kurtz SM. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2006;446:22–28. doi: 10.1097/01.blo.0000214439.95268.59. [DOI] [PubMed] [Google Scholar]
- 23.Patil S, Garbuz DS, Greidanus NV, Masri BA, Duncan CP. Quality of life outcomes in revision vs primary total hip arthroplasty: a prospective cohort study. J Arthroplasty. 2008;23:550–553. doi: 10.1016/j.arth.2007.04.035. [DOI] [PubMed] [Google Scholar]
- 24.Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;392:15–23. doi: 10.1097/00003086-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466:1710–1715. doi: 10.1007/s11999-008-0209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, Hozack WJ. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23(6 suppl 1):139–145. [DOI] [PubMed]
- 27.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975–1997: an update with special emphasis on 41,223 knees operated on in 1988–1997. Acta Orthop Scand. 2001;72:503–513. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 28.Roder C, Parvizi J, Eggli S, Berry DJ, Muller ME, Busato A. Demographic factors affecting long-term outcome of total hip arthroplasty. Clin Orthop Relat Res. 2003;417:62–73. doi: 10.1097/01.blo.0000096812.78689.f0. [DOI] [PubMed] [Google Scholar]
- 29.Sadr Azodi O, Adami J, Lindstrom D, Eriksson KO, Wladis A, Bellocco R. High body mass index is associated with increased risk of implant dislocation following primary total hip replacement: 2, 106 patients followed for up to 8 years. Acta Orthop. 2008;79:141–147. doi: 10.1080/17453670710014897. [DOI] [PubMed] [Google Scholar]
- 30.Sheng PY, Konttinen L, Lehto M, Ogino D, Jamsen E, Nevalainen J, Pajamaki J, Halonen P, Konttinen YT. Revision total knee arthroplasty: 1990 through 2002. A review of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2006;88:1425–1430. doi: 10.2106/JBJS.E.00737. [DOI] [PubMed] [Google Scholar]
- 31.Sierra RJ, Cooney WP 4th, Pagnano MW, Trousdale RT, Rand JA. Reoperations after 3200 revision TKAs: rates, etiology, and lessons learned. Clin Orthop Relat Res. 2004;425:200–206. [PubMed]
- 32.Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009;467:166–173. doi: 10.1007/s11999-008-0566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suarez J, Griffin W, Springer B, Fehring T, Mason JB, Odum S. Why do revision knee arthroplasties fail? J Arthroplasty. 2008;23(6 suppl 1):99–103. [DOI] [PubMed]