Abstract
According to the published data, most primary central nervous system lymphomas (pcnsls) are B-cell lymphomas; primary T-cell lymphomas are rare. In a search of the medline database, we found only 6 cases of primary T-cell pcnsl. Here, we present the case of a 43-year-old man with aids, not on highly active antiretroviral therapy, who presented with focal neurologic symptoms and was found on magnetic resonance imaging to have multiple brain lesions. A biopsy showed T-cell lymphoma, and the patient was subsequently treated with whole-brain radiation, to marked clinical response. Reported cases from the literature of primary T-cell pcnsl in aids patients are summarized in this review.
Keywords: Primary cns lymphoma, T cells, non-Hodgkin lymphoma, aids
1. INTRODUCTION
Primary central nervous system lymphomas (pcnsls) are an uncommon form of extranodal non-Hodgkin lymphoma, but they are becoming increasingly more frequent 1. Currently, the incidence has increased to 4%–7% of newly diagnosed primary central nervous system (cns) tumours, and in the general population, the incidence rate is approximately 30 cases per million person–years 2. More than 95% of pcnsls are B-cell lymphomas. T-Cell pcnsl is less well defined; its biologic behaviour and response to treatment have been difficult to evaluate because of its rarity.
In aids patients, the reported incidence of pcnsl is 1000 times that seen in the general population 3,4. Most of the reported cases are B-cell pcnsl. A search of the medline database for pcnsl in aids patients found only 6 cases 5–9. Here, we present another case of an aids patient with T-cell pcnsl, treated successfully with whole-brain radiation and highly active antiretroviral therapy (haart).
2. CASE DESCRIPTION
A 43-year-old man presented to our hospital with headaches and right facial twitching for few days, associated with nausea and dizziness. His past medical history was significant for infection with hiv diagnosed 10 years earlier. Because of financial circumstances, the patient had stopped his haart 10 months earlier.
On physical examination, the patient was alert and oriented. His vital signs were normal. He had a mild word-finding deficit, right facial droop, right pronator drift, and mild right arm hyperreflexia. The rest of the physical examination was normal.
Laboratory work up showed a white blood cell count of 3400/mL, a CD4 count of 78/mL (normal: 493–1666/mL), an hiv viral load above 500,000/mL, positive Toxoplasma immunoglobulin G antibodies, negative serum cryptococcal antigen, and a nonreactive rapid plasma reagin test.
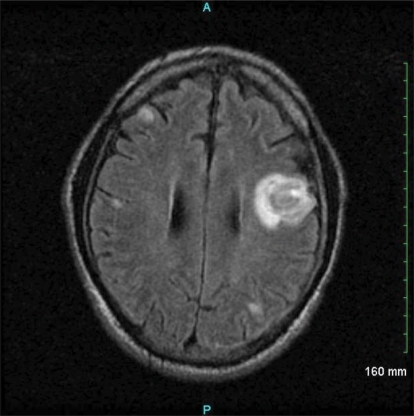
Magnetic resonance imaging (mri) of the brain showed a large mass in the left frontoparietal region, with small non-enhancing lesions in the brain (Figure 1). A presumptive diagnosis of cerebral toxoplasmosis was made, for which the patient was treated with pyrimethamine, sulfadiazine, and leucovorin, with phenytoin for seizure prophylaxis. To avoid possible complications of anemia and immune reconstitution syndrome, haart was planned to be restarted 2 weeks later.
Figure 1.
Magnetic resonance imaging of the brain demonstrates an enhancing 2×3-cm mass involving the left frontoparietal region, and some small non-enhancing lesions in the brain bilaterally.
The patient improved symptomatically and was discharged home. A follow-up brain mri 10 days later demonstrated no significant changes.
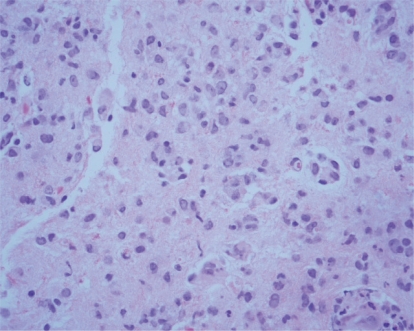
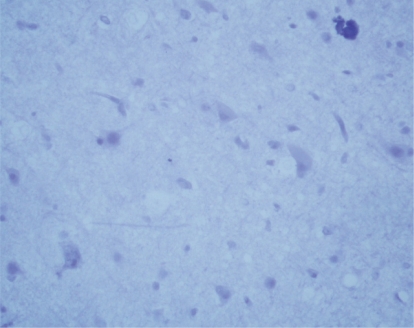
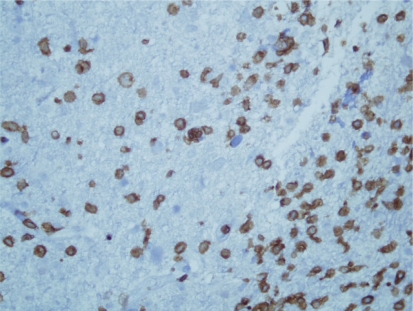
One month later, the man came to our emergency department with a history of progressively increasing partial focal seizures that had started after he had stopped his medications 2 weeks earlier because of financial concerns. Brain mri showed a slight increase of the old left frontoparietal lesion and small new enhancing lesions bilaterally. A computed tomography–guided brain biopsy showed atypical lymphocytes (Figure 2), positive staining for lymphocyte common antigen and the T-cell marker CD3 (Figure 3), and no staining for the Bcell marker CD20 (Figure 4). Immunoperoxidase staining for cytomegalovirus, Herpes simplex virus, and Toxoplasma was also negative. Giemsa, Gram, and acid-fast stains were also negative.
Figure 2.
Brain mass biopsy shows atypical lymphocytes (40× magnification).
Figure 3.
Immunoperoxidase staining of the brain mass biopsy with the T-cell marker CD3 is extensive.
Figure 4.
Immunoperoxidase staining of the brain mass biopsy with the B-cell marker CD20 is absent.
The patient refused chemotherapy, but underwent whole-brain external-beam radiation therapy and was started on haart. At the time of writing, he has been closely followed for 31 months; serial brain mri has shown stable disease, and the patient has been symptom-free.
3. DISCUSSION
A search of the medline database found only 6 other cases of T-cell pcnsl in aids patients 5–9. Table i summarizes the clinical features of those cases and the present case. Median age of the patients is 38 years. The patients are predominantly male.
Table I.
Cases of primary central nervous system T-cell lymphoma in the literature
| Characteristic |
Case and reference |
||||||
|---|---|---|---|---|---|---|---|
| 1 Aydin et al., 19987 | 2 Smith et al., 19968 | 3 Rao et al., 19899 | 4 Bataille et al., 200010 | 5 Chappell et al., 199211 | 6 Bashir et al., 200012 | 7 (present case) | |
| Age (years) | 43 | 36 | 38 | 53 | 30 | 36 | 43 |
| Sex | Male | Male | Male | Male | Female | Male | Male |
| Presenting symptoms | Fever, seizures, altered mental status | Dysarthria, headache, arm weakness | Headache, hearing loss, amblyopia | Progressive ataxia | Ataxia | Seizures | Nausea, dizziness facial palsy, hyperreflexia |
| CD4 count (cells/mL) | na | <50 | 28–90 | 110 | na | na | 78 |
| haart at time of diagnosis? | Yes | Yes | na | Yes | na | na | na |
| History of opportunistic infections | na | pcp | Disseminated mac, Candida esophagitis, salmonellosis, hsv | Oral candidiasis | na | na | na |
| Presenting lesions | Single | Single | Multiple | Multiple | Single | Multiple | Multiple |
| Site of disease | Left parietal | Right cerebellum | Right frontoparietal | Right frontoparietal and left cerebellum | Cerebellar vermis | na | Bilateral frontoparietal |
| Method of diagnosis | Stereotactic biopsy | na | Stereotactic biopsy | Brain biopsy | Brain biopsy | Brain biopsy | ct-guided brain biopsy |
| Pathology | Extranodal nk cell and T-cell lymphoma | na | na | Atypical pleomorphic lymphocytes | Pleomorphic immunoblastic T-cell lymphoma | Pleomorphic large T-cell lymphoma | na |
| Immunophenotype | Positive for CD45, CD3 (cytoplasmic), CD2, CD56, perforin; negative for CD20, CD4, CD8 | na | Positive for CB3 | Positive for CD45 (lca), CD45RO; negative for CD20 | Positive for pan T-cell marker, negative for pan B-cell marker | Positive for pan T-cell marker, negative for pan B-cell marker | Positive for CD45 (lca), CD3 |
| pcr for ebv | Positive | na | Positive | na | na | na | na |
| Other serology | Negative for Toxoplasma IgM antibody, Cryptococcus antigen | Serum Toxoplasma titres < 1:16 | Negative for Toxoplasma antibody | na | na | na | Positive for Toxoplasma IgG antibody; negative for serum Cryptococcus antigen |
| Treatment | na | na | na | Whole-brain radiation and cns chemotherapy | na | na | Whole-brain radiation |
| Outcome | Death a few days after diagnosis | na | Death months later | Clinically improved | Death | na | Clinically improved |
na = not available; haart = highly active antiretroviral therapy; pcp = Pneumocystis carinii pneumonia; mac = Mycobacterium avium complex; hsv = Herpes simplex virus; ct = computed tomography; nk = natural killer; lca = leukocyte common antigen; pcr = polymerase chain reaction; ebv = Epstein–Barr virus; IgM = immunoglobulin M; IgG = immunoglobulin G; cns = central nervous system.
Primary central nervous system lymphoma can present with focal or non-focal signs and symptoms that have usually been present for fewer than 3 months. Patients with aids are more likely than other patients to present with altered mental status and seizures (50% vs. 35%) and less likely to show increased intracranial pressure (14% vs. 32%) 10. Most of the patients in this review presented with focal neurologic symptoms.
Patients with aids presenting with signs and symptoms suggestive of cns disease should be evaluated radiologically. On computed tomography imaging, pcnsl usually appears as a well-defined focal lesion that can be isodense or hyperdense. The diagnostic yield is higher with mri.
In immunocompetent patients, T-cell lymphomas present more frequently as infratentorial lesions. In the present review, most patients had lesions in the supratentorial region (Table i).
Measurement of Epstein–Barr viral dna in a sample of cerebrospinal fluid can aid in making the diagnosis, but stereotactic brain biopsy remains the definitive method 11. Diagnosis of T-cell tumours can be difficult, and their incidence, despite being low, is possibly overestimated. Furthermore, B-cell neoplasms are frequently infiltrated by reactive T cells, complicating the interpretation of immunophenotyping. Staging is generally not indicated because pcnsl almost always remains confined to the cns.
Optimal treatment for pcnsl in aids patients is not yet defined. Standard first-line treatment of radiation therapy and corticosteroids can achieve a complete response in 20%–50% of patients; median survival is 13.5 months, however 12. The short survival reflects deaths from the opportunistic infections that are a result of the profound immunodeficiency that most patients with pcnsl already have 13. Chemotherapy combined with radiation therapy may provide some benefit to patients with relatively high CD4 counts 13,14. Among the patients in our review, treatment was reported for only 2, both of whom were treated with whole-brain radiation.
Some studies have suggested that survival is longer for patients with T-cell pcnsl 15. Of the 7 patients in this review, 3 died soon after diagnosis, and the 2 that received treatment improved clinically; the fates of the other 2 were not reported (Table i).
4. CONCLUSIONS
In general, T-cell pcnsl is rare; it appears to be even more rare in immunocompromised patients. More reports of cases are needed to help improve diagnosis, treatment, and prognosis in this kind of lymphoma.
Footnotes
5. CONFLICT OF INTEREST DISCLOSURES
All authors declare that no financial conflicts of interest exist.
6. REFERENCES
- 1.Fine HA, Mayer RJ. Primary central nervous system lymphoma. Ann Intern Med. 1993;119:1093–104. doi: 10.7326/0003-4819-119-11-199312010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Corn BW, Marcus SM, Topham A, Hauck W, Curran WJ., Jr Will central nervous system lymphoma be the most frequent brain tumor diagnosed in the year 2000? Cancer. 1997;79:2409–13. [PubMed] [Google Scholar]
- 3.Flinn IW, Ambinder RF. aids primary central nervous system lymphoma. Curr Opin Oncol. 1996;8:373–6. doi: 10.1097/00001622-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 4.MacMahon EM, Glass JD, Hayward SD, et al. Epstein–Barr virus in aids-related primary central nervous system lymphoma. Lancet. 1991;338:969–73. doi: 10.1016/0140-6736(91)91837-k. [DOI] [PubMed] [Google Scholar]
- 5.Cobo F, Talavera P, Busquier H, Concha A. cnk/T-cell brain lymphoma associated with Epstein–Barr virus in a patient with aids. Neuropathology. 2007;27:396–402. doi: 10.1111/j.1440-1789.2007.00784.x. [DOI] [PubMed] [Google Scholar]
- 6.Bindal AK, Blisard KS, Melin–Aldama H, Warnick RE. Primary T-cell lymphoma of the brain in acquired immunodeficiency syndrome: case report. J Neurooncol. 1997;31:267–71. doi: 10.1023/a:1005769406324. [DOI] [PubMed] [Google Scholar]
- 7.Aydin F, Bartholomew PM, Vinson DG. Primary T-cell lymphoma of the brain in a patient at advanced stage of acquired immunodeficiency syndrome. Arch Pathol Lab Med. 1998;122:361–5. [PubMed] [Google Scholar]
- 8.Smith GH, MacLeod JD, Routy JP. Primary brain T-cell lymphoma in an aids patient [abstract 4225] Int Conf AIDS. 1996;11:289. [Available online at: gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102220516.html; cited July 20, 2010] [Google Scholar]
- 9.Rao C, Wrzolek M, Koszlowski PB, Anzil AP, Thelmo WK, Sher JH. Primary T cell central nervous system lymphoma in aids [abstract] J Neuropathol Exp Neurol. 1989;48:302. [Google Scholar]
- 10.Bataille B, Delwail V, Menet E, et al. Primary intracerebral malignant lymphoma: report of 248 cases. J Neurosurg. 2000;92:261–6. doi: 10.3171/jns.2000.92.2.0261. [DOI] [PubMed] [Google Scholar]
- 11.Chappell ET, Guthrie BL, Orenstein J. The role of stereotactic biopsy in the management of hiv-related focal brain lesions. Neurosurgery. 1992;30:825–9. doi: 10.1227/00006123-199206000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Abrey LE, Yahalom J, DeAngelis LM. Treatment for primary cns lymphoma: the next step. J Clin Oncol. 2000;18:3144–50. doi: 10.1200/JCO.2000.18.17.3144. [DOI] [PubMed] [Google Scholar]
- 13.Forsyth PA, Yahalom J, DeAngelis LM. Combined-modality therapy in the treatment of primary central nervous system lymphoma in aids. Neurology. 1994;44:1473–9. doi: 10.1212/wnl.44.8.1473. [DOI] [PubMed] [Google Scholar]
- 14.DeMario MD, Liebowitz DN. Lymphomas in the immunocompromised patient. Semin Oncol. 1998;25:492–502. [PubMed] [Google Scholar]
- 15.McCue MP, Sandrock AW, Lee JM, Harris NL, Hedley–Whyte ET. Primary T-cell lymphoma of the brainstem. Neurology. 1993;43:377–81. doi: 10.1212/wnl.43.2.377. [DOI] [PubMed] [Google Scholar]