Abstract
A dental unit water line (DUWL) equipped with a device designed to automatically and continually flush a bacteriostatic solution of hydrogen peroxide (WHE) and a discontinuous disinfecting system (BIOSTER) was evaluated. In the first instance a preliminary sensitivity test on a large number of microorganisms (bacteria and fungi) was tried with a H2O2 range from 100 to 800 ppm. The bacteria frequently reported in DUWL (including Pseudomonas spp, Streptococcus spp., Staphylococcus spp., E. coli) and some periodontal pathogens showed a minimum inhibitory concentration from 100 to 300 H2O2 ppm (also including M. marinum and C. albicans). However, H2O2 did not show any inhibitory effects against: A. actinomycetemcomitans, C. glabrata C. parapsilos, F. nucleatum, M. micros. In a second step, the DUWL was experimentally infected with S. faecalis, E. coli, P. aeruginosa, S. aureus. After disinfection steps with 3% H2O2, the inhibitory effect on planktonic forms and on sessile biofilm was measured. In a third step, the count of 16S rRNA gene copies by real time PCR at different points of the DUWL described an accrue of bacterial slime in “hot spot” regions characterized by irregular/slow water flux (valves, elbows). However these results suggest that hydrogen peroxide is not only able to inhibit bursts of planktonic bacteria inside the DUWL, but that it could also be effective against sessile biofilm containing heterotrophic microorganisms derived from domestic water line contamination. In addition some oral pathogens could be contaminating and surviving in DUWL.
Keywords: Dental Unit Water Lines, Hydrogen Peroxide, Biofilm.
INTRODUCTION
Dental units are the core of dental clinics. The handpieces (air–water syringes, ultrasonic scalers, prophy-angles, turbines, micromotors) are connected to dental units by a network of small-bore plastic tubes through which water and air travel to activate or cool the instruments. Different authors have shown that this system is extensively colonized by microorganisms with at least 40 different species including: oral streptococci, Pseudomonas spp., Enterobacteria, Candida albicans, Legionella pneumophila and non–tuberculous Mycobacterium spp. [1-4]. Inside this waterline, chemical-physical conditions, such as: water flux, temperature, variations in tube surfaces and the chemical composition of the tubes, vary greatly in different parts of the DUWL; consequently the resident bacterial biofilm shows different qualitative/qualitative biological characteristics [5, 6]. These microbial biofilms comprise mainly a matrix of highly hydrated complex exopolysaccharides secreted by bacteria, housing micro-colonies and single cells, heterogeneously interspersed by channels or pores [7, 8].
Planktonic forms of microorganisms and pieces of biofilm are shed from here and seed biofilm-forming microorganisms elsewhere in the waterline network. The same microorganisms are then transferred directly into the mouths of patients during dental procedures.
The exopolymer matrix can restrict the diffusion of substances and bind antimicrobials. This provides effective resistance for cells enclosed in a biofilm against a large number of antimicrobial molecules [9]. In recent years manufacturers have responded to the evident need for changes in DUWL engineering and design to control DUWL biofilms [10]. Several strategies have been evolved to reduce bacterial colonization and growth, including the use of waterline flushing, independent water reservoir systems, distilled or pasteurized water, ultraviolet light, filtration and periodic or continuous chemical disinfection [11]. Among chemical disinfectants, hydrogen peroxide-based compounds play a central role in disinfection strategies of European leading dental unit manufacturers [12]. Hydrogen peroxide has been shown to possess a wide spectrum of antimicrobial activity, in that it is active against bacteria, yeasts, fungi, viruses and spores [13-15]; normally, these protocols make use of a 0.25-3% H2O2 concentration range. The efficacy of hydrogen peroxide depends on many factors, for example: concentration, pH, temperature, reaction time, use in combination with physical agents [16]; moreover it depends on bacterial/viral concentration, the microbial species under consideration and their biological phase (e.g. spore or vegetative status), the presence of organic substances, the nature of the surface to be treated (presence of pores, micro-cracks) and bacterial genetic proprieties [17].
The action of H2O2 on microbes is due to the presence of the hydroxyl radical (OH·) in the solution. The hydroxyl radical is said to be the strongest oxidant known; transition metals are believed to catalyze the formation of the hydroxyl radical. It can attack membrane lipids, DNA, and other essential cell components. Different mechanisms are described for biofilm inhibition by H2O2. Recent studies showed in Staphylococci a reduction (by H2O2) of icaADB cassette expression (involved in polysaccharide intercellular adhesion) [18]. Moreover, in Gram negative bacteria the production of internal H2O2 by AlpP-gene may play an important role in biofilm formation: some of the biofilm-forming cells are killed by internally produced H2O2, and this leads to differentiation, dispersal, and phenotypic variation among dispersal cells [19].
Based on previous experiments described in different publications [12, 20, 21], this work evaluates by a in vitro platform: (a) large numbers of microorganisms tested with different H2O2 concentrations, (b) a DUWL contamination model performed using a mix suspension of four microorganisms: Escherichia coli, Pseudomonas aeruginosa, Streptococcus faecalis, Staphylococcus aureus, (c) DUWL biofilm mass monitoring, using molecular and cultural methods.
MATERIALS AND METHODOLOGY
Strains Used in this Work
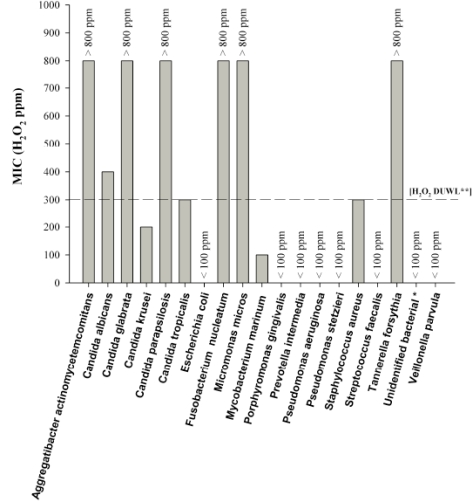
DUWL microflora have been described by other authors. It has been demonstrated that bacterial forms are the dominant part in these biofilms, while fungi and protozoa are less common. However, following the latest publications, we used the following species, Fig. (1).
Gram positive bacteria: Staphylococcus aureus ATCC 6538, Streptococcus (Enterococcus) faecalis ATCC 29212 [22, 23].
Gram negative bacteria: heterotrophic aerobic species are the most represented in DUWL. We used: Escherichia coli ATCC 7075, Pseudomonas aeruginosa ATCC 27853, Pseudomonas stutzeri, isolate OG7 and unidentified bacterial species, isolates: OG4-OG5 (these three strains were isolates from DUWL domestic water line and characterized by 16S rRNA sequence). We also evaluated a sensitivity test with Gram negative periodontal pathogens: Prevotella intermedia CCUG 2404 (Culture Collection, University of Göteborg, Sweden), Aggregatibacter actinomycetemcomitans, CCUG 37005, (genotype 652) Porphyromonas gingivalis CCUG 25893, Tannerella forsythensis cip 105220 (Institut Pasteur, Paris, France), Fusobacterium nucleatum DSMZ 19508, Parvimonas micra DSMZ 20468, Veillonella parvula DSMZ 2008 (Deutsche Sammlung von Mikroorganismen und Zellkulturen GmbH).
Fungi: Candida albicans has been associated with dental unit water systems [24]; in this work 5 different oral clinical isolates of Candida spp. (designed from OG11 to OG15) were tested with a H2O2 sensitivity test. These specimens were plated in Sabouraud glucose agar for 48 h at 35°C (Microbiol, Uta, Cagliari, Italy). The colonies were identified with an API ID32C system (Biomerieux, St Louis, MO) and maintained at –20°C in skimmed milk (Oxoid, Basingstoke, UK).
Mycobacteria: in accordance with the presence of non tuberculosis Mycobacterium spp in DUWL [25], a simulation model with Mycobacterium marinum was performed. Aerobic bacteria were cultured in Müller Hinton agar, (MH Microbiol, UTA, Cagliari Italy). Anaerobic bacteria were maintained at –80°C in vials containing Schaedler Broth with 15% glycerol and cultured in Columbia agar blood (Microbiol, UTA, Cagliari, Italy) at 37°C with 5% CO2 in jar (Biomérieux Marcy l’Etoile, France). M. marinum was cultured in tubes of Middlebrook 7H10 agar with OADC supplement (Microbiol, UTA, Cagliari, Italy) and stored at room temperature. Visible colonies were observed after 2-4 weeks of incubation. Nucleotide sequence accession numbers: the 16S rRNA gene sequences from Gram negative bacteria isolates OG4, OG5, OG6 have been deposited in GenBank under the following accession numbers: GU057341, GU057340, GU057339.
Fig. (1).
H2O2 susceptibility pattern of the most common microorganisms isolated in DUWLs.
* Corresponding to the 16S rRNA, sequence deposited in GenBank as accession n. GU 057339, GU 057340, GU 057341
** H2O2 concentration normally used in a continuous mode inside the DUWL, according to the manufacturer's instructions.
H2O2 in vitro Susceptibility Testing
Baseline MICs were determined in accordance with the Committee for Clinical Laboratory Standards [NCCLSNCCLS, http://http://www.clsi.org/] by using a broth dilution method.
H2O2 was diluted in tubes containing 5 ml of liquid medium with a concentration range from 100 to 800 ppm (Fig. 1). These tubes contained an inoculum titre of 106 CFU/ml for bacteria and 105 CFU ml for Candida spp.
Log 10 Bacterial Reduction (LR)
The LR value (logarithm of the bacterial reduction) was performed by using a DUWL disinfection system (simulator) comprising: a WHE system, approved by DVGW (Deutsche Vereinigung des Gas- und Wasserfaches) for the continuous addition of H2O2 at a final concentration of 300 ppm and a BIOSTER system for dental unit water line disinfection, which draws 3% H2O2 from a dedicated tank and leaves it to stand within the dental unit water lines for a time pre-set by the dental operator, within a chosen time range (not shorter than 5 minutes and not longer than 30 minutes; standard contact time 10 minutes), after which dental unit water lines are automatically flushed with water from the public water system. WHE (Water Hygienisation System) and BIOSTER are the commercial names of optional hygiene devices which may be optionally present on CEFLA Dentale dental units.
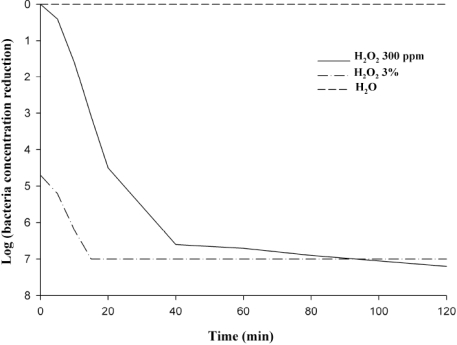
100 ml of Müller Hinton Broth was inoculated with a mix of the following bacterial species: P. aeruginosa, E. coli, S. aureus, S. faecalis until a final concentration of 108 CFU/ml for each bacterial species. Subsequently, H2O2 was added to the different tubes by the simulator with a concentration of 3%, when used for final disinfection, or at 300 ppm, when used in a continuous manner; 100 µl was plated in MH Agar every 20 minutes for 2 hours. The colonies on each plate were counted after incubation at 37° C for 48 hours. The result was expressed as the average number of colony forming units per ml of sample computed from the triplicate plates (Fig. 2).
Fig. (2).
Geometric mean of viable bacteria reduction Log, corresponding to bacterial suspension composed of: E. coli, P. aeruginosa, S.aureus and S. faecalis.
Biofilm Model Construction Inside the Complete DUWL
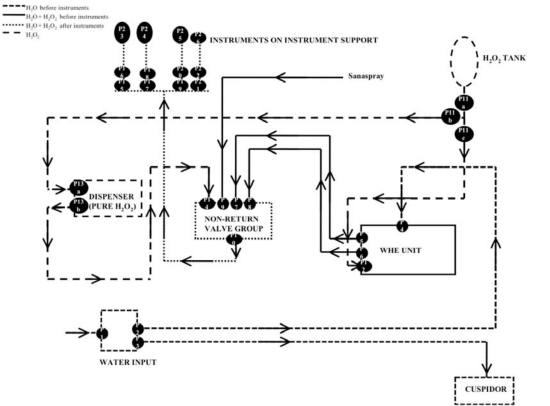
For our study we used a complete prototype of Stern 300 dental unit (CEFLA Dentale), provided with a BIOSTER system integrated into the hydro group and a WHE system with separate joint, Fig. (3).
Fig. (3).
Schematic representation of the DUWL used in this work, the black circles labelled from 1 to 26, correspond to specimen points.
A mix of the four species, previously described for LR, was used as the contaminant system.
The artificial biofilm was constructed as follows: (a) inoculation of ten liters of a suspension of 106 CFU/ml for each species in saline solution into the DUWL, (b) after four weeks, bacterial vitality was controlled by plating 1 cm2 of DUWL biofilm specimen in Müller Hinton agar (c) subsequently the DUWL tubes were reconditioned by threefold washing with a new sterile saline solution followed by a disinfection program with 3% H2O2 according to the DUWL manufacturer’s instructions.
1 ml of DUWL water post disinfection was plated in Müller Hinton agar for evaluation of bacterial vitality presence. Successfully we evaluated the possible presence of signs of bacterial biofilm; the biofilms were scraped at 26 different points from 1 sq. cm surfaces, by using a sterile swab scraper (Nunc, Wiesbaden, Germany). The swab was suspended in 1.5 ml of sterile saline solution: 1 ml was used for strain isolation by plating in Müller Hinton agar and 0.4 ml was used for DNA extraction [23]. Biofilm bacterial mass was measured by a real time PCR procedure.
Real Time PCR
As described in a previous publication [23], real time PCR were performed by using OG 33 (5’ – GACTACCAGGGTATCTAATC -3’) and OG 123 (5’-AGCAGCCGCGGTAATA -3’) primers, these oligos were designed by using a bacterial common (non variable) region of the 16S rRNA gene sequence, extracted from the NCBI database GenBank with accession number AY692453.
RESULT AND DISCUSSION
Microcolonies of proliferating micro-organisms forming a highly resistant biofilm [5, 26] on the inner surface of DUWL water lines are thought to be the source of bacterial contamination within the dental unit water supply. These biofilms are heterogeneous in species and morphology and are enveloped in a polysaccharide slime layer known as a glycocalyx. Numerous procedures have been suggested for overcoming the problem of the microbial contamination of dental unit water supplies [27]. The Centers for Disease Control (CDC) recommend that all water lines should, at the very least, be made to run and discharge water for several minutes at the beginning of each day and for a shorter interval between patient appointments [28].
One problem of protocols based on chemical agents for the control of biofilm is that they have to be bactericidal but not toxic to patients. The chemical treatment detaches biofilm and discourages its subsequent reformation, while protecting the dental unit’s internal components from corrosion. If the chemical agent is delivered continuously in treatment water, it is inexpensive and easy to use [11].
Among the micro-organisms capable of transmitting cross-infections, it is possible to find [10, 24, 25, 29] vegetative bacteria (S. aureus, P. aeruginosa, L. pneumophila, Mycobacterium spp. and others), fungi (Candida spp.), and viruses with abundant lipidic components (HIV; HCV; HBV etc.). In this work we evaluated the H2O2 activity following three different procedures.
(a). Large Numbers of Microorganisms Tested In Vitro with Different H2O2 Concentrations
We evaluated the effectiveness of a disinfection system based on the addition of H2O2 in continuous with [H2O2] at 300 ppm. In the first step a total of 19 different strains were tested by the H2O2 susceptibility test using [H2O2] from 100 to 800 ppm; the results are shown in Fig. (1), the tested microorganisms can be classified into 4 groups: (I) highly sensitive, MIC ≤100 ppm such as P. intermedia, P, gingivalis V. parvula, E. coli, Pseudomonas spp, S. faecalis; (II) sensitive, 100 MIC ≤300 ppm, S. aureus, M. marinum, C. Krusei and C. tropicalis, (III) resistant MIC >300 ppm, C. albicans, (IV) highly resistant, MIC >800 ppm, periodontal pathogens: A. actinomycetemcomitans F. nucleatum, P. micra, T. forsythia and two Candida spp., C. glabrata, C. parapsilosis. These results have confirmed and extended earlier works on H2O2 activity against different potential human pathogens described in the DUWL [12-17, 20, 21]. We observed that the majority of species contaminating DUWL through the domestic water line are H2O2 susceptible if evaluated in the planktonic status in vitro including P. aeruginosa and P. stutzeri (Fig. 1). However all tested strains showed a complete inhibition with [H2O2] at 3%.
(b). DUWL Simulator Contamination Model Performed Using a Mix Suspension of Four Microorganisms: Escherichia Coli, Pseudomonas aeruginosa, Streptococcus faecalis, Staphylococcus aureus
The kinetics of planktonic bacteria log reduction in the presence of H2O2 at 3% and 300 ppm as discontinuous or continuous disinfection respectively, were performed by using a mix of four of these highly sensitive species inoculated inside the DUWL disinfection system (simulator) (Fig. 2). These results suggest that a substantial inactivation of these microorganisms was observed with hydrogen peroxide, a mean of 5 log reduction was shown after 5 and 15 minutes with 3% and 300 ppm of H2O2 respectively. This suggests that an initial contamination of these planktonic forms could be quickly inactivated by this DUWL disinfection system.
On the contrary, evaluating the results showed in chapter (a), some Candida spp and some periodontal pathogens showed considerable H2O2 resistance [20, 30]. Our results suggest a possible risk for contamination and permanence of these microorganisms in DUWL handpieces if the final disinfection is inactive. They can be transferred through the DUWL from subjects with clinical or subclinical forms of candidosis (C. glabrata, C. parapsilosis) or periodontitis (i.e A. actinomycetemcomitans).
In this context strict control of the final parts of DUWL, i.e. handpieces, is crucial. All handpieces have to be mandatorily submitted to sterilization in a water vapor autoclave.
(c). DUWL Biofilm Mass Monitoring, Using Molecular and Cultural Methods
Later on the set of four aerobic bacteria was used for contamination and subsequent biofilm formation inside DUWL water lines. These species showed good H2O2 susceptibility if evaluated as planktonic forms (see Fig. 1), but, as reported by Szymańska et al. [2], and other authors, the possibility of the formation of a resistant biofilm from planktonic bacteria is very high, in particular for Pseudomonas spp [17, 31].
Our aim in this part of the experiment was to test H2O2 susceptibility in sessile biofilm. After the initial inoculum, the bacterial biofilm formed by the four species was let to stand in the dental unit for 4 weeks. First, after the four 4 weeks we checked the vitality of the biofilm present by cultural methods, and they showed a of CFU/cm2 range of 103-5*107 in 26 specimens (by a mean of 3 different countings). Second, a disinfecting step with BIOSTER (3% H2O2 with a contact time of 10 minutes) was performed. After the disinfecting cycle the evaluation of the living bacteria was performed. It was encouraging to note a mean of 99,9-100% inhibitory effect (E. coli 2 CFU/cm2, P. aeruginosa 0 CFU/cm, S. aureus 0 CFU/cm2, and S. faecalis 5 CFU/cm2), in comparison to the titre checked before the disinfecting cycle.
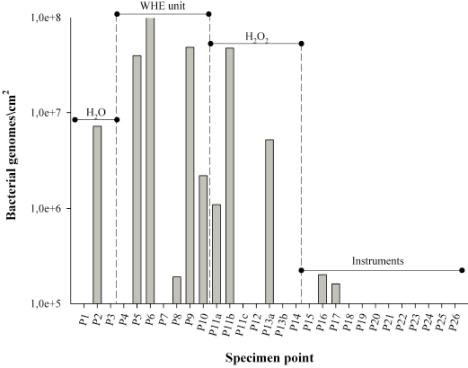
Moreover, we wanted to evaluate the entire bacterial population present (vital + inactivated bacteria). Therefore we performed an evaluation of the biofilm present (≥105 bacterial genomes/cm2, limit of detection of the method) by PCR real time at 26 different points in the DUWL after bacterial contamination and subsequent disinfection (Figs. 3 and 4). The greatest amount of critical biofilm mass (inactivated + vital) was reported in the WHE system, 5 out of 6 points. We suspect that the considerable presence of regulation valves/curves, which are able to determine a laminar irregular flow, are responsible for the biofilm formation. In laminar flow conditions, biofilm can flourish with minimal risk of being dislodged. This is one of the principal reasons why the flushing of waterlines can temporarily lower suspended planktonic microorganisms as recommended by the British Dental Association (BDA) and the CDC, although it is not usually effective in removing biofilms [28, 32].
Fig. (4).
Geometrical mean of representative biofilm mass, recognized after 4 weeks, inside the DUWL after contamination with four bacteria : E. coli, P. aeruginosa. S. faecalis and S.aureus, in the absence of any H2O2 treatment.
This result is particularly interesting because it shows how a biofilm tends to accumulate in points of the DUWL which are harder to be reached by H2O2 or which show a lower water flux.
CONCLUSION
This study has proven the utility of the hydrogen peroxide disinfection system in eradicating biofilm from dental unit waterlines and in controlling the bacterial count in water against several bacterial species. In addition, possible DUWL contamination with some Candida or anaerobic periodontal species in patients remains a central point of attention for prophylactic measures such as: autoclaving of handpieces, handpiece replacement between patients, flushing of the unit prior to use and anti-contamination devices to prevent retrograde aspiration of oral secretions into the water supply line.
ACKNOWLEDGEMENTS
This work was supported by Cefla Dentale SPA and by a grant from the Università degli studi di Cagliari “start-up giovani ricercatori”.
REFERENCES
- 1.Molinari JA. Dental unit water contamination. Compend Contin Educ Dent. 1999;20(4):358–362. [PubMed] [Google Scholar]
- 2.Szymanska J, Sitkowska J, Dutkiewicz J. Microbial contamination of dental unit waterlines. Ann Agric Environ Med. 2008;15(2):173–179. [PubMed] [Google Scholar]
- 3.Uzel A, Cogulu D, Oncag O. Microbiological evaluation and antibiotic susceptibility of dental unit water systems in general dental practice. Int J Dent Hyg. 2008;6(1):43–47. doi: 10.1111/j.1601-5037.2007.00269.x. [DOI] [PubMed] [Google Scholar]
- 4.Tippett BF, Edwards JL, Jenkinson HF. Bacterial contamination of dental unit water lines--a possible source of cross-infection. N Z Dent J. 1988;84(378):112–113. [PubMed] [Google Scholar]
- 5.Barbeau J, Gauthier C, Payment P. Biofilms, infectious agents, and dental unit waterlines: a review. Can J Microbiol. 1998;44(11):1019–1028. doi: 10.1139/cjm-44-11-1019. [DOI] [PubMed] [Google Scholar]
- 6.Szymanska J. Biofilm and dental unit waterlines. Ann Agric Environ Med. 2003;10(2):151–157. [PubMed] [Google Scholar]
- 7.Davey ME, O'Toole G A. Microbial biofilms: from ecology to molecular genetics. Microbiol Mol Biol Rev. 2000;64(4):847–867. doi: 10.1128/mmbr.64.4.847-867.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watnick P, Kolter R. Biofilm, city of microbes. J Bacteriol. 2000;182(10):2675–2679. doi: 10.1128/jb.182.10.2675-2679.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shigeta M, Tanaka G, Komatsuzawa H, Sugai M, Suginaka H, Usui T. Permeation of antimicrobial agents through Pseudomonas aeruginosa biofilms: a simple method. Chemotherapy. 1997;43(5):340–345. doi: 10.1159/000239587. [DOI] [PubMed] [Google Scholar]
- 10.Coleman DC, O'Donnell MJ, Shore AC, Russell RJ. Biofilm problems in dental unit water systems and its practical control. J Appl Microbiol. 2009;106(5):1424–1437. doi: 10.1111/j.1365-2672.2008.04100.x. [DOI] [PubMed] [Google Scholar]
- 11.Ozcan M, Kulak Y, Kazazoglu E. The effect of disinfectant agents in eliminating the contamination of dental unit water. J Oral Rehabil. 2003;30(3):290–294. doi: 10.1046/j.1365-2842.2003.01067.x. [DOI] [PubMed] [Google Scholar]
- 12.Linger JB, Molinari JA, Forbes WC, Farthing CF, Winget WJ. Evaluation of a hydrogen peroxide disinfectant for dental unit waterlines. J Am Dent Assoc. 2001;132(9):1287–91. doi: 10.14219/jada.archive.2001.0374. [DOI] [PubMed] [Google Scholar]
- 13.Brudzynski K. Effect of hydrogen peroxide on antibacterial activities of Canadian honeys. Can J Microbiol. 2006;52(12):1228–37. doi: 10.1139/w06-086. [DOI] [PubMed] [Google Scholar]
- 14.Glockmann E, Wiesner J, Oehring H, Glockmann I. Antibacterial efficiency and toxicity of hydrogen peroxide and other antiseptics. Dtsch Stomatol. 1990;40(11):462–3. [PubMed] [Google Scholar]
- 15.Tschernjawskaja MA, Belowa AS. Antibacterial mechanism of action of hydrogen peroxide preparations. Z Gesamte Hyg. 1990;36(2):86–8. [PubMed] [Google Scholar]
- 16.Feuerstein O, Moreinos D, Steinberg D. Synergic antibacterial effect between visible light and hydrogen peroxide on Streptococcus mutans. J Antimicrob Chemother. 2006;57(5):872–6. doi: 10.1093/jac/dkl070. [DOI] [PubMed] [Google Scholar]
- 17.Choi YS, Shin DH, Chung IY, Kim SH, Heo YJ, Cho YH. Identification of Pseudomonas aeruginosa genes crucial for hydrogen peroxide resistance. J Microbiol Biotechnol. 2007;17(8):1344–52. [PubMed] [Google Scholar]
- 18.Glynn AA, O'Donnell ST, Molony DC, Sheehan E, McCormack DJ, O'Gara JP. Hydrogen peroxide induced repression of icaADBC transcription and biofilm development in Staphylococcus epidermidis. J Orthop Res. 2009;27(5):627–30. doi: 10.1002/jor.20758. [DOI] [PubMed] [Google Scholar]
- 19.Mai-Prochnow A, Lucas-Elio P, Egan S, et al. Hydrogen peroxide linked to lysine oxidase activity facilitates biofilm differentiation and dispersal in several gram-negative bacteria. J Bacteriol. 2008;190(15):5493–501. doi: 10.1128/JB.00549-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Szymanska J. Antifungal efficacy of hydrogen peroxide in dental unit waterline disinfection. Ann Agric Environ Med. 2006;13(2):313–7. [PubMed] [Google Scholar]
- 21.Zanetti F, De Luca G, Tarlazzi P, Stampi S. Decontamination of dental unit water systems with hydrogen peroxide. Lett Appl Microbiol. 2003;37(3):201–6. doi: 10.1046/j.1472-765x.2003.01378.x. [DOI] [PubMed] [Google Scholar]
- 22.Wirthlin MR, Marshall GW Jr, Rowland RW. Formation and decontamination of biofilms in dental unit waterlines. J Periodontol. 2003;74(11):1595–609. doi: 10.1902/jop.2003.74.11.1595. [DOI] [PubMed] [Google Scholar]
- 23.Denotti G, Piga R, Montaldo C, et al. In Vitro Evaluation of Enterococcus faecalis Adhesion on Various Endodontic Medicaments. Open Dent J. 2009;3(3):120–4. doi: 10.2174/1874210600903010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walker JT, Bradshaw DJ, Finney M, et al. Microbiological evaluation of dental unit water systems in general dental practice in Europe. Eur J Oral Sci. 2004;112(5):412–8. doi: 10.1111/j.1600-0722.2004.00151.x. [DOI] [PubMed] [Google Scholar]
- 25.Porteous NB, Redding SW, Jorgensen JH. Isolation of non-tuberculosis mycobacteria in treated dental unit waterlines. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(1):40–44. doi: 10.1016/j.tripleo.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Porteous NB, Partida MN. The effect of frequent clinical use of dental unit waterlines on contamination. N Y State Dent J. 2009;75(3):20–4. [PubMed] [Google Scholar]
- 27.Ching B. Dental unit water line maintenance. Hawaii Dent J. 2005;36(3) [PubMed] [Google Scholar]
- 28.waqqas s. Recommended infection-control practices for dentistry, 1993. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1993;42(RR-8):1–12. [PubMed] [Google Scholar]
- 29.Szymanska J. Microbiological risk factors in dentistry. Current status of knowledge. Ann Agric Environ Med. 2005;12(2):157–63. [PubMed] [Google Scholar]
- 30.Montebugnoli L, Sambri V, Cavrini F, Marangoni A, Testarelli L, Dolci G. Detection of DNA from periodontal pathogenic bacteria in biofilm obtained from waterlines in dental units. New Microbiol. 2004;27(4):391–7. [PubMed] [Google Scholar]
- 31.Al-Hiyasat AS, Ma'ayeh SY, Hindiyeh MY, Khader YS. The presence of Pseudomonas aeruginosa in the dental unit waterline systems of teaching clinics. Int J Dent Hyg. 2007;5(1):36–44. doi: 10.1111/j.1601-5037.2007.00221.x. [DOI] [PubMed] [Google Scholar]
- 32.Mills SE. The dental unit waterline controversy: defusing the myths, defining the solutions. J Am Dent Assoc. 2000;131(10):1427–41. doi: 10.14219/jada.archive.2000.0054. [DOI] [PubMed] [Google Scholar]