Abstract
Objectives
To identify and compare predictors of job satisfaction between the instructional and clinical faculty tracks.
Method
A 61-item faculty job satisfaction survey was distributed to 1,898 academic faculty at the University of Michigan Medical School. The anonymous survey was web-based. Questions covered topics on departmental organization, research, clinical and teaching support, compensation, mentorship, and promotion. Levels of satisfaction were contrasted between the two tracks, and predictors of job satisfaction were identified using linear regression models.
Results
The response rates for the instructional and clinical tracks were 43.1% and 41.3%, respectively. Clinical faculty reported being less satisfied with how they are mentored, and fewer reported understanding the process for promotion. There was no significant difference in overall job satisfaction between faculty tracks. Surprisingly, clinical faculty with mentors were significantly less satisfied with how they were being mentored, with career advancement and overall job satisfaction, compared to instructional faculty mentees. Additionally, senior-level clinical faculty were significantly less satisfied with their opportunities to mentor junior faculty compared to senior-level instructional faculty. Significant predictors of job satisfaction for both tracks included areas of autonomy, meeting career expectations, work-life balance, and departmental leadership. Unique to the clinical track, compensation and career advancement variables also emerged as significant predictors.
Conclusion
Greater effort must be placed in the continued attention to faculty well-being both at the institutional level and at the level of departmental leadership. Success in enhancing job satisfaction is more likely if directed by locally designed assessments involving department chairs, specifically in fostering more effective mentoring relationships focused on making available career advancement activities such as research activities. Our findings show this strategy to significantly impact the job satisfaction and retention of clinical track faculty members.
Critical to the infrastructure of a strong academic medical center is the medical faculty. Attention to job satisfaction of academic medical faculty has gained national attention in part due to the current economic climate in which recruitment of faculty to replace those who leave is costly. Recent national survey data from the American Association of Medical Colleges (AAMC) reported a staggering 38–40% attrition rate of academic medical faculty over a ten year period.1 Because faculty retention and job satisfaction are intimately linked, understanding what drives and satisfies academic medical faculty is invaluable for providing continuos and quality patient care,2 teaching the next generation of physicians, and minimizing the high cost of recruiting new faculty.3, 4
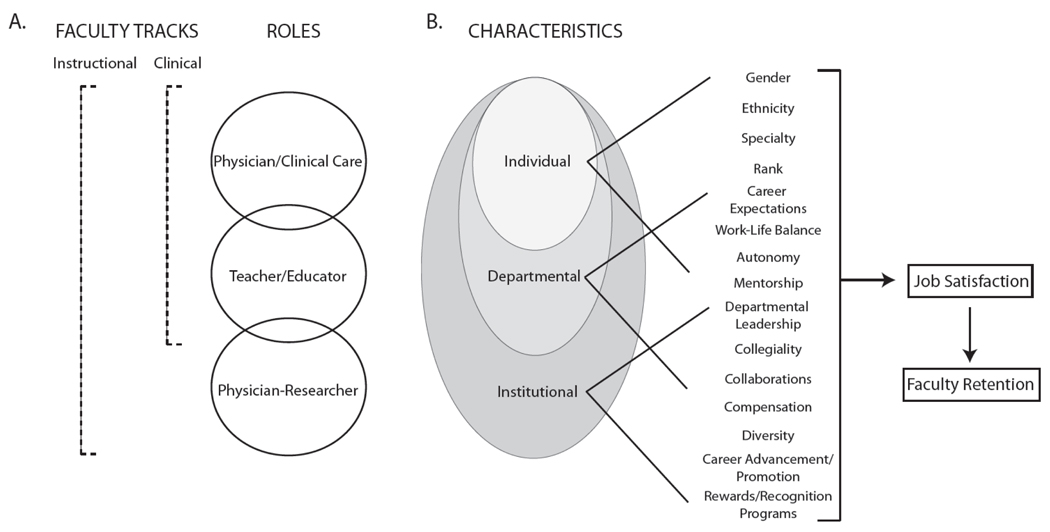
Despite being a relatively new track, the number of clinical track faculty is currently nearly comparable with the instructional track, which emphasizes the traditional tripartite missions of patient care, research and teaching.5 By contrast, the clinical track’s primary missions are in patient care and teaching (Figure 1A). This striking increase in the non-tenure clinical track faculty reflects a national trend6 and makes retention of faculty in the clinical track equally important to retention in the instructional track, so that an academic medical center can meet its responsibilities to its patients and maintain financial stability.
Figure 1.
Conceptual Framework for Comparing Instructional and Clinical Track Faculty Job Satisfaction
Because the clinical track is structurally different from the instructional track, we sought to identify and contrast predictors of job satisfaction between the two tracks by conducting a medical school faculty survey. We designed a conceptual framework7 to illustrate the overlapping yet distinct roles of an academic faculty member, representing the track’s primary responsibilities (Figure 1A) and categorized overlapping individual, departmental and institutional characteristics previously described in the literature as influencing faculty job satisfaction (Figure 1B). Academic medical faculty surveys have been used to examine differences in job satisfaction among clinical track faculty,8 to investigate gender differences,9, 10 or all academic medical faculty,11–14 and have suggested that job satisfaction is largely related to autonomy,13 work-life balance,10, 15 departmental leadership,11 salary compensation,11, 13 and having a mentor.16, 17 Our conceptual framework is structured to reflect these findings from these previous studies, which describe characteristics that can be derived from varying hierarchical levels as well as literature supporting a strong association between job satisfaction with faculty retention.11
To our knowledge, no prior study has directly compared predictors of job satisfaction between the two faculty tracks despite the differing primary missions. We formulated the following hypotheses: (1) similar areas of job satisfaction will emerge for both faculty tracks due to overlapping missions of teaching and patient care, and (2) because of the different expectations of the instructional and clinical faculty tracks, predictors of job satisfaction will vary and different strategies will need to be proposed for each faculty track to enhance faculty satisfaction.
METHODS
This anonymous web-based satisfaction survey18 was conducted during November and December 2008 at UMMS. Academic medical faculty members were informed that the online survey tool would not track any electronic information and confidentiality was assured. Faculty members were also given the option of completing the survey on paper and having staff enter the data confidentially. Eight-weeks were allotted for the completion of the survey. One email was sent to inform faculty members about the survey and a second email to encourage participation.
Ethics
The survey was considered a non-regulated application by the Institutional Review Board because no private health information was collected and approval was given to analyze the collected data.
Sample
The target population included all faculty members at UMMS holding an appointment as an assistant, associate, or full professor. Faculty were asked to identify themselves as being in the instructional, clinical, or research tracks. However, only data from the instructional and clinical track faculty were used for analysis due to the low response rate from the research track (see Results). Clinical lecturers and adjunct or visiting professors were excluded from analyses.
Survey Instrument
The UMMS Faculty Survey was piloted in prior years to the medical faculty and a modified version was utilized in 2008. The survey included 11 demographic questions addressing gender, ethnicity, academic rank, faculty track, degree, specialty, length of service at UMMS, and whether they previously held an appointment at one or more academic medical centers. Three questions identified the extent of teaching, clinical activities, and research activities.
The remaining 47 questions were designed to measure faculty satisfaction in areas of overall job satisfaction, departmental leadership, clinical activities, research activities, teaching role, career advancement, mentorship, and compensation.
Statistical Analysis
The survey response rate was calculated by the number of respondents divided by the total number of faculty present in 2008. Respondents who started but did not complete at least half of the survey questions were excluded from all analyses. Chi-square analysis was used to test for differences in demographic variables between the false-starters and survey respondents. Independent two-sample Student’s t-test was used to compare mean satisfaction scores between faculty tracks, and significance level was set at p<0.05.
Exploratory factor analysis was performed to reduce and categorize a large number of variables into fewer domains (i.e. factors) that have common and related characteristics.19 Several rounds of factor analyses were performed until no variables with factor loadings less than 0.45 remained. Cronbach’s α indexes were calculated to test the internal reliability of each factor derived from factor analysis. Excluded questions were reviewed, and questions of relevance to job satisfaction (e.g., promotion16 and mentorship8, 14, 17) were identified. The final regression models predicted job satisfaction separately for each track with job satisfaction as the dependent (outcome) variable. Each model included the factors derived from the factor analysis, gender, ethnicity, rank, and relevant promotion, mentorship, and research related questions. STATA (Special Edition 11.0, Statacorp, College Station, Texas, 2010) and SPSS (PASW Statistic 17.0.3, Chicago, Illinois, 2009) statistics software were used for analyses.
RESULTS
Demographic Information
The complete response rate for the UMMS Faculty Survey in 2008 was 41.3% (n=783 of 1,898 eligible faculty members). By faculty track, the response rate was 43.1% (n=353 of 819) among the instructional track faculty, 46.7 % (n=360 of 771) among the clinical track faculty, and 22.7% (n=70 of 308) among the research track faculty. Because of the low response rate, data from research track faculty were excluded from further analyses. In addition, no statistically significant differences emerged in any of the demographic variables between the false-starters and survey respondents. The proportions of gender, rank (assistant versus associate versus full professors), specialty choices and ethnicity were significantly different between the instructional and clinical track faculty (Table 1).
Table 1.
Characteristics of Two Faculty Cohorts at the University of Michigan Medical School in 2008
| Characteristics | Faculty Track§ | p-value | |
|---|---|---|---|
| Instructional Track |
Clinical Track |
||
| Gender | <0.0001* | ||
| Male | 76% (n=246) | 57% (n=195) | |
| Female | 24% (n=79) | 43% (n=146) | |
| Degree† | |||
| M.D. | 42% (n=232) | 58% (n=322) | |
| Ph.D. | 76% (n=157) | 24% (n=49) | |
| Rank | <0.0001* | ||
| Assistant Professor | 19% (n=68) | 66% (n=238) | |
| Associate Professor | 25% (n=89) | 22% (n=78) | |
| Full Professor | 56% (n=196) | 12% (n=44) | |
| Specialty| | <0.0001* | ||
| Medical | 57% (n=184) | 84% (n=287) | |
| Surgical | 27% (n=86) | 15% (n=51) | |
| Basic Science | 16% (n=53) | 1% (n=5) | |
| Ethnicity | 0.4492 | ||
| White | 86% (n=272) | 82% (n=265) | |
| Non-White‡ | 14% (n=46) | 18% (n=59) | |
Research track was not reported due to the low response rate 22.7% (n=70/308 faculty).
Because some faculty members have dual degrees (e.g. MD/PhD), the percentages exceed 100%. No statistical test was performed because the groups were not mutually exclusive.
Non-white ethnic groups consist of Arab, Asian, Black/African American, Hispanic/Latino, and multiple ethnic groups.
p<0.0001, Chi-square analysis of independence was performed to test differences between proportions in the instructional and clinical track.
Medical: Dermatology, neurology, physical medicine and rehabilitation, psychiatry, anesthesiology, emergency medicine, pathology, radiation oncology, radiology, Family medicine, internal medicine, pediatrics and communicable diseases
Surgical: Neurosurgery, obstetrics & gynecology, ophthalmology, orthopaedic surgery, general surgery, urology
Basic Science: Anatomical sciences, bioinformatics, biological chemistry, cell and developmental biology, human genetics, microbiology and immunology, molecular and integrative physiology, pharmacology, unit for laboratory animal medicine
Areas of satisfaction
Table 2 summarizes mean satisfaction scores between the instructional and clinical track faculty on areas of job satisfaction, teaching and research support, career advancement, collaboration, mentorship and compensation. Generally, mean scores for clinical track faculty were lower compared to instructional track faculty but were significantly lower in areas of research support, career advancement, satisfaction with collaborations, and mentorship.
Table 2.
Satisfaction Score of 353 Instructional and 360 Clinical Track Faculty at the University of Michigan Medical School in 2008
| Question‡ | Instructional Track |
Clinical Track |
p-value |
|---|---|---|---|
| Satisfaction | |||
| Please rate your overall job satisfaction | 5.53 | 5.46 | 0.54 |
| I have a sense of control over my career. | 4.90 | 4.83 | 0.55 |
| My career expectations are being met. | 5.02 | 4.95 | 0.52 |
| I am likely to look for appointments at other institutions in the coming 12 months.§ |
4.78 | 5.32 | 0.001§ |
| If I had to do it all over, I again would choose an academic career.* |
6.35 | 5.81 | <0.0001* |
| Teaching Support | |||
| Support to develop your teaching skills. | 4.50 | 4.65 | 0.25 |
| Overall, how satisfied are you with your teaching role at the Medical School. |
5.19 | 5.26 | 0.49 |
| Research Support | |||
| Administrative support for managing grants.§ | 5.15 | 4.64 | 0.001§ |
| Guidance with writing grants.§ | 4.30 | 3.89 | 0.009§ |
| Collaboration | |||
| Collaboration with faculty in my department or other departments is important to me. |
4.62 | 4.54 | 0.07 |
| I am satisfied with the collaboration I have with faculty in my department or other departments.§ |
4.05 | 3.91 | 0.03§ |
| Career Advancement | |||
| I understand the process for promotion. * | 6.03 | 5.30 | <0.0001* |
| Criteria for promotion are applied consistently to faculty across comparable positions.§ |
4.89 | 4.46 | 0.002§ |
| Mentorship | |||
| I am satisfied with how I am being mentored.* | 5.11 | 4.36 | <0.0001* |
| Overall, how satisfied are you with your opportunity to be a mentor.* |
5.80 | 5.38 | <0.0001* |
| Compensation | |||
| My total compensation (salary, incentive pay, and total benefits) is competitive with my peers at other comparable U.S. academic medical centers. |
4.43 | 4.33 | 0.48 |
Survey questions were asked on a Likert scale from 1 (poor/very dissatisfied/very unlikely) to 7 (excellent/very satisfied/very likely). Collaboration-related questions were asked on a Likert scale from 1 (very dissatisfied/strongly disagree) to 5 (very satisfied/strongly agree).
p<0.001
p<0.05
Research Support
To better understand research-related differences, we identified faculty members by the extent of their research related activities by a survey question that asked, “I spend a majority of my time on research” versus “I am involved in research-related activities, but research does not take a majority of my time.” Among faculty who identified themselves as the latter, significant differences in mean satisfaction score about collaborations (4.13 (n=143 instructional track faculty) versus 3.91 (n=227 clinical track faculty), p=0.01) and about guidance with writing grants (4.34 (n=119 instructional track faculty) versus 3.90 (n=149 clinical track faculty), p=0.03) emerged between faculty tracks. Additionally, there was a significant difference in overall job satisfaction between this group of faculty members who actively engaged in some research (5.65 (n=142 instructional track) versus 5.37 (n=227 clinical track, p=0.05)). This finding was surprising, suggesting that among clinical track faculty involved in research, having research support significantly impacts overall job satisfaction despite not being a primary mission of this faculty track.
Mentorship
We next examined whether having a mentor also significantly enhanced overall job satisfaction and satisfaction with research-related activities, such as collaborations and grant support. Indeed, faculty members who reported having a mentor were significantly more satisfied with their job than those who did not have a mentor in both tracks (p<0.0001 for the instructional track, p<0.0001 for the clinical track). But despite having a mentor, clinical track faculty still remained significantly less satisfied with their overall job satisfaction (mean satisfaction score 4.34, n=312 clinical track faculty) than instructional track faculty (5.07, n=248, p<0.0001), reported they did not understand promotion processes as well as instructional track faculty (p<0.0001), nor did they believe criteria for promotion were applied consistently compared to instructional track faculty (p=0.03). They also reported significantly less satisfaction with administrative support for managing grants (p=0.007) than their instructional track faculty counterparts. No significant difference emerged in mean satisfaction scores between the two tracks with mentors in satisfaction with collaborations (p=0.46) or with guidance in writing grants (p=0.12). These findings suggest that more effective mentoring relationships among clinical track faculty are needed and simply having a mentor is insufficient to enhance job satisfaction.
Because the results showed that clinical track faculty mentees were significantly less satisfied than instructional track faculty mentees, we questioned whether the mentors themselves were satisfied with their ability or opportunity to mentor junior level faculty. Indeed, a significant difference in mean satisfaction scores emerged between senior level faculty members (e.g. associate and full professors) between the instructional and clinical tracks (mean satisfaction score 5.81 (n=262 instructional track faculty) versus 5.47 (n=101 clinical track faculty), p=0.007). This finding suggests that providing senior clinical track faculty members with opportunities to mentor junior faculty and working to facilitate effective relationships may improve overall satisfaction of the clinical faculty track, given that this track is largely comprised of assistant professors (Table 1).
Factor Analysis
Six factors emerged from the factor analysis of all faculty (Table 3). Based on the associated survey questions, each factor was renamed by the authors as “Departmental Leadership,” “Autonomy, Expectations, Balance,” “Basic Science Research,” “Clinical Support,” “Teaching Support,” and “Compensation.” Cronbach’s alpha was greater than 0.8 for each factor, demonstrating high internal reliability.
Table 3.
Factor Analysis Results for 713 Academic Medical Faculty at the University of Michigan Medical School in 2008
| Factors§ | Cronbach’s α | Eigenvalue | Factor Loadings† |
|---|---|---|---|
| Departmental Leadership | 0.94 | 7.22 | |
| My department chair addresses faculty concerns. | 0.89 | ||
| My department chair sets reasonable expectations. | 0.89 | ||
| My department chair advocates for my career growth. | 0.89 | ||
| My department chair provides useful feedback about my career performance. |
0.78 | ||
| Autonomy, Expectations, Balance | 0.87 | 2.34 | |
| My colleagues respect me as a person. | 0.56 | ||
| My colleagues are supportive of one another. | 0.57 | ||
| I am satisfied with the collaboration I have with faculty in my department or other departments. |
0.55 | ||
| Overall, how satisfied are you with the quality of work you are able to perform as it relates to research? |
0.49 | ||
| I feel balanced between work, family and personal growth. | 0.59 | ||
| My career expectations are being met. | 0.78 | ||
| I have a sense of control over my career. | 0.79 | ||
| If I had to do it all over, I again would choose to work at UM. | 0.57 | ||
| Basic Science Research | 0.85 | 2.00 | |
| Amount of research laboratory space available to you. | 0.66 | ||
| Relevance of available biomedical research cores to your research. | 0.60 | ||
| UCUCA reviews of applications for the use of animals. | 0.83 | ||
| ULAM’s care for your animals, considering your scientific objectives. | 0.84 | ||
| Clinical Support | 0.81 | 1.65 | |
| Clerical support in the clinic. | 0.68 | ||
| Nursing support in clinical activities. | 0.59 | ||
| Support provided by medical assistants. | 0.63 | ||
| Timeliness of diagnostic tests and procedures. | 0.55 | ||
| Patient scheduling in clinic. | 0.66 | ||
| Teaching Support | 0.81 | 1.48 | |
| Your opportunity to teach. | 0.59 | ||
| Feedback given to you about your teaching by learners. | 0.67 | ||
| Feedback given to you about your teaching by division director or department chair. |
0.58 | ||
| Support to develop your teaching skills. | 0.56 | ||
| Overall, how satisfied are you with your teaching role at the Medical School. |
0.63 | ||
| Compensation | 0.96 | 1.20 | |
| My total compensation (salary, incentive pay, and total benefits) is competitive with my peers at other comparable U.S. academic medical centers. |
0.93 | ||
| My total compensation (salary, incentive pay, and total benefits) is competitive with my peers at other Midwestern academic medical centers. |
0.93 | ||
Factors derived from factor analysis results were renamed by the authors.
Variables with factor loadings less than 0.45 were excluded from the analysis, by convention.
Predictors of Job Satisfaction among Instructional Track and Clinical Track Faculty at UMMS
Two significant predictors of job satisfaction emerged among the instructional track faculty (Table 4). Adjusting for all demographic variables, research support, career advancement and mentorship variables, “Departmental Leadership” and “Autonomy, Expectations, Balance” emerged as the two strongest significant predictors by the β-coefficient. By contrast, 5 significant predictors emerged for the clinical track faculty (Table 5). Similar to the instructional track faculty, “Departmental Leadership” and “Autonomy, Expectations, Balance” were significant predictors. However, in addition, “Compensation” and career advancement variables also emerged as significant predictors, adjusting for all demographic variables as well as clinical-research related and mentorship variables.
Table 4.
Linear Regression Results Predicting Job Satisfaction of 353 Instructional Track Faculty at the University of Michigan Medical School in 2008
| Variables | β Coefficient |
95% Confidence Interval |
p-value |
|---|---|---|---|
| Factors | |||
| Departmental Leadership* | 0.50 | 0.31–0.68 | <0.0001* |
| Autonomy, Expectations, Balance* | 0.96 | 0.71–1.21 | <0.0001* |
| Basic Science Research | 0.11 | −0.06–0.27 | 0.20 |
| Clinical Support | 0.03 | −0.20–0.26 | 0.80 |
| Teaching Support | −0.12 | −0.35–0.12 | 0.33 |
| Compensation | 0.15 | −0.02–0.32 | 0.09 |
| Gender | |||
| Female versus Male | 0.08 | −0.38–0.53 | 0.74 |
| Ethnicity† | |||
| White versus Non-white | 0.21 | −0.34–0.77 | 0.45 |
| Specialty| | |||
| Medical versus Surgery | −0.13 | −0.50–0.25 | 0.50 |
| Rank | |||
| Associate versus Assistant | 0.18 | −0.23–0.60 | 0.39 |
| Full versus Assistant | 0.28 | −0.30–0.86 | 0.34 |
| Research | |||
| Administrative support for managing grants. |
0.02 | −0.11–0.15 | 0.72 |
| Guidance with writing grants. | 0.06 | −0.06–0.18 | 0.30 |
| Career Advancement | |||
| I understand the process for promotion. |
−0.05 | −0.19–0.10 | 0.53 |
| Criteria for promotion are applied consistently to faculty across comparable positions. |
0.07 | −0.05–0.19 | 0.25 |
| Mentorship | |||
| I am satisfied with how I am being mentored. |
−0.02 | −0.10–0.06 | 0.66 |
| Overall how satisfied are you with your opportunity to be a mentor. |
−0.05 | −0.26–0.15 | 0.61 |
Non-white ethnic groups consist of Arab, Asian, Black/African American, Hispanic/Latino, and multiple ethnic groups.
Medical: Dermatology, neurology, physical medicine and rehabilitation, psychiatry, anesthesiology, emergency medicine, pathology, radiation oncology, radiology, family medicine, internal medicine, pediatrics and communicable diseases
Surgical: Neurosurgery, obstetrics & gynecology, ophthalmology, orthopaedic surgery, general surgery, urology
p<0.001
Table 5.
Linear Regression Results Predicting Job Satisfaction of 360 Clinical Track Faculty at the University of Michigan Medical School in 2008
| Variables Factors |
β Coefficient |
95% Confidence Interval |
p-value |
|---|---|---|---|
| Departmental Leadership* | 0.39 | 0.19–0.58 | <0.0001* |
| Autonomy, Expectations, Balance* | 0.75 | 0.52–0.98 | <0.0001* |
| Basic Science Research | 0.005 | −0.30–0.31 | 0.97 |
| Clinical Support | 0.03 | −0.20–0.25 | 0.82 |
| Teaching Support | 0.20 | −0.04–0.43 | 0.10 |
| Compensation* | 0.40 | 0.22–0.59 | <0.0001* |
| Gender | |||
| Female versus Male | −0.11 | −0.46–0.24 | 0.54 |
| Ethnicity † | |||
| White versus Non-white | 0.26 | −0.18–0.69 | 0.25 |
| Specialty | |||
| Medical versus Surgery | −0.48 | −0.98–0.01 | 0.06 |
| Basic Science versus Surgery | −0.89 | −2.21–0.43 | 0.18 |
| Rank | |||
| Associate versus Full | 0.44 | −0.08–0.96 | 0.10 |
| Assistant versus Full | 0.38 | −0.11–0.87 | 0.13 |
| Research | |||
| Administrative support for managing grants. |
0.05 | −0.04–0.14 | 0.30 |
| Guidance with writing grants. | −0.02 | −0.12–0.08 | 0.71 |
| Career Advancement | |||
| I understand the process for promotion.§ |
0.21 | 0.07–0.35 | 0.003§ |
| Criteria for promotion are applied consistently to faculty across comparable positions.§ |
−0.11 | −0.21– −0.01 | 0.04§ |
| Mentorship | |||
| I am satisfied with how I am being mentored. |
−0.02 | −0.12–0.08 | 0.65 |
| Overall how satisfied are you with your opportunity to be a mentor. |
−0.04 | −0.23–0.15 | 0.68 |
Non-white ethnic groups consist of Arab, Asian, Black/African American, Hispanic/Latino, and multiple ethnic groups.
p<0.001
p<0.05
DISCUSSION
Although many studies address the satisfaction or concerns of all academic medical faculty11–14 or only the clinical track faculty,8 this study is the first study to contrast predictors of job satisfaction for both the instructional and clinical track faculty members within one academic medical center. Because the missions of the instructional and clinical tracks differ in fundamental ways,5 these two tracks were analyzed separately. Our results contribute to the growing literature about predictors of job satisfaction of academic medical faculty, specifically the importance of the role a departmental chair’s leadership. Second, our results contribute original and new insight about the clinical track faculty are two-fold. First, more effective mentoring relationships are required to improve overall job satisfaction. Second, effective mentoring relationships require engaging mentees in promotion-related activities, given that career advancement variables were strong predictors of job satisfaction among clinical track faculty.
The strongest predictors of job satisfaction for both faculty tracks emerged in areas of autonomy, meeting career expectations, work-life balance and departmental leadership. These results are consistent with the findings of an AAMC focus group study of academic medical faculty where both “clinician-educators” and “clinician-scholars” agreed that interpersonal relationships and work environment, specifically “the culture at the institution, peers, and feelings of being valued,” are important to their overall job satisfaction.15 Because the tone and culture of a department are set by department chairs, the finding that departmental leadership is also a significant predictor of job satisfaction is not surprising and consistent with the literature.11, 20 In fact, departmental leadership was also found to be a predictor of research productivity, in a model proposed by Bland et al., categorizing characteristics into individual, institutional, and leadership features.20, 21 They found that a highly regarded department head is a predictor of both job satisfaction and research productivity.20 The findings reported by Bland et al., have implications for clinical track faculty in our study, given that our results revealed significantly lower mean satisfaction scores related to research-related activities, promotion, and mentorship among clinical track faculty. Department chairs are in a position to provide resources, facilitate informal networking events, foster collaborations, and most importantly, provide a perception of autonomy and recognition for achievements to enhance job satisfaction and research productivity.20 Being experienced, they may also be ideal mentors to younger faculty members within their departments.22
Menaker and Bahn evaluated different types of leadership behaviors in department chairs and surveyed faculty to assess which type of leadership behavior enhanced physician satisfaction.12 Not surprisingly, leadership attributes inherent in mentoring relationships, (e.g., instilling pride and confidence, spending time teaching, and considering each individual’s needs and abilities) best correlated with physician satisfaction.
Mentorship did not emerge as a significant predictor for either faculty track. However, consistent with other studies,17, 23 our results revealed that mentees were significantly more satisfied with their jobs compared to those without a mentor. It may, however, be difficult for one chair to be accessible to all junior faculty members within a department given time-constraints and other departmental responsibilities. Thus, formalized faculty development programs to mentor junior faculty have been implemented elsewhere and demonstrated improved feelings of “empowerment” and enhanced career advancement,24 and departmental leaders can facilitate the appropriate pairing of mentors and mentees and periodically monitor the progress of the relationship with bidirectional feedback or the outcomes of a project that is in alignment of the pair’s professional interests.25
At UMMS, the Team Mentoring Pilot Program was recently developed to employ team-based mentoring strategies. This program assists in matching multiple mentors to each junior faculty member to facilitate a team-based mentoring approach to enhance early research careers. This initiative also works to improve many areas of satisfaction, such as research support, collaborations, and career advancement, for which mean satisfaction scores among clinical track faculty were significantly lower than instructional track faculty.
Interestingly, our results suggest that a root-cause strategy to improving overall clinical track faculty job satisfaction is to create effective mentoring relationships, and simply having a mentor is insufficient. Surprisingly, despite having a mentor, clinical track faculty reported significantly less job satisfaction and understanding career advancement criteria than instructional track faculty. Moreover, because career advancement variables were predictors of job satisfaction for clinical track faculty, working to improve mentoring relationships, specifically in regards to career advancement and promotion-oriented activities or goals, may be an important strategy to enhance vitality in this track. Further insight was elicited from free text comments among clinical track faculty members stating, “My ability to mentor others is challenged by my own lack of a mentor;” and “It is difficult to feel satisfied and competent as a mentor when I am not being mentored in a manner in which I believe is important for my career development.” These comments indicate the need to improve mentoring abilities, and faculty development programs on effective mentoring may be a strategy to enhance overall faculty vitality.
In addition, in our conceptual framework, mentorship and departmental leadership fall within the departmental characteristics category (Figure 1B). Despite differences between the two tracks, our framework suggests that the greatest influence may be conveyed locally, within a department, where direct interactions, assessments, and bidirectional feedback may be more feasible. Further work examining the influence of the physical environment and extent of change is warranted.
Comparisons of additional free text comments between the two tracks provided further insight into individualized concerns and possible strategies. For example, even though many of the instructional faculty’s comments were related to cost (e.g. increasing difficulty in obtaining funding and the rising cost of research), the clinical faculty’s comments were related to time-management and access to resources (e.g. assistance with data collection, grant writing, and opportunities for collaboration). One faculty member suggested better recognizing team scholarship. Although instructional track faculty may have protected time and more research staff, collaborations with clinical track faculty to help recruit patients would emphasize team work.
This team-based approach underlines the mission of the Team Mentoring Pilot Program initiated by UMMS and also involves establishing new interdepartmental and inter-institutional collaborations. Second, many clinical track faculty member stressed the lack of time and inability to attend lectures scheduled during the “prime-time.” In contrast, instructional track faculty members, provided with protected time, reported invaluable experiences with career advancement programs at national meetings. Solutions to this issue include scheduling lectures in the evening, cutting the program into several shorter sessions, or the department chairs reinforcing the importance of faculty participation in such programs in the annual performance review. Such strategies were successfully used by the Pennsylvania State University Junior Faculty Development program.24
There are several limitations to our study. First, 41.3% of our academic medical faculty responded to this survey. However, this response rate is comparable to other physician surveys.26 Second, this study may be vulnerable to non-response bias because comparisons between non-responders and responders could not be evaluated due to the anonymous nature of the survey. Demographic variables between false-starters and responders, however, did not show any significant differences. Third, only one research-intensive university affiliated institution was surveyed. Despite these limitations, we believe our results are quite informative. Comparing and contrasting the two tracks revealed similar predictors, such as the need for strong departmental leadership, and feelings of autonomy and career balance. However, our results revealed career advancement processes to be a significant predictor of job satisfaction among clinical track faculty. A strategy to improve job satisfaction among clinical track faculty may be to focus on more effective mentoring relationships emphasizing career advancement policies and research-related activities which facilitate promotion.
Acknowledgements
The authors would like to acknowledge Heidi Reichert, MA for her help with the statistical analysis.
Sources of funding:
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
Footnotes
All authors made substantial contributions to the conception and design, or acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and provided final approval of the manuscript version to be published.
Competing interests: A competing interest exists when professional judgement concerning a primary interest (such as patients’ welfare or the validity of research) may be influenced by secondary interests (personal matters such as financial gain, personal relationships or professional rivalry).
None.
Authors are required to seek ethical review for all research on human subjects. Ethical approval for this study was granted by
The anonymous survey was considered a non-regulated application by the Institutional Review Board because no private health information was collected; thus an Institutional Review Board letter of approval was generated to proceed with the project to analyze collected data.
NOTE: Where ethical approval has been waived, a statement should be included within the manuscript confirming that ethical principles have been adhered to and addressing ethical implications. For instance, individuals other than the author should not be identifiable without their written permission, and no plausible harms should arise from publication.
Some submitted manuscripts may be of a type not published in Medical Education and, at the discretion of the Editor, could be referred to the editorial team of The Clinical Teacher for consideration (please see www.theclinicalteacher.com for further information). If you do NOT wish your manuscript to be considered by the Editor of The Clinical Teacher, please check this box.
NOTE ON AUTHORSHIP:
Papers submitted to Medical Education MUST be in accordance with the ICMJE Uniform requirements for manuscripts submitted to biomedical journals. The full document is available on http://www.mededuc.com/doclib/Vancouver%20Guidelines%20Oct%202001.pdf
The following is an extract from the Uniform requirements:
- substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content;
- final approval of the version to be published.
Other contributors to the paper should be acknowledged in ‘Acknowledgements’.
Contributor Information
Kevin C. Chung, Professor of Surgery, Section of Plastic Surgery, Assistant Dean for Instructional Faculty, University of Michigan Medical School.
Jae W. Song, Research Fellow, Section of Plastic Surgery, University of Michigan Medical School.
H. Myra Kim, Associate Research Scientist, Center for Statistical Consultation and Research, University of Michigan.
James O. Woolliscroft, Professor of Internal Medicine, Dean of University of Michigan Medical School.
Elisabeth H. Quint, Professor of Obstetrics and Gynecology, Assistant Dean for Clinical Faculty, University of Michigan Medical School.
Nicholas W. Lukacs, Professor of Pathology, Assistant Dean for Research Faculty, University of Michigan Medical School.
Margaret R. Gyetko, Professor of Internal Medicine, Associate Dean for Faculty Affairs, University of Michigan Medical School.
REFERENCES
- 1.Alexander H, Lang J. The long-term retention and attrition of U.S. medical school faculty. AAMC Analysis in Brief. 2008;8:1–2. [Google Scholar]
- 2.Linzer M, Konrad TR, Douglas J, et al. Managed care, time pressure, and physician job satisfaction: Results from the physician worklife study. J Gen Intern Med. 2000;15(7):441–450. doi: 10.1046/j.1525-1497.2000.05239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schloss EP, Flanagan DM, Culler CL, Wright AL. Some hidden costs of faculty turnover in clinical departments in one academic medical center. Acad Med. 2009;84(1):32–36. doi: 10.1097/ACM.0b013e3181906dff. [DOI] [PubMed] [Google Scholar]
- 4.Waldman JD, Kelly F, Arora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev. 2004;29(1):2–7. doi: 10.1097/00004010-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Faculty handbook 2008–2009. [Accessed August 21, 2009]. University of Michigan Medical School. Criteria for appointment and promotion. Available at: www.med.umich.edu/Medschool/faculty/handbook.pdf. [Google Scholar]
- 6.Bunton SA, Mallon WT. The continued evolution of faculty appointment and tenure policies at U.S. medical schools. Acad Med. 2007;82(3):281–289. doi: 10.1097/ACM.0b013e3180307e87. [DOI] [PubMed] [Google Scholar]
- 7.Bordage G. Conceptual frameworks to illuminate and magnify. Med Educ. 2009;43(4):312–319. doi: 10.1111/j.1365-2923.2009.03295.x. [DOI] [PubMed] [Google Scholar]
- 8.Farrell SE, Digioia NM, Broderick KB, Coates WC. Mentoring for clinician-educators. Acad Emerg Med. 2004;11(12):1346–1350. doi: 10.1197/j.aem.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Foster SW, McMurray JE, Linzer M, Leavitt JW, Rosenberg M, Carnes M. Results of a gender-climate and work-environment survey at a Midwestern academic health center. Acad Med. 2000;75(6):653–660. doi: 10.1097/00001888-200006000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Shollen SL, Bland CJ, Finstad DA, Taylor AL. Organizational climate and family life: How these factors affect the status of women faculty at one medical school. Acad Med. 2009;84(1):87–94. doi: 10.1097/ACM.0b013e3181900edf. [DOI] [PubMed] [Google Scholar]
- 11.Demmy TL, Kivlahan C, Stone TT, Teague L, Sapienza P. Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center. Acad Med. 2002;77(12 Pt 1):1235–1240. doi: 10.1097/00001888-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Menaker R, Bahn RS. How perceived physician leadership behavior affects physician satisfaction. Mayo Clin Proc. 2008;83(9):983–988. doi: 10.4065/83.9.983. [DOI] [PubMed] [Google Scholar]
- 13.Coyle YM, Aday LA, Battles JB, Hynan LS. Measuring and predicting academic generalists' work satisfaction: Implications for retaining faculty. Acad Med. 1999;74(9):1021–1027. doi: 10.1097/00001888-199909000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Bunton SA. U.S. medical school faculty job satisfaction. AAMC Analysis in Brief. 2008;8:1–2. [Google Scholar]
- 15.Bunton SA. Medical faculty job satisfaction: Thematic overviews from ten focus groups. AAMC. 2006:1–22. [Google Scholar]
- 16.Buckley LM, Sanders K, Shih M, Hampton CL. Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. results of a survey. Arch Intern Med. 2000;160(17):2625–2629. doi: 10.1001/archinte.160.17.2625. [DOI] [PubMed] [Google Scholar]
- 17.Wasserstein AG, Quistberg DA, Shea JA. Mentoring at the university of Pennsylvania: Results of a faculty survey. J Gen Intern Med. 2007;22(2):210–214. doi: 10.1007/s11606-006-0051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faculty Satisfaction: 2008 Faculty Satisfaction Survey. [Accessed August 2009]; Revised 2008. http://www.med.umich.edu/i/quality/reports/faculty.html.
- 19.Pett MA, Lackey NR, Sullivan JJ. Making Sense of Factor Analysis. Thousand Oaks, California: Sage Publications; 2003. [Google Scholar]
- 20.Bland CJ, Center BA, Finstad DA, Risbey KR, Staples JG. A theoretical, practical, predictive model of faculty and department research productivity. Acad Med. 2005;80(3):225–237. doi: 10.1097/00001888-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Bland CJ, Seaquist E, Pacala JT, Center B, Finstad D. One school's strategy to assess and improve the vitality of its faculty. Acad Med. 2002;77(5):368–376. doi: 10.1097/00001888-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Souba WW. The Achilles’ heels of an academic surgeon: A leadership tale. J Surg Res. 2005;123(2):320–327. doi: 10.1016/j.jss.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 23.Chew LD, Watanabe JM, Buchwald D, Lessler DS. Junior faculty's perspectives on mentoring. Acad Med. 2003;78(6):652. doi: 10.1097/00001888-200306000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Thorndyke LE, Gusic ME, George JH, Quillen DA, Milner RJ. Empowering junior faculty: Penn state's faculty development and mentoring program. Acad Med. 2006;81(7):668–673. doi: 10.1097/01.ACM.0000232424.88922.df. [DOI] [PubMed] [Google Scholar]
- 25.Thorndyke LE, Gusic ME, Milner RJ. Functional mentoring: A practical approach with multilevel outcomes. J Contin Educ Health Prof. 2008;28(3):157–164. doi: 10.1002/chp.178. [DOI] [PubMed] [Google Scholar]
- 26.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001;35(6):1347–1355. [PMC free article] [PubMed] [Google Scholar]