Abstract
Key components of the metabolic syndrome (MetS), ie, obesity and insulin resistance, are associated with increased aldosterone production and mineralocorticoid receptor (MR) activation. Both MetS and hyperaldosteronism are proinflammatory and pro-oxidative states associated with cardiovascular disease. This review discusses emerging data that MR activation may contribute to abnormalities seen in MetS. In view of these data, MR antagonists may be beneficial in MetS, not only by controlling hypertension but also by reversing inflammation, oxidative stress, and defective insulin signaling at the cellular-molecular level. Clinical trials have demonstrated benefits of MR antagonists in heart failure, hypertension, and diabetic nephropathy, but additional trials are needed to demonstrate the clinical significance of MR blockade in MetS.
Keywords: Aldosterone, Mineralocorticoid receptor, Obesity, Insulin resistance, Spironolactone, Eplerenone
Introduction
Metabolic syndrome (MetS) is a cluster of several abnormalities, including obesity, insulin resistance, hyperglycemia, hypertriglyceridemia, low high-density lipoprotein (HDL), and hypertension, that occur together and increase the risk of vascular disease and diabetes mellitus. Although experts disagree about the exact definition of MetS, the term is extensively used to describe a typical profile of individuals at very high risk of cardiovascular disease (CVD) and diabetes. The presence of MetS confers a 1.5 to 2 times higher risk of a major cardiovascular event [1], 2 to 3 times higher risk of chronic renal insufficiency [2], and more than 4 times higher risk of type 2 diabetes mellitus [3]. The incidence of congestive heart failure [4] and cardiovascular mortality is also increased in the presence of MetS [5]. Controversy remains as to whether the diagnosis of MetS improves CVD prediction, compared with the cumulative predictive value of factors included in the Framingham risk score [6], but it is clear that MetS is associated with increased risk of CVD.
This article reviews the recent literature to address the possibility that elevated aldosterone, increased activity of its receptor, the mineralocorticoid receptor (MR), or both may be involved in the pathogenesis of MetS and may contribute to the increased risk of CVD in individuals with MetS.
Mineralocorticoid Receptor Signaling
Recent studies demonstrate that the biology of MR signaling is more complex than initially thought [7, 8], and this complexity may allow for the myriad of clinical effects now being attributed to MR activation [9, 10]. Aldosterone and cortisol activate the human MR with equal efficiency. However, in many tissues, such as the kidney, colon, endothelium, and vascular smooth muscle, the MR is protected from cortisol activation by the enzyme 11β hydroxysteroid dehydrogenase 2, which converts cortisol to inactive cortisone. Further, the ability of cortisol to activate MR may be influenced by the intracellular redox state, with increased oxidative stress resulting in increased MR activation by cortisol [11]. This effect may be particularly relevant in cells that do not express 11β hydroxysteroid dehydrogenase 2, such as cardiomyocytes, monocytes/macrophages, adipocytes, and neuronal cells, in which cortisol is likely to be the primary ligand for MR because of the higher circulating levels of free cortisol versus aldosterone. Nonselective MR antagonists (spironolactone) and selective MR antagonists (eplerenone) block MR activation by cortisol and aldosterone.
MR is a well-characterized nuclear steroid receptor whose activation regulates transcription of target genes such as the epithelial sodium channel and the serum-and-glucocorticoid–induced protein kinase 1 (sgk1) [7]. In addition, recent studies demonstrate rapid, nongenomic effects of MR activation by aldosterone, including activation of extracellular-regulated kinase/mitogen-activated protein (ERK/MAP) kinase pathways and phosphorylation of c-SRC, JNK, and NF-κB [8]. Aldosterone also increases oxidative stress through decreases in glucose-6-phosphate dehydrogenase activity and activation of NAD(P)H oxidase [8, 12]. MR signaling is further complicated by the ability of Rac1, a member of the Rho family of GTPases, to activate MR [13] and by the cross-talk between MR and the receptors for epidermal growth factor and angiotensin II [7]. The genomic and nongenomic actions of aldosterone are differentially influenced by the activity of the angiotensin II type 1a and 1b receptors [14]. This interaction between MR and angiotensin II receptors suggests a role for blockade of both receptors in treating disorders associated with an activated renin-angiotensin-aldosterone system (RAAS).
Aldosterone in Hypertension and in Cardiovascular and Renovascular Injury
It is well recognized that elevated aldosterone levels and excess activation of MR in renal collecting ducts lead to salt and water retention, volume expansion, and hypertension. Primary hyperaldosteronism (excess unilateral or bilateral adrenal production of aldosterone) is present in 5% to 10% of patients with essential hypertension and up to 20% of individuals with resistant hypertension [9]. Treatment with drugs that antagonize the activation of the MR reduces blood pressure in individuals with essential hypertension and is particularly effective at reducing blood pressure in resistant hypertension [9]. Further, preclinical and clinical studies have demonstrated an important role for MR in the pathophysiology of stroke, cardiac disease, and renal disease, through mechanisms that are in large part independent of effects on blood pressure. MR blockade improved cardiac morbidity and mortality in two clinical trials of heart failure, the Randomized Aldactone Evaluation Study (RALES) [15] and the Eplerenone Post–Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) [16]. As a result of these trials, MR antagonists received an American Heart Association/American College of Cardiology class I recommendation for use in heart failure. Further, MR blockade has beneficial effects on the vasculature, heart, and albuminuria in patients with early-stage chronic kidney disease [17] and reduces left ventricular hypertrophy in patients with hypertension [18]. In patients with diabetic nephropathy during treatment with maximal doses of angiotensin-converting enzyme (ACE) inhibitors, the addition of spironolactone provided greater reduction in albuminuria than the addition of placebo, and this renoprotection was not attributable to decreases in blood pressure [19].
The mechanisms involved in aldosterone-induced cardiovascular injury involve MR-mediated endothelial dysfunction, vascular reactivity impairment, vascular inflammation, vascular injury, increases in plasminogen activator protein-1, and alterations in autonomic control of cardiovascular functions, as well as cardiomyocyte apoptosis and cardiac fibrosis. MR activation is implicated in the pathophysiology of atherosclerosis, impaired coronary flow reserve, and diastolic dysfunction. Given our understanding of the role of MR in the pathophysiology of cardiovascular and renovascular injury and the prominence of cardiac and renal disease in patients with MetS, the question arises as to whether aldosterone and activation of MR could have a role in the pathophysiology of MetS.
Aldosterone and Obesity in Metabolic Syndrome
Aldosterone levels in obesity have been studied mainly in the context of an association between obesity and hypertension. One of the mechanisms of obesity-induced hypertension may involve increased MR activity. We recently demonstrated high urinary aldosterone excretion and high angiotensin II–stimulated serum aldosterone levels in overweight individuals on a high-sodium diet [20]. The association between elevated aldosterone and obesity may be related to adipocyte biology. Adipocytes express MR, and activation of MR is essential for the differentiation of preadipocytes into adipocytes [21]. Further, some studies have demonstrated increased activity of the renin-angiotensin system in adipocytes of obese individuals [22]. Other studies have shown evidence of increased adrenal production of aldosterone in response to mineralocorticoid-releasing factors from the adipocytes [23]. Still another hypothesis suggests that hepatic intermediaries have a role in stimulating adrenals in obese people [24]. High levels of aldosterone in obesity decrease with weight loss. In one study, a 5% reduction in body weight led to reduced RAAS activity in plasma and adipose tissue, explaining the reduction in blood pressure after weight loss [25]. High aldosterone levels in obesity may not only contribute to hypertension, but also may contribute to insulin resistance and other components of MetS, as detailed below and in Fig. 1.
Fig. 1.
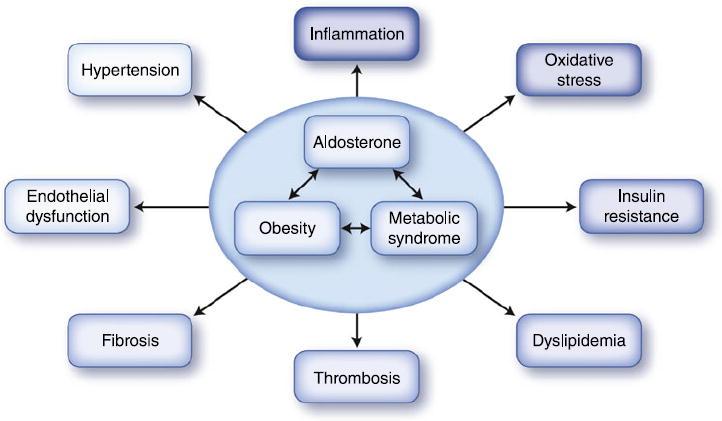
Aldosterone, obesity, and the metabolic syndrome share common features that underlie the pathophysiology of cardiovascular disease
Aldosterone and Insulin Resistance in Metabolic Syndrome
Hyperaldosteronism is associated with impaired carbohydrate metabolism, attributed for many years mainly to altered insulin release from the pancreatic beta cells owing to hypokalemia, fibrosis, or a direct inhibitory effect of corticosteroid on the beta cells [26, 27]. However, a growing body of evidence from observational studies and clinical trials, as well as from animal and cellular models, supports an important and direct role of aldosterone and the MR in the development and progression of insulin resistance. Although the association between hyperaldosteronism and fasting plasma glucose was recently questioned [28], epidemiologic data are available from patients with primary hyperaldosteronism in whom the prevalence of insulin resistance (which may not necessarily manifest as fasting hyperglycemia) has been reported to be as high as 50% [29-31, 32•]. Additional support for such an association is the observation that treatment of hyperaldosteronism either surgically or medically with MR antagonists restores normal insulin sensitivity [31, 33]. We have demonstrated an association between aldosterone production and insulin resistance, as assessed by the homeostasis model assessment (HOMA) and oral glucose tolerance test, in healthy and overweight individuals [20, 34••]. In addition, recent data from the Aliskiren Observation of Heart Failure Treatment study (ALOFT) demonstrated a strong and positive correlation between fasting insulin and both plasma and urinary aldosterone [35]. Moreover, patients who had aldosterone “escape” from the inhibitory effect of RAAS blockade were found to have elevated HOMA values, consistent with the concept that aldosterone contributes to insulin resistance.
Observations from epidemiologic studies and clinical trials have only implied an association between aldosterone action and insulin resistance, but causality has been suggested from studies in animal models. Aldosterone administration to rats resulted in decreased skeletal muscle expression and translocation to the plasma membrane of the insulin responsive glucose transporter, GLUT4 [36]. Decreased expression of liver GLUT2 was also observed after aldosterone treatment, and when taken together, these may account for both skeletal muscle and hepatic insulin resistance observed in these animals [36]. Further, treatment of Zucker diabetic rats with a hemeoxygenase inducer not only alleviates insulin resistance and oxidative stress but also lowers aldosterone levels, raising the possibility of a role for aldosterone in insulin resistance and oxidative stress [37]. When studied in animal models of obesity-induced insulin resistance (ob/ob and db/db mice), eplerenone treatment resulted in improvement in glucose tolerance, reduced HOMA levels, and decreased fasting levels of triglycerides [38••, 39••].
Several cellular mechanisms have been suggested to account for the induction of insulin resistance by aldosterone. Aldosterone has been demonstrated to exert direct effects on insulin signal transduction, both at the level of gene expression of key proteins in the insulin signal apparatus as well as in alterations in function and cellular trafficking following insulin stimulation. Direct interaction of the MR with the glucocorticoid response elements (GRE) located in the promoter of the insulin receptor gene has been shown, which may lead to downregulation of the insulin receptor [40]. More recently, aldosterone treatment promoted the degradation of insulin receptor substrate (IRS) 1 and IRS2 via glucocorticoid receptor–mediated production of reactive oxygen species, and activation of IκB kinase β and mTOR complex 1 leading to impaired Akt phosphorylation and glucose uptake in cultured adipocytes [41•]. MR blockade reduced aldosterone-induced oxidative damage and reversed aldosterone-mediated gene repression of adiponectin and peroxisome proliferator-activated receptor-γ (PPARγ) [38••, 39••].
Mineralocorticoids and Lipids in Metabolic Syndrome
In a recent small clinical trial, eplerenone treatment was found to decrease triglyceride levels among hypertensive individuals by approximately 35 mg/dL within 24 weeks of treatment. Of note, hypertensive subjects in that study who also met the International Diabetes Federation diagnostic criteria for MetS had a mean decrease in their triglyceride level of nearly 80 mg/dL [42]. These data are supported by observations in several mouse models of obesity-induced insulin resistance (ob/ob, db/db, and a high-fat, high-fructose fed C57BL/6 mouse), in which treatment with an MR antagonist reduced triglyceride levels [38••, 39••, 43•]. Further, MR blockade reduced hepatic steatosis in the mice fed a high-fat, high-fructose diet [43•].
Aldosterone and Inflammation in Metabolic Syndrome
MetS is a known proinflammatory state. The higher the number of MetS components, the higher the levels of inflammatory markers [44]. High aldosterone levels in MetS may contribute to its proinflammatory state. Aldosterone has been shown to exert proinflammatory effects on the vasculature [10], including increasing expression of the intercellular adhesion molecule (ICAM)1 gene [45], increasing 12-lipooxygenase and 15-lipooxygenase expression in human vascular smooth muscle cells, increasing the generation of 12 hydroxyeicosatetraenoic acid (12-HETE) and 15-HETE, and enhancing LDL oxidation [46••], which may lead to vascular dysfunction, atherosclerosis, or both. MR blockade reduces inflammation, reactive oxygen species production, and expression of proinflammatory cytokines in adipose tissue of db/db and ob/ob mice [38••, 39••]. In vitro studies of preadipocytes demonstrated stimulatory effects of aldosterone on expression of inflammatory cytokines and inhibitory effects on expression of adiponectin and PPARγ [38••].
Conclusions
In view of the above discussion, it is conceivable that MR antagonists have an effect at multiple levels in MetS. Besides reducing blood pressure, they may also improve insulin sensitivity, decrease the proinflammatory state of MetS, and reduce CVD. The beneficial cardiac effects of combining MR antagonists with ACE inhibitors or angiotensin receptor blockers (ARBs) have been demonstrated in patients with heart failure [15, 16]. Smaller studies have shown beneficial effects of combined MR blockade and ACE inhibitor therapy on renal function [19] and coronary circulatory function [47]. Further, a few small clinical studies have demonstrated a reduction in left ventricular mass and improvement in diastolic cardiac function with the use of MR antagonists [48, 49]. However, there are currently no clinical trials supporting the use of MR antagonists in obese insulinresistant patients, with the aim of preventing further metabolic deterioration to overt diabetes. Of interest is the recent observation from the large prospective trial of Nateglinide and Valsartan in Impaired Glucose Tolerance Outcomes Research (NAVIGATOR), which demonstrated that among patients with impaired glucose tolerance (most of them meeting the MetS diagnostic criteria), the use of valsartan (an ARB) led to a relative reduction of 14% in the incidence of diabetes [50•].
Thus, available clinical data suggest that using MR antagonists in addition to standard therapy may be beneficial in heart failure, left ventricular hypertrophy, and diastolic dysfunction. Some data also suggest a beneficial effect of MR antagonists when used in combination with ACE inhibitors or ARBs in preventing diabetic nephropathy. Currently, MR antagonists are not recommended for patients with diabetes and microalbuminuria because of the risk of hyperkalemia. Further clinical trials are needed to determine the safety and long-term cardiovascular and renovascular effects of MR antagonists in individuals with MetS, but increasing evidence suggests that MR antagonists may prove to be important therapeutic agents in reducing clinical complications of MetS.
Acknowledgments
This work is supported in part by a grant from the National Institutes of Health, R01HL 087060 (GKA and RG).
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported.
Contributor Information
Amir Tirosh, Email: atirosh@partners.org.
Rajesh Garg, Email: rgarg@partners.org.
Gail K. Adler, Email: gadler@partners.org.
References
Papers of particular interest, published recently, have been highlighted as:
-
•
Of importance
-
••
Of major importance
- 1.McNeill AM, Rosamond WD, Girman CJ, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the Atherosclerosis Risk in Communities study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385. [DOI] [PubMed] [Google Scholar]
- 2.Chen J, Muntner P, Hamm LL, et al. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med. 2004;140:167–174. doi: 10.7326/0003-4819-140-3-200402030-00007. [DOI] [PubMed] [Google Scholar]
- 3.Wilson PW, D’Agostino RB, Parise H, et al. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 4.Wang J, Sarnola K, Ruotsalainen S, et al. The metabolic syndrome predicts incident congestive heart failure: a 20-year follow-up study of elderly Finns. Atherosclerosis. 2010;210:237–242. doi: 10.1016/j.atherosclerosis.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 5.Wang J, Ruotsalainen S, Moilanen L, et al. The metabolic syndrome predicts cardiovascular mortality: a 13-year follow-up study in elderly non-diabetic Finns. Eur Heart J. 2007;28:857–864. doi: 10.1093/eurheartj/ehl524. [DOI] [PubMed] [Google Scholar]
- 6.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165:2644–2650. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 7.Odermatt A, Atanasov AG. Mineralocorticoid receptors: emerging complexity and functional diversity. Steroids. 2009;74:163–171. doi: 10.1016/j.steroids.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Grossmann C, Gekle M. New aspects of rapid aldosterone signaling. Mol Cell Endocrinol. 2009;308:53–62. doi: 10.1016/j.mce.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Gaddam KK, Pimenta E, Husain S, Calhoun DA. Aldosterone and cardiovascular disease. Curr Probl Cardiol. 2009;34:51–84. doi: 10.1016/j.cpcardiol.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Brown NJ. Aldosterone and vascular inflammation. Hypertension. 2008;51:161–167. doi: 10.1161/HYPERTENSIONAHA.107.095489. [DOI] [PubMed] [Google Scholar]
- 11.Funder JW. Reconsidering the roles of the mineralocorticoid receptor. Hypertension. 2009;53:286–290. doi: 10.1161/HYPERTENSIONAHA.108.119966. [DOI] [PubMed] [Google Scholar]
- 12.Leopold JA, Dam A, Maron BA, et al. Aldosterone impairs vascular reactivity by decreasing glucose-6-phosphate dehydrogenase activity. Nat Med. 2007;13:189–197. doi: 10.1038/nm1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shibata S, Nagase M, Yoshida S, et al. Modification of mineralocorticoid receptor function by Rac1 GTPase: implication in proteinuric kidney disease. Nat Med. 2008;14:1370–1376. doi: 10.1038/nm.1879. [DOI] [PubMed] [Google Scholar]
- 14.Lemarie CA, Simeone SM, Nikonova A, et al. Aldosterone-induced activation of signaling pathways requires activity of angiotensin type 1a receptors. Circ Res. 2009;105:852–859. doi: 10.1161/CIRCRESAHA.109.196576. [DOI] [PubMed] [Google Scholar]
- 15.Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 16.Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309–1321. doi: 10.1056/NEJMoa030207. [DOI] [PubMed] [Google Scholar]
- 17.Edwards NC, Steeds RP, Stewart PM, et al. Effect of spironolactone on left ventricular mass and aortic stiffness in early-stage chronic kidney disease: a randomized controlled trial. J Am Coll Cardiol. 2009;54:505–512. doi: 10.1016/j.jacc.2009.03.066. [DOI] [PubMed] [Google Scholar]
- 18.Pitt B, Reichek N, Willenbrock R, et al. Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation. 2003;108:1831–1838. doi: 10.1161/01.CIR.0000091405.00772.6E. [DOI] [PubMed] [Google Scholar]
- 19.Mehdi UF, Adams-Huet B, Raskin P, et al. Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximal angiotensin-converting enzyme inhibition in diabetic nephropathy. J Am Soc Nephrol. 2009;20:2641–2650. doi: 10.1681/ASN.2009070737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bentley-Lewis R, Adler G, Perlstein T, et al. Body Mass Index Predicts Aldosterone Production in Normotensive Adults on a High-Salt Diet. J Clin Endocrinol Metab. 2007;92:4472–4475. doi: 10.1210/jc.2007-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caprio M, Feve B, Claes A, et al. Pivotal role of the mineralocorticoid receptor in corticosteroid-induced adipogenesis. FASEB J. 2007;21:2185–2194. doi: 10.1096/fj.06-7970com. [DOI] [PubMed] [Google Scholar]
- 22.Lamounier-Zepter V, Ehrhart-Bornstein M, Bornstein SR. Mineralocorticoid-stimulating activity of adipose tissue. Best Pract Res Clin Endocrinol Metab. 2005;19:567–575. doi: 10.1016/j.beem.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Ehrhart-Bornstein M, Lamounier-Zepter V, Schraven A, et al. Human adipocytes secrete mineralocorticoid-releasing factors. Proc Natl Acad Sci U S A. 2003;100:14211–14216. doi: 10.1073/pnas.2336140100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodfriend TL, Egan BM, Kelley DE. Plasma aldosterone, plasma lipoproteins, obesity and insulin resistance in humans. Prostaglandins Leukot Essent Fatty Acids. 1999;60:401–405. doi: 10.1016/s0952-3278(99)80020-9. [DOI] [PubMed] [Google Scholar]
- 25.Engeli S, Bohnke J, Gorzelniak K, et al. Weight loss and the renin-angiotensin-aldosterone system. Hypertension. 2005;45:356–362. doi: 10.1161/01.HYP.0000154361.47683.d3. [DOI] [PubMed] [Google Scholar]
- 26.Ferrannini E, Seghieri G, Muscelli E. Insulin and the renin-angiotensin-aldosterone system: influence of ACE inhibition. J Cardiovasc Pharmacol. 1994;24(Suppl 3):S61–S69. [PubMed] [Google Scholar]
- 27.Pierluissi J, Navas FO, Ashcroft SJ. Effect of adrenal steroids on insulin release from cultured rat islets of Langerhans. Diabetologia. 1986;29:119–121. doi: 10.1007/BF00456122. [DOI] [PubMed] [Google Scholar]
- 28.Matrozova J, Steichen O, Amar L, et al. Fasting plasma glucose and serum lipids in patients with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2009;53:605–610. doi: 10.1161/HYPERTENSIONAHA.108.122002. [DOI] [PubMed] [Google Scholar]
- 29.Catena C, Colussi G, Di Fabio A, et al. Mineralocorticoid antagonists treatment versus surgery in primary aldosteronism. Horm Metab Res. 2010 Jan 29; doi: 10.1055/s-0029-1246185. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 30.Giacchetti G, Sechi LA, Rilli S, Carey RM. The renin-angiotensin-aldosterone system, glucose metabolism and diabetes. Trends Endocrinol Metab. 2005;16:120–126. doi: 10.1016/j.tem.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Catena C, Lapenna R, Baroselli S, et al. Insulin sensitivity in patients with primary aldosteronism: a follow-up study. J Clin Endocrinol Metab. 2006;91:3457–3463. doi: 10.1210/jc.2006-0736. [DOI] [PubMed] [Google Scholar]
- 32•.Fallo F, Della Mea P, Sonino N, et al. Adiponectin and insulin sensitivity in primary aldosteronism. Am J Hypertens. 2007;20:855–861. doi: 10.1016/j.amjhyper.2007.03.012.. Patients with primary aldosteronism had more insulin resistance (higher HOMA index) and lower levels of adiponectin than patients with low-renin essential hypertension in the absence of MetS.
- 33.Sindelka G, Widimsky J, Haas T, et al. Insulin action in primary hyperaldosteronism before and after surgical or pharmacological treatment. Exp Clin Endocrinol Diabetes. 2000;108:21–25. doi: 10.1055/s-0032-1329211. [DOI] [PubMed] [Google Scholar]
- 34••.Garg R, Hurwitz S, Williams GH, et al. Aldosterone production and insulin resistance in healthy adults. J Clin Endocrinol Metab. 2010;95:1986–1990. doi: 10.1210/jc.2009-2521.. In normotensive healthy adults, high angiotensin II–stimulated aldosterone level was an independent predictor of insulin resistance even after adjusting for age, body mass index, and diastolic blood pressure.
- 35.Freel EM, Tsorlalis IK, Lewsey JD, et al. Aldosterone status associated with insulin resistance in patients with heart failure—data from the ALOFT study. Heart. 2009;95:1920–1924. doi: 10.1136/hrt.2009.173344. [DOI] [PubMed] [Google Scholar]
- 36.Selvaraj J, Muthusamy T, Srinivasan C, Balasubramanian K. Impact of excess aldosterone on glucose homeostasis in adult male rat. Clin Chim Acta. 2009;407:51–57. doi: 10.1016/j.cca.2009.06.030. [DOI] [PubMed] [Google Scholar]
- 37.Ndisang JF, Lane N, Jadhav A. The heme oxygenase system abates hyperglycemia in Zucker diabetic fatty rats by potentiating insulin-sensitizing pathways. Endocrinology. 2009;150:2098–2108. doi: 10.1210/en.2008-0239. [DOI] [PubMed] [Google Scholar]
- 38••.Guo C, Ricchiuti V, Lian BQ, et al. Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines. Circulation. 2008;117:2253–2261. doi: 10.1161/CIRCULATIONAHA.107.748640.. In obese, db/db mice, MR blockade reduced circulating triglyceride levels, decreased adipose tissue expression of inflammatory cytokines, and increased expression of adiponectin and PPARγ. In 3 T3-L1 preadipocytes, aldosterone increased expression of inflammatory cytokines and decreased expression of adiponectin and PPARγ, supporting a direct effect of aldosterone on gene expression.
- 39••.Hirata A, Maeda N, Hiuge A, et al. Blockade of mineralocorticoid receptor reverses adipocyte dysfunction and insulin resistance in obese mice. Cardiovasc Res. 2009;84:164–172. doi: 10.1093/cvr/cvp191.. In obese, db/db and ob/ob mice, MR blockade reduced insulin resistance and improved adipose tissue inflammation (decreased reactive oxygen species and macrophage infiltration). In 3 T3-L1 adipocytes, aldosterone increased intracellular reactive oxygen species.
- 40.Calle C, Campion J, Garcia-Arencibia M, et al. Transcriptional inhibition of the human insulin receptor gene by aldosterone. J Steroid Biochem Mol Biol. 2003;84:543–553. doi: 10.1016/s0960-0760(03)00072-4. [DOI] [PubMed] [Google Scholar]
- 41•.Wada T, Ohshima S, Fujisawa E, et al. Aldosterone inhibits insulin-induced glucose uptake by degradation of insulin receptor substrate (IRS) 1 and IRS2 via a reactive oxygen species-mediated pathway in 3 T3-L1 adipocytes. Endocrinology. 2009;150:1662–1669. doi: 10.1210/en.2008-1018.. Aldosterone treatment in the adipocyte cell line resulted in IRS-1 serine phosphorylation and degradation, leading to decreased insulin stimulation of both Akt activation and glucose uptake. This mechanism was suggested to involve aldosterone-mediated intracellular oxidative stress.
- 42.Sato A, Fukuda S. Clinical effects of eplerenone, a selective aldosterone blocker, in Japanese patients with essential hypertension. J Hum Hypertens. 2009 Oct 29; doi: 10.1038/jhh.2009.81. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 43•.Wada T, Kenmochi H, Miyashita Y, et al. Spironolactone improves glucose and lipid metabolism by ameliorating hepatic steatosis and inflammation and suppressing enhanced gluconeogenesis induced by high-fat and high-fructose diet. Endocrinology. 2010;151:2040–2049. doi: 10.1210/en.2009-0869.. MR blockade improved glucose metabolism (assessed by the glucose tolerance test and insulin tolerance test), reduced triglyceride and cholesterol levels, reduced hepatic inflammation (decreased hepatic expression of TNFα, interleukin-6, and MCP-1), and reduced hepatic steatosis in mice fed a high-fat and high-fructose diet.
- 44.Kirilmaz B, Asgun F, Alioglu E, et al. High inflammatory activity related to the number of metabolic syndrome components. J Clin Hypertens (Greenwich) 2010;12:136–144. doi: 10.1111/j.1751-7176.2009.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Caprio M, Newfell BG, la Sala A, et al. Functional mineralocorticoid receptors in human vascular endothelial cells regulate intercellular adhesion molecule-1 expression and promote leukocyte adhesion. Circ Res. 2008;102:1359–1367. doi: 10.1161/CIRCRESAHA.108.174235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46••.Limor R, Kaplan M, Sharon O, et al. Aldosterone up-regulates 12- and 15-lipoxygenase expression and LDL oxidation in human vascular smooth muscle cells. J Cell Biochem. 2009;108:1203–1210. doi: 10.1002/jcb.22352.. Treating vascular smooth muscle cells with aldosterone resulted in increased expression of 12- and 15-lipoxygenase expression and increased LDL oxidation. These effects were blocked by MR antagonists or an EGF-receptor antagonist, demonstrating potential interactions between these two receptors.
- 47.Joffe HV, Kwong RY, Gerhard-Herman MD, et al. Beneficial effects of eplerenone versus hydrochlorothiazide on coronary circulatory function in patients with diabetes mellitus. J Clin Endocrinol Metab. 2007;92:2552–2558. doi: 10.1210/jc.2007-0393. [DOI] [PubMed] [Google Scholar]
- 48.Izawa H, Murohara T, Nagata K, et al. Mineralocorticoid receptor antagonism ameliorates left ventricular diastolic dysfunction and myocardial fibrosis in mildly symptomatic patients with idiopathic dilated cardiomyopathy: a pilot study. Circulation. 2005;112:2940–2945. doi: 10.1161/CIRCULATIONAHA.105.571653. [DOI] [PubMed] [Google Scholar]
- 49.Grandi AM, Imperiale D, Santillo R, et al. Aldosterone antagonist improves diastolic function in essential hypertension. Hypertension. 2002;40:647–652. doi: 10.1161/01.hyp.0000036399.80194.d8. [DOI] [PubMed] [Google Scholar]
- 50•.The NAVIGATOR Study Group. Effect of valsartan on the incidence of diabetes and cardiovascular events. N Engl J Med. 2010;363:1477–1490. doi: 10.1056/NEJMoa1001121.. In this large, placebo-controlled, randomized trial among patients with impaired glucose tolerance (many of whom met the MetS diagnostic criteria), the use of valsartan for 5 years led to a relative reduction of 14% in the incidence of diabetes. This study supports a role for blockade of the RAAS in preventing progression to diabetes.


