Abstract
Objective
The objectives of this study were twofold: to verify whether the type of metastasis (lymphatic vs. hematogenous) is a prognostic factor, and to identify molecular markers associated with survival in patients with disseminated cervical cancer.
Methods
Between April 1997 and May 2008, 30 patients with disseminated cervical cancer who had supraclavicular lymph node (N=13) or hematogenous metastases (N=17) were initially treated at our institute. We reviewed medical records to extract clinicopathologic variables. For 17 patients with available pathological specimens, we evaluated the association of immunohistochemical staining for metalloproteinase (MMP)-2, vascular endothelial growth factor (VEGF)-A, and laminin V gamma (LAMC)-2 with survival and clinicopathologic variables via a log-rank test and Cox regression analysis.
Results
Patients who had only lymphatic metastasis (odds ratio [OR], 5.3; 95% confidence interval [CI], 1.4 to 19.5) or completed initial treatment (OR, 3.2; 95% CI, 1.1 to 9.9) showed better survival than patients who did not, but none of the molecular markers were associated with survival. Out of 13 patients with only lymphatic metastasis, three patients who had received volume-directed radiation with concurrent chemotherapy had a long-term survival of over two years. However, patients with hematogenous metastasis showed extremely poor prognosis.
Conclusion
The type of metastasis and completion of initial treatment were associated with prolonged survival in patients with disseminated cervical cancer, and over 20% of patients with lymphatic metastasis were salvaged with volume-directed radiation with concurrent chemotherapy. None of the molecular markers were associated with survival in patients with disseminated cervical cancer.
Keywords: Uterine cervical neoplasm, Neoplasm metastasis, Lymphatic metastasis, Radiotherapy, Cancer chemotherapy
INTRODUCTION
Cervical cancer is one of the most common gynecological cancers. According to the GLOBOCAN 2002 database, the worldwide incidence of cervical cancer is 16.2/100,000, but that of uterine and ovarian cancer is 6.5/100,000 and 6.6/100,000, respectively.1 In contrast to localized cervical cancer, the cervical cancer with distant metastasis (disseminated cervical cancer) is known to have a poor prognosis.2,3 For example, the 5-year survival rate of patients with stage 4B cervical cancer is about 9%.2 Therefore, the goal of treatment for disseminated cervical cancer is not disease cure, but the prolongation of life with disease or palliation of symptoms. However, some patients with disseminated cervical cancer have long-term survival and the prognostic factors that predict this rare long-term survival are unclear.4,5
We theorized that the type of metastasis may be a prognostic factor in patients with disseminated cervical cancer. Thus, we hypothesized that patients with hematogenous metastasis had a worse prognosis than patients with only lymphatic metastasis, because of their aggressive behavior. Molecular markers associated with hematogenous metastasis may therefore be potential prognostic factors in patients with disseminated cervical cancer. In the literature, three markers are associated with hematogenous metastasis; metalloproteinase-2 (MMP-2), vascular endothelial growth factor-A (VEGF-A), and laminin V gamma-2 (LAMC-2). In breast cancer, MMP-2 and VEGF-A are differentially expressed in liver and lymph node (LN) metastasis.6,7 Similarly, LAMC-2 expression was associated with hematogenous metastasis in bladder cancer.8 Therefore, we examined whether the type of metastasis (lymphatic vs. hematogenous) and molecular markers were associated with survival in patients with disseminated cervical cancer.
MATERIALS AND METHODS
1. Patients
We abstracted the clinicopathologic data from the cancer registry database of our department. Patients with disseminated cervical cancer were defined as patients who had clinically evident or biopsy-proven supraclavicular lymph node (SCLN) or hematogenous metastatic lesions. Patients with recurrent tumors were excluded. Patients with SCLN or hematogenous metastatic lesions that the physician believed were 'clinically evident' were included in this study, even if the patients did not receive a lesion biopsy. Patients with only paraaortic or mediastinal LNs metastasis on imaging were excluded as they did not indicate disseminated cervical cancer. Clinicopathologic data included age, histology type, number of involved sites, type of metastasis, type of primary treatment, treatment completion, chronic complications, and duration of survival after treatment.
The institutional review board approved this study (K-1001-002-036) and permitted us to waive informed consent.
2. Variables
Pretreatment computed tomography (CT) or magnetic resonance imaging (MR) of the abdomen, pelvis, and chest area was performed in all patients. In addition, positron emission tomography (PET) or PET/CT was performed in 22 of 30 patients. The number of involved sites and the type of metastasis were determined by the imaging findings. Specifically, metastatic lesions detected by CT or MR were regarded as positive lesions. LNs whose shortest diameter was longer than 1 cm were regarded as positive. Interpretation of lesions in the other organs was at the attending radiologist's discretion. However, lesions detected by only PET or PET/CT but not by CT or MR were regarded as negative because PET or PET/CT has high false positive rates.9 SCLNs that were enlarged or had fluorodeoxyglucose (FDG) uptake in the imaging studies were biopsied. The number of involved sites was the number of involved organs, except that LNs were further classified into pelvic, para-aortic, mediastinal, and supraclavicular LNs. When the involved sites outside of the pelvic organs were all LNs, the type of metastasis was regarded as lymphatic; otherwise, the type of metastasis was designated as hematogenous.
3. Molecular markers
For 17 patients whose histological specimens were available, immunohistochemical staining for MMP-2, VEGF-A, and LAMC-2 were performed. MMP-2 (low vs. high) and VEGF-A (low, medium, or high) staining were graded qualitatively by a specialized pathologist who was blinded to the clinical data. LAMC-2 staining was graded as low if the percentage of stained cells was below 10%; otherwise, LAMC-2 was graded as high.
4. Analysis
The survival curves were plotted with the Kaplan-Meier method. The association of overall survival (OS) with clinicopathologic variables and the expression levels of MMP-2, VEGF-A, and LAMC-2 were tested via the log-rank test. With variables associated with OS in log-rank test, we performed multivariate analysis using the Cox proportional hazard model. All statistical analysis was performed with SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
1. Clinical characteristics of patients
Between April, 1997, and May, 2008, 30 patients with disseminated cervical cancer were initially treated at our institute. The median age was 51 years and the most common histologic type was squamous cell carcinoma. Excluding the uterine cervix itself, pelvic and para-aortic LNs were the most commonly involved sites. The body of the uterus, bladder, mediastinal LNs, SCLNs, inguinal LNs, bone, lung, pancreas, liver, omentum, adrenal gland, peritoneum, and psoas muscle were listed as other involved sites.
Primary treatment was volume-directed radiation with concurrent chemotherapy (VDRCC), chemotherapy alone, or radiation alone in 17, 6, and 7 patients, respectively. VDRCC was defined as radiation to areas where tumors were radiologically present with concurrent chemotherapy. The chemotherapy regimens in VDRCC were as follows: cisplatin 75 mg/m2 every three weeks in 10 patients, weekly cisplatin 40 mg/m2 in 3 patients, and 5-fluorouracil (FU) 1,000 mg/m2 for five days plus cisplatin 50 mg/m2 every three weeks in 4 patients. In patients who underwent VDRCC, the radiation field included the whole pelvis area and other areas where lesions were identified by imaging. Specifically, radiation was administered to para-aortic LNs, mediastinal LNs, SCLNs, bone, and liver in 13, 3, 12, 1, and 1 patient, respectively. For pelvic radiation, the four-field box technique was employed. In some patients, a boost radiation to point B was administered at the discretion of attending radiation oncologists. The cumulative radiation dose to point A was between 81 and 91 Gy in 11 patients with vaginal brachytherapy. Radiation to areas other than the pelvis was performed simultaneously with pelvic radiation. Cumulative doses to para-aortic LNs, mediastinal LNs, SCLNs, and bone were 50-70 Gy, 45-56 Gy, 59-72 Gy, and 20 Gy, respectively. A patient received radiation to a hepatic lesion through image-guided stereotactic body radiation therapy using the cyberknife. In patients who received chemotherapy alone, the regimens were: paclitaxel plus cisplatin in 3 patients, 5-FU plus cisplatin in 2 patients, and topotecan plus cisplatin in 1 patient. Among seven patients who received radiation alone, 4 patients received only pelvic radiation, and 3 patients underwent radiation to para-aortic LNs and SCLNs in addition to pelvic radiation. Radiation to para-aortic LNs and SCLNs were performed simultaneously with pelvic radiation and cumulative doses were similar in patients who received VDRCC.
In 13 patients with lymphatic metastasis, the primary treatment was VDRCC, chemotherapy alone, or radiation alone in 9, 2, and 2 patients, respectively. In 17 patients with hematogenous metastasis, VDRCC, chemotherapy alone and radiation alone were performed in 8, 4, and 5 patients, respectively.
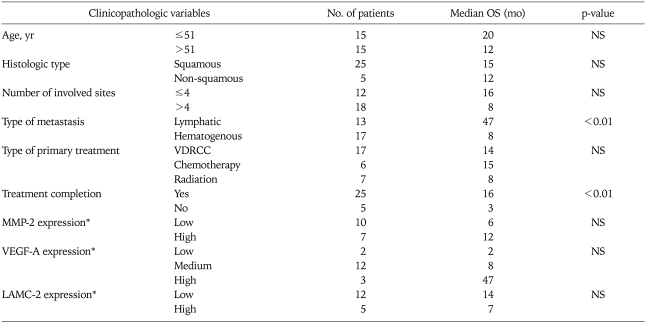
Among 30 patients, 5 could not finish the planned primary treatments and 4 patients experienced chronic complications of treatment. Namely, in the VDRCC group, one incomplete treatment, one esophageal stricture, and one rectovaginal fistula were observed. In the chemotherapy alone group, a subsequent radiation for persistent diseases after chemotherapy caused a rectovaginal fistula in a patient. In the radiation alone group, four incomplete treatment and one bowel obstruction from radiation colitis occurred (Table 1).
Table 1.
Clinicopathologic characteristics of patients with disseminated cervical cancer and its association with overall survival via univariate analysis
OS: overall survival, NS: not significant, VDRCC: volume-directed radiation with concurrent chemotherapy, MMP-2: metalloproteinase-2, VEGF-A: vascular endothelial growth factor-A, LAMC-2: laminin V gamma-2.
*MMP-2, VEGF-A, LAMC-2 expressions were evaluated in 17 patients.
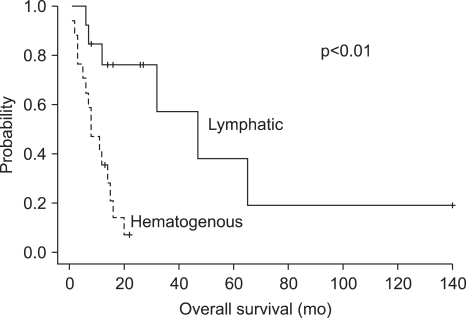
The median follow-up duration was 13 months (range, 1 to 140 months), and 21 deaths were observed. The median OS was 14 months and the 2-year OS rate was 36%. The 2-year OS rate of patients with hematogenous metastasis was 7%, but that of patients with lymphatic metastasis was 75%.
2. Expression of molecular markers
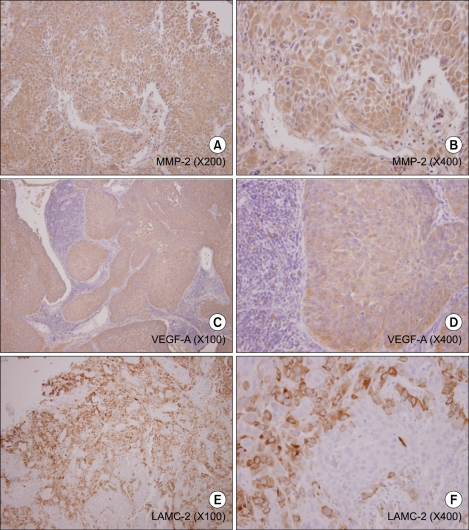
Immunohistochemical staining showed variable degrees of MMP-2, VEFG-A, LAMC-2 expressions (Fig. 1). The expression profiles of molecular markers are presented at Table 1.
Fig. 1.
High expressions of metalloproteinase-2 (MMP-2), vascular endothelial growth factor-A (VEGF-A), laminin V gamma-2 (LAMC-2) detected by immunohistochemical staining. (A-D) Immunohistochemical staining results of cervical punch biopsy specimens from a patient who had pelvic, para-aortic, inguinal and supraclavicular lymph node metastasis; (E and F) Immunohistochemical staining results of cervical punch biopsy specimens from another patient who had pelvic, para-aortic, and supraclavicular lymph node metastasis.
3. Association of clinicopathologic variables with OS
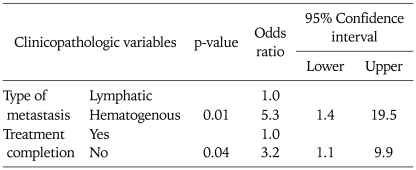
In univariate and multivariate analysis, the type of metastasis and treatment completion were associated with OS (Table 1, Fig. 2). Patients with hematogenous metastasis had a 5.3-fold higher risk of death than those with lymphatic metastasis, and patients who could not finish the planned primary treatment had a 3.2-fold higher risk of death than those who finished the primary treatment (Table 2). However, none of the molecular markers showed association with OS.
Fig. 2.
Overall survival curves according to type of metastasis.
Table 2.
Association of clinicopathologic variables with overall survival via multivariate analysis
4. Prognosis of patients with lymphatic vs. hematogenous metastasis
Nine of 13 patients with lymphatic metastasis underwent VDRCC. Four of nine patients who underwent VDRCC had no evidence of disease (NED) at six months after primary treatment. Furthermore, three of four patients with NED at six months were disease-free at two years after primary treatment. However, all patients with hematogenous metastasis had persistent lesions at six months after primary treatment.
DISCUSSION
Our results suggest that disseminated cervical cancer patients with only lymphatic metastasis showed a better prognosis than hematogenous metastasis. Specifically, 3 of 9 patients who had only lymphatic metastasis and underwent VDRCC were NED at two years after treatment. However, the prognosis of patients with hematogenous metastasis was extremely poor regardless of the treatment modalities. Our findings suggest that a more individualized and intrepid approach might be beneficial in disseminated cervical cancer patients with only lymphatic metastases. In other words, while VDRCC might be overtreatment for patients with hematogenous metastases, it may be adequate for patients with only lymphatic metastasis. Prospective clinical trial testing of the efficacy and toxicities of VDRCC for disseminated cervical cancer patients with only lymphatic metastasis is warranted.
Studies on patients with disseminated cervical cancer are extremely rare and generally report poor prognosis. For instance, a retrospective study reported that none of nine patients with biopsy-proven SCLN metastasis were alive at 14 months after diagnosis,10 and another study showed that the median OS of 14 patients was 7.5 months.11 However, in studies with a curative intent, tumor targeting chemoradiation was used and reported more favorable prognosis. Specifically, in a study including 33 patients with histologically confirmed SCLN metastasis, the 5-year survival rate was 16.5%.5 In addition, another study including 12 patients with SCLN metastasis reported a 24.7% 2-year OS rate.4 The survival rates of the latter two studies were similar to our study.
Metastasis type and treatment completion were both associated with prolonged survival. However, it is unclear whether treatment completion itself is a prognostic factor, because a good performance status may contribute to prolonged survival. We were unable to obtain reliable toxicity data from medical records, and could not compare the toxicity of VDRCC with other treatments. However, treatment completion rates and chronic complications rates were similar in the VDRCC group and other treatment groups, indicating that VDRCC is a feasible treatment option for patients with disseminated cervical cancer.
In patients with disseminated cervical cancer, the type of metastasis and treatment completion are potential prognostic factors for prolonged survival. VDRCC might be overtreatment for those with hematogenous metastases, but a promising approach for those who have only lymphatic metastases. A prospective trial evaluating the efficacy and toxicity of VDRCC in disseminated cervical cancer patients with only lymphatic metastasis is warranted.
ACKNOWLEDGEMENTS
We thank for our clinical research coordinator (Younha Kim) for data collection for this study.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.IARC Cancer Epidemiology Database [Internet] Lyon: International Agency for Research on Cancer; [cited 2009 May 27]. Available from: http://www-dep.iarc.fr/ [Google Scholar]
- 2.Quinn MA, Benedet JL, Odicino F, Maisonneuve P, Beller U, Creasman WT, et al. Carcinoma of the cervix uteri. FIGO 6th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006;95:S43–S103. doi: 10.1016/S0020-7292(06)60030-1. [DOI] [PubMed] [Google Scholar]
- 3.Aziz MF. Gynecological cancer in Indonesia. J Gynecol Oncol. 2009;20:8–10. doi: 10.3802/jgo.2009.20.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chao A, Ho KC, Wang CC, Cheng HH, Lin G, Yen TC, et al. Positron emission tomography in evaluating the feasibility of curative intent in cervical cancer patients with limited distant lymph node metastases. Gynecol Oncol. 2008;110:172–178. doi: 10.1016/j.ygyno.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Qiu JT, Ho KC, Lai CH, Yen TC, Huang YT, Chao A, et al. Supraclavicular lymph node metastases in cervical cancer. Eur J Gynaecol Oncol. 2007;28:33–38. [PubMed] [Google Scholar]
- 6.Van den Eynden GG, Van der Auwera I, Van Laere SJ, Trinh XB, Colpaert CG, van Dam P, et al. Comparison of molecular determinants of angiogenesis and lymphangiogenesis in lymph node metastases and in primary tumours of patients with breast cancer. J Pathol. 2007;213:56–64. doi: 10.1002/path.2211. [DOI] [PubMed] [Google Scholar]
- 7.Van den Eynden GG, Van Laere SJ, Van der Auwera I, Gilles L, Burn JL, Colpaert C, et al. Differential expression of hypoxia and (lymph)angiogenesis-related genes at different metastatic sites in breast cancer. Clin Exp Metastasis. 2007;24:13–23. doi: 10.1007/s10585-006-9049-3. [DOI] [PubMed] [Google Scholar]
- 8.Smith SC, Nicholson B, Nitz M, Frierson HF, Smolkin M, Hampton G, et al. Profiling bladder cancer organ site-specific metastasis identifies LAMC2 as a novel biomarker of hematogenous dissemination. Am J Pathol. 2009;174:371–379. doi: 10.2353/ajpath.2009.080538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang S, Kim SK, Chung DC, Seo SS, Kim JY, Nam BH, et al. Diagnostic value of (18)F-FDG PET for evaluation of paraaortic nodal metastasis in patients with cervical carcinoma: a metaanalysis. J Nucl Med. 2010;51:360–367. doi: 10.2967/jnumed.109.066217. [DOI] [PubMed] [Google Scholar]
- 10.Horowitz NS, Tamimi HK, Goff BA, Koh WJ, Schmidt RA, Greer BE, et al. Pretreatment scalene node biopsy in gynecologic malignancy: prudent or passe? Gynecol Oncol. 1999;75:238–241. doi: 10.1006/gyno.1999.5571. [DOI] [PubMed] [Google Scholar]
- 11.Tran BN, Grigsby PW, Dehdashti F, Herzog TJ, Siegel BA. Occult supraclavicular lymph node metastasis identified by FDG-PET in patients with carcinoma of the uterine cervix. Gynecol Oncol. 2003;90:572–576. doi: 10.1016/s0090-8258(03)00402-5. [DOI] [PubMed] [Google Scholar]