Abstract
Chemokines and their receptors have crucial roles in the trafficking of leukocytes, and are of particular interest in the context of the unique immune responses elicited in the central nervous system (CNS). The chemokine system CC ligand 2 (CCL2) with its receptor CC receptor 2 (CCR2), as well as the receptor CXCR2 and its multiple ligands CXCL1, CXCL2 and CXCL8, have been implicated in a wide range of neuropathologies, including trauma, ischemic injury and multiple sclerosis. This review aims to overview the current understanding of chemokines as mediators of leukocyte migration into the CNS under neuroinflammatory conditions. We will specifically focus on the involvement of two chemokine networks, namely CCL2/CCR2 and CXCL8/CXCR2, in promoting macrophage and neutrophil infiltration, respectively, into the lesioned parenchyma after focal traumatic brain injury. The constitutive brain expression of these chemokines and their receptors, including their recently identified roles in the modulation of neuroprotection, neurogenesis, and neurotransmission, will be discussed. In conclusion, the value of evidence obtained from the use of Ccl2- and Cxcr2-deficient mice will be reported, in the context of potential therapeutics inhibiting chemokine activity which are currently in clinical trial for various inflammatory diseases.
Keywords: monocyte chemoattractant protein-1, traumatic brain injury
Introduction
Chemokines, or chemotactic cytokines, are classically defined by their ability to induce directional migration and activation of leukocyte subsets into inflammatory sites. Since the identification of the first human chemokines nearly two decades ago, extensive research has accumulated showing the significant contribution of these small, peptide mediators to inflammatory conditions. In the central nervous system (CNS), chemokines such as CC ligand 2 (CCL2) and its receptor CC receptor 2 (CCR2) have been implicated in neuropathologies ranging from traumatic brain injury (TBI) to autoimmune diseases.
Chemokines are classified on the basis of structural features, which in turn, give rise to their functional specificity. The two main categories recognized are CXC or α-chemokines and CC or β-chemokines; CXC chemokines have one amino-acid residue separating two conserved cysteines and are primarily chemotactic for neutrophils, whereas CC chemokines that contain two adjacent cysteines are attractants for monocytic cells and lymphocytes (Zlotnik and Yoshie, 2000). There is considerable overlap and interaction between related chemokines and their receptors, whereby one chemokine can bind to various receptors, resulting in redundancy within the signaling network.
This review aims at providing an outline of the CCL2/CCR2 and CXCL8/CXCR2 chemokine networks in the brain, their functions, and contribution to pathologic conditions. Constitutive expression of chemokines in the CNS and the proposed roles of these mediators in neurogenesis, neuroprotection, and neurotransmission will also be discussed. Finally, we will report the current progress and issues associated with drug development aimed at therapeutically targeting chemokines in the CNS and systemic diseases. Multiple database searches were conducted from 2006 to 2009 to identify relevant references, and retrieved documents were hand-searched for additional publications. References included in this review were those deemed significant to the development of a solid understanding of the chemokine networks discussed.
The macrophage chemoattractant CCL2
There are five known members of the monocyte chemoattractant protein (MCP) family, designated as CCL2, CCL8, CCL7, CCL13, and CCL12 (MCP-1-5, respectively). Each family member attracts a different subset of leukocytes after binding with different affinities to several receptors (Gouwy et al, 2004). Although CCL2, CCL7, and CCL8 are able to signal through the CCR2 receptor, CCL2 is the most potent at activating signal transduction pathways leading to monocyte transmigration (Sozzani et al, 1994).
CCL2, also known as MCP-1/JE, was the first human chemokine to be characterized (Rollins, 1996; Yoshimura et al, 1989). Its ability to activate and attract cells of the monocyte lineage including macrophages, monocytes, and microglia has been repeatedly shown by in vitro assays (Rollins, 1991; Yoshimura and Leonard, 1992). Targeted Ccl2 overexpression in the thymus and CNS of transgenic mice resulted in the accumulation of macrophages in these organs, which is further evidence of chemotactic function (Fuentes et al, 1995; Gunn et al, 1997; Wang et al, 2002). Conversely, mice deficient in Ccl2 are reportedly unable to effectively recruit monocytes in response to an inflammatory stimulus, despite the presence of normal circulating leukocyte numbers (Lu et al, 1998).
In the brain, a positive correlation has been found between the level of Ccl2 expression and the number of infiltrated macrophages after a cortical aspiration lesion (Hausmann et al, 1998). Concordantly, recombinant CCL2 injected into the murine hippocampus induced leukocyte accumulation, with greater potency than did other monocyte chemokines, such as CCL5 (Bell et al, 1996). Besides monocytic cells, CCL2 is reportedly also a chemoattractant for T lymphocytes, basophils, natural killer cells, and astrocytes in vitro (Ge and Pachter, 2004; Rollins, 1996; Woldemar Carr et al, 1994). However, the physiologic impact of CCL2-mediated recruitment of these cells in vivo needs to be determined.
CCR2 receptor structure and intracellular signaling in the central nervous system
CCL2 binds primarily to the G-protein-coupled receptor CCR2, an interaction that is responsible for the initial phase of monocyte recruitment (Dzenko et al, 2001; Dzenko et al, 2005; Kuziel et al, 1997). Dimerized CCL2 binds the receptor, which is then internalized and removed from the cell surface. This process has been proposed to regulate extracellular CCL2 levels (Mahad et al, 2006; Tylaska et al, 2002; Zhang and Rollins, 1995). Downstream targets of CCR2 signaling include phosphatidylinositol-3 kinase, mitogen-activated protein kinases, and protein kinase C, indicating that a wide range of intracellular pathways may be involved in cellular responses elicited by CCL2 (Stamatovic et al, 2005; Wain et al, 2002).
In the CNS, CCR2 expression has been reported on various cell types, including neurons, astrocytes, microglia, neural progenitor cells, and microvascular endothelial cells (Banisadr et al, 2002, 2005; Coughlan et al, 2000; Gourmala et al, 1997; Stamatovic et al, 2005). During normal conditions, expression seems to be at consistently low levels. Astrocyte and microglial CCR2 expression seems to be quite heterogeneous and subject to significant upregulation during an inflammatory response (Andjelkovic et al, 2002; Croitoru-Lamoury et al, 2003; White et al, 2005).
Consistent with studies using Ccl2 knockout mice, deficiency of the Ccr2 gene results in impaired macrophage recruitment in several injury and disease models (Göser et al, 2005). Decreased leukocyte adhesion and monocyte infiltration have been shown in Ccr2−/− mice after an immune challenge with intraperitoneal thioglycollate injections (Kurihara et al, 1997), whereas delayed monocyte extravasation was observed after spinal cord contusion injuries in Ccr2−/− mice (Ma et al, 2002). Emerging evidence indicates that CCR2 expression distinguishes the two subsets of blood monocytes in mice: the Ly-6Chigh(Gr-1high) CCR2+CX3CR1low phenotype is found on phagocytic monocyte cells which readily infiltrate into inflammatory sites, whereas Ly-6Clow(Gr-1low)CCR2−CX3CR1high cells are less effective at transmigration and are believed to give rise to resident tissue macrophages (Geissmann et al, 2003). These subsets correspond, respectively, to the CCR2+CD16− and CCR2−CD16+ monocyte populations in humans.
The CCL2/CCR2 network in the central nervous system
In the brain, CCL2 is predominantly produced by astrocytes and resident microglia, and to a lesser extent, by endothelial cells (Barna et al, 1994; Berman et al, 1996; Glabinski et al, 1996; Hanisch, 2002; Harkness et al, 2003). CCL2 is also released by infiltrating macrophages upon their migration into the brain parenchyma, implying the presence of autocrine regulation that perpetuates cell recruitment and activation (Clavo et al, 1996; Gourmala et al, 1997; Gunn et al, 1997; Peterson et al, 1997). Neurons are yet another source, producing detectable levels of CCL2 after brain ischemia (Che et al, 2001; Gourmala et al, 1997), transection of facial or hypoglossal nerves (Flugel et al, 2001), and lipopolysaccharide administration (Gourmala et al, 1997).
A wide range of stimuli can trigger CCL2 production and release during an inflammatory response. Treatment with lipopolysaccharide, interferon, interleukin-1 beta (IL-1β), colony-stimulating factor-1, transforming growth factor-β, and tumor necrosis factor-α (TNFα) can induce CCL2 expression in different cell types either in vivo or in vitro (Clavo et al, 1996; Harkness et al, 2003; Huang et al, 2000; Hurwitz et al, 1995; Thibeault et al, 2001). In contrast, retinoic acid, glucocorticoids, and estrogen reportedly inhibit CCL2 production (Melgarejo et al, 2009). A more comprehensive understanding of these mechanisms may provide fundamental evidence, whereby pathological neuroinflammation may be therapeutically manipulated.
The CCL2/CCR2 network in brain development and neurotransmission
A distinct pattern of CCL2 and CCR2 expression has been identified at different embryonic stages in relation to the cytoarchitectural organization of the CNS, implying a role for this chemokine network during brain development (Meng et al, 1999; Rezaie et al, 2002). Treatment of rat embryonic cultures with CCL2 and CCL7 increased the differentiation of cells toward a dopaminergic phenotype (Edman et al, 2008). Complementing these data, the application of CCL2 to dopaminergic neurons in vivo increased cell excitability, dopamine release, and locomotor activity in rats (Guyon et al, 2009). These novel findings show a previously unknown role for this chemokine in mediating dopaminergic neuron signaling and development.
CCL2 as a modulator of blood–brain barrier permeability
The highly selective blood–brain barrier (BBB) is largely impervious to circulating leukocytes. As CCL2 production in the brain is primarily intraparenchymal, it is still unclear how this hydrophilic protein communicates with the periphery to attract blood-borne monocytes. It is conceivable that CCL2 is released directly into the bloodstream by astrocytes and brain microvascular endothelial cells, which comprise the BBB. Alternatively, CCL2 may be transported transcellularly across the BBB, possibly by interaction with specific carrier molecules, such as caveolin-1 (Ge and Pachter, 2004).
In addition to its chemotactic properties, recent evidence indicates that CCL2 has direct effects on BBB permeability (Dzenko et al, 2005; Song and Pachter, 2004). Stamatovic et al (2005) showed that exposure of astrocytes and brain microvascular endothelial cells to CCL2 in vitro induced changes in actin cytoskeletal structure and redistribution of tight junction protein expression, thereby rendering the BBB more porous and facilitating the transendothelial migration of blood-borne leukocytes into the brain. These effects were attenuated in CCL2-treated animals that had been previously depleted of peripheral macrophages, indicating that this chemokine acts directly on endothelial cells of the BBB, and indirectly, by the recruitment of macrophages and subsequent changes in BBB permeability (Stamatovic et al, 2005). In a separate study by the same group, a reduction in BBB permeability resulted from the use of antisense oligonucleotides or neutralizing antibodies blocking CCL2 in an in vitro model of ischemia–reperfusion injury (Dimitrijevic et al, 2006). According to this model, CCL2 modulation of BBB permeability appears to be mediated specifically by CCR2 expressed on endothelial cells, as tight junction protein distribution and BBB permeability were not altered by CCL2 treatment in Ccr2−/− mice (Stamatovic et al, 2003).
The CCL2/CCR2 network in brain pathologies
Multiple Sclerosis
Multiple sclerosis (MS) is a chronic autoimmune disease characterized by extensive demyelination and inflammation, leading to a severe and progressive neurologic impairment. Inflammation has a critical role in MS, predominantly mediated by auto-reactive T cells infiltrating the brain parenchyma (Mahad and Ransohoff, 2003). The presence of CCL2 has been shown in autopsy tissue obtained from patients with both active and chronic MS, correlating with regions of hypertrophic astrocytes and macrophage infiltration, thus implicating CCL2 in this pathology (McManus et al, 1998; Simpson et al, 1998; Van Der Voorn et al, 1999). Interestingly however, CCL2 levels measured in the cerebrospinal fluid (CSF) of patients with MS was consistently attenuated compared with healthy individuals, perhaps as a result of its binding to circulating monocytes, which then downregulate CCR2 as they cross the BBB (Franciotta et al, 2001; Sindern et al, 2001).
Multiple sclerosis can be modeled in rodents by inducing experimental autoimmune encephalomyelitis (EAE), after inoculation of a myelin component, such as myelin basic protein. Elevated astrocytic Ccl2 mRNA has been shown in conjunction with EAE relapses (Ransohoff et al, 1993), although subsequent to the entry of leukocytes into the brain, suggesting that this chemokine has an amplifying effect rather than an initiating role in MS (Glabinski et al, 1995). Both Ccl2−/− and Ccr2−/− mice show impaired macrophage recruitment during the course of EAE, and show less severe clinical symptoms compared with wild-type animals (Fife et al, 2000; Huang et al, 2001). Neutralizing antibodies or DNA vaccination against CCL2 before EAE induction similarly alleviate the disease in mice (Kennedy et al, 1998; Youssef et al, 1999).
Ischemic Brain Injury
After cerebral stroke in patients, elevated CCL2 has been detected in both serum and CSF (Arakelyan et al, 2005; Losy and Zaremba, 2001). Transient occlusion of the middle cerebral artery (MCAO), an experimental model of ischemic stroke, similarly triggers CCL2 production in the rodent brain (Che et al, 2001; Gourmala et al, 1997). In transgenic Ccl2 mice, MCAO induced enhanced recruitment of inflammatory cells and exacerbation of infarct volumes (Chen et al, 2003). In contrast, introduction of a nonfunctional Ccl2 gene into rats by the adenoviral vector significantly reduced infarct volume and macrophage infiltration compared with control animals (Kumai et al, 2004). Similarly, Hughes et al (2002) showed that Ccl2 deficiency is neuroprotective, as gene knockout mice exhibited smaller infarct volumes after MCAO as compared with wild-type mice, accompanied by a reduction in macrophage accumulation at 2 weeks (Hughes et al, 2002). A recent study has investigated the underlying mechanisms of CCL2's role in ischemic damage, by using green fluorescent protein transgenic bone marrow chimeras to differentiate between resident CNS microglia and blood-borne macrophages. Despite similar microglial activation early after MCAO, by 7 days, attenuated macrophage infiltration was apparent in both Ccl2- and Ccr2-deficient mice (Schilling et al, 2009a, 2009b). These data corroborate the unequivocal function of Ccl2 for the recruitment of blood-borne macrophages but not of microglia, and supports an association between macrophage accumulation and tissue damage.
Traumatic Brain Injury
Although implicated in TBI, the precise function of CCL2 in the time course of delayed brain damage after trauma still needs to be fully elucidated. A unique role for this chemokine in TBI is substantiated by the observation that Ccl2 mRNA and protein levels are increased acutely in several models of mechanical injury to the brain. Ccl2 expression was markedly increased by 3 h after stab wound injury, followed by an increase in protein levels at 12h (Glabinski et al, 1996), whereas enhanced CCL2 has been detected as early as 2 h after aspiration cortical damage (Hausmann et al, 1998; Muessel et al, 2000). Increased CCL2 has also been reported after diffuse axonal injury (Babcock et al, 2003; Rancan et al, 2001), spinal cord contusion (Ma et al, 2002; McTigue et al, 1998), facial nerve injury (Flugel et al, 2001), and cryogenic cerebral trauma (Grzybicki et al, 1998). Our laboratory has shown that CCL2 that was upregulated after diffuse traumatic axonal injury parallels the increase in sICAM (soluble intracellular adhesion molecule-1), which mediates leukocyte adhesion (Rancan et al, 2001). The involvement of sICAM-1 after TBI is supported by human studies, whereby increased sICAM-1 levels in the CSF correlate with brain contusion size and BBB dysfunction in patients with TBI (Pleines et al, 1998).
Most studies investigating the production of CCL2 in TBI have used noncontusional models, with some involving surgical penetration of the cortex (Babcock et al, 2003; Glabinski et al, 1996) or resection of the brain tissue (Hausmann et al, 1998; Muessel et al, 2000). Lateral fluid percussion and closed head injury models should be considered superior for examining inflammation associated with mechanisms of cerebral contusion formation and thus, most accurately reproducing human TBI. A recent study using a lateral fluid percussion model showed a transient increase in CCL2 peaking at 8 to 12 h in the injured cortex (Rhodes et al, 2009). In our laboratory, CCL2 protein levels peaked between 4 and 12 h after focal closed head injury in the mouse (Semple et al, manuscript in preparation). As this upregulation preceded the accumulation of mononuclear phagocytes in the brain peaking at 3 to 5 days after injury, we hypothesize that CCL2 expression is an early, intrinsic response to TBI, of primary importance in immune cell recruitment. The underlying mechanisms for this time discrepancy, between the early peak in CCL2 production and the delayed arrival of macrophages in the parenchyma several days later, are still unknown.
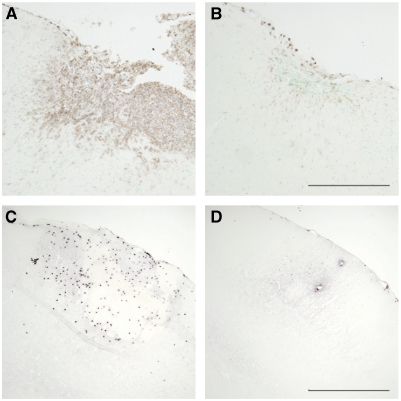
Although most chemokines target more than one receptor and most chemokine receptors bind to multiple ligands in vivo (Kurihara et al, 1997; Lu et al, 1998), additional evidence needs to be acquired to support the nonredundant role of CCL2 in recruiting macrophages in TBI pathology. One group using the aspiration cortical lesion model in Ccl2−/− mice reported attenuated microglial activation correlating with transiently improved survival of thalamic neurons (Muessel et al, 2002). A recently completed study in our laboratory showed that Ccl2−/− mice subjected to closed head injury developed smaller cortical lesions with reduced neuronal loss, diminished macrophage accumulation and astrocyte activation at 4 weeks after injury (Semple et al, manuscript in preparation, Figure 1). A parallel improvement in the neurological outcome of Ccl2−/− mice supports a primarily deleterious role of CCL2 after focal TBI.
Figure 1.
Effect of chemokine ligand or receptor deficiency on leukocyte infiltration after experimental focal traumatic brain injury. Upper microscope images illustrate the accumulation of macrophages and activated microglia in the injured cortex at 4 weeks after closed head injury, which was considerably reduced in Ccl2−/− mice (panel B) compared with wild-type controls (panel A). Lower images show the influx of neutrophils peaking at 12 h after injury in wild-type mice (panel C). In contrast, few neutrophils are able to infiltrate the brains of Cxcr2−/− mice (panel D). Stainings were performed with monoclonal anti-mouse F4/80 and NIMP-R14 antibodies (Serotec, Raleigh, NC, USA), for macrophages/microglia and neutrophils, respectively. Scale bar (panels A and B)=200 μm; (panels C and D)=500 μm. Unpublished data are obtained from the study by BD. Semple.
Neuroprotective and neurotrophic properties of CCL2-mediated signaling
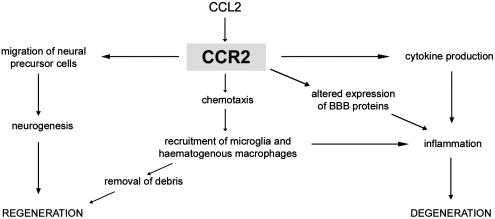
Despite robust experimental evidence indicating that elevated CCL2 and subsequent recruitment of macrophages into the brain is detrimental, awareness of the fact that chemokines also possess pleiotropic and beneficial properties, beyond chemotaxis, is increasing. A potential role in tissue repair has been identified in the context of a skin wound model, with Ccl2−/− mice exhibiting delayed wound reepithelization, angiogenesis, and impaired collagen synthesis compared with wild-type animals (Low et al, 2001). The apparent paradox of CCL2 function indicated by such data may be attributed to the heterogeneity of the macrophage response. After myocardial infarction, e.g., infiltration of Ly-6ChighCCR2+ macrophages dominates early, with cells exhibiting a phagocytic and inflammatory phenotype. Ly-6ClowCCR2− cells that enter the tissue later display attenuated inflammatory properties and may be associated with tissue repair and regeneration (Nahrendorf et al, 2007). Neuroprotective effects associated with a reduction in CCL2-mediated macrophage infiltration after stroke or TBI may relate not only to the overall number of leukocytes present but also to their altered phenotypic state. Furthermore, any attempts to inhibit CCL2 production or to reduce CCR2 expression for therapeutic purposes under pathological conditions should be weighed carefully against its role in health maintenance and repair (Figure 2).
Figure 2.
The roles of CCL2/CCR2 in brain inflammation and injury. CCL2 induces the recruitment of macrophages, production of cytokines, and direct alteration of the expression of endothelial cell tight-junction proteins to increase blood–brain barrier (BBB) permeability, which contributes to inflammation in the brain, potentially exacerbating neuronal loss. CCL2-mediated macrophage accumulation may also be beneficial, as these phagocytic cells remove myelin debris, which otherwise inhibits regeneration. Furthermore, CCL2 is chemotactic for neural precursor cells and thus, may influence repair after injury by enhancing neurogenesis.
In the brain, speculation that CCL2 may be important in neurogenesis has been gaining momentum over the past decade, as recombinant CCL2 was first shown to promote glial cell proliferation and growth in vitro (Rezaie et al, 2002). The ability of CCL2 to induce stem-cell migration into sites of damage in the adult injured brain has since been illustrated using hippocampal brain slices from ligand and receptor knockout mice (Belmadani et al, 2006; Widera et al, 2004). Cultured neural precursor cells migrate in response to CCL2 in vitro, whilst they move toward sites of recombinant CCL2 infused into the brain in vivo (Magge et al, 2009). Most recently, the first evidence that CCL2 may also direct differentiation of precursor cells into neurons, astrocytes, and oligodendrocytes has been published (Chintawar et al, 2009).
To date, the role of CCL2 in adult neurogenesis after brain injury has been investigated most thoroughly in models of stroke. Lui et al (2007) showed that MCAO induced a strong upregulation of CCL2 within the neurogenic subventricular zone. CCL2 reportedly promoted motility of adult neural progenitor cells and enhanced their differentiation into neurons, whereas the neutralization of the chemokine abolished these effects (Lui et al, 2007). Another group has also identified CCL2/CCR2-dependent migration of neuroblasts within the brain to sites of ischemic damage (Yan et al, 2007).
Current strategies for the therapeutic targeting of CCL2/CCR2
Accumulating preclinical data indicate that the CCL2/CCR2 network is a promising target to therapeutically reduce inflammatory cell infiltrates and tissue damage. Thus far, the pharmaceutical industry has primarily focused on the use of CCR2 antagonists, resulting in several compounds entering the early phases of clinical trials for application in peripheral inflammatory conditions, including rheumatoid arthritis (small molecule antagonist INCB3284, Incyte, Wilmington, DE, USA), atherosclerotic cardiovascular disease (neutralizing antibody MLN1202, Millenium Pharmaceuticals, Cambridge, MA, USA), and IgA nephropathy (CCL2-LPM, Osprey Pharmaceuticals, Saint-Laurent, QC, Canada) (Horuk, 2009).
Information on the progress of clinical trials with CCR2 antagonists is scarce, with many companies reporting either no or only slight developments in their research. This lack of progress may reflect the complexity and redundancy of the chemokine network and its interactions, thus our limited understanding of this signaling network in disease (Horuk, 2009). Application of innovative technologies may assist in effectively targeting the CCL2/CCR2 network in neuroinflammation, e.g., with the use of interference RNA to silence specific genes, RNA oligonucleotides, or dominant negative mutants of chemokine ligands to eliminate receptor function.
The question also remains as to whether CCR2 antagonists would be able to effectively cross the BBB for treatment of CNS conditions, such as TBI, MS, or stroke. In the context of TBI, we know that the BBB has increased permeability for a short period of time after injury, which allows the infiltration of serum proteins and circulating leukocytes into the CNS (Habgood et al, 2007). This time course of BBB dysfunction may provide a therapeutic window for the administration of drugs which cannot normally cross the intact BBB.
The neutrophil chemoattractants CXCL1, CXCL2, and CXCL8
Just as CCL2 is considered to be the prototypical monocyte-attracting CC chemokine, CXCL8 (also known as IL-8) is the most intensely studied CXC chemokine, first identified as a powerful mediator able to induce morphologic changes and degranulation of neutrophils (Baggiolini et al, 1989). Since then, evidence for the role of CXCL8 as a key player in neutrophil transmigration has been shown both in vivo (Bell et al, 1996) and in vitro (Huber et al, 1991). Human CXCL8 can bind two receptors: CXCR2, which has been shown to be the most important receptor in chemotaxis, and CXCR1, which is believed to mediate activation of the neutrophil respiratory burst and release of myeloperoxidase (Rose et al, 2004). The CXCR2 receptor is 75% identical in humans and mice; however, no direct homology of the human ligand CXCL8 has been found in rodents to date. In addition, mice lack a corresponding homolog of CXCR1 (Lee et al, 1995).
In rodents, two main ligands perform the same functions as human CXCL8, namely CXCL1 (also known as keratinocyte-derived chemokine, KC) and CXCL2 (macrophage inflammatory protein, MIP-2). These chemokines share 78% sequence homology, and have been recognized as the most critical CXCR2 ligands mediating the neutrophil influx characteristic of inflammatory disorders, including psoriasis, rheumatoid arthritis, atherosclerosis, and irritable bowel disease. Compounding this nomenclature confusion further, CXCL1 and CXCL2 have also been identified in humans as growth-regulated gene-alpha (GROα) and GROβ, respectively.
CXCR2 receptor structure and intracellular signaling in the central nervous system
As is the case for all known chemokine receptors, CXCR2 is a seven transmembrane G-protein-coupled receptor. Chemokines that are able to bind CXCR2 and mediate neutrophil chemotaxis contain the glutamic acid–leucine–arginine (ELR) tripeptide motif in their N-terminal domain, as opposed to non-ELR CXC chemokines (such as CXCL12), which lack this motif and generally attract lymphocytes. Upon ligand binding, CXCR2 activates G-protein-mediated phosphoinositide hydrolysis to generate diacylglycerol and inositol 1,4,5-trisphosphate, which then activate protein kinase C allowing the mobilization of calcium to initiate cellular responses (Wu et al, 1993). The ligand–receptor complex is phosphorylated and endocytosed after signaling through clathrin-dependent pathways, and once internalized, CXCR2 may be either degraded or transported back to the cell membrane for reexpression (Rose et al, 2004). Receptor endocytosis is believed to be essential for the regulation of chemotactic migration, although the evidence for this is still controversial (Rose et al, 2004; Yang et al, 1999). A recent study using receptor knockout mice has elegantly shown that functional CXCR2 is essential for the removal and thus, for the regulation of chemokines in the circulation and brain, identifying a novel scavenging role of these receptors in chemokine homeostasis (Cardona et al, 2008).
Cxcr2−/− mice generated by homologous recombination have been widely used to show the crucial role of CXCR2 in neutrophil recruitment (Cacalano et al, 1994). Despite increased circulating neutrophils, the number of neutrophils recruited in Cxcr2−/− mice in response to peritoneum thioglycollate injections was one-fifth that of wild-type mice (Cacalano et al, 1994; Luan et al, 2001). Neither human CXCL8 nor murine CXCL1 or CXCL2 can induce neutrophil accumulation in Cxcr2−/− mice, confirming that CXCR2 is the primary receptor for these ligands. However, it is worth noting that neutrophils from Cxcr2−/− mice can still respond to other chemotactic molecules, such as leukotriene B4, a lipid mediator which acts through a different receptor, indicating normal neutrophil locomotor activity (Mihara et al, 2005).
The CXCL8/CXCR2 network in the central nervous system
As with the CCL2/CCR2 network, ligands of the CXCR2 receptor appear to be expressed at low basal levels in the brain and upregulated in pathology. Reported sources of CXCL1, CXCL2, and CXCL8 include activated microglia, astrocytes, and endothelial cells; in addition, infiltrated neutrophils themselves are a major source of CXC chemokines, potentially amplifying leukocyte recruitment (Lu et al, 2005; Valles et al, 2006).
Peripherally, the receptor CXCR2 is most highly and uniformly expressed by neutrophils, although it has also been shown on eosinophils, mast cells, and on a small subset of effector T cells (Lippert et al, 2004). In the CNS, widespread neuronal CXCR2 has been detected by immunohistochemistry and in situ hybridization within several regions of the brain and spinal cord of nondiseased autopsied human tissue (Horuk et al, 1997). In the normal rat CNS, CXCR2 immunoreactivity has been reported within neurons of the cortex and striatum, as well as in several thalamic, hypothalamic, mesencephalic, and pontine nuclei (Luan et al, 2001; Valles et al, 2006). In contrast, astrocytes and microglia seem to express the CXCR2 receptor only once activated, e.g., in vitro by proinflammatory cytokines such as IL-1β and TNFα, or in vivo after TBI or demyelination (Aloisi et al, 1992; Lindner et al, 2008; Otto et al, 2000; Saas et al, 2002). As with the CCR2 receptor and several other transmembrane receptors, the lack of specificity of commercially available antibodies continues to confound a clear understanding of expression localization (Semple et al, unpublished observations).
The CXCL8/CXCR2 network in brain development and neurotransmission
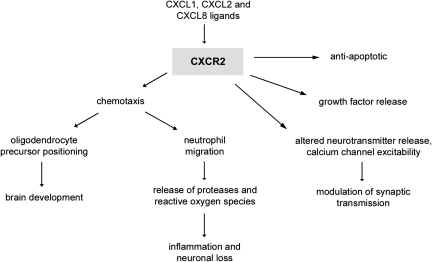
Recent data substantiating the involvement of CXCR2 signaling in neuronal electrical activity, neurotransmitter release, and synaptic plasticity in the CNS have contributed to the emerging concept of the ‘chemokinergic' system as a new class of neurotransmitters (Parsadaniantz and Rostene, 2008). Giovannelli et al (1998) found that Purkinje neurons in mouse cerebellar slices respond to CXCL8 and CXCL1 treatment with a transient increase in calcium, neurotransmitter release, and impaired long-term depression. A separate study showed that CXCR2, when coexpressed on cerebellar Purkinje neurons with the Glut1 subunit of AMPA (α-amino-3-hydroxyl-5-methyl-4-isoxazole-propionate) receptors, can alter the functional profile of these ion channel receptors by increasing channel opening frequency and thus, enhancing glutaminergic activity (Lax et al, 2002). The ability of CXCL8 to modulate calcium channel excitability through CXCR2 on rat septal neurons has also been shown (Puma et al, 2001). These findings corroborate a function for CXCR2 signaling beyond neutrophil chemoattraction, which is supported by widespread constitutive CXCR2 expression throughout the adult brain.
A role for this chemokine system in brain maturation has also been suggested, as the expression of both CXCL2 and CXCR2 is widely distributed during early developmental stages in the mouse forebrain, hippocampus, thalamus, and floor plate (Luan et al, 2001). Considering the chemotactic properties attributed to this chemokine family, it is conceivable that signaling through CXCR2 may contribute to the trafficking of neuronal processes to form appropriate synapses during brain development.
Furthermore, constitutive expression of CXCR2 by human oligodendrocytes has been shown both in vitro and in vivo (Omari et al, 2006). CXCR2-mediated signaling is reportedly crucial for oligodendrocyte development, as Cxcr2−/− mice exhibit reduced oligodendrocyte precursors which are abnormally localized within the spinal cord, in conjunction with altered myelination distribution (Padovani-Claudio et al, 2006). By signaling through CXCR2, the ligand CXCL1 was shown to inhibit precursor cell migration, thus negatively regulating this developmental process (Tsai et al, 2002).
The CXCR2 network in brain pathologies
Multiple Sclerosis
The CXCL1/CXCR2 system seems to be involved in the pathology of MS. First, elevated CXCL8 was detected in the CSF of MS patients compared with controls, a phenomenon which is attenuated in patients receiving interferonβ-1a therapy (Lund et al, 2004). Expression of CXCR2 has been described in normal and proliferating oligodendrocytes within active MS lesions (Omari et al, 2006), as well as on activated microglia bordering the lesion (Filipovic et al, 2003). Proximal reactive astrocytes reportedly secrete the ligand CXCL1, the production of which can also be induced in vitro with the proinflammatory cytokine IL-1β, leading the authors to propose that this chemokine network may be involved in recruiting oligodendrocytes to mediate repair (Omari et al, 2006). A recent study showing that blockage of CXCR2 resulted in BBB compromise and heightened clinical manifestations in EAE mice, supports a role for this chemokine network in tissue repair of this autoimmune disease (Carlson et al, 2008).
Ischemic Brain Injury
A substantial number of studies have shown pronounced neutrophil infiltration in ischemic brain tissue (Emerich et al, 2002). Attenuation of neutrophil transmigration by an anti-CXCL8 antibody resulted in a 60% reduction in infarct volume after transient focal ischemia in rabbits (Matsumoto et al, 1997). The chemokine-mediated infiltration of neutrophils appears to contribute to reperfusion injury rather than to the formation of the initial infarct, as blockage of CXCR2 signaling by the noncompetitive allosteric inhibitor reparixin, was able to significantly reduce tissue damage after transient, but not permanent, MCAO in rats (Garau et al, 2005). Although reparixin binds with higher affinity to CXCR1 than to CXCR2, this compound has been shown to reduce neutrophil infiltration by 40–50%, reduce infarct volume, inhibit long-term inflammation, and improve recovery of sensorimotor function after experimental stroke (Garau et al, 2005; Villa et al, 2007). Another compound which was generated as a dual inhibitor of CXCR1 and CXCR2, DF2156A, showed similar neuroprotective effects (Garau et al, 2006).
Interestingly, several studies have detected the elevation of CXCL1 and CXCL8 in the periphery after ischemic brain injury, indicating the occurrence of systemic inflammatory events resulting from damage to the CNS. Circulating levels of CXCL8 were reportedly elevated in patients after stroke (Kostulas et al, 1998). CXCL1 was found to be increased in the plasma, liver, and lungs of mice after experimental MCAO at times preceding the peak of chemokine expression in the injured cortex and striatum (Chapman et al, 2009). These data illustrate the fact that chemokine expression in the body is both spatial and temporal, indicating that local production of chemokines within the brain parenchyma may be only one of the mechanisms contributing to the chemotactic gradients which regulate leukocyte migration.
Traumatic Brain Injury
In the clinic, we along with others have reported that CXCL8 elevated in the CSF of patients after severe TBI in both adults and children correlated with severe BBB dysfunction (Kossmann et al, 1997) and increased mortality (Whalen et al, 2000), suggesting that measurement of CSF CXCL8 may be an indicator of poor prognosis. Levels of CXCL8 were significantly higher in the CSF than in the serum, supporting intrathecal production as the prominent source. Our laboratory has previously shown that the adhesion molecule sICAM-1, the concentration of which in the CSF of TBI patients correlated with the severity of BBB breakdown (Pleines et al, 1998), is able to induce CXCL2 production in cultured mouse astrocytes and brain microvascular endothelial cells (Otto et al, 2002).
A prominent influx of neutrophils into the damaged brain parenchyma within the early hours after experimental TBI has been repeatedly shown by our group (Bye et al, 2007; Stahel et al, 2000). However, little work has been carried out to investigate the mechanisms underlying the contribution of CXCR2-mediated signaling to secondary tissue damage after TBI. We have previously shown that CXCL2 and CXCR2 are acutely increased in the ipsilateral hemisphere after closed head injury in mice, peaking between 4 and 8 h after injury (Otto et al, 2001). In a separate study, using a controlled cortical impact model in rats, Valles et al (2006) showed that production of the ligands CXCL1 and CXCL2 was increased as early as 2 h after trauma, remaining elevated for more than 24 h. Levels of the CXCR2 receptor were elevated in the ipsilateral cortex by 8 h after injury (Valles et al, 2006). Another study detected upregulated CXCR2 expression in the contused hemisphere by 4 h after lateral fluid percussion injury in mice (Rhodes et al, 2009). Recently completed work from our laboratory showing reduced accumulation of neutrophils in Cxcr2−/− mice by ∼80%, compared with wild-type controls after closed head injury (Semple et al, manuscript in preparation, Figure 1), emphasizes the essential role of CXCR2 in mediating neutrophil infiltration into the injured brain.
Interestingly, neither CXCL2 elevation nor neutrophil infiltration was observed by our group in a rat model of diffuse traumatic axonal injury (Rancan et al, 2001), suggesting that these key features of focal brain injury are not as relevant for patterns of diffuse brain damage. Clearly, more research into the specific role of CXCR2 in the context of different forms of TBI is warranted.
Neuroprotective and neurotrophic properties of CXCR2-mediated signaling
A robust neutrophilic infiltration is often the first cellular response to acute infection or injury. Rather than contributing to tissue damage, neutrophils in infectious diseases seem to have a vital role in the containment and neutralization of bacteria to minimize tissue degradation. For example, after inoculation with Staphylococcus aureus, mice depleted of neutrophils exhibit more severe brain abscesses and higher bacterial burdens than do controls (Kielian et al, 2001). The involvement of the CXCL8/CXCR2 network was shown by blockage of CXCR2, which increased bacterial load by up to 100-fold in animals with several pulmonary infections, resulting in higher mortality (Khan et al, 2007; Reutershan, 2006).
Independent of their chemotactic properties, additional neuroprotective and neurotrophic functions of the ligands CXCL8, CXCL1, and CXCL2 are emerging (Figure 3). First, it has been shown that CXCR2 signaling is involved in the resistance of astrocytes and neurons to cell death in vitro. CXCL8 released by astrocytes signals in an autocrine manner, binding to CXCR2 expressed on their own cell surface to provide protection against Fas-mediated apoptosis in a self-defense mechanism (Saas et al, 2002). CXCL8 treatment of cerebellar granule neurons enhanced cell survival, an effect which was abolished by the inhibition of phosphatidylinositol-3 kinase signaling (Limatola et al, 2002). In hippocampal neurons, the ligand CXCL2 was shown to protect against amyloid-induced cell death by the activation of mitogen-activated protein kinase and phosphatidylinositol-3 kinase pathways (Watson and Fan, 2005). Conversely, a separate study has shown that CXCL2 can induce dose-dependent neurotoxicity of cultured primary motor neurons, illustrating the fact that consequences of CXCR2 signaling may depend on the ligand, concentration, cell type, and stimulus involved (De Paola et al, 2007).
Figure 3.
The multiple functions mediated by CXCR2 signaling in the CNS. CXCR2 is the main receptor involved in neutrophil chemotaxis, leading to cell migration into the brain during injury, infection or disease. Neutrophils perpetuate the neuroinflammatory response by the release of enzymes such as proteases, contributing to neuronal degeneration. Independent of this role, CXCR2 signaling is involved in chemotaxis of oligodendrocyte precursors during development, the release of growth factors, mediating self-defense mechanisms against Fas-initiated apoptotic cell death, and modulating synaptic transmission through altering calcium channel excitability and neurotransmitter release.
Second, neurotrophic properties have been attributed to ligands signaling through CXCR2 in vitro. One group has shown that CXCL1 treatment of primary mouse cortical neurons stimulated mitogen-activated protein kinase and phosphatidylinositol-3 kinase-mediated growth factor signaling in a more potent manner as compared with known mediators, such as nerve growth factor and fibroblast growth factor (Xia and Hyman, 2002). Our laboratory has previously shown that CXCL8 stimulates nerve growth factor production by cultured astrocytes, when applied either as a recombinant peptide or as an endogenous chemokine collected from human CSF after TBI (Kossmann et al, 1997).
Both CXCL2 and CXCL8 have also been shown to be neurotrophic for cerebellar granule neurons, as treatment with these chemokines in vitro prevented potassium-depletion-induced cell death, an effect which appeared to be mediated by an association with AMPA-type ionotrophic glutamate receptors (Limatola et al, 2000). Furthermore, exposure to CXCL8 increased the survival of cultured hippocampal neurons, likely by enhancing the proliferation of cocultured glial cells (Araujo and Cotman, 1993). Further investigation is required to examine whether these chemokines actually function in vivo as growth factors, with a potential impact in health or disease states.
Current strategies for the therapeutic targeting of CXCR2
Previous attempts to reduce neutrophil infiltration by the administration of neutralizing antibodies to individual chemokines have produced mixed results. This variability may depend on the model, the chemokine, and the organ being targeted. Experimentally, neutralizing antibodies against the receptor CXCR2 almost completely inhibited neutrophil infiltration in an intraperitoneal inflammation murine model, whereas blocking either CXCL1 or CXCL2 ligands alone produced only a partial attenuation (Tanimoto et al, 2007). Such studies emphasize the advantage of blocking receptors to combat the considerable redundancy within chemokine networks, as neutralization of an individual chemokine may be compensated by another chemokine binding the same receptor. Any issues caused by currently unknown differences between human CXCL8 and its murine homolog ligands may also be avoided by targeting the joint receptor, CXCR2.
The alternative approach to study the role of CXCR2 is by modeling inflammatory diseases in mice overexpressing or genetically deficient for the specific gene. It is important to remember that, although they are invaluable for defining the roles of particular molecules in vivo, there are numerous drawbacks when using gene knockout and transgenic animal models. For example, although the Cxcr2−/− phenotype is viable, these mice respond poorly to environmental stress, reproduce at low rates, and have smaller body weights. Upon autopsy of adult mice, abnormalities including splenomegaly, lymph node enlargement, and increased white bone marrow have been observed (Cacalano et al, 1994). A marked increase in total blood neutrophil counts and a considerable increase in myelopoiesis in Cxcr2−/− mice suggests that this chemokine network has a vital role in inhibiting the differentiation of immune cells and in maintaining a healthy balance of all blood cell types (Broxmeyer et al, 1996; Coughlan et al, 2000; Luan et al, 2001).
Although these abnormalities provide important information on the role of CXCR2 in development and physiology, they can interfere with experimental studies investigating the role of this chemokine network in disease paradigms. Abnormalities present in knockout mice provide clues as to the possible side effects that may result from CXCR2 antagonism, indicating that patients who receive CXCR2-targeted therapeutics should be monitored carefully during clinical trials.
Conclusions
Chemokines are multifunctional mediators in the brain, both in health and pathology. The best characterized chemokine–receptor networks involving CCL2/CCR2 and CXCL8/CXCR2 have nonredundant functions not only in regulating immune cell infiltration into the CNS during neuropathology but also in physiologic processes, including neurogenesis, neuroprotection, and neurotransmission. The use of gene knockout and transgenic mice has been invaluable to increase our understanding of the different mechanisms regulated by chemokines. For conditions in which neuroinflammation is a key pathologic event such as MS, stroke, and TBI, therapeutic targeting of chemokine networks to reduce the inflammatory infiltrate and its consequences may have considerable potential benefit. Ultimately, targeting chemokines in heterogeneous conditions such as TBI with the aim of improving patient outcomes will most likely require the admission of multiple drug agents targeting several deleterious pathways, such as excitotoxicity and oxidative stress, all of which contribute to downstream neuronal degeneration and subsequent neurologic impairment.
Footnotes
Disclosure/conflict of interest
The authors declare no conflict of interest.
References
- Aloisi F, Care A, Borsellino G, Gallo P, Rosa S, Bassani A, Cabibbo A, Testa U, Levi G, Peschle C. Production of haemolymphopoietic cytokines (IL-6, IL-8 and colony-stimulating factors) by normal human astrocytes in response to IL-1β and tumor necrosis factor-α. J Immunol. 1992;149:2358–2366. [PubMed] [Google Scholar]
- Andjelkovic AV, Song L, Dzenko KA, Cong H, Pachter JS. Functional expression of CCR2 by human fetal astrocytes. J Neurosci Res. 2002;70:219–231. doi: 10.1002/jnr.10372. [DOI] [PubMed] [Google Scholar]
- Arakelyan A, Petrkova J, Hermanova Z, Boyajyan A, Lukl J, Petrek M. Serum levels of the MCP-1 chemokine in patients with ischemic stroke and myocardial infarction. Mediators Inflamm. 2005;3:175–179. doi: 10.1155/MI.2005.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo DM, Cotman CW. Trophic effects of interleukin-4, -7 and -8 on hippocampal neuronal cultures: potential involvement of glial-derived factors. Brain Res. 1993;600:49–55. doi: 10.1016/0006-8993(93)90400-h. [DOI] [PubMed] [Google Scholar]
- Babcock AA, Kuziel WA, Rivest S, Owens T. Chemokine expression by glial cells directs leukocytes to sites of axonal injury in the CNS. J Neurosci. 2003;23:7922–7930. doi: 10.1523/JNEUROSCI.23-21-07922.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggiolini M, Walz A, Kunkel SL. Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J Clin Invest. 1989;84:1045–1049. doi: 10.1172/JCI114265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banisadr G, Gosselin R-D, Mechighel P, Rostene W, Kitabgi P, Parsadaniantz SM. Constitutive neuronal expression of CCR2 chemokine receptor and its colocalisation with neurotransmitters in normal rat brain: functional effect of MCP-1/CCL2 on calcium mobilisation in primary cultured neurons. J Comp Neurol. 2005;492:178–192. doi: 10.1002/cne.20729. [DOI] [PubMed] [Google Scholar]
- Banisadr G, Queraud-Lesaux F, Boutterin MC, Pelaprat D, Zalc B, Rostene W, Haour F, Parsadaniantz SM. Distribution, cellular localisation and functional role of CCR2 chemokine receptors in adult rat brain. J Neurochem. 2002;81:257–269. doi: 10.1046/j.1471-4159.2002.00809.x. [DOI] [PubMed] [Google Scholar]
- Barna BP, Pettay J, Barnett GH, Zhou P, Iwasaki K, Estes ML. Regulation of monocyte chemoattractant protein-1 expression in adult human non-neoplastic astrocytes is sensitive to tumor necrosis factor (TNF) or antibody to the 55-kDa TNF receptor. J Neuroimmunol. 1994;50:101–107. doi: 10.1016/0165-5728(94)90220-8. [DOI] [PubMed] [Google Scholar]
- Bell MD, Taub DD, Perry VH. Overriding the brain's intrinsic resistance to leukocyte recruitment with intraparenchymal injections of recombinant chemokines. Neuroscience. 1996;74:283–292. doi: 10.1016/0306-4522(96)00083-8. [DOI] [PubMed] [Google Scholar]
- Belmadani A, Tran PB, Ren D, Miller RJ. Chemokines regulate the migration of neural progenitors to sites of neuroinflammation. J Neurosci. 2006;26:3182–3191. doi: 10.1523/JNEUROSCI.0156-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman JW, Guida MP, Warren J, Amat J, Brosnan CF. Localisation of monocyte chemoattractant peptide-1 expression in the central nervous system in experimental autoimmune encephalomyelitis and trauma in the rat. J Immunol. 1996;156:3017–3023. [PubMed] [Google Scholar]
- Broxmeyer HE, Cooper S, Cacalano G, Hague NL, Bailish E, Moore MW. Involvement of interleukin (IL) 8 receptor in negative regulation of myeloid progenitor cells in vivo: evidence from mice lacking the murine IL-8 receptor homologue. J Exp Med. 1996;184:1825–1832. doi: 10.1084/jem.184.5.1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bye N, Habgood MD, Callaway JK, Malakooti N, Potter A, Kossmann T, Morganti-Kossmann MC. Transient neuroprotection by minocycline following traumatic brain injury is associated with attenuated microglial activation but no changes in cell apoptosis or neutrophil infiltration. Exp Neurol. 2007;204:220–233. doi: 10.1016/j.expneurol.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Cacalano G, Lee J, Kikly K, Ryan AM, Pitts-Meek S, Hultgren B, Wood WI, Moore MW. Neutrophil and B cell expansion in mice that lack the murine IL-8 receptor homolog. Science. 1994;265:682–684. doi: 10.1126/science.8036519. [DOI] [PubMed] [Google Scholar]
- Cardona AE, Sasse ME, Mizutani M, Cardona SM, Liu L, Savarin C, Hu T, Ransohoff RM. Scavenging roles of chemokine receptors: chemokine receptor deficiency is associated with increased levels of ligand in circulation and tissues. Blood. 2008;112:256–263. doi: 10.1182/blood-2007-10-118497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson T, Kroenke M, Rao P, Lane TE, Segal B. The Th17-ELR+ CXC chemokine pathway is essential for the development of central nervous system autoimmune disease. J Exp Med. 2008;205:811–823. doi: 10.1084/jem.20072404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman KZ, Dale VQ, Denes A, Bennett G, Rothwell NJ, Allan SM, McColl BW. A rapid and transient peripheral inflammatory response precedes brain inflammation after experimental stroke. J Cereb Blood Flow Metab. 2009;29:1764–8. doi: 10.1038/jcbfm.2009.113. [DOI] [PubMed] [Google Scholar]
- Che X, Ye W, Panga L, Wu DC, Yang GY. Monocyte chemoattractant protein-1 expressed in neurons and astrocytes during focal ischemia in mice. Brain Res. 2001;902:171–177. doi: 10.1016/s0006-8993(01)02328-9. [DOI] [PubMed] [Google Scholar]
- Chen Y, Hallenbeck JM, Ruetzler C, Bol D, Thomas K, Berman NEJ, Vogel SN. Overexpression of monocyte chemoattractant protein-1 in the brain exacerbates ischemic brain injury and is associated with recruitment of inflammatory cells. J Cereb Blood Flow Metab. 2003;23:748–755. doi: 10.1097/01.WCB.0000071885.63724.20. [DOI] [PubMed] [Google Scholar]
- Chintawar S, Cayrol R, Antel J, Pandolfo M, Prat A. Blood-brain barrier promotes differentiation of human fetal neural precursor cells. Stem Cells. 2009;27:838–846. doi: 10.1002/stem.25. [DOI] [PubMed] [Google Scholar]
- Clavo C-F, Yoshimura T, Gelman M, Michel M. Production of monocyte chemotactic protein-1 by rat brain macrophages. Eur J Neurosci. 1996;8:1725–1734. doi: 10.1111/j.1460-9568.1996.tb01316.x. [DOI] [PubMed] [Google Scholar]
- Coughlan C, McManus C, Sharron M, Gao Z, Murphy D, Jaffer S, Choe W, Chen W, Hesselgesser J, Gaylord H, Kalyuzhny A, Lee VM, Wolf B, Doms RW, Kolson DL. Expression of multiple functional chemokine receptors and monocyte chemoattractant protein-1 in human neurons. Neuroscience. 2000;97:591–600. doi: 10.1016/s0306-4522(00)00024-5. [DOI] [PubMed] [Google Scholar]
- Croitoru-Lamoury J, Guillemin GJ, Boussin FD, Mognetti B, Gigout LI, Cheret A, Vaslin B, Le Grand R, Brew BJ, Dormont D. Expression of chemokines and their receptors in human and simian astrocytes: evidence for a central role of TNFα and IFNγ in CXCR4 and CCR2 modulation. Glia. 2003;41:354–370. doi: 10.1002/glia.10181. [DOI] [PubMed] [Google Scholar]
- De Paola M, Buanne P, Biordi L, Bertini R, Ghezzi P, Mennini T. Chemokine MIP-2/CXCL2, acting on CXCR2, induces motor neuron death in primary cultures. Neuroimmunomodulation. 2007;14:310–316. doi: 10.1159/000123834. [DOI] [PubMed] [Google Scholar]
- Dimitrijevic OB, Stamatovic SM, Keep RF, Andjelkovic AV. Effects of the chemokine CCL2 on blood-brain barrier permeability during ischemia-reperfusion injury. J Cereb Blood Flow Metab. 2006;26:797–810. doi: 10.1038/sj.jcbfm.9600229. [DOI] [PubMed] [Google Scholar]
- Dzenko KA, Andjelkovic AV, Kuziel WA, Pachter JS. The chemokine receptor CCR2 mediates the binding and internalisation of monocyte chemoattractant protein-1 along brain microvessels. J Neurosci. 2001;21:9214–9223. doi: 10.1523/JNEUROSCI.21-23-09214.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzenko KA, Song L, Ge S, Kuziel WA, Pachter JS. CCR2 expression by brain microvascular endothelial cells is critical for macrophage transendothelial migration in response to CCL2. Microvasc Res. 2005;70:53–64. doi: 10.1016/j.mvr.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Edman LC, Mira H, Arenas E. The beta-chemokines CCL2 and CCL7 are two novel differentiation factors for midbrain dopaminergic precursors and neurons. Exp Cell Res. 2008;314:2123–2130. doi: 10.1016/j.yexcr.2008.02.019. [DOI] [PubMed] [Google Scholar]
- Emerich DF, Dean RLr, Bartus RT. The role of leukocytes following cerebral ischemia: pathogenic variable or bystander reaction to emerging infarct. Exp Neurol. 2002;173:168–181. doi: 10.1006/exnr.2001.7835. [DOI] [PubMed] [Google Scholar]
- Fife BT, Huffnagle GB, Kuziel WA, Karpus WJ. CC chemokine receptor 2 is critical for induction of experimental autoimmune encephalomyelitis. J Exp Med. 2000;192:805–899. doi: 10.1084/jem.192.6.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipovic R, Jakovcevski I, Zecevic N. GRO-alpha and CXCR2 in the human fetal brain and multiple sclerosis lesions. Dev Neurosci. 2003;25:279–290. doi: 10.1159/000072275. [DOI] [PubMed] [Google Scholar]
- Flugel A, Hager G, Horvat A, Spitzer C, Singer GMA, Graeber MB, Kreutzberg GW, Schwaiger F-W. Neuronal MCP-1 expression in response to remote nerve injury. J Cereb Blood Flow Metab. 2001;21:69–76. doi: 10.1097/00004647-200101000-00009. [DOI] [PubMed] [Google Scholar]
- Franciotta D, Martino G, Zardini E, Furlan R, Bergamaschi R, Andreoni L, Cosi V. Serum and CSF levels of MCP-1 and IP-10 in multiple sclerosis patients with acute and stable disease and undergoing immunomodulatory therapies. J Neuroimmunol. 2001;115:192–198. doi: 10.1016/s0165-5728(01)00261-2. [DOI] [PubMed] [Google Scholar]
- Fuentes ME, Durham SK, Swedel MR, Lewin AC, Barton DS, Megill JR, Bravo R, Lira SA. Controlled recruitment of monocytes and macrophages to specific organs through transgenic expression of monocyte chemoattractant protein-1. J Immunol. 1995;155:5769–5776. [PubMed] [Google Scholar]
- Garau A, Bertini R, Colotta F, Casilli F, Bigini P, Cagnotto A, Mennini T, Ghezzi P, Villa P. Neuroprotection with the CXCL8 inhibitor repertaxin in transient brain ischemia. Cytokine. 2005;30:125–131. doi: 10.1016/j.cyto.2004.12.014. [DOI] [PubMed] [Google Scholar]
- Garau A, Bertini R, Mosca M, Bizzarri C, Anacardio R, Triulzi S, Allegretti M, Ghezzi P, Villa P. Development of a systemically-active dual CXCR1/CXCR2 allosteric inhibitor and its efficacy in a model of transient cerebral ischemia in the rat. Eur Cytokine Netw. 2006;17:35–41. [PubMed] [Google Scholar]
- Ge S, Pachter JS. Caveolin-1 knockdown by small interfering RNA suppresses responses to the chemokine monocyte chemoattractant protein-1 by human astrocytes. J Biol Chem. 2004;279:6688–6695. doi: 10.1074/jbc.M311769200. [DOI] [PubMed] [Google Scholar]
- Geissmann F, Jung S, Littman DR. Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity. 2003;19:71–82. doi: 10.1016/s1074-7613(03)00174-2. [DOI] [PubMed] [Google Scholar]
- Giovannelli A, Limatola C, Ragozzino D, Mileo AM, Ruggieri A, Ciotti MT, Mercanti D, Santoni A, Eusebi F. CXC chemokines interleukin-8 (IL-8) and growth-related gene product α (GROα) modulate Purkinje neuron activity in mouse cerebellum. J Neuroimmunol. 1998;92:122–132. doi: 10.1016/s0165-5728(98)00192-1. [DOI] [PubMed] [Google Scholar]
- Glabinski AR, Balasingam V, Tani M, Kunkel SL, Strieter RM, Wee Yong V, Ransohoff RM. Chemokine monocyte chemoattractant protein-1 is expressed by astrocytes after mechanical injury to the brain. J Immunol. 1996;156:4363–4368. [PubMed] [Google Scholar]
- Glabinski AR, Tani M, Tuohy VK, Tuthill RJ, Ransohoff RM. Central nervous system chemokine mRNA accumulation follows initial leukocyte entry at the onset of acute murine experimental autoimmune encephalomyelitis. Brain Behav Immun. 1995;9:315–330. doi: 10.1006/brbi.1995.1030. [DOI] [PubMed] [Google Scholar]
- Göser S, Ottl R, Brodner A, Dengler TJ, Torzewski J, Egashira K, Rose NR, Katus HA, Kaya Z. Critical role for monocyte chemoattractant protein-1 and macrophage inflammatory protein-1alpha in induction of experimental autoimmune myocarditis and effective anti-monocyte chemoattractant protein-1 gene therapy. Circulation. 2005;112:3400–3407. doi: 10.1161/CIRCULATIONAHA.105.572396. [DOI] [PubMed] [Google Scholar]
- Gourmala NG, Buttini M, Limonta S, Sauter A, Boddeke HW. Differential and time-dependent expression of monocyte chemoattractant protein-1 mRNA by astrocytes and macrophages in rat brain: effects of ischemia and peripheral lipopolysaccharide administration. J Neuroimmunol. 1997;74:35–44. doi: 10.1016/s0165-5728(96)00203-2. [DOI] [PubMed] [Google Scholar]
- Gouwy M, Struyf S, Catusse J, Proost P, Van Damme J. Synergy between proinflammatory ligands of G protein-coupled receptors in neutrophil activation and migration. J Leukoc Biol. 2004;76:185–194. doi: 10.1189/jlb.1003479. [DOI] [PubMed] [Google Scholar]
- Grzybicki D, Moore SA, Schelper R, Glabinski AR, Ransohoff RM, Murphy S. Expression of monocyte chemoattractant protein (MCP-1) and nitric oxide synthase-2 following cerebral trauma. Acta Neuropathol. 1998;95:98–103. doi: 10.1007/s004010050770. [DOI] [PubMed] [Google Scholar]
- Gunn MD, Nelken NA, Liao X, Williams LT. Monocyte chemoattractant protein-1 is sufficient for the chemotaxis of monocytes and lymphocytes in transgenic mice but requires an additional stimulus for inflammatory activation. J Immunol. 1997;158:376–383. [PubMed] [Google Scholar]
- Guyon A, Skrzydelski D, De Giry I, Rovere C, Conductier G, Trocello JM, Dauge V, Kitabgi P, Rostene W, Nahon JL, Melik-Parsadaniantz S. Long term exposure to the chemokine CCL2 activates the nigrostriatal dopamine system: a novel mechanism for the control of dopamine release. Neuroscience. 2009;162:1072–80. doi: 10.1016/j.neuroscience.2009.05.048. [DOI] [PubMed] [Google Scholar]
- Habgood MD, Bye N, Dziegielewska KM, Ek CJ, Lane MA, Potter A, Morganti-Kossmann C, Saunders NR. Changes in blood-brain barrier permeability to large and small molecules following traumatic brain injury in mice. Eur J Neurosci. 2007;25:231–238. doi: 10.1111/j.1460-9568.2006.05275.x. [DOI] [PubMed] [Google Scholar]
- Hanisch UK. Microglia as a source and target of cytokines. Glia. 2002;40:140–155. doi: 10.1002/glia.10161. [DOI] [PubMed] [Google Scholar]
- Harkness KA, Sussman JD, Davies-Jones GAB, Greenwood J, Woodroofe MN. Cytokine regulation of MCP-1 expression in brain and retinal microvascular endothelial cells. J Neuroimmunol. 2003;142:1–9. doi: 10.1016/s0165-5728(03)00251-0. [DOI] [PubMed] [Google Scholar]
- Hausmann EHS, Berman NEJ, Wang Y-Y, Meara JB, Wood GW, Klein RM. Selective chemokine mRNA expression following brain injury. Brain Res. 1998;788:49–59. doi: 10.1016/s0006-8993(97)01160-8. [DOI] [PubMed] [Google Scholar]
- Horuk R. Chemokine receptor antagonists: overcoming developmental hurdles. Nat Rev Drug Discov. 2009;8:23–33. doi: 10.1038/nrd2734. [DOI] [PubMed] [Google Scholar]
- Horuk R, Martin AW, Wang Z, Schweitzer L, Gerassimides A, Guo H, Lu Z, Hesselgesser J, Perez HD, Kim J, Parker J, Hadley TJ, Peiper SC. Expression of chemokine receptors by subsets of neurons in the central nervous system. J Immunol. 1997;158:2882–2890. [PubMed] [Google Scholar]
- Huang D, Han Y, Sandhya Rani MR, Glabinski AR, Trebst C, Sorensen T, Tani M, Wang J, Chien P, O'Bryan S, Bielecki B, Zhou ZL, Majumder S, Ransohoff RM. Chemokines and chemokine receptors in inflammation of the nervous system: manifold roles and exquisite regulation. Immunol Rev. 2000;177:52–67. doi: 10.1034/j.1600-065x.2000.17709.x. [DOI] [PubMed] [Google Scholar]
- Huang DR, Wang J, Kivisakk P, Rollins BJ, Ransohoff RM. Absence of monocyte chemoattractant protein-1 in mice leads to decreased local macrophage recruitment and antigen-specific T helper cell type 1 immune response in experimental autoimmune encephalomyelitis. J Exp Med. 2001;193:713–726. doi: 10.1084/jem.193.6.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber AR, Kunkel SL, Todd RF, Weiss SJ. Regulation of transendothelial neutrophil migration by endogenous interleukin-8. Science. 1991;254:99–102. doi: 10.1126/science.1718038. [DOI] [PubMed] [Google Scholar]
- Hughes PM, Allegrini PR, Rudin M, Perry HV, Mir AK, Weissner C. Monocyte chemoattractant protein-1 deficiency is protective in a murine stroke model. J Cereb Blood Flow Metab. 2002;22:308–317. doi: 10.1097/00004647-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Hurwitz AA, Lyman WD, Berman JW. Tumor necrosis factor alpha and transforming growth factor beta upregulate astrocyte expression of monocyte chemoattractant protein-1. J Immunol. 1995;57:193–198. doi: 10.1016/0165-5728(95)00011-p. [DOI] [PubMed] [Google Scholar]
- Kennedy KJ, Strieter RM, Kunkel SL, Lukacs NW, Karpus WJ. Acute and relapsing experimental autoimmune encephalomyelitis are regulated by differential expression of the CC chemokines macrophage inflammatory protein-1alpha and monocyte chemotactic protein-1. J Neuroimmunol. 1998;92:98–108. doi: 10.1016/s0165-5728(98)00187-8. [DOI] [PubMed] [Google Scholar]
- Khan S, Cole N, Hume EB, Garthwaite L, Conibear TCR, Miles DH, Aliwaga Y, Krockenberger MB, Willcox MDP. The role of CXC chemokine receptor 2 in Pseudomonas aeruginosa corneal infection. J Leukoc Biol. 2007;81:315–318. doi: 10.1189/jlb.0506344. [DOI] [PubMed] [Google Scholar]
- Kielian T, Barry B, Hickey WF. CXC chemokine receptor-2 ligands are required for neutrophil-mediated host defense in experimental brain abscesses. J Immunol. 2001;166:4634–4643. doi: 10.4049/jimmunol.166.7.4634. [DOI] [PubMed] [Google Scholar]
- Kossmann T, Stahel PF, Lenzlinger PM, Redl H, Dubs RW, Trentz O, Schlag G, Morganti-Kossmann MC. Interleukin-8 released into the cerebrospinal fluid after brain injury is associated with blood-brain barrier dysfunction and nerve growth factor production. J Cereb Blood Flow Metab. 1997;17:280–289. doi: 10.1097/00004647-199703000-00005. [DOI] [PubMed] [Google Scholar]
- Kostulas N, Kivisäkk P, Huang Y, Matusevicius D, Kostulas V, Link H. Ischemic stroke is associated with a systemic increase of blood mononuclear cells expressing interleukin-8 mRNA. Stroke. 1998;29:462–466. doi: 10.1161/01.str.29.2.462. [DOI] [PubMed] [Google Scholar]
- Kumai Y, Ooboshi H, Takada J, Kamouchi M, Kitazono T, Egashira K, Ibayashi S, Iida M. Anti-Monocyte Chemoattractant Protein-1 gene therapy protects against focal brain ischemia in hypertensive rats. J Cereb Blood Flow Metab. 2004;24:1359–1368. doi: 10.1097/01.WCB.0000143534.76388.3C. [DOI] [PubMed] [Google Scholar]
- Kurihara T, Warr G, Loy J, Bravo R. Defects in macrophage recruitment and host defence in mice lacking the CCR2 chemokine receptor. J Exp Med. 1997;186:1757–1762. doi: 10.1084/jem.186.10.1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuziel WA, Morgan SJ, Dawson TC, Griffin S, Smithies O, Ley K, Maeda N. Severe reduction in leukocyte adhesion and monocyte extravasation in mice deficient in CC chemokine receptor 2. Proc Natl Acad Sci USA. 1997;94:12053–12058. doi: 10.1073/pnas.94.22.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lax P, Limatola C, Fucile S, Trettel F, Di Bartolomeo S, Renzi M, Ragozzino D, Eusebi F. Chemokine receptor CXCR2 regulates the functional properties of AMPA-type glutamate receptor GluR1 in HEK cells. J Neuroimmunol. 2002;129:66–73. doi: 10.1016/s0165-5728(02)00178-9. [DOI] [PubMed] [Google Scholar]
- Lee J, Cacalano G, Camerato T, Toy K, Moore MW, Wood WI. Chemokine binding and activities mediated by the mouse IL-8 receptor. J Immunol. 1995;155:2158–2164. [PubMed] [Google Scholar]
- Limatola C, Ciotti MT, Mercanti D, Santoni A, Eusebi F. Signaling pathways activated by chemokine receptor CXCR2 and AMPA-type glutamate receptors and involvement in granule cells survival. J Neuroimmunol. 2002;123:9–17. doi: 10.1016/s0165-5728(01)00472-6. [DOI] [PubMed] [Google Scholar]
- Limatola C, Ciotti MT, Mercanti D, Vacca F, Ragozzino D, Giovannelli A, Santoni A, Eusebi F, Miledi R. The chemokine growth-related gene product beta protects rat cerebellar granule cells from apoptotic cell death through alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionate receptors. Proc Natl Acad Sci USA. 2000;97:6197–6201. doi: 10.1073/pnas.090105997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindner M, Trebst C, Heine S, Skripuletz T, Koutsoudaki PN, Stangel M. The chemokine receptor CXCR2 is differentially regulation on glial cells in vivo but is not required for successful remyelination after cuprizone-induced demyelination. Glia. 2008;56:1104–1113. doi: 10.1002/glia.20682. [DOI] [PubMed] [Google Scholar]
- Lippert U, Zachmann K, Henz BM, Neumann C. Human T lymphocytes and mast cells differentially express and regulate extra- and intracellular CXCR1 and CXCR2. Exp Dermatol. 2004;13:520–525. doi: 10.1111/j.0906-6705.2004.00182.x. [DOI] [PubMed] [Google Scholar]
- Losy J, Zaremba J. Monocyte chemoattractant protein-1 is increased in the cerebrospinal fluid of patients with ischemic stroke. Stroke. 2001;32:2695–2696. doi: 10.1161/hs1101.097380. [DOI] [PubMed] [Google Scholar]
- Low QEH, Drugea IA, Duffner LA, Quinn DG, Cook DN, Rollins BJ, Kovacs EJ, DiPietro LA. Wound healing in MIP-1a −/− and MCP-1 −/− mice. Am J Pathol. 2001;159:457–463. doi: 10.1016/s0002-9440(10)61717-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu B, Rutledge BJ, Gu L, Fiorillo J, Lukacs NW, Kunkel SL, North R, Gerald C, Rollins BJ. Abnormalities in monocyte recruitment and cytokine expression in monocyte chemoattractant protein 1-deficient mice. J Exp Med. 1998;187:601–608. doi: 10.1084/jem.187.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Maheshwari A, Misiuta I, Fox SE, Chen N, Zigova T, Christensen RD, Calhoun DA. Neutrophil-specific chemokines are produced by astrocytic cells but not by neuronal cells. Dev Brain Res. 2005;155:127–134. doi: 10.1016/j.devbrainres.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Luan J, Furuta Y, Du J, Richmond A. Developmental expression of two CXC chemokines, MIP-2 and KC, and their receptors. Cytokine. 2001;14:253–263. doi: 10.1006/cyto.2001.0882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lui SX, Zhang ZG, Zhang RL, Gregg SR, Wang L, Yier T, Chopp M. Chemokine ligand 2 (CCL2) induces migration and differentiation of subventricular zone cells after stroke. J Neurosci Res. 2007;85:2120–2125. doi: 10.1002/jnr.21359. [DOI] [PubMed] [Google Scholar]
- Lund BT, Ashikian N, Tan HQ, Chakryan Y, Manoukian K, Groshen S, Gilmore W, Cheema GS, Stohl W, Burnett ME, Ko D, Kachuck NJ, Weiner LP. Increased CXCL8 (IL-8) expression in multiple sclerosis. J Neuroimmunol. 2004;155:161–171. doi: 10.1016/j.jneuroim.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Ma M, Wei T, Boring L, Charo IF, Ransohoff RM, Jakeman LB. Monocyte recruitment and myelin removal are delayed following spinal cord injury in mice with CCR2 chemokine receptor deletion. J Neurosci Res. 2002;68:691–702. doi: 10.1002/jnr.10269. [DOI] [PubMed] [Google Scholar]
- Magge SN, Malik SZ, Royo NC, Chen HI, Yun L, Snyder EY, O'Rourke DM, Watson DJ. Role of monocyte chemoattractant protein-1 (MCP-1/CCL2) in migration of neural progenitor cells toward glial tumors. J Neurosci Res. 2009;87:1547–1555. doi: 10.1002/jnr.21983. [DOI] [PubMed] [Google Scholar]
- Mahad D, Callahan MK, Williams KA, Ubogu EE, Kivisäkk P, Tucky B, Kidd G, Kingsbury GA, Chang A, Fox RJ, Mack M, Sniderman MB, Ravid R, Staugaitis SM, Stins MF, Ransohoff RM. Modulating CCR2 and CCL2 at the blood-brain barrier: relevance for multiple sclerosis pathogenesis. Brain. 2006;129:212–223. doi: 10.1093/brain/awh655. [DOI] [PubMed] [Google Scholar]
- Mahad DJ, Ransohoff RM. The role of MCP-1 (CCL2) and CCR2 in multiple sclerosis and experimental autoimmune encephalomyelitis (EAE) Semin Immunol. 2003;15:23–32. doi: 10.1016/s1044-5323(02)00125-2. [DOI] [PubMed] [Google Scholar]
- Matsumoto T, Ikeda K, Mukaida N, Harada A, Matsumoto Y, Yamashita J, Matsushima K. Prevention of cerebral edema and infarct in cerebral reperfusion injury by an antibody to interleukin-8. Lab Invest. 1997;77:119–125. [PubMed] [Google Scholar]
- McManus C, Berman JW, Brett FM, Staunton H, Farrell M, Brosnan CF. MCP-1, MCP-2 and MCP-3 expression in multiple sclerosis lesions: an immunohistochemical and in situ hybridisation study. J Neuroimmunol. 1998;86:20–29. doi: 10.1016/s0165-5728(98)00002-2. [DOI] [PubMed] [Google Scholar]
- McTigue DM, Tani M, Krivacic K, Chernosky A, Kelner GS, Maciejewski D, Maki R, Ransohoff RM, Stokes BT. Selective chemokine mRNA accumulation in the rat spinal cord after contusion injury. J Neurosci Res. 1998;53:368–376. doi: 10.1002/(SICI)1097-4547(19980801)53:3<368::AID-JNR11>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Melgarejo E, Medina MA, Sanchez-Jimenez F, Urdiales JL. Monocyte chemoattractant protein-1: a key mediator in inflammatory processes. Int J Biochem Cell Biol. 2009;41:998–1001. doi: 10.1016/j.biocel.2008.07.018. [DOI] [PubMed] [Google Scholar]
- Meng SZ, Oka A, Takashima S. Developmental expression of monocyte chemoattractant protein-1 in the human cerebellum and brainstem. Brain Dev. 1999;21:30–35. doi: 10.1016/s0387-7604(98)00065-5. [DOI] [PubMed] [Google Scholar]
- Mihara K, Smit M-J, Krajnc-Franken M, Gossen J, Rooseboom M, Dokter W. Human CXCR2 (hCXCR2) takes over functionalities of its murine homolog in hCXCR2 knockin mice. Eur J Immunol. 2005;35:2573–2582. doi: 10.1002/eji.200526021. [DOI] [PubMed] [Google Scholar]
- Muessel MJ, Berman NEJ, Klein RM. Early and specific expression of monocyte chemoattractant protein-1 in the thalamus induced by cortical injury. Brain Res. 2000;870:211–221. doi: 10.1016/s0006-8993(00)02450-1. [DOI] [PubMed] [Google Scholar]
- Muessel MJ, Klein RM, Wilson AM, Berman NEJ. Ablation of the chemokine monocyte chemoattractant protein-1 delays retrograde neuronal degeneration, attenuates microglial activation, and alters expression of cell death molecules. Mol Brain Res. 2002;103:12–27. doi: 10.1016/s0169-328x(02)00158-4. [DOI] [PubMed] [Google Scholar]
- Nahrendorf M, Swirski FK, Aikawa E, Stangenberg L, Wurdinger T, Figueiredo JL, Libby P, Weissleder R, Pittet MJ. The healing myocardium sequentially mobilizes two monocyte subsets with divergent and complementary functions. J Exp Med. 2007;204:3037–3047. doi: 10.1084/jem.20070885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omari KM, John GR, Lango R, Raine CS. Role of CXCR2 and CXCL1 on glia in multiple sclerosis. Glia. 2006;53:24–31. doi: 10.1002/glia.20246. [DOI] [PubMed] [Google Scholar]
- Otto V, Gloor S, Frentzel S, Gilli U, Ammann E, Hein A, Folkers G, Kossmann T, Morganti-Kossmann M. The production of macrophage inflammatory protein-2 induced by soluble intercellular adhesion molecule-1 in mouse astrocytes is mediated by src tyrosine kinases and p42/44 mitogen-activated protein kinase. J Neurochem. 2002;80:824–834. doi: 10.1046/j.0022-3042.2001.00748.x. [DOI] [PubMed] [Google Scholar]
- Otto V, Heinzel-Pleines U, Gloor S, Trentz O, Kossmann T, Morganti-Kossmann M. sICAM-1 and TNF-α induce MIP-2 with distinct kinetics in astrocytes and brain microvascular endothelial cells. J Neurosci Res. 2000;60:733–742. doi: 10.1002/1097-4547(20000615)60:6<733::AID-JNR5>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Otto VI, Stahel PF, Rancan M, Kariya K, Shohami E, Yatsiv I, Eugster H-P, Kossmann T, Trentz O, Morganti-Kossmann MC. Regulation of chemokines and chemokine receptors after experimental closed head injury. NeuroReport. 2001;12:2059–2064. doi: 10.1097/00001756-200107030-00053. [DOI] [PubMed] [Google Scholar]
- Padovani-Claudio DA, Liu L, Ransohoff RM, Miller RH. Alterations in the oligodendrocyte lineage, myelin and white matter in adult mice lacking the chemokine receptor CXCR2. Glia. 2006;54:471–483. doi: 10.1002/glia.20383. [DOI] [PubMed] [Google Scholar]
- Parsadaniantz SM, Rostene W. Chemokines and neuromodulation. J Neuroimmunol. 2008;198:62–68. doi: 10.1016/j.jneuroim.2008.04.022. [DOI] [PubMed] [Google Scholar]
- Peterson PK, Hu S, Salak-Johnson J, Molitor TW, Chao CC. Differential production of and migratory response to beta chemokines by human microglia and astrocytes. J Infect Dis. 1997;175:478–481. doi: 10.1093/infdis/175.2.478. [DOI] [PubMed] [Google Scholar]
- Pleines UE, Stover JF, Kossmann T, Trentz O, Morganti-Kossmann MC. Soluble ICAM-1 in CSF coincides with the extent of cerebral damage in patients with severe traumatic brain injury. J Neurotrauma. 1998;15:399–409. doi: 10.1089/neu.1998.15.399. [DOI] [PubMed] [Google Scholar]
- Puma C, Danik M, Quirion R, Ramon F, Williams S. The chemokine interleukin-8 acutely reduces Ca2+ currents in identified cholinergic septal neurons expressing CXCR1 and CXCR2 receptor mRNAs. J Neurochem. 2001;78:960–971. doi: 10.1046/j.1471-4159.2001.00469.x. [DOI] [PubMed] [Google Scholar]
- Rancan M, Otto VI, Hans VHJ, Gerlach I, Jork R, Trentz O, Kossmann T, Morganti-Kossmann MC. Upregulation of ICAM-1 and MCP-1 but not of MIP-2 and sensorimotor deficit in response to traumatic axonal injury in rats. J Neurosci Res. 2001;63:438–446. doi: 10.1002/1097-4547(20010301)63:5<438::AID-JNR1039>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Ransohoff RM, Hamilton TA, Tani M, Stoler MH, Shick HE, Major JA, Estes ML, Thomas DM, Tuohy VK. Astrocyte expression of mRNA encoding cytokines IP-10 and JE/MCP-1 in experimental autoimmune encephalomyelitis. Faseb J. 1993;7:592–600. doi: 10.1096/fasebj.7.6.8472896. [DOI] [PubMed] [Google Scholar]
- Reutershan J. CXCR2- The receptor to hit. Drug News Perspect. 2006;19:615–623. doi: 10.1358/dnp.2006.19.10.1068009. [DOI] [PubMed] [Google Scholar]
- Rezaie P, Trillo-Pazos G, Everall IP, DK Expression of beta-chemokines and chemokine receptors in human fetal astrocyte and microglial co-cultures: potential role of chemokines in the developing CNS. Glia. 2002;37:64–75. doi: 10.1002/glia.1128. [DOI] [PubMed] [Google Scholar]
- Rhodes JKJ, Sharkey J, Andrews PJD. The temporal expression, cellular localisation, and inhibition of the chemokines MIP-2 and MCP-1 after traumatic brain injury in the rat. J Neurotrauma. 2009;26:1–19. doi: 10.1089/neu.2008.0686. [DOI] [PubMed] [Google Scholar]
- Rollins BJ. JE/MCP-1: an early-response gene encodes a monocyte-specific cytokine. Cancer Cells. 1991;3:517–524. [PubMed] [Google Scholar]
- Rollins BJ. Monocyte chemoattractant protein-1: a potential regulator of monocyte recruitment in inflammatory disease. Mol Med Today. 1996;2:198–204. doi: 10.1016/1357-4310(96)88772-7. [DOI] [PubMed] [Google Scholar]
- Rose JJ, Foley JF, Murphy PM, Venkatesan S. On the mechanism and significance of ligand-induced internalisation of human neutrophil chemokine receptors CXCR1 and CXCR2. J Biol Chem. 2004;279:24372–24386. doi: 10.1074/jbc.M401364200. [DOI] [PubMed] [Google Scholar]
- Saas P, Walker PR, Quiquerez A-L, Chalmers DE, Arrighi J-F, Lienard A, Boucraut J, Dietrich P-Y. A self-defence mechanism of astrocytes against Fas-mediated death involving interleukin-8 and CXCR2. NeuroReport. 2002;13:1921–1924. doi: 10.1097/00001756-200210280-00018. [DOI] [PubMed] [Google Scholar]
- Schilling M, Strecker JK, Ringerstein EB, Schäbitz WR, Kiefer R. The role of CC chemokine receptor 2 on microglia activation and blood-borne cell recruitment after transient focal cerebral ischemia in mice. Brain Res. 2009a;1289:79–84. doi: 10.1016/j.brainres.2009.06.054. [DOI] [PubMed] [Google Scholar]
- Schilling M, Strecker JK, Schäbitz WR, Ringerstein EB, Kiefer R. Effects of monocyte chemoattractant protein-1 on blood-borne cell recruitment after transient focal cerebral ischemia in mice. Neuroscience. 2009b;161:806–812. doi: 10.1016/j.neuroscience.2009.04.025. [DOI] [PubMed] [Google Scholar]
- Simpson JE, Newcombe J, Cuzner ML, Woodroofe MN. Expression of monocyte chemoattractant protein-1 and other beta-chemokines by resident glia and inflammatory cells in multiple sclerosis lesions. J Neuroimmunol. 1998;84:238–249. doi: 10.1016/s0165-5728(97)00208-7. [DOI] [PubMed] [Google Scholar]
- Sindern E, Niederkinkhaus Y, Henschel M, Ossege LM, Patzold T, Malin JP. Differential release of beta chemokines in serum and CSF of patients with relapsing-remitting multiple sclerosis. Acta Neurol Scand. 2001;104:88–91. doi: 10.1034/j.1600-0404.2001.104002088.x. [DOI] [PubMed] [Google Scholar]
- Song L, Pachter JS. Monocyte chemoattractant protein-1 alters expression of tight junction-associated proteins in brain microvascular endothelial cells. Microvasc Res. 2004;67:78–89. doi: 10.1016/j.mvr.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Sozzani S, Zhou D, Locati M, Rieppi M, Proost P, Magazin M, Vita N, van Damme J, Mantovani A. Receptors and transduction pathways for monocyte chemotactic protein-2 and monocyte chemotactic protein-3. Similarities and differences with MCP-1. J Immunol. 1994;152:3615–3622. [PubMed] [Google Scholar]
- Stahel PF, Shohami E, Younis FM, Kariya K, Otto VI, Lenzlinger PM, Grosjean MB, Eugster H-P, Trentz O, Kossmann T, Morganti-Kossmann MC. Experimental closed head injury: analysis of neurological outcome, blood-brain barrier dysfunction, intracranial neutrophil infiltration, and neuronal cell death in mice deficient in genes for pro-inflammatory cytokines. J Cereb Blood Flow Metab. 2000;20:369–380. doi: 10.1097/00004647-200002000-00019. [DOI] [PubMed] [Google Scholar]
- Stamatovic SM, Keep RF, Kunkel SL, Andjelkovic AV. Potential role of MCP-1 in endothelial cell tight junction ‘opening:' signaling via Rho and Rho kinase. J Cell Sci. 2003;116:4615–4628. doi: 10.1242/jcs.00755. [DOI] [PubMed] [Google Scholar]
- Stamatovic SM, Shakui P, Keep RF, Moore BB, Kunkel SL, Rooijen NV, Andjelkovic AV. Monocyte chemoattractant protein-1 regulation of blood-brain barrier permeability. J Cereb Blood Flow Metab. 2005;25:593–606. doi: 10.1038/sj.jcbfm.9600055. [DOI] [PubMed] [Google Scholar]
- Tanimoto N, Terasawa M, Nakamura M, Kegai D, Aoshima N, Kobayashi Y, Nagata K. Involvement of KC, MIP-2 and MCP-1 in leukocyte infiltration following injection of necrotic cells into the peritoneal cavity. Biochem Biophys Res Commun. 2007;361:533–536. doi: 10.1016/j.bbrc.2007.07.060. [DOI] [PubMed] [Google Scholar]
- Thibeault I, Laflamme N, Rivest S. Regulation of the gene encoding the monocyte chemoattractant protein 1 (MCP-1) in the mouse and rat brain in response to circulating LPS and proinflammatory cytokines. J Comp Neurol. 2001;434:461–477. doi: 10.1002/cne.1187. [DOI] [PubMed] [Google Scholar]
- Tsai HH, Frost E, To V, Robinson S, ffrench-Constant C, Geertman R, Ransohoff RM, Miller RH. The chemokine receptor CXCR2 controls positioning of oligodendrocyte precursors in developing spinal cord by arresting their migration. Cell. 2002;110:373–383. doi: 10.1016/s0092-8674(02)00838-3. [DOI] [PubMed] [Google Scholar]
- Tylaska LA, Boring L, Weng W, Aiello R, Charo IF, Rollins BJ, Gladue RP. CCR2 regulates the level of MCP-1/CCL2 in vitro and at inflammatory sites and controls T cell activation in response to alloantigen. Cytokine. 2002;18:184–190. doi: 10.1006/cyto.2002.1031. [DOI] [PubMed] [Google Scholar]
- Valles A, Grijpink-Ongering L, de Bree FM, Tuinstra T, Ronken E. Differential regulation of the CXCR2 chemokine network in rat brain trauma: Implications for neuroimmune interactions and neuronal survival. Neurobiol Dis. 2006;22:312–322. doi: 10.1016/j.nbd.2005.11.015. [DOI] [PubMed] [Google Scholar]
- Van Der Voorn P, Tekstra J, Beelen RHJ, Tensen CP, Van Der Valk P, De Groot CJA. Expression of MCP-1 by reactive astrocytes in demyelinating multiple sclerosis lesions. Am J Pathol. 1999;154:45–51. doi: 10.1016/S0002-9440(10)65249-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villa P, Triulzi S, Cavalieri B, Di Bitondo R, Bertini R, Barbera S, Bigini P, Mennini T, Gelosa P, Tremoli E, Sironi L, Ghezzi P. The interleukin-8 (IL-8/CXCL8) receptor inhibitor reparixin improves neurological deficits and reduces long-term inflammation in permanent and transient cerebral ischemia in rats. Mol Med. 2007;13:125–133. doi: 10.2119/2007-00008.Villa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wain JH, Kirby JA, Ali S. Leukocyte chemotaxis: examination of mitogen-activated protein kinase and phosphotidylinositide 3-kinase activation by monocyte chemoattractant proteins -1, -2, -3 and -4. Clin Exp Immunol. 2002;127:436–444. doi: 10.1046/j.1365-2249.2002.01764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Asensio VC, Campbell IL. Cytokines and chemokines as mediators of protection and injury in the central nervous system assessed in transgenic mice. Curr Opin Microbiol Immunol. 2002;265:23–48. doi: 10.1007/978-3-662-09525-6_2. [DOI] [PubMed] [Google Scholar]
- Watson K, Fan GH. Macrophage inflammatory protein 2 inhibits beta-amyloid peptide (1–42)-mediated hippocampal neuronal apoptosis through activation of mitogen-activated protein kinase and phosphatidylinositol 3-kinase signaling pathways. Mol Pharmacol. 2005;67:757–765. doi: 10.1124/mol.104.004812. [DOI] [PubMed] [Google Scholar]
- Whalen MJ, Carlos TM, Kockanek PM, Wisniewski SR, Bell MJ, Clark RS, DeKosky ST, Marion DW, Adelson PD. Interleukin-8 is increased in cerebrospinal fluid of children with severe head injury. Crit Care Med. 2000;28:929–934. doi: 10.1097/00003246-200004000-00003. [DOI] [PubMed] [Google Scholar]
- White FA, Sun J, Waters SM, Ma C, Ren D, Ripsch M, Steflik J, Cortright DN, LaMotte RH, Miller RJ. Excitatory monocyte chemoattractant protein-1 signaling is up-regulated in sensory neurons after chronic compression of the dorsal root ganglion. Proc Natl Acad Sci USA. 2005;102:14092–14097. doi: 10.1073/pnas.0503496102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widera D, Holtkamp W, Entschladen F, Niggemann B, Zanker K, Kaltschmidt B, Kaltschmidt C. MCP-1 induces migration of adult neural stem cells. Eur J Cell Biol. 2004;83:381–387. doi: 10.1078/0171-9335-00403. [DOI] [PubMed] [Google Scholar]
- Woldemar Carr M, Roth SJ, Luther E, Rose SS, Springer TA. Monocyte chemoattractant protein 1 acts as a T-lymphocyte chemoattractant. Proc Natl Acad Sci USA. 1994;91:3652–3656. doi: 10.1073/pnas.91.9.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu D, LaRosa GJ, Melvin SI. G protein-coupled signal transduction pathways for interleukin-8. Science. 1993;261:101–103. doi: 10.1126/science.8316840. [DOI] [PubMed] [Google Scholar]
- Xia M, Hyman BT. GROalpha/KC, a chemokine receptor CXCR2 ligand, can be a potent trigger for neuronal ERK1/2 and PI-3 kinase pathways and for tau hyperphosphorylation-a role in Alzheimer's disease. J Neuroimmunol. 2002;122:55–64. doi: 10.1016/s0165-5728(01)00463-5. [DOI] [PubMed] [Google Scholar]
- Yan YP, Sailor KA, Lang BT, Park SW, Vemuganti R, Dempsey RJ. Monocyte chemoattractant protein-1 plays a critical role in neuroblast migration after focal cerebral ischemia. J Cereb Blood Flow Metab. 2007;27:1213–1224. doi: 10.1038/sj.jcbfm.9600432. [DOI] [PubMed] [Google Scholar]
- Yang W, Wang D, Richmond A. Role of clathrin-mediated endocytosis in CXCR2 sequestration, resensitization, and signal transduction. J Biol Chem. 1999;274:11328–11333. doi: 10.1074/jbc.274.16.11328. [DOI] [PubMed] [Google Scholar]
- Yoshimura T, Leonard EJ. Human monocyte chemoattractant protein-1: structure and function. Cytokines. 1992;4:131–152. [PubMed] [Google Scholar]
- Yoshimura T, Robinson EA, Tanaka S, Appella E, Kuratsu J-i, Leonard EJ. Purification and amino acid analysis of two human glioma-derived monocyte chemoattractants. J Exp Med. 1989;169:1449–1459. doi: 10.1084/jem.169.4.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youssef S, Wildbaum G, Karin N. Prevention of experimental autoimmune encephalomyelitis by MIP-1alpha and MCP-1 naked DNA vaccines. J Autoimmun. 1999;13:21–29. doi: 10.1006/jaut.1999.0306. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Rollins BJ. A dominant negative inhibitor indicates that monocyte chemoattractant protein-1 functions as a dimer. Mol Cell Biol. 1995;15:4851–4855. doi: 10.1128/mcb.15.9.4851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnik A, Yoshie O. Chemokines: a new classification system and their role in immunity. Immunity. 2000;12:121–127. doi: 10.1016/s1074-7613(00)80165-x. [DOI] [PubMed] [Google Scholar]