Abstract
Background
The Pain-Free Hospital Project was initiated in 2003 with the aim of improving pain management throughout Germany. We assessed the current state of pain management in German hospitals.
Methods
From 2004 to 2006, data were obtained anonymously from 2252 patients who had undergone surgery, and 999 who had been treated non-surgically, in a total of 25 hospitals. They were interviewed about the intensity of pain they had experienced and about the effectiveness of its treatment.
Results
No pain at all was reported by 12.4% of patients who had undergone surgery and by 16.7% of the non-surgically treated patients. Moderate to severe pain at rest was reported by 29.5% of the surgical group and 36.8% of the non-surgical group. More than 50% of the overall group reported pain on movement. 55% of the surgical group, and 57% of the non-surgical group, were dissatisfied with their pain management. Peak pain tended to occur outside normal working hours. No analgesic treatment at all was given to 39% of patients in the non-surgical group, even though they were in pain; the corresponding figure for the surgical group was 15% (a significant difference, p<0.001). Inadequately effective pain management was reported by 45.6% of patients in the non-surgical group and 29.6% in the operative group (again, a significant difference. Cancer patients were treated more often with potent opioids.
Conclusion
Severe postoperative pain is still too common among hospitalized patients, particularly pain that is induced by movement. Patients being treated on non-surgical wards also often suffer severe pain needlessly. Pain management seems to be worse for non-surgical patients (cancer patients excepted) than for surgical patients: waiting times for medication are longer, and ineffective medications are given more often. On the other hand, a number of hospitals provide positive examples of the potential effectiveness of pain management for both surgical and non-surgical patients.
Severe intolerable pain during a hospital stay should be avoidable these days—regardless of whether the pain occurs after surgery or subsequent to acute or chronic illness (1, 2). Sufficiently safe medications and analgesic procedures to treat pain have been available for decades, and the organizational structures have been in place in order to successfully implement pain management measures. Acute pain services, to give one example, were introduced in Germany and the United States in the 1980s (3– 11, e1– e11).
At least for the treatment of surgical pain, national and international guidelines have recently been updated, as have standards for the nursing management of pain (e1, 12, e12, e13). However, despite all these initiatives, studies from within Germany and from other countries have shown that the analgesic management of inpatients with surgical pain has improved only gradually since the 1980s (1, 4, 11, 13– 16, e3, e4, e13– e15).
Regarding pain management in Germany, many surveys among doctors have been conducted (11, 16, e4, e5, e14), but in contrast to France (13), England (17), and the US (1) there are very few representative multicenter data that are based on comments from patients thus affected (13, 18). Remarkably, data about the efficiency of acute pain therapy in non-surgical wards are altogether lacking worldwide. To fill this gap, the Pain-Free Hospital Project (Projekt Schmerzfreies Krankenhaus, SFK)* was initiated 7 years ago. Further to analyses of processes and structures, surveys of more than 4000 patients in 25 hospitals were used to set up one of the largest databases worldwide, which included data on the effectiveness of pain management in hospitals. By contrast to other projects (18, 19, e14, e16, e17), data on pain management of patients in wards for internal medicine and neurological wards were included.
The primary objective of the project, whose main results are reported in this article, was to capture, on a nationwide, multicenter basis, the frequency, type, and triggers of pain in hospital, as well as therapeutic approaches and their effectiveness. We also analyzed the influence of the main diagnoses, the type of procedure, the underlying illness, and the therapeutic options available in each hospital. We studied which intensity of pain is accepted by patients, so as to deduce realistic and empirically based threshold values for degrees of pain that are classed as acceptable by those affected and may be regarded as not requiring further therapy.
Methods
We selected 25 hospitals out of a total of 88, in which we surveyed 4157 patients (patients receiving non-surgical treatment on day 13; surgical patients on day 1 after surgery) between 2004 and 2006. The ethics committee of Ruhr University Bochum approved the study. We collected pain therapeutic data from the hospitals (for a more detailed explanation, see eBox).
Methods—Additional information.
A total of 88 hospitals had applied to be included in the study. Of these, 25 of different sizes were selected from all German regions. The criteria for inclusion in the study were:
All the large clinical disciplines except pediatrics had to be represented in a hospital (compulsory: internal medicine, trauma surgery or orthopedics or general surgery, optional: neurology, gynecology, urology, geriatric medicine, subdisciplines within internal medicine or surgery)
the written consent of the hospital and its nursing staff and senior doctors to provide all relevant structural data and to permit and support the survey.
Ethics approval was granted (under the aegis of the ethics committee of Bochum’s Ruhr University) to include 4157 patients (a mean of 166 patients [range 77–294] per hospital) between 2004 and 2006) and to capture structural data on pain management (procedure, responsibilities, and pain management plans). The survey was conducted over 14 days in each hospital. Non-surgical patients received the questionnaire on the first 2 days of the survey (random sample, the mean was on the 13th day of the respective inpatient stay). All surgical patients were surveyed on their first postoperative day (cross sectional survey). The questionnaires were distributed by study assistants from within the nursing teams, who did not participate in administering treatment. Additionally, for each surveyed patient a medical case file was started that included the dates of their diagnosis and treatment.
Patients younger than 18 were excluded, as were patients in intensive care, patients with psychiatric or highly infectious disorders (isolation rooms), patients with linguistic impairments (for example, foreign patients without sufficient knowledge of German), and patients with cognitive or treatment related impairments that did not permit questioning.
All questionnaires were logged centrally and anonymously. Conclusions about individual patients were not possible because the questionnaires were kept separately from the patients’ written consent forms. Both groups of patients received a questionnaire whose language was adapted for the respective treatment (surgical, non-surgical). A numerical rating scale (NRS 0–10) was used to capture current resting pain, pain on movement, and maximum pain in the preceding 24 hours). Patients were able to report pain triggering situations and changes in severe pain by time of day. Each patient was asked whether they had reported their pain within the preceding 24 hours and how they had experienced the effectiveness of their analgesia (effective, too short acting or too weak, ineffective). Each patient was asked to award school grades between 1 and 6 (1=very good, 2=good, 3=satisfactory, etc), one grade each for medical staff, nursing staff, the hospital, and the quality of their pain management.
Statistical data analysis was done using SPSS version 14.0. For frequency distributions, the chi square test was used. Mean values of interval scaled variables were compared by using the t test and analysis of variance (significance level p<0.05). Multiple comparisons were not adjusted for because the evaluation aimed to describe the situation and generate hypotheses, not to confirm anything.
Structural characteristics
Stepwise pain management plans in writing were available in 7 of 25 hospitals. All had been set out by anesthesia departments and related almost exclusively to catheter procedures or patient controlled analgesia (PCA). Only one hospital had written agreements between doctors and nurses for general pain management. And again, only one hospital collected data on pain intensity in general wards—that is, outside specialized settings for the purpose of monitoring patients (for example, the recovery room) and independently of the documentation kept by acute pain services.
In 14 of the 25 hospitals in the study (56%), an acute pain service was available that met the published minimum criteria for such a service (8, 6). PCA pumps were used by default in 10 hospitals and in 7 occasionally.
Results of the survey
The Table shows demographic data from the 3251 patients (999 non-surgical, 2252 surgical) who had experienced pain or had remained pain free thanks to pain management. While the distribution by sex showed equal proportions, non-surgical wards included almost twice the number of elderly patients than surgical wards. On surgical wards, patients were less often affected by underlying malignancies (15% versus 21%) and fewer patients had poor general health (according to the study assistants) (Table). Most tumor patients with pain in the non-surgical wards had lung cancers or intestinal malignancies, 8% had lymphomas. Of the remaining non-surgical patients, 25% had cardiovascular disorders and 15% neurological disorders. 15% of surgical patients in the study had undergone surgery for malignant tumors, and of these, 40% had been operated on for bladder and prostate cancers. The remaining procedures had been operations for joint and bone injuries or disorders, followed by intestinal or gynecological operations.
By using an 11-part numerical rating scale (NRS 0–10), we collected scores for current pain in a resting position, pain on movement, and maximum pain within the preceding 24 hours. Further questions related to:
Situations that triggered pain
Difference in pain at different times of day
The effectiveness of the analgesia
Frequency with which patients reported pain.
The work done by doctors and nursing staff, hospital inpatient care, and the quality of pain therapy were scored by the patients using school grades between 1 and 6 (1=very good, 2=good, 3=satisfactory, 4=sufficient, 5=deficient, 6=unacceptable).
As is customary in an international setting, pain was classified into severe (NRS >6), moderate (NRS >3), and mild (2, 13, 15). To gain a measure about the degree of pain that might be acceptable, we used the school grades for pain therapy. Mean values were calculated for pain at rest, pain on movement, and maximum pain in the two groups of patients that had awarded school mark 2 for pain therapy. This pain was used as the threshold value for what constitutes a tolerable degree of pain (figure 1). That is, a patient’s pain was classified as “unacceptable” if the intensity exceeded the threshold value for a minimum of one of the types of pain in the survey (resting pain, pain on movement, and maximum pain).
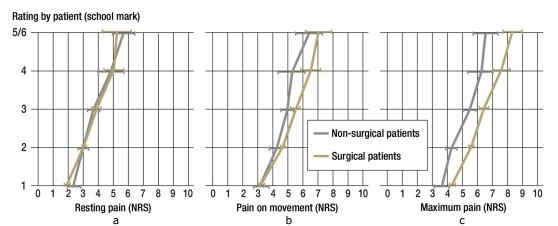
Figure 1.
Mean values (±standard error of mean, SEM) for a) resting pain, b) pain on initial activity/exertion, and c) maximum pain, subdivided into groups of patients who rated their pain therapy differently (school marks 1–6; marks 5 and 6 are combined because the number of cases is too small). NRS, numerical rating scale (NRS 0–10)
Results
The structural characteristics of the participating hospitals are shown in the eBox. 2898 patients received the questionnaire for surgically treated patients and 2778 patients received the questionnaire for non-surgical patients (5676 patients in total; for the original questionnaires please see eQuestionnaires). The response rate for surgical patients was 84.6% and for non-surgical patients, 61.4%. The most common reason for non-participation was poor general health (dyspnea, weakness, or severe fatigue); in very few cases the reason was lacking consent. Of the 4157 returned questionnaires, 86 (2.1%) were not evaluated because of lacking information about the intensity of pain. Lacking information for secondary items (listed in the Table and eTable) did not result in exclusion.
Table. Demographic data and main diagnoses for non-surgical patients and surgical patients with or without malignancy.
| Non-surgical | Surgical | P value (non-surgical vs surgical) | ||||||
| With malignancy | Without malignancy | Total | With malignancy | Without malignancy | Total | |||
| Sample | 213 (21.3%) | 786 (78.7%) | 999 | 344 (15.3%) | 1908 (84.7%) | 2 252 | ||
| Sex | Male | 112 (55.2%) | 383 (51.8%) | 495 (52.5%) | 194 (56.6%) | 903 (50.6%) | 1097 (51.6%) | 0.628 |
| Female | 91 (44.8%) | 356 (48.2%) | 447 (47.5%) | 149 (43.4%) | 880 (49.4%) | 1029 (48.4%) | ||
| N/A | 10 | 47 | 57 | 1 | 125 | 126 | ||
| Age (years) | <40 | 8 (4.0%) | 69 (9.4%) | 77 (8.2%) | 18 (5.3%) | 386 (21.7%) | 404 (19.0%) | <0.001 |
| 40–70 | 111 (55.0%) | 384 (52.5%) | 495 (53.0%) | 229 (67.0%) | 1047 (58.8%) | 1276 (60.1%) | ||
| >70 | 83 (41.1%) | 279 (38.1%) | 362 (38.8%) | 95 (27.8%) | 349 (19.6%) | 444 (20.9%) | ||
| N/A | 11 | 54 | 65 | 2 | 126 | 128 | ||
| General health | Good | 99 (50.0%) | 516 (72.5%) | 615 (67.6%) | 266 (82.1%) | 1401 (82.4%) | 1667 (82.3%) | <0.001 |
| Reduced/poor | 99 (50.0%) | 196 (27.5%) | 295 (32.4%) | 58 (17.9%) | 300 (17.6%) | 358 (17.7%) | ||
| N/A | 15 | 74 | 89 | 20 | 207 | 227 | ||
| Main diagnosis | Eye pathology | – | – | – | 1 (0.3%) | 34 (1.8%) | 35 (1.6%) | |
| Endocrine disorder | 1 (0.5%) | 26 (3.3%) | 27 (2.7%) | 2 (0.6%) | 68 (3.6%) | 70 (3.1%) | ||
| Back/spinal disorder | 4 (1.9%) | 59 (7.5%) | 63 (6.3%) | 3 (0.9%) | 49 (2.6%) | 52 (2.3%) | ||
| Disorder of skin, muscle tissue, connective tissue | 3 (1.4%) | 18 (2.3%) | 21 (2.1%) | 5 (1.5%) | 87 (4.6%) | 92 (4.1%) | ||
| Facial or neck pathology | 4 (1.9%) | 1 (0.1%) | 5 (0.5%) | 20 (5.8%) | 134 (7.0%) | 154 (6.8%) | ||
| Gastroenterological disorder | 53 (24.9%) | 117 (14.9%) | 170 (17.0%) | 47 (13.7%) | 327 (17.1%) | 374 (16.6%) | ||
| Gynecological disorder | 12 (5.6%) | – | 12 (1.2%) | 86 (25.0%) | 212 (11.1%) | 298 (13.2%) | ||
| Hematological or other internal disorder | 32 (15.0%) | 16 (2.0%) | 48 (4.8%) | 1 (0.3%) | – | 1 (0.04%) | ||
| Cardiovascular disorder | 14 (6.6%) | 232 (29.5%) | 246 (24.6%) | 2 (0.6%) | 105 (5.5%) | 107 (4.8%) | ||
| Disorder of bone or joint | 9 (4.2%) | 104 (13.2%) | 113 (11.3%) | 18 (5.2%) | 656 (34.4%) | 674 (29.9%) | ||
| Renal pathology | – | 14 (1.8%) | 14 (1.4%) | – | – | – | ||
| Neurological disorder | 5 (2.3%) | 114 (14.5%) | 119 (11.9%) | 2 (0.6%) | 10 (0.5%) | 12 (0.5%) | ||
| Mental disorder | 1 (0.5%) | 9 (1.1%) | 10 (1.0%) | – | – | – | ||
| Lung pathology | 67 (31.5%) | 68 (8.7%) | 135 (13.5%) | 26 (7.6%) | 6 (0.3%) | 32 (1.4%) | ||
| Urological disorder | 6 (2.8%) | – | 6 (0.6%) | 131 (38.1%) | 119 (6.2%) | 250 (11.1%) | ||
| Uncertain pathology* | 2 (0.9%) | 8 (1.0%) | 10 (1.0%) | – | 101 (5.3%) | 101 (4.5%) | ||
*Percentages relate to the respective number of questionnaires completed for this variable
eTable. Results of the patient survey on the intensity of pain, pain triggering conditions, and pain management in non-surgical and surgical patients with and without malignancy.
| Non-surgical | Surgical | P value (non-surgical vs surgical) | |||||||
| With malignancy | Without malignancy | P value | Total | With malignancy | Without malignancy | P value | Total | ||
| Evaluable responses | 213 (21.32%) | 786 (78.68%) | 999 | 344 (15.28%) | 1908 (84.72%) | 2252 | |||
| Intensity of pain | |||||||||
| Mean intensity of pain at rest (±SD) | 3.0 (3.0%) | 3.0 (2.8%) | 1 | 3.0 (2.9%) | 2.0 (2.2%) | 2.7 (2.4%) | <0.001 | 2.6 (2.4%) | <0.001 |
| Mean intensity of pain on movement (±SD) | 3.9 (3.4%) | 3.9 (3.3%) | 1 | 3.9 (3.3%) | 3.2 (3.1%) | 4.0 (3.0%) | <0.001 | 3.9 (3.1%) | 1 |
| Mean intensity of maximum pain (±SD) | 4.2 (3.5%) | 4.2 (3.3%) | 1 | 4.2 (3.3%) | 3.9 (3.2%) | 5.0 (3.2%) | <0.001 | 4.8 (3.2%) | <0.001 |
| Proportion of patients with | |||||||||
| Severe resting pain (>6) | 33 (15.49%) | 100 (12.72%) | 0.291 | 133 (13.31%) | 17 (4.94%) | 167 (8.75%) | <0.05 | 184 (8.17%) | <0.001 |
| Severe pain on movement (>6) | 54 (25.35%) | 194 (24.68%) | 0.841 | 248 (24.82%) | 56 (16.28%) | 455 (23.85%) | <0.01 | 511 (22.69%) | 0.185 |
| Severe maximum pain (>6) | 64 (30.05%) | 219 (27.86%) | 0.530 | 283 (28.33%) | 77 (22.38%) | 714 (37.42%) | <0.001 | 791 (35.12%) | <0.001 |
| Moderate resting pain (4–6) | 51 (23.9%) | 184 (23.4%) | 0.871 | 235 (23.5%) | 53 (15.4%) | 427 (22.4%) | <0.01 | 480 (21.3%) | 0.161 |
| Moderate pain on movement (4–6) | 52 (24.4%) | 204 (26.0%) | 0.648 | 256 (25.6%) | 84 (24.4%) | 539 (28.2%) | 0.144 | 623 (27.7%) | 0.227 |
| Moderate maximum pain (4–6) | 46 (21.6%) | 209 (26.6%) | 0.138 | 255 (25.5%) | 97 (28.2%) | 536 (28.1%) | 0.968 | 633 (28.1%) | 0.127 |
| Intensity of pain (qualitative) | |||||||||
|
41 (19.25%) | 126 (16.03%) | 0.4726 | 167 (16.72%) | 64 (18.60%) | 216 (11.32%) | <0.001 | 280 (12.43%) | <0.001 |
|
51 (23.94%) | 209 (26.59%) | 0 | 260 (26.03%) | 141 (40.99%) | 586 (30.71%) | 0 | 727 (32.28%) | 0 |
|
121 (56.81%) | 451 (57.38%) | 0 | 572 (57.26%) | 139 (40.41%) | 1 106 (57.97%) | 0 | 1245 (55.28%) | 0 |
| Intensity of pain and details of trigger and timing of pain | |||||||||
| Time of most severe pain (multiple responses) | |||||||||
| Evaluable responses | 184 | 699 | 883 | 291 | 1 721 | 2012 | |||
|
66 (35.87%) | 263 (37.63%) | 0.661 | 329 (37.26%) | 71 (24.40%) | 483 (28.07%) | 0.195 | 554 (27.53%) | <0.001 |
|
62 (33.70%) | 269 (38.48%) | 0.233 | 331 (37.49%) | 77 (26.46%) | 555 (32.25%) | <0.05 | 632 (31.41%) | <0.01 |
|
94 (51.09%) | 346 (49.50%) | 0.702 | 440 (49.83%) | 112 (38.49%) | 858 (49.85%) | <0.001 | 970 (48.21%) | 0.422 |
|
46 (25.00%) | 155 (22.17%) | 0.416 | 201 (22.76%) | 29 (9.97%) | 316 (18.36%) | <0.001 | 345 (17.15%) | <0.001 |
| Occurrence of very severe pain (most mentions) | |||||||||
| Evaluable responses | 184 | 699 | 883 | 291 | 1721 | 2012 | |||
|
80 (43.48%) | 301 (43.06%) | 0.919 | 381 (43.15%) | 99 (34.02%) | 689 (40.03%) | 0.052 | 788 (39.17%) | <0.05 |
|
51 (27.72%) | 126 (18.03%) | <0.01 | 177 (20.05%) | 105 (36.08%) | 589 (34.22%) | 0.537 | 694 (34.49%) | <0.001 |
|
16 (8.70%) | 44 (6.29%) | 0.250 | 60 (6.80%) | 32 (11.00%) | 248 (14.41%) | 0.120 | 280 (13.92%) | <0.001 |
| Pain management | |||||||||
| Evaluable responses | 199 | 711 | 910 | 336 | 1748 | 2084 | |||
| Received analgesia | 150 (75.38%) | 405 (56.96%) | <0.001 | 555 (60.99%) | 282 (83.93%) | 1492 (85.35%) | 0.501 | 1774 (85.12%) | <0.001 |
| Received no analgesia in spite of pain | 49 (24.62%) | 306 (43.04%) | 0 | 355 (39.01%) | 54 (16.07%) | 256 (14.65%) | 0 | 310 (14.88%) | 0 |
| Of which: patients with unacceptable pain*1 | |||||||||
| Evaluable responses | 111 | 399 | 510 | 138 | 1021 | 1159 | |||
| Received analgesia | 87 (78.38%) | 234 (58.65%) | <0.001 | 321 (62.94%) | 128 (92.75%) | 925 (90.60%) | 0.410 | 1053 (90.85%) | <0.001 |
| Received no analgesia | 24 (21.62%) | 165 (41.35%) | 0 | 189 (37.06%) | 10 (7.25%) | 96 (9.40%) | 0 | 106 (9.15%) | 0.000 |
| How patients rated the effectiveness of their analgesia | |||||||||
| Evaluable responses | 150 | 491 | 641 | 227 | 1379 | 1606 | |||
|
93 (62.00%) | 256 (52.14%) | 0.099 | 349 (54.45%) | 164 (72.25%) | 965 (69.98%) | 0.780 | 1129 (70.30%) | <0.001 |
|
41 (27.33%) | 163 (33.20%) | 0.000 | 204 (31.83%) | 53 (23.35%) | 351 (25.45%) | 0.000 | 404 (25.16%) | 0 |
|
16 (10.67%) | 72 (14.66%) | 0.000 | 88 (13.73%) | 10 (4.41%) | 63 (4.57%) | 0.000 | 73 (4.55%) | 0 |
| Patient’s request for analgesia | |||||||||
| Evaluable responses | 126 | 481 | 607 | 181 | 1187 | 1368 | |||
| Patients in pain requesting analgesic treatment | 100 (79.37%) | 266 (55.30%) | <0.001 | 366 (60.30%) | 134 (74.03%) | 757 (63.77%) | <0.01 | 891 (65.13%) | <0.05 |
| Patients not requesting analgesia in spite of pain | 26 (20.63%) | 215 (44.70%) | 0 | 241 (39.70%) | 47 (25.97%) | 430 (36.23%) | 0 | 477 (34.87%) | 0 |
| Waiting time after requesting analgesia | |||||||||
| Evaluable responses | 97 | 260 | 357 | 109 | 654 | 763 | |||
| Waiting time less than or equal to 30 minutes after request | 71 (73.20%) | 170 (65.38%) | 0.161 | 241 (67.51%) | 96 (88.07%) | 538 (82.26%) | 0.134 | 634 (83.09%) | <0.001 |
| Waiting time longer than 30 minutes after request | 26 (26.80%) | 90 (34.62%) | 0 | 116 (32.49%) | 13 (11.93%) | 116 (17.74%) | 0 | 129 (16.91%) | 0 |
| Poorly rated by patients (school grades worse than “good”) | |||||||||
| Evaluable responses | 156 | 512 | 668 | 242 | 1429 | 1671 | |||
|
58 (37.18%) | 210 (41.02%) | 0.392 | 268 (40.12%) | 48 (19.83%) | 363 (25.40%) | 0.063 | 411 (24.60%) | <0.001 |
| Evaluable responses | 205 | 760 | 965 | 339 | 1853 | 2192 | |||
|
18 (8.78%) | 107 (14.08%) | <0.05 | 125 (12.95%) | 20 (5.90%) | 153 (8.26%) | 0.139 | 173 (7.89%) | <0.001 |
| Evaluable responses | 204 | 765 | 969 | 342 | 1873 | 2215 | |||
|
21 (10.29%) | 89 (11.63%) | 0.5919 | 110 (11.35%) | 22 (6.43%) | 114 (6.09%) | 0.806 | 136 (6.14%) | <0.001 |
| Evaluable responses | 202 | 751 | 953 | 324 | 1828 | 2152 | |||
|
59 (29.21%) | 169 (22.50%) | <0.05 | 228 (23.92%) | 51 (15.74%) | 308 (16.85%) | 0.622 | 359 (16.68%) | <0.001 |
| Analgesia by steps of effectiveness | |||||||||
| Evaluable responses | 150 | 405 | 555 | 282 | 1492 | 1774 | |||
|
1 (0.7%) | 2 (0.5%) | 3 (0.5%) | 20 (7.1%) | 68 (4.6%) | 88 (5.0%) | |||
|
7 (4.7%) | 16 (4.0%) | 23 (4.1%) | 7 (2.5%) | 74 (5.0%) | 81 (4.6%) | |||
| Steps on WHO analgesic ladder*2 | |||||||||
|
41 (28.9%) | 273 (70.5%) | <0.001 | 314 (59.4%) | 103 (40.4%) | 694 (51.4%) | <0.001 | 797 (49.7%) | <0.001 |
|
23 (16.2%) | 59 (15.2%) | 82 (15.5%) | 47 (18.4%) | 260 (19.3%) | 307 (19.1%) | |||
|
78 (54.9%) | 55 (14.2%) | 133 (25.1%) | 105 (41.2%) | 396 (29.3%) | 501 (31.2%) | |||
SD = standard deviation from the mean;
*1 Pain is classed as acceptable or unacceptable on the basis of the threshold values based on school grades.
*2 Percentages relate to classifiable elements excluding regional anesthesia.
668 patients in the non-surgical wards (16% of returned questionnaires)—of these, 22.7% with and 77.3% without malignancies—completed the questionnaire according to the protocol after responding to only few questions, because they had not experienced any pain at any time during their inpatient stay and, according to their medical case files, had not received analgesia. Data from patients who were pain free without receiving analgesia were not included in this study of pain management (Table and eTable).
The demographic data of the remaining 3251 patients (999 non-surgical, 2252 surgical) who had experienced pain or were pain free under analgesia are listed in the Table (detailed data are in the eBox). In 112 surgical patients, the diagnosis could not be ascertained.
How patients rated their pain management
Significantly more surgical patients than non-surgical patients awarded school grades such as “good” or “very good” to the doctors, nursing staff, hospital, or pain therapy (eTable). The proportion of good grades was significantly higher for doctors and nursing staff—88% to 90% (p<0.0001)—than for pain therapy. Only 75% of surgical patients and 60% of non-surgical patients awarded high marks.
Resting pain in patients who had scored their pain therapy as “good” was rated at an average of NRS 3. In surgical patients with such a high rating, the mean tolerability level for pain on initial activity was NRS 4 and for maximum pain, NRS 5. The corresponding threshold values for non-surgical patients were NRS 4 for both pain on movement and maximum pain (figure 1).
Frequency and intensity of pain
The mean intensity of resting pain among non-surgical patients was significantly higher than in surgical patients, as was the proportion with very severe resting pain (etable). Pain on movement was comparable; maximum pain was higher in surgical patients. Patients with malignancies experienced less pain postoperatively than patients without tumors (etable). On the basis of the threshold levels for acceptable pain, 1817 (56%) of subjects—and of these 55% of all surgical patients and 58% of non-surgical patients—experienced unacceptable levels of pain—that is, at least one of the three values for resting pain, pain on movement, and maximum pain was above the defined threshold value. This was least often (<50%) the case for surgical patients with malignancies.
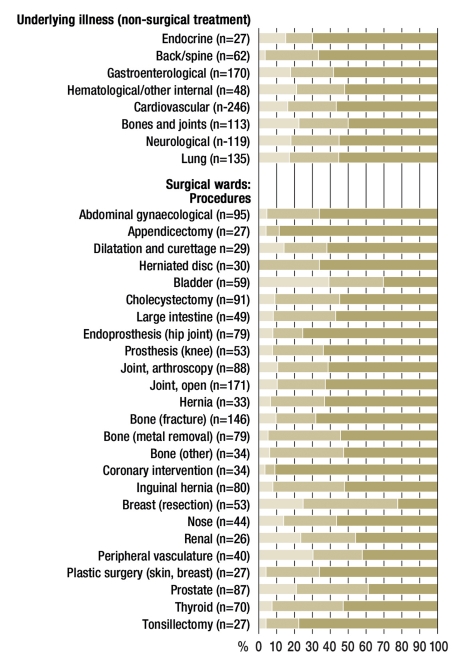
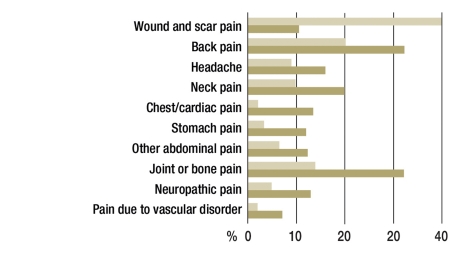
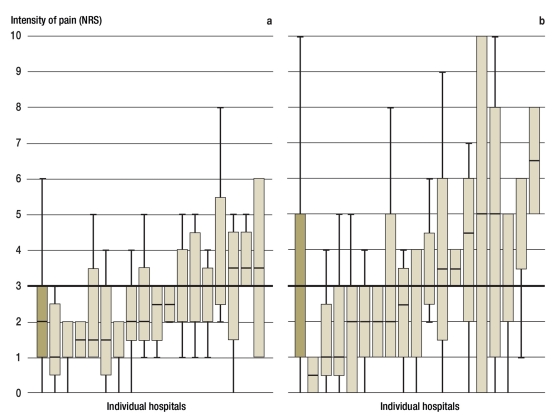
For some major operations—for example, surgery for urological malignancies on bladder or prostate, but also vascular surgery—the proportion of patients with unacceptable pain levels was lower than for operations with low degrees of tissue trauma—for example, appendicectomy, endoscopic cholecystectomy, or tonsillectomy (Figure 2, bottom). Within the different non-surgical departments the proportions of patients with unacceptable pain were comparable (Figure 2, top). These patients had different types of pain that were not necessarily associated with their diagnosis on admission; most self reported pain was arthritic pain or back pain (Figure 3). For all diagnostic groups, large differences existed between individual hospitals. Figure 4 shows this for the example of herniotomy and cardiac pain in patients with coronary heart disease.
Figure 2.
Proportion of pain-free patients receiving pain therapy (light olive shading), patients with acceptable (medium olive shading) and unacceptable (dark olive shading) pain scores; data about resting pain, pain on initial activity/exertion, and maximum pain combined, respectively; patients with pain: top: patients on wards delivering non-surgical treatment, classified by underlying pathology. Bottom: surgical patients after different procedures. The list includes disorders/operations only where n>25
Figure 3.
Frequency of severe pain (different types of pain) in surgical patients (light olive bar) and non-surgical patients (dark olive bar)
Figure 4.
Distribution of resting pain (box plot with 25%/75% quartiles and median) in different hospitals (dark olive box plot: mean value of all listed hospitals) in 80 patients after surgery for inguinal hernia (left, 17 hospitals) and 98 patients with cardiac pain due to coronary heart disease (right, 18 hospitals). NRS, numerical rating scale (NRS 0–10)
When prompted for the time when their pain was particularly severe, almost half of all patients reported nocturnal peaks. Even when multiple mentions were taken into account, 69% of non-surgical patients and 66% surgical patients reported maximum pain for times outside working hours. The main trigger for severe pain was getting out of bed and changing position. Some 15% of surgical patients and 7% of non-surgical patients named in this context medical measures such as lumbar puncture, endoscopic procedures, catheter insertion, and removal of drains (eTable).
Pain management
85% of surgical patients received painkilling drugs; this was significantly less often (57%) the case for non-surgical patients without malignancies (eTable). The subgroup of 1649 patients with unacceptable levels of pain showed comparable differences: 41% of non-surgical patients without malignancies received no analgesia at all in spite of highly intense pain. Of the patients with unacceptable tumor pain, 21% remained without analgesia, whereas less than 10% of surgical patients with unacceptable pain had to make do without analgesia (eTable).
70.3% of surgical patients categorized their analgesia as effective and less than 5% rated it as ineffective. Of non-surgical patients with or without malignancies, only half felt they had received effective treatment (eTable). Patients with malignancies called for assistance more often if they had pain; this was extremely rarely the case for patients without malignancies on non-surgical wards. With regard to the frequency of calls for assistance, notable differences existed between hospitals, with a range of 3.3% to 60%. Non-surgical patients often had to wait longer for a reaction from doctors or nursing staff than surgical patients, even if they had requested help (eTable).
At the time of the survey, 84 (5%) of patients received regional analgesia for pain relief. Pharmacotherapy with highly potent opioids was given more rarely in non-surgical wards than in surgical wards, and most often to patients with malignancies (eTable).
Discussion
This is the first study worldwide that investigated pain management in a larger cohort of surgical and non-surgical patients; the finding was that more than 80% of all hospital inpatients are still experiencing pain. Of the surgical and non-surgical patients, about one third complained of moderate to severe resting pain; more than 50% in each group reported pain of such intensity on initial activity after a period of inactivity. When combined, 56% of patients in the survey reported having experienced unacceptable pain.
In spite of all advances in these presumably positively pre-selected hospitals—participation was voluntary—the need for optimizing pain management could not be more obvious. This reflects the patients’ perception of the state of affairs: They awarded far poorer marks for their pain management than for the work done by doctors and nursing staff (eTable).
Another objective of this study was to define threshold values in Germany for an acceptable level of pain at rest, pain on movement, and maximum pain. The literature tends to classify these into mild, moderate, and severe (13, 15, 19). In order to conclude for a patient whether they are experiencing acceptable or unacceptable pain levels, details for all three types of pain are required. The following statements regarding acceptable pain thus reflect how many patients in a hospital mentioned a level for all forms of pain that is acceptable for the majority of patients thus affected (9, 20). The authors chose school grades as the measure to assess pain therapy; this was largely consistent with published data on pain tolerability (15, 19, 20, 22). Levels of pain that still incurred a decent school mark for pain therapy reached a mean value of NRS 3 for resting pain, NRS 4 for pain on movement, and NRS 5 for maximum pain. Comparable values applied to non-surgical patients; maximum pain occurred almost always on movement. This may explain the lack of a difference between pain on movement and maximum pain. In future, these pain scores can be used as empirically confirmed thresholds to assess the quality of pain therapy. They have been adopted as the basis of the certification of hospitals by medical societies, which has been running for a few years now (24).
Severe pain on movement and maximum pain after operations, which cause problems for surgical recovery (15), were reported by 23% and 35% of patients. This may come as a surprise in view of the fact that research into the subject now dates back several decades (1, 4, 7, 10, 12, 16, 18, e1, e4, e13, e14). The rate of patients with severe resting pain was notably lower than in earlier studies, which reported proportions of up to 36% (15, 17, 23, e6) but notably higher than in a simultaneous French study with a comparable proportion of severe pain on movement (13). For some procedures (Figure 2), the proportion of unacceptable pain is even higher than in older studies (15, e6). In our study cohort, this included patients who had surgical procedures that incurred a rather lower degree of tissue trauma—such as appendicectomies, endoscopic cholecystectomies, metal removal, or strumectomies (Figure 2).
A positive development is the fact that nowadays, patients with malignancies and patients after major surgery receive better pain management than in the past (15, 14, e18). One explanation is probably that after major surgery, many hospitals nowadays use highly effective procedures—such as analgesia administered through a peridural catheter. Further to high quality analgesia, a faster recovery is an additional advantage—for example, after “fast track surgery” (4, 5, 8, 14, e1– e4, e19). Such complex analgesic methods are, however, not indicated in most patients who undergo small and medium procedures. However, especially for these particularly common procedures, hardly any interdisciplinary agreements exist regarding pain management or treatment algorithms.
Pain management in wards for internal medicine, neurological wards, and orthopedic-rehabilitative wards is apparently even poorer (eTable). This study has shown for the first time that the majority of patients in such wards experience pain of different origin and at levels of moderate to high intensity.
The reported frequency of severe back pain or joint pain in our study is not surprising in view of its high incidence (25). Underprovision of pain care may be explained with the fact that many people experience pain that is not associated with the current diagnosis for which they are receiving treatment. But even angina pectoris, painful polyneuropathies, or abdominal syndromes (Figure 2)—lead symptoms of an underlying internal disorder—are often not treated to a sufficient degree. Patients register this as underprovision of pain management too. In patients without malignancies, medical professionals significantly more often react late to reported pain. Such patients receive insufficiently effective medication significantly more often than tumor patients and therefore report less often, despite the fact that they’re in pain (eTable). Although there are gaps in physicians’ knowledge in the literature (e20, e21), hospital doctors seem to be far more familiar with pain management for tumors than, for example, for neuropathic pain (e22, e23). The fact that patients with treatment resistant angina often do not receive adequate pain management has been common knowledge for decades, but seems to be the rule even now (e24, e25).
After the experiences in the surgical setting, the first crucial step in non-surgical departments would be to guarantee special treatment for patients with severe or treatment resistant pain by means of an acute pain service (4, 7, 10– 12, 16, 18, 19, e7, e10, e19). Further, even in non-surgical wards, more prophylactic measures should be delivered for the most common situations that trigger pain—such as mobilization, positioning at rest, and physical therapy.
By contrast, this study shows that in some hospitals, pain can be treated adequately in most surgical and non-surgical patients (Figure 4). Effective pain management in hospitals thus seems possible, especially since data relating to nausea and constipation (not shown here) imply that effective therapy is not synonymous with more serious adverse effects. Underprovision of pain management might therefore presumably be avoided if we successfully improved the knowledge and motivation of the professional groups involved in pain management, as well as streamlining organizational structures (1, 7, 11– 13, 17, 20, 23). Including nursing staff in any such measures, setting up acute pain clinics, and devising benchmark projects may well be the decisive steps (1, 7, 9, 12, 18, 19, e1, e8, e12, e26).
Patients do not expect the total absence of pain but adequate pain relief, rapid help when required, and administration of effective medication. This expectation on patients’ part should be met on a population-wide level.
Key Messages.
Surgical pain in the first 24 hours after surgery and on initial activity is still too severe in many patients.
Even patients who have had surgery resulting in very little tissue trauma often have severe pain.
On non-surgical wards, the proportion of patients with moderate to severe pain—for example, back pain, joint pain, or neurological pain—is no smaller than on surgical wards.
Pain management for tumor patients receiving non-surgical treatment is better than that for patients with non-malignant diagnoses. This is obvious from shorter waiting times after pain has been reported, and better efficacy of medications.
The positive example set by individual hospitals has shown that effective pain therapy is possible in both surgical and non-surgical settings.
Acknowledgments
The authors thank the remaining members of the working group Pain-Free Hospital: Dr Susanne Stehr-Zirngibl (Wuppertal-Bochum), Dr Doris Kindler (Bochum), Susanne Herzog (Datteln), Jutta Klostermann (Bochum), Andre Ewers (Salzburg), Dr Elena Clemens (Bonn), Professor Eberhard Klaschik (Bonn). They also thank the patients and coordinating doctors and nursing staff, the nursing sector, and doctors and nursing staff, without whose commitment and courage to expose the status quo a study of this kind would not have been feasible. The participating hospitals and coordinators were: Professor Dr E Pogatzki-Zahn, A Rausch: University Medical Center Münster; Dr Reimund Stögbauer, S Cassel: Stiftung Krankenhaus Bethanien Moers [Bethany Hospital Foundation for Moers]; Dr H P Hansen, T König: Malteser Krankenhaus St Franziskus-Hospital, Flensburg; C Zinecker, F Kaschowitz, Dr G Fischle: BG Trauma Clinic Tübingen; B Ide, Dr Michel: Hospital Martha-Maria Halle-Dölau; Dr M Czorny-Rütten, A Nazlier: St Marien-Hospital, Ahaus; Dr G Kroczek, C Schreiner: Medical Park Bad Rodach; Dr J Barthels, R. Knight: Medical Center Bad Salzungen gGmbH; Dr S Kljucar, C Grobe: DRK Hospitals Berlin-Westend; Dr T Klein, D Schütz: Böblingen District Hospital; Dr M-B. Berkel, D Schäfer: Medical Center Lippe-Detmold gGmbH; Dr T Jung, S Riegert: St Elisabeth Hospital Dorsten; Dr H Bauermeister, U Grimm, H Galeja: St Georg Medical Center gGmbH, Eisenach; Dr S Schulz, Dr U Ringeler, Simone Spangenberg: Krupp Hospital, Protestant Hospital Lutherhaus; PD Dr M Paul, A Adolphs: Gummersbach District Hospital GmbH; Dr R Ohme, H Rafler: BG Kliniken Bergmannstrost, Halle; C Zschuckelt, M Makowe: Asklepios Hospital Nord/Heidberg, Hamburg; Dr C Männle, J Klein-Schütz: Thorax Hospital Heidelberg gGmbH; Dr A Simpfendörfer, I Glockenstein: SLK Medical Center Heilbronn GmbH; Dr A Schmidt, F Montag: Krankenhaus der Barmherzigen Brüder [Hospital of the Merciful Brothers], Munich; Dr O Djuren, Dr C Schorer, N Hingst: Oldenburg Medical Center gGmbH; Professor Dr F K Pühringer, L Binder, M Weiß: Medical Center at Steinenberg Reutlingen; Dr S Geiger, I Gose: Medical Center Riesa-Großenhain gGmbH; Dr J Schulz-Wendler, C Fischer: Medical Center Salzgitter GmbH; Dr J Wiesler, C Wöretshofer: Medical Center Starnberg.
* The Pain-Free Hospital Project (Projekt Schmerzfreies Krankenhaus, SFK) has been conducted since 2003 by Ruhr University Bochum in collaboration with the Private University Witten/Herdecke. It is in receipt of sponsorship from Mundipharma GmbH. The patrons of the project are the German Society for the Study of Pain (DGSS) and the German Society for Interdisciplinary Medicine (MEDICA).
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
Professor Maier has received honoraria for speaking and advisory board membership from Gruenenthal, MSD, Köhler Chemie, Mundipharma, Pfizer, and Wyeth.
Ms Nestler has financial ties to Mundipharma, Pfizer, and Wyeth.
Mr Richter has received financial gifts from Mundipharma.
Professor Hardinghaus has received financial support from Mundipharma.
Professor Pogatzki-Zahn has received honoraria for speaking and advisory activities from Janssen-Cilag, Mundipharma, MSD, Bristol Meyer-Squibb, Köhler Chemie, Pfizer, and Wyeth Pharma.
Professor Zenz has received honoraria from Mundipharma, Janssen-Cilag, and Grunenthal.
Professor Osterbrink has received honoraria for collaborating with Mundipharma Limburg and Vienna.
References
- 1.Jage J, Tryba M, Neugebauer E, et al. Postoperative Schmerztherapie - eine interdisziplinäre Notwendigkeit. Dtsch Arztebl. 2005;102(6) [Google Scholar]
- 2.AWMF. S3-Leitlinie: Behandlung akuter perioperativer und post-traumatischer Schmerzen. www.uni-duesseldorf.de/AWMF/ll/041-001.htm [Google Scholar]
- 3.Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA, Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290:2455–2463. doi: 10.1001/jama.290.18.2455. [DOI] [PubMed] [Google Scholar]
- 4.Brodner G, Mertes N, Buerkle H, Marcus MA, Van Aken H. Acute pain management: analysis, implications and consequences after prospective experience with 6349 surgical patients. Eur J Anaesth. 2000;17:566–575. doi: 10.1046/j.1365-2346.2000.00738.x. [DOI] [PubMed] [Google Scholar]
- 5.de Leon-Casasola O, Lema MJ, Karabella D, Harrison P. Epidural analgesia versus intravenous patient-controlled analgesia: Differences in the postoperative course of cancer patients. Reg Anesth. 1994;19:307–315. [PubMed] [Google Scholar]
- 6.Walder B, Schafer M, Henzi I, Tramèr MR. Efficacy and safety of patient-controlled opioid analgesia for acute postoperative pain: A quantitative systematic review. Acta Anaesthesiol Scand. 2001;45:795–804. doi: 10.1034/j.1399-6576.2001.045007795.x. [DOI] [PubMed] [Google Scholar]
- 7.Maier C, Kibbel K, Mercker S, Wulf H. Postoperative Schmerztherapie auf Allgemeinen Krankenpflegestationen: Analyse der achtjährigen Tätigkeit eines Anästhesiologischen Akutschmerzdienstes. Anaesthesist. 1994;43:385–397. doi: 10.1007/s001010050071. [DOI] [PubMed] [Google Scholar]
- 8.Pöpping DM, Zahn PK, Van Aken HK, Dasch B, Boche R, Pogatzki-Zahn EM. Effectiveness and safety of postoperative pain management: a survey of 18 925 consecutive patients between 1998 and 2006 (2nd revision): a database analysis of prospectively raised data. Br J Anaesth. 2008;101:832–840. doi: 10.1093/bja/aen300. [DOI] [PubMed] [Google Scholar]
- 9.Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89:409–423. [PubMed] [Google Scholar]
- 10.Rawal N. 10 years of acute pain services—achievements and challenges. Reg Anesth Pain Med. 1999;24:68–73. doi: 10.1016/s1098-7339(99)90168-2. [DOI] [PubMed] [Google Scholar]
- 11.Stamer U, Mpasios N, Stüber F, Maier C. A survey of acute pain services in Germany and a discussion of international survey data. Reg Anesth Pain Med. 2002;27:125–131. doi: 10.1053/rapm.2002.29258. [DOI] [PubMed] [Google Scholar]
- 12.Deutsches Netzwerk zur Qualitätsentwicklung in der Pflege (ed.) Expertenstandard „ Schmerzmanagement in der Pflege bei akuten oder tumorbedingten chronischen Schmerzen“. Schriftenreihe des Deutschen Netzwerks zur Qualitätsentwicklung in der Pflege. Osnabrück. 2005 [Google Scholar]
- 13.Fletcher D, Fermanian C, Mardaye A, Aegerter P. Pain and Regional Anesthesia Committee of the French Anesthesia and Intensive Care Society (SFAR): A patient-based national survey on postoperative pain management in France reveals significant achievements and persistent challenges. Pain. 2008;137:441–451. doi: 10.1016/j.pain.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 14.Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North America. 2005;23:21–36. doi: 10.1016/j.atc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER. Patient experience of pain after elective noncardiac surgery. Anesth Analg. 1997;85:117–123. doi: 10.1097/00000539-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Neugebauer E, Sauerland S, Keck V, Simanski C, Witte J. Leitlinien Akutschmerztherapie und ihre Umsetzung in der Chirurgie: Eine deutschlandweite Klinikumfrage. Chirurg. 2003;74:235–238. doi: 10.1007/s00104-003-0615-9. [DOI] [PubMed] [Google Scholar]
- 17.Bruster S, Jarman B, Bosanquet N, Weston D, Erens R, Delbanco TL. National survey of hospital patients. BMJ. 1994;309:1542–1546. doi: 10.1136/bmj.309.6968.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meissner W, Ullrich K, Zwacka S. Benchmarking as a tool of continuous quality improvement in postoperative pain management. Eur J Anaesthesiol. 2006;23:142–148. doi: 10.1017/S026502150500205X. [DOI] [PubMed] [Google Scholar]
- 19.Harmer M, Davies KA, Lunn JN. A survey of acute pain services in the United Kingdom. BMJ. 1995;311(7001):360–361. doi: 10.1136/bmj.311.7001.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McQuay HJ, Poon Kh, Derry S, Moore RA. Acute pain: combination treatments and how we measure their efficacy. Br j Anaesth. 2008;101:69–76. doi: 10.1093/bja/aen108. [DOI] [PubMed] [Google Scholar]
- 21.Osterbrink J. Pain management in nursing care-experts standard. Fortschr Med. 2005;14 [PubMed] [Google Scholar]
- 22.Moore A, Mhuircheartaigh R, Straube S, Derry S, McQuay H. Defining the border between mild and moderate pain. Eur J Pain. 2009;13 [Google Scholar]
- 23.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–540. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 24.Certkom: www.certkom.com (last accessed: 22.02.2010) [Google Scholar]
- 25.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- e1.Schwenk W, Raue W, Haase O, Junghans T, Müller JM. „Fast-track“-Kolonchirurgie - erste Erfahrungen mit dem klinischen Verfahren der beschleunigten postoperativen Gesundung. Chirurg. 2004;75:508–514. doi: 10.1007/s00104-003-0785-5. [DOI] [PubMed] [Google Scholar]
- e2.Pennefather SH, Gilby S, Danecki A, Russell GN. The changing practice of thoracic epidural analgesia in the United Kingdom: 1997-2004. Anaesthesia. 2006;61:363–369. doi: 10.1111/j.1365-2044.2006.04549.x. [DOI] [PubMed] [Google Scholar]
- e3.Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362:1921–1928. doi: 10.1016/S0140-6736(03)14966-5. [DOI] [PubMed] [Google Scholar]
- e4.Neugebauer E, Sauerland S, Keck V, Simanski C, Witte J. Leitlinien Akutschmerztherapie und ihre Umsetzung in der Chirurgie. Eine deutschlandweite Klinikumfrage. Chirurg. 2003;74:235–238. doi: 10.1007/s00104-003-0615-9. [DOI] [PubMed] [Google Scholar]
- e5.Neugebauer E, Hempel K, Sauerland S, Lempa M, Koch G. Situation der perioperativen Schmerztherapie in Deutschland. Ergebnisse einer repräsentativen, anonymen Umfrage von 1 000 chirurgischen Kliniken. AG Schmerz. Chirurg. 1998;69:461–466. doi: 10.1007/s001040050439. [DOI] [PubMed] [Google Scholar]
- e6.Warfield CA, Kahn CH. Acute pain management. Programs in U.S. hospitals and experiences and attitudes among U.S. adults. Anesthesiology. 1995;83:1090–1094. doi: 10.1097/00000542-199511000-00023. [DOI] [PubMed] [Google Scholar]
- e7.Wulf H, Neugebauer E, Maier C. Empfehlungen einer interdisziplinären Expertenkommission. Stuttgart, New York: Georg Thieme Verlag; 1997. Die Behandlung akuter perioperativer und posttraumatischer Schmerzen. [Google Scholar]
- e8.Gould TH, Crosby DL, Harmer M, et al. Policy for controlling pain after surgery: effect of sequential changes in management. BMJ. 1992;305:1187–1193. doi: 10.1136/bmj.305.6863.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e9.Ready LB, Oden R, Chadwick HS, et al. Development of an anesthesiology-based postoperative pain management service. Anesthesiology. 1988;68:100–106. doi: 10.1097/00000542-198801000-00016. [DOI] [PubMed] [Google Scholar]
- e10.Werner MU, Soholm L, Rothboll-Nielsen P, Kehlet H. Does an acute pain service improve postoperative outcome? Anesth Analg. 2002;95:1361–1372. doi: 10.1097/00000539-200211000-00049. [DOI] [PubMed] [Google Scholar]
- e11.Troidl H, Angelini L, Klimek D, Finken U. Zur Situation der postoperativen Schmerzbehandlung aus operativer Sicht. [The status of postoperative pain treatment from the surgical viewpoint] Chirurg BDC. 1994;33:1–7. [PubMed] [Google Scholar]
- e12.American Society of Anesthesiologists. Practice guidelines for acute pain management in the perioperative setting. Anesthesiol. 2004;100:1573–1781. doi: 10.1097/00000542-200406000-00033. [DOI] [PubMed] [Google Scholar]
- e13.Australian and New Zealand College of Anaesthesists and Faculty of Pain Medicine. Acute pain management: scientific evidence. Second edition. Melbourne: ANZCA & FPM; 2005. [Google Scholar]
- e14.Benhamou D, Berti M, Brodner G, et al. Postoperative analgesic therapy observational survey (PATHOS): a practice pattern study in 7 central/southern European countries. Pain. 2008;136:134–141. doi: 10.1016/j.pain.2007.06.028. [DOI] [PubMed] [Google Scholar]
- e15.Stamer U, Mpasios N, Stüber F, Laubenthal H, Maier C. Postoperative Schmerztherapie in Deutschland. Ergebnisse einer Umfrage. Anaesthesist. 2002;51:248–257. doi: 10.1007/s00101-002-0288-7. [DOI] [PubMed] [Google Scholar]
- e16.Neugebauer E, Schulz K, Bouillon B, et al. Concept of a „Pain Free Clinic“ - from vision to reality. Periodicum Biologorum. 2007;109:231–233. [Google Scholar]
- e17.Meissner W, Mescha S, Rothaug J, et al. Quality improvement in postoperative pain management—results from the QUIPS Project [Qualitätsverbesserung der postoperativen Schmerztherapie -Ergebnisse des QUIPS-Projekts] Dtsch Arztebl Int. 2008;105(50):865–870. doi: 10.3238/arztebl.2008.0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e18.de Leon-Casasola OA, Parker BM, Lema MJ, et al. Epidural analgesia versus intravenbmous patient-controlled analgesia. Differences in the postoperative course of cancer patients. Reg Anesth. 1994;19:307–315. [PubMed] [Google Scholar]
- e19.Stadler M, Schlander M, Braeckman M, Nguyen T, Boogaerts JG. A cost-utility and cost-effectiveness analysis of an acute pain service. J Clin Anesth. 2004;161:59–67. doi: 10.1016/j.jclinane.2003.06.002. [DOI] [PubMed] [Google Scholar]
- e20.Grond S, Zech D, Dahlmann H, Schug SA, Stobbe B, Lehmann KA. Überweisungsgrund: „Therapieresistente“ Tumorschmerzen: Analyse der Schmerzmechanismen und der medikamentösen Vorbehandlung. Schmerz. 1990;4:193–200. doi: 10.1007/BF02527903. [DOI] [PubMed] [Google Scholar]
- e21.Breivik H, Cherny N, Collett B, et al. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009;20:1420–1433. doi: 10.1093/annonc/mdp001. [DOI] [PubMed] [Google Scholar]
- e22.Wasner G, Baron R, Birklein F, et al. Leitlinie Therapie neuro-pathischer Schmerzen. www.dgn.org. 2008 [Google Scholar]
- e23.Christo PJ, Mazloomdoost D. Cancer pain and analgesia. Ann N Y Acad Sci. 2008;1138:278–298. doi: 10.1196/annals.1414.033. [DOI] [PubMed] [Google Scholar]
- e24.DeJongste MJ, Tio RA, Foreman RD. Chronic therapeutically refractory angina. pectoris. Heart. 2004;90:225–230. doi: 10.1136/hrt.2003.025031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e25.Theres H, Eddicks S, Schenk M, Maier-Hauff K, Spies C, Baumann G. Neurostimulation zur Behandlung der refraktären Angina pectoris. Dtsch Arztebl. 2003;100(15):A 997–A 1003. [Google Scholar]
- e26.Rawal N. Acute pain services revisited—good from far, far from good? Reg Anesth Pain Med. 2002;27:117–121. doi: 10.1053/rapm.2002.29110. [DOI] [PubMed] [Google Scholar]