Abstract
Background
The mood disorders are prevalent and problematic. We review randomized controlled psychotherapy trials to find those that are empirically supported with respect to acute symptom reduction and the prevention of subsequent relapse and recurrence.
Methods
We searched the PsycINFO and PubMed databases and the reference sections of chapters and journal articles to identify appropriate articles.
Results
One hundred twenty-five studies were found evaluating treatment efficacy for the various mood disorders. With respect to the treatment of major depressive disorder (MDD), interpersonal psychotherapy (IPT), cognitive behavior therapy (CBT), and behavior therapy (BT) are efficacious and specific and brief dynamic therapy (BDT) and emotion-focused therapy (EFT) are possibly efficacious. CBT is efficacious and specific, mindfulness-based cognitive therapy (MBCT) efficacious, and BDT and EFT possibly efficacious in the prevention of relapse/recurrence following treatment termination and IPT and CBT are each possibly efficacious in the prevention of relapse/recurrence if continued or maintained. IPT is possibly efficacious in the treatment of dysthymic disorder. With respect to bipolar disorder, CBT and family-focused therapy (FFT) are efficacious and interpersonal social rhythm therapy (IPSRT) possibly efficacious as adjuncts to medication in the treatment of depression. Psycho-education (PE) is efficacious in the prevention of mania/hypomania (and possibly depression) and FFT is efficacious and IPSRT and CBT possibly efficacious in preventing bipolar episodes.
Conclusions
The newer psychological interventions are as efficacious as and more enduring than medications in the treatment of MDD and may enhance the efficacy of medications in the treatment of bipolar disorder.
Keywords: Randomized controlled trials, major depression, dysthymia, bipolar disorder, qualitative review
INTRODUCTION
The mood disorders are characterized by episodes of depression or mania and are among the most prevalent of the psychiatric disorders.[1] Major depressive disorder (MDD) and the less severe but more chronic dysthymic disorder (DD) involve depression only, whereas bipolar disorder (BD) requires episodes of mania or hypomania.[2] The mood disorders account for the vast majority of suicides and are a leading cause of disability.[3]
Both psychotherapy and medications are widely used in the treatment of the mood disorders.[4] Historically, the primary focus of treatment development was on symptom reduction, but there has been a growing recognition of the need to develop strategies that prevent subsequent relapse and recurrence.[5] Medication treatment has long been considered the standard of treatment for more severe depression and bipolar disorder and has gained market share relative to psychotherapy in recent years with the advent of less problematic medications.[6] Nonetheless, not everyone responds to medications and there is no evidence that drugs do anything to reduce risk for subsequent symptom return once their use is discontinued. Some patients respond to psychotherapy who are refractory to medications and it has long been claimed that psychotherapy has enduring effects that can reduce subsequent risk in ways that medications cannot.
In this article, we review studies of psychological therapies for the mood disorders in adults to determine which ones are empirically supported using the criteria defined by Chambless and Hollon.[7] According to these criteria, a therapy is considered efficacious and specific if there is evidence from at least two settings that it is superior to a pill or psychological placebo or another bona fide treatment. If there is evidence from two or more settings that the therapy is superior to no treatment it is considered efficacious. If there is support from one or more studies from just a single setting, the therapy is considered possibly efficacious pending replication. We further differentiate between the effects of treatment on the reduction of acute symptoms versus the prevention of subsequent relapse or recurrence and pay particular attention to comparisons to medications. Earlier reviews have applied these criteria and we update those reviews.[8,9]
This approach is similar to the one taken by the FDA in determining when a medication can be marketed in the United States. It puts a premium on well-formed studies in fully clinical populations that speak to the efficacy and specificity of a given intervention and requires direct comparisons to draw inferences regarding the relative efficacy of different interventions. As a consequence, it sometimes leads to different conclusions than are drawn from meta-analyses that tend to include all studies in a literature (regardless of quality) and that estimate differential effect sizes in the absence of direct comparisons between conditions. Meta-analytic reviews often find comparable effect sizes between different psychotherapies even when only some of those interventions would meet FDA criteria for efficacy and specificity.[10] In such instances, we are reluctant to declare a treatment efficacious (much less specific) if we cannot find a single well-formed study that supports that conclusion. To do so would be tantamount to accepting the null hypothesis and interpreting the absence of differences between treatments as evidence of comparable efficacy (or specificity). We highlight this distinction when it occurs in the following review.
Despite our preference for the FDA approach, we do think that meta-analyses have considerable value in highlighting the relative impact of different control conditions and other related factors. For example, Cuijpers and colleagues reported that comparisons between all psychotherapies aggregated versus no treatment controls generated an effect size of d = .88 across the depression literature.[11] This can be translated into a number-needed-to-treat (NNT) of 2.15 and means that one additional patient gets better for just over every two patients treated relative to what would have happened in the absence of treatment. Such comparisons are sufficient to establish efficacy. Non-specific controls (including especially pill-placebos) more than halved the effect size (d = .35), which translates into a considerably larger NNT of 5.15. This means that over twice as many patients would need to be treated to produce one additional positive outcome relative to comparison conditions that mobilize nonspecific factors associated with going into treatment. This is still quite respectable; by way of contrast, antihypertensive medications produce an NNT of 15. Such comparisons are necessary to establish specificity. In brief, it is easier to show that something works than it is to establish that it works for specific reasons that go beyond the mere provision of treatment. Curiously, comparisons to “treatment-as-usual” were associated with an intermediate effect size of d = .52 with a corresponding NNT of 3.50. This likely reflects the fact that what passes as “treatment-as-usual” can be quite heterogeneous across studies (and even across patients within studies), ranging from minimal contact to rather extensive care. It is important to note that all such indices are relative in nature and can only be interpreted in terms of the comparison or control conditions against which they were generated.
METHOD
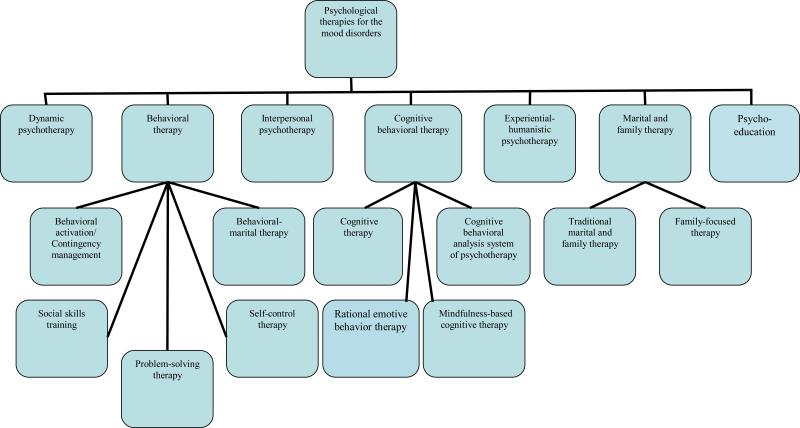
The method of this review is very similar to those of two other reviews we carried out to determine which psychological therapies are empirically supported for adults with social phobia[12] or acute stress and posttraumatic stress disorders.[13] We carried out a literature search of the PsycINFO and PubMed databases and the reference sections of chapters and journal articles to identify randomized controlled trials (RCTs) of psychological therapies for the mood disorders through the end of 2009. Trials were included only if adult patients with a diagnosed mood disorder were randomly allocated to different treatments including one or more psychosocial interventions. The method of the intervention had to be clearly described and the articles written in English. Therapeutic approaches evaluated in the trials were classified as dynamic, interpersonal, cognitive-behavioral, behavioral, experiential-humanistic, marital/family, or psycho-educational (see Figure 1). Chambless & Hollon's (1998) criteria were used to draw conclusions about the efficacy of each.[7]
Figure 1.
Classification of psychological therapies for the mood disorders
RESULTS
Major Depressive Disorder
As shown in Table 1, 101 RCTs were identified with respect to MDD. These trials evaluated the efficacy of dynamic psychotherapy (N=17), interpersonal psychotherapy (IPT) (N=19), cognitive-behavior therapy (CBT) (N=64), behavior therapy (BT) (N=22), experiential-humanistic psychotherapy (N=6), and marital/family therapy (N=2).
Table 1.
Major Depressive Disorder (Adult and Geriatric)
| Study | Treatment/s | Number of Sessions | Control Condition/s | Age of subjects | Sample size | Diagnosis | Setting | Therapists' qualification | Results |
|---|---|---|---|---|---|---|---|---|---|
| Dynamic: | |||||||||
| Covi et al 1974[15] | Dynamic psychotherapy vs brief supportive contacts crossed with medication vs placebo | 16 90-minute group sessions over 17 weeks | Pill-placebo plus brief supportive contacts | Adults aged 20-50 | 207 assigned of whom 146 completed | Depressed outpatients with elevated symptoms | Outpatient research clinic at university medical center | Experienced psychiatrists | Dynamic psychotherapy less efficacious than medications and no better than pill-placebo and did nothing to enhance the efficacy of medications |
| McLean & Hakstian 1979[14] | Dynamic psychotherapy vs contingency management (BT) vs medication | 10 weekly 60-minute sessions | Relaxation therapy (RT) | Adult aged 20-60 | 196 assigned of whom 154 completed | Feighner criteria definite depressive syndrome | Outpatient research clinic at university medical center | Psychiatrists and psychologists with greater or lesser experience | Dynamic psychotherapy less efficacious than other conditions with BT most efficacious of all |
| Gallagher & Thompson 1982[29] | Dynamic psychotherapy vs cognitive therapy (CT) vs behavior therapy (BT) | 16 sessions 12 weeks (1 year naturalistic follow-up) | None | Elderly aged 55 plus | 30 assigned (attrition not reported) | RDC MDD | Geriatric clinic at university medical center | Pre- and post-doctoral psychologists | No differences in terms of acute response although better maintenance of gains for CT or BT than for dynamic psychotherapy |
| Kornblith et al 1983[18] | Dynamic psychotherapy vs three different versions of self-control therapy (SCT) | 12 weekly group sessions | None | Adult women aged 18-60 | 49 assigned of whom 39 completed | RDC MDD | Outpatient research clinic in academic psychology department | Graduate students in psychology (SCT) and MSW candidate (dynamic) | No differences between the groups |
| Hersen et al 1984[17] | Dynamic psychotherapy vs social skills training crossed with medication vs placebo | 12 weekly sessions (plus 6-8 subsequent visits over 6 months) | None | Adult women aged 21-60 | 120 assigned of whom 82 completed | Feighner criteria primary depression (DSM-III MDD) | Outpatient research clinic at university medical center | Experienced psychologists (psychotherapy conditions) and medical clinic personal (medications) | No differences with respect to acute response |
| Steuer et al 1984[33] | Dynamic psychotherapy vs cognitive behavior therapy (CT) | 46 two-hour group sessions over 9 months | None | Elderly aged 55 plus | 35 assigned of whom 20 completed | DSM-III MDD | Geriatric clinic at VA medical center | Pre/post-doctoral psychologists and masters level social workers | CT better than dynamic psychotherapy with respect to acute response |
| Covi et al 1987[16] | Dynamic psychotherapy vs cognitive therapy (CT) with and without medications | 16 group sessions over 14 weeks then 4 weeks of individual sessions | None | Adults aged 18-70 | 90 assigned of whom 70 completed | RDC MDD | Outpatient research clinic at university medical center | Psychiatrist and psychologist | Dynamic psychotherapy less efficacious than CT with or without medications |
| Thompson et al 1987[30] | Dynamic psychotherapy vs cognitive therapy (CT) vs behavior therapy (BT) | 16-20 sessions in 12 weeks | 6-week delayed treatment control | Elderly aged 60 plus | 109 assigned of whom 91 completed | RDC MDD | Geriatric clinic at VA medical center | Doctoral level clinical psychologists | Active treatments did not differ and better than delayed treatment when pooled |
| Gallagher-Thompson et al 1990[31] | No differences in follow-up | ||||||||
| Gallagher-Thompson & Steffen, 1994[32] | Brief psychodynamic psychotherapy vs cognitive therapy (CT) | 16-20 sessions over 12 weeks | None | Adult caregivers of frail elderly | 66 assigned of whom 52 completed | RDC Major, Minor, or Intermittent Depression | Geriatric clinic at VA medical center | Doctoral level clinical psychologists and masters level social workers | Short-term caregivers did better in dynamic and long-term caregivers better in CT |
| Shapiro et al 1994[19] | Dynamic interpersonal psychotherapy vs cognitive behavior therapy (CBT) | 8 or 16 sessions | None | Adults mean age 40 (± 10) | 150 assigned of whom 117 completed | DSM-III MDD | Research clinic | Clinical psychologists | No differences on most measures (CBT better on one) but longer treatment better for more severe |
| Barkham et al 1996[20] | 36 additional patients added | ||||||||
| De Jonghe et al 2001[24] | Dynamic psychotherapy plus medication vs medication alone | 16 sessions (weekly for 8 weeks then biweekly thereafter) | None | Adults aged 18-60 | 167 assigned of whom 129 completed | DSM-III-R MDD | Outpatient research clinic at university medical center | Experienced psychotherapists (discipline unspecified) and psychiatric residents | Combined treatment reduced attrition and thereby increased overall rates of recovery over ADM alone |
| Kool et al 2003[25] | |||||||||
| Combined treatment better than medications alone for patients with personality disorders | |||||||||
| Burnand et al 2002[22] | Dynamic psychotherapy plus medication vs supportive care plus medication | 10 week treatment program (session frequency not stated) | None | Adults aged 20-65 | 95 assigned of whom 74 completed | DSM-IV MDD | Community mental health center | Experienced research nurses under psychoanalytic supervision | No differences on symptom measures but dynamic psychotherapy reduced rates of MDD and promoted work adjustment better than supportive care |
| Cooper et al 2003[21] | Dynamic therapy vs cognitive behavior therapy vs non-directive counseling | Weekly sessions from week 8 to18 postpartum | Routine primary care | Adult women aged 17-42 | 193 assigned of whom 171 completed | DSM-III-R MDD post-partum women | Patient homes | Specialists in the research treatment and non-specialists | Active treatments all superior to control at 4.5 months but not at 9 months post-partum and only dynamic reduced rates of diagnosed depression relative to routine care |
| Maina et al 2007[27] | Brief dynamic therapy plus antidepressant medications (BDT/ADM) | 15 to 30 sessions over 6 months of active treatment followed by 6 months of medication continuation | Brief supportive psychotherapy plus antidepressant medications (BSP/ADM_ | Adults aged 18-65 | 148 assigned of whom*** completed | DSM-IV MDD single episode and presence of focal problem or precipitant life event | Research clinic at university medical center | Psychiatrists who had completed personal training in psychodynamic psychotherapy | Adding BDT to ADM no better than adding BSP at end of treatment but BDT showed continued improvement across 6-month continuation phase |
| Maina et al 2009[28] | Prior BDT reduced rates of recurrence across 48 month treatment-free follow-up | ||||||||
| Dekker et al., 2008[26] | Short-term psychodynamic supportive psychotherapy (SPSP) vs antidepressant medication (ADM) | 8 weekly sessions | None | Adults aged 18-65 | 141 assigned of whom 103 completed treatment | DSM-IV MDD | Community mental health center | Trained psychiatrists and psychotherapists not otherwise specified | Medication superior to SPSP but differences diminishing from weeks 4 through 8 |
| Salminen et al., 2008[23] | Short-term psychodynamic psychotherapy (STPP) vs medication | 16 weekly session | None | Adults aged 20-60 | 51 assigned of whom 40 completed | DSM-IV MDD (mild and moderate) | General practice setting | Experienced psychiatrists and psychologists with two years training in STDP | No differences between groups on any outcomes |
| Interpersonal: | |||||||||
| Klerman et al 1974 (relapse)[36] | Interpersonal psychotherapy (IPT) vs medication vs combined treatment | 32-36 weekly sessions in 8 months | Pill-placebo vs no pill (alone and combined with IPT) | Adult women with a median age in the late 30's and range unspecified | 150 assigned of whom 139 completed | DSM-II neurotic depression (with bipolar) | Outpatient research clinics at university medical centers | Masters' level social workers | IPT as efficacious as medications in preventing relapse if provided without pill-placebo |
| Weissman et al 1974 (social adjustment)[37] | IPT had delayed effect on enhance social adjustment | ||||||||
| Weissman et al 1979 (acute)[38] | Interpersonal psychotherapy (IPT) vs medications vs combined treatment | 16 sessions 16 weeks | Treatment-on-demand nonspecific control | Adults aged 18-65 | 96 assigned of whom 81 completed | RDC MDD (primary) | Outpatient research clinics at university medical centers | Psychiatrists | IPT as efficacious as medications and combined better still with all superior to nonspecific control (acute) |
| DiMascio et al 1979 (acute)[39] | |||||||||
| Weissman et al 1981 (social adjustment / relapse prevention)[40] | 1 year naturalistic follow-up | IPT again had delayed effect on social adjustment but not relapse | |||||||
| Elkin et al 1989, 1995(acute)[41,42] | Interpersonal psychotherapy (IPT) vs cognitive therapy (CT) vs medication | 16-20 sessions over 16 weeks | Pill-placebo | Adults with a mean age of 35 ± 8.5 years | 250 assigned of whom 155 completed | RDC MDD (primary) | Outpatient research clinics at university medical centers | Psychiatrists and doctoral level clinical psychologists | IPT or medications better than CT or pill-placebo among more severe patients with no differences among less severe patients (acute) |
| Watkins et al., 1993[43] | |||||||||
| Drugs faster than IPT or CT | |||||||||
| Shea et al., 1992 (relapse prevention)[99] | Prior CBT vs prior IPT vs prior medications | 18 month naturalistic follow-up | Medication withdrawal | No differences with respect to relapse prevention | |||||
| Frank et al 1990[59] | Maintenance phase interpersonal psychotherapy (IPT) vs maintenance medication vs combined treatment | 36 monthly sessions (after up to 36 weeks treatment with IPT plus drugs) | Pill-placebo control (alone and combined with IPT) | Adults aged 21-65 | 128 assigned of whom 106 completed | RDC MDD with history of recurrence and currently in recovery | Outpatient research clinic at university medical center | Social workers, psychologists, or nurse clinicians with masters or doctorates | IPT more efficacious than pill-placebo control but less efficacious than and did little to enhance the efficacy of maintenance medication in prevention of recurrence |
| Schulberg et al 1996[52] | Interpersonal psychotherapy (IPT) vs medication | 16 weekly sessions (and 4 monthly sessions) | Treatment as usual (TAU) | Adults aged 18-64 | 276 assigned of whom 150 completed | DSM-III-R MDD | Primary care setting | Psychiatrists and clinical psychologists | IPT as efficacious as medications and both superior to TAU |
| Markowitz et al 1998[49] | Interpersonal psychotherapy (IPT) vs cognitive behavior therapy (CBT) vs medications | 16 sessions 17 weeks | Supportive therapy | Adults (HIV) aged 24-59 | 101 assigned of whom 69 completed | HIV+ with depression (about half met for DSM III-R MDD) | Outpatient research clinic at university medical center | Psychiatrists and social workers (IPT) and clinical psychologists (CBT) | IPT or medications both produced better acute response than either CBT or supportive psychotherapy |
| Reynolds, Frank et al 1999[61] | Maintenance phase interpersonal psychotherapy (IPT) vs maintenance medication vs combined treatment | 36 monthly sessions (after up to 36 weeks of combined treatment) | Pill-placebo control (alone and combined with IPT) | Elderly aged 60 or older | 107 assigned of whom 96 completed | RDC MDD with history of recurrence and currently in recovery | Outpatient research clinic at university medical center | Masters level social workers and masters and doctoral level psychologists | IPT more efficacious than pill-placebo control and comparable to and enhanced the efficacy of maintenance medications in prevention of recurrence |
| Reynolds, Miller et al 1999[57] | Interpersonal psychotherapy (IPT) vs medication vs combined treatment | 16 sessions over 16 weeks | Pill-placebo control (alone and combined with IPT) | Elderly aged 50 or older | 80 assigned of whom 73 completed | RDC MDD in recently bereaved | Outpatient research clinic at university medical center | Psychiatrists | IPT no better than placebo and did nothing to enhance the efficacy of medications |
| O'Hara et al., 2000[44] | Interpersonal psychotherapy (IPT) | 12 weekly 60-minute sessions | Wait list control | Adult women aged 18 and above | 120 assigned of whom 99 completed | DSM-IV MDD in postpartum females | Private practice settings | Doctoral level clinical or counseling psychologists | IPT reduced depressive symptoms and improved social adjustment |
| Judd et al 2001[53] | Interpersonal psychotherapy (IPT) plus medication | 12 sessions | Treatment as usual (TAU) plus ADM | Adults aged 18-65 | 32 assigned of whom 28 completed | DSM-IV MDD | General practice | General practitioners | Depression improved in both treatments but no differences between conditions |
| Bolton et al., 2003[50] | Interpersonal psychotherapy (IPT) | 16 weekly 90-minute group sessions | No treatment | Adults | 341 assigned of whom 224 completed | DSM-IV MDD (and sub-thresh) | Rural Ugandan villages | Indigenous nonprofessionals trained in IPT | Group IPT superior to no treatment control |
| Bass et al., 2006[51] | Differences favoring IPT sustained over 6 month follow-up | ||||||||
| Spinelli & Endicott 2003[45] | Interpersonal psychotherapy (IPT) modified for antepartum depression | 16 weekly sessions | Didactic parent education | Adult women aged 18-45 | 50 assigned of whom 38 completed | DSM-IV MDD in pregnant women | Outpatient research clinic | Experienced therapists | IPT produced greater rate of improvement than did didactic parenting control (60% vs 15%) |
| Reynolds et al 2006[62] | Maintenance phase interpersonal psychotherapy (IPT) vs clinical management crossed with maintenance medications (ADM) vs pill-placebo | Monthly maintenance sessions for two years | Pill-placebo control (alone and combined with IPT) | Geriatric aged 70 and above | 116 assigned of whom 90 completed maintenance phase | DSM-IV MDD and response to combined treatment | Outpatient research clinic | Experienced IPT therapists (nurses, social workers, and psychologists) | ADM better than placebo with or without IPT but no effect for IPT with or without medications |
| Carreira et al 2009[63] | IPT protects against recurrence in cognitively impaired unmedicated patients | ||||||||
| Van Schaik et al 2006[58] | Interpersonal psychotherapy (IPT) | 10 sessions over 5 months | Treatment as usual (TAU) | Geriatric aged 55 and older | 143 assigned of whom 120 completed | PRIME-MD depression | General practice settings (x12) | Psychologists and psychiatric nurses | IPT associated with fewer patients who still met criteria for depression than TAU but no differences in more stringent rates of remission |
| Luty et al 2007 (acute)[46] | Interpersonal psychotherapy (IPT) vs cognitive behavior therapy (CBT) | 8-19 sessions over 16-20 weeks | None | Adults aged 18 and above | 177 assigned of whom 159 completed | DSM-IV MDD | Outpatient research clinic | Experienced therapists with MD or PhD | CBT better than IPT at level of nonsignificant trend in full sample and superior for more severe or Axis II patients |
| Joyce et al 2007 (personality)[47] | |||||||||
| Schramm et al 2007[54] | Interpersonal psychotherapy plus antidepressant medication (Comb) vs antidepressant medication alone | 15 individual and 8 group sessions over 5 weeks | None | Adults aged 18-65 | 130 assigned of whom 105 completed | DSM-IV MDD (included bipolar II) | Inpatient psychiatric hospital | Psychiatrists and psychologists who completed 3-year training program in IPT | Combined treatment superior to medications alone |
| Schramm et al 2008[55] | Indications of enduring effect for prior IPT | ||||||||
| Marshall et al 2008[48] | Interpersonal psychotherapy (IPT) vs cognitive behavior therapy (CBT) vs antidepressant medications | 16 weekly sessions | None | Adults (age unspecified) | 159 assigned of whom 102 completed | DSM-IV MDD | University affiliated research clinic | Doctoral level psychologists and pre-doctoral psychology graduate students | IPT less efficacious than medication with CT not differing from either |
| Swartz et al 2008[56] | Interpersonal psychotherapy for mothers of children with psychiatric illnesses (IPT-MOMS) | Engagement interview followed by 8 sessions of IPT | Treatment as usual (TAU) | Adults aged 18-65 | 65 assigned of whom 47 completed | DSM-IV MDD | Pediatric mental health clinic | Masters or doctoral level therapists with degrees in social work, nursing, psychology, or psychiatry | IPT-MOMS more efficacious than TAU in terms of depressive symptoms and global functioning in moms and depression in offspring |
| Cognitive: | |||||||||
| Rush et al 1977 (acute)[66] | Cognitive therapy (CT) vs antidepressant medication (ADM) | 20 sessions 12 weeks | None | Adults aged 18-65 | 41 assigned of whom 32 completed | Feighner definite depression (DSM-II neurotic) | Outpatient research clinic at university medical center | Psychiatrists, psychiatric residents and pre- and post-doctoral psychologists | CBT better than ADM (acute) |
| Kovacs et al 1981 (relapse)[93] | Prior CBT | 12 month naturalistic follow-up | Medication withdrawal | Prior CBT better than prior ADM at preventing relapse | |||||
| Blackburn et al 1981 (acute)[67] | Cognitive therapy (CT) vs antidepressant medication (ADM) vs combined | 15-20 sessions in 12-20 weeks | None | Adults aged 18-65 | 88 assigned of whom 64 completed | RDC primary major depression | Outpatient research clinic at university medical center and general practice clinic | Doctoral level clinical psychologists | CBT (with or without ADM) better than ADM alone in community sample with combined better than either monotherapy in psychiatric setting (acute) |
| Blackburn et al 1986 (relapse / recurrence)[94] | Prior CBT with boosters through month six | 24 month naturalistic follow-up | Medication withdrawal after month six | Prior CBT (with or without ADM) better than prior ADM preventing recurrence | |||||
| Murphy et al 1984 (acute)[68] | Cognitive therapy (CT) vs antidepressant medication (ADM) vs combined | 20 sessions in 12 weeks | Placebo (only in combination with CBT) | Adults aged 18-60 | 95 assigned of whom 70 completed | Feighner definite depression RDC MDD primary | Outpatient research clinic at university medical center | Psychiatrists, psychiatric residents and pre- and post-doctoral psychologists | No differences between conditions (acute) |
| Simons et al 1986 (relapse)[95] | Prior CBT | 12 month naturalistic follow-up | Medication withdrawal | Prior CBT better than prior ADM at preventing relapse | |||||
| Teasdale et al 1984[87] | Cognitive therapy (CT) added to treatment as usual | 20 sessions over 12 weeks | Treatment-as-usual including medications (TAU) | Adults aged 18-60 | 44 assigned of whom 34 completed | RDC MDD | General practice | Doctoral level clinical psychologists trained in CT at Center for Cognitive Therapy | Adding CT enhanced the effects of TAU |
| Miller et al., 1989[84] | Cognitive therapy plus antidepressant medications (CT/ADM) vs behavior therapy plus antidepressant medications (BT/ADM) vs antidepressant medications (ADM) | Daily sessions during inpatient stay and then 20 weekly outpatient sessions | None | Adults with a mean age in the mid-to-late 30's | 46 assigned of whom 32 completed | DIS MDD | Inpatient medical setting | Experienced clinical psychologists (CT and BT) and research psychiatrists (ADM) | CT and BT both enhanced the efficacy of ADM alone although differences did not emerge until after discharge from inpatient setting |
| Bower et al 1990[85] | Cognitive therapy plus antidepressant medications (CT/ADM) vs behavior therapy plus antidepressant medications (BT/ADM) vs antidepressant medications (ADM) | 12 session in 30 days | None | Adults aged 18-60 | 30 assigned of whom 30 completed | DSM-III MDD | Inpatient medical setting | Single experienced clinical psychologist (study author) | CT and BT each enhanced efficacy of ADM |
| Selmi et al 1990[129] | Computer-administered cognitive behavioral therapy (CaCBT) vs therapist-administered CBT | 6 weekly sessions | Wait list | Adults with mean age in late 20's | 36 assigned of whom 36 completed | RDC major, minor, or intermittent depression | Outpatient research clinic at university medical center | Graduate students in clinical psychology | Computer-assisted CBT as efficacious as therapist-administered CBT and both superior to wait list |
| Hollon et al 1992 (acute)[70] | Cognitive therapy (CT) vs antidepressant medication (ADM) vs combined | 20 sessions in 12 weeks | None (acute) | Adults aged 18-65 | 107 assigned of whom 64 completed | RDC primary major depressive disorder | Outpatient research clinic at medical center and community | Doctoral level psychologist and ICSW level social workers | No differences between conditions (acute) |
| Evans et al 1992 (relapse)[96] | Prior CBT vs continue ADM | 24 month naturalistic follow-up | Medication withdrawal | mental health clinic | Prior CBT as efficacious as continued ADM and better than ADM withdrawal at preventing relapse | ||||
| Scott & Freeman 1992[89] | Cognitive behavior therapy (CBT) vs antidepressant medication (ADM) vs social work counseling (SWC) | 16 weekly sessions | Treatment-as-usual (TAU) | Adults aged 18-65 | 121 assigned of whom 105 completed | DSM-III MDD | General practice clinics | Clinical psychologists (CBT) and social workers (SWC) | Few differences among the conditions but those that were evident tended to favor social work counseling |
| Fava et al., 1994[100] | WBT added to ADM vs ADM alone in recovered patients with history of recurrence | 10 sessions in 20 weeks to 24 month naturalistic follow-up | Medication withdrawal during 24 month naturalistic follow-up | Adults with mean age in mid-40's | 43 assigned of whom 40 completed | DSM-III-R MDD in full remission | Outpatient research clinic at university medical center | Single research psychiatrist | Prior exposure to CBT reduced residual symptoms relative to clinical management following medication withdrawal |
| Murphy et al 1995[68] | Cognitive behavior therapy (CBT) vs relaxation training (RT) vs antidepressant medications (ADM) | 20 sessions over 16 weeks | None | Adults aged 18-60 | 37 assigned of whom 24 completed | Feighner criteria for MDD | Outpatient research clinic with patients recruited via advertisement | Graduate students in psychology, doctoral level psychologist and clinical social worker | CBT and RT both superior to ADM and did not differ from one another (it is not clear why ADM did so poorly in this study) |
| Blackburn & Moore 1997[83] | Cognitive therapy followed by cognitive therapy (CT/CT) vs antidepressant medication followed by antidepressant medications (ADM/ADM) vs antidepressant medications followed by cognitive therapy (ADM/CT) | 16 weekly sessions (acute)/27 monthly sessions over next 2 years (maintenance) | None | Adults aged 18-65 | 75 assigned of whom 67 completed | RDC MDD primary | Outpatient research clinic (UMC) with referrals from general practice | Experienced clinical psychologists | No differences between treatments during acute or maintenance treatment |
| Scott et al., 1997[86] | Cognitive behavior therapy plus treatment-as-usual (CBT/TAU) | 6 weekly 30-minute sessions | Treatment- as-usual (TAU) | Adults aged 18-65 | 48 assigned of whom 34 completed | DSM-III-R MDD | Primary care | Professional discipline not specified | Combined treatment with CBT better than TAU alone |
| Fava et al., 1998[101] | WBT added to ADM vs ADM alone in recovered patients with history of recurrence | 10 sessions in 20 weeks to 24 month naturalistic follow-up | Medication withdrawal during 24 month naturalistic follow-up | Adults with mean age in late 40's | 40 assigned of whom 40 completed | RDC major depressive disorder in full remission | Outpatient research clinic at university medical center | Single research psychiatrist | Prior exposure to WBT prevented recurrence following medication withdrawal |
| Bright et al 1999[80] | Cognitive behavior therapy (CBT) vs mutual support group therapy (MSG) | Weekly 90-minute sessions over 10 weeks | None | Adults aged 18-60 | 98 assigned of whom 68 completed | DSM-III-R MDD or dysthymia or depression NOS | Outpatient psychology department clinic | Professional therapists and para-professional therapists | No differences between the treatment conditions with some indications of advantage for professional therapists within CBT conditions |
| Jarrett et al 1999[75] | Cognitive therapy (CT) vs antidepressant medication (ADM) | 20 sessions over 10 weeks | Pill-placebo | Adults with mean age in late 30's | 108 assigned of whom 71 completed | DSM-III-R MDD (atypical subtype) | Outpatient research clinic at university medical center | Psychiatrist and doctoral level psychologists | CBT or ADM both superior to pill-placebo (acute) |
| Paykel et al 1999[102] | Cognitive therapy added to ongoing antidepressant medication (CT plus ADM) vs antidepressant medication (ADM) for residual depression | 16 sessions in 20 weeks (with 2 extra booster sessions) followed by 48 week follow-up phase during which ADM continued | None | Adults aged 21-65 | 158 patients of whom 127 completed | DSM-III-R MDD in partial remission with residual symptoms | Outpatient research clinic at two university medical centers | Professional discipline not specified but all experienced | Adding CBT enhanced the efficacy of ADM in terms of enhancing full remission and preventing subsequent relapse and recurrence |
| Paykel et al 2005[103] | Six year follow-up found that enduring effects persisted through the first three years of follow-up | ||||||||
| Keller et al 2000 (acute)[116] | Cognitive behavioral analytic system for psychotherapy (CBASP) vs antidepressant medication (ADM) vs combination (CBASP/ADM) | 16 sessions in 12 weeks (acute phase) | None | Adults aged 18-75 | 681 assigned of whom 519 completed | DSM-IV chronic major depressive disorder or current MDD superimposed on dysthymia | Outpatient research clinics at university medical centers | Psychiatrists, doctoral level psychologists, and MSW level social workers | Combined treatment better than either single modality which did not differ (acute) |
| Klein et al 2004 (recurrence)[118] | CBASP | 13 monthly sessions over 52 weeks of maintenance | Assessment only control | Adults mean age 45.1 ± 11.4 years | 82 assigned of whom 61 completed | Acute and crossover CBASP responders | Maintenance CBASP reduced rate of recurrence relative to assessment only | ||
| Teasdale et al 2000[109] | Mindfulness-based cognitive therapy (MBCT) superimposed on treatment-as-usual (TAU) | 8 weekly two hour sessions followed by 52 week naturalistic follow-up | Treatment-as-usual (TAU) | Adults aged 18-65 | 145 assigned of whom 132 completed | DSM-III-R MDD with history of recurrence in full remission or recovery | Outpatient research clinics | Doctoral level clinical psychologists | MBCT plus TAU better than TAU at preventing relapse and recurrence in recovered patients with 3 or more prior episodes |
| Jarrett et al 2001[119] | Continuation cognitive therapy (C-CT) (following 20 sessions of acute phase CT) | 10 sessions in 8 months (followed by 16 months of naturalistic follow-up) | Assessment only control (following 20 sessions of acute phase CT) | Adults aged 18-65 | 84 assigned of whom 76 completed | DSM-IV MDD recurrent in remission | Outpatient research clinic at university medical center | Professional discipline not specified but all experienced | C-CT better than assessment only control in reducing risk for relapse and recurrence in remitted patients |
| Thompson et al (2001)[124] | Cognitive behavior therapy (CBT) vs antidepressant medication (ADM) vs combined treatment (CBT/ADM) | 16-20 sessions over 12-16 weeks | None | Geriatric aged 60 and over | 102 assigned of whom 71 completed | RDC MDD as ascertained by SADS | Outpatient research clinic at VA hospital and university medical center | Clinical psychologists with at least 1-year experience treating geriatric patients | Combined treatment generally better than ADM alone (especially with more severely depressed patients) with CBT alone intermediate and closer to combined |
| Perlis et al 2002 (sequential)[107] | Cognitive therapy added to ongoing antidepressant medication (CT/ADM) vs antidepressant medication (ADM) | 12 weekly sessions followed by 7 biweekly sessions | None | Adults aged 18-65 | 132 assigned of whom 85 | DSM-III-R MDD in remission | Outpatient research clinic | Doctoral level clinical psychologists | Adding CBT to ADM no better than increasing ADM dose in reducing relapse or residual symptoms |
| Miranda et al 2003[90] | Cognitive behavior therapy (CBT) vs antidepressant medication (ADM) | 8 weekly sessions followed by 8 more if needed | Community referral (CR) | Adults mean age 29.3 ± 7.9 years | 267 | DSM-IV MDD in mostly low-income minority women | County clinics, research offices and patient homes | Experienced psychotherapists | Both CBT and ADM reduced depression more than CR |
| Miranda et al 2005[91] | 12- month follow-up | Both continued CBT and ADM superior to CR | |||||||
| Ma & Teasdale 2004[110] | Mindfulness-based cognitive therapy (MBCT) superimposed on treatment-as-usual (TAU) | 8 weekly two hour sessions followed by 52 week naturalistic follow-up | Treatment-as-usual (TAU) | Adults aged 18-65 | 75 assigned of whom 69 completed | DSM-III-R MDD with history of recurrence in full remission or recovery | Outpatient research clinic | Experienced cognitive therapists | MBCT plus TAU better than TAU alone at preventing relapse and recurrence in recovered patients with 3 or more prior episodes |
| Bockting et al 2005[104] | Cognitive behavior therapy (CBT) superimposed on treatment-as-usual (TAU) | 8 two-hour weekly sessions | Treatment-as-usual (TAU) | Adults with mean age in mid 40's | 187 assigned of whom 165 completed | DSM-IV MDD with at least 2 prior episodes | Recruited from psychiatric centers via advertisements | Psychologists (including first author) | CBT plus TAU better than TAU alone at preventing relapse and recurrence with larger effects for patients with more prior episodes |
| Cuijpers et al 2005[92] | Cognitive behavior therapy (CBT) | Mean of 10 sessions (SD 11) | Treatment-as-usual (TAU) | Adults aged 18-65 | 425 assigned of whom 288 completed | DSM-IV MDD | Outpatient mental health centers | Experienced therapists | No differences among less severe but CBT superior to TAU among more severe |
| DeRubeis et al 2005 (acute)[76] | Cognitive therapy (CT) vs antidepressant medication (ADM) | 24 sessions 16 weeks | Pill-placebo | Adults aged 18-65 | 240 assigned of whom 204 completed | DSM-IV MDD (severe) | Outpatient research clinics at university medical centers | Doctoral level psychologists and psychiatric nurse | CT or ADM superior to pill-placebo control |
| Hollon et al 2005 (relapse)[97] | Prior CT vs continuation ADM | Medication withdrawal onto pill-placebo | Prior CT as efficacious as continued ADM and better than placebo withdrawal at preventing relapse | ||||||
| Wright et al 2005[130] | Computer-assisted cognitive therapy (CaCT) vs cognitive therapy alone (CT) | 9 sessions in 8 weeks | Wait list (WL) | Adults aged 18-65 | 45 assigned of whom 40 completed | DSM-IV MDD | University-affiliated psychiatric center | Master's and doctoral-level clinicians | CaCT comparable to live CT and both better than WL in reducing depression with gains maintained across 6-month follow-up |
| Smit et al 2006[102] | Cognitive behavior therapy plus depression recurrence prevention (CBT/DRP) vs DRP alone | 10-12 weekly sessions CBT then 3 sessions DRP | Treatment-as-usual (TAU) | Adults aged 18-70 | 267 assigned of whom 240 completed | DSM-IV MDD (using CIDI) | Primary care (55 different practices) | Cognitive therapists (educational level and experience unspecified) | No differences between the conditions |
| Strauman et al (2006)[128] | Cognitive therapy (CT) vs self-system therapy (SST) | 20 sessions weekly for first 6 weeks and at least biweekly thereafter | None | Adults age unspecified | 45 assigned of whom 39 completed | DSM-IV MDD or dysthymia (except for six patients) | University-based research clinic | Doctoral-level clinical psychologists and predoctoral interns | No overall differences between the conditions but SST better than CT for patients who lacked promotion goals |
| Rohan et al (2007)[127] | Cognitive behavior therapy (CBT) vs light therapy (LT) vs combined CBT plus LT (CBT/LT) | 12 90-minute sessions twice weekly over six weeks | Wait list | Adults aged 18 and older | 61 assigned of whom 54 completed | DSM-IV MDD recurrent with seasonal pattern | University-based research clinic | Doctoral level psychologist with graduate student co-therapists | All three active treatments comparable and each superior to wait list control |
| Thase et al 2007[126] | Cognitive therapy alone (CT) or in combination with medication (COMB) vs medication switch or augmentation | 16 sessions over 12 weeks | None | Adults aged 18-75 | 304 assigned | DSM-IV MDD with nonresponse to medication treatment | Community mental health and university-based clinics and primary care settings | Doctoral level psychologists, psychiatrists, masters-level social workers and psychiatric nurses | CT did not differ from medication switch but medication augmentation faster than CT augmentation |
| Bagby et al 2008[82] | Cognitive behavior therapy (CBT) vs antidepressant medication (ADM) | 16-20 weekly sessions | None | Adults aged 18-70 | 275 assigned of whom 174 completed | DSM-IV MDD | University-affiliated outpatient clinic | Master's and doctoral-level clinicians | No differences on continuous measures but ADM beat CT on response rates and with neurotic patients |
| Conradi et al 2008[105] | Cognitive behavior therapy plus psychoeducation (CBT/PE) vs psychoeducation (PE) | 10-12 CBT sessions followed by 3 PE sessions | Treatment-as-usual (TAU) | Adults aged 18-70 | 208 assigned with attrition not reported | DSM-IV MDD (using CIDI) | Primary care clinics | No information provided | CBT plus PE but not PE alone superior to TAU among patients with four or more prior episodes |
| David et al 2008[71] | REBT vs CT vs ADM (continued at reduced dose during follow-up) | 20 sessions over 14 weeks with 6 month follow-up | None | Adults with mean age in mid-30's | 170 assigned of whom 151 completed | DSM-IV MDD | Outpatient research clinic in university medical center | Doctoral-level psychologists and psychiatrists | No differences were evident between the conditions at end of treatment; REBT held up better than ADM at 6 months |
| Sava et al 2009[72] | REBT and CT both more cost-effective than ADM | ||||||||
| Faramarzi et al 2008[78] | Cognitive behavior therapy (CBT) vs antidepressant medications (ADM) | 10 weekly two-hour group sessions | Assessment only control | Adult women with fertility problems | 124 assigned of whom 89 completed | DSM-III-R MDD | Outpatient research clinic in university medical center | Experienced clinical therapists | CBT superior to ADM which was in turn superior to assessment only control |
| Kuyken et al 2008[111] | MBCT plus medication taper vs antidepressant medication (ADM) | 8 weekly sessions with four boosters over 52 week naturalistic follow-up | None | Adults aged 18 and above | 123 assigned of whom 104 completed treatment and 96 completed follow-up | DSM-IV MDD in remission with history of 3 or more prior episodes | Primary care | Doctoral level psychologists and occupational therapists | MBCT more effective than ADM in reducing residual symptoms and improving quality of life; 75% of MBCT patients able to discontinue ADM |
| Laidlaw et al 2008[125] | Cognitive behavior therapy (CBT) | 8 sessions (on average) | Treatment-as-usual (TAU) | Geriatric aged 60 and over | 44 assigned of whom 40 completed | DSM-IV MDD | Primary care | Masters level clinical psychologists and one graduate psychologist | CBT superior to TAU with respect to categorical diagnoses (and some continuous measures after controlling for patient characteristics) |
| Manber et al 2008[121] | Cognitive behavior therapy plus antidepressant medication (CBT/ADM) vs sleep hygiene plus ADM | 5 weekly sessions followed by 2 biweekly sessions | None | Adults aged 18-75 | 30 assigned of whom 28 completed | DSM-IV MDD plus insomnia | Outpatient research clinic in university medical center | Two licensed clinical psychologists | CBT plus ADM superior to ADM plus sleep hygiene control in terms of rates of remission from both depression and insomnia |
| Dozois et al 2009[123] | Cognitive therapy plus antidepressant medication (CT/ADM) vs antidepressant medication alone (ADM) | 15 weekly sessions | None | Adults aged 18-65 | 48 assigned of whom 42 completed | DSM-IV MDD | Outpatient tertiary care clinic | Two licensed master's level therapists | Adding CT did little to enhance the effects of ADM but did improve cognitive structure |
| Freedland et al 2009[122] | Cognitive behavior therapy plus usual care (CBT/UC) vs supportive stress management plus usual care (SSM/UC) | 12-16 weekly sessions | Usual care (with approximately half of all participants receiving antidepressant medications) | Adults aged 21 and older | 123 assigned of whom 113 completed | DSM-IV MDD (66%) or minor depressive episode (34%) undergoing coronary bypass surgery in the last year | Outpatient research clinic in university medical center | Experienced doctoral level clinical or counseling psychologists or clinical social workers | CBT and SSM both superior to usual care with CBT having greater and more durable effects than SSM |
| Kocsis et al 2009 (acute)[120] | Cognitive behavioral analytic system for psychotherapy plus antidepressant medication ((CBASP/ADM) vs brief supportive psychotherapy plus antidepressant medication (BSP/ADM) | 16 sessions in 12 weeks | Flexible algorithm-driven individualized antidepressant medication (ADM) | Adults aged 18-75 | 491 assigned of whom 423 completed | DSM-IV chronic major depressive disorder or current MDD superimposed on dysthymia who did not respond to12 weeks of medication treatment | Outpatient research clinics at university medical centers | Psychiatrists, doctoral level psychologists, and MSW level social workers | Augmenting flexible algorithm medication treatment with CBASP (or BSP) no more efficacious than ADM alone |
| Serfaty et al 2009[88] | Cognitive behavioral therapy plus treatment as usual (CBT/TAU) vs talking control plus treatment as usual (TC/TAU) | Up to 12 individual sessions over 4 months | Treatment-as-usual (including medications for about half) (TAU) | Geriatric aged 65 and above | 204 assigned of whom 177 completed | DSM-IV MDD (88%) or minor depression (12%) | Primary care | Experienced cognitive behavioral therapists (degree not specified) | CBT superior to TC when each added to TAU |
| Wilkinson et al 2009[108] | Cognitive behavioral therapy plus antidepressant medication (CBT/ADM) | Up to 8 90-minute group sessions | Antidepressant medication (ADM) | Geriatric aged 60 and above | 45 assigned of whom 36 completed | ICD MDD within last year and remitted for at least 2 months on ADM | General practice and psychiatric clinics | Doctoral level psychologist with experience in CBT | CBT reduced rates of recurrence but differences not significant in small sample |
| Behavioral: | |||||||||
| Nezu 1986[132] | Problem-solving therapy (PST) vs nonspecific therapy | 8 weekly 120-minute group sessions | Wait-list | Adult | 32 assigned of whom 26 completed | RDC MDD | Outpatient research clinic in university mental health center | Pre-doctoral graduate students in psychology | PST superior to either nonspecific or wait-list control |
| Nezu & Perri 1989[133] | Problem-solving therapy (PST) vs abbreviated PST | 10 weekly 90-minute group sessions | Wait-list | Adults aged 18-65 | 43 assigned of whom 39 completed | RDC MDD | Outpatient research clinic in university mental health center | Pre-doctoral graduate students in psychology | PST superior to either abbreviated PST or wait-list control |
| O'Leary & Beach 1990[138] | Behavioral marital therapy (BMT) vs cognitive therapy (CT) | 16 weekly sessions | Wait list | Adults aged 28-59 | 45 assigned of whom 45 completed | DSM-III MDD or dysthymia | Research clinic (recruited volunteers) | Pre- and post-doctoral clinical psychologists | BMT comparable to CT in reducing depression and both better than wait list; BMT better than CT or wait list on reducing marital distress |
| Beach & O'Leary 1992[139] | |||||||||
| Jacobson et al 1991[140] | Behavioral marital therapy (BMT) vs cognitive therapy (CT) vs combined treatment (BMT+CT) | 20 sessions over 12 weeks | None | Adults with mean age in high 30's | 72 assigned of whom 60 completed | DSM-III MDD | Research clinic (referrals and recruited volunteers) | Pre- and post-doctoral clinical psychologists and social worker | CT better than BMT for depression, whereas BMT better than CT for marital distress |
| Jacobson et al 1993[141] | |||||||||
| No differences between the groups across 12 months | |||||||||
| Arean et al 1993[134] | Problem-solving therapy (PST) vs reminiscence therapy (RT) | 12 weekly group sessions | Wait-list | Geriatric aged 55 and above | 75 assigned of whom 59 completed | RDC MDD | Outpatient research clinic in university medical center | Graduate students in clinical psychology | PST superior to RT and each superior to wait list |
| Mynors-Wallis et al 1995[135] | Problem-solving therapy (PST) vs antidepressant medication (ADM) | 6 30-minute sessions over 12 weeks (1st 60-minutes) | Pill-placebo (PLA) | Adults aged 18-65 | 91 assigned of whom 82 completed | Diagnostic method not specified | Primary care clinic | Psychiatrist and general practitioners (including authors) | PST or ADM superior to PLA |
| Van den Hout et al 1995[131] | Self-control therapy plus treatment-as-usual (SCT/TAU) | 12 weekly 90-minute group sessions | Treatment-as-usual (TAU) | Adults aged 20-59 | 49 assigned (number completed not reported) | DSM-III-R MDD or dysthymia | Psychiatric day-treatment center | Professional discipline not specified | Adding SCT enhanced response to TAU alone |
| Emanuels-Zuurveen & Emelkamp 1996[142] | Behavioral marital therapy (BMT) vs cognitive behavior therapy (CBT) | 16 weekly sessions | None | Adults with mean age in the high 30's | 36 assigned of whom 27 completed | DSM-III-R MDD | Outpatient research clinic in academic psychology department | Graduate students in clinical psychology | No differences between the conditions on depression with BMT having a greater impact on relationship variables |
| Jacobson et al 1996[144] | Behavioral component of cognitive therapy (bCT) vs partial cognitive therapy (pCT) vs full cognitive therapy (CT) | 20 sessions in 12 weeks | None | Adult with mean age in late 30's | 150 assigned of whom 137 completed | DSM-III-R MDD | Outpatient university clinic | Doctoral level clinical psychologists | No differences between different components in terms of reduction of acute distress |
| Gortner et al 1999[145] | |||||||||
| Prior CT vs prior pCT vs prior bCT | No differences with respect to prevention of subsequent relapse | ||||||||
| Dowrick et al 2000[137] | Problem-solving therapy (PST) vs depression prevention course (DPC) | 6 sessions (PST) and 8 sessions (DPC) | Assessment only control | Adults aged 18-65 | 425 assigned of whom 317 completed | DSM-IV MDD or Adj Disorder | Community settings | Health care professionals | Both PST and DPC superior to assessment only control |
| Mynors-Wallis et al 2000[136] | Problem-solving therapy (PST) vs antidepressant medication (ADM) vs combined treatment (PST/ADM) | 6 30-minute sessions over 12 weeks (1st 60-minutes) | None | Adults aged 18-65 | 151 assigned of whom 116 completed | RDC MDD | Primary care clinic | General practice physicians and research practice nurses | Combined treatment no more efficacious than PST or ADM (professional discipline of therapists made no difference) |
| Hopko et al., 2003[147] | Behavior activation (BA) vs nonspecific supportive psychotherapy (nSP) | 3 20-minute session per week for two weeks | None | Adults with a mean age of 30 | 25 assigned of whom 25 completed | Major Depression (unstructured psychiatric interviews) | Inpatient psychiatric hospital | Master-level clinicians | BA superior to nSP |
| Dimidjian et al 2006 (acute)[81] | Behavioral activation (BA) vs cognitive therapy (CT) vs antidepressant medication (ADM) | 20 sessions in 16 weeks | Pill-placebo (PLA) | Adults aged 18-60 | 241 of whom 172 completed | DSM-IV MDD | Outpatient research clinic at university medical center | Doctoral level clinical psychologists and social worker (BA or CT) and research psychiatrists (ADM) | BA equals ADM and each better than CT or pill-placebo in reducing acute distress among more severe with no differences among less severe |
| Dobson et al 2008 (relapse)[98] | Prior BT or CT vs ADM continuation | Medication withdrawal onto pill-placebo | |||||||
| Prior BA equals prior CT or continued ADM with prior CT better than withdrawal onto pill-placebo in preventing relapse | |||||||||
| Bodenmann et al 2008[143] | Coping-oriented couples therapy (COCT) vs CBT vs IPT | 10 two-hour biweekly sessions (COCT) vs 20 weekly sessions | None | Adults aged 18 to 60 | 60 assigned of whom 57 completed | DSM-IV MDD (75%) and Dysthymia (25%) | Multisite trial with private practitioners in five Swiss cities | Experienced therapists | No differences between the groups with respect to depression or marital distress although COCT did produce greater change in partner's expressed emotion |
| Experiential-Humanistic: | |||||||||
| Beutler et al 1991[148] | Focused expressive psychotherapy (FEP) vs cognitive behavior therapy (CBT) | 20 weekly group sessions | Supportive self-directive control | Adults aged 22 to 76 | 63 of whom 42 completed | DSM-III MDD | Outpatient research clinic at university medical center | Experienced doctoral level psychologists | Modest main effects favored CBT but resistant patients did best in supportive self-directed control |
| Greenberg & Watson, 1998[149] | Process experiential therapy (PET) components added to client centered therapy (CCT) | 16-20 weekly sessions | None | Adults with a mean age of 40 | 34 of whom 33 completed | DSM-III-R MDD | Outpatient clinic in academic department | Psychiatrist, doctoral psychologists, and graduate students in psychology | No differences between the conditions on measures of depression but PET superior to CCT on measures of interpersonal problems and self-esteem |
| Watson et al 2003[150] | Process experiential therapy (PET) vs cognitive therapy (CT) | 16 sessions over 16 weeks | None | Adults with a mean age in the high 30's | 93 assigned of whom 66 completed | DSM-IV MDD | Outpatient clinic in academic department | Graduate students in counseling psychology and doctoral level psychologists | No differences between the conditions on measures of depression but PET superior to CT on self-reports of interpersonal problems |
| Castonguay et al 2004[153] | Integrative CT (with humanistic and interpersonal strategies) | 16 sessions over 12-15 weeks | Wait list | Adults aged 18-55 | 28 assigned of whom 22 completed | DSM-IV MDD | Outpatient research clinic in psychology department | Graduate students in psychology | ICT superior to wait list control |
| Goldman et al 2006[151] | Emotion-focused therapy (EFT) vs client-centered therapy (CCT) | 16-20 sessions over 16 weeks | None | Adults with mean age in late 30's | 83 assigned of whom 72 completed | DSM-III-R MDD | Outpatient clinic in academic department | EFT superior to CCT | |
| Ellison et al 2009[152] | Responders to EFT less likely to relapse over subsequent 18 months than CCT responders | ||||||||
| Constantino et al 2008[154] | Integrative CT (with humanistic and interpersonal strategies) vs CT alone | 16 sessions over 13-16 weeks | None | Adults aged 18-65 | 22 assigned of whom 19 completed | DSM-IV MDD | Outpatient research clinic in university medical center | Graduate students in psychology | ICT superior to CT |
| Marital and Family: | |||||||||
| Freidman 1975[155] | Dynamic marital therapy vs antidepressant medication (ADM) vs combined treatment | 12 weekly sessions | Pill-placebo | Adults aged 21-67 | 196 assigned of whom 168 completed | Primary diagnosis of depression | Outpatient research clinic | Professional discipline unspecified | ADM better at reducing depression and dynamic marital therapy better at reducing marital distress; combined treatment retained specific benefits of each |
| Clarkin et al 1990[156] | Family therapy plus milieu therapy with antidepressant medication | 6 family sessions in 36 days | Milieu therapy with antidepressant medication | Adults with mean age in mid-30's | 56 assigned of whom 50 completed | DSM-III MDD (n=30) or BD (n=26) | Inpatient research setting at university medical center | Social workers | Female bipolar patients benefited from addition of family therapy but not unipolar patients |
Dynamic Psychotherapy
The dynamic psychotherapies represent the oldest treatments for depression. Early findings were generally unimpressive, although the approach was often included as a comparator by investigators with other allegiances. For example, McLean and Hakstian found brief dynamic therapy less efficacious than their preferred behavioral intervention or medications[14] and Covi and colleagues found dynamic group psychotherapy no better than placebo and less efficacious than medications in one study[15] and less efficacious than CBT (with or without medications) in another.[16] No differences were found relative to social-skills training[17] or self-control therapy[18] in a pair of studies implemented by behaviorally-oriented researchers and few differences were found between psychodynamic interpersonal psychotherapy and CBT in a pair of studies by investigators with little expertise with CBT.[19,20]
Recent studies by investigators with expertise in dynamic psychotherapy have been somewhat more supportive but still less than wholly compelling. A study by Cooper and colleagues in England found that psychodynamic psychotherapy did not differ from CBT or non-directive counseling and that each produced greater change on measures of depression than did routine primary care in the treatment of postpartum depression.[21] A study by Burnand and colleagues in Switzerland found that adding dynamic psychotherapy to medication reduced the proportion of patients who met criteria for MDD following treatment and led to better work adjustment, although there were no differences on measures of depressive symptoms.[22] A study by Salminen and colleagues in Finland on patients with mild-to-moderate MDD in a general practice setting found no differences between short-term dynamic psychotherapy versus fluoxetine antidepressant medication, but the sample was too small to draw firm conclusions.[23] De Jonghe and colleagues in the Netherlands found that adding short-term dynamic psychotherapy increased the proportion of patients responding to medications by virtue of reducing rates of attrition[24] and that patients with personality disorders may have been more likely to respond to combined treatment than to medications alone.[25] A subsequent study by this same group found that antidepressant medications worked more rapidly than short-term dynamic psychotherapy and were superior after eight weeks of treatment.[26] Maina and colleagues in Italy found that brief dynamic therapy was no more efficacious than brief supportive psychotherapy when added to medications at the end of treatment, but that patients continued to improve over a subsequent six-month continuation phase[27] and that patients previously treated with dynamic psychotherapy were less likely to experience a recurrence over a subsequent 48-month treatment-free follow-up.[28]
One of these studies found clear evidence of efficacy relative to routine care[21] and adding psychodynamic psychotherapy enhanced the efficacy of medication on at least some measures in a second,[22] and for at least some patients in a third.[24,25] This is better than it had done in those earlier trials. Perhaps most interesting were the indications that patients treated with brief dynamic psychotherapy plus medications continued to improve after the end of active treatment[27] and were less likely to recur than patients previously treated with supportive psychotherapy plus medications.[28] At the same time, none of these studies found dynamic psychotherapy superior to a nonspecific control or alternative treatment; results were more promising than early trials but hardly impressive.
Dynamic psychotherapy has rarely been tested in the treatment of geriatric depression, but the samples studied have been so small and the quality of the alternative interventions suspect; it is not clear that anything but null findings would have been expected. Gallagher and Thompson found few differences between brief dynamic therapy and either CBT or BT,[29] findings replicated in a second study in which all three active treatments pooled were superior to a wait list control.[30] Treatment gains produced by either CBT or BT were better maintained than those produced by dynamic therapy in the first study but not in the second.[31] A third study by this group found that short-term caregivers did better in brief psychodynamic psychotherapy than they did in CBT, whereas long-term caregivers showed the opposite pattern.[32] Conversely, Steuer and colleagues found CBT superior to dynamic psychotherapy delivered in a groups.[33] There is simply little in this literature to warrant a designation of efficacious or specific.
On the whole, although there is still not compelling evidence speaking to the efficacy of dynamic psychotherapy, it would be premature to conclude that it is not efficacious solely on the basis of early trials by advocates of other approaches. More recent studies by investigators who have an investment in and expertise with the approach do offer some limited support and meta-analyses that aggregate across studies regardless of quality find it no less efficacious than alternative types of psychotherapies.10,11 Although none of the studies in the literature provide strong support for the approach relative to either medications or alternative psychotherapies, one study does suggest an advantage over routine primary care[21] and two others suggest that it can enhance the efficacy of medications on at least some measures[22] and for at least some patients.[24,25] Yet another recent study suggests that its effect may build over time[27] and protect against subsequent recurrence.[28] It seems fair to say that dynamic psychotherapy is possibly efficacious with respect to acute response and the prevention of subsequent relapse/recurrence.
Interpersonal Psychotherapy
Interpersonal psychotherapy (IPT) springs from dynamic roots, but draws on attachment theory and theoretical revisions that focus on interpersonal relationships.[34] It is more structured than dynamic psychotherapy (but less so than cognitive or behavioral approaches) and focuses on current interpersonal difficulties rather than childhood recollections or the therapeutic relationship.[35]
IPT has fared well in a series of controlled trials in fully clinical populations. Klerman and colleagues found that patients treated to remission with the combination of IPT and medications were no more likely to relapse if continued on IPT alone than if continued on medications[36] and patients treated with IPT showed a greater (if somewhat delayed) improvement in interpersonal functioning than did patients treated with medications alone.[37] In a subsequent study, Weissman and colleagues found that outpatients treated with IPT did as well as patients treated with medications and better than patients provided with treatment-on-demand in terms of symptom reduction and that patients treated with combined treatment did better still.[38] Drugs produced more rapid change,[39] but IPT again had a delayed effect on interpersonal functioning.[40] This study speaks to the efficacy of IPT in the reduction of acute symptoms.
IPT also fared well in the placebo-controlled NIMH Treatment of Depression Collaborative Research Project (TDCRP), one of the largest and most influential studies of its time.[41] Among more severely depressed patients, both IPT and drugs outperformed pill-placebo, whereas CBT did not; no differences were evident among less severely depressed patients or in the sample as a whole.[42] Once again, drugs produced faster change than IPT, which showed more change later in treatment.[43] IPT also reduced depressive symptoms and improved social adjustment in women suffering from postpartum depression over wait list in one study[44] and was superior to didactic parent education in a sample of pregnant women with MDD in another.[45] This last study and the TDCRP suggest that IPT is efficacious and specific in the treatment of MDD.
Subsequent studies have not been as supportive. A study conducted in New Zealand found that IPT was less efficacious than CT for patients with more severe depression[46] or perhaps personality disorders.[47] Similarly, a recent Canadian trial found IPT less efficacious than medications.[48] Internal analyses indicated that IPT did particularly poorly with patients high on self-criticism. Although efficacious and specific according to Chambless and Hollon's (1998) criteria,[7] findings with respect to IPT are no longer as consistent as they once were when only advocates conducted trials on the approach.
Studies in special populations also are worthy of note. IPT was as efficacious as drugs (imipramine) plus supportive therapy and more efficacious than either CT or supportive psychotherapy alone in the treatment of depression in a sample of HIV-positive patients; this study would speak to both efficacy and specificity except that only about half the sample met criteria for MDD.[49] Bolton and colleagues found that indigenous nonprofessionals in rural Uganda could be trained to provide group IPT to fellow villagers that reduced rates of depression and improved functioning[50] and that these differences were sustained across a six month follow-up.[51] IPT was as efficacious as medications (if somewhat slower acting) and more efficacious than treatment-as-usual in one study in a primary care setting,[52] although training physicians to provide IPT-based education did little to enhance response to medication in a small general practice sample in another.[53] Adding IPT enhanced response to medication in an inpatient sample,[54] including patients with chronic depression,[55] and there were indications that these differences extended beyond the end of treatment. Finally, a version of the approach adapted for depressed mothers of offspring with psychiatric disorders (IPT-MOMS) was more efficacious than treatment-as-usual in reducing depression in both the mothers and their offspring.[56] On the other hand, Reynolds and colleagues found that IPT did not differ from pill-placebo and was less efficacious than medication in reducing acute distress in a “young” geriatric sample (aged 50 and above) with a history of recent bereavement[57] and no better than usual care with respect to rates of remission or measures of symptom change in another study on a geriatric primary care sample aged 55 and over, although it did reduce the proportion of patients who continued to meet criteria for depression at posttreatment.[58]
Frank and colleagues found monthly maintenance IPT superior to withdrawal onto pill-placebo in a sample of recurrent patients treated to recovery with combined treatment, but maintenance medication (imipramine) was more efficacious still and combined treatment did nothing to improve on medications alone.[59] Maintenance IPT was most efficacious when the sessions maintained a high level of interpersonal focus suggesting the importance of quality of implementation.[60] When this design was replicated in that same setting in a “young” geriatric sample (mainly 60 to 75 years of age), both maintenance IPT and maintenance medications were superior to pill-placebo, with combined treatment best of all.[61] These studies suggest that maintenance IPT is possibly efficacious for the prevention of recurrence, although a subsequent replication found maintenance IPT no more efficacious than pill-placebo and less efficacious than maintenance medication in the treatment of depression in an older geriatric sample aged 70 and above.[62] IPT was protective of cognitively impaired unmedicated elders.[63]
Although negative findings do exist,[46-48] IPT appears to be efficacious and specific in the reduction of acute distress[42,45] and may forestall both relapse and recurrence so long as it is continued or maintained, although perhaps not so well as medications.[36,59,61] In some studies, combined treatment improved on drugs alone,[38,54] although that was not always the case. There also were indications that IPT has a delayed effect on interpersonal skills and relationship quality that builds over time.[37,40] This represents a specific benefit of IPT and may enhance its value as an adjunct to medications. It also appears to be efficacious in the treatment of perinatal depression.[44,45] This is important since pregnant and lactating women may have special reasons to prefer not to be on medication. Recent trials by investigators outside of the core IPT group have not been as uniformly supportive as earlier trials by advocates for the intervention, but the efficacy of the approach appears to be well established when implemented by well-trained therapists.
Cognitive Behavior Therapy
The cognitive behavioral therapies (CBT), of which cognitive therapy (CT) is the most widely practiced variant, assume that negative beliefs and maladaptive information processing contribute to the onset and maintenance of depression. These interventions seek to produce change by teaching patients to evaluate the accuracy of their beliefs (or the relation between their thoughts and feelings in the newer meditation-based approaches), often by using their own behaviors to test their beliefs. CBT has been tested extensively and typically found to be superior to minimal treatment controls and at least as efficacious as other empirically supported interventions.[64] Nonetheless, questions remain as to how it compares to drugs in the treatment of severe depression.[65]
Early studies suggested that CT might be superior to drugs, but often implemented medications in a less than adequate fashion.[66,67] The same appeared to be the case in a later trial that found both CT and relaxation training (included as a nonspecific control) superior to tricyclic ADM in a very small sample with an uncharacteristically poor response to medication.[68] These studies could be taken as support for the specific efficacy of CT since even inadequately implemented medication conditions should have controlled for nonspecific factors, but we are not prepared to go so far. Subsequent studies suggested that CT and drugs are comparable in efficacy when each is adequately implemented[69,70] and an even more recent study suggests that the same may be true for rational emotive behavior therapy (REBT),[71] with either type of psychotherapy more cost-effective.[72] As previously described, CT was less efficacious than either IPT or medications and no more efficacious than pill-placebo in the treatment of severe depression in the TDCRP, the largest and best controlled study of its time,[41,42] but response to treatment varied across sites and CT did as well as medication in the site with more experienced cognitive therapists.[73] DeRubeis and colleagues reanalyzed individual response data on severely depressed patients from the studies just cited and found no differences between CT and drugs across the pooled samples.[74] However, we are reluctant to base a claim of efficacy solely on equivalence to an established standard.[7]
A more recent trial by Jarrett and colleagues found CT as efficacious as medications and superior to pill-placebo in patients with atypical depression[75] and a subsequent study by DeRubeis and colleagues essentially replicated these findings among patients with more severe depressions.[76] These trials are important because they demonstrate that CT can do as well as medications in fully clinical samples that respond to medications.[77] The fact that CT was superior to pill-placebo in each speaks to both efficacy and specificity. An even more recent trial from Iran found CBT superior to medications and both superior to a no treatment control in a sample of depressed women with fertility problems.[78]
However, the efficacy of CT may be moderated both by patient characteristics and therapist experience. In the study by DeRubeis and colleagues,[76] patients with Axis II disorders did better on medications than they did in CT, whereas patients free from such disorders showed the opposite pattern.[79] Moreover, CT was less efficacious than medications at the site with less experienced cognitive therapists[76] (see also the study by Bright and colleagues).[80] This is reminiscent of earlier findings from the TDCRP and consistent with the poor showing by somewhat less experienced cognitive therapists with more severe and complicated patients in a placebo-controlled comparison to medication or behavioral activation described in a subsequent section.[81] Similarly, Bagby and colleagues found that patients with higher neuroticism scores did better on medications than they did in CBT in a study that otherwise found no main effect for treatment.[82] On the other hand, a recent trial from New Zealand found that CT was more efficacious than IPT among patients with more severe depression[46] or Axis II disorders.[47] Although the therapists in that trial were all experienced, it is not clear just how expert they were with either treatment. These findings suggest that CT's efficacy with more severe and complicated patients may vary across studies and depend in part on therapist experience.
Another recent study found CT as efficacious as drugs in recurrent patients[83] and adding CT typically enhanced the efficacy of medication treatment in inpatient samples.[84,85] Studies in primary care settings have found that adding CT typically enhances the efficacy of usual care[86,87] and did so in one study over and above the benefits provided by a contact control,[88] although that has not always been the case.[89] CT was as efficacious as medications and superior to community referral in a sample of mostly low-income minority women with MDD[90] and its effects extended across a one-year follow-up.[91] CBT was superior to treatment-as-usual (TAU) among severely depressed outpatients.[92] In general, these findings are consistent with the notion that CBT is efficacious (if not necessarily specific) in the treatment of MDD.
Patients treated to remission with CT are less likely to relapse following treatment termination than patients treated to remission with drugs alone;[93-95] the magnitude of this effect is at least as great as keeping patients on continuation medication[96] and superior to placebo withdrawal.[97,98] Only the TDCRP failed to find an enduring effect for prior CT.[99] Moreover, these effects may extend to the prevention of recurrence, although comparisons to placebo controls typically do not extend beyond the period of risk for relapse.[97,98] These studies indicate that CT has an enduring effect that is both efficacious and specific in the prevention of relapse and efficacious with respect to recurrence.
Studies also have shown that CBT can be added following initial medication treatment to prevent subsequent symptom return and that this enduring effect can last for up to several years.[100-103] Providing group CBT to remitted patients reduced risk for subsequent relapse or recurrence among patients with more prior episodes[104] and a similar moderated effect was found for acute CBT followed by brief psychoeducation (but not psychoeducation alone) for patients with four or more prior episodes.[105] An earlier trial by this latter group found no differences between a depression recurrence prevention program with or without CBT relative to usual care in a general practice sample.[106] The only studies that failed to find an enduring effect for CBT provided following remission compared it to continuation medication.[107,108]
Teasdale and colleagues have shown in two studies that training in mindfulness-based cognitive therapy (MBCT) can reduce risk for relapse or recurrence in patients initially treated with medications.[109,110] MBCT had its strongest preventive effects on patients with three or more prior episodes, a pattern of moderation that suggests that it may work through different mechanisms than standard CBT. A subsequent trial found MBCT more effective than maintenance medication in reducing residual depressive symptoms and improving quality of life; 75% of the MBCT patients in that trial were able to discontinue medications.[111] Differences in rates of relapse/recurrence favored MBCT but were not significant. Given that multiple sites were involved in one of the trials,[109] we consider MBCT to be efficacious in the prevention of relapse/recurrence.[110]
Combined treatment typically retains the specific benefits of either modality alone (more rapid or robust change for drugs versus more enduring change for CT), but differences in acute response relative to either monotherapy were not believed to be all that large.[112,113] However, more recent studies suggest a larger incremental effect; d=.25 relative to psychotherapy alone with an NNT = 7.14[114] and d=.31 relative to medications alone with an NNT of 5.75.[115] It was a recent trial by Keller and colleagues that renewed interest in combined treatment.[116] In that study, the combination of drugs (nefazodone) and a novel cognitive behavioral analysis system for psychotherapy (CBASP) targeted at interpersonal change and incorporating dynamic elements was more efficacious than either monotherapy in patients with chronic depression. Drugs worked best early on, while CBASP worked better late, and combined treatment retained the temporal advantages of each. This study suggests that CBASP is possibly efficacious in the treatment of chronic depression and there was no indication that meeting criteria for a personality disorder did anything to moderate the effects of treatment.[117] Continuing CBASP after recovery reduced risk for recurrence,[118] as does continuing CT with respect to relapse and recurrence.[119] These trials suggested that maintenance CBASP is possibly efficacious in the prevention of recurrence and that continuation CT is possibly efficacious in the prevention of relapse and recurrence. However, a subsequent effort at replication by several of the same investigators found that augmentation with CBASP was no more efficacious than individualized pharmacotherapy alone in chronic patients who failed to respond to three months of initial medication treatment.[120]
CBT was superior to sleep hygiene with respect to remission in both depression and insomnia when each was added to medication in the treatment of patients diagnosed with both MDD and insomnia[121] and superior to treatment-as-usual (often involving antidepressant medications) in the treatment of depression following coronary bypass surgery (especially among the two-thirds of the sample that met criteria for MDD).[122] Dozois and colleagues found that adding CT did little to enhance the efficacy of algorithm-driven pharmacotherapy in a small sample but did produce greater change in underlying cognitive structure.[123] Thompson and colleagues found that combined treatment was superior to medication alone in a geriatric sample with CBT alone intermediate and different from neither.[124] Laidlaw and colleagues found that geriatric patients treated with CBT alone were less likely to meet criterion for MDD than patients treated with treatment-as-usual including medication in a general practice setting.[125]
Cognitive therapy did not differ from medication as a second-step treatment for patients who did not respond to citalopram in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) project, although augmentation with medication resulted in significantly more rapid remission than augmentation with CT.[126] Rohan found CT comparable to light therapy and both superior to a wait list control in a sample of patients with seasonal affective disorder.[127] Strauman and colleagues found no overall differences between CT and their preferred self-system therapy (SST), although the latter was superior to CT for some patients.[128] Two studies have found that computer-assisted CT was as efficacious as therapist-administered CT with both superior to a wait list control.[129,130] Finally, as previously noted, a recent trial found REBT comparable to either CT or fluoxetine in the treatment of MDD and superior to continuation medication at a cross-sectional six month follow-up.[71] We are reluctant to categorize REBT as possibly efficacious with respect to acute response on the basis of null findings in a single trial or with respect to the prevention of relapse on the basis of cross-sectional assessment (since patients had ample time to relapse and subsequently remit in the interim) but note that the findings for REBT in this study were promising and merit further consideration.
On the whole, it appears that CBT (and especially CT) is as efficacious and specific as medications in the treatment of MDD,[75,76] although therapist competence may be an important moderating factor with more severe or complicated patients.[42,81] Early indications of general superiority to medications[66-68] or any specific inferiority among more severely depressed patients (the latter from the TDCRP) have not held up in subsequent trials in which each modality was adequately implemented.[69-71,75,76, 83] There are consistent indications that CT has an enduring effect that protects against subsequent relapse and possibly recurrence regardless of when it is applied[93-98,100-105] and indications that the same might be the case for MBCT.[109-111] This is especially important given the recurrent nature of depression and the fact that medications appear to have no lasting effect following treatment termination. Continuation/maintenance CT has been found to reduce risk for relapse/recurrence in MDD[119] and CBASP has been found to reduce acute distress[116] and subsequent recurrence when maintained in chronic MDD[118] in single studies and can be said to be possibly efficacious.
Behavior Therapy
Behavioral interventions include contextual approaches based on functional analyses (contingency management and behavioral activation), social skills training, self-control therapy, problem-solving therapy, and behavioral marital therapy. Although these approaches have not been tested as extensively as CBT, they have generally done well in controlled trials.[4] BT typically has been found to be superior to minimal treatment and at least as efficacious as other interventions, but studies in fully clinical populations have been few and comparison treatments sometimes suspect.
As previously described, McLean and Hakstian found a modest advantage for contingency management relative to drugs alone or brief dynamic psychotherapy,[14] but dosages were low and the dynamic intervention questionable. Hersen and colleagues found no differences between social skills training (SST) with or without medications and either amitriptyline alone or brief dynamic psychotherapy when each was adequately implemented.[17] Kornblith and colleagues found no differences between self-control therapy (SCT) and dynamic therapy,[18] whereas the addition of self-control therapy (SCT) enhanced response relative to usual care in a day-treatment program.[131]
Nezu and colleagues found problem-solving therapy (PST) superior to nonspecific or wait list controls in two studies with recruited adults,[132,133] as did Arean and colleagues in a geriatric sample.[134] Mynors-Wallis and colleagues found PST comparable to drugs and superior to placebo in one study in a general practice sample[135] and comparable to medications in another.[136] A large multicenter randomized trial by Dowrick and colleagues found PST superior to an assessment only control in reducing levels of depression in participants across five European countries.[137] These studies suggest in aggregate that PST is efficacious and possibly specific in the treatment of MDD. The fact that only one used a pill-placebo control in a bona-fide clinical sample reduces our confidence in this conclusion somewhat since nonspecific psychological controls are hard to implement in a convincing fashion and recruited samples reduce generalizability.
Behavior marital therapy (BMT) was as efficacious as CBT and superior to a wait list control in the treatment of depression in couples with marital distress.[138,139] A second study found BMT as efficacious as CBT in reducing depression for women with marital distress, but less efficacious than CBT for women without marital problems[140,141] and a third found no differences between the two on measures of depression.[142] These studies fall short of suggesting that BMT is possibly efficacious in the treatment of MDD since the first recruited patients with either major depression or dysthymia and the others had small sample sizes that limited the conclusions one could draw on the basis of null findings.[7] Nonetheless, BMT was more efficacious than CT in reducing marital distress in all three studies. A recent trial found coping-oriented couples therapy (COCT) that included many elements of behavioral marital therapy comparable to either CT or IPT in terms of the reduction of depressive symptoms but no better with respect to the resolution of marital distress.[143] However, this study suffered from a small sample size.
Despite these early successes, interest in BT stagnated before Jacobson and colleagues found that the behavioral activation component of CT produced as much change during acute treatment as the full treatment package,[144] with no differences in rates of subsequent relapse.[145] These findings were so unexpected that they led Jacobson and colleagues to conduct a placebo-controlled trial to compare a more comprehensive contextual version of behavioral activation (BA) against both CT alone and medications. In that trial, Dimidjian and colleagues found that BA and medications were comparably efficacious and each was superior to CT or pill-placebo in the treatment of more severely depressed patients.[81] Moreover, Dobson and colleagues found that among remitted patients, those previously treated with BA were no more likely to relapse following treatment termination than patients previously treated with CT or than patients kept on continuation medications and showed a marginal advantage relative to medication withdrawal with respect to both relapse and recurrence.[98] Had the effect been fully significant or the sample larger we would have been tempted to suggest that BA has an enduring effect with respect to the prevention of subsequent relapse or recurrence, but we are not prepared to go quite that far as yet. Nonetheless, these findings are promising in that respect and deserve to be followed up in future studies.
The fact that prior exposure to CT showed an enduring effect in Dobson and colleagues relative to withdrawal onto a pill-placebo for previously medicated patients goes along with findings from Hollon and colleagues to establish the specific efficacy of prior CT with respect to the prevention of subsequent relapse.[97,98] CT's poor performance with more severe and complicated patients was reminiscent of earlier findings from the TDCRP and may reflect the difficulties inherent when less experienced cognitive therapists try to implement a complicated treatment in a time-limited fashion.[146] That being said it is worth noting that BA encountered no such difficulties. Given that BA appears to be less complex and easier to learn than CT, this study has generated renewed interest in behavior therapy as a cost-effective alternative to medication in the treatment of MDD and another recent trial found behavioral activation superior to supportive psychotherapy in an inpatient sample.[147] Combined with the results from the earlier study by McLean and Hakstian,[14] these studies indicate that behavior activation is efficacious and specific in the treatment of MDD.
On the whole, these studies suggest that BT is efficacious and specific in the treatment of MDD. The evidence is most compelling for the contextual approaches (BA and contingency management) that have been tested against other efficacious interventions in fully clinical samples. [14,81,147] PST also met our criteria for being efficacious and specific, although the supporting studies come from recruited volunteers[132,134] or general practice samples.[135] BMT falls short of being possibly efficacious with respect to depression (although it is clearly efficacious for marital distress) since outcomes are mixed at best and the samples too small for equivalence to support efficacy.[138-143]
Experiential-Humanistic Psychotherapy
Although widely practiced in clinical settings, experiential-humanistic psychotherapy has been tested only rarely in the treatment of depression but has shown promise in recent trials. Beutler and colleagues found modest main effects for CBT and better response among resistant patients to a self-directed control but little specific benefit for a focused expressive psychotherapy based on Gestalt principles.[148] Greenberg and Watson found no difference between client-centered psychotherapy or a process-experiential therapy (PET) that incorporated gestalt principles on measures of depression, although PET produced greater change on measures of interpersonal processes and self-esteem.[149] Watson and colleagues similarly found no differences between PET and CT (adequacy unknown) on measures of depression, although PET again produced greater change on self-reports of interpersonal problems.[150] That same research group found emotion-focused therapy (EFT) superior to client-centered therapy (CCT)[151] and that responders to EFT were less likely to relapse over the next 18 months than responders to CCT.[152] This is the most promising trial in a rather limited literature and suggests that experiential therapy might be possibly efficacious with respect to both acute response and subsequent prevention.
Castonguay and colleagues added humanistic and interpersonal strategies to standard CT to repair ruptures in the working alliance and found this integrative approach superior to a wait list control in one study [153] and superior to standard CT in a second.[154] While the approach is not wholly experiential in nature and the studies relied on relatively inexperienced graduate student therapists, these findings do suggest that humanistic and interpersonal strategies might be a useful adjunct to CT.
Marital and Family Therapy
Marital and family problems are common in depression and may contribute to its etiology and complicate its treatment. Nonetheless, traditional marital and family therapies have been little studied in the treatment of depression. Friedman found that drugs were better than marital therapy in the reduction of acute distress, whereas marital therapy produced greater changes in the quality of relationships.[155] Clarkin and colleagues found that adding psycho-educational family therapy designed to reduce criticism of the patient enhanced response to standard inpatient treatment (including medication) among female patients (males actually did worse), but that only patients with bipolar disorders retained those gains.[156] Traditional marital and family therapy may have a role to play in the treatment of MDD, but the studies are too few and the findings too mixed to draw firm conclusions.
Summary
IPT, CBT (especially CT), and two different variants of BT (BA and maybe PST) are as efficacious as medications (even among more severely depressed patients) and specific in the treatment of MDD, although those findings may be conditioned upon therapist experience and patient characteristics (at least for CT). Results for dynamic and experiential-humanistic interventions are mixed (with later studies conducted by advocates rising to the level of possible efficacy) and marital and family therapies rarely tested. There are indications that IPT (and possibly BMT) may improve the quality of interpersonal relationships and that CT and MBCT (and possibly BA) have enduring effects (specific for CT) that last beyond the end of treatment and may extend to the prevention of recurrence. This suggests a greater breadth and stability of response than found for drugs and makes these interventions attractive alternatives or additions to medications. CBASP is possibly efficacious as an adjunct to medication in the treatment of chronic depression and preventive so long as it is maintained and continuation CT also appears to be possibly efficacious in the prevention of relapse and subsequent recurrence.
Dysthymic Disorder
As shown in Table 2, nine RCTs were identified that satisfied our inclusion criteria with respect to dysthymic disorder (DD). One evaluated dynamic psychotherapy and included a humanistic comparison condition, four evaluated IPT, and two each evaluated CBT and PST respectively. All but two involved comparisons to antidepressant medications.
Table 2.
Dysthymia (Adult and Geriatric)
| Study | Treatment/s | Number of Sessions | Control Condition/s | Age of subjects | Sample size | Diagnosis | Setting | Therapists' qualification | Results |
|---|---|---|---|---|---|---|---|---|---|
| Dynamic: | |||||||||
| Maina et al., 2005[157] | Brief dynamic therapy (BDT) vs brief supportive psychotherapy (BSP) | 15-30 weekly sessions | Wait list | Adults aged 18-60 | 30 assigned of whom 30 completed | DSM-IV NOS (50%); DD (30%); Adjust Dis (20%) | Outpatient clinic in university medical center | Two psychiatrists with personal training in psychodynamic psychotherapy | BDT and BSP both superior to wait list control at post-treatment (9 months) with BDT superior to BSP at 6-month follow-up |
| Interpersonal: | |||||||||
| Feijó de Mello et al 2001[159] | Interpersonal psychotherapy (IPT) and antidepressant medication (ADM) vs ADM alone | 16 weekly sessions during acute and 6 monthly boosters | None | Adults aged 18 to 60 | 35 assigned of whom 18 completed | DSM-IV dysthymia | Outpatient clinic at university medical center | Single psychiatrist | Adding IPT led to non-significant advantage over ADM alone |
| Browne et al 2002[160] | Interpersonal psychotherapy (IPT) vs antidepressant medication (ADM) vs combined treatment (IPT/ADM) | 12 hourly sessions over six months | None | Adults aged 18-74 | 707 assigned of whom 604 completed | DSM-IV dysthymia | Primary care clinic | Masters level counselors | Combined treatment no more efficacious than ADM alone and each better than IPT alone |
| Markowitz et al 2005[161] | Interpersonal psychotherapy (IPT) vs antidepressant medication (ADM) vs combined (IPT/ADM) | 16-18 sessions over 16 weeks | Brief supportive psychotherapy | Adults aged 18-60 | 94 assigned of whom 70 completed | DSM-IV dysthymia (early onset) | Outpatient research clinic at university medical center | Professional discipline unspecified | ADM alone or in combination better than either IPT or brief supportive psychotherapy control which did not differ |
| Markowitz et al 2008[162] | Interpersonal psychotherapy (IPT) | 16-18 sessions over 16 weeks | Brief supportive psychotherapy | Adults aged 18-60 | 26 assigned of whom 15 completed | DSM-IV dysthymia and DSM-IV substance abuse | Outpatient research clinic at university medical center | Doctoral level psychologists and masters-level social workers | IPT superior to brief supportive psychotherapy on self-reports of depression |
| Cognitive: | |||||||||
| Dunner et al 1996[166] | Cognitive behavior therapy (CBT) vs antidepressant medication (ADM) | 16 weekly sessions | None | Adults aged 18-60 | 31 assigned of whom 25 completed | DSM-III-R dysthymia | Outpatient research clinic | Doctoral level psychologists | No differences between the treatment conditions on measures of depression |
| Ravindran et al 1999[165] | Cognitive behavior therapy (CBT) vs antidepressant medication (ADM) vs combined (CBT/ADM) | 12 weekly 90-minute group sessions | Pill-placebo | Adults aged 21-54 | 97 assigned of whom 94 completed | DSM-III or DSM-IV dysthymia | Outpatient research clinic (recruited volunteers) | Professional discipline not specified | Combined treatment no more efficacious than ADM alone and each better than CBT or placebo |
| Behavioral: | |||||||||
| Barrett et al 2001[167] | Problem-solving therapy (PST) vs antidepressant medication (ADM) | 6 sessions over 11 weeks | Pill-placebo | Adults aged 18-59 | 241 assigned of whom 191 completed | DSM-IIIR dysthymia or minor depression | Primary care settings | Doctoral level psychologists trained in PST | ADM but not PST superior to pill-placebo on continuous measures whereas both ADM and PST beat placebo on rates of response |
| Williams et al 2000[168] | Problem-solving therapy (PST) vs antidepressant medication (ADM) | 6 sessions over 11 weeks | Pill-placebo control | Geriatric aged 60 and above | 415 assigned | DSM-IIIR dysthymia or minor depression | Primary care settings | Doctoral level psychologists, MSW social workers, and masters level counselors | ADM but not PST superior to pill-placebo |
Dynamic Psychotherapy
A recent trial found both brief dynamic therapy (BDT) and brief supportive psychotherapy (BSP) superior to a wait list control over nine months of acute treatment and BDT superior to BSP across a six-month follow-up in a sample of patients with less severe depression.[157] Only about a third of the sample met criteria for DD, so as to preclude drawing conclusions about the efficacy of BDT for this disorder.
Interpersonal Psychotherapy
IPT has been modified for DD by conceptualizing lifelong traits as chronic but treatable states.[158] Results have been mixed. Adding IPT produced a small but nonsignificant advantage relative to medications alone in the treatment of a small sample of dysthymic patients; most also met criteria for MDD.[159] A subsequent study found that IPT was less efficacious than drugs alone and did nothing to enhance efficacy when added in combination.[160] A third study found IPT less efficacious than medications and no more efficacious than a brief supportive control, although there was turnover from more to less experienced IPT therapists over the course of the study.[161] A fourth study found IPT more efficacious than brief supportive psychotherapy in a sample of dysthymic patients with secondary substance abuse or dependence.[162] This last study is sufficient to meet criteria for possible efficacy, but the bulk of this literature suggests that IPT is less efficacious than and adds little to drugs in the treatment of DD.
Cognitive Behavior Therapy
CBT has been adapted in recent years to deal with chronic problems like dysthymia and underlying personality disorders,[163] but has yet to be formally tested. Similarly, recent work by McCullough developing CBASP for patients with chronic depression will likely have relevance for patients with dysthymia as well.[164] These developments are noteworthy because conventional CBT did little to enhance the efficacy of medications and did not separate from placebo in one study with a large sample[165] and did not differ from medications in another smaller trial.[166]
Behavior Therapy
Two studies with largely overlapping protocols have explored the effectiveness of problem-solving therapy (PST) in the treatment of dysthymia. In each, six sessions of PST was compared to antidepressant medication in the context of a pill-placebo control in samples that included patients who met criteria for either dysthymia or minor depression. Barrett and colleagues found no differences between the three conditions in reducing depressive symptoms although both PST and medication treatment produced greater rates of response than did pill-placebo in an adult sample under the age of 60.[167] Williams and colleagues found medications but not PST superior to pill-placebo in a geriatric sample over the age of 60.[168] Neither study provides much support for PST in primary care, although session number was quite low (only six sessions).
Summary
Efforts to modify existing interventions for use with dysthymia are relatively recent and show mixed results at best. One would think that the same interventions that are efficacious for MDD also would prove to be of use with dysthymia, but results to date have not been encouraging, although IPT may be considered possibly efficacious for the treatment of DD. It should be noted that few of the trials testing IPT or CBT were conducted by investigators expert in those approaches (Markowitz being the sole exception) and that the studies involving PST compared a very limited number of sessions to full-dose medication. Whether subsequent studies will provide greater support for those interventions remains to be seen, but neither the studies that have been conducted to date nor the results they obtained have been all that impressive.
Bipolar Disorder
Whereas the psychosocial interventions represent a viable alternative to drugs in the treatment of MDD, they have only recently begun to be explored as adjuncts to medication in bipolar patients. There is little evidence that the psychosocial interventions can forestall the onset of manic episodes (with the possible exception of psychoeducation intended to enhance medication adherence) and mood stabilizers like lithium and the anticonvulsants remain the standard of treatment.[169] Nonetheless, in the face of growing evidence that drugs are less than wholly adequate, there has been increased interest in adapting psychosocial interventions to the treatment of bipolar disorder. These efforts have focused on the newer interpersonal, cognitive-behavioral, and family-focused interventions, as well as psychoeducation. As shown in Table 3, fifteen RCTs satisfied our inclusion criteria with respect to BD, including three for psychoeducation (PE), two for IPT, eight for CBT, three for family-focused therapy (FFT). These studies are sometimes hard to categorize, since patients may or may not be in episode at the time of randomization (making it difficult to determine whether the trial is focused on acute treatment or subsequent prevention) and cumulative episode onset often is analyzed over the course of several years (making it hard to separate relapse from recurrence). Moreover, only some of the studies report separate analyses as a function of polarity and talk instead of bipolar episodes (making it hard to tell whether treatment effects pertain to mania or depression). With those caveats in mind we review the relevant studies.
Table 3.
Bipolar Disorder (Adult and Geriatric)
| Study | Treatment/s | Number of Sessions | Control Condition/s | Age of subjects | Sample size | Diagnosis | Setting | Therapists' qualification | Results |
|---|---|---|---|---|---|---|---|---|---|
| Psychoeducation: | |||||||||
| Perry et al 1999[170] | Patient education (PE) added to routine care with most but not all on medication | 7-12 sessions | Routine care with most but not all on medication | Adults aged 18-75 | 69 assigned of whom 68 completed | DSM-III-R bipolar disorder I or II remitted with at least one relapse in last year | NHS mental health services | Research psychologists | PE significantly decreased number of subsequent manic but not depressive episodes, improved social functioning, and increased performance at work |
| Colom et al 2003[171] | Group patient education (PE) added to routine care including medication | 21 90-minute weekly sessions | Unstructured groups added to routine care including medication | Adults aged 18-65 | 120 of whom 97 completed | DSM-IV bipolar I or II disorder euthymic last six months and no comorbidity | University hospital clinic | Experienced psychologists | PE reduced recurrence rates for depression and mania/hypomania and number of times patients were hospitalized |
| Colom et al 2009[172] (5-year follow-up) | PE reduced recurrence within bipolar II patients considered as subgroup | ||||||||
| Reinares et al 2008[173] | Patient education (PE) for caregivers added to treatment as usual with medication | 12 90-minute sessions | Treatment as usual with medication | Adult caregivers of medicated bipolar patients | 113 assigned | DSM-IV bipolar disorder I and II euthymic last three months and living with caregiver | University based research clinic | Research psychologists | PE provided to caregivers reduced rates of relapse/recurrence with respect to mania/hypomania but not depression |
| Interpersonal: | |||||||||
| Frank et al 2005[175] | Medication plus either interpersonal social rhythm therapy (IPSRT) or intensive clinical management (ICM) during acute phase with patients either continued on same or switched to other during maintenance | Weekly during acute phase until stabilized for four weeks and monthly thereafter during 2-year maintenance | None | Adults aged 18-60 | 175 assigned of whom 125 achieved stabilization and entered maintenance phase and 93 completed all treatment | RDC/DSM-IV Bipolar I (manic, depressed, or mixed) with 9% schizoaffective manic subtype | Outpatient research clinic in university medical center | Social workers, nurses, and psychologists | Time to stabilization did not differ during acute treatment but patients who received IPSRT during acute phase went longer without new episodes than patients who received ICM regardless of what they received during the maintenance phase |
| Miklowitz et al 2007[177] | Medication plus either interpersonal and social rhythm therapy (IPSRT), cognitive behavior therapy (CBT) or family-focused therapy (FFT) | Up to 30 sessions across 9 months | Medication plus collaborative care (3 sessions across 6 weeks) | Adults aged 18 and above | 293 assigned of whom 195 completed study year | DSM-IV bipolar disorder (I or II) with current MDE | Fifteen outpatient clinics participating in STEP-BD program | Therapists of unspecified background who completed six hour workshops in the respective modalities | Pooled intensive treatments superior to collaborative care in terms of recovery with no differences between treatments and no specific comparisons to collaborative care |
| Cognitive: | |||||||||
| Cochrane 1984[178] | Cognitive therapy added to lithium (CT/L) vs lithium alone (L) | 6 weekly 1 hour sessions | None | Adults aged 24-60 | 28 assigned of whom 26 completed | RDC Bipolar I or II and stable | Outpatient research clinic | Pre-doctoral clinical psychologists | Adding CT to L enhanced drug compliance and reduced hospitalizations |
| Lam et al., 2000[183] | Cognitive therapy added to mood stabilizer medication (CT/MSM) vs mood stabilizer medication alone (MSM) | 12-20 sessions | None | Adults aged 18-65 | 25 assigned of whom 23 completed | DSM-IV Bipolar I (currently euthymic) | Outpatient research clinic in university medical center | Experienced clinical psychologists | Adding CT to medications led to fewer bipolar episodes and improved social functioning relative to medications alone |
| Scott et al 2001[186] | Cognitive therapy (CT) added to treatment as usual (93% on mood stabilizers) | Up to 25 sessions over 6 months | Treatment as usual and CT waiting-list | Adults with mean age in late 30's | 42 assigned of whom 33 completed | Bipolar I or II disorder (about 40% in episode most depression) | Outpatient research clinic | Experienced therapists with expertise in CT for mood disorders (first two authors) | Adding CT to treatment as usual reduced depressive symptoms and improved global functioning |
| Lam et al., 2003[184] | Cognitive therapy added to mood stabilizer medication (CT/MSM) vs mood stabilizer medication alone (MSM) | 12-18 sessions over 1st six months and 2 boosters over 2nd six months | None | Adults aged 18-70 | 103 assigned of whom 87 completed | DSM-IV Bipolar I in full or partial remission with at least two episodes in last two years | Outpatient research clinic in university medical center | Doctoral level clinical psychologists (minimum 5 years experience) | Adding CT to medications led to fewer bipolar episodes and improved social functioning relative to medications alone |
| Lam et al 2005[185] | Subsequent 18-month follow-up sans CT | CT gains extend over subsequent 18-month follow-up but with no indication of effect on recurrence prevention | |||||||
| Ball et al 2006[181] | Cognitive therapy with emotive techniques added (CT) plus mood stabilizers | 20 weekly sessions over 6 months | Treatment as usual (TAU) plus mood stabilizers | Adults | 52 assigned | DSM-IV Bipolar Disorder I or II in full or partial remission | Outpatient research clinic | CT reduced levels of depression and rates of relapse (trend) relative to TAU | |
| Scott et al 2006[186] | Cognitive-behavioral therapy (CBT) plus treatment as usual with medication | 20 sessions weekly through week 15 and less frequently until week 26 with two subsequent booster sessions | Treatment as usual with medication | Adults aged 18 and above | 253 assigned of whom 200 completed | DSM-IV Bipolar Disorder I or II with about a third currently in episode (mostly depressed) | Outpatient clinics (x5) including teaching and nonteaching | Therapists profession unspecified with 1-year post-qualification training in CBT with additional 3 months training in CBT for bipolar disorder | Adding CBT did not enhance response to treatment as usual including medications across whole sample; number of prior episodes moderates effects of CBT in post hoc analysis (CBT better for less and worse for more) |
| Zaretsky et al 2008[182] | Cognitive behavior therapy added to patient education plus mood stabilizer medication (CBT/PE/MSM) vs patient education plus mood stabilizer medication alone (PE/MSM) | 14 sessions of CBT added to 6 sessions of PE vs 6 sessions of PE alone over 20 weeks in patients on mood stabilizer followed twelve months | None | Adults aged 18-60 | 79 assigned of whom 53 completed treatment and 46 completed 12-month follow-up | Bipolar I (66%) or II (34%) in full or partial remission | University teaching hospital | Therapists not specified | Participants who received CBT had reduced depressive symptoms, 50% fewer depressed days, and fewer medication increases |
| Family: | |||||||||
| Miklowitz et al 2000[189] Miklowitz et al 2003[190] |
Family-focused therapy (FFT) vs crisis management (CM) in medicated patients | 21 hourly sessions (12 weekly/ 6 biweekly/ 3 monthly) | None | Adults aged 18-62 | 101 assigned of whom 78 completed | DSM-III-R Bipolar I recently hospitalized and partially stable | Outpatient research clinic | Doctoral, masters', and bachelors level psychologists | FFT led to fewer relapses and fewer depressed symptoms than CM (crisis management) in medicated patients |
| Rea et al., 2003[191] | Family-focused therapy (FFT) vs individual focus therapy (IFT) in medicated patients | 21 sessions (12 weekly/ 6 biweekly/ 3 monthly) over 9 months of one year active treatment with subsequent one year follow-up | None | Adults aged 18-46 | 53 assigned | DSM-III-R Bipolar I manic type recently hospitalized and partially stable | Outpatient research clinic | Professional discipline not specified | No differences in time to first relapse but FFT led to fewer total relapses when multiple relapses considered and fewer recurrences during post-treatment follow-up; fewer FFT patients hospitalized overall but differences largely due to post-treatment follow-up |
| Miller et al 2004[187] | Medication alone or in combination with family therapy (FT) or multi-family psychoeducational group therapy (MFPE) | FT: mean 12 (SD 13) sessions MFPE: 6 sessions | None | Adults aged 18-65 | 92 assigned of whom 60 completed | DSM-III-R bipolar I disorder mostly manic and all in acute episode | University-affiliated psychiatric hospital | Social workers and doctoral level psychologists | Adding family therapy did not enhance the efficacy of medications |
Psychoeducation
Adding simple psychoeducation (PE) in which patients are trained to identify prodromes and to seek prompt treatment was found to reduce risk for relapse/recurrence with respect to mania but not depression over routine care in a sample of patients who had relapsed within the previous year.[170] A subsequent study in a sample of euthymic patients past the period of risk for relapse essentially replicated these findings relative to recurrence with respect to mania and hypomania and also found evidence of prevention with respect to depression relative to an unstructured nonspecific support group[171] and a subsequent reanalysis found that these results held even among the small subset of bipolar II patients across a five-year follow-up.[172] Providing PE to caregivers of euthymic patients with BD who had been euthymic for the last three months resulted in lower rates of relapse/recurrence with respect to mania and hypomania, but not depression.[173] These studies suggest that PE is efficacious as an adjunct to medications for the prevention of subsequent episodes of mania and hypomania in BD. Since patients in all three studies were euthymic at the time of entry it is not possible to tell whether PE had an impact on the reduction of acute distress. Moreover, since not all patients had been euthymic long enough (at least six months) at study entry to be past the point of risk for relapse and since the analyses typically aggregated cumulative episodes across time (the study by Colom and colleagues being the exception in both respects), it was difficult to distinguish between relapse and recurrence in these trials. Therefore, we are inclined to conclude that PE is efficacious in the prevention of undifferentiated relapse/recurrence with respect to mania/hypomania in the treatment of BD (with the study by Colom and colleagues suggesting that this effect might be specific relative to controls and fully evident with respect to recurrence)[170,171,173] and possibly efficacious in the prevention of recurrence in depression (the latter based solely on Colom and colleagues).[171]
Interpersonal Psychotherapy
Frank and colleagues modified IPT to serve as an adjunct to drugs in the treatment of BD based on the notion that social interactions (social Zeitgebers) provide order in daily life and to help maintain affective stability.[174] Activity scheduling and efforts to regularize sleep were added to conventional IPT to produce a hybrid intervention called interpersonal social rhythms therapy (IPSRT). Frank and colleagues found no differences between IPSRT and intensive clinical management (ICM) in the time it took to stabilize symptoms (patients could be depressed, manic, or mixed), but did find that patients who received IPSRT during acute treatment went longer without another episode of mood disturbance during a subsequent two-year maintenance phase, regardless of whether they were kept on IPSRT or switched to ICM.[175] Additionally, more regularized social rhythms over acute treatment predicted lower risk for recurrence during maintenance, suggestive of mediation. Given that half of the recurrences involved manic (31%) or mixed episodes (19%) it would appear that any preventive effect for acute phase IPSRT was not limited to depression. Two things are important to note. First, despite its name, ICM was not all that different from the standard clinical management typically provided as part of pharmacotherapy in the unipolar literature. Although implemented by the same therapists as IPSRT, ICM involved only about half as much contact time and focused largely on issues related to medication management. Therefore, we do not consider it sufficient to speak to specificity. Second, although patients in this trial were said to enter maintenance treatment and to be at risk for recurrence after four weeks of stabilization, the convention in the literature is to refer to the first several months of treatment following remission as continuation treatment (rather than maintenance) and to view patients as being at risk for relapse (the return of the treated episode) rather than recurrence (the onset of a wholly new episode).[176] We therefore are prepared to say that IPSRT is possibly efficacious in the prevention of relapse/recurrence with respect to bipolar episodes, but cannot differentiate between relapse and recurrence or mania and depression in this study.
A subsequent effectiveness study compared up to 30 sessions of IPSRT (or CBT or FFT) across 9 months to an abbreviated collaborative care (three sessions across six weeks) in a sample of medicated bipolar patients (I or II) who all met criteria for current major depressive episode as part of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD).[177] The three intensive psychotherapies pooled were superior to collaborative care in terms of both time to recovery and proportion of patients recovered and there were no differences among the intensive treatments. Although not reported in the published article, the authors did find that both IPSRT and FFT (but not CBT) were superior to collaborative care in post hoc analyses that did not control for multiple comparisons (Miklowitz, personal communication, December 2009). Given the brevity of the collaborative care condition, it is not clear that this study can be used to speak to specificity, since it provided only minimal control for nonspecific factors, but it is interesting that the results observed were achieved with relatively minimal training and low-intensity supervision (that is why the trial is classified as an effectiveness and not an efficacy study). On the whole, we are prepared to say that IPSRT is possibly efficacious as an adjunct to medication in the acute treatment of depression in BD.
Cognitive Behavior Therapy
As for IPT, there is growing interest in adapting CBT for the treatment of bipolar disorder. One early study found that CBT could be used to enhance adherence to medication and reduce rates of hospitalization but did not find a difference with respect to the frequency of affective episodes.[178] More recent work also has focused on regularizing everyday routines and coping with negative life events.[179] In an early pilot study, adding CT to treatment-as-usual (which in most cases involved mood stabilizers and psychiatric support) improved global functioning and reduced depressive symptoms in a group of patients with bipolar disorder heterogeneous with respect to current affective state.[180] The addition of CT plus emotive techniques to mood stabilizer medication reduced levels of depression and delayed depressive relapse at the level of a nonsignificant trend in an Australian study[181] and adding CBT to PE in bipolar patients currently stabilized on medications resulted in reduced symptom levels, 50% fewer days spent depressed, and fewer medication increases in a Canadian study.[182] All three studies speak to the efficacy (but not the specificity) of CBT with respect to the reduction of depressive symptoms; although suggestive, none provides sufficient data to speak directly to the prevention of subsequent relapse. As previously noted, CBT (unlike IPSRT and FFT) did not differ from a less intensive collaborative care in the treatment of depression in bipolar patients stabilized on medications in the STEP-BD project.[177]
In another early pilot trial, Lam and colleagues found that adding six months of CT to ongoing medication treatment reduced hospitalizations and the occurrence of bipolar episodes across the course of a year and improved residual functioning in a sample of bipolar I patients not currently in acute episode.[183] A subsequent study in a larger sample found that adding CT to medications both reduced residual depression across the course of treatment and essentially replicated the findings from the pilot study just described with respect to the prevention of bipolar relapse (in this larger sample differences were significant with respect to both depressive and manic episodes) and hospitalizations.[184] Although gains associated with CT were maintained across a subsequent 18-month follow-up (for depressive episodes but not for mania), there was no indication that prior CT had any additional preventive effect on subsequent recurrence.[185] Given that both studies were done by the same group, they suggest that CT is possibly efficacious as an adjunct to medications in prevention of relapse/recurrence for bipolar episodes, but that those effects were limited with respect to mania (relapse only) and recurrence (differences with respect to depression were maintained but not enhanced across the extended follow-up suggesting that most of the effect was concentrated during the period of risk for relapse). It should be noted that what differentiated this study from others in the literature was that separate analyses were conducted with respect to both relapse and recurrence and both mania and depression; it is not clear that those other trials would have found a separate effect for recurrence over and above what they found for relapse had separate analyses been conducted.
However, in the largest trial to date in this literature, Scott and colleagues found that adding CBT provided no additional benefit over treatment-as-usual including medication in a sample of bipolar patients heterogeneous with respect to whether they were currently euthymic or in episode other than mania.[186] Post hoc analyses did find a moderating effect for number of prior episodes, with CBT doing better than treatment-as-usual for patients with fewer prior episodes and worse for patients with more, although no specific tests of significance were conducted within those patient subgroups. Unlike the earlier trials by Lam and colleagues, which were largely restricted to euthymic patients currently stabilized on medications, about a third of the patients in Scott et al. were in episode at the time of randomization. This might have contributed to the differences in findings between the trials, something that Scott and colleagues could have addressed by conducting secondary analyses restricted to patients similar to those found in the earlier Lam studies. It is also possible that treatment was more competently implemented in those earlier trials, as therapists in the study by Scott and colleagues were unable to get through the full course of CBT with about 40% of the patients. As was the case for both IPT and CBT in the treatment of MDD, the literature points to efficacy in the acute treatment[180-182,184] and prevention of bipolar disorder (particularly with respect to depressive symptoms),[183,184] but a major study exists with findings to the contrary.[186]
Marital and Family Therapy
Traditional family therapy has not fared well as an adjunct to medication in the treatment of bipolar disorder.[187] However, one of the more promising innovations in the treatment of bipolar disorder has been the adaptation of a family-focused therapy (FFT) originally developed to reduce the high levels of expressed emotion (criticism) in families of schizophrenic patients.[188] As previously noted, the multi-center STEP-BD program found that FFT was superior to a less intensive collaborative care control in the treatment of depression in medicated bipolar patients.[177]
A nine-month course of FFT has been shown to reduce depressive symptoms and risk for relapse through twelve months relative to a less intensive crisis management intervention in a sample of medicated bipolar patients recruited shortly after an illness episode (predominantly manic or mixed).[189] The benefits of FFT extended across a second follow-up year to the prevention of recurrence with respect to both depression and mania, with the latter mediated by enhanced compliance with the medication regime.[190] A subsequent study found that a similar nine-month course of FFT did not differ from individually-focused treatment matched for frequency and duration of contact (but not session length) across a one-year medication treatment phase but did reduce rates of recurrence and hospitalization across a subsequent one-year post-treatment follow-up.[191] The fact that differences favoring FFT did not emerge until after the end of active treatment suggests that nonspecific factors may be sufficient to protect against relapse and enhance medication compliance during active treatment but that the specific benefits provided by a skills-training approach like FFT do not become evident until after the end of treatment. Both studies speak to the efficacy of FFT (as does STEP-BD)[177] and the second speaks in part to its specificity.[191] FFT can be said to be efficacious in the reduction of depressive symptoms[177,189] and efficacious (and enduring) in the prevention of subsequent relapse/recurrence in BD.[189-191]
Summary
Several of the newer psychosocial interventions including PE, IPSRT, CBT, and FFT appear to be useful adjuncts to medication in the treatment of BD. All focus on maintaining regular schedules and all seek to reduce interpersonal conflicts that can trigger episode onset. Controlled trials are still few in number and the evidence for preventive effects with respect to mania or hypomania is most clear for PE, but it does appear that the others each enhance the efficacy of drugs in the treatment of depressive symptoms and the prevention of relapse and recurrence. Given the chronic and episodic nature of BD and the disability that it can cause, any such indications are most welcome.
DISCUSSION
As shown in Table 4, IPT,[41,42,45,49] CBT (especially CT),[75,76] and at least two variants of BT (BA[14,81,147] and maybe PST[132,134,131]) meet the Chambless and Hollon criteria for being efficacious and specific in the treatment of MDD.[7] In most instances these conclusions are based on placebo-controlled comparisons to medication or other bona fide therapies and not simply comparisons to nonspecific psychological control conditions that lack credibility to both patients and therapists.[192] All appear to be comparable to drugs in the hands of experienced therapists and to enhance the efficacy of medications when added in combination (including CBASP for chronic depression[116]). There was little support for more traditional dynamic, experiential-humanistic, or marital and family approaches in the treatment of MDD in the older literature, but more recent studies by investigators expert in the respective approaches have been more encouraging with respect to the short-term dynamic[21] and experiential-humanistic psychotherapies.[151] CBT[96-98] and MBCT[109-111] appear to have enduring effects that prevent subsequent relapse and possibly recurrence following treatment termination (with CBT specific)[97,98] and the same may be true for BDT[28] and EFT[152] although the evidence is scant for each. In a chronic recurrent disorder in which current practice now calls for keeping patients on medications indefinitely, this is a boon that could lead to major cost savings. Early trials provide little support for the efficacy of psychotherapy in the treatment of DD, although a recent study suggests that IPT is possibly efficacious.[162] As adjuncts to medication in the treatment of BD, CBT[180-182,184] and FFT[177,189,190] are efficacious with respect to the reduction of depressive symptoms (with IPSRT possibly efficacious[177]) and FFT efficacious with respect to the prevention of subsequent relapse and perhaps recurrence[189-191] (with IPSRT[175] and CBT[183-185] possibly efficacious), with PE efficacious in the prevention of mania/hypomania[170,171,173] and possibly depression.[171]
Table 4.
Empirically supported psychological therapies for the treatment of and the prevention of relapse or recurrence in the mood disorders: Categorizations are based on 1998 Chambless & Hollon criteria[7]
| Mood disorder | Level of support | Therapy | Evidence |
|---|---|---|---|
| Major depressive disorder (MDD) | Efficacious and specific | Interpersonal psychotherapy for the treatment of MDD | Elkin et al (1989/1995)[41,42] Spinelli & Endicott (2003)[45] But see also: Reynolds et al (1999)[57] Luty/Joyce et al (2007)[46,47] Marshall et al (2008)[48] |
| Cognitive behavior therapy for the treatment of MDD | Jarrett et al (1999)[75] DeRubeis et al (2005)[76] But see also: Dimidjian et al (2006)[81] Elkin et al (1989/1995)[41,42] |
||
| Problem-solving therapy for the treatment of MDD | Nezu (1986)[132] Arean et al (1993)[134] Mynors-Wallis et al (1995)[135] |
||
| Behavioral activation/contingency management for the treatment of MDD | McLean & Hakstian (1979)[14] Hopko et al (2003)[147] Dimidjian et al. (2006)[81] |
||
| Prior cognitive behavior therapy to prevent relapse in MDD (efficacious but not specific with respect to recurrence) | Hollon et al (2005)[97] Dobson et al (2008)[98] But see also: Shea et al (1992)[99] |
||
| Efficacious | Mindfulness-based cognitive therapy to prevent relapse/recurrence in MDD | Teasdale et al (2000)[109] Ma & Teasdale (2004)[110] Kuyken et al (2008)[110] |
|
| Possibly efficacious | Dynamic psychotherapy for the treatment of MDD | Cooper et al (2003)[21] | |
| Prior dynamic psychotherapy to prevent recurrence in MDD | Maina et al (2009)[28] | ||
| Maintenance interpersonal psychotherapy to prevent recurrence in MDD | Frank et al (1990)[59] Reynolds et al (1999)[61] But see also: Reynolds et al (2006)[62] |
||
| Continuation cognitive therapy to prevent relapse/recurrence in MDD | Jarrett et al (2001)[119] | ||
| CBASP for the treatment of chronic MDD | Keller et al (2000)[116] But see also: Kocsis et al (2009)[120] |
||
| Maintenance CBASP to prevent recurrence in chronic MDD | Klein et al (2004)[118] | ||
| Emotion-focused therapy for the treatment of MDD | Goldman et al (2006)[151] | ||
| Emotion-focused therapy to prevent relapse in MDD | Ellison et al (2009)[148] | ||
| Dysthymic disorder (DD) | Possibly efficacious | Interpersonal psychotherapy for the treatment of DD | Markowitz et al (2008)[158] But see also: Browne et al (2002)[160] Markowitz et al (2005)[161] |
| Bipolar disorder (BD) | Efficacious | Psycho-education as an adjunct to medication to prevent manic/hypomanic relapse/recurrence in BD | Perry et al (1999)[170] Colom et al. (2003)[171] Reinares et al (2008)[173] |
| Cognitive behavior therapy as an adjunct to medication for the treatment of depression in BD | Ball et al (2006)[181] Scott et al (2001)[180] Lam (2003)[184] Zaretsky et al (2008)[182] |
||
| Family-focused therapy as an adjunct to medication for the treatment of depression in BD | Miklowitz et al (2000/2003)[189,190] Miklowitz et al (2007)[177] |
||
| Family-focused therapy as an adjunct to medication to prevent relapse/recurrence in BD | Miklowitz et al (2000/2003)[189,190] Rea et al (2003)[191] |
||
| Possibly efficacious | Psycho-education as an adjunct to medication to prevent depressive recurrence in BD | Colom et al. (2003)[171] | |
| Interpersonal and social rhythm therapy as an adjunct to medication for the treatment of depression in BD | Miklowitz et al (2007)[177] | ||
| Interpersonal and social rhythm therapy as an adjunct to medication to prevent relapse/recurrence in BD | Frank et al (2005)[175] | ||
| Cognitive behavior therapy as an adjunct to medication to prevent relapse/recurrence in BD | Lam et al (2000)[183] Lam et al (2003/2005)[184,185] But see also: Scott et al (2006)[186] |
Our findings are consistent with and build upon those of earlier reviews that used similar criteria. DeRubeis & Crits-Christoph determined that CBT was efficacious and specific in the treatment of MDD and that both IPT and BA were efficacious and PST possibly efficacious.[8] Numerous studies regarding MDD have been published since the time of their review and they covered neither dysthymia nor bipolar disorder. Chambless and Ollendick updated that review and included bipolar patients, but did not include dysthymia.[9] Roth & Fonagy included all the mood disorders but did not differentiate between treatments that were efficacious and specific from those that were simply efficacious.[193] They found evidence for the efficacy of both IPT and CBT for MDD and limited support for short-term psychodynamic psychotherapy. They also concluded that psychotherapy was less efficacious than medications alone in the treatment of dysthymia and noted some support for the efficacy of IPSRT, CBT, FFT, and PE as adjuncts to medication in bipolar disorder. None of these reviews provided separate classifications with respect to acute response and prevention of relapse and recurrence. Our conclusions also are largely consistent with those reached by the National Institute for Clinical Excellence (NICE) in England, although we are somewhat more positive about the dynamic and experiential/humanistic approaches based on our reading of recent trials.[194]
The bulk of the RCTs of psychological interventions for mood disorders included in this review evaluated the efficacy of newer interpersonal or cognitive behavioral treatments. We still know little regarding the efficacy of more traditional dynamic or experiential-humanistic approaches and neither was always implemented adequately in those few studies that have been done. Absence of empirical support for these approaches does not necessarily mean that they offer no benefit to patients suffering from mood disorders, but further research is required to determine whether or not they do. [195]
It is especially important that these studies be done by research groups that include experts in the implementation of those interventions and that is starting to be the case. Quality of implementation of the respective interventions is perhaps the biggest source of variance with respect to outcomes in the literature and a major reason why we prefer the minimum number of positive studies approach adopted by the FDA to more conventional meta-analyses to summarize the literature. Those interventions like IPT or CBT that have been more extensively tested can survive the occasional study in which they are less than adequately implemented, but leaving research solely in the hands of advocates of other approaches has been a major problem for the more traditional dynamic and experiential-humanistic interventions. Absence of evidence is not necessarily evidence of absence with regard to efficacy, but absence of evidence will likely lead to absence of inclusion in any third-party or single-payer health care systems. RCTs are far from perfect and care must be used in interpreting their results (especially with respect to the adequacy of implementation of the respective interventions), but they represent the “gold standard” for drawing causal inferences regarding treatment efficacy. Advocates for the more traditional interventions avoid their use at the peril of their preferred interventions.
Finally, two recent meta-analytic reviews suggest that severity moderates the effects of both psychotherapy and medication treatment in a surprisingly similar fashion among non-bipolar patients. In placebo-controlled medication trials, “true” drug effects (drug-placebo differences) were negligible among patients with less severe depressions (with effect sizes less than d=.20 and NNTs greater than 10) but grew in magnitude as severity increased (with effect sizes greater than d=.50 and NNTs less than 4).[196] Given that over half the patients who meet criteria for MDD fall on the “less severe” end of the severity continuum, this suggests that many patients for whom medications are prescribed derive no real “pharmacological” benefit from taking them. That is, when such patients improve (as they often do), they do so largely for nonspecific psychological reasons.
What is even more surprising is that the same appears to be the case for psychological treatments. When different types of psychotherapies prove to be superior to nonspecific controls (whether pill-placebos or nonspecific psychotherapy controls) such differences are only apparent among more severely depressed patients.[197] Among randomized controlled trials with nonspecific controls that have tested for moderation, MDD patients with less severe depression show effect sizes that are small at best (d=.22; NNT = 8.06) whereas MDD patients with more severe depressions show effect sizes that are considerably larger (d=.63; NNT = 2.91). What this suggests is that nonspecific processes may be sufficient to produce change among patients with less severe depressions but that specific mechanisms that go beyond the simple provision of contact with a therapist and the expectation of change may be required for patients with more severe depressions.
These findings may have implications for mental health policy. It may be the case that many patients with less severe (or chronic) depressions can be adequately treated by less expert therapists using generic psychological interventions (as opposed to medications with their attendant side effects), whereas treatments with specific effects (whether pharmacological or psychotherapeutic) conducted by more expert therapists may be required for patients with more severe (or chronic) depressions or bipolar disorder. Moreover, given that CBT and possibly BA have enduring effects and IPT greater breadth of effect not found for medications and that neither appears to depend upon patient severity or chronicity, it may be wise to choose one of these approaches as the first line of treatment (rather than medications) as is currently being done in England.[198]
ACKNOWLEDGEMENTS
This work was supported by Grant 1003551 to Myrna M. Weissman from the Josiah Macy Jr. Foundation and Independent Scientist Award MH01697 to Steven D. Hollon from the National Institute of Mental Health.
REFERENCES
- 1.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS, the National Comorbidity Survey Replication The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. DSM-IV. [Google Scholar]
- 3.Murray CJL, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 4.Hollon SD, Thase ME, Markowitz JC. Treatment and prevention of depression. Psychol Sci Pub Int. 2002;3:39–77. doi: 10.1111/1529-1006.00008. [DOI] [PubMed] [Google Scholar]
- 5.Hollon SD, Stewart MO, Strunk D. Cognitive behavior therapy has enduring effects in the treatment of depression and anxiety. Ann Rev Psychol. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. 2006. [DOI] [PubMed] [Google Scholar]
- 6.Olfson M, Marcus SC, Druss B, et al. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–209. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- 7.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- 8.DeRubeis RJ, Crits-Christoph P. Empirically supported individual and group psychological treatments for adult mental disorders. J Consult Clin Psychol. 1998;66:37–52. doi: 10.1037//0022-006x.66.1.37. [DOI] [PubMed] [Google Scholar]
- 9.Chambless DL, Ollendick TH. Empirically supported psychological interventions: Controversies and evidence. Ann Rev Psychol. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- 10.Cuijpers P, van Straten A, Andersson G, et al. Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. J Consult Clin Psychol. 2008;76:909–922. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- 11.Cuijpers P, van Straten A, Warmerdam L, et al. Characteristics of effective psychological treatments of depression: A metaregression analysis. Psychother Res. 2007;18:225–236. doi: 10.1080/10503300701442027. [DOI] [PubMed] [Google Scholar]
- 12.Ponniah K, Hollon SD. Empirically supported psychological interventions for social phobia in adults: A qualitative review of randomized controlled trials. Psychol Med. 2008;38:3–14. doi: 10.1017/S0033291707000918. [DOI] [PubMed] [Google Scholar]
- 13.Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: A review. Dep Anx. 2009;26:1086–1109. doi: 10.1002/da.20635. [DOI] [PubMed] [Google Scholar]
- 14.McLean PD, Hakstian AR. Clinical depression: comparative efficacy of outpatient treatments. J Consult Clin Psychol. 1979;47:818–836. doi: 10.1037//0022-006x.47.5.818. [DOI] [PubMed] [Google Scholar]
- 15.Covi L, Lipman RS, Derogatis LR, et al. Drugs and group psychotherapy in neurotic depression. Am J Psychiatry. 1974;131:191–198. doi: 10.1176/ajp.131.2.191. [DOI] [PubMed] [Google Scholar]
- 16.Covi L, Lipman RS. Cognitive behavioral group psychotherapy combined with imipramine in major depression: a pilot study. Psychopharmacol Bull. 1987;23:173–176. [PubMed] [Google Scholar]
- 17.Hersen M, Bellack AS, Himmelhoch JM, Thase ME. Effects of social skill training, amitriptyline, and psychotherapy in unipolar depressed women. Behav Ther. 1984;15:21–40. [Google Scholar]
- 18.Kornblith SJ, Rehm LP, O'Hara MW, Lamparski DM. The contribution of self-reinforcement training and behavioral assignments to the efficacy of self-control therapy for depression. Cogn Ther Res. 1983;7:499–528. [Google Scholar]
- 19.Shapiro DA, Barkham M, Rees A, et al. Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioral and psychodynamic-interpersonal psychotherapy. J Consult Clin Psychol. 1994;62:522–534. doi: 10.1037/0022-006x.62.3.522. [DOI] [PubMed] [Google Scholar]
- 20.Barkham M, Rees A, Stiles WB, et al. Dose-effect relations in time-limited psychotherapy for depression. J Consult Clin Psychol. 1996;64:927–935. doi: 10.1037//0022-006x.64.5.927. [DOI] [PubMed] [Google Scholar]
- 21.Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression. I. Impact on maternal mood. Br J Psychiatry. 2003;182:412–419. [PubMed] [Google Scholar]
- 22.Burnand Y, Andreoli A, Kolatte E, et al. Psychodynamic psychotherapy and clomipramine in the treatment of major depression. Psychiatr Serv. 2002;53:585–590. doi: 10.1176/appi.ps.53.5.585. [DOI] [PubMed] [Google Scholar]
- 23.Salminen JK, Karlsson H, Hietala J, et al. Short-term dynamic psychotherapy and fluoxetine in major depressive disorder: A randomized comparative study. Psychother Psychosom. 2008;77:351–357. doi: 10.1159/000151388. [DOI] [PubMed] [Google Scholar]
- 24.De Jonghe F, Kool S, van Aalst G, et al. Combining psychotherapy and antidepressants in the treatment of depression. J Affect Disord. 2001;64:217–229. doi: 10.1016/s0165-0327(00)00259-7. [DOI] [PubMed] [Google Scholar]
- 25.Kool S, Dekker J, Duijsens IJ, et al. Efficacy of combined therapy and pharmacotherapy for depressed patients with and without personality disorders. Harv Rev Psychiatry. 2003;11:133–141. doi: 10.1080/10673220303950. [DOI] [PubMed] [Google Scholar]
- 26.Dekker JJM, Koelen JA, Van HL, et al. Speed of action: The relative efficacy of short psychodynamic supportive psychotherapy and pharmacotherapy in the first 8 weeks of a treatment algorithm for depression. J Affect Disord. 2008;109:183–188. doi: 10.1016/j.jad.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 27.Maina G, Rosso G, Crespi C, Bogetto F. Combined brief dynamic therapy and pharmacotherapy in the treatment of major depressive disorder: A pilot study. Psychother Psychosom. 2007;76:298–305. doi: 10.1159/000104706. [DOI] [PubMed] [Google Scholar]
- 28.Maina G, Rosso G, Bogetto F. Brief dynamic therapy combined with pharmacotherapy in the treatment of major depressive disorder: Long-term results. J Affect Disord. 2009;114:200–207. doi: 10.1016/j.jad.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 29.Gallagher DE, Thompson LW. Treatment of major depressive disorder in older adult outpatients with brief psychotherapies. Psychother: Theory Res Pract. 1982;19:482–490. [Google Scholar]
- 30.Thompson LW, Gallagher D, Breckenridge JS. Comparative effectiveness of psychotherapies for depressed elders. J Consult Clin Psychol. 1987;55:385–390. doi: 10.1037//0022-006x.55.3.385. [DOI] [PubMed] [Google Scholar]
- 31.Gallagher-Thompson D, Hanley-Peterson P, Thompson LW. Maintenance of gains versus relapse following brief psychotherapy for depression. J Consult Clin Psychol. 1990;58:371–374. doi: 10.1037//0022-006x.58.3.371. [DOI] [PubMed] [Google Scholar]
- 32.Gallagher-Thompson D, Steffen AM. Comparative effects of cognitive-behavioral and brief psychodynamic psychotherapies for depressed family caregivers. J Consult Clin Psychol. 1994;62:543–549. doi: 10.1037//0022-006x.62.3.543. [DOI] [PubMed] [Google Scholar]
- 33.Steuer JL, Mintz J, Hammen CL, et al. Cognitive-behavioral and psychodynamic group psychotherapy in treatment of geriatric depression. J Consult Clin Psychol. 1984;52:180–189. doi: 10.1037//0022-006x.52.2.180. [DOI] [PubMed] [Google Scholar]
- 34.Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal psychotherapy of depression. Basic Books; New York: 1984. [Google Scholar]
- 35.Weissman MM, Markowitz JC. Interpersonal psychotherapy: current status. Arch Gen Psychiatry. 1994;51:599–606. doi: 10.1001/archpsyc.1994.03950080011002. [DOI] [PubMed] [Google Scholar]
- 36.Klerman GL, DiMascio A, Weissman M, et al. Treatment of depression by drugs and psychotherapy. Am J Psychiatry. 1974;131:186–191. doi: 10.1176/ajp.131.2.186. [DOI] [PubMed] [Google Scholar]
- 37.Weissman MM, Klerman GL, Paykel ES, et al. Treatment effects on the social adjustment of depressed patients. Arch Gen Psychiatry. 1974;30:771–778. doi: 10.1001/archpsyc.1974.01760120033006. [DOI] [PubMed] [Google Scholar]
- 38.Weissman MM, Prusoff BA, DiMascio A, et al. The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. Am J Psychiatry. 1979;136:555–558. [PubMed] [Google Scholar]
- 39.DiMascio A, Weissman M, Prusoff BA, et al. Differential symptom reduction by drugs and psychotherapy in acute depression. Arch Gen Psychiatry. 1979;36:1450–1456. doi: 10.1001/archpsyc.1979.01780130068008. [DOI] [PubMed] [Google Scholar]
- 40.Weissman MM, Klerman GL, Prusoff B, et al. Depressed outpatients: results one year after treatment with drugs and/or interpersonal therapy. Arch Gen Psychiatry. 1981;38:51–55. doi: 10.1001/archpsyc.1981.01780260053005. [DOI] [PubMed] [Google Scholar]
- 41.Elkin I, Shea MT, Watkins JT, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- 42.Elkin I, Gibbons RD, Shea T, et al. Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol. 1995;63:841–847. doi: 10.1037//0022-006x.63.5.841. [DOI] [PubMed] [Google Scholar]
- 43.Watkins JT, Leber WR, Imber SD, et al. Temporal course of change of depression. J Consult Clin Psychol. 1993;61:858–864. doi: 10.1037//0022-006x.61.5.858. [DOI] [PubMed] [Google Scholar]
- 44.O'Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry. 2000;57:1039–1045. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- 45.Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry. 2003;160:555–562. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- 46.Luty SE, Carter JD, McKenzie JM, et al. Randomised controlled trial of interpersonal psychotherapy and cognitive-behavioural therapy for depression. Br J Psychiatry. 2007;190:496–502. doi: 10.1192/bjp.bp.106.024729. [DOI] [PubMed] [Google Scholar]
- 47.Joyce PR, McKenzie JM, Carter JD, et al. Temperament, character and personality disorders as predictors of response to interpersonal psychotherapy and cognitive-behavior therapy for depression. Br J Psychiatry. 2007;190:503–508. doi: 10.1192/bjp.bp.106.024737. [DOI] [PubMed] [Google Scholar]
- 48.Marshall MB, Zuroff DC, McBride C, Bagby RM. Self-criticism predicts differential response to treatment for depression. J Clin Psychol. 2008;64:231–244. doi: 10.1002/jclp.20438. [DOI] [PubMed] [Google Scholar]
- 49.Markowitz JC, Kocsis JH, Fishman B, et al. Treatment of depressive symptoms in human immunodeficiency virus-positive patients. Arch Gen Psychiatry. 1998;55:452–457. doi: 10.1001/archpsyc.55.5.452. [DOI] [PubMed] [Google Scholar]
- 50.Bolton P, Bass J, Neugebauer R, et al. Group interpersonal psychotherapy for depression in rural Uganda: A randomized controlled trial. JAMA. 2003;289:3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- 51.Bass J, Neugebauer R, Clougherty KF, et al. Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes. Br J Psychiatry. 2006;188:567–573. doi: 10.1192/bjp.188.6.567. [DOI] [PubMed] [Google Scholar]
- 52.Schulberg HC, Block MR, Madonia MJ, et al. Treating major depression in primary care practice: eight-month clinical outcomes. Arch Gen Psychiatry. 1996;53:913–919. doi: 10.1001/archpsyc.1996.01830100061008. [DOI] [PubMed] [Google Scholar]
- 53.Judd FK, Piterman L, Cockram AM, et al. A comparative study of venlafaxine with a focused education and psychotherapy program versus venlafaxine alone in the treatment of depression in general practice. Hum Psychopharmacol. 2001;16:423–428. doi: 10.1002/hup.311. [DOI] [PubMed] [Google Scholar]
- 54.Schramm E, van Calker D, Kykierek P, et al. An intensive treatment program of interpersonal psychotherapy plus pharmacotherapy for depressed inpatients: Acute and long-term results. Am J Psychiatry. 2007;164:768–777. doi: 10.1176/ajp.2007.164.5.768. [DOI] [PubMed] [Google Scholar]
- 55.Schramm E, Schneider D, Zobel I, et al. Efficacy of interpersonal psychotherapy plus pharmacotherapy in chronically depressed patients. J Affect Disord. 2008;109:65–73. doi: 10.1016/j.jad.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 56.Swartz HA, Frank E, Zuckoff A, et al. Brief interpersonal psychotherapy for depressed mothers whose children are receiving psychiatric treatment. Am J Psychiatry. 2008;165:1155–1162. doi: 10.1176/appi.ajp.2008.07081339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reynolds CF, III, Miller MD, Pasternakm RE, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999;156:202–208. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- 58.Van Schaik A, van Marwijk H, Ader H, et al. Interpersonal psychotherapy for elderly patients in primary care. Am J Geriatr Psychiatry. 2006;14:777–786. doi: 10.1097/01.JGP.0000199341.25431.4b. [DOI] [PubMed] [Google Scholar]
- 59.Frank E, Kupfer DJ, Perel JM, et al. Three-year outcomes for maintenance therapies in recurrent depression. Arch Gen Psychiatry. 1990;47:1093–1099. doi: 10.1001/archpsyc.1990.01810240013002. [DOI] [PubMed] [Google Scholar]
- 60.Frank E, Kupfer DJ, Wagner EF, et al. Efficacy of interpersonal psychotherapy as a maintenance treatment of recurrent depression: Contributing factors. Arch Gen Psychiatry. 1991;48:1053–1059. doi: 10.1001/archpsyc.1991.01810360017002. [DOI] [PubMed] [Google Scholar]
- 61.Reynolds CF, III, Frank E, Perel JM, et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent depression: A randomized controlled trial in patients older than 59 years. JAMA. 1999;281:39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- 62.Reynolds CF, III, Dew MA, Pollock BG, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354:1130–1138. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 63.Carreira K, Miller MD, Frank E, et al. A controlled evaluation of monthly maintenance interpersonal psychotherapy in late-life depression with varying levels of cognitive function. Int J Geriatr Psychiatry. 2009;23:1110–1113. doi: 10.1002/gps.2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gaffan EA, Tsaousis I, Kemp-Wheeler SM. Researcher alliance and meta-analysis: the case of cognitive therapy for depression. J Consult Clin Psychol. 1995;63:966–980. doi: 10.1037//0022-006x.63.6.966. [DOI] [PubMed] [Google Scholar]
- 65.American Psychiatric Association Practice guideline for the treatment of patients with major depressive disorder (revision). Am J Psychiatry. 2000;157(suppl 4):1–45. [PubMed] [Google Scholar]
- 66.Rush AJ, Beck AT, Kovacs M, Hollon SD. Comparative efficacy of cognitive therapy and pharmacotherapy in the treatment of depressed outpatients. Cognit Ther Res. 1977;1:17–38. [Google Scholar]
- 67.Blackburn IM, Bishop S, Glen AIM, et al. The efficacy of cognitive therapy in depression: a treatment trial using cognitive therapy and pharmacotherapy, each alone and in combination. Br J Psychiatry. 1981;139:181–189. doi: 10.1192/bjp.139.3.181. [DOI] [PubMed] [Google Scholar]
- 68.Murphy GE, Carney RM, Knesevich MA, et al. Cognitive behavior therapy, relaxation training, and tricyclic antidepressant medication in the treatment of depression. Psychol Rep. 1995;77:403–420. doi: 10.2466/pr0.1995.77.2.403. [DOI] [PubMed] [Google Scholar]
- 69.Murphy GE, Simons AD, Wetzel RD, Lustman PJ. Cognitive therapy and pharmacotherapy, singly and together, in the treatment of depression. Arch Gen Psychiatry. 1984;41:33–41. doi: 10.1001/archpsyc.1984.01790120037006. [DOI] [PubMed] [Google Scholar]
- 70.Hollon SD, DeRubeis RJ, Evans MD, et al. Cognitive therapy and pharmacotherapy for depression: Singly and in combination. Arch Gen Psychiatry. 1992;49:774–781. doi: 10.1001/archpsyc.1992.01820100018004. [DOI] [PubMed] [Google Scholar]
- 71.David D, Szentagotai A, Lupu V, Cosman D. Rational emotive behavior therapy, cognitive therapy, and medication in the treatment of major depressive disorder: A randomized clinical trial, posttreatment outcomes, and six-month follow-up. J Clin Psychol. 2008;64:728–746. doi: 10.1002/jclp.20487. [DOI] [PubMed] [Google Scholar]
- 72.Sava FA, Yates BT, Lupu V, et al. Cost-effectiveness and cost-utility of cognitive therapy, rational emotive behavioral therapy, and fluoxetine (Prozac) in treatment depression: A randomized clinical trial. J Clin Psychol. 2009;55:36–52. doi: 10.1002/jclp.20550. [DOI] [PubMed] [Google Scholar]
- 73.Jacobson NS, Hollon SD. Prospects for future comparisons between drugs and psychotherapy: lessons from the CBT-versus-pharmacotherapy exchange. J Consult Clin Psychol. 1996;64:104–108. doi: 10.1037//0022-006x.64.1.104. [DOI] [PubMed] [Google Scholar]
- 74.DeRubeis RJ, Gelfand LA, Tang TZ, Simons AD. Medication versus cognitive behavior therapy for severely depressed outpatients: mega-analysis of four randomized comparisons. Am J Psychiatry. 1999;156:1007–1013. doi: 10.1176/ajp.156.7.1007. [DOI] [PubMed] [Google Scholar]
- 75.Jarrett RB, Schaffer M, McIntire D, et al. Treatment of atypical depression with cognitive therapy or phenelzine: a double-blind, placebo-controlled trial. Arch Gen Psychiatry. 1999;56:431–437. doi: 10.1001/archpsyc.56.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs. medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62:409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- 77.Klein DF. Preventing hung juries about therapy studies. J Consult Clin Psychol. 1996;64:81–87. doi: 10.1037//0022-006x.64.1.81. [DOI] [PubMed] [Google Scholar]
- 78.Faramarzi M, Alipor A, Esmaelzadeh S, et al. Treatment of depression and anxiety in infertile women: Cognitive behavioral therapy versus fluoxetine. J Affect Disord. 2008;108:159–164. doi: 10.1016/j.jad.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 79.Fournier JC, DeRubeis RJ, Shelton RC, et al. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. Br J Psychiatry. 2008;192:124–129. doi: 10.1192/bjp.bp.107.037234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bright JI, Baker KD, Neimeyer RA. Professional and paraprofessional group treatments for depression: A comparison of cognitive-behavioral and mutual support interventions. J Consult Clin Psychol. 1999;67:491–501. doi: 10.1037//0022-006x.67.4.491. [DOI] [PubMed] [Google Scholar]
- 81.Dimidjian S, Hollon SD, Dobson KS, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- 82.Bagby RM, Quilty LC, Segal ZV, et al. Personality and differential treatment response in major depression: A randomized controlled trial comparing cognitive-behavioral therapy and pharmacotherapy. Can J Psychiatry. 2008:53361–370. doi: 10.1177/070674370805300605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Blackburn IM, Moore RG. Controlled acute and follow-up trial of cognitive therapy and pharmacotherapy in outpatients with recurrent depression. Br J Psychiatry. 1997;171:328–334. doi: 10.1192/bjp.171.4.328. [DOI] [PubMed] [Google Scholar]
- 84.Miller IW, Norman WH, Keitner GI, et al. Cognitive-behavioural treatment of depressed inpatients. Behav Ther. 1989;20:25–47. doi: 10.1176/ajp.146.10.1274. [DOI] [PubMed] [Google Scholar]
- 85.Bowers WA. Treatment of depressed in-patients: cognitive therapy plus medication, relaxation plus medication, and medication alone. Br J Psychiatry. 1990;156:73–78. doi: 10.1192/bjp.156.1.73. [DOI] [PubMed] [Google Scholar]
- 86.Scott C, Tacchi MJ, Jones R, Scott J. Acute and one-year outcome of a randomized controlled trial of brief cognitive therapy for major depressive disorder in primary care. Br J Psychiatry. 1997;171:131–134. doi: 10.1192/bjp.171.2.131. [DOI] [PubMed] [Google Scholar]
- 87.Teasdale JD, Fennell MJV, Hibbert GA, Amies PL. Cognitive therapy for major depressive disorder in primary care. Br J Psychiatry. 1984;144:400–406. doi: 10.1192/bjp.144.4.400. [DOI] [PubMed] [Google Scholar]
- 88.Serfaty MA, Haworth D, Blanchard M, et al. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: A randomized controlled trial. Arch Gen Psychiatry. 2009;66:1332–1340. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- 89.Scott AIF, Freeman CPL. Edinburgh primary care depression study: Treatment outcome, patient satisfaction, and cost after 16 weeks. BMJ. 1992;304:883–887. doi: 10.1136/bmj.304.6831.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Miranda J, Chung JY, Green BL, et al. Treating depression in predominantly low-income young minority women. A randomized controlled trial. JAMA. 2003;290:57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 91.Miranda J, Green BL, Krupnick JL, et al. One-year outcomes of a randomized clinical trial treating depression in low-income minority women. J Consult Clin Psychol. 2006;74:99–111. doi: 10.1037/0022-006X.74.1.99. 2006. [DOI] [PubMed] [Google Scholar]
- 92.Cuijpers P, van Lier PAC, van Straten A, Donker M. Examining differential effects of psychological treatment of depressive disorder: An application of trajectory analyses. J Affect Disord. 2005;89:137–146. doi: 10.1016/j.jad.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 93.Kovacs M, Rush AJ, Beck AT, Hollon SD. Depressed outpatients treated with cognitive therapy or pharmacotherapy. Arch Gen Psychiatry. 1981;38:33–39. doi: 10.1001/archpsyc.1981.01780260035003. [DOI] [PubMed] [Google Scholar]
- 94.Blackburn IM, Eunson KM, Bishop S. A two-year naturalistic follow-up of depressed patients treated with cognitive therapy, pharmacotherapy and a combination of both. J Affect Disord. 1986;10:67–75. doi: 10.1016/0165-0327(86)90050-9. [DOI] [PubMed] [Google Scholar]
- 95.Simons AD, Murphy GE, Levine JE, Wetzel RD. Cognitive therapy and pharmacotherapy for depression: sustained improvement over one year. Arch Gen Psychiatry. 1986;43:43–49. doi: 10.1001/archpsyc.1986.01800010045006. [DOI] [PubMed] [Google Scholar]
- 96.Evans MD, Hollon SD, DeRubeis RJ, et al. Differential relapse following cognitive therapy and pharmacotherapy for depression. Arch Gen Psychiatry. 1992;49:802–808. doi: 10.1001/archpsyc.1992.01820100046009. [DOI] [PubMed] [Google Scholar]
- 97.Hollon SD, DeRubeis RJ, Shelton RC, et al. Prevention of relapse following cognitive therapy versus medications in moderate to severe depression. Arch Gen Psychiatry. 2005;62:417–422. doi: 10.1001/archpsyc.62.4.417. [DOI] [PubMed] [Google Scholar]
- 98.Dobson KS, Hollon SD, Dimidjian S, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression. J Consult Clin Psychol. 2008;76:468–477. doi: 10.1037/0022-006X.76.3.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shea MT, Elkin I, Imber SD, et al. Course of depressive symptoms over follow-up: findings from the National Institute of Mental Health Treatment of Depression Collaborative Research Program. Arch Gen Psychiatry. 1992;49:782–787. doi: 10.1001/archpsyc.1992.01820100026006. [DOI] [PubMed] [Google Scholar]
- 100.Fava GA, Grandi S, Zielezny M, et al. Cognitive behavioral treatment of residual symptoms in primary major depressive disorder. Am J Psychiatry. 1994;151:1295–1299. doi: 10.1176/ajp.151.9.1295. [DOI] [PubMed] [Google Scholar]
- 101.Fava GA, Rafanelli C, Grandi S, et al. Prevention of recurrent depression with cognitive behavioral therapy. Arch Gen Psychiatry. 1998;55:816–820. doi: 10.1001/archpsyc.55.9.816. [DOI] [PubMed] [Google Scholar]
- 102.Paykel ES, Scott J, Teasdale JD, et al. Prevention of relapse in residual depression by cognitive therapy. Arch Gen Psychiatry. 1999;56:829–835. doi: 10.1001/archpsyc.56.9.829. [DOI] [PubMed] [Google Scholar]
- 103.Paykel ES, Scott J, Cornwall PL, et al. Duration of relapse prevention after cognitive therapy for residual depression: Follow-up of controlled trial. Psychol Med. 2005;35:59–68. doi: 10.1017/s003329170400282x. [DOI] [PubMed] [Google Scholar]
- 104.Bockting CL, Schene AH, Spinhoven P, et al. Preventing relapse/recurrence in recurrent depression with cognitive therapy: A randomized controlled trial. J Consult Clin Psychol. 2005;73:647–657. doi: 10.1037/0022-006X.73.4.647. [DOI] [PubMed] [Google Scholar]
- 105.Conradi HJ, de Jonge P, Ormel J. Cognitive behavioural therapy v. usual care in recurrent depression. Br J Psychiatry. 2008;193:505–506. doi: 10.1192/bjp.bp.107.042937. [DOI] [PubMed] [Google Scholar]
- 106.Smit A, Kluiter H, Conradi HJ, et al. Short-term effects of enhanced treatment for depression in primary care: Results from a randomized controlled trial. Psychol Med. 2006;36:15–26. doi: 10.1017/S0033291705006318. [DOI] [PubMed] [Google Scholar]
- 107.Perlis RH, Nierenberg AA, Alpert JE, et al. Effects of adding cognitive therapy to fluoxetine dose increase on risk of relapse and residual depressive symptoms in continuation treatment of major depressive disorder. J Clin Psychopharmacol. 2002;22:474–480. doi: 10.1097/00004714-200210000-00006. [DOI] [PubMed] [Google Scholar]
- 108.Wilkinson P, Adler N, Juszczak E, et al. A pilot randomised controlled trial of a brief cognitive behavioural group intervention to reduce recurrence rates in late life depression. Int J Geriatr Psychiatry. 2009;24:68–75. doi: 10.1002/gps.2076. [DOI] [PubMed] [Google Scholar]
- 109.Teasdale JD, Segal Z, Williams JMG, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68:615–23. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 110.Ma SH, Teasdale JH. Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004;72:31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- 111.Kuyken W, Byford S, Taylor RS, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol. 2008;76:966–978. doi: 10.1037/a0013786. [DOI] [PubMed] [Google Scholar]
- 112.Friedman MA, Detweiler-Bedell JB, Leventhal HE, et al. Combined psychotherapy and pharmacotherapy for the treatment of major depressive disorder. Clin Psychol Sci Pract. 2004;11:47–68. [Google Scholar]
- 113.Pampallona S, Bollini P, Tibaldi G, et al. Combined pharmacotherapy and psychological treatment for depression: A systematic review. Arch Gen Psychiatry. 2004;61:714–719. doi: 10.1001/archpsyc.61.7.714. [DOI] [PubMed] [Google Scholar]
- 114.Cuijpers P, van Straten A, Hollon SD, et al. The contribution of active medication to combined treatments of psychotherapy and pharmacotherapy for adult depression: A meta-analysis. Acta Psychiatrica Scandinavica. doi: 10.1111/j.1600-0447.2009.01513.x. in press. [DOI] [PubMed] [Google Scholar]
- 115.Cuijpers P, Dekker J, Hollon SD, et al. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: A meta-analysis. J Clin Psychiatry. 2009;70:1219–1229. doi: 10.4088/JCP.09r05021. 2009. [DOI] [PubMed] [Google Scholar]
- 116.Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- 117.Maddux RE, Riso LP, Klein DN, et al. Select comorbid personality disorders and the treatment of chronic depression with nefazodone, target psychotherapy, or their combination. J Affect Disord. 2009;117:174–179. doi: 10.1016/j.jad.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 118.Klein DN, Santiago NJ, Vivian D, et al. Cognitive-behavioral analysis system of psychotherapy as a maintenance treatment for chronic depression. J Consult Clin Psychol. 2004;72:681–688. doi: 10.1037/0022-006X.72.4.681. [DOI] [PubMed] [Google Scholar]
- 119.Jarrett RB, Kraft D, Doyle J, et al. Preventing recurrent depression using cognitive therapy with and without a continuation phase: A randomized clinical trial. Arch Gen Psychiatry. 2001;58:381–388. doi: 10.1001/archpsyc.58.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kocsis JH, Gelenberg AJ, Rothbaum BO, et al. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: The REVAMP Trial. Arch Gen Psychiatry. 2009;66:1178–1188. doi: 10.1001/archgenpsychiatry.2009.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Manber R, Edinger JD, Gress JL, et al. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Freedland KE, Skala JA, Carney RM, et al. Treatment of depression after coronary artery bypass surgery: A randomized controlled trial. Arch Gen Psychiatry. 2009;66:387–396. doi: 10.1001/archgenpsychiatry.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dozois DJA, Bieling PJ, Patelis-Siotis I, et al. Changes in self-schema structure in cognitive therapy for major depressive disorder: A randomized clinical trial. J Consult Clin Psychol. 2009;77:1078–1088. doi: 10.1037/a0016886. [DOI] [PubMed] [Google Scholar]
- 124.Thompson LW, Coon DW, Gallagher-Thompson D, et al. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. Am J Geriatr Psychiatry. 2001;9:225–240. [PubMed] [Google Scholar]
- 125.Laidlaw K, Davidson K, Toner H, et al. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late life depression. Int J Geriatr Psychiatry. 2008;23:843–850. doi: 10.1002/gps.1993. [DOI] [PubMed] [Google Scholar]
- 126.Thase ME, Friedman ES, Biggs MM, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: A STAR*D report. Am J Psychiatry. 2007;164:739–752. doi: 10.1176/ajp.2007.164.5.739. [DOI] [PubMed] [Google Scholar]
- 127.Rohan KJ, Roecklein KA, Lindsey KT, et al. A randomized controlled trial of cognitive-behavioral therapy, light therapy, and their combination for seasonal affective disorder. J Consult Clin Psychol. 2007;75:489–500. doi: 10.1037/0022-006X.75.3.489. [DOI] [PubMed] [Google Scholar]
- 128.Strauman TJ, Vieth AZ, Merrill KA, et al. Self-system therapy as an intervention for self-regulatory dysfunction in depression: A randomized comparison with cognitive therapy. J Consult Clin Psychol. 2006;74:367–376. doi: 10.1037/0022-006X.74.2.367. [DOI] [PubMed] [Google Scholar]
- 129.Selmi PM, Klein MH, Greist JH, et al. Computer-administered cognitive-behavioral therapy for depression. Am J Psychiatry. 1990;147:51–56. doi: 10.1176/ajp.147.1.51. [DOI] [PubMed] [Google Scholar]
- 130.Wright JH, Wright AS, Albano AM, et al. Computer-assisted cognitive therapy for depression: Maintaining efficacy while reducing therapist time. Am J Psychiatry. 2005;162:1158–1164. doi: 10.1176/appi.ajp.162.6.1158. [DOI] [PubMed] [Google Scholar]
- 131.Van den Hout JH, Arntz A, Kunkels FH. Efficacy of a self-control therapy program in a psychiatric day-treatment center. Acta Psychiatr Scand. 1995;92:25–29. doi: 10.1111/j.1600-0447.1995.tb09538.x. [DOI] [PubMed] [Google Scholar]
- 132.Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. J Consult Clin Psychol. 1986;54:196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- 133.Nezu AM, Perri MG. Social problem-solving therapy for unipolar depression: An initial dismantling investigation. J Consult Clin Psychol. 1989;57:408–413. 1989. [PubMed] [Google Scholar]
- 134.Arean PA, Perri MG, Nezu AM, et al. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatments for depression in older adults. J Consult Clin Psychol. 1993;61:1003–1110. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- 135.Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mynors-Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ. 2000;320:26–30. doi: 10.1136/bmj.320.7226.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Dowrick C, Dunn G, Ayuso-Mateos JL, et al. Problem solving treatment and group psychoeducation for depression: Multicentre randomised controlled trial. BMJ. 2000;321:1–6. doi: 10.1136/bmj.321.7274.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.O'Leary KD, Beach SRH. Marital therapy: A viable treatment for depression and marital discord. Am J Psychiatry. 1990;147:183–186. doi: 10.1176/ajp.147.2.183. [DOI] [PubMed] [Google Scholar]
- 139.Beach SRH, O'Leary KD. Treating depression in the context of marital discord: Outcome and predictors of response of marital therapy versus cognitive therapy. Behav Ther. 1992;23:507–528. [Google Scholar]
- 140.Jacobson NS, Dobson K, Fruzzetti AE, et al. Marital therapy as a treatment for depression. J Consult Clin Psychol. 1991;59:547–557. doi: 10.1037//0022-006x.59.4.547. [DOI] [PubMed] [Google Scholar]
- 141.Jacobson NS, Fruzzetti AE, Dobson K, et al. Couple therapy as a treatment for depression: II. The effects of relationship quality and therapy on depressive relapse. J Consult Clin Psychol. 1993;61:516–519. doi: 10.1037//0022-006x.61.3.516. [DOI] [PubMed] [Google Scholar]
- 142.Emanuels-Zuurveen L, Emmelkamp PMG. Individual behavioural-cognitive therapy v. marital therapy for depression in martially distressed couples. Br J Psychiatry. 1996;169:181–188. doi: 10.1192/bjp.169.2.181. [DOI] [PubMed] [Google Scholar]
- 143.Bodenmann G, Plancherel B, Beach SRH, et al. Effects of coping-oriented couple's therapy on depression: A randomized clinical trial. J Consult Clin Psychol. 2008;76:944–954. doi: 10.1037/a0013467. [DOI] [PubMed] [Google Scholar]
- 144.Jacobson NS, Dobson KS, Truax PA, et al. A component analysis of cognitive-behavior treatment for depression. J Consult Clin Psychol. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- 145.Gortner ET, Gollan JK, Dobson KS, Jacobson NS. Cognitive-behavioral treatment for depression: relapse prevention. J Consult Clin Psychol. 1998;66:377–384. doi: 10.1037//0022-006x.66.2.377. [DOI] [PubMed] [Google Scholar]
- 146.Coffman S, Martell CR, Dimidjian S, et al. Extreme non-response in cognitive therapy: Can behavioral activation succeed where cognitive therapy fails? J Consult Clin Psychol. 2007;75:531–541. doi: 10.1037/0022-006X.75.4.531. [DOI] [PubMed] [Google Scholar]
- 147.Hopko DR, Lejuez CW, Le Page JP, et al. A brief behavioural activation treatment for depression. Behav Modif. 2003;27:458–469. doi: 10.1177/0145445503255489. [DOI] [PubMed] [Google Scholar]
- 148.Beutler LE, Engle D, Mohr D, et al. Predictors of differential response to cognitive, experiential, and self-directed psychotherapeutic procedures. J Consult Clin Psychol. 1991;59:333–340. doi: 10.1037//0022-006x.59.2.333. [DOI] [PubMed] [Google Scholar]
- 149.Greenberg LS, Watson JC. Experiential therapy of depression: Differential effects of client-centered relationship conditions and process experiential interventions. Psychother Res. 1998;8:210–224. [Google Scholar]
- 150.Watson JC, Gordon LB, Stermac L, et al. Comparing the effectiveness of process-experiential with cognitive-behavioral psychotherapy in the treatment of depression. J Consult Clin Psychol. 2003;71:773–781. doi: 10.1037/0022-006x.71.4.773. [DOI] [PubMed] [Google Scholar]
- 151.Goldman RN, Greenberg LS, Angus L. The effects of adding emotion-focused interventions to the client-centered relationship conditions in the treatment of depression. Psychother Res. 2006;16:537–549. [Google Scholar]
- 152.Ellison JA, Greenberg LS, Goldman RN, Angus L. Maintenance of gains following experiential therapies for depression. J Consult Clin Psychol. 2009;77:103–112. doi: 10.1037/a0014653. [DOI] [PubMed] [Google Scholar]
- 153.Castonguay LG, Schut AJ, Aikins DE, et al. Integrative cognitive therapy for depression: A preliminary investigation. J Psychother Integrat. 2004;14:4–20. [Google Scholar]
- 154.Constantino MJ, Marnell ME, Haile AJ, et al. Integrative cognitive therapy for depression: A randomized pilot comparison. Psychother Theory Res Pract Train. 2008;45:122–134. doi: 10.1037/0033-3204.45.2.122. [DOI] [PubMed] [Google Scholar]
- 155.Friedman AS. Interaction of drug therapy with marital therapy in depressive patients. Arch Gen Psychiatry. 1975;32:619–637. doi: 10.1001/archpsyc.1975.01760230085007. [DOI] [PubMed] [Google Scholar]
- 156.Clarkin JF, Glick ID, Haas GL, et al. A randomized clinical trial of inpatient family intervention: V. results for affective disorders. J Affect Disord. 1990;18:17–28. doi: 10.1016/0165-0327(90)90113-m. [DOI] [PubMed] [Google Scholar]
- 157.Maina G, Forner F, Bogetto F. Randomized controlled trial comparing brief dynamic and supportive therapy with waiting list condition in minor depressive disorder. Psychother Psychosom. 2005;74:43–50. doi: 10.1159/000082026. [DOI] [PubMed] [Google Scholar]
- 158.Markowitz JC. Interpersonal psychotherapy for dysthymic disorder. American Psychiatric Press; Washington DC: 1998. [Google Scholar]
- 159.Feijó de Mello M, Myczowisk LM, Menezes PR. A randomized controlled trial comparing monclobemide and moclobemide plus interpersonal psychotherapy in the treatment of dysthymic disorder. J Psychother Pract Res. 2001;10:117–123. [PMC free article] [PubMed] [Google Scholar]
- 160.Browne G, Steiner M, Roberts J, et al. Sertraline and/or interpersonal psychotherapy for patients with dysthymic disorder in primary care: 6-month comparison with longitudinal 2-year follow-up of effectiveness and costs. J Affect Disord. 2002;68:317–330. doi: 10.1016/s0165-0327(01)00343-3. [DOI] [PubMed] [Google Scholar]
- 161.Markowitz JC, Kocsis JH, Bleiberg KL, et al. A comparative trial of psychotherapy and pharmacotherapy for “pure” dysthymic patients. J Affect Disord. 2005;89:167–175. doi: 10.1016/j.jad.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 162.Markowitz JC, Kocsis JH, Christos P, et al. Pilot study of interpersonal psychotherapy versus supportive psychotherapy for dysthymic patients with secondary alcohol abuse or dependence. J Nerv Ment Dis. 2008;196:468–474. doi: 10.1097/NMD.0b013e31817738f1. [DOI] [PubMed] [Google Scholar]
- 163.Beck AT, Freeman A. Associates. Cognitive therapy of personality disorders. Guilford Press; New York: 1990. [Google Scholar]
- 164.McCullough JP. Treatment for chronic depression: Cognitive behavioral analysis system of psychotherapy. Guilford Press; New York: 2000. [DOI] [PubMed] [Google Scholar]
- 165.Ravindran AV, Anisman H, Merali Z, et al. Treatment of primary dysthymia with group cognitive therapy and pharmacotherapy: Clinical symptoms and functional impairments. Am J Psychiatry. 1999;156:1608–1617. doi: 10.1176/ajp.156.10.1608. [DOI] [PubMed] [Google Scholar]
- 166.Dunner DL, Schmaling KB, Hendrickson H, et al. Cognitive therapy versus fluoxetine in the treatment of dysthymic disorder. Dep. 1996;4:34–41. doi: 10.1002/(SICI)1522-7162(1996)4:1<34::AID-DEPR4>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 167.Barrett JE, Williams JW, Oxman TE, et al. Treatment of dysthymia and minor depression in primary care: a randomized trial in patients aged 18 to 59 years. J Fam Pract. 2001;50:405–412. [PubMed] [Google Scholar]
- 168.Williams JW, Barrett J, Oxman T, et al. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. JAMA. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 169.Belmaker RH. Bipolar disorder. N Eng J Med. 2004;351:476–486. doi: 10.1056/NEJMra035354. 2004. [DOI] [PubMed] [Google Scholar]
- 170.Perry A, Tarrier N, Morriss R, et al. Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. BMJ. 1999;318:149–153. doi: 10.1136/bmj.318.7177.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Colom F, Vieta E, Martinez-Aran A, et al. A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Arch Gen Psychiatry. 2003;60:402–407. doi: 10.1001/archpsyc.60.4.402. [DOI] [PubMed] [Google Scholar]
- 172.Colom F, Vieta E, Sanchez-Moreno J, et al. Psychoeducation for bipolar II disorder: An explanatory 5-year outcome subanalysis. J Affect Disord. 2009;112:30–35. doi: 10.1016/j.jad.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 173.Reinares M, Colom F, Sanchez-Moreno J, et al. Impact of caregiver group psychoeducation on the course and outcome of bipolar patients in remission: A randomized controlled trial. Bipolar Disord. 2008;10:511–519. doi: 10.1111/j.1399-5618.2008.00588.x. [DOI] [PubMed] [Google Scholar]
- 174.Ehlers CL, Frank E, Kupfer DJ. Social zeitgebers and biological rhythms: A unified approach to understanding the etiology of depression. Arch Gen Psychiatry. 1988;45:948–952. doi: 10.1001/archpsyc.1988.01800340076012. [DOI] [PubMed] [Google Scholar]
- 175.Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- 176.Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- 177.Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar disorder: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419–427. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cochrane SD. Preventing medical noncompliance in the outpatient treatment of bipolar affective disorders. J Consult Clin Psychol. 1984;52:873–878. doi: 10.1037//0022-006x.52.5.873. [DOI] [PubMed] [Google Scholar]
- 179.Basco MR, Rush AJ. Cognitive-behavioral therapy for bipolar disorder. Guilford Press; New York: 1996. [Google Scholar]
- 180.Scott J, Garland A, Moorhead S. A pilot study of cognitive therapy in bipolar disorders. Psychol Med. 2001;31:459–467. doi: 10.1017/s0033291701003373. [DOI] [PubMed] [Google Scholar]
- 181.Ball JR, Mitchell PB, Corry JC, et al. A randomized controlled trial of cognitive therapy for bipolar disorder: Focus on long-term change. J Clin Psychiatry. 2006;67:277–286. doi: 10.4088/jcp.v67n0215. [DOI] [PubMed] [Google Scholar]
- 182.Zaretsky A, Lancee W, Miller C, et al. Is cognitive-behavioural therapy more effective than psychoeducation in bipolar disorder? Can J Psychiatry. 2008;53:441–448. doi: 10.1177/070674370805300709. [DOI] [PubMed] [Google Scholar]
- 183.Lam DH, Bright J, Jones S, et al. Cognitive therapy in bipolar illness – a pilot study of relapse prevention. Cognit Ther Res. 2000;24:503–520. [Google Scholar]
- 184.Lam DH, Watkins ER, Hayward P, et al. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: Outcome of the first year. Arch Gen Psychiatry. 2003;60:145–152. doi: 10.1001/archpsyc.60.2.145. [DOI] [PubMed] [Google Scholar]
- 185.Lam DH, Hayward P, Watkins ER, et al. Relapse prevention in patients with bipolar disorder: Cognitive therapy outcome after 2 years. Am J Psychiatry. 2005;162:324–329. doi: 10.1176/appi.ajp.162.2.324. [DOI] [PubMed] [Google Scholar]
- 186.Scott J, Paykel E, Morriss R, et al. Cognitive-behavioural therapy for severe and recurrent bipolar disorders. Br J Psychiatry. 2006;188:313–320. doi: 10.1192/bjp.188.4.313. [DOI] [PubMed] [Google Scholar]
- 187.Miller IW, Solomon DA, Ryan CE, Keitner GI. Does adjunctive family therapy enhance recovery from bipolar I mood episodes? J Affect Disord. 2004;82:431–436. doi: 10.1016/j.jad.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 188.Miklowitz DJ, Goldstein MJ. Bipolar disorder: A family-focused treatment approach. Guilford Press; New York: 1997. [Google Scholar]
- 189.Miklowitz DJ, Simoneau TL, George EL, et al. Family-focused treatment of bipolar disorder: One-year effects of psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry. 2000;48:582–592. doi: 10.1016/s0006-3223(00)00931-8. [DOI] [PubMed] [Google Scholar]
- 190.Miklowitz DJ, George EL, Richards JA, et al. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Arch Gen Psychiatry. 2003;60:904–912. doi: 10.1001/archpsyc.60.9.904. [DOI] [PubMed] [Google Scholar]
- 191.Rea MM, Thompson M, Miklowitz DJ, et al. Family focused treatment vs individual treatment for bipolar disorder: Results of a randomized clinical trial. J Consult Clin Psychol. 2003;71:482–492. doi: 10.1037/0022-006x.71.3.482. [DOI] [PubMed] [Google Scholar]
- 192.Baskin TW, Tierney SC, Minami T, et al. Establishing specificity in psychotherapy: A meta-analysis of structural equivalence of placebo controls. J Consult Clin Psychol. 2003;71:973–979. doi: 10.1037/0022-006X.71.6.973. [DOI] [PubMed] [Google Scholar]
- 193.Roth A, Fonagy P. What works for whom? A critical review of psychotherapy research. 2nd ed. Guilford Press; New York: 2005. [Google Scholar]
- 194.National Institute for Clinical Excellence Depression: Management of depression in primary and secondary care (Rep. No. Clinical Guideline 23)
- 195.Westen D, Novotny CM, Thompson-Brenner H. The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychol Bull. 2004;130:631–663. doi: 10.1037/0033-2909.130.4.631. [DOI] [PubMed] [Google Scholar]
- 196.Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: A patient-level meta-analysis. JAMA. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Driessen E, Cuijpers P, Hollon SD, et al. Does pre-treatment severity moderate the efficacy of psychological treatment of adult outpatient depression? A meta-analysis. J Consult Clin Psychol. doi: 10.1037/a0020570. in press. [DOI] [PubMed] [Google Scholar]
- 198.Clark DM, Layard R, Smithies R, et al. Improving access to psychological therapy: Initial evaluation of two UK demonstration sites. Behav Res Ther. 2009;47:910–920. doi: 10.1016/j.brat.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]