Abstract
Objectives
We examined whether similarities and differences exist in the association between perceived discrimination and poor mental and physical health among Asian-American adult women and men. We also tested whether Asian-American women would have a lower perceived discrimination threshold for developing negative health outcomes than Asian-American men.
Methods
Data were derived from the National Latino and Asian-American Study (2002–2003). A nationally representative sample of Asian-American adults (1,075 women and 972 men) was examined.
Results
There were more gender similarities than differences in the strong association between discrimination and health. More prominent gender differences were found for the specific level of discrimination and its potential health effects. Specifically, for both Asian women and men, a high level of perceived discrimination showed stronger associations with mental health than with physical health outcomes. And yet, compared with men, the threshold of discrimination was lower for women in affecting mental and physical health status.
Conclusion
The findings underscore that a high level of discrimination was associated with negative mental and physical health outcomes for both women and men. However, women had more negative mental and physical health outcomes when exposed to a lower threshold of discrimination than men. These findings suggest that failing to examine women and men separately in discrimination research may no longer be appropriate among the Asian-American population. Future research should focus attention on the biological, social, and political mechanisms that mitigate the adverse health effects of discrimination in order to develop a more comprehensive approach to eliminate disparities in health.
Introduction
Accumulating evidence has documented that perceived discrimination has been found to have robust links to poor health status among ethnic minorities. For instance, previous research has shown that perceived discrimination among African Americans and Hispanic Americans is strongly associated with depression, psychological distress, and generalized poor mental health (Amaro, Russo, & Johnson, 1987; Araujo & Borrell, 2006; Branscombe, Schmitt, & Harvey, 1999; Brown et al., 2000; Finch, Kolody, & Vega, 2000; Gee, Ryan, Laflamme, & Holt, 2006; Schulz, Williams et al., 2000; US Department of Health and Human Services, 2001), as well as cardiovascular conditions (Finch, Hummer, Kol, & Vega, 2001; Guyll, Matthews, & Bromberger, 2001; Krieger & Sidney, 1996), diabetes (Finch et al., 2001), and poor overall physical health (Ryan, Gee, & Laflamme, 2006; Schulz, Israel et al., 2000). Although these studies highlight the deleterious effects of discrimination on mental and physical health among African Americans and Hispanics, the study of discrimination is still in its infancy. This is more true for Asian Americans, despite the fact that they are among the fastest growing populations in the United States (U.S. Census Bureau, 2002). Two major gaps in those studies that focused on health effects of discrimination among Asian Americans were identified.
First, few studies have investigated physical health outcomes. One of the few researchers who examined the relationship between discrimination and health among Asian immigrants narrowed the scope to solely mental health outcomes (Noh, Beiser, Kaspar, Hou, & Rummens, 1999; Noh & Kaspar, 2003). The lack of epidemiological data on health outcomes and discrimination among Asian Americans may have also limited research in these areas. Analyzing both mental and physical health outcomes is particularly important for Asian Americans owing to the common viewpoint among Asian cultures that the body and mind are holistic rather than dualistic, and because Asians tend to manifest their mental health problems as physical illnesses (Chang, 2002; Lin & Cheung, 1999). So far, only the study by Gee, Spencer, Chen, and Takeuchi (2007) has tested the association between discrimination and chronic physical health conditions. It was found that perceived discrimination increased numbers of chronic health conditions among Asian Americans. More examination of the relationship between perceived discrimination and physical health is warranted to replicate the result.
Second, little attention has been given to the role of gender in the relationship between discrimination and health, which has left several important questions. Is the pattern of association for perceived discrimination and poor mental and physical health the same for Asian-American women and men? Do Asian-American women have a lower threshold of perceived discrimination than men regarding potential effects on health outcomes? To our knowledge, this is the first study to test the degree to which differing levels of discrimination impact the mental and physical health of Asian-American women and men. Research has shown some health disparities between Asian-American women and Asian-American men. Asian-American women have been found to suffer from higher rates of stroke, cancer, and arthritis (National Health Interview Survey [NHIS], 2007). They also have, on average, slightly higher rates of fair or poor self-reported health status according to a 25-year data accumulation from the NHIS (2007). A recent study also showed that U.S.-born Asian-American women had a substantially higher prevalence of suicidal ideation (16.0% vs 8.5%, respectively) and suicide attempts (6.3% vs 1.4%, respectively) than U.S.-born Asian-American men (Duldulao, Takeuchi, & Hong, 2009).
These poorer health statuses among Asian-American women could be connected to the fact that they have faced a “double minority status” as both women and ethnic minorities (Okazaki, 1998), often forcing them to cope with both racial and gender discrimination. The combination of multiple forms of discrimination may result in a lower socioeconomic status because there are fewer educational resources, lower salary, limited attainment of supervisory authority, and limited access to health care (Kim & Lewis, 1994; Williams, 1999; Williams & Williams-Morris, 2000). In addition, Asian-American women may be more vulnerable than men to the effects of perceived discrimination because it may act as an additional psychosocial stressor for women who are already dealing with their devalued status owing to sexism both in traditional Asian culture (Ho, 1990) and American culture (Klonoff & Landrine, 1995). These cumulative effects may act as a chronic stressor among women.
Stress sensitization theory (van Winkel, Stefanis, & Myin-Germeys, 2008) offers a useful framework in developing our hypothesis, although we did not formally test this theory. Stress sensitization theory, while integrating biological, psychological, and sociological approaches, provides some explanation on how stress plays a role in the onset as well as recurrence of a depressive episode (van Winkel et al., 2008). This theory postulates that prior stressors and depressive episodes cause neurobiological alteration, thus affecting the threshold at which stress is required to precipitate subsequent depression. The repeated stressors or depressive episodes then contribute to progressive changes in information processing, thus resulting in reduction of the threshold for triggering recurrences. In other words, if an individual is sensitized to stress, then he or she is at risk for succumbing to lower levels of stress after repeated recurrences (Post, 1992). Perceived discrimination is a stressor because it embodies the aggregation of daily hassles and series of minor or serious events that are associated with minority status (Clark, Anderson, Clark, & Williams, 1999).
In contrast, it is also possible that Asian-American women may not necessarily be more vulnerable than men to such effects because persistent exposure to discrimination may lead to patterns of habituation, helping to ameliorate the effects of discrimination. That is, in response to exposure to discrimination, women may foster adaptations that eventually extinguish prior stressors; thus, stressors become progressively less consequential and therefore desensitized, reducing negative health effects (Kendler, Neale, Kessler, Heath, & Eaves, 1993).
Building on previous literature, we hypothesize that 1) a higher level of discrimination is associated with higher odds of mental and physical health problems for both genders, and 2) the threshold of discrimination in negative health effects will be lower for women than for men. Investigating the effect modification of gender on discrimination and health considers how discrimination and its responses may have a varying impact on health, with respect to gender. In this paper, the terms “perceived discrimination” and “discrimination” were used interchangeably.
Our study aims to raise important questions regarding physical and mental health among Asian-Americans and under-explored issues regarding gender-based reactivity of health to discrimination.
Methods
Participants and Sample Design
The data for this study were taken from the National Latino and Asian-American Study (NLAAS), the first national epidemiological survey of Asian Americans in the United States. The NLAAS surveyed a nationally representative sample of Asian-American adults (ages 18 and older) living in the United States between 2002 and 2003. The sampling procedures have been described extensively elsewhere (Heeringa et al., 2004). A total of 2,095 Asian Americans (Chinese, Filipino, Vietnamese, and other Asian decent) were interviewed, resulting in a 65.6% response rate. Interviews were conducted by trained, bilingual interviewers and took place primarily in-person at the respondents' homes, although telephone interviews were permitted.
Measures
The NLAAS interviews utilized computer-based software and were offered in English, Cantonese, Mandarin, Tagalog, Vietnamese, and Spanish. Measures were translated with standard translation and back-translation techniques. Sociodemographic characteristics included gender, age (18–25, 26–44, or 45–75 years), and education (<9 years of school completed, some high school completed, and high school diploma or beyond achieved).
Measures of outcome variables
We identified three outcomes for mental health problems. Lifetime major depressive disorder (“Have you ever been diagnosed with DSM-IV major depressive disorder [MDD]?”) and lifetime suicidal thoughts (“Have you ever thought seriously about committing suicide?”) were used to measure internalized mental health problems. Lifetime intermittent explosive disorder (“Have you ever been diagnosed with DSM-IV intermittent explosive disorder [IED]?”) was used to measure externalized mental health problems.
We selected four outcomes for physical health problems: Chronic headaches, chronic pain, high blood pressure, and diabetes/high blood sugar. Respondents were asked if they had ever had or been diagnosed with any of these problems. We dichotomously coded each of the mental and physical health outcomes (0 = never, 1= at least once). We chose to focus on chronic illnesses as physical health outcomes because they affect more than 50 million Americans, resulting in a serious public health problem with steep costs and potential negative consequences for quality of life, economic productivity, and health care utilization (American Pain Foundation, 2006; National Center for Health Statistics, 2006; Stewart, Ricci, Chee, & Morganstein, 2003).
We also selected both mental and physical outcomes with a greater than 7% prevalence to ensure sufficient statistical power. In our sample, the only variable that did not meet this criterion was IED. Despite the lower prevalence (4%) compared with other outcomes, we chose to examine IED because it was the most appropriate outcome for a measure of externalization for adults. Moreover, IED has not been systematically examined in the context of discrimination among Asian Americans.
Measures of Independent Variables
Perceived discrimination
This measure was based on a Detroit area study (Williams, Yu, Jackson, & Anderson, 1997) and has been frequently used to measure racial discrimination (Chae et al., 2008; Gee et al., 2007; Perez, Fortuna, & Alegria, 2008). Perceived discrimination was measured through self-reported frequency of respondents' being treated with less courtesy, being treated with less respect, receiving poorer services, people thinking they are not smart, people being afraid of them, people thinking they are dishonest, people thinking they are not as good as others, being called names, and being threatened. Responses ranged from 1 (never) to 6 (almost every day), and were summed for a final scale of 9 to 54 (mean 16, SD 6.6, alpha =0.91). Scores were classified into three levels of perceived discrimination: low (scores of 9–15, >1 SD below the mean), medium (scores of 16–22, within 1 SD of the mean), and high (scores of 23–54, >1 SD above the mean).
Family cohesion
Studies have documented that low family cohesion is associated with low mental health functioning, and also with depressive symptoms among Asians (Farrell & Barnes, 1993; Greenberger & Chen, 1996). Based on this evidence, it is important to control for family cohesion as a possible confounder in the model.
To measure family cohesion, respondents indicated levels of agreement with the following statements regarding their families: respect one another, similar values and beliefs, things work well as a family, trust and confide in each other, loyal, proud of the family, express feelings with each other, spend free time with each other, feel very close to each other, and family togetherness is very important. Scores were scaled from 1 (strongly agree) to 4 (strongly disagree) and combined for a final score ranging from 10 to 40 (mean 36.8; SD 4.6, alpha =0.93). In our analysis, the code was reversed and a higher score indicated greater family cohesion. Values below the mean were categorized as low and values including and above the mean were categorized as high.
Acculturative stress
Research shows that higher levels of acculturative stress is associated with depression and anxiety among Korean immigrants (Noh & Kaspar, 2003), and, in another study, the use of Spanish language versus English language for interviews was associated with poorer self-assessed health status among Hispanics (Angel & Guarnaccia, 1989). Because this evidence indicates that acculturation can play a critical role in health among minorities, it is important to control acculturative stress when testing the effect of discrimination.
Respondents were asked if they experienced any of the following: Difficulties interacting with others because of language barriers, being treated poorly because of their lack of proficiency in English, difficulty finding work because of their ethnic origins, concern and fear of being deported, and avoiding seeking health services because of fear of immigration officials. Responses were measured on a scale ranging from 0 (the least) to 5 (the highest; mean 0.9, SD 1.1, alpha = 0.58), and scores were divided into three groups using a categorization method similar to that used to measure perceived discrimination: Low (0), medium (1–2), and high (3–5).
Statistical Analysis
Stata 10.0 was used for all analyses (StataCorp, 2007). Stata survey procedures were applied for bivariate and multivariate analyses to account for regional stratification as well as population weights. First, we conducted chi-square tests for association between each explanatory variable with mental and physical health outcome variables, stratified by gender (Table 1). Next, we used chi-square tests to compare the prevalence of mental and physical health outcomes among women and men by three levels of perceived discrimination (Table 2). Finally, we fit a series of multiple logistic regression models to estimate the relative contribution of perceived discrimination to mental health and physical health problems, controlling for age, education, acculturative stress, and family cohesion, stratified by gender (Table 3).
Table 1.
Sample Characteristics of Asian-American Adults by Gender, The US National Latino and Asian-American Study (n = 2,047)
| Total (n = 2047) n (%) | Women (n = 1075) n (%) | Men (n = 972) n (%) | p-Value | |
|---|---|---|---|---|
| Age (yrs) | ||||
| 18–25 | 310 (16.7) | 160 (15.6) | 150 (18.0) | |
| 26–44 | 977 (47.2) | 518 (46.8) | 459 (47.7) | |
| 45–75 | 760 (36.1) | 397 (37.6) | 363 (34.3) | |
| Education | ||||
| Up to 8th grade | 158 (7.8) | 108 (9.7) | 50 (5.6) | |
| Some high school | 134 (5.8) | 73 (5.6) | 61 (6.1) | * |
| High school graduate or beyond | 1755 (86.4) | 894 (84.7) | 861 (88.3) | |
| Acculturative stress | ||||
| Low | 735 (54.5) | 376 (55.8) | 359 (53.0) | |
| Medium | 494 (33.0) | 267 (32.4) | 227 (33.6) | |
| High | 166 (12.5) | 85 (11.7) | 81 (13.4) | |
| Family cohesion | ||||
| Low | 646 (32.8) | 339 (31.4) | 307 (34.3) | |
| High | 1401 (67.2) | 736 (68.6) | 665 (65.7) | |
| Perceived discrimination | ||||
| Low | 986 (47.8) | 561 (51.6) | 425 (43.7) | |
| Medium | 679 (34.5) | 326 (33.2) | 353 (35.9) | * |
| High | 308 (17.6) | 138 (15.1) | 170 (20.3) | |
| Mental health outcomes | ||||
| Major depressive disorder | 194 (9.3) | 115 (10.1) | 79 (8.5) | |
| Suicidal ideation | 136 (9.4) | 86 (10.8) | 50 (7.8) | |
| Intermittent explosive disorder | 82 (3.9) | 37 (3.6) | 45 (4.4) | |
| Physical health outcomes | ||||
| Chronic headaches | 283 (13.7) | 192 (17.8) | 91 (9.0) | *** |
| Chronic pain | 148 (6.9) | 84 (6.7) | 64 (7.1) | |
| Diabetes | 138 (7.0) | 76 (8.1) | 62 (5.7) | |
| High blood pressure | 312 (16.1) | 144 (15.1) | 168 (17.2) |
p < .05
p < .01
p < .001.
Table 2.
Weighted Percentage of Asian-American Women and Men According to the Level of Discrimination, by Explanatory Variables
| Low Perceived Discrimination, % (95% CI) | Medium Perceived Discrimination, % (95% CI) | High Perceived Discrimination, % (95% CI) | p-Value | |
|---|---|---|---|---|
| Women | ||||
| n | 561 | 326 | 138 | |
| Mental health outcomes | ||||
| Major depressive disorder | 4.7 (3.2–7.0) | 15.0 (10.9–20.5) | 18.5 (11.9–27.6) | *** |
| Suicidal ideation | 5.1 (3.3–7.7) | 17.4 (12.3–23.9) | 15.9 (9.1–26.2) | *** |
| Intermittent explosive disorder | 1.8 (0.8–4.1) | 4.3 (2.4–7.6) | 8.2 (4.3–15.2) | ** |
| Physical health outcomes | ||||
| Chronic headaches | 12.3 (9.4–16.0) | 22.4 (17.1–28.8) | 27.4 (19.3–37.4) | *** |
| Chronic pain | 6.1 (4.2–8.9) | 8.7 (5.9–12.6) | 4.5 (2.1–9.3) | |
| Diabetes | 9.6 (6.2–14.8) | 4.8 (2.6–8.6) | 7.0 (2.8–16.6) | |
| High blood pressure | 16.5 (11.9–22.3) | 12.0 (8.5–16.7) | 13.2 (7.2–22.7) | |
| Men | ||||
| n | 425 | 353 | 170 | |
| Mental health outcomes | ||||
| Major depressive disorder | 5.4 (3.3–8.9) | 7.2 (4.7–10.8) | 17.9 (10.5–29.0) | *** |
| Suicidal ideation | 3.7 (1.8–7.4) | 5.7 (3.2–9.7) | 18.6 (10.7–30.5) | *** |
| Intermittent explosive disorder | 2.6 (1.3–5.3) | 4.0 (2.2–7.1) | 9.1 (4.9–16.2) | * |
| Physical health outcomes | ||||
| Chronic headaches | 5.4 (3.4–8.5) | 10.9 (7.7–15.3) | 13.6 (7.3–23.8) | * |
| Chronic pain | 5.4 (3.2–9.0) | 5.7 (3.6–9.0) | 13.7 (7.1–25.0) | * |
| Diabetes | 6.9 (4.4–10.6) | 5.9 (3.6–9.4) | 2.2 (1.0–4.9) | * |
| High blood pressure | 18.7 (14.6–23.8) | 12.9 (9.3–17.5) | 22.0% (14.0–32.8) |
All percentages are weighted. For an explanation of low, medium, and high perceived discrimination, see Methods section.
p < .05
p < .01
p < .001.
Table 3.
Adjusted Odds Ratios (and 95% Confidence Intervals) From Multiple Logistic Regression Models Assessing Association Between Perceived Discrimination and Odds of Mental or Physical Health Problems, by Gender
| Low Perceived Discrimination, OR (95% CI) | Medium Perceived Discrimination OR, (95% CI) | High Perceived Discrimination OR, (95% CI) | |
|---|---|---|---|
| Women | |||
| n | 561 | 326 | 138 |
| Mental health outcomes | |||
| Major depressive disorder | 1.00 | 2.22 (1.37–3.59)** | 2.30 (1.28–4.12)** |
| Suicidal ideation | 1.00 | 2.03 (1.16–3.55)* | 1.64 (0.82–3.32) |
| Intermittent explosive disorder | 1.00 | 3.09 (1.25–7.65)* | 4.96 (1.88–13.08)** |
| Physical health outcomes | |||
| Chronic headaches | 1.00 | 1.53 (1.05–2.22)* | 1.91 (1.19–3.05)** |
| Chronic pain | 1.00 | 1.58 (0.93–2.70) | 0.89 (0.39–2.03) |
| Diabetes | 1.00 | 0.94 (0.52–1.70) | 0.93 (0.39–2.21) |
| High blood pressure | 1.00 | 1.41 (0.88–2.25) | 1.58 (0.94–2.67) |
| Men | |||
| n | 425 | 353 | 170 |
| Mental health outcomes | |||
| Major depressive disorder | 1.00 | 1.26 (0.70–2.25) | 2.29 (1.23–4.27)*** |
| Suicidal ideation | 1.00 | 1.24 (0.55–2.83) | 3.29 (1.48–7.32)** |
| Intermittent explosive disorder | 1.00 | 1.44 (0.65–3.19) | 2.55 (1.10–5.90)* |
| Physical health outcomes | |||
| Chronic headaches | 1.00 | 1.51 (0.89–2.57) | 1.96 (1.07–3.62)* |
| Chronic pain | 1.00 | 1.38 (0.74–2.57) | 1.91 (0.94–3.86) |
| Diabetes | 1.00 | 1.35 (0.74–2.48) | 0.82 (0.33–1.99) |
| High blood pressure | 1.00 | 0.92 (0.60–1.41) | 1.58 (0.94–2.67) |
We controlled for age, education, acculturative stress, and family cohesion. See Methods for an explanation of low, medium, and high perceived discrimination.
p < .05
p < .01
p < .001.
Results
Gender Differences in Background Characteristics and Health Outcomes
Our sample was composed of Asian-American women and men between 18 and 75 years old (n = 2,047; Table 1). A larger proportion of men reported medium and high levels of perceived discrimination compared with women (56.2% vs. 48.3%; p= .01). There were no significant gender differences for the three mental health outcomes: MDD, suicidal ideation, and IED (Table 1). The lack of gender differences in mental health outcomes was surprising, because many studies have revealed that women have higher rates of mood disorders (Kessler et al., 2005; Rieker & Bird, 2005). There was also little evidence of between-gender differences in poor physical health outcomes, with an exception of chronic headaches, for which women reported double the prevalence of men (17.8% vs. 9.0%; p =.001).
The Association between Perceived Discrimination and Mental Health and Physical Health Outcomes
Table 2 describes the proportion of mental and physical health outcomes based on the level of perceived discrimination, stratified by gender. Among women who experienced low perceived discrimination, only 4.7% reported having lifetime MDD; 5.1% reported having lifetime suicidal ideation; and 1.8% reported lifetime IED. In contrast, prevalence of mental health problems was significantly higher among those who reported medium or high levels of perceived discrimination.
For the majority of women, poor physical health outcomes were not significantly associated with perceived discrimination, with the exception of chronic headaches. Among men, the associations between levels of perceived discrimination and mental and physical health outcomes were similar to that of women.
Gender Modifies the Potential Effect of Perceived Discrimination of Mental and Physical Health Problems
Similar to our bivariate analyses (Table 2), a series of logistic regression models (Table 3) also demonstrated significant associations among both genders between higher levels of perceived discrimination and the lifetime odds of having MDD, suicidal ideation, IED, and chronic headaches. However, gender differences were identified with respect to vulnerability to perceived discrimination in both mental and physical health outcomes. Among women, after controlling for age, education, acculturative stress, and family cohesion, both medium levels of discrimination (odds ratio [OR] for MDD = 2.22; OR for suicidal thoughts= 2.03; OR for IED = 3.09) and high levels of discrimination (OR for MDD = 2.30; OR for IED =4.96) were independent predictors for mental health outcomes.
However, among men, only high levels of perceived discrimination were associated with MDD (OR= 2.29), suicidal thoughts (OR =3.29), and IED (OR= 2.55), whereas medium levels of discrimination showed no significant associations. This suggests that the threshold for the potential effect of discrimination on mental health for women was lower than that for men. Another important finding was that gender differences identified for mental health outcomes were similar to those for physical health outcomes.
We formally tested for effect modification by including a gender-by-discrimination interaction term in all models (not shown in table) for each of the mental and physical health outcomes. This interaction was statistically significant for MDD (OR = 2.0; p =.008), suicidal ideation (OR 3.0; p = .001), and chronic headaches (OR = 2.2; p =.001), suggesting that gender modified the potential mental and physical health effects of perceived discrimination.
Figure 1 illustrates adjusted ORs and 95% confidence intervals for each of the three mental health outcomes and chronic headaches, stratified by gender and discrimination level. The dotted line denotes the null value (OR= 1). Figure 1 illustrates the magnitude of the association between each level of perceived discrimination and each health outcome. The pattern suggests that under a high level of discrimination, there is little gender difference in the magnitude of odds in the outcome variables, whereas under the mid level of discrimination, women have significantly higher odds of predicting outcome variables than men.
Figure 1.
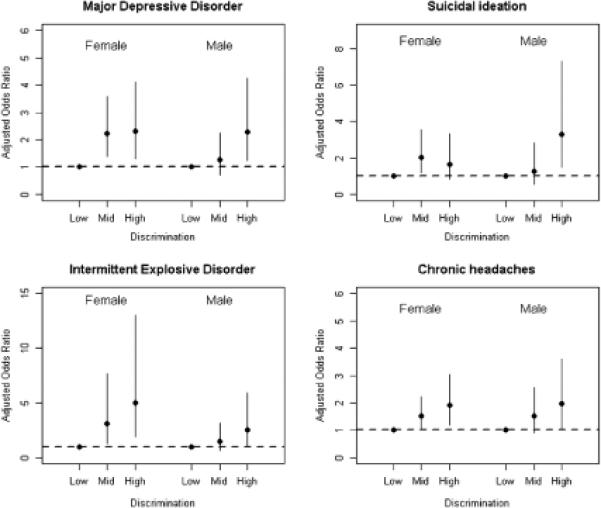
Adjusted odds ratios (ORs) and 95% confidence intervals for each of the three mental health outcomes and chronic headaches, stratified by gender and discrimination level.
Discussion
Perceived Discrimination was More Consistently Associated with Poor Mental Health than Physical Health for Both Women and Men
In accordance with our first hypothesis, we found that perceived discrimination is associated with both mental and physical health problems among women and men. However, a high level of perceived discrimination impacted mental health outcomes more than physical health outcomes for both genders. Specifically, among men, a high level of perceived discrimination increased the likelihood of having all three mental health outcomes. Among women, a high level of perceived discrimination increased the likelihood of having MDD and IED. For physical health outcomes, only chronic headaches were associated with a high level of discrimination for both genders.
This finding corroborates a review by Williams, Neighbors, and Jackson (2003), which analyzed population-based studies examining the association between discrimination and health; positive associations were found by 80% (20 of 25) of the mental health studies and half of the physical health studies (6 of 11). Gee (2002) also found a stronger association for mental health than physical health and speculated that a higher discrimination threshold may be needed for physical health effects. Similarly, our study found that a high level of discrimination was more consistently associated with mental health than physical health outcomes. One plausible explanation is that since discrimination may provoke intense and immediate emotions (such as fear, anger, and distress; Krieger, 2000), the effect of mental health may be more immediate, whereas it may take a longer time for discrimination to ultimately affect physical health (Krieger, 1999). A longitudinal study should be conducted to test this hypothesis.
The Threshold of Discrimination was Lower for Women
Unlike other ethnic groups that have shown a higher prevalence of poor health outcomes among women (Burt et al., 1995; Munce & Stewart, 2007; Weissman et al., 1999; the majority of samples are White), our univariate analysis (Table 1) demonstrated that the prevalence of mental and physical health problems among Asian American women and men were strikingly similar—the only significant difference was found for chronic headaches. Those similarities were possibly due in part to higher rates of illness reported among Asian men, compared with men of other ethnic groups, which narrows gender differences among Asian Americans (Munce & Stewart, 2007).
However, health outcomes by gender were more differentiated when comparing outcomes by specific levels of perceived discrimination (Table 2). A significantly greater proportion of women who reported experiencing medium and high levels of discrimination had physical and mental health problems. Specifically, 32% to 50% of women who reported medium to high levels of discrimination had MDD, suicidal ideation, or chronic headaches, whereas only 25% of men reporting medium to high discrimination displayed these problems. These results are noteworthy because more men reported medium to high discrimination than women (56.2% vs. 48.3%; p =.01; Table 1).
For women, even after controlling for age, education, acculturative stress, and family cohesion, a medium level of perceived discrimination consistently increased odds of every mental health outcome and chronic headaches, whereas a medium level failed to increase odds of any outcome for men. These findings, as well as findings from all the models that tested for effect modification by including a gender-by-discrimination interaction term (not shown in table), provide additional evidence for differential gender vulnerability to the potential health effects of discrimination. Therefore, our second hypothesis was supported by our data, and our finding provides indirect evidence for rejecting the idea that Asian women's persistent exposure to discrimination may lead to habituation of unfair treatment without displaying health problems.
We have three plausible explanations for this finding. First, this difference may be due to the relative decline in status for Asian women in U.S. society. Asian-American women's status relative to White women (grades and supervisory authority) has fallen significantly between the late 1970s and early 1990s (Kim & Lewis, 1994). Meanwhile, the status of Asian men relative to White men has risen, following the general societal trend toward greater equality (Kim & Lewis, 1994). Thus, institutional discrimination may contribute to many of the economic inequalities and restrictions Asian women may endure, increasing their vulnerability to lower thresholds of discrimination. Also, it is possible that Asian-American women have become more vulnerable to discrimination owing to the chronic, subtle, or overt experiences of unfair treatment stemming from their double minority status.
Second, we need to consider that the mean age of our sample of women was 40 years old and the majority (80%) were born in Asian countries. These women might have been exposed to greater sexism in their native Asian countries (Clark, 2000; Pek & Leong, 2003). It is possible that they may have not developed adequate coping skills to deal with unfair events, resulting in passive acceptance of unfair treatment in their native countries. Having effective coping skills appears to reduce the effects of discrimination on physical health outcomes among minorities (James, Lovato, & Khoo, 1994; James, LaCroix, & Kleinbaum, 1984). The NLASS did not include an adequate measure for coping skills related to discrimination. Future studies should conduct a more thorough examination of the role of coping mechanisms in mitigating the adverse health effects of discrimination.
A third explanation is that these women experience a higher level of psychological distress than men in general, including anxiety, guilt, and conflicting demands, although the distress does not necessarily meet DSM-IV criteria (Verbrugge, 1985). Therefore, this higher level of psychological distress may make them more susceptible to sensitization to discrimination than men with similar experiences. For mental health professionals working with Asian Americans, diversity training that promotes understanding of the gender dimensions of health effects of discrimination and coping strategies for women and men could reduce the potential harm of discrimination. The findings also suggest that not examining women and men separately in discrimination research may no longer be appropriate for Asian Americans. Future research needs to attend to the potential gendered nature of responses to discrimination and systematically assess the possible discrimination threshold effects on health among other ethnic minorities.
Study Limitations
Limitations of this study include the fact that we did not stratify our samples by ethnicity because data are sparse within smaller cell sizes. However, Gee, in observing Asian subgroup differences, noted that discrimination was associated with pain and respiratory conditions for both Vietnamese and Filipinos, but not for Chinese (Gee et al., 2007). Therefore, gender differences should be further examined within each Asian subgroup. Second, our use of cross-sectional data limits causal inference of the effect of discrimination on health, illustrating an urgent need for a longitudinal study (Williams, 1999). A third limitation involves our measurement of discrimination. This scale only captures the frequency of discriminatory experiences and lacks time-related factors such as duration, intensity of exposure, and period of exposure (ever versus recently; Krieger, 1999). Also, discrimination may be under- or over-reported based on bias or differing interpretations of discriminatory experiences by participants.
Conclusion
This study underscores that the health of both women and men are negatively affected by discrimination; however, the perceived discrimination threshold was lower for women in affecting their mental and physical health. We still need to search for answers to several important questions on this topic: What are the biological, social, and political mechanisms or processes by which discrimination can lead to changes in health? Does discrimination require less time to affect mental health than physical health? What are the protective factors for discrimination and how do these factors differ by gender? Ameliorating human suffering and addressing social justice is the foundation of public health (Krieger, 1999). Eradicating health problems associated with discrimination requires an interpersonal, bottom-up approach, which involves behavioral interventions aimed at the individual level (Noh & Kaspar, 2003; Rollock & Gordon, 2000). However, this individualized intervention alone will not eliminate health disparities; the health of minority women is determined in the context of larger historical, geographic, sociopolitical, and economic levels (Williams, Costa, Odunlami, & Mohammed, 2008). Therefore, an institutional, top-down approach is also needed to strengthen public health policies and laws that protect human rights of ethnic minorities (Rollock & Gordon, 2000; United Nations, 2001). Health policy should incorporate gender-based strategies that highlight the importance of gender differences, gender sensitivity, and gender-specific needs in delivering health care (Khoury & Weisman, 2002). Promotion of these approaches will be a key to reducing health disparities among both Asian-American women and men.
Acknowledgments
An earlier version of this article was presented at the annual meeting of American Public Health Association, Philadelphia, November, 2009.
Funded by Research Supplement to Promote Diversity in Health-Related Research, National Institute on Alcohol Abuse and Alcoholism (5P60AA1375905).
References
- Amaro H, Russo NF, Johnson J. Family and work predictors of psychological well-being among Hispanic women professionals. Psychology of Women Quarterly. 1987;11:505–521. [Google Scholar]
- American Pain Foundation Voices of chronic pain survey. 2006 Available: http://www.painfoundation.org/newsroom/reporter-resources/voices-survey-report.pdf.
- Angel R, Guarnaccia PJ. Mind, body, and culture: somatization among Hispanics. Social Science & Medicine. 1989;28:1229–1238. doi: 10.1016/0277-9536(89)90341-9. [DOI] [PubMed] [Google Scholar]
- Araujo BY, Borrell LN. Understanding the link between discrimination, mental health outcomes, and life chances among Latinos. Hispanic Journal of Behavioral Sciences. 2006;28:245. [Google Scholar]
- Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: Implications for group identification and well-being. Journal of Personality and Social Psychology. 1999;77:135–149. [Google Scholar]
- Brown TN, Williams DR, Jackson JS, Neighbors HW, Torres M, Sellers SL, et al. “Being black and feeling blue”: The mental health consequences of racial discrimination. Race and Society. 2000;2:117–131. [Google Scholar]
- Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25:305–313. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. American Journal of Public Health. 2008;98:485–492. doi: 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang DF. Understanding the rates and distribution of mental disorders. In: Kurasaki KS, Sue S, Okazaki S, editors. Asian-American Mental Health: Assessment Theories and Methods. Kluwer Academic/ Plenum Publishers; New York: 2002. [Google Scholar]
- Clark DN. Culture and customs of Korea. Greenwood Publishing Group; Westport, CT: 2000. [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. The American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Duldulao AA, Takeuchi DT, Hong S. Correlates of suicidal behaviors among Asian Americans. Archives of Suicide Research. 2009;13:277–290. doi: 10.1080/13811110903044567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell MP, Barnes GM. Family systems and social support: A test of the effects of cohesion and adaptability on the functioning of parents and adolescents. Journal of Marriage and the Family. 1993;55:119–132. [Google Scholar]
- Finch BK, Hummer RA, Kol B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hispanic Journal of Behavioral Sciences. 2001;23:399. [Google Scholar]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000;41:295–313. [PubMed] [Google Scholar]
- Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. American Journal of Public Health. 2002;92:615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: The added dimension of immigration. American Journal of Public Health. 2006;96:1821–1828. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health. 2007;97:1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberger E, Chen C. Perceived family relationships and depressed mood in early and late adolescence: A comparison of European and Asian Americans. Developmental Psychology. 1996;32:707–716. [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: Relationship to cardiovascular reactivity among African American and European American women. Health Psychology. 2001;20:315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho CK. An analysis of domestic violence in Asian American communities. Women & Therapy. 1990;9:129–150. [Google Scholar]
- James K, Lovato C, Khoo G. Social identity correlates of minority workers' health. Academy of Management Journal. 1994:383–396. [Google Scholar]
- James SA, LaCroix AZ, Kleinbaum DG. John Henryism and Blood pressure differences among Black men II: The role of occupational stressors. Journal of Behavioral Medicine. 1984;7:259–275. doi: 10.1007/BF00845359. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. A longitudinal twin study of personality and major depression in women. Archives of General Psychiatry. 1993;50:853–862. doi: 10.1001/archpsyc.1993.01820230023002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Khoury AJ, Weisman CS. Thinking about women's health: the case for gender sensitivity. Womens Health Issues. 2002;12:61–65. doi: 10.1016/s1049-3867(01)00146-3. [DOI] [PubMed] [Google Scholar]
- Kim PS, Lewis GB. Asian Americans in the public service: Success, diversity, and discrimination. Public Administration Review. 1994:285–290. [Google Scholar]
- Klonoff EA, Landrine H. A measure of lifetime and recent sexist discrimination in women's lives. Psychology of Women Quarterly. 1995;19:439–470. [Google Scholar]
- Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger N. Discrimination and health. In: Berkman L, Kawachi I, editors. Social epidemiology. Oxford University Press; Oxford, England: 2000. pp. 36–75. [Google Scholar]
- Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86:1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin KM, Cheung F. Mental health issues for Asian Americans. Psychiatric Services. 1999;50:774. doi: 10.1176/ps.50.6.774. [DOI] [PubMed] [Google Scholar]
- Munce SE, Stewart DE. Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics. 2007;48:394–399. doi: 10.1176/appi.psy.48.5.394. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics . Health, United States with chartbook on trends in the health of Americans. Author; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- National Health Interview Survey (NHIS) National Center for Health Statistics. [Accessed November 23, 2009];Health Data Interactive. 2007 Available: www.cdc.gov/nchs/hdi.htm.
- Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. Journal of Health and Social Behavior. 1999;40:193–207. [PubMed] [Google Scholar]
- Noh S, Kaspar V. Perceived discrimination and depression: Moderating effects of coping, acculturation, and ethnic support. American Journal of Public Health. 2003;93:232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okazaki S. Teaching gender issues in Asian American psychology. Psychology of Women Quarterly. 1998;22:33–52. [Google Scholar]
- Pek JCX, Leong FTL. Sex-related self-concepts, cognitive styles and cultural values of traditionality-modernity as predictors of general and domain-specific sexism. Asian Journal of Social Psychology. 2003;6:31–50. [Google Scholar]
- Perez DJ, Fortuna L, Alegria M. Prevalence and correlates of everyday discrimination among US Latinos. Journal of Community Psychology. 2008;36 doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. American Journal of Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- Rieker PP, Bird CE. Rethinking gender differences in health: why we need to integrate social and biological perspectives. The Journal of Gerontology. Series B. Psychological Sciences and Social Sciences. 2005;60(Spec No 2):40–47. doi: 10.1093/geronb/60.special_issue_2.s40. [DOI] [PubMed] [Google Scholar]
- Rollock D, Gordon EW. Racism and mental health into the 21st century: Perspectives and parameters. American Journal of Orthopsychiatry. 2000;70:5–13. doi: 10.1037/h0087703. [DOI] [PubMed] [Google Scholar]
- Ryan AM, Gee GC, Laflamme DF. The Association between self-reported discrimination, physical health and blood pressure: Findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. Journal of Health Care for the Poor and Underserved. 2006;17(2 Suppl):116–132. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and white women in the Detroit metropolitan area. Social Science & Medicine. 2000;51:1639–1653. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- Schulz A, Williams D, Israel B, Becker A, Parker E, James SA, et al. Unfair treatment, neighborhood effects, and mental health in the Detroit metropolitan area. Journal of Health and Social Behavior. 2000;41:314–332. [PubMed] [Google Scholar]
- StataCorp . Stata Statistical Software: Release 10. Author; College Station, TX: 2007. [Google Scholar]
- Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. Journal of Occupational and Environmental Medicine. 2003;45:1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- United Nations . Gender Dimensions of Racial Discrimination. Office of the High Commissioner for Human Rights; Geneva, Switzerland: 2001. [Google Scholar]
- US Census Bureau . Asian population, by age and sex in the United States: 2000. Author; Washington, DC: 2002. [Google Scholar]
- US Department of Health and Human Services . Mental Health: Culture, race, and ethnicity—A supplement to mental health: A report of the Surgeon General. US Department of Health and Human Services, Substance Abuse and Mental Health Administration, Center for Mental Health Services; Rockville, MD: 2001. [PubMed] [Google Scholar]
- van Winkel R, Stefanis NC, Myin-Germeys I. Psychosocial stress and psychosis. A review of the neurobiological mechanisms and the evidence for gene-stress interaction. Schizophrenia Bulletin. 2008 doi: 10.1093/schbul/sbn101. doi:10.1093/schbul/sbn101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM. Gender and health: an update on hypotheses and evidence. Journal of Health and Social Behavior. 1985;26:156–182. [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychological Medicine. 1999;29:9–17. doi: 10.1017/s0033291798007867. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Science. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. Journal of Public Health Management and Practice. 2008 November;(Suppl):S8–S17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethnicity and Health. 2000;5(3–4):243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2:335. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]


