Abstract
Two-thirds of those with HIV worldwide live in sub-Saharan Africa. Alcohol use is associated with the HIV epidemic through risky sex and suboptimal ARV adherence. In western Kenya, hazardous drinking was reported by HIV (53%) and general medicine (68%) outpatients. Cognitive behavioral treatment (CBT) has demonstrated strong efficacy to reduce alcohol use. This article reports on a systematic cultural adaptation and pilot feasibility study of group paraprofessional-delivered CBT to reduce alcohol use among HIV-infected outpatients in Eldoret, Kenya. Following adaptation and counselor training, five pilot groups were run (n=27). Overall attendance was 77%. Percent days abstinent from alcohol (PDA) before session 1 was 52%–100% (women) and 21–36% (men), and by session 6 was 96%–100% (women) and 89%–100% (men). PDA effect sizes (Cohen’s d) between first and last CBT session were 2.32 (women) and 2.64 (men). Participants reported treatment satisfaction. Results indicate feasibility, acceptability and preliminary efficacy for CBT in Kenya.
Keywords: alcohol, cognitive behavioral therapy, cultural adaptation, HIV, Kenya
Introduction
Approximately two-thirds of the world’s 33.2 million individuals infected with the HIV virus live in sub-Saharan Africa.1 Alcohol has been associated with the HIV epidemic2 through its contribution to risky sex.3 Alcohol is associated with suboptimal (antiretroviral) ARV adherence4 and poorer medical outcomes among those who are HIV-infected.5 Several Africa-based studies have demonstrated a high rate of alcohol dependence (using internationally validated instruments (e.g., AUDIT and CAGE), diagnostic criteria (e.g., ICD-10 and DSM-IV), or World Health Organization criteria),6–8 often involving the consumption of inexpensive local brew with high ethanol content.9 In Eldoret, Kenya, our previous work has also shown that an average chang’aa drink (locally made spirit) is equal to two U.S. standard drinks9 and prevalence of hazardous drinking was reported by 53% of HIV and 68% of general medicine outpatients (a score of ≥ 8 using the AUDIT survey).10 There is growing evidence in both the U.S. and Africa that heavy drinking limits the success of HIV prevention efforts.11,12 These data suggest the need for alcohol interventions in sub-Saharan Africa to curb the HIV epidemic.
This article describes an effort to adapt Cognitive-Behavioral Therapy (CBT) to reduce alcohol use among HIV-infected outpatients in Eldoret, Kenya and to conduct a preliminary evaluation of its feasibility, or practical ability to be conducted, in that setting. CBT is a highly structured, skills-based approach largely informed by social learning theory,13 which construes the maintenance of addictive behaviors at least in part as learned behaviors to cope with stress and problems.14 CBT teaches patients coping skills to handle high-risk substance use situations. CBT was selected for this Kenyan adaptation because of its strong empirical support in both individual and group formats to reduce substance abuse,15–17 durability of treatment effects, and prior successful applications in sub-Saharan Africa to reduce risky sexual behaviors among HIV-infected Zambian couples18 and to improve mood among Nigerian surgical patients.19 Furthermore, because of its highly structured format, we felt CBT was feasible for training paraprofessionals and for delivery to those with limited formal education.
Cultural adaptation refers to the process of making psychotherapy goals, language, content and process20 consistent with those of the target population to enhance treatment relevance, credibility, and efficacy.21 Cultural adaptation of treatments is important because many evidence-based behavioral interventions have been developed and tested among Caucasian middle-class Americans.20 Further, beliefs about behavior change, sociopolitical influences, socioeconomic resources and health knowledge may differ substantially across cultural settings. For example, limited educational opportunities in resource-limited settings may merit unique approaches to delivery, such as training lay persons or paraprofessionals, those with little or no background in psychology or counseling, in contrast to employing masters- or doctoral-level therapists in industrialized countries.
Various frameworks have been posited for culturally adapting psychotherapies. Most are geared toward minority groups living in the U.S.22–25 Bernal and colleagues have developed a framework for enhancing cultural ecology when adapting psychotherapy for treatment outcome research.20 They described eight overlapping cultural dimensions and features of the treatment population that should be incorporated into psychotherapy outcome research: concepts, language, persons, content, metaphors, goals, methods and context. Concepts refer to the conceptualization of the target problem and of the underlying treatment constructs. Language is the main vehicle of expression within one’s culture. Persons indicate factors related to similarities and differences between the patient and the counselor. Content signifies the counselor’s knowledge of the patient’s cultural values, traditions and beliefs. Metaphors refer to the use of symbols within a culture. Goals specify the relevance and framing of treatment goals. Methods indicate procedures such as treatment delivery format and implementation. Finally, context includes the social, economic and political context of treatment, as well as process of acculturation, when relevant. As this framework provided heuristic value, we adapted CBT with attention to these eight dimensions.
While a cultural adaptation framework guides the focus of adaptations being considered for a psychotherapy, we relied upon a stage model of psychotherapy development26 to organize the process of making cultural adaptations and testing their feasibility. The first stage of this three-stage model involves therapy development and pilot testing. Therapeutic principles/mechanisms of action, key strategies and techniques, implementation guidelines and procedures, and differences from available treatments are specified. Treatment manuals and therapist fidelity rating systems are developed. Focus groups with individuals likely to deliver or receive the treatment indicate the potential feasibility and acceptability of treatment. A small pilot trial then determines patient acceptance of treatment, promise for producing targeted outcomes, and identification of key study implementation issues. The second stage establishes treatment efficacy and mechanisms under well-controlled research conditions. The third stage determines efficacy in a community setting of a proven treatment.
This report describes the developmental process by which we adapted CBT for alcohol treatment to the Kenyan culture. It is part of the Kenya Health Behavior Study (R21AA016884) in which a randomized clinical trial is underway of group CBT to reduce alcohol use among HIV-infected outpatients, emanating from the developmental work described in this article. We first describe how we adapted CBT to the cultural elements in Eldoret, Kenya. We next present our pilot study and the results, which reflect upon acceptability and preliminary efficacy of the adapted CBT. To our knowledge, this article is the first published description of a systematic adaptation of CBT in a sub-Saharan African setting.
Methods
Setting
Kenya is a country in East Africa with 39 million citizens. HIV prevalence was estimated to be 7.4% in 2007.27 Our collaborators, the U.S. Agency for International Development - Academic Model for Providing Access to Healthcare (USAID - AMPATH) partnership, currently provide HIV care for more than 60,000 patients in 23 clinics in western Kenya and utilize an electronic medical records system.28 This healthcare delivery system evolved as a result of a 20-year collaboration between the medical schools of Indiana University and Moi University in Kenya. The site of our study was the AMPATH HIV outpatient clinic in Eldoret in western Kenya, with 13,500 current patients representing predominantly four ethnic groups but including several others. Nearly 100% of the patients at this clinic speak Kiswahili, one of two national languages of Kenya (the other language is English).
Eighty percent of Kenyans are farmers, typically at subsistence levels.29 Unemployment (40%) and poverty (50%) are high, with an educational expectancy of 10 years,30 and monthly income averaging U.S. $30.31 There are few professional resources for treating alcohol use disorders; in 2005, there were 47 psychiatrists serving the entire country.32
In Kenya, like other African countries, strong social networks support and strengthen communities.33 For example, there is a cultural custom that residents of a village will share financial resources with each other in times of need, and child care is often shared or taken over by those with adequate resources. However, HIV stigma often breaks down social networks and results in discrimination and rejection by families and communities.29 For example, 46% of participants in the pre-testing of our Kiswahili baseline survey (n=14) reported losing a job or place to stay due to HIV, and 57% reported that it was important to keep HIV a secret. Women infected with HIV who drink alcohol are particularly vulnerable to rejection, due to a secondary cultural and political status. Polygamy is a common cultural practice permitted exclusively for men. Women compose 89% of the farming workforce and only 5% of landowners, due to the traditional law restriction against female inheritance of land and other property, except under special circumstances.34 These cultural elements shaped the CBT adaptation.
Participants
Two types of participants were involved in this study. First, a multidisciplinary Kenyan panel served as a focus group for the treatment development phase of the study. The participants included three psychologists, a psychiatrist, two physicians and a lay representative of the community, including two alcoholics in recovery. Second, HIV-infected outpatients from the Eldoret clinic served as focus group and pilot study participants. Inclusion criteria were: having drunk any amount of alcohol in the past month, residing and planning to stay within one hour travel distance time from the clinic during the pilot study, willing to participate in a group treatment, and able to speak Kiswahili or English, depending on the specific group. Exclusion criteria were active suicidality or psychosis and having attended the small onsite peer-led alcohol support group. This study was approved by local and collaborating institutional review boards.
Procedures
Cultural adaptation
The process of culturally adapting CBT involved several steps over 2½ years starting in June 2006. Information about the Kenyan culture was gathered from multiple sources: qualitative data gathered within a clinical context and derived from patient interviews, multidisciplinary and lay panel discussions, focus groups to pre-test the Kiswahili baseline survey, CBT training and piloting, and participant debriefings. During clinical interviews with 14 Kenyan HIV-infected outpatients with drinking concerns and eight hours of observation of the local alcohol peer support group, CBT compatibility with the local conceptual model of drinking was assessed. A 6-session CBT treatment manual, a paraprofessional training manual, and a paraprofessional training workbook, were developed and vetted by the panel and the research team. Once the treatment manual had been adapted and revised, a counselor fidelity rating and monitoring system based on the Yale Adherence and Competence Scale (YACS) 35 was developed. The YACS measures adherence, the extent to which counselors follow the treatment protocol, and competence, the skill level with which counselors deliver treatment.
Counselor training
Because of the dearth of mental health professionals, we hired and trained paraprofessionals. Hiring procedures employed case conceptualization essays and behavioral role plays in an effort to select those who demonstrated natural talents – empathy, emotional perceptiveness, good communication skills and analytical thinking (ability to match participant statements with appropriate emotional and verbal responses). Training and initial piloting were conducted in English to enable supervision by RP. Subsequent piloting and the randomized trial were conducted in Kiswahili, after Kiswahili skills were acquired by RP, with translational support provided as necessary. Initial training in CBT included classroom work utilizing frequent role plays, videotaped feedback and training in ethics and basic health education. Each counselor was then supervised using YACS-based adherence and competence ratings of their videotaped role plays with medical students as simulated patients. Counselors who met the minimum criteria, a frequency rating of 4 on at least 50% of YACS items, with a skill rating of 4 on these items, all on a 7-point scale,35 could then conduct 6-session videotaped pilot groups. Certification to participate in the randomized trial required a minimum delivery of one group in English, and one group in Kiswahili. Two of five trainees met certification procedures and were hired. The two counselors (one male, one female, one HIV-infected) possessed high school and psychological counseling diplomas, and received 175 and 300 hours, respectively, of total training/supervision time prior to the trial.
Pilot feasibility study
Overview
Following protocol adaptation and counselor training, we ran a within-subjects pilot feasibility study of the 6-session CBT. The study purposes were to further train the counselors, fine-tune the treatment manual and to refine recruitment and treatment procedures. Additionally, we sought to evaluate acceptability and whether the treatment had an impact on alcohol use. Together these results would indicate whether adjustments were needed in study procedures, counselor training or the CBT protocol prior to running the trial. Five groups (three for women, two for men) were run by same-sex counselors. Two groups were run from October to December 2007 before study procedures were interrupted by post-election violence following a disputed December 27th presidential election. Three groups were run from August to October 2008 once violence abated.
Recruitment
Patients were approached in the HIV clinic by same-sex staff and asked for verbal consent for a brief interview to describe a health behavior study. Those who consented were taken to a private area, given study details and were interviewed for eligibility. Eligible participants who gave written consent were assigned consecutively to a group until full.
Measurement
We tracked treatment attendance, acceptability, and alcohol use. Treatment attendance was operationalized as those who attended the session. It did not include those who missed sessions due to a positive alcohol saliva test or to a psychiatric or medical referral. Treatment acceptability was assessed through post-treatment group debriefings.
Prior to each CBT session, we estimated use of local brew by asking participants how much money they spent on it, and use of commercial drink by asking volume drunk, both in the past 7 days, using the adapted Timeline Followback,9 a retrospective calendar-based measure employing memory cues demonstrated to be reliable and valid in previous studies.36 At every visit, we also assessed withdrawal symptoms using the validated CIWA-Ar37 and objective alcohol consumption using the Alco Screen® saliva tests donated by Chematics, Inc. This assay assesses alcohol consumed approximately in the last 1 to 6 hours at indications of .02, .04, .08 or .30% as reflected by swab color.38 A positive saliva test precluded participants from attending the CBT group due to possible alcohol triggers for other participants. The CIWA-Ar and TLFB were adapted to the culture and language using World Health Organization-modified methods.39
Data Analysis
We conducted all analyses using independent, individual-level methods rather than controlling for group membership, although we recognize that within-group data may be correlated. Percent days abstinent (PDA) from alcohol was calculated for each participant for each reporting period by dividing the number of days in which the participant did not drink by the total number of days in the reporting period. For example, not drinking on 7 out of 7 days would represent 100% abstinence, while not drinking on 3 out of 7 days would represent 43% abstinence. Individual mean percentages were then averaged across participants attending a session to obtain a mean group PDA for that session. In one pilot group in which sessions were doubled up for several weeks (i.e., the 6-session intervention occurred over 4½ weeks), some participants’ reports overlapped, resulting in fewer unique reporting days than for the other groups (32 versus 42 days). We analyzed the first report because of recency and less recall bias. We also calculated PDA based on fewer than 7 days (e.g, 3 or 4 days) for relevant sessions, since each session provided an opportunity to change behavior. Cohen's d was calculated to estimate the effect size within groups between the first and last session, dividing the within-group change by the pooled SD.40 Effect sizes were disaggregated by gender and then averaged to get a mean score.
Results
CBT cultural adaptations
Cultural adaptations made to CBT are organized according to Bernal and colleagues’ eight overlapping cultural dimensions and treatment population features (Table 1).
Table 1.
Features of cultural adaptation applied to cognitive behavioral therapy
| Cultural dimensions of treatment20 |
Kenyan cultural elements | Resulting adaptation |
|---|---|---|
| Concepts | First systematic CBT adaptation in Kenya: local conceptual model unknown |
–Clinical observations and interviews and panel discussion confirmed conceptual compatibility |
| Language | Kiswahili most common national language |
–Initial training and piloting conducted in English; subsequent piloting and treatment conducted in Kiswahili |
| Persons | HIV-infected Kenyan population | –Treatment delivered by Kenyans |
| –Serostatus disclosure by counselors not necessary | ||
| Metaphors | Rural and resource-limited setting with unique vernacular |
–Examples utilized rural images, local activities, group member names |
| Content | Unique Kenyan cultural traditions and beliefs |
–Treatment delivered in participant country of origin by Kenyan counselors to maximize integration |
| Goals | Salience for quitting drinking in Kenya |
–Goals to quit drinking developed by community |
| –Local motivation for behavior change integrated | ||
| Methods | Implementation and delivery format adapted to features of Kenyan culture and setting |
–CBT implemented in gender-stratified group format |
| –No significant other involvement | ||
| –Transport and problem-solving features added | ||
| Context | Influence of limited formal education, poverty, high unemployment, HIV stigma, and secondary status of women |
–HIV-alcohol risk educational component |
| –Illustrations, step-by-step, repetitive format | ||
| –Enhanced alcohol refusal and problem- solving skills | ||
Concepts
During clinical interactions with HIV-infected outpatients, drinking behaviors were discussed using behaviorally driven concepts such as cravings to drink, substituting sodas for alcohol, avoiding “drinking friends,” and experiencing consequences such as missing ARV doses. These observations suggested that CBT was compatible with the local conceptual model of drinking. The multidisciplinary Kenyan panel agreed that the content and techniques of the CBT protocol were fully suitable to Kenyan culture, however, that exercises should be adapted to the local setting, for example, addressing peer pressure to drink at chang’aa dens.
Language
Treatment in the trial was provided in Kiswahili, with spoken Kiswahili required for participation. Those who could not read Kiswahili (one woman in the pilot) were encouraged to obtain support to complete extra-session exercises. As Kiswahili is a relatively young language, many words have shared meanings and so were explained in a wider context. Counselors also used local idioms, for example, “take” rather than “drink” alcohol; “mama pima” as a woman who sells chang’aa; “kumi kumi” as a drink of chang’aa, and “matatu” as common transportation. The PI acquired Kiswahili skills during the project to provide training and supervision.
Persons
Treatment was provided by Kenyan counselors of various ethnic backgrounds. Our team felt it was unnecessary to stratify clients and counselors according to ethnicity because of the ground rules of confidentiality and respect conveyed and modeled by counselors. Indeed, after post-election violence subsided, our groups were attended by persons of all major ethnic groups in the region. Because of HIV stigma, our initial plan was for CBT to be delivered by only HIV-infected counselors. However, this was not feasible because this restriction resulted in too few HIV-infected applicants who could meet CBT performance thresholds to lead the intervention. We found that counselor skills in listening, empathy and respect resulted in adequate bonding and group cohesion, without disclosing a shared medical condition.
Metaphors
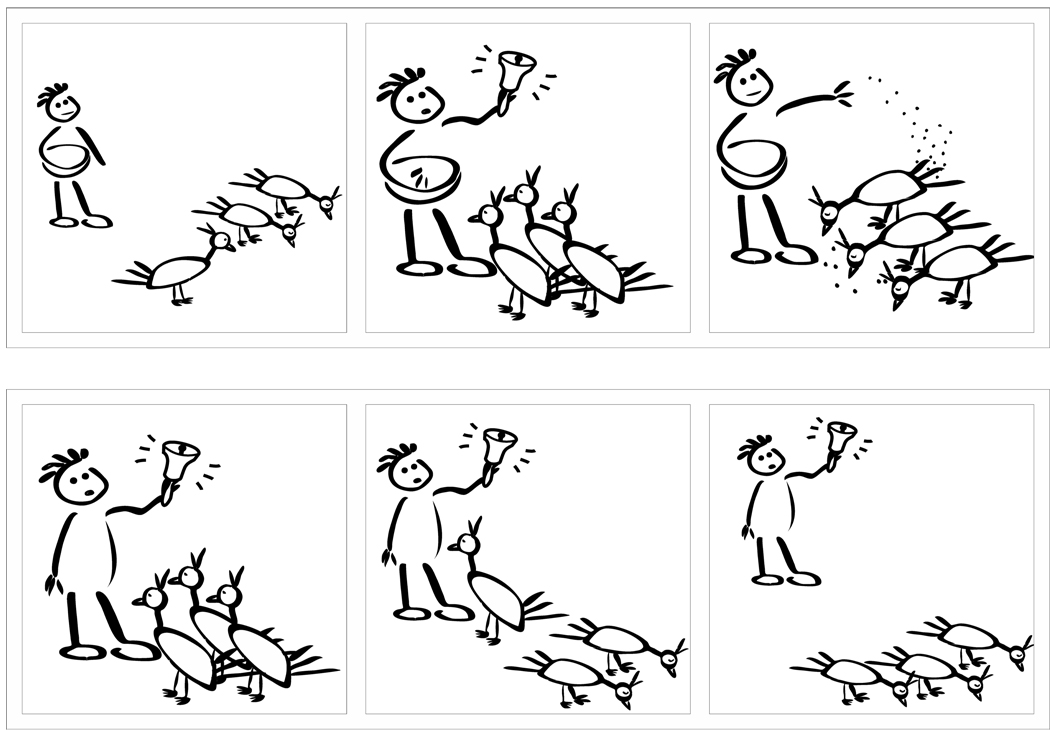
We employed rural images in visual aids and treatment materials, for example, in illustrations of conditioned cravings, those cravings developed by associating drinking behavior with usual drinking establishments, friends or other cues. Counselors described how chickens learn to gather for food after the farmer has repeatedly rung the bell before feeding (Figure 1, top row), and how these responses diminish once the farmer repeatedly rings the bell without providing food (Figure 1, bottom row). Additional illustrations depicted conditioned cravings using an example of drinking friends outside the chang’aa den, where local brew is made and sold. An illustration of the brief duration of drinking cravings showed a person walking up and down a hill, with the hilltop representing the peak of cravings. Exercises referred to chang’aa dens rather than bars, and walking rather than driving. Additionally, our previous work in this setting showed that participants had difficulty with conceptualizing examples employing the names of individuals they did not know. Conversely, participants would attribute to similarly named individuals the same behaviors. To avoid any such confusion, we employed within exercises only names of concurrent group members.
Figure 1.
Rural illustration of conditioned cravings
Acknowledgment: created by Robert Skipworth Comer, Indiana University School of Informatics
Content
Every person who treated and interacted with participants was Kenyan, with the exception of one U.S. physician residing in Kenya and occasional psychiatric risk assessments performed by the U.S. PI. The Kenyan team gave input at every stage of development and project implementation, maximizing integration of cultural values, traditions and beliefs.
Goals
The primary treatment goal to reduce alcohol use, rather than focus on other HIV risk related behaviors, was derived locally, as the project was initiated at the urging of the community to treat drinking problems as the first step toward curbing the HIV epidemic. Counselors often framed the goal to quit drinking in locally salient ways described by participants, including as a method for saving money, and to promote better health and longevity.
Methods
To enhance feasibility for paraprofessional delivery, we reduced the CBT protocol, typically 12 sessions, to six sessions. Other modifications to treatment implementation methods included the group therapy format because of the heavy reliance on social networks in Kenyan culture.33 In addition, groups were gender-stratified and assessments did not incorporate significant other involvement for verification of alcohol use because of the secondary status of women. We also provided general, rather than specific, text message reminders for appointments, so as not to disclose a clinical affiliation. No initial abstinence period was required due to patient unfamiliarity with detoxification procedures; however, a scheduled quit day was incorporated after session two. We objectively assessed alcohol consumption using saliva tests rather than Breathalyzers because our team learned that the latter had been recently adopted by Kenyan police and might evoke negative associations. Our project included transportation reimbursement for all appointments and frequent phone and text appointment reminders to enhance retention. Because of low attendance in some pilot groups (Table 2), staff also began to transport willing participants to the first CBT session only to boost treatment engagement in the randomized trial. We further added a 10-minute problem-solving checklist about potential barriers to attendance and brief weekly contact calls during non-treatment phases.
Table 2.
Demographic and retention characteristics of five pilot groups
| Gender | Language | Education* m(sd) |
Age (in years) m(sd) |
Percent on ARV |
Attended ≥ 1 session |
Number non-attenders |
Percent CBT attendance |
|---|---|---|---|---|---|---|---|
| Women | English | 11.4(2.6) | 33.4(5.0) | 62.5 | 8 | 0 | 87.5 |
| Women | English | 10.6(3.6) | 31.0(5.2) | 80.0 | 5 | 4 | 76.7 |
| Women | Kiswahili | 9.8(2.7) | 33.2(7.4) | 40.0 | 5 | 4 | 66.7 |
| Men | Kiswahili | 7.8(2.5) | 36.4(5.9) | 80.0 | 5 | 4 | 70.0 |
| Men | English | 12.0(0.0) | 38.5(7.6) | 75.0 | 4 | 2 | 79.2 |
| Total sum or m(sd) | 10.4(2.8) | 34.2(6.1) | 66.7 | 27 | 14 | 77.2 | |
highest year of education completed
Context
Our treatment protocol was adapted to socioeconomic, legal and psychosocial contextual issues. To accommodate educational levels (M=10.4 completed years), we demonstrated CBT using a step-by-step format, repeated explanations and illustrations. Misinformation about traditional brew was common, for example, beliefs that chang’aa could cure typhoid or prevent HIV transmission under certain conditions and, busaa, homemade beer, was beneficial during pregnancy and needed for proper lactation. Hence, we added a 45-minute risk education module to the first CBT session. Topics included the association of alcohol with adverse medical outcomes (e.g., during pregnancy), depression, risky sex, family violence, ARV adherence as well as HIV transmission facts and myths. Additionally, counselors facilitated examination of evidence for beliefs, consistent with the cognitive component of CBT. Because of high unemployment, counselors suggested volunteerism over employment as a means of building productivity and promoting recovery. They also capitalized on mobility due to unemployment by discussing avoidance techniques that included the possibility of temporarily changing residences during the initial recovery period, to avoid triggers associated with neighborhood chang’aa dens.
Because of stigma concerns, recommendations for disclosing serostatus outside the group generally were not made by counselors unless initiated by participants. In the face of poverty, unemployment and discrimination, income-generating activities for women often included making and selling traditional brew and engaging in transactional sex, the rendering of sex in exchange for goods, rent, money or school fees. Six of the 18 women reported making or selling traditional brew, or working in a bar. Counselors initiated problem-solving discussions focused on the frequent exposure to alcohol triggers and the perceived obligation to taste brew for customers before selling it. Three women reported engaging in transactional sex. For these women, serostatus disclosure to sexual partners was reported to be equivalent to loss of income. Similarly, refusing alcohol from partners or initiating condom use were feared to evoke suspicion of HIV infection. Hence, we adapted alcohol refusal skills to include possible medical excuses (e.g., acute infection, pregnancy, high blood pressure) for not drinking. For men as well, because of the cultural value to avoid “loss of face,” or awkwardness or rejection due to disagreement or refusal, we placed heavy emphasis on practice of alcohol refusal skills. All groups were engaged in problem-solving around drinking, and expanded practice of refusal in pairs.
Pilot feasibility study results
Participant characteristics and attendance
Among those who attended ≥ 1 session (n=27, 66%), mean attendance across the 6 sessions was 78% for women and 74% for men. Attendance among the Kiswahili groups was lowest, 67% compared to 82% for English groups (Table 2). Men (M=37.3, SD=6.3) were older (in years) than women (M=32.7, SD=5.6), while women (M=10.7, SD=2.8) were more educated than men (M=9.7, SD=2.8), as defined by the highest year of education completed.
Treatment acceptability
All groups reported satisfaction with treatment and the group format. Participants described enthusiasm for their counselors, and stated that a similar counselor serostatus was not necessary; however, two groups reported that a similar serostatus would render additional satisfaction. Two primary motivations reported for behavior change were concerns for health and money spent on drinking.
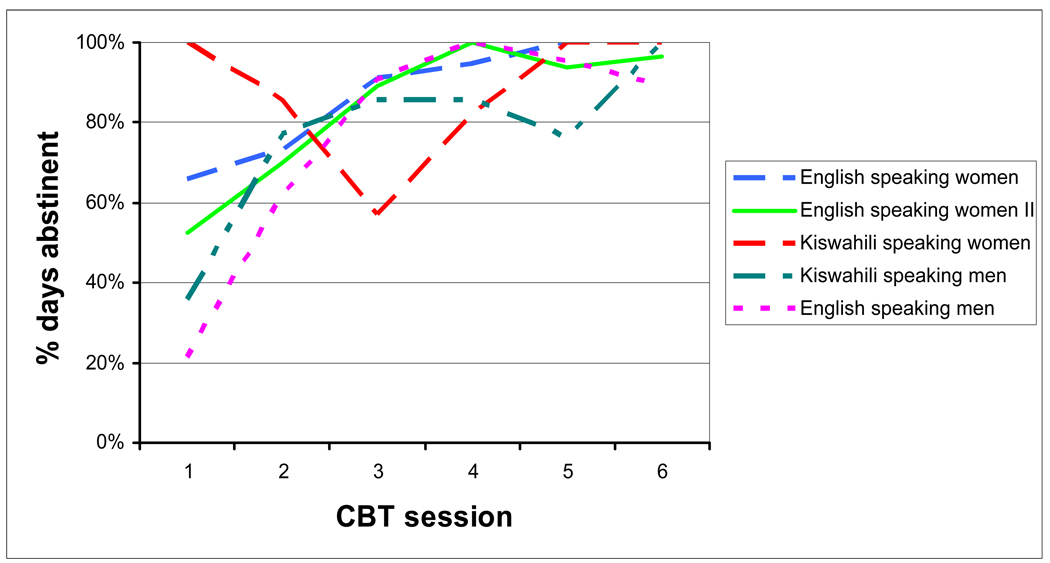
Alcohol use
In the three women’s groups, PDA ranged from 52% to 100% before session one (In one group, only one concurrently abstinent participant attended session one.) and from 96% to 100% before session six (Figure 2). In the two men’s groups, PDA ranged from 21% to 36% before session one, and from 89% to 100% before session six. All groups performed better at the conclusion of the CBT sessions, with mean immediate effect sizes of 2.32 for women and 2.64 for men. There were eight positive alcohol saliva tests among participants. Three tests were positive for a woman who enrolled in a pilot group, dropped out, joined the next pilot group and subsequently demonstrated negative test results. Five tests were positive for four participants, all of whom subsequently demonstrated negative test results.
Figure 2.
Mean reported abstinence from alcohol prior to each CBT session for five pilot groups
Discussion
This is the first published description of a systematic adaptation of CBT in a sub-Saharan African setting. Our adaptation was guided by two approaches that were combined to increase utility: Bernal’s heuristic framework for the focus of cultural dimensions of treatment,20 and the stage model of psychotherapy development for the process of adaptation.26 Together these approaches formed a paradigm of both focus and process for integrating Kenyan cultural adaptations into CBT. Results showed that Kenyan paraprofessional counselors were able to meet modest standards of CBT performance employed in U.S. CBT trials. Further, groups of both men and women reported substantial reductions in alcohol use over six sessions, demonstrating large immediate effects, and also reported satisfaction with the treatment. Together, these results suggest that CBT can be feasibly delivered by paraprofessionals and has promise for alcohol reduction among HIV-infected Kenyans with alcohol use disorders.
A key feature of our adaptation was the training of paraprofessionals to deliver group CBT, in an effort to both accommodate local levels of counseling resources as well as increase the potential for rollout should CBT be shown to be effective. While counselor training was comprehensive and lengthy (175–300 hours), it was relatively brief compared to U.S. standards of CBT delivery, where most counselors who deliver this treatment have a masters degree. Developing the Kenyan paraprofessional workforce to deliver addiction treatment services could have multiple positive public health ramifications.
Gender stratification was another feature of CBT delivery deemed necessary to avoid reinforcement of the secondary status of women and encourage their open discussion and engagement in treatment. Indeed, it is our clinical observation that this format facilitated discussion among women of sensitive issues such as transactional sex and disclosure issues.
One noteworthy diversion from our original plan was treatment delivery by counselors with an undisclosed serostatus. Although we thought delivery by an HIV-infected counselor would be necessary to gain trust, several indicators suggest success without serostatus disclosure. Counselors also gained credibility to sensitively contradict local myths about traditional brew. This trust was likely the product of several efforts. Counselors and staff appeared to be conferred a professional status (they were often called “daktari,” which means ‘doctor’ in Kiswahili), likely due to the project location in the AMPATH center on a medical campus, as well as the local goodwill established by the AMPATH collaboration. Counselors also made consistent endeavors to prevent misunderstandings during treatment, such as immediately correcting misinformation stated by one participant that medication given for alcohol withdrawal symptoms was poisoning clients. CBT also utilizes a professional delivery model not predicated on the counselor and client sharing the same presenting issues, in contrast to many peer delivery models. Finally, CBT cognitive techniques focus on examining evidence for beliefs to highlight any irrational beliefs, and are not predicated on the counselor having a shared experience per se.
Women and men in pilot groups and debriefings reported that learning about harmful effects of alcohol was motivating to reduce drinking. While many participants were unaware of consequences of drinking among HIV-infected persons, women in particular reported little prior knowledge about harmful effects of alcohol. Several men reported that discussion of the financial cost of drinking brew was influential in behavior change. Because traditional brew is often drunk as a cheaper alternative to commercial drink, our adaptation included an emphasis on financial cost of drinking in two ways. First, counselors reflected during various exercises (pros and cons of drinking, and unrealistic thinking) that participants reported lack of money as both a reason for drinking and a reason for quitting, and the subsequent contradiction between these two lines of thought. Second, staff assessed use of local brew by asking participants how much money they spent on it. Men reported these exercises increased their awareness of spending.
A limitation of our adaptation is that we did not specifically target risky sexual behavior in the intervention. Targeting alcohol as the first HIV risk behavior is consistent with a growing literature showing that alcohol reduction is needed for successful HIV prevention.11,12 Because paraprofessional delivery was exploratory, we also did not want to increase the number of sessions. Finally, we did not want to address risky sexual behavior without an understanding of the local influences on low condom use, considering the potential exacerbation of gender violence.41 It should be noted that counselors did highlight reports of risky sexual behaviors during the groups. There is some evidence that targeting substance abuse behaviors including alcohol results in reduced risky sexual behaviors.42 In the ongoing randomized trial, we also measure and will analyze both risky sexual behaviors and reasons for low condom use. Another limitation of our study is the self-report alcohol measure. However, our study also utilized the alcohol saliva test, which provides a point-prevalence objective measure of alcohol use.
Another potential limitation of our study was the longer than planned onsite time commitment (one year) by the PI. While local psychologists were initially planned to take over the supervision of the intervention, competing interests for time precluded this commitment. Nevertheless, although unplanned, the extended local stay resulted in a stronger local team for future projects, consistent with capacity-building efforts, including counselors who may function as future trainers. Finally, we acknowledge that the methods and results of this study conducted among clinical patients may not generalize to community residents.
Acknowledgments
This research was sponsored by NIAAA-funded R21AA016884, NIDA-funded P50DA09241 and supported in part by a grant to the USAID-AMPATH Partnership from the United States Agency for International Development as part of the President’s Emergency Plan for AIDS Relief. We acknowledge Emmanuel Wamalwa and Serah Chepseba for their assistance with data collection. We also thank Robert Skipworth Comer from the Indiana University School of Informatics for the contribution and development of locally relevant CBT illustrations. Finally, we extend our appreciation to Chematics, Inc. of North Webster, Indiana for the generous donation of alcohol saliva tests for this project.
Contributor Information
Rebecca K. Papas, Email: Rebecca_papas@brown.edu, Alpert Medical School of Brown University, Department of Psychiatry and Human Behavior, Providence, RI, USA.
John E. Sidle, Moi University School of Medicine, Department of Medicine, Eldoret, Kenya
Steve Martino, Yale University School of Medicine, Department of Psychiatry, New Haven, CT, USA.
Joyce B. Baliddawa, Moi University School of Medicine, Department of Behavioral Sciences, Eldoret, Kenya
Rogers Songole, Moi University School of Medicine, Department of Mental Health Services, Eldoret, Kenya.
Otieno E. Omolo, Moi University School of Medicine, Department of Mental Health Services, Eldoret, Kenya
Benson N. Gakinya, Moi University School of Medicine, Department of Mental Health Services, Eldoret, Kenya
Michael M. Mwaniki, Kenya Health Behavior Study, Eldoret, Kenya
Japheth O. Adina, Kenya Health Behavior Study, Eldoret, Kenya
Tobista Nafula, Kenya Health Behavior Study, Eldoret, Kenya.
Willis D. Owino-Ong’or, Moi University School of Medicine, Department of Medicine, Eldoret, Kenya
Kendall J. Bryant, National Institute of Alcohol Abuse and Alcoholism, Rockville, MD
Kathleen M. Carroll, Yale University School of Medicine, Department of Psychiatry, New Haven, CT, USA
Joseph L. Goulet, Yale University School of Medicine, Department of Medicine, New Haven, CT, USA
Amy C. Justice, Yale University School of Medicine, Department of Medicine, New Haven, CT, USA
Stephen A. Maisto, Syracuse University, Department of Psychology, Syracuse, NY, USA
Reference List
- 1.UNAIDS/WHO. Geneva: UNAIDS/WHO; AIDS epidemic update: December 2007.
- 2.Ayisi JG, van Eijk AM, ter Kuil OF, et al. Risk factors for HIV infection among asymptomatic pregnant women attending an antenatal clinic in western Kenya. Int J STD AIDS. 2000;11:393–401. doi: 10.1258/0956462001916119. [DOI] [PubMed] [Google Scholar]
- 3.Seage GR3, Holte S, Gross M, et al. Case-crossover study of partner and situational factors for unprotected sex. J Acquir Immune Defic Syndr. 2002;31:432–439. doi: 10.1097/00126334-200212010-00010. [DOI] [PubMed] [Google Scholar]
- 4.Braithwaite RS, McGinnis KA, Conigliaro J, et al. A temporal and dose-response association between alcohol consumption and medication adherence among veterans in care. Alcohol Clin Exp Res. 2005;29:1190–1197. doi: 10.1097/01.alc.0000171937.87731.28. [DOI] [PubMed] [Google Scholar]
- 5.Justice AC, Lasky E, McGinnis KA, et al. Comorbid disease and alcohol use among veterans with HIV infection: a comparison of measurement strategies. Med Care. 2006;44 Suppl 2:S52–S60. doi: 10.1097/01.mlr.0000228003.08925.8c. [DOI] [PubMed] [Google Scholar]
- 6.Othieno CJ, Kathuku DM, Ndetei DM. Substance abuse in outpatients attending rural and urban health centres in Kenya. East Afr Med J. 2000;77:592–595. doi: 10.4314/eamj.v77i11.46728. [DOI] [PubMed] [Google Scholar]
- 7.Saunders JB, Aasland OG, Amundsen A, Grant M. Alcohol consumption and related problems among primary health care patients: WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-I. Addiction. 1993;88:349–362. doi: 10.1111/j.1360-0443.1993.tb00822.x. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Geneva: WHO; Global Status Report on Alcohol 2004.
- 9.Papas RK, Sidle JE, Wamalwa ES, et al. Estimating alcohol content of traditional brew in western Kenya using culturally relevant methods: The case for cost over volume. AIDS Behav. doi: 10.1007/s10461-008-9492-z. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaffer DN, Njeri R, Justice AC, Odero WW, Tierney WM. Alcohol abuse among patients with and without HIV infection attending public clinics in western Kenya. East Afr Med J. 2004;81:594–598. [PubMed] [Google Scholar]
- 11.Kalichman SC, Simbayi LC, Vermaak R, et al. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Ann Behav Med. doi: 10.1007/s12160-008-9067-2. In press. [DOI] [PubMed] [Google Scholar]
- 12.Chesney MA, Donnell D, Seage GR, Bryant KL. Project EXPLORE: Impact of alcohol use on HIV sero-incidence among high-risk MSM in a large-scale prospective prevention intervention. Alcohol Clin Exp Res. 2009;33 Suppl 1 [Google Scholar]
- 13.Bandura A. Principles of Behavior Modification. New York: Holt, Rinehart & Winston; 1969. [Google Scholar]
- 14.Monti PM, Kadden RM, Rohsenow DJ, Cooney NL, Abrams DB. Treating Alcohol Dependence: A Coping Skills Training Guide. 2nd ed. New York: The Guilford Press; 2002. [Google Scholar]
- 15.Kadden RM, Cooney NL, Getter H, Litt MD. Matching alcoholics to coping skills or interactional therapy: Posttreatment results. J Consult Clin Psychol. 1989;57:698–704. doi: 10.1037//0022-006x.57.6.698. [DOI] [PubMed] [Google Scholar]
- 16.Miller WR, Zweben J, Johnson WR. Evidence-based treatment: Why, what, where, when and how? J Subst Abuse Treat. 2005;29:267–276. doi: 10.1016/j.jsat.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Project Match Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 18.Jones DL, Ross D, Weiss SM, Bhat G, Chitalu N. Influence of partner participation on sexual risk behavior reduction among HIV-positive Zambian women. J Urban Health. 2005;82(3 Suppl 4):iv92–iv100. doi: 10.1093/jurban/jti111. [DOI] [PubMed] [Google Scholar]
- 19.Osinowo HO, Olley BO, Adejumo AO. Evaluation of the effect of cognitive therapy on perioperative anxiety and depression among Nigerian surgical patients. West Afr J Med. 2003;22:338–342. doi: 10.4314/wajm.v22i4.28060. [DOI] [PubMed] [Google Scholar]
- 20.Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: Issues for cultural adaptation and development of psychosocial treatments with Hispanics. J Abnorm Child Psychol. 1995;23:67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- 21.Sue S, Zane N. The role of culture and cultural techniques in psychotherapy. A critique and reformulation. Am Psychol. 1987;42:37–45. doi: 10.1037//0003-066x.42.1.37. [DOI] [PubMed] [Google Scholar]
- 22.Hall GCN. Psychotherapy research with ethnic minorities: Empirical, ethical and conceptual issues. J Consult Clin Psychol. 2001;69:502–510. doi: 10.1037//0022-006x.69.3.502. [DOI] [PubMed] [Google Scholar]
- 23.Betz NE, Fitzgerald LF. Individual and diversity: Theory and research in counseling psychology. Annu Rev Psychol. 1993;44:343–381. doi: 10.1146/annurev.ps.44.020193.002015. [DOI] [PubMed] [Google Scholar]
- 24.Ramirez M. Multicultural psychotherapy: An approach to individual and cultural differences. Boston: Allyn & Bacon; 1999. [Google Scholar]
- 25.Sue DW, Ivey AE, Petersen PB. A Theory of Multicultural Counseling and Therapy. Pacific Grove, CA: Brooks and Cole; 1996. [Google Scholar]
- 26.Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clin Psychol Sci Pract. 2001;8:133–142. [Google Scholar]
- 27.National AIDS and STI Programme, Ministry of Health Kenya. Nairobi, Kenya: Kenya AIDS Indicator Survey 2007: Preliminary Report.
- 28.Einterz RM, Kimaiyo S, Mengech HNK, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82:818. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 29.National AIDS Control Council, Office of the President Kenya. Nairobi: NACC; UNGASS 2008 Country Report for Kenya.
- 30.Central Intelligence Agency. [Accessed August 2, 2009];CIA - The World Factbook - Kenya. Available at: https://www.cia.gov/library/publications/the-world-factbook/geos/ke.html.
- 31.World Bank. Washington, DC: World Bank; World Development Report. 2002
- 32.Njenga FG, Kigamwa PA. Mental health policy and programmes in Kenya. London: Royal College of Psychiatrists. Bulletin of the Board of International Affairs of the Royal College of Psychiatrists; 2005. [PMC free article] [PubMed] [Google Scholar]
- 33.Ayuku D, Odero W, Kaplan C, De Bruyn R, De Vries M. Social network analysis for health and social interventions among Kenyan scavenging street children. Health Policy Plan. 2003;18:109–118. doi: 10.1093/heapol/18.1.109. [DOI] [PubMed] [Google Scholar]
- 34.POLICY Project - Kenya. From Despair to Hope: Women's Right to Own and Inherit Property. Nairobi, Kenya: POLICY Project - Kenya; Kenya National Commission on Human Rights; 2005. [Google Scholar]
- 35.Carroll KM, Nich C, Sifry RL, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- 36.Sobell LC, Sobell MB. Timeline Followback: A Technique for Assessing Self-Reported Alcohol Consumption. In: Litten RZ, Allen J, editors. Measuring Alcohol Consumption. 1st ed. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 37.Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-Ar) Brit J Addiction. 1989;84:1353–1357. doi: 10.1111/j.1360-0443.1989.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 38.Chematics, Inc. Alco-Screen Technical Information. North Webster, Indiana: Chematics, Inc.; 2004. [Google Scholar]
- 39.World Health Organization. [Accessed August 12, 2009];WHO - Process of translation and adaptation of instruments. Available at: http://www.who.int/substance_abuse/research_tools/translation/en/index.html.
- 40.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 41.Alio AP, Daley EM, Nana PN, Duan J, Salihu HM. Intimate partner violence and contraception use among women in Sub-Saharan Africa. Int J Gynecol Obstet. doi: 10.1016/j.ijgo.2009.05.002. In press. [DOI] [PubMed] [Google Scholar]
- 42.Carey MP, Carey KB, Maisto SA, Gordon CM, Schroeder KEE, Vanable PA. Reducing HIV risk behavior among adults receiving outpatient psychiatric treatment: results from a randomized controlled trial. J Consult Clin Psychol. 2004;72:252–268. doi: 10.1037/0022-006X.72.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]