Abstract
BACKGROUND:
Obesity and overweight in children are an escalating problem in Canada and worldwide. Currently, little is known about the manner in which primary health care providers are responding to Canada’s obesity epidemic.
OBJECTIVE:
To determine the views, practices, challenges/barriers, and needs of a national sample of family physicians (FPs) and community paediatricians (CPs) with respect to paediatric obesity identification and management.
METHODS:
A self-administered questionnaire was mailed to a random sample of 1200 FPs and 1200 CPs across Canada between 2005 and 2006.
RESULTS:
A total of 464 FPs and 396 CPs participated. The majority of practitioners viewed paediatric obesity as an ‘important’/‘very important’ issue. Although the majority reported providing dietary (more than 85%) and exercise (98%) advice to their overweight/obese patients, practitioners’ perceived success rate in treating paediatric obesity was limited (less than 22%). Approximately 30% of FPs and 60% of CPs (P<0.05) used the recommended method to identify paediatric obesity. At least 50% of practitioners indicated that too few government-funded dietitians, a lack of success in controlling paediatric patients’ weight, time constraints and limited training were key barriers to their success. To support efforts to identify or manage paediatric obesity, practitioners identified the need for office tools, patient educational materials and system-level changes.
DISCUSSION:
Canadian primary health care providers are not adequately equipped to deal with the paediatric obesity epidemic. Effective assessment tools and treatment resources, dissemination of clinical practice guidelines, enhanced undergraduate medical education and postgraduate continuing medical education, and system-level changes are urgently needed to address this health problem.
Keywords: Child, Obesity, Prevention and control, Primary health care
Abstract
HISTORIQUE :
L’obésité et l’embonpoint chez les enfants sont un problème croissant au Canada et dans le monde. On ne sait pas encore grand-chose de la manière dont les dispensateurs de soins primaires répondent à l’épidémie d’obésité au Canada.
OBJECTIF :
Déterminer les points de vue, les pratiques, les défis, les obstacles et les besoins d’un échantillon national de médecins de famille (MF) et de pédiatres communautaires (PC) dans le cadre du dépistage et de la prise en charge de l’obésité juvénile.
MÉTHODOLOGIE :
Un échantillon aléatoire de 1 200 MF et 1 200 PC du Canada a reçu par la poste, entre 2005 et 2006, un questionnaire autoadministré.
RÉSULTATS :
Au total, 464 MF et 396 PC ont participé. La majorité des praticiens percevaient l’obésité juvénile comme un problème « important » ou « très important ». Même si la majorité déclaraient fournir des conseils en matière d’alimentation (plus de 85 %) et d’exercice (98 %) à leurs patients obèses ou qui faisaient de l’embonpoint, leur taux de succès perçu à traiter l’obésité juvénile était limité (moins de 22 %). Environ 30 % des MF et 60 % des PC (P<0,05) faisaient appel à la méthode recommandée pour dépister l’obésité juvénile. Au moins 50 % des praticiens indiquaient que le trop petit nombre de diététistes financés par le gouvernement, l’absence de succès à contrôler le poids des patients pédiatriques, les contraintes de temps et la formation limitée constituaient les principaux obstacles à leur succès. Pour soutenir les efforts en vue de dépister ou de prendre en charge l’obésité juvénile, les praticiens ont souligné le besoin de ressources pour leur bureau, de documents d’éducation des patients et de modifications au système.
EXPOSÉ :
Les dispensateurs de soins primaires du Canada sont mal outillés pour affronter l’épidémie d’obésité juvénile. Des outils d’évaluation et des ressources thérapeutiques efficaces, la diffusion de guides de pratique clinique, une meilleure formation médicale de premier cycle et un perfectionnement professionnel continu après la fin des études, de même que des modifications au système s’imposent de toute urgence pour faire face à ce problème de santé.
Obesity and overweight in children are an escalating problem, with one in three Canadian children currently either overweight or obese (1–5). Because of the health consequences often associated with these chronic conditions and the resulting burden on the health care system, identifying effective interventions targeting childhood overweight and obesity must be a priority (6,7). While population-based primary prevention strategies are undoubtedly essential to curbing the nation’s epidemic, secondary prevention of paediatric overweight/obesity is equally important (8). Given Canada’s universal primary health care system, primary care providers are well placed to help prevent and manage obesity. Intervention through primary health care settings offers an excellent opportunity to address this major health problem (8–10).
Currently, little is known about the level of preparedness for, or the manner in which primary care providers are responding to, Canada’s obesity epidemic. If primary care practitioners are not equipped to address this issue among their patients, the health and economic consequences of paediatric obesity will become burdensome to the nation’s health care system. There is an urgent need to better understand primary care providers’ preparedness and needs with respect to paediatric obesity assessment and management to identify strategies to address gaps in care; therefore, the objective of the current study was to identify the views, practices, challenges/barriers and needs of a national sample of family physicians (FPs) and community paediatricians (CPs) with respect to paediatric obesity assessment and management.
METHODS
The present descriptive study used a cross-sectional design. The research ethics boards at The University of Western Ontario (London, Ontario) and Brescia University College (London, Ontario) approved the study. The study was conducted across Canada between 2005 and 2006.
Subjects
Physicians with a practice emphasis in family medicine and community paediatricians in primary paediatric care across Canada were studied. A stratified random sampling strategy was used. Up-to-date contact information for Canadian FPs and CPs was obtained from Scotts Medical Lists, a Toronto-based company. Twelve hundred FPs and 1200 CPs were proportionally and randomly selected by province/territory and language from separate databases of 9487 FPs and 2044 CPs across Canada.
Survey instrument
The instrument was a self-administered 39-item survey regarding childhood and adolescent overweight/obesity identification and management in a primary health care setting. The instrument’s five sections assessed FPs’/CPs’ views toward paediatric overweight/obesity; current clinical practices pertaining to the identification of paediatric overweight/obesity; current clinical practices pertaining to paediatric overweight/obesity management; perceived barriers toward managing paediatric overweight/obesity; and perceived needs with regard to supporting efforts to clinically manage paediatric overweight/obesity. The format of the survey included questions that were mainly close-ended with a list of checkbox options and an ‘other’ option, and questions that were Likert-style format. A few questions were fill-in-the-blank (for estimated percentages or time) and open-ended questions (regarding resources or opinions). The questionnaire was pilot tested with 11 practitioners for readability and clarity, which resulted in minor wording changes to improve the clarity of a few questions.
Data collection
A modified Dillman’s mail survey method (11,12) was used. First, the survey (along with a letter of information), a self-addressed postage-paid return envelope and a $20 ‘Chapters’ gift certificate were mailed to the randomly selected sample. Second, a reminder card was mailed to all nonresponders five weeks after the initial mailing. Third, a second survey package was mailed to any remaining nonresponders 10 weeks after the reminder cards were sent. Finally, a third survey package was mailed to the remaining non-responders five weeks after the second mailing. Participants had the option to complete either a hard copy of the survey or an online version with a preassigned user name and password.
Data analyses
Data were entered and analyzed using SPSS version 16 (SPSS Inc, USA) for Windows (Microsoft Corporation, USA). Continuous variables were expressed as mean ± SD, while categorical variables were expressed as a percentage and 95% CI. The frequency of responses to survey questions were tabulated and summarized. χ2 procedures were performed to test for differences in survey responses between FPs and CPs. During the statistical analyses, missing values were excluded listwise, when appropriate. The level of significance for all statistical tests was set at 0.05.
RESULTS
Study populations
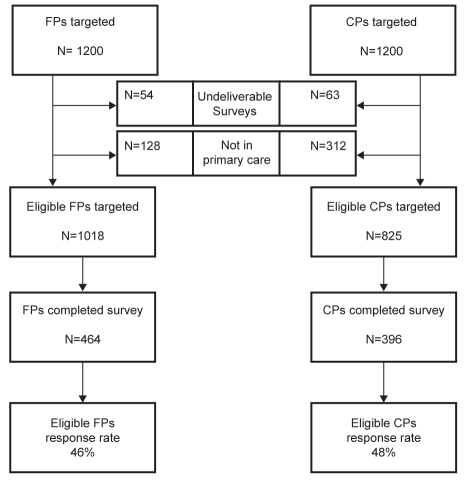
A total of 464 FPs and 396 CPs completed the survey (Figure 1). Among the 860 participants, 51 FPs and 50 CPs completed the survey online. Subjects’ demographic profiles (Table 1) revealed a diverse group of FPs and CPs.
Figure 1).
Participants’ eligibility and response rate. CPs Community paediatricians; FPs Family physicians
TABLE 1.
Demographic profile of the study population
| Demographic profile | FPs (n=464), % | CPs (n=396), % |
|---|---|---|
| Practice setting | ||
| Solo/family clinic/group | 88 | 52 |
| Community hospital | 3 | 6 |
| Teaching hospital | 3 | 27 |
| Practice in multipractitioner setting | 6 | 15 |
| Years in practice | ||
| <10 | 37 | 28 |
| 11–20 | 39 | 31 |
| >20 | 25 | 41 |
| Paediatric patient load per week | ||
| <25 | 57 | 14 |
| 26–50 | 36 | 28 |
| 51–100 | 5 | 26 |
| >100 | 2 | 32 |
| Sex | ||
| Male | 47 | 53 |
| Female | 53 | 47 |
CPs Community paediatricians; FPs Family physicians
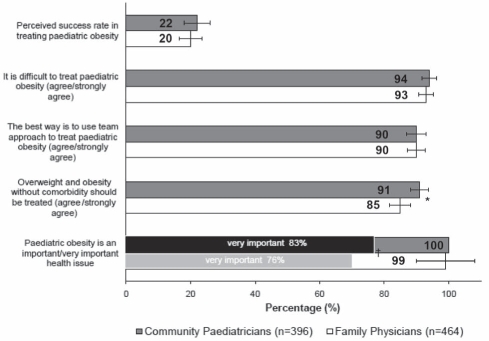
Practitioners’ views/attitudes pertaining to paediatric overweight/obesity (Figure 2)
Figure 2).
Practitioners’ views and attitudes toward paediatric obesity (error bars are 95% CI). *P<0.01 by χ2 test; †P<0.01 when comparing community paediatricians and family physicians who responded ‘very important’
Both CPs (88%) and FPs (78%) reported seeing an increase in overweight and obese paediatric patients in their practices (P<0.01) over the past 9.1±5.2 years. They estimated that the prevalence of overweight and obesity among paediatric patients was 23% and 12%, respectively. Almost all practitioners viewed paediatric obesity as an important issue, but reported a relatively low ‘perceived success rate in treating paediatric obesity’ of 20%. Significantly more CPs (91%) than FPs (85%) agreed that overweight/obesity should be treated even when no comorbidity exists, and 90% of practitioners called for a team approach to address paediatric obesity.
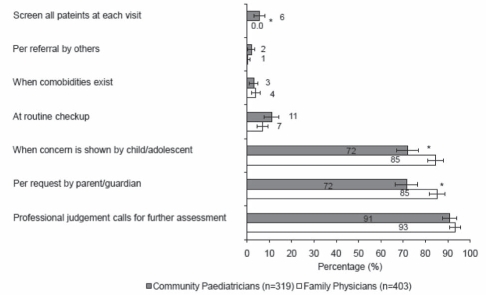
Clinical practices pertaining to paediatric overweight/obesity assessment and identification
More than 90% of the time, practitioners’ professional judgment influenced them to assess their patients for overweight and obesity (Figure 3). Also, only a small proportion of practitioners assessed patients’ weight status at routine checkups or screened all patients at each office visit.
Figure 3).
Circumstances in which practitioners assessed patients for paediatric obesity (error bars are 95% CI). *P<0.01 by χ2 test
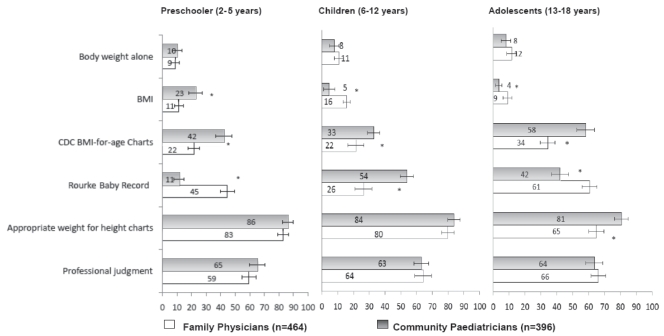
Practitioners used different methods to assess patients for paediatric overweight/obesity (Figure 4). Significantly more FPs than CPs used the Rourke Baby Record. Close to 60% of CPs, but only approximately 30% of FPs, reported using the recommended method/tool for classifying overweight and obesity among Canadian children and adolescents, ie, the United States Centers for Disease Control and Prevention (CDC)’s body mass index (BMI)-for-age references (13).
Figure 4).
Methods used by practitioners to assess paediatric obesity (error bars are 95% CI). *P<0.01 by χ2 test. BMI Body mass index; CDC Centers for Disease Control and Prevention (USA)
Practitioners also used different criteria to diagnose overweight and obesity among paediatric patients (Table 2). Significantly more CPs than FPs reported using the CDC BMI-for-age 85th and 95th percentile criteria recommended for screening Canadian children and adolescents for overweight and obesity (13).
TABLE 2.
Criteria used by practitioners to diagnose overweight and obesity, by age group
| Identification criteria by age group |
Overweight |
Obesity |
||||||
|---|---|---|---|---|---|---|---|---|
|
FPs |
CPs |
FPs |
CPs |
|||||
| n (%) | 95% CI | n (%) | 95% CI | n (%) | 95% CI | n (%) | 95% CI | |
| Preschoolers (2–5 years) | 340 | – | 304 | – | 337 | – | 304 | – |
| >120% of ideal body weight | 55 (16) | 12–20 | 112 (37) | 32–42** | – | – | – | – |
| Weight-for-height >85th percentile | 43 (13) | 9–17 | 57 (19) | 15–23 | 18 (5) | 3–7 | 18 (6) | 3–9 |
| Weight-for-height >95th percentile | 81 (24) | 19–29 | 127 (42) | 36–48** | 181 (54) | 49–59 | 133 (44) | 38–50 |
| A BMI >25 kg/m2 for overweight or >30 kg/m2 for obesity | 32 (9) | 6–12 | 37 (12) | 8–16 | 61 (18) | 14–22 | 72 (24) | 19–29 |
| BMI-for-age >85th percentile | 146 (43) | 38–48 | 94 (31) | 26–36* | 9 (3) | 1–5 | 14 (5) | 3–7 |
| BMI-for-age >95th percentile | 82 (24) | 19–29 | 73 (24) | 19–29 | 111 (33) | 28–38 | 149 (49) | 43–55* |
| Children (6–12 years) | 368 | – | 314 | – | 360 | – | 314 | – |
| >120% of ideal body weight | 69 (19) | 15–24 | 111 (35) | 30–40* | – | – | – | – |
| Weight-for-height >85th percentile | 77 (21) | 17–26 | 81 (26) | 21–31 | 19 (5) | 3–7 | 23 (7) | 4–10 |
| Weight-for-height >95th percentile | 107 (29) | 25–34 | 151 (48) | 42–54** | 167 (46) | 41–51 | 129 (41) | 36–46 |
| A BMI >25 kg/m2 for overweight or >30 kg/m2 for obesity | 39 (11) | 8–15 | 41 (13) | 9–17 | 107 (30) | 25–35 | 102 (33) | 28–38 |
| BMI-for-age >85th percentile | 137 (37) | 32–42 | 95 (30) | 25–35 | 13 (4) | 2–6 | 22 (7) | 4–10 |
| BMI-for-age >95th percentile | 91 (25) | 21–30 | 73 (23) | 18–28 | 136 (38) | 33–43 | 171 (55) | 49–61* |
| Adolescents (13–18 years) | 404 | – | 320 | – | 382 | – | 312 | – |
| >120% of ideal body weight | 77 (19) | 15–23 | 109 (34) | 29–39* | – | – | – | – |
| Weight-for-height >85th percentile | 86 (21) | 17–25 | 89 (28) | 23–33 | 14 (4) | 2–6 | 24 (8) | 5–11 |
| Weight-for-height >95th percentile | 50 (12) | 9–15 | 70 (22) | 17–27* | 108 (28) | 23–33 | 123 (39) | 34–44* |
| A BMI >25 kg/m2 for overweight or >30 kg/m2 for obesity | 216 (54) | 49–59 | 104 (33) | 28–38** | 226 (59) | 54–64 | 117 (38) | 33–43* |
| BMI-for-age >85th percentile | 103 (26) | 22–30 | 160 (50) | 45–55** | 12 (3) | 1–5 | 28 (9) | 6–12 |
| BMI-for-age >95th percentile | 38 (9) | 6–12 | 48 (15) | 11–19 | 124 (33) | 28–38 | 181 (58) | 53–63** |
Subjects with missing values were excluded.
P<0.05;
P<0.01 by χ2 test. BMI Body mass index; CPs Community paediatrician; FPs Family physician
After diagnosis, the majority of practitioners assessed patients’ weight history, physical activity and eating patterns, home environment, risk factors for diabetes, patients’ and their parents’ expectation of weight management, as well as other metabolic abnormalities (Table 3).
TABLE 3.
Practitioners’ practices on diagnosing paediatric overweight and obesity
|
Family physicians |
Community paediatricians |
|||
|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | |
| Further assessment | 410 | – | 325 | – |
| Patients’ weight history | 357 (87) | 84–90 | 312 (96) | 94–98* |
| Patients’ physical activity patterns independent of an exercise physiologist | 314 (77) | 73–81 | 264 (81) | 77–85 |
| Patients’ dietary patterns independent of a dietitian | 310 (76) | 71–80 | 268 (83) | 78–87 |
| Patients’ home environment for supportive structures | 310 (76) | 71–80 | 272 (84) | 80–88* |
| Risk factors for type 2 diabetes | 301 (73) | 69–78 | 239 (74) | 69–78 |
| Childs’/adolescents’ expectations of weight management (eg, realistic goals) | 299 (73) | 69–77 | 242 (75) | 70–79 |
| Parents’/guardians’ expectations of weight management (eg, realistic goals) | 281 (69) | 64–73 | 240 (74) | 69–79 |
| Investigate for metabolic abnormalities associated with obesity | 231 (56) | 51–61 | 195 (60) | 55–65 |
| Patients’ attitude/interest toward change at first contact (eg, using ‘stages of change’ model) | 225 (55) | 50–60 | 174 (54) | 48–59 |
| Patients’ dietary patterns with the aid of a dietitian | 165 (40) | 35–45 | 177 (55) | 49–60* |
| Patients’ physical activity patterns with the aid of an exercise physiologist | 13 (3) | 1–5 | 16 (5) | 3–7 |
| Actions taken on identification | 408 | – | 328 | – |
| See patients together with parent or guardian | 388 (95) | 93–97 | 317 (97) | 95–99 |
| Discuss health consequences of paediatric obesity | 330 (81) | 77–85 | 295 (90) | 87–93* |
| Inform the parent/guardian about children’s need to control/lose weight | 327 (80) | 76–84 | 290 (88) | 85–92* |
| Refer patients to other health care professionals | 253 (62) | 57–67 | 217 (66) | 61–71 |
| Prescribe medication for associated metabolic abnormalities such as hyperlipidemia | 33 (8) | 5–11 | 24 (7.3) | 4–10 |
| Prescribe medication to help control appetite | 3 (1) | 0–2 | 2 (0.6) | 0–1 |
| Prescribe weight-management medication | 3 (1) | 0–2 | 4 (1.2) | 0–2 |
Subjects with missing values were excluded.
P<0.05 by χ2 test
Clinical practices pertaining to paediatric overweight/obesity management
On average, FPs spent 13±8.8 min and 10±6.0 min in initial and follow-up consultations, respectively, with overweight/obese paediatric patients, while CPs took significantly more time (23±17 min for initial and 13±8.3 min for follow-up visits). More than 85% of practitioners reported that they routinely provided both dietary (eg, to ‘increase overall consumption of fruits and vegetables’) and physical activity (eg, to ‘increase patient’s physical activity level’) advice to the parents of overweight/obese children and adolescents (Table 4).
TABLE 4.
Practitioners’ advice on lifestyle modification on identifying overweight and obesity
|
Family physicians |
Community paediatricians |
|||
|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | |
| Dietary advice | 381 | – | 306 | – |
| To increase overall consumption of fruits and vegetables | 339 (89) | 86–92 | 264 (86) | 82–90 |
| To choose healthier snacks | 329 (86) | 83–90 | 264 (86) | 82–90 |
| To follow Canada’s Food Guide | 310 (81) | 77–85 | 207 (68) | 62–73 |
| To choose water over sugary beverages | 310 (81) | 77–85 | 259 (85) | 81–89 |
| To make healthy choices for the family as a whole | 293 (77) | 73–81 | 254 (83) | 79–87 |
| To have smaller portion sizes at home or when eating out | 269 (71) | 66–75 | 226 (74) | 69–79 |
| To select whole grain breads and cereals more often | 264 (69) | 65–74 | 210 (69) | 63–74 |
| To eat out less often at fast food restaurants | 263 (69) | 64–74 | 205 (67) | 62–72 |
| To reduce total fat intake | 252 (66) | 61–71 | 183 (60) | 54–65 |
| For parents/guardians to serve as a role model for healthy eating | 246 (65) | 60–69 | 220 (72) | 67–77 |
| To use healthier cooking methods | 232 (61) | 56–66 | 152 (50) | 44–55 |
| To eat fewer total kilocalories | 224 (59) | 54–64 | 213 (70) | 64–75* |
| To read food labels | 195 (51) | 46–56 | 136 (44) | 39–50 |
| To select reduced-fat dairy foods more often | 163 (43) | 38–48 | 156 (51) | 45–57 |
| To keep food records to maintain a healthy eating pattern | 80 (21) | 17–25 | 70 (23) | 18–28 |
| To follow a low-carbohydrate diet | 76 (20) | 16–24 | 63 (21) | 16–25 |
| To reduce overall consumption of red meat/ground meat | 74 (19) | 15–23 | 46 (15) | 11–19 |
| To follow a high-protein diet | 25 (7) | 4–9 | 22 (7) | 4–10 |
| Physical activity advice | 398 | – | 308 | – |
| To increase patient’s physical activity level | 391 (98) | 97–100 | 303 (98) | 97–100 |
| To increase family’s physical activity level | 303 (76) | 72–80 | 253 (82) | 78–86 |
| To incorporate various types of appropriate physical activity into the patient’s daily lifestyle | 289 (73) | 68–77 | 239 (78) | 73–82 |
| For parents to serve as a role model for physical activity | 256 (64) | 60–69 | 197 (64) | 59–69 |
| To decrease screen viewing time | 251 (63) | 58–68 | 251 (82) | 77–86* |
| To follow Canada’s guidelines for increasing physical activity using the appropriate ‘physical activity’ | 92 (23) | 19–27 | 99 (32) | 27–37* |
| To follow the advice and activities using the Canadian Paediatric Society’s “Prescription for Healthy Active Kids” | 54 (14) | 10–17 | 139 (45) | 40–51* |
| To enroll patient in a community slimming group | 19 (5) | 3–7 | 44 (14) | 10–18* |
Subjects with missing values were excluded.
P<0.05 by χ2 test
Perceived barriers/challenges to managing paediatric overweight/obesity (Table 5)
TABLE 5.
Practitioners’ perceived barriers to paediatric overweight and obesity management
|
Family physicians |
Community paediatricians |
|||
|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | |
| Practice barriers | 412 | – | 320 | |
| Too few government-funded dietitians to refer patients to | 292 (71) | 66–75 | 214 (67) | 62–72 |
| Lack of success in controlling paediatric patients’ weight | 210 (51) | 46–56 | 200 (63) | 57–68* |
| Time constraints prevent meaningful discussion and monitoring | 269 (66) | 61–71 | 160 (50) | 44–56* |
| Limited professional training | 265 (65) | 60–70 | 162 (50) | 44–56* |
| Lack of availability of team support for family-based intervention | 245 (60) | 55–65 | 223 (69) | 64–74 |
| Concern regarding hurting patients’ self-esteem | 197 (48) | 43–53 | 105 (33) | 28–39* |
| Too few specialists to refer patients to | 211 (51) | 46–56 | 143 (45) | 40–51 |
| Lack of appropriate education materials for primary caregivers | 188 (46) | 41–51 | 93 (29) | 24–34* |
| Lack of appropriate education materials for parents and/or patients | 179 (44) | 39–49 | 121 (38) | 33–44 |
| Billing constraints | 151 (37) | 32–42 | 82 (26) | 21–31* |
| Concern that discussing overweight/obesity with adolescents may precipitate an eating disorder | 113 (27) | 23–32 | 64 (20) | 16–25 |
| Lack of culturally sensitive education materials for parents and/or patients | 120 (29) | 25–34 | 109 (34) | 29–40 |
| Concern that discussing overweight/obesity with children may precipitate an eating disorder | 65 (16) | 13–20 | 35 (11) | 8–15 |
| Patients’ barriers | 403 | – | 320 | – |
| Parents/guardians who are overweight/obese serve as poor role models | 352 (87) | 84–91 | 289 (90) | 87–94 |
| Patients show poor compliance with recommendations to make lifestyle changes | 318 (79) | 75–83 | 275 (86) | 82–90 |
| Lack of interest on the part of child/adolescent to change lifestyle behaviours | 282 (70) | 66–74 | 234 (73) | 68–78 |
| Lack of interest on the part of parent/guardian to help paediatric patients change lifestyle | 249 (62) | 57–67 | 217 (68) | 63–73 |
| Lack of family financial resources toward healthy food choices and physical activity | 228 (57) | 52–61 | 144 (45) | 40–50 |
| Parents/guardians become defensive when the issue of their child’s weight is addressed | 196 (49) | 44–53 | 159 (50) | 44–55 |
| Lack of patient compliance as communicated by parents/guardians | 184 (46) | 41–51 | 182 (57) | 51–62* |
| Parents/guardians deny their child has a weight problem | 150 (37) | 32–42 | 143 (45) | 39–50 |
| Parents use food as a means of reward/punishment | 150 (37) | 32–42 | 137 (43) | 37–48 |
| System barriers | 410 | – | 321 | – |
| Children live in an obesogenic environment/society | 294 (72) | 68–76 | 243 (76) | 71–81 |
| Lack of healthy public policies, eg, federal and provincial program/services | 132 (32) | 27–37 | 117 (36) | 31–41 |
Subjects with missing values were excluded.
P<0.05 by χ2 test
More than one-half of practitioners indicated that the key practice barriers to managing paediatric overweight/obesity included too few government-funded dietitians to refer patients to; a lack of success in controlling paediatric patients’ weight; time constraints that prevent meaningful discussion with, and monitoring of patients; limited professional training; and a lack of available team support for family-based interventions. More than 60% of practitioners indicated that the key barriers to obesity management that pertain to patients and their families include overweight/obese parents/guardians who are poor role models; patients’ poor compliance with recommended lifestyle changes; child/adolescent patients’ lack of interest in changing their lifestyle behaviours; and parents’/guardians’ lack of interest in helping paediatric patients change their lifestyle. Finally, more than 70% of practitioners identified the obesogenic environment/society in which children live as a key system barrier to paediatric obesity management.
Perceived needs to support the management of paediatric overweight/obesity (Table 6)
TABLE 6.
Practitioners’ perceived needs with regard to paediatric obesity assessment and management
|
Family physicians |
Community paediatricians |
|||
|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | |
| System needs | 411 | – | 323 | – |
| To reinforce quality daily physical activity in schools | 344 (83.7) | 80–87 | 264 (82) | 77–86 |
| To develop/reinforce healthy food policies/programs in schools | 319 (77.6) | 74–82 | 253 (78) | 74–83 |
| To increase access to government-funded outpatient dietitians | 317 (77.1) | 73–81 | 225 (70) | 65–75 |
| To increase community-based fitness programs/services | 298 (73) | 68–77 | 246 (76) | 72–81 |
| To establish/increase outpatient weight management clinics/programs | 264 (64) | 60–69 | 235 (73) | 68–78 |
| To stop/control unhealthy/junk food commercials | 260 (63) | 59–68 | 219 (68) | 63–73 |
| To stop/tax unhealthy/junk foods selling | 227 (55) | 50–60 | 180 (56) | 50–61 |
| To amend billing code to include paediatric obesity identification/management | 216 (53) | 48–57 | 154 (48) | 42–53 |
| To develop/revise clinical practice guidelines pertaining to paediatric obesity identification/management | 172 (42) | 37–47 | 134 (42) | 36–47 |
| Needs for office tools/resources | 376 | – | 310 | – |
| Body mass index-for-age chart | 325 (86) | 83–90 | 256 (83) | 78–87 |
| Local effective family-based intervention programs/outpatient weight management clinics | 241 (64) | 59–69 | 214 (69) | 64–74 |
| Prescription for healthy active kids | 236 (63) | 58–68 | 196 (63) | 58–69 |
| Prescription for healthy living | 229 (61) | 56–66 | 190 (61) | 56–67 |
| Healthy active living | 217 (58) | 53–63 | 209 (67) | 62–73 |
| Childhood overweight assessment and action flow chart | 211 (56) | 51–61 | 180 (58) | 53–64 |
| Computerized information | 140 (37) | 32–42 | 119 (38) | 33–44 |
| Resources/materials for patients | 363 | – | 292 | – |
| Canada’s Food Guide | 307 (85) | 81–88 | 253 (87) | 83–91 |
| Family guide to physical activity for children | 278 (77) | 72–81 | 227 (78) | 73–82 |
| Family guide to physical activity for youth | 273 (75) | 71–80 | 227 (78) | 73–82 |
| Canada’s Physical Activity Guide for children | 260 (72) | 67–76 | 214 (73) | 68–78 |
| Canada’s Physical Activity Guide for adolescents/youth | 250 (69) | 64–74 | 203 (70) | 64–75 |
| Physical activity chart and stickers | 190 (52) | 47–57 | 161 (55) | 49–61 |
| Healthy recipes to take home | 125 (34) | 30–39 | 120 (41) | 35–47 |
Subjects with missing values were excluded
The primary needs that practitioners indicated would support their efforts to manage paediatric overweight/obesity include system-level change (reinforced quality daily physical activity in schools, development of reinforced healthy food policies/programs in schools, increased access to government-funded dietitians, increased community-based fitness programs/services, and amended billing codes that include clinical activities related to the identification and management of paediatric overweight/obesity); ready availability of office tools (eg, BMI-for-age charts); and patient resources such as educational materials for overweight/obese patients and their families.
DISCUSSION
The present study was the first of its kind to systematically explore a representative random sample of Canadian FPs’ and CPs’ current views, practices, and perceived challenges and needs as they relate to diagnosing and managing paediatric overweight and obesity. The present study indicated that Canadian primary care providers are inadequately equipped to address the burgeoning paediatric obesity epidemic. The key practice barriers to successfully managing paediatric overweight/obesity listed by practitioners included the following: too few government-funded dietitians, a lack of success in controlling paediatric patients’ weight, time constraints, limited professional training and a lack of available team support for family-based interventions. Practitioners identified a need for system-level changes, office tools and patient education materials to support their clinical efforts to manage their paediatric patients’ weight. Given Canada’s universal health care system, timely action is needed to sufficiently equip primary care providers to address this national epidemic. In addition, differences were observed between FPs’ and CPs’ views and practices in identifying, managing and advising overweight/obese paediatric patients, suggesting that FPs are in greater need of support, resources and training than CPs.
Although it is encouraging that practitioners perceived paediatric obesity as an important health issue and correctly estimated the trend of obesity prevalence in Canada, it appears that the primary care system is not sufficiently equipped to combat this extremely complex issue. Practitioners in the current study believed that they had limited professional training in how to manage/treat paediatric obesity, which is consistent with research in other countries where primary care professionals felt challenged and considered themselves ill-equipped to deal with this escalating health problem (7,14–18). Our results indicated that time constraints only allowed practitioners to spend a limited amount of time with their overweight/obese patients. For instance, FPs spent, on average, 13 min for initial and 10 min for follow-up consultations. One-half of practitioners believed that current billing codes limit their ability to provide preventive care for paediatric patients and their families. Furthermore, many practitioners reported relying on their professional judgment or adult diagnostic criteria to identify paediatric obesity because they were unaware of, or lacked access to, appropriate diagnostic tools and guidelines. These issues, in addition to the key practice, patient/family and system barriers identified, may explain why the practitioners’ perceived success rate in treating overweight/obesity among their paediatric patients was relatively low, even though the majority of practitioners provided consultation encouraging healthy eating and active living.
The present study identified challenges/needs that must be addressed to better equip Canada’s primary care practitioners to identify and manage paediatric overweight/obesity. First, enhanced undergraduate medical education and postgraduate continuing medical education, including ‘childhood obesity webinars/webcasts/podcasts’, are urgently needed to educate and encourage practitioners to use the recommended method (ie, CDC’s BMI-for-age references) to diagnose paediatric overweight and obesity. However, for this to be successful in supporting the accurate identification of overweight/obesity among paediatric patients, there must be improved dissemination of the recent Canadian clinical practice guidelines on the management and prevention of obesity (13). Practitioners also indicated a need for relevant office tools to support the accurate identification and management of paediatric obesity. Convenient paediatric BMI calculators and accessible BMI charts should, therefore, be made available to practitioners to facilitate their use of the CDC age- and sex-specific BMI references to diagnose paediatric overweight and obesity in primary care settings. Second, brief strategies are needed to help busy practitioners identify patients’ obesity-related risk factors during short routine appointments and provide patients with appropriately tailored healthy lifestyle messages/materials. An obesity risk factor checklist to review with patients, along with a series of age-appropriate educational resources for those diagnosed with or at risk of overweight/obesity, may aid health practitioners in customizing healthy living messages to facilitate timely behavioural change. Third, as emphasized by practitioners in the present study, team support is necessary to address the complex issue of paediatric weight management. An interdisciplinary team approach, such as Ontario’s ‘Family Health Teams’ in which FPs and other complementary professionals (eg, nurses, nurse practitioners and dietitians) work collaboratively, would offer enhanced opportunities for paediatric obesity management in the Canadian primary health care setting, as well as support for family-based interventions (19). Furthermore, when appropriate, an expert in behaviour change, such as a psychologist or psychiatrist, may be added to the health care team (20). Fourth, effective – yet nonjudgmental – strategies should be developed and implemented by primary health care teams to help parents understand and recognize their children’s weight problems. Parents’ actions as positive role models, as well as their support and active involvement in family-based lifestyle changes, are essential to paediatric weight management. Fifth, system changes, such as revised billing codes, would facilitate the primary care system’s redirection toward a more bottom-up approach – ie, preventive care – to address obesity from childhood as opposed to through secondary prevention. Finally, it is important that, among other strategies, policy and decision makers strive to reinforce quality daily physical activity and develop/reinforce healthy food policies/programs in schools in an effort to change the obesogenic environment in which our children and adolescents currently grow up.
The authors acknowledge that there are limitations to the present study. First, the mail-out survey resulted in response rates of 46% and 48% in FPs and CPs, respectively. There may have been self-selection bias, in that respondents may have been keener to discuss the issue of paediatric obesity than nonrespondents; however, these response rates were comparable with those of similar research (21,22). Second, data obtained through the questionnaires in the current study were subjective measures, which may be subject to social desirability bias and may have also influenced their ‘perceived success rate in treating paediatric obesity’. Participants may have checked options on the questionnaire with respect to clinical practices that they believed were correct, based on their professional conscience. An alternative data collection method, such as chart audits, may more accurately reflect practitioners’ current practices.
Acknowledgments
This study was jointly funded by the Canadian Institutes of Health Research and The Heart and Stroke Foundation of Canada. The authors are very appreciative of Ms Mandy Ho (Research Assistant) for her extreme dedication toward sampling study subjects, data collection, entering and verifying data. The authors are very grateful to Ms Melissa van Zandvoort (Research Associate) and Ms Gillian Mandich (Research Assistant for the Public Health Research, Education and Development Program at the Middlesex-London Health Unit) for their dedicated work in revising and formatting the draft manuscript, and to Mr Bernie Lueske (Data Analyst for the Public Health Research, Education and Development Program at the Middlesex-London Health Unit) for his assistance in data analysis. The authors sincerely thank all family physicians and community paediatricians who took time out of their busy schedules to participate in the study. Appreciation is also extended to the students in the Work-Study Program at Brescia University College for their assistance in survey mailing, data entry and verification.
Footnotes
SOURCES OF SUPPORT: This study was jointly funded by the Canadian Institutes of Health Research and The Heart and Stroke Foundation of Canada.
REFERENCES
- 1.Tremblay MS, Katzmarzyk PT, Willms JD. Temporal trends in overweight and obesity in Canada, 1981–1996. Int J Obes Relat Metab Disord. 2002;26:538–43. [PubMed] [Google Scholar]
- 2.Canning PM, Courage ML, Frizzell LM. Prevalence of overweight and obesity in a provincial population of Canadian preschool children. CMAJ. 2004;171:240–2. doi: 10.1503/cmaj.1040075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He M, Sutton J. Using routine growth monitoring data for the tracking of obesity prevalence in young children. Can J Public Health. 2004;95:419–23. doi: 10.1007/BF03403984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He M, Beynon C. Prevalence of overweight and obesity in school-aged children. Can J Diet Pract Res. 2006;67:125–9. doi: 10.3148/67.3.2006.125. [DOI] [PubMed] [Google Scholar]
- 5.Tjepkema M, Shields M. Measured obesity: Overweight Canadian children and adolescents. Ottawa: Statistics Canada; 2005. [Google Scholar]
- 6.Price JH, Desmond SM, Ruppert ES, Stelzer CM. Pediatricians’ perceptions and practices regarding childhood obesity. Am J Prev Med. 1989;5:95–103. [PubMed] [Google Scholar]
- 7.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–4. [PubMed] [Google Scholar]
- 8.Wake MA, McCallum Z. Secondary prevention of overweight in primary school children: What place for general practice? Med J Aust. 2004;181:82–4. doi: 10.5694/j.1326-5377.2004.tb06179.x. [DOI] [PubMed] [Google Scholar]
- 9.Fowler-Brown A, Kahwati LC. Prevention and treatment of overweight in children and adolescents. Am Fam Physician. 2004;69:2591–8. [PubMed] [Google Scholar]
- 10.Shephard RJ. Role of the physician in childhood obesity. Clin J Sport Med. 2004;14:161–8. doi: 10.1097/00042752-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Dillman D. Mail and Internet surveys: The tailored designed method. 2 edn. Toronto: John Wiley & Sons; 2000. [Google Scholar]
- 12.Harris SB, Petrella RJ, Anita Lambert-Lanning A, Leadbetter W, Cranston L. Lifestyle management for type 2 diabetes. Can Fam Physician. 2004;50:1235–43. [PMC free article] [PubMed] [Google Scholar]
- 13.Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary] CMAJ. 2007;176:S1–13. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36:669–75. doi: 10.1016/s0091-7435(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 15.Fogelman Y, Vinker S, Lachter J, Biderman A, Itzhak B, Kitai E. Managing obesity: A survey of attitudes and practices among Israeli primary care physicians. Int J Obes Relat Metab Disord. 2002;26:1393–7. doi: 10.1038/sj.ijo.0802063. [DOI] [PubMed] [Google Scholar]
- 16.Jelalian E, Boergers J, Alday CS, Frank R. Survey of physician attitudes and practices related to pediatric obesity. Clin Pediatr (Phila) 2003;42:235–45. doi: 10.1177/000992280304200307. [DOI] [PubMed] [Google Scholar]
- 17.Franc C, van GM, Le VM, Rosman S, Pelletier-Fleury N. French pediatricians’ knowledge, attitudes, beliefs towards and practices in the management of weight problems in children. Health Policy. 2009;91:195–203. doi: 10.1016/j.healthpol.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 18.van GM, Franc C, Rosman S, Le VM, Pelletier-Fleury N. Primary care physicians’ knowledge, attitudes, beliefs and practices regarding childhood obesity: A systematic review. Obes Rev. 2009;10:227–36. doi: 10.1111/j.1467-789X.2008.00532.x. [DOI] [PubMed] [Google Scholar]
- 19.Ontario Ministry of Health and Long-Term Care Understanding Family Health Teams. 2008.
- 20.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154:220–6. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 21.Trowbridge FL, Sofka D, Holt K, Barlow SE. Management of child and adolescent obesity: Study design and practitioner characteristics. Pediatrics. 2002;110:205–9. [PubMed] [Google Scholar]
- 22.Siemens R, Issenman RM. Healthy active living: A goal or a mirage? A survey of Canadian paediatricians. Paediatr Child Health. 2004;9:163–5. doi: 10.1093/pch/9.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]