Abstract
Suboptimum blood pressure is estimated to be the leading risk factor for death worldwide and is associated with 13.5% of deaths globally. The clinical diagnosis of hypertension affects one in four adults globally and is expected to increase by 60% between 2000 and 2025. Clearly, global efforts to prevent and control hypertension are important health issues. While Canada had a prevalence of hypertension similar to that of the United States in the early 1990s, the treatment and control rate was only 13% compared with 25% in the United States. A national strategic plan was developed, and a coalition of organizations and health care professional and scientist volunteers actively implemented parts of the strategy. Specific initiatives that have evolved include the development of hypertension knowledge translation programs for health professionals, the public and people with hypertension, an outcomes research program to assess the impact of hypertension and guide national-, regional- and community-based knowledge translation interventions, and a program to reduce the prevalence of hypertension by decreasing sodium additives in food. These initiatives have relied on the active involvement of health care professional volunteers, health care professional and scientific organizations and various government departments. There have been large increases in the diagnosis and treatment of hypertension, with corresponding reductions in cardiovascular disease and total mortality associated with the start of the hypertension initiatives. As a result, Canada is becoming recognized as a world leader in the prevention, treatment and control of hypertension.
Keywords: Education, Epidemiology, High blood pressure, Hypertension, Knowledge translation
Abstract
On estime qu’une tension artérielle sous-optimale est le principal facteur de risque de décès et s’associe à 13,5 % des décès sur la scène mondiale. Le diagnostic clinique d’hypertension touche un adulte sur quatre sur la planète et devrait augmenter de 60 % entre 2000 et 2025. De toute évidence, les efforts mondiaux pour prévenir et contrôler l’hypertension constituent d’importants enjeux de santé. Tandis que le Canada avait une prévalence d’hypertension similaire à celle des États-Unis au début des années 1990, le taux de traitement et de contrôle s’élevait seulement à 13 % par rapport à 25 % aux États-Unis. On a élaboré un plan stratégique national, et une coalition d’organisations et de professionnels de la santé et scientifiques bénévoles ont mis en œuvre des volets de la stratégie. Des initiatives spécifiques ont évolué, dont l’élaboration de programmes de transfert du savoir sur l’hypertension pour les professionnels de la santé, le public et les hypertensifs, un programme de recherche sur les issues pour évaluer les répercussions de l’hypertension et orienter les interventions de transfert du savoir nationales, régionales et communautaires, ainsi qu’un programme pour réduire la prévalence d’hypertension en diminuant les ajouts de sodium dans les aliments. Ces initiatives se fondaient sur la participation active de professionnels de la santé bénévoles, de professionnels de la santé et d’organisations scientifiques ainsi que sur divers ministères du gouvernement. On constate de fortes augmentations du diagnostic et du traitement de l’hypertension et des réductions correspondantes de maladies cardiovasculaires et de mortalité totale associées à l’amorce des initiatives liées à l’hypertension. Par conséquent, le Canada se taille une place comme chef de file mondial de la prévention, du traitement et du contrôle de l’hypertension.
Increased blood pressure is estimated by the WHO to be the leading risk factor for death, and is associated with 7.6 million deaths per year (13.5% of deaths worldwide) (1). Hypertension has a high prevalence in the developed world, estimated at one in five to one in three adults (2). Fifty-four per cent of strokes and 47% of cardiac deaths are attributed to suboptimal blood pressure control (1). Approximately 20% of chronic kidney failure is caused by hypertension and 40% by diabetes (although it is noteworthy that one-half of chronic kidney failure in diabetic individuals is caused by increased blood pressure; hence, at least 40% of chronic kidney failure is caused by hypertension) (3). In the Framingham study (4–6), 91% of heart failures, 84% of strokes and 70% of myocardial infarctions occurred in hypertensive individuals. Recently, it has been estimated that increased blood pressure accounts for US$370 billion in health care costs worldwide and, in developed countries, accounts for approximately 10% of overall direct health costs (7). Indirect costs are estimated at US$3.6 trillion worldwide. Clearly, hypertension and elevated blood pressure within the ‘normotensive’ range should represent a major national and international health priority. Unfortunately, this is not the case and, as a consequence, many people with hypertension are unaware, untreated or undertreated. The vast majority of individuals with hypertension are uncontrolled.
Historically, in Canada and other countries, the detection and management of hypertension has been dismal (2). In the past, many Canadians with hypertension were not diagnosed, most were not treated and of those who were treated, relatively few were treated to the recommended blood pressure targets (8). National surveys conducted in the 1980s and early 1990s found that relative to Americans with hypertension, Canadians were more likely to be unaware that their blood pressure was high, to not be treated and to have uncontrolled blood pressure (8). The treatment and control rate in Canada was 13%, while in the United States the treatment and control rate was 25% (8). The disparity in hypertension awareness, treatment and control led to extensive discussions between the Public Health Agency of Canada (PHAC, formerly Health Canada), the Heart and Stroke Foundation of Canada, the Canadian Hypertension Society, and Blood Pressure Canada (formerly the Canadian Coalition for High Blood Pressure Prevention and Control) on what needed to be accomplished. Suffice to say, the reasons for national disparity in hypertension prevention and control were uncertain, translational medicine was not topical and there was little interventional or observational data on which to guide the creation of national programs to improve hypertension awareness, treatment and control. The discussions resulted in the development of a national strategic plan for hypertension prevention and control (9) followed by a knowledge translation program for health care professionals (the Canadian Hypertension Education Program [CHEP]) (10). More recent developments have included the development of an outcomes research program to assess and guide knowledge translation initiatives (11), a national leadership position (the Canadian Chair in Hypertension Prevention and Control) (12), a public and patient hypertension knowledge translation program to improve self-efficacy in the prevention and management of hypertension (13), and an advocacy and education program to reduce the addition of sodium to food to prevent hypertension. The present article reviews these developments and the associated outcomes that have resulted in Canada becoming recognized as a world leader in hypertension prevention and control (14).
In the mid 1990s, Health Canada provided a grant and logistic support to Blood Pressure Canada to develop a national strategic plan for the prevention and control of hypertension in Canada (9). Implementing the overall plan relied heavily on extensive resource support from federal and provincial governments, which was never actualized. However, an implementation committee was formed to operationalize components of the plan that were deemed feasible. Two separate interventions resulted. One intervention was to develop an annually updated education program (CHEP) based on recommendations to improve the management of hypertension by health care professionals (15). The second initiative was a social marketing intervention to improve public knowledge on hypertension. An extensive pilot of the social marketing strategy was expensive and resulted in only a small short-term change in public knowledge (15) and, therefore, was discontinued. In 2006, a National Chair in Hypertension Prevention and Control was initiated to provide a funded leadership position for hypertension initiatives (12). The Chair funding facilitated the development of a public education initiative and a program to reduce sodium additives in food as well as enhancements to existing programs.
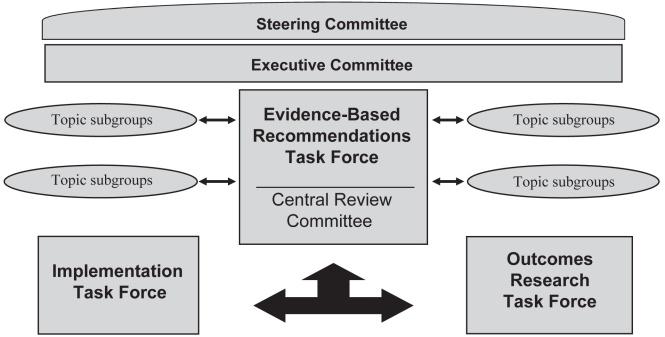
The CHEP currently represents an extensive partnership of health care professional and health scientist volunteers, government, nongovernment and national health and scientific organizations to improve clinical hypertension management in Canada (16). The Steering Committee has active representation from the national primary care professional associations (the College of Family Physicians of Canada, the Canadian Council of Cardiovascular Nurses and the Canadian Pharmacists Association). CHEP was developed to be a more systematic and rigorous, evidence-based medicine process than previous hypertension recommendations processes. In addition, CHEP was innovative in creating a separate interdisciplinary knowledge translation process and, later, a comprehensive evaluation process. The separate processes for developing recommendations (Recommendations Task Force), knowledge translation (Implementation Task Force) and evaluation (Outcomes Research Task Force) are run by chairs and vice-chairs and, together, these individuals form an executive committee that oversees the day-to-day functions of CHEP. The CHEP structure is shown in Figure 1.
Figure 1).
The structure of the Canadian Hypertension Education Program (CHEP). The Steering Committee includes the Canadian Hypertension Society, Blood Pressure Canada, The Public Health Agency of Canada, The Heart and Stroke Foundation of Canada, The College of Family Physicians of Canada, the Canadian Council of Cardiovascular Nurses and the Canadian Pharmacists Association, plus the co-chairs of the Task Forces. There are more than 100 volunteers involved with CHEP. Figure reproduced with permission of CHEP
Currently, the Recommendations Task Force is divided into 15 subgroups that review literature and develop draft management recommendations on topics important to the treatment and control of hypertension (www.hypertension.ca) (17,18). Each year, the subgroups perform critical reviews of the evidence based on systematic literature searches performed by a Cochrane librarian, and develop and revise management recommendations. A committee of experts in evidence-based medicine (the Central Review Committee) oversee the incorporation of evidence into the recommendations to ensure that a consistent standardized approach is used. Members of the Central Review Committee have no financial conflicts of interest. The evidence and draft recommendations are reviewed and discussed annually by the full Recommendations Task Force with the purpose of achieving consensus. The full Recommendations Task Force and Executive vote on the draft recommendations; only recommendations that achieve more than 70% support are adopted.
Following the finalization of the annual recommendations, the CHEP executive updates ‘core’ education resources and selects a theme. The core resources include four to eight ‘key messages’ to highlight the essential aspects of hypertension management, a one-page summary, a short clinical and scientific summary as well as six PowerPoint (Microsoft Corporation, USA) slide sets. All resources feature the year’s theme, which is selected to highlight an important clinical care ‘gap’. The Central Review Committee also annually updates comprehensive scientific documents that outline the specific management recommendations and their scientific rationale. An Implementation Task Force formed with members who have primary care, education and knowledge translation expertise, tailor the core education resources to be relevant to primary care and assist in dissemination.
Recently, a survey (unpublished) of primary care practitioners found substantial hypertension knowledge gaps, and that many were not aware of the hypertension recommendations. Therefore, in 2010, CHEP will focus on new and enhanced methods of knowledge translation to primary care providers. Specifically, a website has been developed (www.htnupdate.ca) that allows health care professionals or organizations to register for electronic updates when new or updated material becomes available. In addition, an interactive Internet-based lecture series on important hypertension topics is being developed, as well as more extensive training sessions to develop community hypertension experts and leaders. To receive notices, the reader can register at www.htnupdate.ca.
The CHEP also developed an Outcomes Research Task Force to assist governments in the development of a national hypertension surveillance program to examine the impact of the CHEP program and to identify gaps in clinical care. Much of the surveillance data gathered suggest that CHEP has had a major impact on the management and outcomes of hypertensive Canadians. The start of the CHEP program was associated with very large increases in diagnosis and treatment of hypertension, and by a reduction in total and cardiovascular mortality (19–22). In Ontario, the treatment and control rate for hypertension increased more than fivefold – from 12% to 66% (23). Table 1 provides an update of the prevalence of diagnosed and treated hypertension in Canada using previously published methods from the Canadian Community Health Survey (24). In 2007, there were slightly more than 4.8 million Canadians diagnosed with hypertension, and almost nine in 10 of those diagnosed were taking antihypertensive drugs. An indication of the extent of treatment is the observation that 46% of Canadian women 60 years of age and older are taking antihypertensive medications.
TABLE 1.
Number and percentage of adult Canadians reporting a diagnosis or treatment for hypertension
|
Hypertension rates among population ≥20 years of age, % |
Individuals with hypertension |
|||
|---|---|---|---|---|
| Province | Diagnosed | Treated | Diagnosed, n | Treated, n (%) |
| Newfoundland and Labrador | 25.3 | 23.3 | 100,218 | 92,303 (92.1) |
| Prince Edward Island | 21.3 | 19.8 | 22,227 | 20,729 (93.3) |
| Nova Scotia | 22.3 | 20.2 | 162,092 | 146,659 (90.5) |
| New Brunswick | 22.8 | 20.3 | 132,286 | 117,490 (88.8) |
| Quebec | 19.0 | 17.5 | 1,132,654 | 1,041,552 (92.0) |
| Ontario | 20.0 | 17.5 | 1,933,704 | 1,691,287 (87.5) |
| Manitoba | 19.6 | 17.8 | 172,285 | 156,064 (90.6) |
| Saskatchewan | 21.0 | 18.8 | 154,035 | 137,825 (89.5) |
| Alberta | 16.8 | 14.3 | 438,788 | 373,810 (85.2) |
| British Columbia | 17.0 | 14.8 | 566,240 | 492,940 (87.1) |
| Yukon | 17.7 | 14.0 | 4327 | 3419 (79.0) |
| Northwest Territories | 13.8 | 9.6 | 4119 | 2859 (69.4) |
| Nunavut | 8.0 | 4.8 | 1412 | 851 (60.3) |
| Canada | 19.2 | 17.1 | 4,825,324 | 4,278,738 (88.7) |
Data from reference 24
In 2010, Statistics Canada will release the results of a national physical measures survey that indicates the prevalence of hypertension as well as the rate of awareness of the diagnosis, and treatment and control rates. Also in 2010, a joint Statistics Canada-PHAC survey will report on the knowledge, attitudes and behaviours of hypertensive Canadians. In 2010, PHAC will also release the first analysis of the prevalence and incidence of diagnosed hypertension in Canada along with mortality rates. CHEP continues to work on methodology that will enable PHAC and the provinces to link administrative databases to track the diagnosis and treatment of hypertension and specific outcomes. The enhanced methods should be available by 2011 and will potentially enable PHAC to track the full population of Canadians who are diagnosed as hypertensive.
In 2006, Blood Pressure Canada started a comprehensive program to educate Canadians about hypertension and, particularly for Canadians with hypertension, on how to manage their condition (13). The education program is based on the CHEP health care professional recommendations. An extensive array of resources have been developed and disseminated by a Public Education Task Force (www.hypertension.ca/bpc). The Task Force has more than 30 health care professional volunteers who develop and annually update public and patient hypertension education resources. In 2010, a hypertension patient association will be formed and will electronically update Canadians with hypertension. Patients will be able to register at www.myBPsite.ca.
In addition, Canada has a well-organized effort to reduce sodium additives to food to decrease the prevalence of hypertension and to improve blood pressure control. Although started by a group of concerned health care professionals and national health organizations, the effort is now led by a Health Canada Intersectoral Working Group that is tasked with reducing dietary sodium to levels that are currently recommended for good health. The initiative is based on voluntary reductions of sodium additives to food by the food industry, with strong government oversight. In addition, the Working Group is tasked with ensuring Canadians are educated about the health risks of high dietary sodium and the health benefits of reducing dietary sodium, and to ensuring that the required research to lower sodium intake to desired levels is conducted. A report from the Working Group is expected in 2010. It is conservatively estimated that reducing dietary sodium to recommended levels will reduce the prevalence of hypertension by 30%, double the treatment and control rate and reduce cardiovascular disease by more than 8%, while saving approximately $2 billion dollars per year in health care costs (25,26). A Blood Pressure Canada Committee composed of more than 20 health care professionals has developed extensive resources (www.lowersodium.ca) to aid both health care professionals and patients become knowledgeable about the health consequences of high dietary sodium and how to reduce dietary sodium.
CONCLUSIONS
The Canadian hypertension community has led the development of programs for the prevention of hypertension, improvement of hypertension knowledge and awareness among Canadians, and improvement of hypertension treatment and control by health care professionals. Collaboration with government is establishing an extensive surveillance program, and initial evaluation has found significant increases in the rates of diagnosis and treatment of hypertension in Canada following educational efforts. Several of the initiatives were started in the past few years and, therefore, it is anticipated that there will be continued improvements in the treatment and control of hypertension, reduced or stable prevalence and, most importantly, reduced complications.
GRANT ACKNOWLEDGEMENT:
Drs N Campbell and G Chen acknowledge the Canadian Institutes of Health Research for their support of the Canada Chair in Hypertension Prevention and Control.
REFERENCES
- 1.Lawes CM, Vander HS, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: A systematic review. J Hypertens. 2004;22:11–9. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Bild D, Teutsch SM. The control of hypertension in persons with diabetes: A public health approach. Public Health Rep. 1987;102:522–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KKL. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62. [PubMed] [Google Scholar]
- 5.Kannel WB, Wolf PA, Verter J, McNamara PM. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham Study. JAMA. 1970;214:301–10. [PubMed] [Google Scholar]
- 6.Haider AW, Chen L, Larson MG, Evans JC, Chen MH, Levy D. Antecedent hypertension confers increased risk for adverse outcomes after initial myocardial infarction. Hypertension. 1997;30:1020–4. doi: 10.1161/01.hyp.30.5.1020. [DOI] [PubMed] [Google Scholar]
- 7.Gaziano TA, Bitton A, Anand S, Weinstein MC. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–77. doi: 10.1097/HJH.0b013e32832a9ba3. [DOI] [PubMed] [Google Scholar]
- 8.Joffres MR, Hamet P, MacLean DR, L’Italien GJ, Fodor G. Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens. 2001;14:1099–105. doi: 10.1016/s0895-7061(01)02211-7. [DOI] [PubMed] [Google Scholar]
- 9.Chockalingam A, Campbell N, Ruddy T, Taylor G, Stewart P. Canadian National High Blood Pressure Prevention and Control Strategy. Can J Cardiol. 2000;16:1087–93. [PubMed] [Google Scholar]
- 10.Zarnke KB, Campbell NRC, McAlister FA, Levine M. A novel process for updating recommendations for managing hypertension: Rationale and methods. Can J Cardiol. 2000;16:1094–102. [PubMed] [Google Scholar]
- 11.Campbell NR, Onysko J. The Outcomes Research Task Force and the Canadian Hypertension Education Program. Can J Cardiol. 2006;22:556–8. doi: 10.1016/s0828-282x(06)70276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campbell NRC. Canada Chair in hypertension prevention and control: A pilot project. Can J Cardiol. 2007;23:557–60. doi: 10.1016/s0828-282x(07)70800-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell NR, Petrella R, Kaczorowski J. Public education on hypertension: A new initiative to improve the prevention, treatment and control of hypertension in Canada. Can J Cardiol. 2006;22:599–603. doi: 10.1016/s0828-282x(06)70282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Califf RM. A virtuous cycle to improve hypertension outcomes at a national level: Linking public health and individualized medicine. Hypertension. 2009;53:105–7. doi: 10.1161/HYPERTENSIONAHA.108.121608. [DOI] [PubMed] [Google Scholar]
- 15.Petrella RJ, Speechley M, Kleinstiver PW, Ruddy T. Impact of a social marketing media campaign on public awareness of hypertension. Am J Hypertens. 2005;18:270–5. doi: 10.1016/j.amjhyper.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Campbel NRC. Hypertension prevention and control in Canada. J Am Soc Hypertens. 2008;2:97–105. doi: 10.1016/j.jash.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Khan NA, Hemmelgarn B, Herman RJ, et al. The 2009 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 2 – therapy. Can J Cardiol. 2009;25:287–98. doi: 10.1016/s0828-282x(09)70492-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAlister FA. The Canadian Hypertension Education Program – A unique Canadian initiative. Can J Cardiol. 2006;22:559–64. doi: 10.1016/s0828-282x(06)70277-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onysko J, Maxwell C, Eliasziw M, Zhang J, Johansen H, Campbell N. Large increases in hypertension diagnosis and treatment in Canada following a health care professional education program. Hypertension. 2006;48:853–60. doi: 10.1161/01.HYP.0000242335.32890.c6. [DOI] [PubMed] [Google Scholar]
- 20.Hemmelgarn BR, Chen G, Walker R, et al. Trends in antihypertensive drug prescriptions and physician visits in Canada between 1996 and 2006. Can J Cardiol. 2008;24:507–12. doi: 10.1016/s0828-282x(08)70627-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell NR, Brant R, Johansen H, et al. Increases in antihypertensive prescriptions and reductions in cardiovascular events in Canada. Hypertension. 2009;53:128–34. doi: 10.1161/HYPERTENSIONAHA.108.119784. [DOI] [PubMed] [Google Scholar]
- 22.McAlister FA, Feldman RD, Wyard K, Brant R, Campbell NR. The impact of the CHEP in its first decade. Eur Heart J. 2009;30:1434–9. doi: 10.1093/eurheartj/ehp192. [DOI] [PubMed] [Google Scholar]
- 23.Leenen FH, Dumais J, McInnis NH, et al. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ. 2008;178:1441–49. doi: 10.1503/cmaj.071340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell NR, So L, Amankwah E, Quan H, Maxwell C. Characteristics of hypertensive Canadians not receiving drug therapy. Can J Cardiol. 2008;24:485–90. doi: 10.1016/s0828-282x(08)70623-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Penz ED, Joffres MR, Campbell NR. Reducing dietary sodium and decreases in cardiovascular disease in Canada. Can J Cardiol. 2008;24:497–501. doi: 10.1016/s0828-282x(08)70625-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joffres M, Campbell NRC, Manns B, Tu K. Estimate of the benefits of a population-based reduction in dietary sodium additives on hypertension and its related health care costs in Canada. Can J Cardiol. 2007;23:437–43. doi: 10.1016/s0828-282x(07)70780-8. [DOI] [PMC free article] [PubMed] [Google Scholar]