Abstract
The objective of this study was to examine lay health advisor (LHA) programs designed to promote health among US Latinos and the extent to which educator-only versus educator-plus-bridge programs differed in designs and outcomes achieved. Two independent coders reviewed 128 published articles on LHAs yielding information at two levels: (i) study design and participant and LHA characteristics from 61 studies that broadly compared educator-only versus educator-plus-bridge programs and (ii) implementation features and outcomes from 17 randomized controlled trials or quasi-experimental studies with outcome data. LHA programs have been widely used with Latinos in certain US regions; our findings indicate that LHAs are effective intervention agents. We identified differences between educator-only and educator-plus-bridge LHA programs, although the small number of educator-plus-bridge programs with outcome data limited comparisons. Major gaps remain in research targeting Latino subgroups other than Mexican immigrants/Mexican Americans. Sufficient research has evaluated LHA programs among Latinos on their ability to achieve health behavior and/or health status changes. In the future, more of a focus on organizational and policy changes is warranted. Questions remain about diversity in LHAs’ characteristics and roles, which influence not only outcomes but also program sustainability and dissemination.
Introduction
In 2002, Latinos became the largest minority population and the fastest growing subgroup in the United States. Current estimates place the US Latino population at 44.3 million; Latino growth rate in the United States is three times that of the total population [1]. With this population surge, health care systems are faced with the challenge of finding the most effective methods for addressing Latino health needs, especially access to health care services. Citizenship and language barriers limit access for Latinos to the health care safety net [2]. Approximately 30% of Latinos report having had a problem communicating with health providers over the past year [3]. In addition, a Kaiser Family Foundation study found that 36% of Latinos have no health insurance—the highest percentage of any US subpopulation. Among low-wage workers, 63% of Latino non-US citizens and 36% of Latino US citizens are uninsured.
Language and cultural difference, and lack of familiarity with American health care delivery models require innovative strategies to increase Latinos’ access to health care. Compounding these challenges are barriers imposed by the structure of health care organizations that often fail to include adequate systems for reaching vulnerable populations [4]. Lay health advisors (LHAs) have emerged as a potentially effective approach for improving Latinos’ access to care, health outcomes, and health behaviors. The LHA approach trains community members who are similar to the target population and, in some cases, known and trusted members of the community. LHAs are known by many other names, including promotoras(es), community health workers (CHWs), community health advisors, community health aides, natural helpers, peer educators, and peer outreach workers. (In Spanish, promoter is masculine and promotora feminine/singular; promotoras is feminine/plural and promotores masculine or mixed gender/plural.) [5]. In January 2009, the Office of Management and Budget formally recognized CHW as an occupational classification and it is now listed in the 2010 Standard Occupation Classifications. Regardless of the term used, these individuals, once trained, serve to bridge the gap between their communities’ needs and the delivery of health services [6–10].
The LHA movement worldwide accelerated following the Alma Ata Declaration in 1978 [11]; the Declaration defined health holistically as a state of ‘physical, mental and social well-being, and not just the absence of disease’ [11]. This broad definition of health spurred the role development of LHAs as a necessary link between primary health care delivery systems and communities in need of better health services. LHAs were envisioned as integral members of national health care teams, working hand in hand with professional staff to serve the ‘unmet curative, preventive and promotive needs of village communities’ [10].
The range of activities and issues addressed by LHAs is broad and their geographic reach wide [12]. In Latin America, the work of the Brazilian educator Paulo Freire and others in the popular education movement in the 1960s and 1970s catalyzed this approach, leading to the creation of a formalized role for LHAs across the continent. Examples are numerous, including the following: Guatemala, where indigenous LHAs have been trained to deliver messages to rural men on reproductive health as a method to increase rates of vasectomies [13]; Mexico, where LHAs provided breastfeeding education and support to mothers [14]; and Brazil, where CHWs were successfully trained to promote oral health [15]. LHAs often have other primary responsibilities, such as in Bolivia, where soldiers are trained as LHAs to provide nutrition and childhood illness information to their communities when they return home following military duty [12].
In the United States, the LHA model began receiving attention in the 1960s with the passage of the Migrant Act of 1962 and the creation of the Indian Health Service's Community Health Representative Program in 1968. In the late 1960s and early 1970s, a Great Society program known as ‘New Careers’ pursued the creation of LHA jobs as entry-level positions for career development. Interest in the LHA model for spreading clinical services and bridging primary health care delivery and communities reemerged in the 1990s with initiatives by the Centers for Disease Control and Prevention [16] as well as by the Health Resources and Services Administration [17]. Since the 1960s, when the US federal government first endorsed the use of LHAs to help expand access to health care for underserved populations [18], LHAs have been increasingly used to reach marginalized and otherwise hard-to-reach populations in the United States [5, 7, 19, 20].
The role of LHAs in the United States can range from information dissemination and health education to policy and community advocacy, and from negotiating agency services to providing preventive and curative care [7, 10, 21]. In a 1994 report, the US Centers for Disease Control and Prevention defined the LHA's role as providing informal, community-based, health-related services and establishing vital links between health providers and persons in the community [22]. The National Community Health Advisor Study, published in 1998, went further, identifying seven core roles of LHAs, among them: cultural mediation, informal counseling and support, health education, advocacy and service provision [20]. Other LHA intervention studies identified these same core roles [8, 18, 23] and former LHA managers endorsed the role as diverse and expansive [24]. Without this knowledge, practitioners wishing to initiate or improve LHA outreach lack an informed basis from which to move forward.
Present study
We conducted a systematic review of the LHA model in US Latino communities to examine differences between research on programs in which LHAs served primarily in an educator role and research on programs that formally extended the LHA role to include serving as a bridge to other services (educator plus bridge). This extension has ramifications for program design, including LHA recruitment, training needs, support and evaluation. For the purpose of this analysis, the educator-only role was defined as providing one-on-one or group contact with the target audience, whereas the educator-plus-bridge role was defined as providing education plus informational and instrumental support for groups accessing health care services. This role comparison was driven, in part, by our experience developing LHA interventions in new and established Latino immigrant-receiving communities [25]. To illustrate, one could consider the experience of a Spanish-language-dominant immigrant attempting to access health care services in a new immigrant-receiving community compared with an established one. New immigrant-receiving communities are those with little to no Latino migration prior to 1990 such as those found in Georgia and North Carolina. In contrast, established immigrant-receiving communities are those with a long history and tradition of serving as an immigrant gateway into the United States such as those found in the Southwest region of the United States [26]. Given language differences and other cultural barriers, Spanish-language-dominant immigrants living in new immigrant-receiving communities may need LHAs to serve as a bridge by acting as cultural brokers or intermediaries between the predominantly English-speaking service organizations and their Spanish-speaking clients. Latinos living in traditional immigrant-receiving communities may not need this type of bridging support. This led us to consider differences between LHA models in which the LHA was primarily tasked with providing health education via one-on-one or group contact versus those in which the LHA was given the additional responsibility of bridging to other services and systems. Using all studies identified, we examined two initial research questions:
(i) To what extent do educator-only versus educator-plus-bridge programs differ on study design and participant characteristics?
(ii) To what extent do educator-only versus educator-plus-bridge programs differ on LHA characteristics?
Using a subset of studies employing rigorous study designs and reporting outcome data, we examined two additional questions:
(iii) To what extent do educator-only versus educator-plus-bridge programs differ on implementation features important for program replication, dissemination and sustainability?
(iv) To what extent do educator-only versus educator-plus-bridge programs differ on outcomes targeted and achieved?
Examining these features can further our understanding of how to design and evaluate disseminable interventions [27–29]. Our review provides important evidence for future intervention research [30] and organizational policy change [31].
Methods
Data retrieval process
Using methods developed by Cooper [32], we identified articles published by March 2009 for study inclusion in three ways: database literature searches, searching articles’ references meeting inclusion criteria (presented below) and published bibliography reviews on the topic. Three literature searches were conducted using five databases: Medline, PsychINFO, CINAHL, SocioFile and Web of Science (WOS). The WOS database included literature from the Science Citation Index Expanded, the Social Sciences Citation Index and the Arts and Humanities Citation Index.
A pilot database search using four key terms (lay health advisors, community health workers, promotores/as and outreach workers) identified only 24 articles. Subsequently, we expanded our search to the list of key terms in Box 1. We selected these terms either because they were analogous to terms in articles on LHAs or because they were associated with the training and/or work of LHAs [20]. These terms captured the role of the LHAs/CHWs as defined by the World Health Organization [11], the Centers for Disease Control and Prevention [22] and an extensive review conducted by Rosenthal [20].
Box 1.
Descriptors of LHAs in the Latino community.
Descriptors: abuelas; community health advisors/workers; consejeras; family educators; health promoter; home visitors; lay health advisors/educators/workers; natural caregivers/helpers; neighborhood workers; outreach workers; paraprofessionals; peer counselor; peer health educators/leaders; promotor(es/as); volunteers
To answer the first two research questions, we included articles in the review if the model described met our definition of an LHA. We began with the WHO definition: ‘Workers who live in the community they serve, are selected by that community, are accountable to the community they work within, receive a short, defined training, and are not necessarily attached to any formal institution’ [11]. Consistent with the multiple operationalization approach recommended for literature reviews [32], we then broadened this definition during the review process to include workers selected in collaboration with community members by institution personnel (e.g. university, church, clinic) and temporarily attached to an institution during the course of the study. We limited our literature searches to those studies conducted with Latinos/Hispanics using the following key terms: Latino/a, Hispanic, Spanish speaking, Chicano/a, Spanish, Mexican American, Puerto Rican, Latin immigrant, Central American and South American. We included only those studies published in peer-reviewed journals between 1965 and the present (1980 to present in WOS), available in Spanish or English, and that addressed a physical health, mental health or quality-of-life issue. Literature searches were downloaded into EndNote to eliminate duplicates and to facilitate the review process. We excluded dissertations or non-peer reviewed publications and manuscripts insufficiently detailed for evaluation purposes. To minimize the potential for bias or errors in the selection of articles, we evaluated on inclusion/exclusion criteria a random sample of 50% of the articles identified during the search process. Figure 1 illustrates decision stages employed and their outcomes in terms of number of articles identified and included.
Fig. 1.
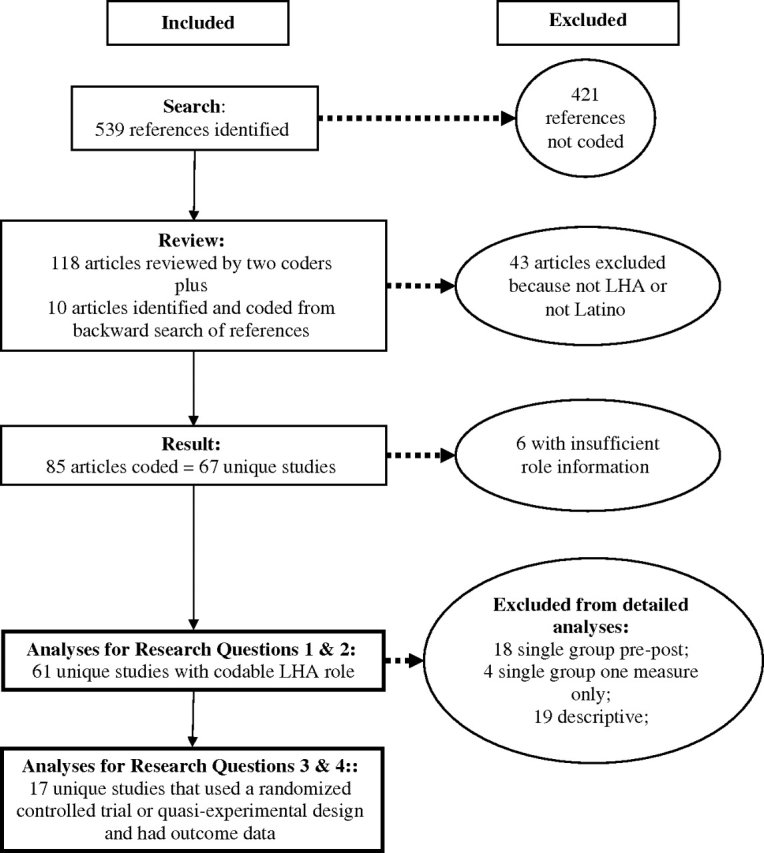
Literature included during the review process.
To answer the second two research questions, we retained articles from those identified above that used a rigorous study design (randomized controlled trial or two-group, pre–post quasi-experimental study) and reported participant outcomes (knowledge, psychosocial factors, behaviors, health care use and health status).
Data coding
Using Cooper's ‘Method-Description Approach’ (p. 86) [32], we created a coding sheet to capture pertinent information. Reviewers coded all relevant LHA role information available as well as participant characteristics, other LHA characteristics, implementation features and outcomes.
LHA role
The LHA role was captured using descriptions from the articles, as well as any qualitative or quantitative information reported on, such as dose delivered. We conceptualized two roles to answer the research questions. The educator-only role was defined as the LHA providing direct health education, behavioral skill development, and/or informational or emotional support. The educator-plus-bridge role included any, or all three, of these activities in addition to activities where the LHA linked participants to agencies, provided referrals or assisted with the coordination of care.
Participant characteristics
We examined the following variables pertaining to study participants: number of participants recruited, age, gender, education, income, ethnicity, country of origin and acculturation status.
LHA characteristics
LHAs were classified according to the number reported in each study, their age, gender, education, income, ethnicity, country of origin and acculturation status. We categorized LHAs as either paid staff members or volunteers, with additional information coded on material benefits provided during training or intervention delivery (e.g. food, transportation, child care, graduate certificate, monetary stipend). We also coded the number of hours and structure of the training.
Implementation features
Intervention features included delivery setting (home, community, organization), duration, type of contact, including whether the LHA had individual and/or group contact with the participants as well as whether other professionals were involved and other intervention methods used by the LHAs to promote change, such as print or audiovisual materials, demonstrations, mass media or health fairs. Additional study design characteristics we examined included targeted health issue; research design and unit of randomization, if a randomized controlled trial; geographic location; target audience (adult female, adult male, family or organization); and sampling methods (random sample, convenience sample or LHA identified).
Efficacy
To examine these studies’ efficacy and effectiveness, we coded information on types of outcomes targeted and outcome and process evaluation results achieved. Outcomes were categorized into five groups: (i) knowledge, (ii) psychosocial (e.g. health beliefs, attitudes, self-efficacy), (iii) behavioral (e.g. dietary intake, i.v. drug use, use of protective eyewear), (iv) health care use (e.g. cancer screening, prenatal visits) and (v) health status (e.g. depression, body mass index, hemoglobin A1c).
Review process
Several strategies were used to ensure accurate coding of information. First, three reviewers were trained on coding definitions and the appropriate use of the coding sheet. This training included discussions about each variable; testing the coding sheet with several articles; comparing results, addressing discrepancies and revising the coding sheet as needed; testing the coding sheet with additional articles (two articles per testing period) until adequate interrater reliability estimates were obtained between raters; and double coding all articles for verification purposes, with discrepancies addressed using a consensus approach [32].
All articles were reviewed by two reviewers and discrepancies were resolved by a third. Interrater reliability estimates obtained during the review process ranged from 0.73 to 0.99, with more errors observed on coding of LHA's payment status and fewer errors observed on coding study design characteristics. Data were then entered into SPSS 11.0 using a double data-entry verification process.
Results
Results of the literature search are outlined in Fig. 1. A total of 128 articles were identified and coded. Of these, 43 were excluded after the coding process primarily because they either did not describe an LHA program or did not include Latinos. This yielded a sample of 85 articles, or 67 unique studies, of which 6 were excluded at the analysis stage because insufficient data were available to classify LHA role [33–38]. The process yielded a final sample size of 61 studies. These studies are presented by study design: participant and LHA characteristics in Tables I and II, health target in Fig. 2 and geographic region in Fig. 3. Of the 61 studies with LHA role information, 17 studies met our final inclusion criteria of employing a rigorous study design (randomized controlled trial or two-group, pre–post quasi-experimental study) and reporting outcomes. These studies are described further in Tables III (implementation) and IV (efficacy). The tables are organized by role type (educator only or educator plus bridge).
Table I.
Study design and participant characteristics by LHA role from earliest to latest studies published (N = 61; 33 educator only and 28 educator plus bridge)
| Study | Study design | Health issue targeted | Participants |
|||||
| n | Mean age (years) | % Female | % <high school | % Latino; % country of birth; acculturation | ||||
| Educator | Brand [47] | Program description | Diet | 100 | ||||
| Pilisuk et al. [48] | Program description | Mental health | 16 | |||||
| Tiernan [49] | Program description | Chronic disease risk | ||||||
| Amezcua et al. [50] | Not codable | Multiple risk behaviors | ||||||
| Brownstein et al. [51] | Not codable | Cancer screening | ≥35 | 100 | NR; Mexican American and Yaqui; NR | |||
| Watkins et al. [52, 53]* | Quasi-experimental | Prenatal care | 470 | 100 | 100%; NR; Spanish speaking | |||
| May et al. [54] | RCT: community | Chronic disease risk | 42 | 47 | 90 | NR; NR; Spanish speaking | ||
| Navarro et al. [55–57]* | RCT: LHA | Cancer screening | 512 | 34 | 100 | Median = 7 years | 100%; 92% Mexican born; 2.00a | |
| Ramirez et al. [58] | Not codable | Cancer screening | 100 | |||||
| Wiist et al. [59] | RCT: community | Mental health | 1887 | 10–13 | 6th graders | |||
| Hanson [60]* | RCT: county | Asthma | 303 | 92 | 23 | |||
| Alcalay et al [61]; Balcazar et al. [62, 63] | Program description | Chronic disease risk | 344 | 18–54 | 50 | ‘Low’ | 100%; NR; NR | |
| Bell et al. [64]* | Quasi-experimental | Food safety | 165 | ‘Hispanic residents’; NR; NR | ||||
| Buller et al. [65]; Larkey et al. [66]* | RCT: social network | Diet | 905b | 42 | 25 | 17 | 42%; NR; 2.05 (0.93)a | |
| Whitehorse et al. [67] | 1 group pre–post | Physical activity | 487 | 51%, 18–59 | 97 | 63 | 92%; 81% foreign born; 84% Spanish speaking | |
| Cravey et al. [68] | Program description | Environmental health | ||||||
| Taylor et al. [69, 70] | 1 group pre-post | Diet | 337 | <20 to >60 | 98 | 26 | 98%; NR; 46% Spanish speaking | |
| Ramos et al. [71] | 1 group pre–post | Environmental health | 100%; 65% US born; NR | |||||
| Watson et al. [72] | Program description | Oral health | ||||||
| Woodruff et al. [73]* | RCT: individual | Smoking cessation | 313 | 42 | 51 | Median = 9–11 years | 100%; 78% Mexican born; 2.13 (0.84)a | |
| Kim et al. [74] | 1 group pre–post | Chronic disease risk | 272 | 38 | 98 | Mean = 9 years | 100%; NR; NR | |
| Conway et al. [75]; Rodriguez et al. [76]; Woodruff et al. [77]* | RCT: family | Environmental tobacco smoke | 143 | 4 | 55 | 100 | 100%; 85% Mexican born; 2.00a | |
| Forst et al. [78]* | Quasi-experimental | Eye safety | 786 | 33 | 19 | 75 | 100%; Mexicanc; 100% Spanish speaking | |
| Elder et al. [43, 44, 79]* | RCT: individual | Diet | 357 | 40 | 100 | 52 | 100%; 95% Mexican born; −1.86 (.90)d | |
| Staten et al. [80] | 1 group pre–post | Chronic disease risk | 248 | 49 | 92e | 88 | 100%; 92% Mexican borne; 90% Spanish speakinge | |
| Teufel-Shone et al. [81] | 1 group pre–post | Diabetes | 249 | 75%, >18 | 66 | 100%; Mexican American; NR | ||
| Larkey [82] | 1 group pre–post | Cancer screening | 457 | 100 | 72 | 100%; NR; 100% Spanish survey | ||
| Martin et al. [83]* | Quasi-experimental | Child passenger safety | 90 | 31 | 58 | 100%; 87% Mexican born; 1.5a | ||
| Culica et al. [84] | 1 group pre–post | Diabetes | 162 | 48 | 64 | 78%; Mexican American; 73% Spanish speaking | ||
| Joshu et al. [85] | 1 group pre–post | Diabetes | 301 | 60 | 73 | 39 | 100%; NR; NR | |
| Lujan et al. [86]* | RCT: individual | Diabetes | 150 | 58 | 80 | 95 | 100%; Mexican American; 87% <2.00 on 4-point scale | |
| Sauaia et al. [87]; Welsh et al. [88]* | Quasi-experimental | Cancer screening | 6696f | 50–64 | 100 | 22%; NR; NR | ||
| Vincent et al. [89]* | Quasi-experimental | Diabetes | 20 | 56 | 71 | Mean = 10 | 100%; Mexican American; 1.73 (0.60)a | |
| Bridge | Carrillo et al. [90] | 1 group, 1 measure | Prenatal care | 274 | 25 | 100 | 80 | 100%; NR; NR |
| McElmurry et al. [91] | Program description | Access to care | ||||||
| Dawson & Robinson [92]* | RCT: individual | Prenatal care | 172 | 21 | 100 | Median = 11 | 25%; NR; NR | |
| Meister et al. [93]; Warrick et al. [94] | 1 group, 1 measure | Prenatal care | 147 | 25 | 100 | ‘Little formal education’ | 100%; 80% Mexican born; ‘culturally traditional’ | |
| Birkel et al. [95] | 1 group pre–post | HIV/STD/AIDS prevention | 2624 | 32 | 22 | 9–11 | 88%; Mexican & Puerto Rican; NR | |
| Morris et al. [96] | 1 group pre–post | Cancer screening | 432 | 54 | 100 | Mean = 6 | 97%; NR; NR | |
| McFarlane et al. [97]; McFarlane & Fehir [98]; Mahon et al. [99] | Program description | Prenatal care | 100 | 100%; Mexican & Central American; NR | ||||
| Bray & Edwards [100] | 1 group pre–post | Prenatal care | 100 | 100%; NR; NR | ||||
| Nyamathi et al. [101]* | RCT: site | HIV/STD/AIDS prevention | 233 | 31 | 100 | Mean = 10 | 100%; 44% Mexican born; 56% high Marin scaleg | |
| Brown & Hanis [102] | 1 group pre–post | Diabetes | 7 | 61 | 60 | 100%; NR; NR | ||
| Castro et al. [103] | RCT: church | Cancer screening | 668 | 31–51 | 100 | 100%; NR; 2.28–3.68a | ||
| Bird et al. [104]; Pérez-Stable [105] | Program description | Cancer screening | 1601 | 42 | 100 | Mean = 10 | 100%; 35% Mexican & 28% Central American; 75% low Marin scaleg | |
| Singer & Marxuach-Rodriquez [106] | 1 group pre–post | HIV/STD/AIDS prevention | 24 | 25 | 0 | 25 | 100%; 62% Puerto Rican; 33% Spanish speaking | |
| Baker et al. [107] | Program description | Access to care | 610 | 18–81 | ‘Most’ | 100%; NR; NR | ||
| Booker et al. [108] | Program description | Access to care | ||||||
| Corkery et al. [109]* | RCT: individual | Diabetes | 64 | 53 | 74 | 80 | NR; 75% Puerto Rican; 25% Spanish speaking | |
| Warren [110] | Program description | HIV/STD/AIDS prevention | 357 | 32 | 20%; NR; NR | |||
| Flaskerud & Nyamathi [111] | 1 group pre–post | HIV/STD/AIDS prevention | 508 | 100 | 100%; NR; NR | |||
| McQuiston & Uribe [112]; McQuiston & Flaskerud [113]; McQuiston et al. [114] | Program description | HIV/STD/AIDS prevention | ||||||
| Hiatt et al. [115] | 2 groups pre–post | Cancer screening | 1599 | 40–75 | 100 | 33 | 14%; NR; NR | |
| McElmurry et al. [116] | Program description | Access to care | 100%; NR; NR | |||||
| Hunter et al. [39]* | RCT: individual | Comprehensive preventive care | 101 | 50 | 100 | 77 | 96%; 86% Mexican born; NR | |
| Mayo et al. [117] | 1 group, 1 measure | Cancer screening | 89 | 53 | 100 | 44 | NR; 79% US born; 79% English speaking | |
| Hansen et al. [118] | 1 group, 1 measure | Cancer screening | 141 | 22–69 | 100 | 100%; NR; NR | ||
| Martin et al. [119] | 1 group pre–post | Asthma | 103 | 42 | 70 | 79 | 100%; 77% Mexican born; 1.9a | |
| Reinschmidt et al. [120] | RCT: individual | Chronic disease risk | 100 | |||||
| Ingram et al. [121] | 1 group pre–post | Diabetes | 70 | 61 | 77 | 100%; 86% Mexican born; NR | ||
| Thompson et al. [122] | 1 group pre–post | Diabetes | 365 | 57 | 66 | 100%; Mexican American; NR | ||
NR or empty cell = not reported/missing; RCT = randomized controlled trial; asterisks denote articles with outcomes.
Mean ethnic identity and acculturation measured on a 5-point scale from 1 = very Anglo/low to 5 = very ethnic/high; Woodruff and Conway studies used the modified Cuellar et al. [123] scale; Navarro used the short Marin et al. [124] scale.
Initially recruited 2091 to participate in a community intervention; 905 were randomly assigned to peer support or no peer support.
Prior work in community indicated that 90% of the Latino farmworkers were Mexican.
Bidirectional acculturation measured using the bidirectional Cuéllar et al. [125] scale where negative responses are indicative of being more traditional.
Percentages were reported incorrectly in the paper. These percentages are based on a recalculation using the reported numerator and denominator.
Analytic sample of women enrolled in Medicaid fee-for-service longer than 18 months.
Women were classified as high (≥28) or low (<28) on an acculturation scale with a possible range of 12–48 [124].
Table II.
LHA characteristics by LHA role from earliest to latest studies published (N = 61; 33 educator only and 28 educator plus bridge)
| Study | No. of LHAs | LHA mean age (years) | % LHA female | % LHA Latino | Training length | Volunteer (V) or paid (P) | Other incentives | ||
| Educator | Brand [47] | 364 | 42 | 100 | 11 | P | |||
| Pilisuk et al. [48] | 9 | 0 | V | ||||||
| Tiernan [49] | 50 | 45 hours | V | ||||||
| Amezcua et al. [50] | V | Certificate | |||||||
| Brownstein et al. [51] | 100 | ||||||||
| Watkins et al. [52, 53]* | 40 | 15–52 | 100 | 100 | 24 hours | V | Mileage and other reimbursement, child care | ||
| May et al. [54] | 4 | 100 | 100 | P | |||||
| Navarro et al. [55–57]* | 36 | 100 | 100 | 12 weeks | |||||
| Ramirez et al. [58] | 85 | 49 | 97 | V | Certificates, recognition | ||||
| Wiist et al. [59] | 305 | 10–13 | 53 | 52 | 29 hours | V | Field trips | ||
| Hanson [60]* | P (per visit) | ||||||||
| Alcalay et al. [61]; Balcazar et al. [62, 63] | 29–33 | 41 | 100 | 100 | 18 hours + 2 days | P | |||
| Bell et al. [64]* | 15 | ‘Older’ | 100 | 100 | 1 session | V | |||
| Buller et al. [65]; Larkey et al. [66]* | 41 | 41 | 29 | 56 | 16 hours | V | $1800 total + gifts | ||
| Whitehorse et al. [67] | 20 | 92 | 9 hours | ||||||
| Cravey et al. [68] | 66 | 100 | V | Baseball hats | |||||
| Taylor et al. [69, 70] | 36 | 78%, 31–60 | 97 | 97 | 16 hours | V | Certificates, $100 | ||
| Ramos et al. [71] | 100 | 100 | |||||||
| Watson et al. [72] | 7 | Youth | V | Food, certificates | |||||
| Woodruff et al. [73]* | 16 | 41 | 88 | 94 | 25 hours | V | ‘Modest stipend’ | ||
| Kim et al. [74] | 12 | 92 | 100 | 39 hours | P (per class) | Mileage reimbursement | |||
| Conway et al. [75]; Rodriguez et al. [76]; Woodruff et al. [77]* | 11 | 45 | 100 | 100 | 20 hours | V | Monetary incentives and mileage reimbursement | ||
| Forst et al. [78]* | 16 | 100 | 20 hours | ||||||
| Elder et al. [43, 44, 79]* | 4 | 55 | 100 | 100 | 12 sessions | P | $200 for training + certificate, $144 per participant, mileage and other reimbursement | ||
| Staten et al. [80] | 11 | 91 | 6 hours | P | |||||
| Teufel-Shone et al. [81] | 4 | 100 | 100 | 1 day | |||||
| Larkey [82] | 3 | 100 | 100 | ||||||
| Martin et al. [83]* | 16 | 88 | P and V | All received $40 gift certificate | |||||
| Culica et al. [84] | 1 | 27 hours | P | ||||||
| Joshu et al. [85] | 100 | P | |||||||
| Lujan et al. [86]* | 2 | 100 | 60 hours | P | |||||
| Sauaia et al. [87]; Welsh et al. [88]* | 4 | 100 | 100 | P | |||||
| Vincent et al. [89]* | 1 | 100 | 100 | P | |||||
| Bridge | Carrillo et al. [90] | V | |||||||
| McElmurry et al. [91] | 30 | 18 | 93 | 33 | 160 hours | P | Training mileage reimbursement | ||
| Dawson & Robinson [92]* | 100 | 30 hours | P | ||||||
| Meister et al. [93]; Warrick et al. [94] | 9 | 100 | 100 | 34 hours+ | 8 P, 1 V | Benefits, certificate, ESL classes | |||
| Birkel et al. [95] | P | ||||||||
| Morris et al. [96] | 4 | 35–65 | 100 | 100 | Weekly staff meeting | P | |||
| McFarlane et al. [97]; McFarlane & Fehir [98]; Mahon et al. [99] | 14 | 19–68 | 100 | 100 | 8 hours | V | Tote bag | ||
| Bray & Edwards [100] | 3 | 100 | 100 | 3 weeks | P | ||||
| Nyamathi et al. [101]* | 100 | 100 | P | ||||||
| Brown & Hanis [102] | 1 | 100 | P | ||||||
| Castro et al. [103] | 1–3 in 14 churches | 27–67 | 100 | 100 | V | $500/year | |||
| Bird et al. [104]; Pérez-Stable [105] | 78 | Some husbands active | 100 | 18 hours | V | Child care, $500 after 5 months volunteer work, certificate | |||
| Singer & Marxuach-Rodriquez [106] | 6 | 0 | 100 | V | |||||
| Baker et al. [107] | 2 | 100 | P | ||||||
| Booker et al. [108] | 33 | 32 | 50 | 20 hours | P | ||||
| Corkery et al. [109]* | 1 | 100 | 100 | ||||||
| Warren [110] | |||||||||
| Flaskerud & Nyamathi [111] | 100 | 100 | P | ||||||
| McQuiston & Uribe [112]; McQuiston & Flaskerud [113]; McQuiston et al. [114] | 18 | 19–39 | 83 | 100 | 21 hours | V | Incentive, mileage reimbursement, child care | ||
| Hiatt et al. [115] | 7 | 100 | P | ||||||
| McElmurry et al. [116] | 170 hours | P | |||||||
| Hunter et al. [39]* | 1 | 100 | 100 | ||||||
| Mayo et al. [117] | 45 | 100 | V | ||||||
| Hansen et al. [118] | 4 | 40–57 yo | 100 | 100 | 20 hours | V | Mileage reimbursement, child care | ||
| Martin et al. [119] | 11 | 100 | 15 weeks + 12 hours | P | |||||
| Reinschmidt et al. [120] | 1 | 40 | 100 | 100 | |||||
| Ingram et al. [121] | 100 | 100 | P | ||||||
| Thompson et al. [122] | Minimum of 10 at any time | 100 | 100 | 10 sessions + 42 hours | P | ||||
ESL = English as a second language; NR or empty cell = not reported/missing; asterisks denote articles with outcomes.
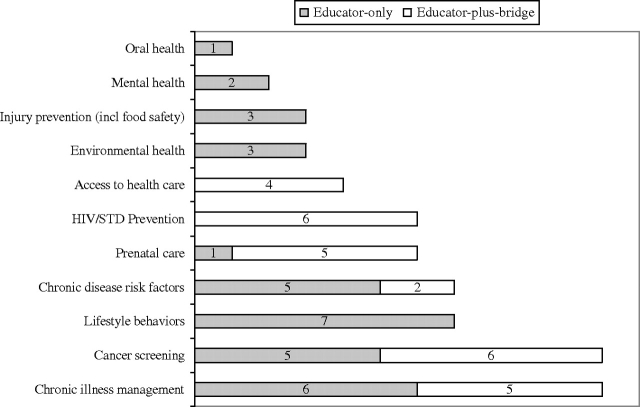
Fig. 2.
Latino LHA studies by health outcome and LHA role (N = 61).
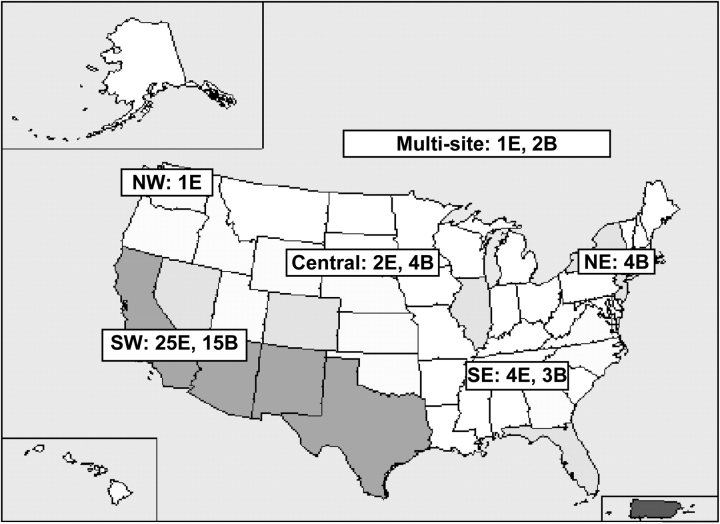
Fig. 3.
Geographic distribution of 61 LHA studies, with darker map zones depicting greater concentrations of Latinos/Hispanics (E = educator only, B = educator plus bridge).
Table III.
Intervention and study design characteristics of rigorously evaluated programs (n = 17; 13 educator only and 4 educator plus bridge)
| Study | Recruitment | Intervention and study design characteristics |
||||
| Target | Setting | Time in months | LHA delivery modes | |||
| Educator | Watkins et al. [52, 53] | Convenience, LHA | Mother/child | Home, organization | Individual contact with LHA; dose and frequency not specified | |
| Navarro et al. [55–57] | LHA | Female | Organization, community | 3 | Twelve weekly LHA-led group classes with demonstrations | |
| Hanson [60] | Convenience | Family | Home, organization | 24 | LHA-led 1- to 2-hour home visits at day 3 or 4 of intervention phase, and 2, 4, 8, 14 and 20 months | |
| Bell et al. [64] | LHA | 9 | LHA-led food preparation demonstrations | |||
| Buller et al. [65]; Larkey et al. [66] | Convenience | Female, male | Organization | 9 | Two hours a week; LHA used various communication and demonstration strategies to deliver messages individually and in groups | |
| Woodruff et al. [73] | Convenience | Female, male, family | Home | 3 | Four 1- to 2-hour LHA home visits and three 15- to 30-min telephone calls tapered over intervention period | |
| Conway et al. [75]; Rodriguez et al. [76]; Woodruff et al. [77] | Convenience | Family | Home | 4 | Six home visits or telephone calls | |
| Forst et al. [78] | LHA | Female, male | Other | 4 | One individual and one group LHA-led session | |
| Elder et al. [43, 44, 79] | Random | Female | Home | 3 | Twelve weekly LHA home visits (or telephone calls if visit not possible) and 12 weekly tailored newsletters | |
| Martin et al. [83] | Convenience | Family | Organization | 1 hour | One-hour-long session on car seat safety with demonstrations | |
| Lujan et al. [86] | Convenience | Female, male | Organization | 6 | Eight weekly 2-hour LHA-led group classes with demonstrations plus biweekly telephone calls, followed by 16 weeks of biweekly postcards | |
| Sauaia et al. [87]; Welsh et al. [88] | Convenience | Female, community | Home, organization | 60 | At least bimonthly LHA outreach visits to assigned church to meet with individuals and conduct groups, plus 1–3 group discussions in homes | |
| Vincent et al. [89]a | Convenience, LHA | Female, male | Organization | 2 | Eight weekly 2-hour group classes with demonstrations and modeling by LHA and weekly LHA telephone calls | |
| Bridge | Dawson & Robinson. [92] | Convenience | Mother/child | Home, organization, community | 16 | Home visitation by LHA to provide social support and help access services (frequency not reported) |
| Nyamathi et al. [101] | Convenience | Female | Organization | 2 hours | One 2-hour meeting with nurse educator and LHA that included demonstrations and referrals to other services (e.g. drug rehab) | |
| Corkery et al. [109] | Convenience | Female, male | Organization | 3.4 | Liaison between the patients, their families and health care providers; facilitated the scheduling of and attended clinic sessions with patients | |
| Hunter et al. [39] | Random | Female | Home, organization | 2 | LHA home visit 2-weeks after appointment card mailed if appointment not made; second LHA home visit at Week 8 to encourage appointment keeping and connect with resources | |
Information reported in this article was inconsistent between the text and the tables. Information reported here is from the table.
Table IV.
Study outcome characteristics of rigorously evaluated programs (n = 17; 13 educator only and 4 educator plus bridge)
| Study | Comparison group(s) | Retention at each follow-up | Assessment type | Outcomes | Process evaluation | |
| Educator | Watkins et al. [52, 53] | Standard care | NR: 68 (14%) | 1, 4, 5 | NR: LHA ↑ knowledge (P ≤ 0.001) and sick child visits (P ≤ 0.05). No change in health status (e.g. child birth weight) and prenatal visits based on medical records | LHA knowledge ↑ (P ≤ 0.05); 66% of clinic visitors had some contact with LHAs |
| Navarro et al. [55–57] | LHA in community living skills | 3 months: 361 (71%); 12 months: NR; 24 months: NR | 3, 4 | 3 months: cancer-specific LHA ↑ self-reported monthly BSE (P ≤ 0.001) and mammograms (P ≤ 0.05) compared with control, and approached significance for Pap tests (P ≤ 0.10). No effect on clinical breast exam. 12 and 24 months: NR | 88% of women who completed pre- and post-test attended at least half of the sessions | |
| Hanson [60] | Standard nurse-delivered asthma care | 6 months: NR; 12 months: 193 (64%); 24 months: 188 (62%) | 2, 3 | 6 months: ↑ self-efficacy in both groups (P ≤ 0.001), but no group-by-time effects. 12 and 24 months: ↑ observed in self-efficacy from baseline was retained at 12 and 24 months in both groups (P ≤ 0.001), but no group-by-time effects on self-reported asthma management and self-efficacy | 51% of home visits completed | |
| Bell et al. [64] | No treatment following a media and physician campaign | Immediate: 165 (100%); 6 months: 47 (28%) | 2, 3, 5 | Immediate: LHA ↑ use of pasteurized milk (P ≤ 0.01) and improved attitudes toward pasteurized milk (P < 0.01) compared with control. No changes in outcome expectations. 6 months: LHA improvements observed at immediate post-intervention maintained (P ≤ 0.01). Decreases in incidence of Salmonella | Similar changes observed in LHAs; LHAs increased requests of pamphlets; control condition improved residents’ knowledge | |
| Buller et al. [65]; Larkey et al. [66] | No treatment following a work site wellness program | 18 months: 664 (73%); 24 months: 559 (62%) | 2, 3 | 18 months: LHA ↑ daily servings of fruits and vegetables based on diet recall (P ≤ 0.001) and Food Frequency Questionnaire (P ≤ 0.01), ↑ awareness of 5-a-day program, and improved 4 of 5 attitudes (Ps ranged from <0.05 to 0.001) compared with control. 24 months: ↑ observed in fruits and vegetables intake maintained on diet recall (P ≤ 0.05) but not Food Frequency Questionnaire, on awareness (P ≤ 0.001); and on 3 of 5 attitudes (Ps ranged from <0.05 to 0.001). | LHA used encouragement and listening communication strategies with individuals, and modeling and creating context with groups | |
| Woodruff et al. [73] | Referral to quit line | 3 months: 282 (90%) | 3 | 3 months: LHA improved 2 abstinence measures compared with control: self-report (P ≤ 0.05) and physiological (P ≤ 0.01) | Abstainers more involved in intervention than non-abstainers, P ≤ 0.05 | |
| Conway et al. [75]; Rodriguez et al. [76]; Woodruff et al. [77] | No treatment | 4 months: 132 (92%); 7 months: 132 (92%); 16 months: 127 (89%) | 3 | 4, 7, 16 months: ↓ in ETS exposure over time in both groups on self-report (P ≤ 0.001) and physiological measures (P ≤ 0.05), but no group-by-time effects | Cost of LHA component was $400/household | |
| Forst et al. [78] | Two groups: LHA distributed protective eyewear but no training and staff distributed protective eyewear | 1–4 months: 703 (89%) | 1, 2, 3 | 4 months: improvements in all 3 groups on self-reported use of protective eyewear (P ≤ 0.001), with LHA training showing greater improvements than LHA distribution alone (P ≤ 0.001) or staff distribution (P ≤ 0.05); LHA training improved knowledge compared with 2 other groups (no P value reported). No improvements in risk beliefs | ||
| Elder et al. [43, 44, 79] | Two groups: tailored and targeted communication conditions | 3 months: 313 (88%); 9 months: 272 (76%); 15 months: 281 (79%) | 2, 3 | 3 months: LHA improved 4 of 11 diet outcomes compared with tailored, and 2 of 11 measures of diet compared with targeted (all Ps ≤ 0.05); LHA improved behavioral strategies to ↓ fat and ↑ fiber compared with tailored and targeted conditions (both Ps ≤ 0.05). 9 months: LHA versus tailored improved family interactions (P ≤ 0.05), but tailored versus LHA ↓ barriers for produce consumption (P ≤ 0.01). No time or group-by-time effects on behavioral strategies to ↓ fat and ↑ fiber, outcome expectations, barriers to low fat and family support. 9 and 15 months: 3 months effects on diet not maintained | Cost of LHA intervention was $135 compared with $45 tailored materials and $9.30 targeted materials. LHA participants more involved in intervention based on home work assignments completed | |
| Martin et al. [83] | No treatment control group | NR: 78 (87%) | 3, 5 | NR months: among rear-facing car seats, LHA ↑ 3 of 11 dimensions of proper car seat placement (all Ps ≤ 0.05). Among front-facing car seats, LHA ↑ adherence to safety standards (P ≤ 0.05), ↑ 6 of 11 dimensions of proper car seat placement (all Ps < 0.05) and ↓ crashes (no P value reported) | ||
| Lujan et al. [86] | Usual care | 3 months: 144 (96%); 6 months: 135 (90%) | 1, 2, 5 | 3 months: no time or group-by-time effects on hemoglobin A1c (HbA1c) and diabetes knowledge and health beliefs. 6 months: LHA improved diabetes control (HbA1c; P < 0.001), ↑ diabetes knowledge (P ≤ 0.01) and worsened diabetes health beliefs (P ≤ 0.01) | ||
| Sauaia et al. [87]; Welsh et al. [88] | Educational print materials | 24 months: registrants | 4 | 24 months: no significant change in mammography rates, although results approached significance (P = 0.07). After adjusting for insurance group, age, income, urbanicity and disability, LHA ↑ screening rates (P ≤ 0.05) | Latinas receiving LHA intervention were younger (P = 0.06) and poorer (P ≤ 0.001) | |
| Vincent et al. [89]a | Usual care | 2 months: 18 (90%); 3 months: 17 (85%) | 1, 2, 5 | 2, 3 months: no group-by-time effects for diabetes knowledge, self-efficacy, weight, body mass index and HbA1c | Weekly promotora telephone calls … seemed to be a successful retention strategy | |
| Bridge | Dawson & Robinson [92] | Routine maternity and pediatric care | 4 months: 146 (85%) | 2, 3 | 4 months: no time or group-by-time effects on observed feeding styles and self-reported attitudes | Moms receiving LHA contact kept more appointments |
| Nyamathi et al. [101] | Education only with nurse and LHA; no skill-building enhancements | 0.5 months: 213 (91%) | 1, 2, 3, 5 | 0.5 months: enhanced LHA condition ↑ self-reported concern (P ≤ 0.01). Changes in both groups on self-reported emotion-focused coping, appraisal, attitudes toward AIDS, knowledge, multiple partners, use of i.v. drugs, use of non-i.v. drugs, depression and distress (all Ps ≤ 0.001). No time or group-by-time effects on problem-focused coping | 60 women who were enrolled in the study refused to participate due to lack of time | |
| Corkery et al. [109] | American Diabetes Association guideline nurse-delivered care | 3.4 months: 40 (63%); 7.7 months: NR | 1, 3, 5 | 3.4, 7.7 months: no group-by-time effects on any measures. Among program completers, changes over time were observed on knowledge (P ≤ 0.001), following a meal plan (P ≤ 0.01), carrying fast-acting sugar (P ≤ 0.001), performing daily foot care (P ≤ 0.001) and measured glycol hemoglobin (P ≤ 0.001) | LHA ↑ participant completion of the program (P ≤ 0.01) | |
| Hunter et al. [39] | Postcard reminders | NR months: 98 (97%) | 4 | NR months: LHA ↑ self-reported health care utilization over control (P ≤ 0.05) |
NR or empty cell = not reported/missing; BSE = breast self-examination; ETS = environmental tobacco smoke; ↑ = increase; ↓ = decrease.
Key to assessment type column: 1 = knowledge; 2 = psychosocial; 3 = behavioral; 4 = health care use; 5 = health status.
Information reported in this article was inconsistent between the text and the tables. Information reported here is from the table.
LHA roles
Educator-only programs represented over half of the 61 studies. Targeted health issues were collapsed into 11 categories: chronic disease management (diabetes, asthma), lifestyle behaviors (diet, physical activity, smoking cessation and multiple risk behaviors), cancer screening, prenatal care, HIV/STD/AIDS prevention, access to health care, injury prevention (food safety, eye safety, child passenger safety), environmental health, mental health, chronic disease risk factors and oral health. The most commonly targeted health issues were chronic disease management (18%), cancer screening (18%), lifestyle behaviors (11%), chronic disease risk factor reduction (11%), prenatal care (10%) and HIV/STD/AIDS prevention (10%) (Fig. 2).
Figure 3 depicts the geographic distribution of LHA programs in the United States. More of the programs took place in the Southwest region of the United States (66%). In addition, proportionally more LHA programs in the Southwest adopted an educator-only approach compared with those conducted in the Central and Northeast regions. Three studies represented multisite initiatives.
Participant characteristics
Data were not reported on a number of characteristics as depicted by the empty cells in tables. Income was the least reported of participant characteristics examined, and therefore, we omitted it. The number of participants reached ranged from 7 to 6696, with a median of 3365 in educator-only programs and 485 in educator-plus-bridge programs. Nearly all the studies that reported the participants’ gender indicated that programs reached mostly women (92%; 45 of 49); 31% (8) reached only women in the educator-only programs compared with 65% (15) in the educator-plus-bridge programs. Nearly half the studies (49%; 30) did not report on participants’ educational status; among those that did, participants generally had less than a high school education. One notable finding was the dearth of studies conducted with Latino subgroups other than less acculturated Mexican immigrants/Mexican Americans. Only 5 of the 61 programs targeted Puerto Ricans (3 programs) and Central Americans (2 programs); all of them educator-plus-bridge programs.
LHA characteristics
Despite our attempts to code a variety of information about the LHAs, the characteristics most frequently reported in these articles were limited to the number of LHAs involved in the intervention, and their gender and ethnicity (Table II). Few studies reported on the LHAs’ age, educational level, income level, country of origin or level of acculturation. Similar to study participants, educator-only programs tended to involve more LHAs (mean = 43) than did educator-plus-bridge programs (mean = 15). In addition, LHAs in 70% of educator-only programs and 80% of educator-plus-bridge programs were all female. Across both types of programs, the majority of LHAs was Latina/Hispanic; all but one educator-plus-bridge program involved only Latinos.
Half of all LHAs in educator-only programs for which data were available were volunteers; in some cases, LHAs received other material incentives such as mileage reimbursements, child care, certificates or other recognitions. The other half were paid staff. For educator-plus-bridge programs, only 33% used volunteers, while the remaining 67% involved paid staff. Few studies reported on the number of training hours; in educator-only programs, training hours ranged from one session to 60 hours. For educator-plus bridge programs, hours ranged from 8 to 160.
Detailed analyses
Further analyses were limited to 17 randomized controlled/quasi-experimental studies with outcome data. We excluded 22 single-group-only studies, 19 descriptive studies and 3 with insufficient information (Fig. 1). The exclusions created a significant imbalance in the number of educator-plus-bridge programs available for review. Initially, 46% (28 of 61) described educator-plus-bridge programs; after these exclusions, only 25% (4 of 17) were educator-plus-bridge programs.
Intervention design characteristics
LHAs in the 17 studies worked with a variety of participants including adult females, adult males and entire families. Similar percentages of educator-only versus educator-plus-bridge programs involved a convenience sample of participants (70% versus 75%). LHAs, however, were involved in recruitment in 40% of the educator-only programs but none of the educator-plus-bridge programs. Intervention activities took place in participants’ homes, within organizations and within communities; two-thirds (61%) of educator-only programs versus 100% of educator-plus-bridge programs occurred in an organizational setting. The intervention delivery modality in educator-only programs usually involved several home visits and/or group classes, whereas educator-plus-bridge programs generally consisted of one or two individual contacts in a participant's home or at the clinic. Finally, educator-only programs were generally much longer in duration than educator-plus-bridge programs.
Outcome evaluation
A third of the educator-only programs versus half of the educator-plus-bridge programs assessed changes in health status; a similar proportion of educator-only and educator-plus-bridge programs assessed changes in health care use (25% versus 23%, respectively). The most common variables assessed in both programs were psychosocial (54% and 50%, respectively) and behavioral outcomes (69% and 75%, respectively). The follow-up time points were much longer in educator-only programs versus the educator-plus-bridge programs, although retention rates in both types of programs were generally high and fairly similar. Together, these latter two findings indicate high participant retention rates of up to 24 months of follow-up.
From this review, it appears that LHA programs can achieve significant changes in a variety of health-related factors for Latino populations. In all but one educator-only program, we observed significant improvements in health behaviors, irrespective of health target. Educator-only programs were also effective at improving health status in three of the five studies assessed. Changes in psychosocial variables were less evident and found only in studies in which lifestyle behavior change was targeted. Two of three educator-only programs reported significant changes in several health care use variables, although results were inconsistent. Among the four educator-plus-bridge programs, only one achieved significant improvements in health care use [39].
Process evaluation activities assessed indicated that educator-only LHA programs were the only ones reporting changes in the LHAs themselves, with increases in knowledge and behaviors observed.
Discussion
In this systematic review of LHA studies targeting US Latinos, our aim was to better understand differences in study design features between educator-only and educator-plus-bridge programs, as well as determine whether those employing a rigorous study design differed on implementation features and study outcomes. Our larger goal was to provide insights on how these two types of programs differed in addressing the health care needs of US Latinos. What we found, however, was that information on most dimensions we examined was seldom reported alongside outcome data in rigorously designed studies, limiting the conclusions that we could draw about key differences that may have been responsible for the outcomes.
Summary of findings
Reflecting on our first two research questions, analyses indicated that educator-only programs, on average, reached significantly more participants than educator-plus-bridge programs. A second important finding was that educator-only programs involved more volunteers than educator-plus-bridge programs; 50% of educator-only versus 33% of educator-plus-bridge programs engaged LHAs as volunteers. Equally interesting was the observation that since 2004, almost all published studies on educator-only programs employed LHAs as paid staff members. Such a trend was not observed in the educator-plus-bridge programs. This may be explained by the greater number of chronic disease management programs published in the last few years and LHAs’ more formal integration in the health care system [40].
Reflecting on our second two research questions, we examined whether educator-only versus educator-plus-bridge programs differed in their intervention delivery modalities so as to suggest differences in feasibility of implementation, and potential to replicate, disseminate and sustain the programs. In this area, we observed few differences by role. Fewer of the educator-only programs involved the direct participation of an organization compared with 100% of the educator-plus-bridge programs that did. Organizational participation may help sustain a program [29]. Educator-plus-bridge programs, however, were more likely to involve one-on-one LHA contact versus group contact and may require more resources to implement. Importantly, we found no differences by role in number of outcomes targeted or achieved.
Unexpected results
An unexpected result of our analysis involving all 61 studies was the greater number of educator-plus-bridge programs conducted in Central and Northeast regions of the United States. This imbalance may reflect geographic differences in the proportion of bilingual/bicultural providers in those regions and, more generally, differences in immigrant-receiving status in those regions [2]. Newer immigrant-receiving communities, perhaps less familiar with the language and cultural needs of non-native-born peoples [26], may make the bridge role of the LHA critical for these groups’ access to health care. But this operationalization of bridging is limited and does not reflect the reciprocal nature of people and the places in which they live. Bridging interventions may be equally important in communities where language is not a barrier because they target multiple levels of the socioecologic framework [41], from the individual to the organization or community. Bridging LHA interventions may better contextualize health behaviors and force program developers to consider the multiple levels of influence on health behavior change.
A second unexpected finding was that most of the 61 studies reached a predominantly Mexican immigrant/Mexican American community. Only five educator-plus-bridge programs involved communities other than this Latino subgroup. Research and practitioners seeking to intervene with other Latino subgroups may need to consider the potential generalizability of current evidenced-based approaches.
Limitations
Conclusions can be difficult to draw from any systematic review given differences in how study information is reported, if at all. By dichotomizing the LHA role, we may have misclassified activities that we were forced to place under one category or the other and, by inference, the value LHAs place on these various activities [42]. We may not fully understand the range of roles that LHAs play. For those studies reviewed, we note the large number of cases with missing data and the limitations that missing data present for drawing meaningful conclusions. The most notable limitation was the lack of available educator-plus-bridge programs to draw from and as a consequence the limited characterization of bridging represented by this research. This limitation highlights where research is clearly lacking. Only one-quarter of the studies with outcome data involved educator-plus-bridge programs, compared with almost 50% of all studies originally included in our review, possibly indicating that educator-plus-bridge programs are more likely to be service delivery programs lacking an efficacy evaluation. Another limitation is that few, if any, studies examined the effect of the intervention on the LHAs themselves. As members of the communities being targeted, their roles and responsibilities may have had significant impact on their lives, which in turn may affect the program's reach and sustainability. Very few studies examined this dimension.
Errors can occur at many stages of a review process, from failing to identify published studies to incorrectly abstracting information from the studies selected [32]. The latter limitation was tempered by the double-verification approach we used at nearly all possible points of comparison, from identifying the literature to abstracting information from the database. As reported, interrater reliabilities supported the validity of the conclusions we drew. They also suggested where improvements in reporting guidelines are needed. For example, where multiple sources of the same study were used to summarize study findings, we identified inconsistencies in the information reported, including from our own research. In one of our own articles, we reported training five promotoras at baseline [43] but, when describing our intervention effects, we reported on only four promotoras who actually delivered the intervention [44]. Both statements are correct but these types of inconsistencies add another layer of complexity when the objective is to examine the application of an intervention approach across a heterogeneous field. With better reporting guidelines for intervention studies, we would be in a stronger position to build the science around peer support interventions in a more systematic efficient manner.
Specific recommendation for future research
What is clear from this review is that future studies need to employ rigorous experimental methods, report on all outcomes and examine the association between intervention methods and their outcomes. This latter research question is best informed by details on program implementation, such as LHA recruitment, training and retention strategies [24]. For example, comparisons of volunteer and paid models [24] may contribute to the design of programs that include both giving LHAs the opportunity to move up a professional ladder and improve their economic situation [24]. Efforts to replicate, disseminate and sustain these types of programs require information on efficacy and implementation.
Conclusions
This review comes on the heels of several recently published studies that complement our findings [45, 46]. Consistent with our categorization scheme, the 200 respondents of the Promovision promotoras’ survey [42] identified several different roles played by HIV prevention promotoras but did not specify how those roles were linked to outcomes. As a first step toward improving this line of research, additional characteristics of the LHAs, their roles and the interventions themselves need to be documented alongside outcomes to determine what roles LHAs are best suited for and which achieve more successful outcomes. Disentangling the most important dimensions of LHA programs will inform a burgeoning area of public health practice and can lead to a cumulative science of public health practice, as well as begin to address recent calls for comparative effectiveness studies (see http://grants.nih.gov/grants/funding/challenge_award/).
Funding
American Cancer Society (RSGPB 113653 to G.X.A.); San Diego Prevention Research Center (U48DP001917-01 to G.X.A. and J.P.E.); Peers for Progress (to G.X.A., J.P.E. and A.C.).
References
- 1.US Census Bureau. Hispanics in the United States. Washington, DC: US Department of Commerce; 2006. [Google Scholar]
- 2.National Council of La Raza. The State of Hispanic America, 2004. Washington, DC: NCLR; 2004. [Google Scholar]
- 3.Pew Hispanic Center and The Henry J. Kaiser Family Foundation. Survey Brief: Health Care Experiences. Washington, DC: Pew Hispanic Center and the Henry J. Kaiser Family Foundation; 2004. [Google Scholar]
- 4.Liebman J, Heffernan D, Sarvela P. Establishing diabetes self-management in a community health center serving low-income Latinos. Diabetes Educ. 2007;33(Suppl. 6) doi: 10.1177/0145721707304075. 132S–8S. [DOI] [PubMed] [Google Scholar]
- 5.Moore A, Earp JA. The long reach to basic healthcare services: partnering with lay health advisors to improve health equity. In: Earp JA, French EA, Gilkey MB, editors. Patient Advocacy for Healthcare Quality: Strategies for Achieving Patient-Centered Care. Sudbury, MA: Jones and Bartlett; 2007. pp. 121–50. [Google Scholar]
- 6.Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: a continuum from natural helping to paraprofessional helping. Health Educ Behav. 1997;24:413–7. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- 7.Eng E, Parker E. Natural helper models to enhance a community's health and competence. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. San Francisco: Jossey-Bass; 2002. pp. 126–56. [Google Scholar]
- 8.Eng E, Young R. Lay health advisors as community change agents. Fam Community Health. 1992;15:24–40. [Google Scholar]
- 9.Service C, Salber E. Community Health Education: The Lay Health Advisor Approach. Durham, NC: Duke University Health Care System; 1979. [Google Scholar]
- 10.Kahssay H, Taylor ME, Berman PA. Community Health Workers: The Way Forward. Geneva, Switzerland: World Health Organization; 1998. [Google Scholar]
- 11.World Health Organization. Declaration of Alma Ata. 1978. Available at: http://www.who.int/hpr/archive/docs/almaata.html. Accessed: 23 January 2005. [Google Scholar]
- 12.Chelala C. Bolivian soldiers double up as health workers. Lancet. 2000;355:2057. doi: 10.1016/s0140-6736(05)73510-8. [DOI] [PubMed] [Google Scholar]
- 13.Bertrand JT, Santiso R, Linder SH, et al. Evaluation of a communications program to increase adoption of vasectomy in Guatemala. Stud Fam Plann. 1987;18:361–70. [Google Scholar]
- 14.Rodriguez-Garcia R, Aumack KJ, Uamos A. A community-based approach to the promotion of breastfeeding in Mexico. J Obstet Gynecol Neonat Nurs. 1990;19:431–8. doi: 10.1111/j.1552-6909.1990.tb01662.x. [DOI] [PubMed] [Google Scholar]
- 15.Frazão P, Marques D. Efetividade de programa de agentes comunitários na promoção da saúde bucal. Rev Saúde Públ. 2009;43:463–71. doi: 10.1590/s0034-89102009000300010. [DOI] [PubMed] [Google Scholar]
- 16.Wilson K, Brownstein JN, Blanton C. Community Health Advisors/Community Health Workers: Selected Annotations and Programs in the United States. Atlanta, GA: US Department of Human Services, Centers for Disease Control and Prevention; 1998. Community health advisor use: insights from a national survey. [Google Scholar]
- 17.HRSA. Impact of Community Health Workers on Access, Use of Services, and Patient Knowledge and Behavior. Rockville, MD: Bureau of Primary Health Care, Health Resources and Services Administration, US Department of Health and Human Services; 1998. [Google Scholar]
- 18.Nemcek MA, Sabatier R. State of evaluation: community health workers. Public Health Nurs. 2003;20:260–70. doi: 10.1046/j.1525-1446.2003.20403.x. [DOI] [PubMed] [Google Scholar]
- 19.Earp JA, Viadro CI, Altpeter M, et al. Lay health advisors: a strategy for getting the word out about breast cancer. Health Educ Behav. 1997;24:432–51. doi: 10.1177/109019819702400404. [DOI] [PubMed] [Google Scholar]
- 20.University of Arizona. A Summary of the National Community Health Advisor Study. Baltimore, MD: Annie E. Casey Foundation; 1998. [Google Scholar]
- 21.Salber EJ, Beery WL, Jackson EJ. The role of the health facilitator in community health education. J Community Health. 1976;2:5–20. doi: 10.1007/BF01349488. [DOI] [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services. Community Health Advisors: Models, Research, and Practice. Atlanta, GA: USDHHS, Public Health Services, Centers for Disease Control and Prevention; 1994. [Google Scholar]
- 23.Witmer A, Seifer SD, Finocchio L, et al. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cherrington A, Ayala GX, Amick H, et al. Implementing the community health worker model within diabetes management: challenges and lessons learned from programs across the U.S. Diabetes Educ. 2008;34:824–33. doi: 10.1177/0145721708323643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elder JP, Ayala GX, Parra-Medina D, et al. Health promotion in the Latino community: communication issues and approaches. Annu Rev Public Health. 2009;30:227–51. doi: 10.1146/annurev.publhealth.031308.100300. [DOI] [PubMed] [Google Scholar]
- 26.Johnson J, Sleath B, Ayala GX, et al. Glaxo-Smith-Kline Report. Chapel Hill, NC: University of North Carolina at Chapel Hill; 2006. A demographic profile of U.S. Hispanic markets. [Google Scholar]
- 27.Glasgow RE, Klesges LM, Dzewaltowski DA, et al. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27:3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 28.Glasgow RE, McKay HG, Piette JD, et al. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44:119–27. doi: 10.1016/s0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 29.Steckler A, Linnan L. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 30.Green LW, Kreuter MW. Health program planning: an educational and ecological approach. 4th edn. New York: McGraw-Hill Higher Education; 2005. [Google Scholar]
- 31.Rogers EM. Diffusion of Innovations. New York: Free Press; 2003. [Google Scholar]
- 32.Cooper H. Synthesizing Research: A Guide for Literature Reviews. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 33.Larson K, McGuire J, Watkins E, et al. Maternal care coordination for migrant farmworker women: program structure and evaluation of effects on use of prenatal care and birth outcome. J Rural Health. 1992;8:128–33. doi: 10.1111/j.1748-0361.1992.tb00338.x. [DOI] [PubMed] [Google Scholar]
- 34.Suarez L, Roche RA, Pulley LV, et al. Why a peer intervention program for Mexican-American women failed to modify the secular trend in cancer screening. Am J Prev Med. 1997;13:411–7. [PubMed] [Google Scholar]
- 35.Suarez L, Nichols DC, Brady CA. Use of peer role models to increase Pap smear and mammogram screening in Mexican-American and black women. Am J Prev Med. 1993;9:290–6. [PubMed] [Google Scholar]
- 36.Suarez L, Nichols DC, Pulley L, et al. Local health departments implement a theory-based model to increase breast and cervical cancer screening. Public Health Rep. 1993;108:477–82. [PMC free article] [PubMed] [Google Scholar]
- 37.Freeman RC, Williams ML, Saunders LA. Drug use, AIDS knowledge, and HIV risk behaviors of Cuban-, Mexican-, and Puerto-Rican-born drug injectors who are recent entrants into the United States. Substance Use Misuse. 1999;34:1765–93. doi: 10.3109/10826089909039426. [DOI] [PubMed] [Google Scholar]
- 38.Sennott-Miller L, May KM, Miller JL. Demographic and health status indicators to guide health promotion for Hispanic and Anglo rural elderly. Patient Educ Couns. 1998;33:13–23. doi: 10.1016/s0738-3991(97)00046-3. [DOI] [PubMed] [Google Scholar]
- 39.Hunter J, de Zapien JG, Papenfuss M, et al. The impact of a promotora on increasing routine chronic disease prevention among women 40 years of age and older at the U.S.-Mexico border. Health Educ Behav. 2004;31:18S–28S. doi: 10.1177/1090198104266004. [DOI] [PubMed] [Google Scholar]
- 40.HRSA. Community Health Worker National Workforce Study. 2007. Available at: ftp://ftp.hrsa.gov/bhpr/workforce/chw307.pdf. Accessed: 14 September 2009. [Google Scholar]
- 41.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10:282–98. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 42.Ramos RL, Hernandez A, Ferreira-Pinto JB, et al. Promovision: designing a capacity-building program to strengthen and expand the role of promotores in HIV prevention. Health Promot Pract. 2006;7:444–9. doi: 10.1177/1524839905278868. [DOI] [PubMed] [Google Scholar]
- 43.Elder JP, Ayala GX, Slymen DJ, et al. Evaluating psychosocial and behavioral mechanisms of change in a tailored communication intervention. Health Educ Behav. 2007;36:366–80. doi: 10.1177/1090198107308373. [DOI] [PubMed] [Google Scholar]
- 44.Elder JP, Ayala GX, Campbell NR, et al. Interpersonal and print nutrition communication for a Spanish-dominant Latino population: Secretos de la Buena Vida. Health Psychol. 2005;24:49–57. doi: 10.1037/0278-6133.24.1.49. [DOI] [PubMed] [Google Scholar]
- 45.Rhodes SD, Foley KL, Zometa CS, et al. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med. 2007;33:418–27. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 46.Viswanathan M, Kraschnewski J, Nishikawa B, et al. Evidence Report/Technology Assessment. No. 181, AHRQ Publication No. 09-E014, RTI International–University of North Carolina Evidence-Based Practice Center. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Outcomes of community health worker interventions. [Google Scholar]
- 47.Brand J. Family planning: extension aides see need. J Ext. 1972;10:25–35. [Google Scholar]
- 48.Pilisuk M, Parks SH, Kelly J, et al. The helping network approach: community promotion of mental health. J Prim Prev. 1982;3:116–32. doi: 10.1007/BF01324670. [DOI] [PubMed] [Google Scholar]
- 49.Tiernan KM. Training volunteers in risk-reduction education: a program in a US-Mexican border community. Fam Community Health. 1988;11:60–72. doi: 10.1097/00003727-198805000-00010. [DOI] [PubMed] [Google Scholar]
- 50.Amezcua C, McAlister AL, Ramirez A, et al. A Su Salud: health promotion in a Mexican-American border community. In: Braecht N, editor. Health Promotion at the Community Level. Newbury Park, CA: Sage; 1990. pp. 257–77. [Google Scholar]
- 51.Brownstein JN, Cheal N, Ackermann SP, et al. Breast and cervical cancer screening in minority populations: a model for using lay health educators. J Cancer Educ. 1992;7:321–6. doi: 10.1080/08858199209528189. [DOI] [PubMed] [Google Scholar]
- 52.Watkins EL, Harlan C, Eng E, et al. Assessing the effectiveness of lay health advisors with migrant farmworkers. Fam Community Health. 1994;16:72–87. [Google Scholar]
- 53.Watkins EL, Larson K, Harlan C, et al. A model program for providing health-services for migrant farmworker mothers and children. Public Health Rep. 1990;105:567–75. [PMC free article] [PubMed] [Google Scholar]
- 54.May KM, Mendelson C, Ferketich S. Community empowerment in rural health care. Public Health Nurs. 1995;12:25–30. doi: 10.1111/j.1525-1446.1995.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 55.Navarro AM, Rock CL, McNicholas LJ, et al. Community-based education in nutrition and cancer: the Por La Vida Cuidandome curriculum. J Cancer Educ. 2000;15:168–72. doi: 10.1080/08858190009528687. [DOI] [PubMed] [Google Scholar]
- 56.Navarro AM, Senn KL, Kaplan RM, et al. Por La Vida intervention model for cancer prevention in Latinas. J Natl Cancer Inst Monogr. 1995;18:137–45. [PubMed] [Google Scholar]
- 57.Navarro AM, Senn KL, McNicholas LJ, et al. Por La Vida model intervention enhances use of cancer screening tests among Latinas. Am J Prev Med. 1998;15:32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- 58.Ramirez AG, McAlister A, Gallion KJ, et al. Community level cancer control in a Texas barrio: Part I—theoretical basis, implementation, and process evaluation. J Natl Cancer Inst Monogr. 1995;18:117–22. [PubMed] [Google Scholar]
- 59.Wiist WH, Jackson RH, Jackson KW. Peer and community leader education to prevent youth violence. Am J Prev Med. 1996;12:56–64. [PubMed] [Google Scholar]
- 60.Hanson J. Parental self-efficacy and asthma self-management skills. J Soc Pediatr Nurs. 1998;3:146–54. doi: 10.1111/j.1744-6155.1998.tb00222.x. [DOI] [PubMed] [Google Scholar]
- 61.Alcalay R, Alvarado M, Balcazar H, et al. Salud para su Corazón: a community-based Latino cardiovascular disease prevention and outreach model. J Community Health. 1999;24:359–79. doi: 10.1023/a:1018734303968. [DOI] [PubMed] [Google Scholar]
- 62.Balcazar H, Alvarado M, Hollen ML, et al. Salud Para Su Corazon-NCLR: a comprehensive Promotora outreach program to promote heart-healthy behaviors among hispanics. Health Promot Pract. 2006;7:68–77. doi: 10.1177/1524839904266799. [DOI] [PubMed] [Google Scholar]
- 63.Balcazar H, Alvarado M, Hollen ML, et al. Evaluation of Salud Para Su Corazón (Health for your Heart)—National Council of La Raza Promotora Outreach Program. Prev Chronic Dis. 2005;2:A09. [PMC free article] [PubMed] [Google Scholar]
- 64.Bell RA, Hillers VN, Thomas TA. The Abuela Project: safe cheese workshops to reduce the incidence of Salmonella typhimurium from consumption of raw-milk fresh cheese. Am J Public Health. 1999;89:1421–4. doi: 10.2105/ajph.89.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Buller DB, Morrill C, Taren D, et al. Randomized trial testing the effect of peer education at increasing fruit and vegetable intake. J Natl Cancer Inst. 1999;91:1491–500. doi: 10.1093/jnci/91.17.1491. [DOI] [PubMed] [Google Scholar]
- 66.Larkey LK, Alatorre C, Buller DB, et al. Communication strategies for dietary change in a worksite peer educator intervention. Health Educ Res. 1999;14:777–90. doi: 10.1093/her/14.6.777. [DOI] [PubMed] [Google Scholar]
- 67.Whitehorse LE, Manzano R, Baezconde-Garbanati LA, et al. Culturally tailoring a physical activity program for Hispanic women: recruitment success of La Vida Buena's salsa aerobics. J Health Educ. 1999;30:S18–24. [Google Scholar]
- 68.Cravey AJ, Arcury TA, Quandt SA. Mapping as a means of farmworker education and empowerment. J Geogr. 2000;99:229–37. doi: 10.1080/00221340008978973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Taylor T, Serrano E, Anderson J. Management issues related to effectively implementing a nutrition education program using peer educators. J Nutr Educ. 2001;33:284–92. doi: 10.1016/s1499-4046(06)60293-5. [DOI] [PubMed] [Google Scholar]
- 70.Taylor T, Serrano E, Anderson J, et al. Knowledge, skills, and behavior improvements on peer educators and low-income Hispanic participants after a stage of change-based bilingual nutrition education program. J Community Health. 2000;25:241–62. doi: 10.1023/a:1005160216289. [DOI] [PubMed] [Google Scholar]
- 71.Ramos IN, May M, Ramos KS. Environmental health training of promotoras in colonias along the Texas-Mexico border. Am J Public Health. 2001;91:568–70. doi: 10.2105/ajph.91.4.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Watson MR, Horowitz AM, Garcia I, et al. A community participatory oral health promotion program in an inner-city Latino community. J Public Health Dent. 2001;61:34–41. doi: 10.1111/j.1752-7325.2001.tb03353.x. [DOI] [PubMed] [Google Scholar]
- 73.Woodruff SI, Talavera GA, Elder JP. Evaluation of a culturally appropriate smoking cessation intervention for Latinos. Tob Control. 2002;11:361–7. doi: 10.1136/tc.11.4.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim S, Koniak-Griffin D, Flaskerud JH, et al. The impact of lay health advisors on cardiovascular health promotion: using a community-based participatory approach. J Cardiovasc Nurs. 2004;19:192–9. doi: 10.1097/00005082-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 75.Conway TL, Woodruff SI, Edwards CC, et al. Intervention to reduce environmental tobacco smoke exposure in Latino Children: null effects on hair biomarkers and parent reports. Tob Control. 2004;13:90–2. doi: 10.1136/tc.2003.004440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rodriguez VM, Conway TL, Woodruff SI, et al. Pilot test of an assessment instrument for Latina community health advisors conducting an ETS intervention. J Immigr Health. 2003;5:129–37. doi: 10.1023/a:1023991818829. [DOI] [PubMed] [Google Scholar]
- 77.Woodruff SI, Conway TL, Elder JP, et al. Pilot study using hair nicotine feedback to reduce Latino children's environmental tobacco smoke exposure. Am J Health Promot. 2007;22:93–7. doi: 10.4278/0890-1171-22.2.93. [DOI] [PubMed] [Google Scholar]
- 78.Forst L, Lacey S, Chen HY, et al. Effectiveness of community health workers for promoting use of safety eyewear by Latino farm workers. Am J Ind Med. 2004;46:607–13. doi: 10.1002/ajim.20103. [DOI] [PubMed] [Google Scholar]
- 79.Elder JP, Ayala GX, Campbell NR, et al. Long-term effects of a communication intervention for Spanish-dominant Latinas. Am J Prev Med. 2006;31:159–66. doi: 10.1016/j.amepre.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 80.Staten LK, Scheu LL, Bronson D, et al. Pasos Adelante: the effectiveness of a community-based chronic disease prevention program. Prev Chronic Dis. 2005;2:A18. [PMC free article] [PubMed] [Google Scholar]
- 81.Teufel-Shone NI, Drummond R, Rawiel U. Developing and adapting a family-based diabetes program at the U.S.-Mexico border. Prev Chronic Dis. 2005;2:A20. [PMC free article] [PubMed] [Google Scholar]
- 82.Larkey L. Las mujeres saludables: reaching Latinas for breast, cervical and colorectal cancer prevention and screening. J Community Health. 2006;31:69–77. doi: 10.1007/s10900-005-8190-2. [DOI] [PubMed] [Google Scholar]
- 83.Martin M, Holden J, Chen Z, et al. Child passenger safety for inner-city Latinos: new approaches from the community. Injury Prev. 2006;12:99–104. doi: 10.1136/ip.2005.009480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Culica D, Walton JW, Prezio EA. CoDE: Community Diabetes Education for uninsured Mexican Americans. Proc (Bayl Univ Med Cent) 2007;20:111–7. doi: 10.1080/08998280.2007.11928263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Joshu CE, Rangel L, Garcia O, et al. Integration of a promotora-led self-management program into a system of care. Diabetes Educ. 2007;33(Suppl. 6) doi: 10.1177/0145721707304076. 151S–8S. [DOI] [PubMed] [Google Scholar]
- 86.Lujan J, Ostwald SK, Ortiz M. Promotora diabetes intervention for Mexican Americans. Diabetes Educ. 2007;33:660–70. doi: 10.1177/0145721707304080. [DOI] [PubMed] [Google Scholar]
- 87.Sauaia A, Min SJ, Lack D, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Prev Chronic Dis. 2007;4:A99. [PMC free article] [PubMed] [Google Scholar]
- 88.Welsh AL, Sauaia A, Jacobellis J, et al. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Prev Chronic Dis. 2005;2:A07. [PMC free article] [PubMed] [Google Scholar]
- 89.Vincent D, Pasvogel A, Barrera L. A feasibility study of a culturally tailored diabetes intervention for Mexican Americans. Biol Res Nurs. 2007;9:130–41. doi: 10.1177/1099800407304980. [DOI] [PubMed] [Google Scholar]
- 90.Carrillo JM, Pust RE, Borbon J. Dar a Luz: a perinatal care program for Hispanic women on the U.S.-Mexico border. Am J Prev Med. 1986;2:26–9. [PubMed] [Google Scholar]
- 91.McElmurry BJ, Swider SM, Grimes MJ, et al. Health advocacy for young, low-income, inner-city women. ANS Adv Nurs Sci. 1987;9:62–75. doi: 10.1097/00012272-198707000-00009. [DOI] [PubMed] [Google Scholar]
- 92.Dawson PM, Robinson JL, Butterfield PM, et al. Supporting new parents through home visits: effects on mother–infant interaction. Top Early Child Spec Educ. 1991;10:29–44. [Google Scholar]
- 93.Meister JS, Warrick LH, de Zapién JG, et al. Using lay health workers: case study of a community-based prenatal intervention. J Community Health. 1992;17:37–51. doi: 10.1007/BF01321723. [DOI] [PubMed] [Google Scholar]
- 94.Warrick LH, Wood AH, Meister JS, et al. Evaluation of a peer health worker prenatal outreach and education program for Hispanic farmworker families. J Community Health. 1992;17:13–26. doi: 10.1007/BF01321721. [DOI] [PubMed] [Google Scholar]
- 95.Birkel RC, Golaszewski T, Koman JJ, 3rd, et al. Findings from the Horizontes Acquired Immune Deficiency Syndrome Education Project: the impact of indigenous outreach workers as change agents for injection-drug users. Health Educ Q. 1993;20:523–38. doi: 10.1177/109019819302000411. [DOI] [PubMed] [Google Scholar]
- 96.Morris DL, Felkner M, McLean CH. Pap screening in the Rio Grande Valley: a case study. Fam Community Health. 1994;17:1–14. [Google Scholar]
- 97.McFarlane J, Kelly E, Rodriguez R, et al. De Madres a Madres: women building community coalitions for health. Health Care Women Int. 1994;15:465–76. doi: 10.1080/07399339409516137. [DOI] [PubMed] [Google Scholar]
- 98.McFarlane J, Fehir J. De Madres a Madres: a community, primary health care program based on empowerment. Health Educ Q. 1994;21:381–94. doi: 10.1177/109019819402100309. [DOI] [PubMed] [Google Scholar]
- 99.Mahon J, McFarlane J, Golden K. De Madres a Madres: a community partnership for health. Public Health Nurs. 1991;8:15–9. doi: 10.1111/j.1525-1446.1991.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 100.Bray ML, Edwards LH. A primary health care approach using Hispanic outreach workers as nurse extenders. Public Health Nurs. 1994;11:7–11. doi: 10.1111/j.1525-1446.1994.tb00383.x. [DOI] [PubMed] [Google Scholar]
- 101.Nyamathi AM, Flaskerud J, Bennett C, et al. Evaluation of two AIDS education programs for impoverished Latina women. AIDS Educ Prev. 1994;6:296–309. [PubMed] [Google Scholar]
- 102.Brown SA, Hanis CL. A community-based, culturally sensitive education and group-support intervention for Mexican Americans with NIDDM: a pilot study of efficacy. Diabetes Educ. 1995;21:203–10. doi: 10.1177/014572179502100307. [DOI] [PubMed] [Google Scholar]
- 103.Castro FG, Elder J, Coe K, et al. Mobilizing churches for health promotion in Latino communities: Companeros en la Salud. J Natl Cancer Inst Monogr. 1995;18:127–35. [PubMed] [Google Scholar]
- 104.Bird JA, Otero-Sabogal R, Ha NT, et al. Tailoring lay health worker interventions for diverse cultures: lessons learned from Vietnamese and Latina communities. Health Educ Q. 1996;23(Suppl.):S105–22. [Google Scholar]
- 105.Pérez-Stable EJ, Otero-Sabogal R, Sabogal F, et al. Pathways to early cancer detection for Latinas: En Acción Contra el Cancer. Health Educ Q. 1996;23:S41–59. [Google Scholar]
- 106.Singer M, Marxuach-Rodriquez L. Applying anthropology to the prevention of AIDS: the Latino gay men's health project. Hum Organ. 1996;55:141–8. [Google Scholar]
- 107.Baker EA, Bouldin N, Durham M, et al. The Latino Health Advocacy Program: a collaborative lay health advisor approach. Health Educ Behav. 1997;24:495–509. doi: 10.1177/109019819702400408. [DOI] [PubMed] [Google Scholar]
- 108.Booker V-K, Robinson JG, Kay BJ, et al. Changes in empowerment: effects of participation in a lay health promotion program. Health Educ Behav. 1997;24:452–64. doi: 10.1177/109019819702400405. [DOI] [PubMed] [Google Scholar]
- 109.Corkery E, Palmer C, Foley ME, et al. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care. 1997;20:254–7. doi: 10.2337/diacare.20.3.254. [DOI] [PubMed] [Google Scholar]
- 110.Warren BE. Sex, truth, and videotape: HIV prevention at the gender identity project in New York city. Int J Transgender. 1999 3: np. [Google Scholar]
- 111.Flaskerud JH, Nyamathi AM. Collaborative inquiry with low-income Latina women. J Health Care Poor Underserved. 2000;11:326–42. doi: 10.1353/hpu.2010.0738. [DOI] [PubMed] [Google Scholar]
- 112.McQuiston C, Uribe L. Latino recruitment and retention strategies: community-based HIV prevention. J Immigrant Health. 2001;3:97–105. doi: 10.1023/A:1009565900783. [DOI] [PubMed] [Google Scholar]
- 113.McQuiston C, Flaskerud JH. ‘If they don't ask about condoms, I just tell them’: a descriptive case study of Latino lay health advisers’ helping activities. Health Educ Behav. 2003;30:79–96. doi: 10.1177/1090198102239260. [DOI] [PubMed] [Google Scholar]
- 114.McQuiston C, Choi-Hevel S, Clawson M. Protegiendo Nuestra Comunidad: empowerment participatory education for HIV prevention. J Transcult Nurs. 2001;12:275–83. doi: 10.1177/104365960101200402. [DOI] [PubMed] [Google Scholar]
- 115.Hiatt RA, Pasick RJ, Stewart S, et al. Community-based cancer screening for underserved women: design and baseline findings from the Breast and Cervical Cancer Intervention Study. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2001;33:190–203. doi: 10.1006/pmed.2001.0871. [DOI] [PubMed] [Google Scholar]
- 116.McElmurry BJ, Park CG, Buseh AG. The nurse-community health advocate team for urban immigrant primary health care. J Nurs Scholarsh. 2003;35:275–81. doi: 10.1111/j.1547-5069.2003.00275.x. [DOI] [PubMed] [Google Scholar]
- 117.Mayo RM, Sherrill WW, Crew L, et al. Connecting rural African American and Hispanic women to cancer education and screening: the Avon Health Connector project. J Cancer Educ. 2004;19:123–6. doi: 10.1207/s15430154jce1902_14. [DOI] [PubMed] [Google Scholar]
- 118.Hansen LK, Feigl P, Modiano MR, et al. An educational program to increase cervical and breast cancer screening in Hispanic women: a Southwest Oncology Group study. Cancer Nurs. 2005;28:47–53. doi: 10.1097/00002820-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 119.Martin MA, Hernández O, Naureckas E, et al. Reducing home triggers for asthma: the Latino community health worker approach. J Asthma. 2006;43:369–74. doi: 10.1080/02770900600709781. [DOI] [PubMed] [Google Scholar]
- 120.Reinschmidt KM, Hunter JB, Fernández ML, et al. Understanding the success of promotoras in increasing chronic diseases screening. J Health Care Poor Underserved. 2006;17:256–64. doi: 10.1353/hpu.2006.0066. [DOI] [PubMed] [Google Scholar]
- 121.Ingram M, Torres E, Redondo F, et al. The impact of promotoras on social support and glycemic control among members of a farmworker community on the US-Mexico border. Diabetes Educ. 2007;33(Suppl. 6) doi: 10.1177/0145721707304170. 172S–8S. [DOI] [PubMed] [Google Scholar]
- 122.Thompson JR, Horton C, Flores C. Advancing diabetes self-management in the Mexican American population: a community health worker model in a primary care setting. Diabetes Educ. 2007;33(Suppl 6) doi: 10.1177/0145721707304077. 159S–65S. [DOI] [PubMed] [Google Scholar]
- 123.Cuellar I, Harris LC, Jasso R. An acculturation scale for Mexican-American normal and clinical populations. Hisp J Behav Sci. 1980;2:199–217. [Google Scholar]
- 124.Marin G, Sabogal F, Marin BV, et al. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 125.Cuéllar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: a revision of the original ARSMA Scale. Hisp J Behav Sci. 1995;17:275–304. [Google Scholar]