Abstract
Interleukin-2 (IL-2) provides a memory differentiation signal to CD8+ T cells during the primary response that impacts the ability of the subsequent memory pool to mount a successful recall response. We find here that while primary effector CTL development is modestly decreased in the absence of IL-2, the persistence of short-term and long-term effector memory CD8+ T cells upon pathogen clearance is greatly diminished. Furthermore, secondary challenge of CD8+ memory T cells lacking the high avidity IL-2 receptor results in a failure to repopulate the effector pool. The role of IL-2 in promoting effector differentiation is not shared with the highly related cytokine, IL-15. While IL-15 supports the survival of effector CD8+ T cells following pathogen clearance, its absence does not impair either primary or secondary effector CTL differentiation, nor does it impact the differentiation of long-term effector memory CD8+ T cells. These findings indicate a unique role for IL-2, but not IL-15, in promoting the differentiation not only of primary effector CD8+ T cells but also of CD8+ memory T cells capable of secondary effector differentiation.
Introduction
Antigen-specific CD8+ T cells receive instructional signals during the primary phase of the immune response to acute infection that dictate later stages of differentiation. Upon antigen recognition, CD8+ T cells undergo massive clonal expansion and acquire effector functions that are critical for the elimination of intracellular pathogens, including cytolytic function and the ability to produce pro-inflammatory cytokines such as IFNγ and TNFα. After the infection is resolved, most of the effector population dies, leaving behind a long-lived population of memory cells capable of rapid secondary protection upon re-exposure to the same or a related pathogen (1, 2).
CD8+ memory T cell precursors can be identified among the effector population at the peak of the response to acute infection based on the expression of cell surface molecules such as IL-7Rα and KLRG1 (3, 4). Intensive efforts are underway to understand the nature of the differentiation signals that differentially promote the emergence of effector cells that express high levels of KLRG1 and low levels of IL-7Rα (short-lived effector cells, or SLEC)3, and memory precursor cells that express low levels of KLRG1 and high levels of IL-7Rα. CD4+ T cell-derived “help” is of particular importance in the generation of functional (capable of secondary responses to antigen) CD8+ memory T cells (5-9). Other studies have suggested that memory potential may depend at least in part on asymmetric division at the initiation of the T cell response (10, 11) or differential expression of the transcription factor T-bet driven by exposure to inflammatory cytokines such as IL-12 (3).
Our recent studies have focused on the role of IL-2 in CD8+ memory T cell differentiation. Like others (12-14), we found that in the absence of IL-2 signals, CD8+ T cells showed only modest impairment in their ability to make robust primary responses following acute infection. However, IL-2 signals during the primary response were required for the ability of the ensuing CD8+ memory cells to generate optimal secondary responses (15). Several other observations indicated that the impact of IL-2 on CD8+ T cells impacted multiple differentiation pathways. For example, memory T cells generated in the absence of IL-2 skewed to a central memory-like phenotype as measured by expression of CD62L and the ability to produce IL-2 upon restimulation (15).
Prior studies have suggested that IL-2 and the closely related cytokine IL-15 differentially regulate certain aspects of CD8+ memory T cell differentiation. While activation in the presence of high levels of IL-2 in vitro preferentially promotes the subsequent in vivo development of effector and effector memory T cells, activation in the presence of IL-15 preferentially promotes central memory differentiation (16, 17). Both of these cytokines have been used or proposed as potential immunotherapeutics. High-dose IL-2 treatment has been used clinically to treat several types of cancer, including renal cell carcinoma and melanoma, with modest effects on a subset of recipients (18-20). The use of IL-15 has been suggested for boosting T and NK cell anti-tumor responses and as a vaccination adjuvant in various model systems (21-27). While IL-15 has a well-described role in promoting the homeostasis and survival of CD8+ memory T cells (28), differing mouse models of acute infection demonstrate either no role (29, 30) or a significant role (31) for IL-15 in the generation of effector CTL responses. In all, it remains unclear how and to what extent IL-2 and IL-15 mediate overlapping, differing or even opposing functions, particularly in the early phases of activation in which T cells enter into their differentiation program (32, 33).
Because CD8+ T cell effector responses were robust even in the absence of IL-2 signals, we hypothesized that related cytokines may compensate for the lack of IL-2 signals during acute infection. IL-15 was an obvious initial candidate. IL-2 and IL-15 belong to a family of cytokines utilizing the common gamma chain (γc) as a component of their receptors. Among this family, IL-2 and IL-15 are particularly related, as they share the β (CD122) and γc (CD132) chains of their heterotrimeric receptor. Therefore, IL-2 and IL-15 promote apparently distinct biological outcomes while utilizing similar JAK/STAT and protein tyrosine kinase (PTK) pathways (34, 35). Because signals through both the IL-2R and the IL-15R are delivered by the β and γc chains, one possibility is that the biological effects of IL-2 and IL-15 signals in driving effector and memory CTL differentiation overlap. However, IL-2 and IL-15 signals differ in magnitude, timing and context. While IL-2 binds its receptor as a soluble molecule, IL-15 is presented in trans by surface-bound IL-15Rα (36, 37), restricting the most potent IL-15 signals to periods of cell-cell contact, such as during the interaction of a T cell with an APC. In support of this idea, dendritic cells are a key source of IL-15 for memory T cell homeostasis and survival (38). Furthermore, expression of the high-affinity IL-2R is largely restricted to the first few days of the response, whereas IL-15 signals are presumably available to T cells during the initiation of the T cell response as well as during memory maintenance. It is possible, therefore, that these differences can be invoked to explain the distinct biological impacts of IL-2 and IL-15 on the T cell response. In this scenario, IL-15, rather than sharing a role with IL-2 during the primary response, could have opposing functions, such as have been suggested in the respective roles of IL-2 and IL-15 in driving the differentiation of effector and memory T cells (16, 17).
In this study, we find that IL-2 plays a central role in the differentiation and survival of effector CTL and short-term effector memory CTL that persist during the first few months after infection, as well as tissue-residing long-term effector memory CTL. IL-2Rα-deficient CD8+ effector T cells responding to acute infection display robust cytokine production but modest decreases in CTL activity. Upon secondary challenge, IL-2Rα-deficient CD8+ memory T cells display a severe defect in their ability to differentiate into secondary effector CTL, maintaining an IL-7Rαhi CD62Lhi phenotype and a cytokine production profile typical of memory CTL, not effector CTL. However, we find little role for IL-15 signals during the primary response, either alone or in combination with IL-2, in promoting effector or effector memory differentiation or programming the recall capacity of CD8+ central memory T cells. Instead, the dominant role of IL-15 was to promote the survival of effector and memory populations after pathogen clearance. While excess IL-15 signals may serve as an adjuvant or have immunotherapeutic benefit for CD8+ T cell responses, our findings suggest that in settings of acute infection, physiological IL-15 signals to T cells during the primary response do not play a significant role in CD8+ effector and memory T cell differentiation, particularly as compared to IL-2.
Materials and Methods
Mice and Infections
6-8 week old C57BL/6 (B6), B6.129S4-Il2ratm1Dw (IL-2Rα-deficient), B6.SJL-PtprcaPepcb/BoyJ B6.SJL, Ly5.1+) and B6.PL-Thy1a/CyJ (B6.PL, Thy1.1+) mice were purchased from Jackson Laboratories (Bar Harbor, ME). C57BL/6NTac-IL15tm1Imx (IL-15-deficient) mice were purchased from Taconic Farms (Germantown, NY). WT and IL-2Rα-deficient P14 TCR transgenic mouse colonies were maintained at the University of Utah. All animal experiments were conducted with the approval of the IACUC committee at the University of Utah. LCMV Armstrong 53b was grown in BHK cells and titered in Vero cells (39). Mice were infected intraperitoneally (i.p.) with 2 × 105 plaque-forming units (PFU). Recombinant Listeria monocytogenes expressing the LCMV GP33-41 peptide (Lm-gp33, generated using described methods) was propagated in BHI broth and agar plates as previously described (40-42). Prior to infection, the bacteria were grown to log phase and concentration determined by measuring the O.D. at 600 nm (O.D. of 1 = 1 × 109 CFU/ml). For secondary challenges, mice were injected intravenously (i.v.) with 2 × 105 colony forming units (CFU). Recombinant vaccinia virus expressing the LCMV glycoprotein (VV-GP, provided by J.L. Whitton) was generated and propagated as described (43). For secondary challenges, mice were injected i.p. with 2 × 106 PFU.
Irradiation Chimeras
To generate WT/IL-2Rα-deficient mixed bone marrow chimeras, recipient mice were given 900 rads using an analytical X-ray irradiator located in the mouse vivarium at the University of Utah. One day later, we harvested bone marrow from the femurs and tibias of WT and IL-2Rα-deficient donors. Following red blood cell lysis, bone marrow cells were incubated with biotinylated anti-CD3 antibodies (eBioscience, San Diego, CA), followed by incubation with anti-biotin magnetic beads (Miltenyi). CD3+ cells were depleted by passage through a magnetic column according to the manufacturer's instructions (Miltenyi). CD3-depleted WT and IL-2Rα-deficient bone marrow cells were mixed 1:1 and injected i.v. into irradiated hosts. By using different combinations of congenic markers, we readily distinguished WT (Ly5.1+), IL-2Rα-deficient (Thy1.2+) and residual host (Thy1.1+) T cells in the periphery of host mice 8-10 weeks later. Similar methods were used to generate P14 irradiation chimeras. P14 irradiation chimeras were generated with a 1:1 mix of WT or IL-2Ra-deficient P14 bone marrow with B6 bone marrow. P14 were harvested a minimum of 8 weeks post-irradiation.
Cell Suspensions and Adoptive Transfers
Splenocytes and lymph node cells were harvested at the indicated time points and re-suspended in RPMI 1640 supplemented with 10% FBS and antibiotics. Liver and lung lymphocytes were harvested by collagenase digestion as previously described (44). Untouched CD8+ P14 T cells were isolated from the spleens and lymph nodes of WT or IL-2Rα-deficient P14 bone marrow chimeras by incubation with a biotinylated antibody cocktail followed by anti-biotin magnetic beads and depletion on a magnetic column, per manufacturer's recommendations (Miltenyi). In addition, we added biotinylated CD44 antibody (eBiosciences, San Diego, CA) to eliminate CD44hi “memory phenotype” P14. TCR transgenic T cell purity was assessed by staining with CD44, Vα2 and Vβ8.1 antibodies, followed by flow cytometric analysis. WT (Thy1.1+) and IL-2Rα-deficient (Thy1.1+Thy1.2+) P14 were mixed 1:1 and co-injected i.v. into naïve B6 (Thy1.2+) mice at the indicated doses one day prior to infection.
Peptide Re-stimulation and Intracellular Cytokine Staining
Splenocytes were re-suspended in RPMI 1640 containing 10% fetal bovine serum and supplemented with antibiotics and L-glutamine. Mice were re-stimulated with 0.1 μM H-2Db-restricted peptide (GP33-41) in the presence of Brefeldin A (1 μl/ml GolgiPlug). Cells were stained with cell surface antibodies, permeabilized and stained with cytokine antibodies (specific to IFNγ, TNFα and IL-2) using a kit per manufacturer's instructions (BDBiosciences, Mountain View, CA).
CTL assays
We utilized a FACS-based cytotoxicity assay as previously described (45). EL4 cells were incubated with 0.1 μM GP33-41 peptide for 2 hours at 37° C. Cells were washed and incubated with FACS-sorted WT or IL-2Rα-deficient P14 CTLs for two hours at 37° C at effector to target ratios ranging from 3:1 to 0.1:1. We stained for expression of Annexin V (BDBiosciences) and measured the percent of Annexin V+ target cells by FACS. Specific killing was determined by comparison to killing of unloaded control targets cells.
Tetramer staining and analysis
The H-2Db-restricted GP33-41 monomer was generated, biotinylated and tetramerized with streptavidin-conjugated allophycocyanin using described methods (46, 47), with modifications as described in protocols available on the NIH Tetramer Core Facility website (http://tetramer.yerkes.emory.edu/). Staining was performed at 4°C for 1 hour in FACS buffer (PBS with 2% fetal bovine serum and .02% sodium azide).
Antibodies and Flow Cytometry
Fluorescent dye-conjugated antibodies were purchased from eBioscience (San Diego, CA), BioLegend (San Diego, CA) or BDBiosciences (Mountain View, CA) with the following specificities: CD8, Thy1.1, Thy1.2, CD45.1, Va2, Vb8.1, CD44, IL-7Ra, KLRG1, CD27, CD62L, CXCR3, CD43, CD122, CD25, Eomes, T-bet, Granzyme B, CD107a, TNFα, IL-2 and IFNγ. Cell surface antibody staining was done in PBS containing 2% FBS, and intracellular cytokine staining was performed as described above. For T-bet and Granzyme B staining, cells were permeabilized using the same buffers as for intracellular cytokine staining (BDBiosciences, Mountain View, CA). For Eomes, cells were permeabilized and stained using the same buffers as those used for the anti-FoxP3 antibody per the manufacturer's instructions (eBioscience, San Diego, CA). For CD107a, the antibody was mixed with re-suspended cells during peptide restimulation prior to intracellular cytokine staining. Multi-paramter (6-7 color) analysis of antibody-stained cells was performed on a FACSCanto II flow cytometer (BDBiosciences, Mountain View, CA) and results analyzed using FlowJo software (TreeStar). Cell sorting was with on a FACSVantage (BDBiosciences, Mountain View, CA) at the University of Utah FACS core facility.
Microarray
RNA was isolated using RNeasy kits (Qiagen) from FACS-sorted P14 cells (day 8 post-infection). Message was amplified and converted to Cy3 or Cy5-labeled cRNA using a commercially available kit per manufacturer's instructions (Agilent Technologies). Four biological duplicates from each group were hybridized to Agilent whole mouse genome microarrays. For each of the four replicates, dual hybridization was performed using RNA obtained from WT and IL-2Rα-deficient P14 isolated from the same animal. Results were normalized and analyzed for differences in log2 expression values using GeneSifter software (Geospiza, Seattle, WA). Microarray data is publicly available at the on-line depository GEO (Accession #GSE19598, http://www.ncbi.nlm.nih.gov/geo/) and conforms to all MIAME guidelines.
Results
Impaired accumulation and survival of CD8+ end-stage effector T cells in the absence of IL-2 signals
Our previous studies found that in the absence of IL-2 signals, developing CD8+ memory T cells rapidly converted to a CD62Lhi phenotype (15). To characterize this finding further, we analyzed the responses of LCMV-specific P14 TCR transgenic T cells either expressing or lacking the IL-2Rα. IL-2Rα-deficiency results in the loss of CD4+CD25+ regulatory T cell function and multi-organ autoimmunity at a young age (48-50). In order to mitigate non-specific effects this environment might have on T cell function, we sought to generate IL-2Rα-deficient P14 donors that lacked autoimmune side effects. We generated mixed bone marrow chimeras by transferring a 1:1 mix of wildtype (WT) B6 and either WT or IL-2Rα-deficient P14 bone marrow (BM) into lethally irradiated B6 hosts, as previously described (15). Because the WT BM gave rise to a functional regulatory T cell population, the chimeras remained healthy with no signs of autoimmunity. Naïve (CD44lo) WT and IL-2Rα-deficient P14 cells were harvested from the chimeras and co-transferred into naïve B6 hosts, followed by LCMV infection. Because of their variable expression of Thy1 alleles, we simultaneously tracked WT P14 (Thy1.1+) and IL-2Rα-deficient P14 (Thy1.1+Thy1.2+) responses in B6 hosts (Thy1.2+) at various time points post-infection.
As previously observed (15), WT P14 responders expanded modestly (~2-fold) better than IL-2Rα-deficient P14 responders by the peak of the response. Both populations also formed memory populations that persisted at stable levels throughout the course of our experiments (Fig. 1A). However, a slightly higher fraction of IL-2Rα-deficient P14 cells was lost during the contraction phase, as compared to the peak of the response (Fig. 1B). To determine the cause of this loss, we analyzed the differentiation of short-lived effector cell and memory precursor populations at the peak of the response and in the transition to memory. Recent studies have found that short-lived effector cells can be differentiated from memory precursor/memory cells based on variable expression of IL-7Rα and KLRG1 (3). At the peak of the primary response (day 8), we observed 2-3-fold fewer KLRG1hiIL7Rαlo effector CTL among the IL-2Rα-deficient P14 responders, as compared to WT P14 (Fig. 1C-D). WT P14 formed a population of detectable KLRG1hi effector phenotype CTL that slowly faded from the memory pool over the course of 4-6 months (referred to here as short-term effector memory cells). In contrast, IL-2Rα-deficient short-term effector memory CTL disappeared rapidly, comprising 10-20-fold lower levels in the spleen at day 42 post-infection (Fig. 1C-D). WT and IL-2Rα-deficient P14 demonstrated no differences in the generation of KLRG1loIL7Rαhi memory precursors at the peak of the response (day 8 post-infection). Numerical differences in the number of WT and IL-2Rα-deficient P14 could almost entirely be ascribed to deficiencies in the generation of effector phenotype cells. Several other markers also confirmed the rapid disappearance of effector cells in the IL-2Rα-deficient P14 population. Besides their expression patterns of KLRG1 and IL-7Rα, differentiated effector populations were CD27lo, CD62Llo, CXCR3lo and CD43lo. Effector cells bearing these characteristics also disappeared rapidly in the absence of IL-2 signals in both the spleen and liver (Supp. Figs. 1 and 2).
Figure 1.
IL-2 drives the differentiation and survival of short-lived effector and short-lived effector memory CTL. Naïve (CD44lo) WT and IL-2Rα-deficient P14 were harvested from the spleens and lymph nodes of P14 bone marrow chimeras, mixed 1:1 (5 × 103 of each), and co-injected into naïve B6 mice one day prior to LCMV infection. The graphs display A, the total number of WT and IL-2Rα-deficient P14 harvested from the spleen, B, the fraction of surviving P14 cells within each group as a compared to the peak (day 8) response, and C, the total number of end-stage effector phenotype P14 (KLRG1hiIL-7Rαlo) at the indicated time points post-infection. Error bars indicate the standard error of the mean (SEM)(n=3-4/time point, statistical significance determined by student's t-test throughout the text). Differences at all time points in panel C are statistically significant (p<.02). D, Representative flow plots display the frequency of end-stage effector P14 (KLRG1hiIL-7Rαlo) and memory precursor/memory P14 (KLRG1loIL-7Rαhi) at the indicated time points post-infection. Results are representative of 5-6 independent experiments.
Lack of IL-2 signals adversely impacts the function of effector CTLs
Because we observed modest but significant and reproducible differences in the number of CD8+ effector CTL at the peak of the response in the absence of IL-2 signals, we tested the hypothesis that IL-2 might also be important for optimal effector function. Previous studies in which CTL received little or no IL-2 signals were disrupted during in vitro activation followed by in vivo adoptive transfer suggested that IL-2 might play an important role in the development of effector function (16). We focused on a time point at which the high affinity IL-2 receptor was expressed at high levels (day 5) as well as the peak of the effector response (day 8), at which time the high affinity IL-2R was no longer expressed (Fig. 2A).
Figure 2.
IL-2Rα-deficient P14 CTLs have modestly decreased cytolytic activity. Effector WT and IL-2Rα-deficient P14 were assessed for expression of effector molecules and function. A, WT (black line) and IL-2Rα-deficient (gray line) P14 were tested for cell surface expression of CD25 and intracellular expression of T-bet, Eomes and Granzyme B on days 5 and 8 post-infection, as indicated. Gray filled histograms are isotype controls. B, We assessed production IFNγ, TNFα and IL-2 by WT and IL-2Rα-deficient P14 as indicated in representative plots following 4 hour ex vivo restimulation with GP33-41 peptide in the presence of Brefeldin A. C, GP33-41 peptide loaded EL4 cells were incubated with WT or IL-2Ra-deficient P14 CTL FACS-sorted from spleens at day 8 post-infection. CTL-induced apoptosis was measured by staining with Annexin V 2 hours later. Error bars represent the SEM (n=3-4/group) and differences between WT and IL-2Rα-deficient (KO) P14 are statistically significant (p<.01)
Initially, we measured intracellular expression of the transcription factors T-bet and Eomes. These related T-box transcription factors have been implicated in the differentiation of effector T cells and in the acquisition of effector T cell function, such as IFNγ production and CTL activity, as well as in the differentiation of functionally and phenotypically normal CD8+ memory T cells (3, 45, 51, 52). We found no differences in expression of T-bet at either day 5 or day 8 post-infection. Conversely, IL-2Rα-deficient P14 demonstrated a reproducible 2-fold increase in the amount of Eomes at day 8 post-infection (Fig. 2A). These differences were not due to differences in the composition of each population, as direct comparison of short-term effector and memory precursor effector populations revealed the same 2-fold disparity in Eomes expression (data not shown). While these differences are modest, they remain of interest given that similar differences in Eomes expression in mice with a single functional allele impacts CD8+ T cell differentiation and effector function (51). Nevertheless, these results are inconsistent with an obligate role for IL-2 in the acquisition of effector function, given that Eomes expression was higher in the absence of IL-2. Furthermore, they suggest that IL-2 influences Eomes expression indirectly, as no expression differences were seen at day 5 when WT P14 responders are still actively receiving IL-2 signals (Fig. 2A).
IL-2Rα-deficient CTL expressed Granzyme B and de-granulated and produced cytokines upon re-stimulation (Fig. 2A-B, Supp. Fig. 3). However, IL-2Rα-deficient CTL demonstrated a modest decrease in CTL activity at day 8 post-infection (Fig. 2C). To assess effector CTL development at this time point, we analyzed RNA expression by WT and IL-2Rα-deficient P14 CTL by microarray. We observed significant up-regulation of effector molecules involved in cytolysis and effector differentiation in WT CTL, including Granzymes and Perforin, as well as an increase in T-bet (Table I). While Blimp-1 was not significantly up-regulated in WT cells, Bcl-6 was significantly up-regulated in IL-2Rα-deficient CTL (Table II). A variety of NK receptors, likely indicators of CTL differentiation (3), also demonstrate increased expression in WT CTL. IL-2Rα-deficient CTL expressed higher levels of IL-2 and TNFα as well as receptors that mediate trafficking to and within secondary lymphoid organs (CCR7 and CXCR5)(Table II). These findings were predicted by cell surface staining and again indicate a skewing away from a differentiated effector phenotype. While we observed differences in expression of several pro- and anti-apoptotic mediators, no clear pattern emerged to explain the failure of IL-2Rα-deficient effector CTL to survive following antigen clearance. However, WT P14 CTL demonstrated enhanced expression of a variety of cell cycle participants, indicating that IL-2 may drive cell division later in the primary response (Supp. Table I). This finding corresponds to previous observations by others (13, 53) and our own finding that WT responders demonstrate enhanced expansion between days 5 and 8 post-infection (15). Overall, while many of the gene expression differences are individually modest, they collectively support a role for IL-2 in driving the differentiation and enhancing the function of primary CTL. One possible interpretation of these results is that differences in cytolytic function (Fig. 2C) and expression of CTL differentiation markers and cytolytic molecules (Table I) reflect differences in the generation of short-lived effector CTL in the absence of IL-2 (Fig. 1C-D), and future studies will be needed to directly compare the differentiation status of purified short-lived and memory precursor effector cell populations in the presence or absence of IL-2 signals.
Table I.
Genes with increased expression in WT P14 8 days post-infection with LCMV.
| Name | fold up (WT) | function |
|---|---|---|
| Granzyme A | 3.3 | cytotoxicity |
| Granzyme B | 1.8 | cytotoxicity |
| Granzyme E | 2.4 | cytotoxicity |
| Perforin | 1.4 | cytotoxicity |
| Klre1 | 1.9 | NK/CTL diff. marker |
| Klrb1b | 2.3 | NK/CTL diff. marker |
| Klrk1 | 1.7 | NK/CTL diff. marker |
| Klrg1* | 1.2 | NK/CTL diff. marker |
| Klrc2 | 1.5 | NK/CTL diff. marker |
| Klra3 | 1.5 | NK/CTL diff. marker |
| Klra7 | 1.8 | NK/CTL diff. marker |
| 2B4 | 1.7 | NK/CTL diff. marker |
| IL12Rb2 | 1.5 | cytokine receptor |
| Tbet | 1.5 | CTL differentiation |
| Blimp-1* | 1.2 | CTL differentiation |
All fold differences are significant (p<.05, n=4)
no significant difference.
Table II.
Genes with increased expression in IL-2Rα-deficient (KO) P14 8 days post-infection with LCMV.
| Name | fold up (KO) | function |
|---|---|---|
| Bcl6 | 1.9 | memory diff. |
| IL-2 | 2.3 | cytokine |
| TNFα | 1.5 | cytokine |
| IL-10 | 1.9 | cytokine |
| IL-17F | 1.7 | cytokine |
| CXCR5 | 5.4 | SLO trafficking |
| CCR7 | 3.3 | SLO trafficking |
| CTLA4 | 1.5 | neg. costimulation |
| CD40 | 2.7 | costimulation |
| CD44 | 1.6 | activation marker |
| TCF-1 | 2.2 | CTL diff. arrest |
| LEF-1 | 1.3 | CTL diff. arrest |
All fold differences are significant (p<.05, n=4).
Poor differentiation of secondary effector T cells in the absence of IL-2
Because CD8+ memory T cells generated in the absence of IL-2 signals mount poor secondary responses, we assessed their ability to become secondary effector cells. To assess polyclonal endogenous recall responses, we generated mixed bone marrow chimeras using a 1:1 mix of bone marrow from WT and IL-2Rα-deficient donors. At 8-10 weeks post-transplant, mice were challenged with LCMV. As measured by MHC Class I tetramers (Fig. 3A) and the frequency of IFNγ-producing cells following peptide restimulation, even in the absence of IL-2 signals CD8+ T cells generated robust primary responses and long-lived memory populations similar to that of wildtype responders. Mice were rechallenged with either a recombinant Listeria monocytogenes expressing the LCMV glycoprotein (Lm-gp33) or a recombinant vaccinia virus expressing the LCMV glycoprotein (VV-GP) at 150 days post-infection. As previously observed (15), IL-2Rα-deficient CD8+ memory T cells demonstrated a significant deficit in their ability to generate secondary responses, as compared to WT. Furthermore, poor recall responses were not due to competition with WT memory CTL. Similar differences were seen when FACS-purified WT and IL-2Ra-deficient memory P14 were transferred into separate naïve B6 hosts prior to rechallenge (Supp. Fig. 4).
Figure 3.
IL-2Rα-deficient CD8+ memory T cells fail to differentiate into secondary effector CTLs following rechallenge. We generated mixed bone marrow chimeras using WT and IL-2Rα-deficient donor bone marrow cells in equal number. At 10 weeks post-transplant, we infected mice with LCMV and assessed CD8+ T cell responses in the spleen using Db-GP33-41 tetramer at the peak of the primary response (1°, day 8 post-infection), during memory maintenance (day 150 post-infection), or at the peak of the secondary response following rechallenge with Lm-gp33 or VV-GP. A, The bar graph indicates the ratio of WT and IL-2Rα-deficient tetramer-binding responders at day 8 after primary LCMV infection (1°), day 150 after primary infection (mem), and 5 days after rechallenge with either Lm-gp33 or VV-GP. Numbers in parentheses indicate fold expansion of WT and IL-2Rα-deficient CTL post-rechallenge. Error bars indicate the SEM (n=3-4/group), and differences in fold expansion are statistically significant (p<.05). B, Representative flow plots, gated on tetramer binding CD8+ T cells, indicate the frequency of effector phenotype (KLRG1hiIL-7Rαlo or CD62Llo) cells among WT or IL-2Rα-deficient (KO) responders at the peak of the primary (day 8 post-infection with LCMV) or secondary (day 5 post-rechallenge with Lm-gp33) response. C, The bar graph indicates the ratio of WT and IL-2Rα-deficient tetramer-binding effector phenotype (KLRG1hiIL-7Rαlo) responders at day 8 after primary LCMV infection and 5 days after rechallenge (at day 150) with either Lm-gp33 or VV-GP. Error bars indicate the SEM (n=3-4/group, p<.05 when comparing ratios after the primary or secondary responses). D, Following 4 hour restimulation with peptide, we assessed the ability of WT and IL-2Rα-deficient responders to make cytokines at either day 150 post-infection with LCMV or day 5 post-rechallenge with Lm-gp33. The pie charts indicate the average frequency of responders within the IFNγ-producing population capable of making TNFα and/or IL-2 (n=3). Results are representative of two separate experiments.
A closer analysis of the tetramer-binding cells at the peak (day 5) of the secondary response revealed that IL-2 signals were required for the generation of secondary effector CTL (KLRG1hiIL-7Rαlo)(Fig. 3B). Furthermore, secondary responders induced in the absence of IL-2 remained CD62Lhi (Fig. 3B), CD27hi and CXCR3hi (Supp. Fig. 5), all characteristics of memory cells, not effector cells. These defects were present but modest at the peak of the primary response and greatly exacerbated upon secondary challenge (Fig. 3B). To assess function, we restimulated splenocytes ex vivo both pre- and post-rechallenge. Prior to rechallenge, both wildtype and IL-2Rα-deficient memory populations primarily consisted of cells capable of simultaneously producing IFNγ and TNFα (double producers), or IFNγ, TNFα and IL-2 (triple producers), with few cells only able to produce IFNγ (single producers). Following rechallenge and the development of secondary effectors, the cytokine-producing profile of WT responders shifted dramatically towards single or double producers, with few triple producers. Conversely, the cytokine-producing profile of IL-2Rα-deficient secondary responders was largely unchanged, again reflecting an inability to generate large numbers of secondary effector CTL (Fig. 3C).
IL-2 promotes the differentiation of CD8+ long-lived effector memory T cells
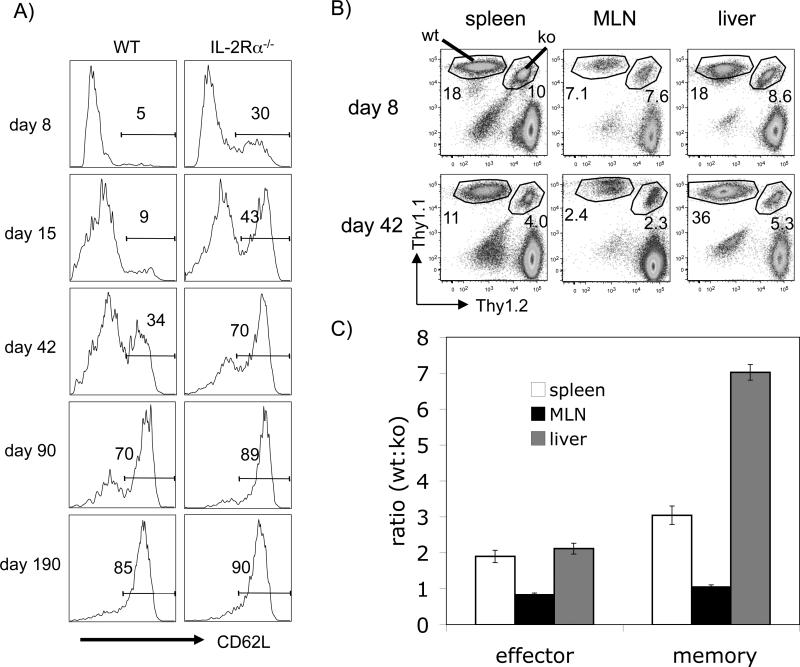
Our prior studies confirmed that CD8+ memory T cells generated in the absence of IL-2 signals quickly converted to a CD62Lhi central memory phenotype (15). However, because in the present study we observed in the absence of IL-2 signals a rapid loss of KLRG1hiIL-7Rαlo effector cells that are also CD62Llo, we considered the possibility that our prior observations simply reflected a loss of this population and not a role for IL-2 in the generation of bona fide tissue-residing long-lived effector memory T cells. To test this possibility we assessed CD62L expression by IL-7Rαhi memory T cells as a measure of true effector memory T cell differentiation and survival. We found that even this population demonstrated a rapid loss of CD62Llo effector memory T cells in the spleen following acute LCMV infection in the absence of IL-2 signals (Fig. 4A). Furthermore, WT tissue-residing memory P14 in the liver demonstrated a selective advantage over time as compared to IL-2Rα-deficient memory P14. This survival advantage was intermediate in the spleen and not observed in the lymph nodes (Fig. 4B-C). We therefore concluded that IL-2 played a central role in the differentiation of effector memory T cells in both the spleen and peripheral sites of infection.
Figure 4.
IL-2 drives the differentiation of long-lived tissue residing effector memory CTLs. We transferred 500 WT and IL-2Rα-deficient P14 cells prior to LCMV infection. A, Representative flow plots indicate the frequency of central memory (CD62Lhi) phenotype cells in the spleen at the indicated time points after LCMV infection. All plots are gated on the memory precursor/memory population (KLRG1loIL-7Rαhi). B, Representative flow plots indicate the relative frequencies of WT and IL-2Rα-deficient P14 (KO) in the spleen, mesenteric lymph nodes (MLN) and liver at days 8 and 42 post-infection. C, The bar graph displays the ratio of WT to IL-Rα-deficient responders at day 8 (effector) and day 42 (memory) post-infection with LCMV in the indicated tissues. Error bars indicate the SEM (n=3) and the results are representative of four separate experiments. The ratio increase in the liver at day 42 is statistically significant as compared to the spleen and lymph nodes (p<.01).
In all, these data indicate that IL-2 influences a wide spectrum of effector differentiation, from end-stage effector cells at the peak of the response to both short-lived and long-lived effector memory CTL in secondary lymphoid tissues and peripheral sites of infection. Numerically, the differentiation of central memory T appears to be independent of IL-2, as we observe roughly similar numbers of central memory phenotype WT and IL-2Rα-deficient CTL at early memory points (data not shown). Because IL-2Rα-deficient memory CTL at early memory time points are largely central memory phenotype already, the overall number of central memory cells remains stable throughout memory maintenance. On the other hand, at early memory time points the WT memory population is largely composed of short-term and long-term effector memory cells. Over time, the memory population remains stable but eventually converts to a central memory phenotype, whether due to conversion of existing effector memory cells to central memory cells (54) or replacement of effector memory cells with central memory cells due to homeostatic mechanisms (55). While the end result at late memory time points is a 3-fold difference in the number of central memory cells (Fig. 1), our results suggest that IL-2 mainly plays a role in effector and effector memory CTL differentiation and that the defect in central memory cells is more precisely one of secondary effector differentiation.
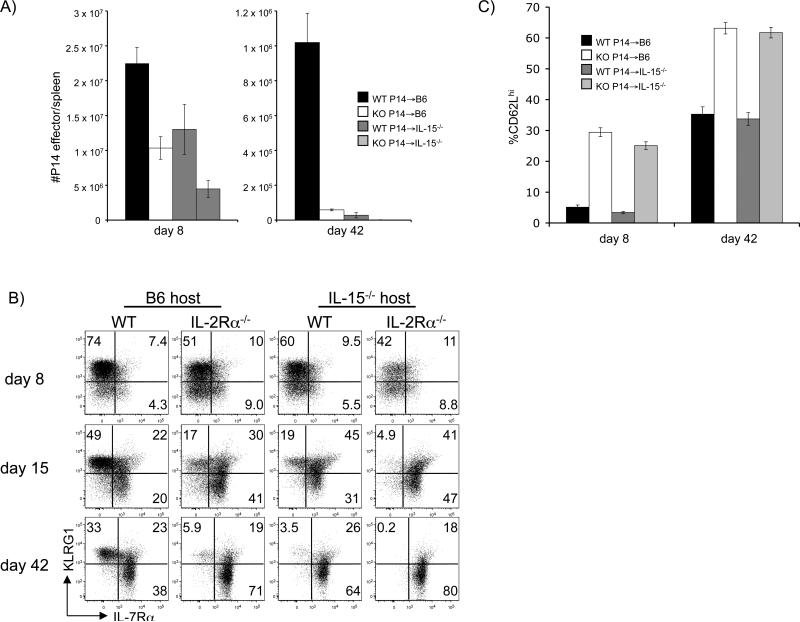
IL-2 and IL-15 jointly promote the emergence and survival of effector CTL
Although IL-2 plays an important role in CD8+ secondary effector T cell differentiation following secondary challenge, we remained puzzled by our observation that IL-2 played a much more modest role in driving robust expansion during the primary response. One likely explanation is that during in vivo infection, other growth and inflammatory factors compensate for the absence of IL-2. Of the potential candidates, we focused on IL-15. Because IL-15 is highly related to IL-2 and shares a similar signaling apparatus, we hypothesized that IL-15 signals during the primary response could cooperate with IL-2 and compensate for the lack of IL-2 signals in the differentiation of CD8+ effector and memory T cells.
In order to probe a joint role for IL-2 and IL-15 signals to CD8+ T cells, we adoptively co-transferred WT and IL-2Rα-deficient P14 cells into either WT or IL-15-deficient hosts. Because mouse CD8+ T cells are not an in vivo source of IL-15 in mice, we were able to assess the response of P14 T cells in the absence of either IL-2 or IL-15 signals, or both. At the peak of the primary response (day 8 post-infection), the absence of either IL-2 or IL-15 alone resulted in a similar decrease (~2-3-fold) in the number of end-stage effector cells (KLRG1hiIL-7Rαlo). The combined absence of both IL-2 and IL-15 signals to CD8+ T cells resulted in a further significant decrease in the number of effector CTL cells at the peak of the response, as compared to the absence of Il-2 or IL-15 signals alone (Fig. 5A-B). By day 42 post-infection, we observed a 10-20-fold decrease in the number of effector phenotype cells in the absence of IL-2 signals, as compared to WT responses. The absence of IL-15 resulted in a similar decrease in the number of effector phenotype cells at this time point. In the joint absence of IL-2 and IL-15 signals, this population was essentially undetectable, indicating a joint role for IL-2 and IL-15 in the differentiation and/or persistence of effector phenotype CD8+ T cells (Fig. 5A-B). These findings were independent of IL-15R expression, as WT and IL-2Rα-deficient P14 cells expressed similar levels of IL-15Rβ (CD122) regardless of the host (Supp. Fig. 6). Furthermore, differences were likely not due to a decrease in the rate of cell division, as similar frequencies of P14 cells expressed the cell cycle indicator Ki-67 at days 5 and 9 post-infection, regardless of the presence of IL-15 or expression of IL-2Rα (Supp. Fig. 6). Little Ki-67 staining was observed for any group at or after day 9, indicating differences in survival, as the loss of short-term effector memory cells largely coincided with a cessation of cell division (Supp. Fig. 6).
Figure 5.
IL-2 and IL-15 jointly promote the persistence of short-lived, but not long-lived, effector memory CTLs. We transferred 5 × 103 WT and IL-2Rα-deficient P14 into B6 and IL-15-deficient hosts and infected with LCMV. A, The bar graphs display the number of effector phenotype (KLRG1hiIL-7Rαlo) WT and IL-2Rα-deficient P14 responders in B6 or IL-15-deficient hosts at days 8 or 42 post-infection. Error bars indicate SEM (n=3). The decrease of P14 cells in the absence of both cytokines, as compared to each cytokine alone, is statistically significant at both time points (p<.05). B, Representative flow plots indicate the relative frequencies of effector (KLRG1hiIL-7Rαlo) and memory (KLRG1loIL-7Rαhi) phenotype cells among WT and IL-2Rα-deficient P14 responders in B6 or IL-15-deficient hosts at the indicated time points post-infection. C, The bar graph indicates the relative frequency of CD62Lhi cells among WT and IL-2Rα-deficient memory phenotype P14 responders (KLRG1loIL-7Rαhi in B6 or IL-15-deficient hosts at the indicated time points post-infection. Error bars represent the SEM (n=3). Results are representative of three separate experiments.
We further sought to determine whether IL-15 played a joint role with IL-2 in promoting the differentiation of effector memory CD8+ T cells, as measured by CD62L expression. In this case, however, IL-15 appeared to play no role. While the absence of IL-2 signals resulted in a more rapid skewing of the IL-7Rαhi memory precursor populations to a CD62Lhi central memory-like phenotype, the absence of IL-15 signals had no such effect, either alone or in combination with the absence of IL-2 signals (Fig. 5C). Because IL-15 is required for the homeostatic division and maintenance of CD8+ memory T cells (28), we did not assess later memory time points, focusing instead on the role of IL-15 in the initial establishment of memory. These findings indicated that IL-15 might play a joint role with IL-2 in promoting the differentiation and/or survival of effector CD8+ T cells but suggested distinct roles for these two cytokines in the differentiation of CD8+ memory T cell subsets. While IL-15 promoted the survival and turnover of CD8+ memory T cells over long periods of time, we saw little impact on CD8+ memory T cell numbers in the absence of IL-15 at the early memory time points assessed in this study, consistent with prior reports (30).
Disparate roles for IL-2 and IL-15 in the differentiation and survival of KLRG1hiIL-7Rαlo effector CTL
We considered two possible roles for IL-15 in promoting short-term effector/effector memory CTL populations. First, IL-15 signals during the priming and expansion phase might be important for their differentiation, similar to the role of IL-2. Our initial transfers of P14 cells into IL-15-deficient animals seemed to imply that this could be the case at least in part, as fewer effector phenotype CTL were present at the peak of the primary response in the absence of IL-15 or IL-2 signals alone, and further decreased in their joint absence. On the other hand, IL-15 has been shown to play a key role in the survival of KLRG1hiIL-7Rαlo effector phenotype CTL during the contraction phase (3, 51, 56), and we considered as an alternative that IL-15 was required only for the survival of these cells, not their differentiation.
In order to distinguish a potential differentiation role for IL-15 during the primary response from its known survival role thereafter, we limited, through adoptive transfer, the availability of IL-15 signals to WT or IL-2Rα-deficient P14 responders to the primary phase (days 0-8) or the contraction phase (days 8-42) of the T cell response. We co-transferred WT and IL-2Rα-deficient P14 in into B6 mice and infected with LCMV. At day 8 post-infection, WT and IL-2Rα-deficient P14 CTL were harvested from the spleen and transferred into infection-matched B6 or IL-15-deficient secondary hosts. We subsequently analyzed the persistence of WT or IL-2Rα-deficient end-stage effector cells that lacked IL-15 signals during the primary response only, during the contraction phase only, or both. As before, we found that the absence of IL-15 during both the primary response and the contraction phase severely curtailed the persistence of KLRG1hiIL-7Rαlo effector cells and that the effect was exacerbated in the additional absence of IL-2 (Fig. 6). Similar results were observed when IL-15 signals were absent during the contraction phase only (Fig. 6). In contrast, the absence of IL-15 during the primary response alone resulted in levels of effector CTL levels similar to those seen following transfer of WT and IL-2Rα-deficient P14 into WT B6 hosts (Fig. 6). These findings conclusively demonstrate that in contrast to IL-2 the primary role for IL-15 in this setting is the survival of KLRG1hi effector phenotype CTL, not their differentiation.
Figure 6.
IL-15 is required for the survival but not differentiation of short-lived effector CTL. We transferred 5 × 103 WT and IL-2Rα-deficient P14 into B6 and IL-15-deficient hosts and infected with LCMV. At day 8 post-infection, we isolated CD8+ T cells from their spleens using magnetic beads and transferred them to infection-matched secondary B6 or IL-15-deficient hosts. Representative flow plots indicate the relative frequencies of effector (KLRG1hiIL-7Rαlo) and memory (KLRG1loIL-7Rαhi) phenotype cells among WT and IL-2Rα-deficient P14 responders in the spleens of secondary hosts at day 42 post-infection.
IL-15 is not required for secondary CD8+ T cell expansion and effector differentiation
We next assessed whether IL-15 shared an overlapping role with IL-2 in the differentiation of CD8+ memory T cells capable of secondary responses. We co-transferred 500 WT and IL-2Rα-deficient P14 into B6 or IL-15-deficient mice and infected with LCMV as previously. At 42 days post-infection, mice were rechallenged with Lm-gp33. WT P14 memory cells expanded robustly by day 5 post-rechallenge regardless of the presence or absence of IL-15 signals (Fig. 7A). They also differentiated into secondary effector CTL as determined by expression of IL-7Rα and KLRG1 (Fig. 7B) and their cytokine production profile (Fig. 7C). As observed previously, IL-2Rα-deficient memory cells responded poorly to secondary challenge and failed to acquire phenotypic or functional (cytokine-producing) characteristics indicative of secondary effector differentiation. However, this phenotype was not exacerbated in the absence of IL-15, again indicating that the functional role of IL-2 and IL-15 in CTL memory differentiation and survival were non-overlapping (Fig. 7A-C).
Figure 7.
IL-15 is not required for the generation of secondary effector CTL. We transferred 500 WT and IL-2Rα-deficient P14 into B6 and IL-15-deficient hosts and infected with LCMV. At day 42 post-infection, we rechallenged mice with Lm-gp33 and assessed recall responses in the spleen 5 days later. A, The bar graph indicates the fold expansion 5 days after rechallenge of WT and IL-2Rα-deficient P14 responders in B6 or IL-15-deficient hosts. Error bars indicate SEM (n=3/group). B, The pie charts indicate the average frequency of WT or IL-2Rα-deficient P14 secondary responders in WT or IL-15-deficient hosts that make IFNγ after 4-hour restimulation and that also produce TNFα and/or IL-2 (n=3). C, Representative plots indicate the relative frequency of effector phenotype secondary responders (KLRG1hiIL-7Rαlo) among WT and IL-2Rα-deficient P14 cells in WT or IL-15-deficient hosts.
Discussion
Our understanding of the role of IL-2 during in vivo immune responses has undergone changes and revisions over the years. Although it was originally thought to be required for T cell expansion, we find robust CD8+ T cell expansion even in the complete absence of high affinity IL-2 signals. However, our findings suggest that IL-2 plays a unique and important role as a fate determination and differentiation signal for activated T cells in vivo. Here again, the role of IL-2 is complex. While IL-2 plays a role in promoting the emergence and function of effector CTLs during the primary response, its impact is particularly pronounced in the rapid disappearance of this population during the contraction phase. Expression of the high affinity IL-2 receptor generally corresponds with bursts of IL-2 production in vivo, with the notable exception of the regulatory T cell subset. We observe little to no expression of IL-2Rα at day 8 post-infection or beyond, indicating that the high affinity IL-2R signal is confined to the primary T cell response and expansion phase. We therefore conclude that IL-2 signals during priming influence the generation of effector CTL during primary expansion and the persistence of short-term effector memory CTL once the virus is cleared. These findings are consistent with previous results demonstrating that IL-2 signals during the first week of infection promote the subsequent survival of IL-7Rαlo and CD62Llo responders during the contraction phase (15). Two recent reports have also demonstrated a role for IL-2 in driving effector CTL differentiation. These studies found that effector CTL differentiation was influenced by the concentration of IL-2 following activation (57) or by the length of time activated CTLs were able to incorporate high affinity IL-2 signals (58). Together with our current report, these studies demonstrate a non-redundant role for IL-2 in enhancing effector CTL differentiation, survival and function. Our report further demonstrates that in the complete absence of high affinity IL-2 signals, secondary effector CTL differentiation is dramatically impaired. One intriguing possibility is that while strong IL-2 signals enhance effector differentiation, some IL-2 signals are required in order for memory precursor effector cells to maintain, perhaps through epigenetic changes, their ability to access the effector differentiation transcriptional program. Thus memory cells generated in the absence of IL-2 signals would be largely unable to enter an effector differentiation pathway upon reactivation. Future studies are needed to identify epigenetic changes as well as changes in transcriptional activity that are influenced by IL-2 signals in differentiating CTL in vivo.
Of particular interest is our finding that the generation and/or survival of secondary effector CTL is largely disabled in the absence of IL-2 signals. Our prior findings have demonstrated that IL-2Rα-deficient CD8+ memory T cells divide rapidly upon rechallenge but fail to accumulate as compared to wildtype memory cells (15). We find here that despite their rapid division, almost no secondary effector CTL emerge in the absence of IL-2 signals. While there is some evidence of effector differentiation, including up-regulation of KLRG1, secondary effector cells rapidly disappear from the response, suggesting that IL-2 provides a differentiation signal to activated T cells that enables or potentiates entry into an effector/effector memory lineage. Prior studies have shown that secondary effector and memory T cells skew more strongly to the effector and/or effector memory lineage, maintaining low levels of CD62L over long periods of time as compared to primary memory T cells (59).
We propose that IL-2 provides a differentiation signal that enables entry into and survival within the effector “program”. This may include epigenetic imprinting during the primary response that enable or potentiate effector differentiation upon subsequent encounters with antigen. Because CD8+ memory T cells are prone to become highly differentiated secondary effector/effector memory cells upon secondary activation, the absence of an IL-2-driven effector differentiation signal during the primary response may specifically and adversely impact the generation of highly differentiated secondary effector CTL. In this sense, IL-2 may be most appropriately described as an effector differentiation factor rather than a memory differentiation factor. While it may not be required for the selection of memory populations during the primary response, its role in driving effector differentiation is a key step in conferring the ability of memory T cells that do emerge to differentiate into effector cells upon secondary engagement with antigen.
The molecular and transcriptional nature of the IL-2-driven effector differentiation program remains unknown. Several transcription factors have been implicated in the differentiation of CD8+ effector T cells. Of particular interest are the Tbox transcription factors T-bet and Eomesodermin (Eomes). T-bet and Eomes drive effector differentiation and are regulated in response to inflammatory signals such as IL-12 or Type I IFNs (3, 60). Eomes impacts the differentiation and survival of CD8+ effector T cells by influencing the expression of effector molecules such as IFNγ and CD122 (51). Another molecule of interest is the transcriptional repressor Blimp-1. While past studies have focused on the role of Blimp-1 in plasma cell differentiation, recent studies suggest an important role for this molecule in CD8+ effector differentiation (61, 62) during acute viral infection and CD8+ T cell exhaustion (63) during chronic viral infection. Blimp-1 induction during in vitro T cell activation is dependent on IL-2 and forms a feedback loop to inhibit IL-2 production (64). Additionally, similar to responding CD8 T cells that do not receive IL-2 signals, Blimp-1 deficient CD8 T cells also show a defect in effector and effector memory differentiation following acute infection (61, 62), as well as a reduced ability of Blimp-1 deficient memory cells to respond to rechallenge (61).
The levels of T-bet and Eomes protein expression, as well as Blimp-1 mRNA expression, were not reduced in the absence of IL-2 signals. While we do not find an obligate role for IL-2 in inducing expression of any of these transcription factors during the in vivo response to viral infection, we do not rule out a role for IL-2 in controlling, directly or indirectly, their transcription factor activity post-transcriptionally or post-translationally. Because Blimp-1, which has recently been shown to promote effector and memory CTL differentiation (61, 62), is a potential repressor of Bcl-6 expression in T cells (65), our finding that Bcl-6 expression is reduced in the absence of IL-2 signals leaves open the possibility that its activity is post-transcriptionally or post-translationally reduced in the absence of IL-2 signals, despite no changes in mRNA expression. Although expression of the transcription factors T-bet, Eomes, and Blimp-1 are associated with effector CTL differentiation, less is known about how these transcription factors function and are regulated. For example, there may be activating and/or repressive binding partners and/or modifications affecting their activity. Thus, although our data shows that IL-2 is not obligatory for induction of expression of these factors, there are several ways in which IL-2 signals could result in alterations to transcriptional activity and, ultimately, the ability of a responding CD8+ T cell to undergo effector differentiation. Furthermore, even modest differences (<2-fold) in expression and/or activity of some of these transcription factors may have a profound impact on T cell differentiation and function. Future studies will be needed to precisely elucidate the combined role of these transcription factors and others (such as the Blimp-1 repressor Bcl-6 (66, 67)) in the differentiation of CD8+ primary and secondary effector and effector memory T cells, along with the impact of inflammatory mediators and cytokines such as IL-2 on their activity.
In the absence of IL-2 signals, effector CTL undergo massive expansion. It is possible that the milieu of growth and inflammatory factors available during the infectious burst can compensate for the lack of IL-2 signals. This hypothesis is supported by the fact that IL-2 is one member of a family of cytokines linked by their receptor usage. Because the signaling apparatus used by IL-2 and IL-15 is largely shared, it is presently unclear what the differences are in the signals that account for their distinct biological effects. While we find a role for IL-15 in the survival of CD8+ effector T cells after antigen clearance, it does not play a role in the differentiation of this population during primary activation, nor is it required for the differentiation of functionally competent CD8+ memory T cells. Instead, our findings suggest that IL-15 plays a fundamentally distinct role from that of IL-2, promoting no the differentiation but survival of CD8+ memory T cells.
Because our prior studies found a role for IL-2 in promoting secondary CTL responses in both LCMV and Listeria infectious model systems (15), we concluded that IL-2 played a broad role in memory CTL differentiation in disparate model systems. While the role of IL-2 in promoting secondary responses following LCMV infection have also been observed by another group (68), one recent study, while also reporting a role for IL-2 in driving effector CTL differentiation following Listeria infection, found that the recall capacity of the resulting memory cells was IL-2 independent (53). It remains possible therefore that the role of IL-2 may depend on the pathogenic stimulus. Clearly the impact of IL-2 in driving the differentiation of effector and memory CTL requires further study. One complicating factor may be the presence of redundancy within the immune system. Several other cytokines, such as IL-7 and IL-21, also utilize the γc as a component of their receptors, and these cytokines send a common TCR-independent proliferative signal via the STAT5 and STAT3 transcription factors (69). It is not clear, however, whether the programming of functional memory cells by IL-2 represents a unique signal from IL-2 that IL-7, IL-21 or other γc -family member cytokines are unable to deliver, or if it represents a common signal, perhaps mediated by STAT5, that any member of the family could redundantly deliver during T cell activation and differentiation, were it present in sufficient amounts and its receptor expressed. Future experiments should focus on both redundancy of family member function as well the nature of the pathogenic stimulus in interpreting the in vivo function of IL-2. Due to its role in effector differentiation, future studies will benefit from analyzing the role of IL-2 in models of localized tissue infection.
Our results suggest that IL-15 signals do not overlap with IL-2 signals, but this may reflect differences in receptor expression and cytokine availability. Because IL-15 is expressed in trans (37), T cells must be in close proximity to potential IL-15 producers. It is unclear the extent to which IL-15 signals are available to differentiating CTLs during the primary response, but IL-15 presented by dendritic cells has been shown to induce homeostatic proliferation of memory T cells (38). It is possible that the levels of IL-15 available to T cells differ depending on the nature of the pathogenic stimulus, and our results do not rule out a potential role for IL-15 during primary T cell differentiation if present at high enough concentrations in other infectious model systems. IL-2, on the other hand, is secreted at high levels upon activation and is probably available to differentiating CTLs throughout the primary expansion phase. One intriguing candidate member of this family with similar induction kinetics is IL-21, which, like IL-2, is largely expressed by CD4+ T cells, is induced upon activation and promotes enhanced cytotoxicity by CD8+ T cells (70). Furthermore, IL-21 has been shown to induce both Blimp-1 and Bcl-6 expression during B cell activation and differentiation, suggesting the intriguing possibility that IL-21 may play an effector/memory differentiation role for T cells (71). Recent studies found that like IL-2 (68), IL-21 signals to T cells were not required for primary CTL expansion but did promote their ability to control chronic infection (72-74).
IL-2 is used as an immunotherapy in situations where the inflammatory burst is comparatively minimal, such as for anti-tumor immune responses (75). IL-2 also appears to play a significant role in maintaining effector/memory responses during chronic infections (68), indicating that the long-term ability to respond to antigen may require IL-2. It is in this way, perhaps, that in vivo responses reflect the need for IL-2 in promoting the establishment and maintenance of T cell lines in vitro. We anticipate that a more detailed understanding of the role of IL-2 in the differentiation and function of antigen-activated T cells will greatly enhance our understanding of memory T cell biology. In particular, defining its role will aid in a variety of therapeutic strategies aimed at manipulating the T cell response. These include vaccination, immunotherapeutic or immunomodulatory strategies aimed at boosting the immune response, tumor eradication by immune cells, and strategies for which immunosuppression is desirable, such as for prevention of autoimmune responses or transplant rejection.
Supplementary Material
Acknowledgements
We acknowledge the technical assistance of J. Strickland and J. Cassiano.
Footnotes
This work was supported by the NIH (K22AI071112) and the Department of Pathology at the University of Utah.
Abbreviations used in this manuscript: short-lived effector cell, SLEC; protein tyrosine kinase, PTK; C57BL/6, B6; lymphocytic choriomeningitis virus, LCMV; vaccinia virus expressing secreted LCMV GP, VV-GP; Listeria monocytogenes expressing LCMV GP34-41, Lm-gp33; plague forming unit, PFU; colony forming unit, CFU; intraperitoneal, i.p.; intravenous, i.v.
References
- 1.Kaech SM, Wherry EJ. Heterogeneity and cell-fate decisions in effector and memory CD8+ T cell differentiation during viral infection. Immunity. 2007;27:393–405. doi: 10.1016/j.immuni.2007.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams MA, Bevan MJ. Effector and memory CTL differentiation. Annu Rev Immunol. 2007;25:171–192. doi: 10.1146/annurev.immunol.25.022106.141548. [DOI] [PubMed] [Google Scholar]
- 3.Joshi NS, Cui W, Chandele A, Lee HK, Urso DR, Hagman J, Gapin L, Kaech SM. Inflammation directs memory precursor and short-lived effector CD8(+) T cell fates via the graded expression of T-bet transcription factor. Immunity. 2007;27:281–295. doi: 10.1016/j.immuni.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaech SM, Tan JT, Wherry EJ, Konieczny BT, Surh CD, Ahmed R. Selective expression of the interleukin 7 receptor identifies effector CD8 T cells that give rise to long-lived memory cells. Nat Immunol. 2003;4:1191–1198. doi: 10.1038/ni1009. [DOI] [PubMed] [Google Scholar]
- 5.Bevan MJ. Helping the CD8(+) T-cell response. Nat Rev Immunol. 2004;4:595–602. doi: 10.1038/nri1413. [DOI] [PubMed] [Google Scholar]
- 6.Janssen EM, Droin NM, Lemmens EE, Pinkoski MJ, Bensinger SJ, Ehst BD, Griffith TS, Green DR, Schoenberger SP. CD4+ T-cell help controls CD8+ T-cell memory via TRAIL-mediated activation-induced cell death. Nature. 2005;434:88–93. doi: 10.1038/nature03337. [DOI] [PubMed] [Google Scholar]
- 7.Janssen EM, Lemmens EE, Wolfe T, Christen U, von Herrath MG, Schoenberger SP. CD4+ T cells are required for secondary expansion and memory in CD8+ T lymphocytes. Nature. 2003;421:852–856. doi: 10.1038/nature01441. [DOI] [PubMed] [Google Scholar]
- 8.Shedlock DJ, Shen H. Requirement for CD4 T Cell Help in Generating Functional CD8 T Cell Memory. Science. 2003;300:337–339. doi: 10.1126/science.1082305. [DOI] [PubMed] [Google Scholar]
- 9.Sun JC, Bevan MJ. Defective CD8 T Cell Memory Following Acute Infection Without CD4 T Cell Help. Science. 2003;300:339–342. doi: 10.1126/science.1083317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang JT, Palanivel VR, Kinjyo I, Schambach F, Intlekofer AM, Banerjee A, Longworth SA, Vinup KE, Mrass P, Oliaro J, Killeen N, Orange JS, Russell SM, Weninger W, Reiner SL. Asymmetric T lymphocyte division in the initiation of adaptive immune responses. Science. 2007;315:1687–1691. doi: 10.1126/science.1139393. [DOI] [PubMed] [Google Scholar]
- 11.Reiner SL, Sallusto F, Lanzavecchia A. Division of labor with a workforce of one: challenges in specifying effector and memory T cell fate. Science. 2007;317:622–625. doi: 10.1126/science.1143775. [DOI] [PubMed] [Google Scholar]
- 12.D'Souza WN, Hedrick SM. Cutting edge: latecomer CD8 T cells are imprinted with a unique differentiation program. J Immunol. 2006;177:777–781. doi: 10.4049/jimmunol.177.2.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D'Souza WN, Lefrancois L. IL-2 is not required for the initiation of CD8 T cell cycling but sustains expansion. J Immunol. 2003;171:5727–5735. doi: 10.4049/jimmunol.171.11.5727. [DOI] [PubMed] [Google Scholar]
- 14.Yu A, Zhou J, Marten N, Bergmann CC, Mammolenti M, Levy RB, Malek TR. Efficient induction of primary and secondary T cell-dependent immune responses in vivo in the absence of functional IL-2 and IL-15 receptors. J Immunol. 2003;170:236–242. doi: 10.4049/jimmunol.170.1.236. [DOI] [PubMed] [Google Scholar]
- 15.Williams MA, Tyznik AJ, Bevan MJ. Interleukin-2 signals during priming are required for secondary expansion of CD8+ memory T cells. Nature. 2006;441:890–893. doi: 10.1038/nature04790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manjunath N, Shankar P, Wan J, Weninger W, Crowley MA, Hieshima K, Springer TA, Fan X, Shen H, Lieberman J, von Andrian UH. Effector differentiation is not prerequisite for generation of memory cytotoxic T lymphocytes. J Clin Invest. 2001;108:871–878. doi: 10.1172/JCI13296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weninger W, Crowley MA, Manjunath N, von Andrian UH. Migratory properties of naive, effector, and memory CD8(+) T cells. J Exp Med. 2001;194:953–966. doi: 10.1084/jem.194.7.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atkins MB, Lotze MT, Dutcher JP, Fisher RI, Weiss G, Margolin K, Abrams J, Sznol M, Parkinson D, Hawkins M, Paradise C, Kunkel L, Rosenberg SA. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17:2105–2116. doi: 10.1200/JCO.1999.17.7.2105. [DOI] [PubMed] [Google Scholar]
- 19.McDermott DF. Immunotherapy of metastatic renal cell carcinoma. Cancer. 2009;115:2298–2305. doi: 10.1002/cncr.24236. [DOI] [PubMed] [Google Scholar]
- 20.Rosenberg SA, Yang JC, Topalian SL, Schwartzentruber DJ, Weber JS, Parkinson DR, Seipp CA, Einhorn JH, White DE. Treatment of 283 consecutive patients with metastatic melanoma or renal cell cancer using high-dose bolus interleukin 2. JAMA. 1994;271:907–913. [PubMed] [Google Scholar]
- 21.Halwani R, Boyer JD, Yassine-Diab B, Haddad EK, Robinson TM, Kumar S, Parkinson R, Wu L, Sidhu MK, Phillipson-Weiner R, Pavlakis GN, Felber BK, Lewis MG, Shen A, Siliciano RF, Weiner DB, Sekaly RP. Therapeutic vaccination with simian immunodeficiency virus (SIV)-DNA + IL-12 or IL-15 induces distinct CD8 memory subsets in SIV-infected macaques. J Immunol. 2008;180:7969–7979. doi: 10.4049/jimmunol.180.12.7969. [DOI] [PubMed] [Google Scholar]
- 22.Oh S, Berzofsky JA, Burke DS, Waldmann TA, Perera LP. Coadministration of HIV vaccine vectors with vaccinia viruses expressing IL-15 but not IL-2 induces long-lasting cellular immunity. Proc Natl Acad Sci U S A. 2003;100:3392–3397. doi: 10.1073/pnas.0630592100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perera LP, Waldmann TA, Mosca JD, Baldwin N, Berzofsky JA, Oh SK. Development of smallpox vaccine candidates with integrated interleukin-15 that demonstrate superior immunogenicity, efficacy, and safety in mice. J Virol. 2007;81:8774–8783. doi: 10.1128/JVI.00538-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waldmann TA. The biology of interleukin-2 and interleukin-15: implications for cancer therapy and vaccine design. Nat Rev Immunol. 2006;6:595–601. doi: 10.1038/nri1901. [DOI] [PubMed] [Google Scholar]
- 25.Leone A, Picker LJ, Sodora DL. IL-2, IL-7 and IL-15 as immunomodulators during SIV/HIV vaccination and treatment. Curr HIV Res. 2009;7:83–90. doi: 10.2174/157016209787048519. [DOI] [PubMed] [Google Scholar]
- 26.Yajima T, Nishimura H, Wajjwalku W, Harada M, Kuwano H, Yoshikai Y. Overexpression of interleukin-15 in vivo enhances antitumor activity against MHC class I-negative and -positive malignant melanoma through augmented NK activity and cytotoxic T-cell response. Int J Cancer. 2002;99:573–578. doi: 10.1002/ijc.10395. [DOI] [PubMed] [Google Scholar]
- 27.Kobayashi H, Dubois S, Sato N, Sabzevari H, Sakai Y, Waldmann TA, Tagaya Y. Role of trans-cellular IL-15 presentation in the activation of NK cell-mediated killing, which leads to enhanced tumor immunosurveillance. Blood. 2005;105:721–727. doi: 10.1182/blood-2003-12-4187. [DOI] [PubMed] [Google Scholar]
- 28.Surh CD, Sprent J. Homeostasis of naive and memory T cells. Immunity. 2008;29:848–862. doi: 10.1016/j.immuni.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Becker TC, Wherry EJ, Boone D, Murali-Krishna K, Antia R, Ma A, Ahmed R. Interleukin 15 is required for proliferative renewal of virus-specific memory CD8 T cells. J Exp Med. 2002;195:1541–1548. doi: 10.1084/jem.20020369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wherry EJ, Becker TC, Boone D, Kaja MK, Ma A, Ahmed R. Homeostatic proliferation but not the generation of virus specific memory CD8 T cells is impaired in the absence of IL-15 or IL-15Ralpha. Adv Exp Med Biol. 2002;512:165–175. doi: 10.1007/978-1-4615-0757-4_22. [DOI] [PubMed] [Google Scholar]
- 31.Schluns KS, Williams K, Ma A, Zheng XX, Lefrancois L. Cutting edge: requirement for IL-15 in the generation of primary and memory antigen-specific CD8 T cells. J Immunol. 2002;168:4827–4831. doi: 10.4049/jimmunol.168.10.4827. [DOI] [PubMed] [Google Scholar]
- 32.Kaech SM, Ahmed R. Memory CD8+ T cell differentiation: initial antigen encounter triggers a developmental program in naive cells. Nat Immunol. 2001;2:415–422. doi: 10.1038/87720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Stipdonk MJ, Hardenberg G, Bijker MS, Lemmens EE, Droin NM, Green DR, Schoenberger SP. Dynamic programming of CD8+ T lymphocyte responses. Nat Immunol. 2003;4:361–365. doi: 10.1038/ni912. [DOI] [PubMed] [Google Scholar]
- 34.Bodnar A, Nizsaloczki E, Mocsar G, Szaloki N, Waldmann TA, Damjanovich S, Vamosi G. A biophysical approach to IL-2 and IL-15 receptor function: localization, conformation and interactions. Immunol Lett. 2008;116:117–125. doi: 10.1016/j.imlet.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 35.Alves NL, Arosa FA, van Lier RA. Common gamma chain cytokines: dissidence in the details. Immunol Lett. 2007;108:113–120. doi: 10.1016/j.imlet.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Burkett PR, Koka R, Chien M, Chai S, Boone DL, Ma A. Coordinate expression and trans presentation of interleukin (IL)-15Ralpha and IL-15 supports natural killer cell and memory CD8+ T cell homeostasis. J Exp Med. 2004;200:825–834. doi: 10.1084/jem.20041389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sandau MM, Schluns KS, Lefrancois L, Jameson SC. Cutting Edge: Transpresentation of IL-15 by Bone Marrow-Derived Cells Necessitates Expression of IL-15 and IL-15R{alpha} by the Same Cells. J Immunol. 2004;173:6537–6541. doi: 10.4049/jimmunol.173.11.6537. [DOI] [PubMed] [Google Scholar]
- 38.Stonier SW, Ma LJ, Castillo EF, Schluns KS. Dendritic cells drive memory CD8 T-cell homeostasis via IL-15 transpresentation. Blood. 2008;112:4546–4554. doi: 10.1182/blood-2008-05-156307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmed R, Salmi A, Butler LD, Chiller JM, Oldstone MB. Selection of genetic variants of lymphocytic choriomeningitis virus in spleens of persistently infected mice. Role in suppression of cytotoxic T lymphocyte response and viral persistence. J Exp Med. 1984;160:521–540. doi: 10.1084/jem.160.2.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shen H, Slifka MK, Matloubian M, Jensen ER, Ahmed R, Miller JF. Recombinant Listeria monocytogenes as a live vaccine vehicle for the induction of protective anti-viral cell-mediated immunity. Proc Natl Acad Sci U S A. 1995;92:3987–3991. doi: 10.1073/pnas.92.9.3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Slifka MK, Shen H, Matloubian M, Jensen ER, Miller JF, Ahmed R. Antiviral cytotoxic T-cell memory by vaccination with recombinant Listeria monocytogenes. J Virol. 1996;70:2902–2910. doi: 10.1128/jvi.70.5.2902-2910.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams MA, Ravkov EV, Bevan MJ. Rapid culling of the CD4+ T cell repertoire in the transition from effector to memory. Immunity. 2008;28:533–545. doi: 10.1016/j.immuni.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whitton JL, Southern PJ, Oldstone MB. Analyses of the cytotoxic T lymphocyte responses to glycoprotein and nucleoprotein components of lymphocytic choriomeningitis virus. Virology. 1988;162:321–327. doi: 10.1016/0042-6822(88)90471-0. [DOI] [PubMed] [Google Scholar]
- 44.Williams MA, Bevan MJ. Shortening the infectious period does not alter expansion of CD8 T cells but diminishes their capacity to differentiate into memory cells. J Immunol. 2004;173:6694–6702. doi: 10.4049/jimmunol.173.11.6694. [DOI] [PubMed] [Google Scholar]
- 45.Cruz-Guilloty F, Pipkin ME, Djuretic IM, Levanon D, Lotem J, Lichtenheld MG, Groner Y, Rao A. Runx3 and T-box proteins cooperate to establish the transcriptional program of effector CTLs. J Exp Med. 2009;206:51–59. doi: 10.1084/jem.20081242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Altman JD, Moss PA, Goulder PJ, Barouch DH, McHeyzer-Williams MG, Bell JI, McMichael AJ, Davis MM. Phenotypic analysis of antigen-specific T lymphocytes. Science. 1996;274:94–96. [PubMed] [Google Scholar]
- 47.Murali-Krishna K, Altman JD, Suresh M, Sourdive DJ, Zajac AJ, Miller JD, Slansky J, Ahmed R. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity. 1998;8:177–187. doi: 10.1016/s1074-7613(00)80470-7. [DOI] [PubMed] [Google Scholar]
- 48.Fontenot JD, Rasmussen JP, Gavin MA, Rudensky AY. A function for interleukin 2 in Foxp3-expressing regulatory T cells. Nat Immunol. 2005;6:1142–1151. doi: 10.1038/ni1263. [DOI] [PubMed] [Google Scholar]
- 49.Malek TR, Bayer AL. Tolerance, not immunity, crucially depends on IL-2. Nat Rev Immunol. 2004;4:665–674. doi: 10.1038/nri1435. [DOI] [PubMed] [Google Scholar]
- 50.Setoguchi R, Hori S, Takahashi T, Sakaguchi S. Homeostatic maintenance of natural Foxp3+ CD25+ CD4+ regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J. Exp. Med. 2005;201:723–735. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Intlekofer AM, Takemoto N, Wherry EJ, Longworth SA, Northrup JT, Palanivel VR, Mullen AC, Gasink CR, Kaech SM, Miller JD, Gapin L, Ryan K, Russ AP, Lindsten T, Orange JS, Goldrath AW, Ahmed R, Reiner SL. Effector and memory CD8+ T cell fate coupled by T-bet and eomesodermin. Nat Immunol. 2005;6:1236–1244. doi: 10.1038/ni1268. [DOI] [PubMed] [Google Scholar]
- 52.Pearce EL, Mullen AC, Martins GA, Krawczyk CM, Hutchins AS, Zediak VP, Banica M, DiCioccio CB, Gross DA, Mao CA, Shen H, Cereb N, Yang SY, Lindsten T, Rossant J, Hunter CA, Reiner SL. Control of effector CD8+ T cell function by the transcription factor Eomesodermin. Science. 2003;302:1041–1043. doi: 10.1126/science.1090148. [DOI] [PubMed] [Google Scholar]
- 53.Obar JJ, Molloy MJ, Jellison ER, Stoklasek TA, Zhang W, Usherwood EJ, Lefrancois L. CD4+ T cell regulation of CD25 expression controls development of short-lived effector CD8+ T cells in primary and secondary responses. Proc Natl Acad Sci U S A. 2009 doi: 10.1073/pnas.0909945107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sarkar S, Teichgraber V, Kalia V, Polley A, Masopust D, Harrington LE, Ahmed R, Wherry EJ. Strength of stimulus and clonal competition impact the rate of memory CD8 T cell differentiation. J Immunol. 2007;179:6704–6714. doi: 10.4049/jimmunol.179.10.6704. [DOI] [PubMed] [Google Scholar]
- 55.Marzo AL, Klonowski KD, Le Bon A, Borrow P, Tough DF, Lefrancois L. Initial T cell frequency dictates memory CD8+ T cell lineage commitment. Nat Immunol. 2005;6:793–799. doi: 10.1038/ni1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rubinstein MP, Lind NA, Purton JF, Filippou P, Best JA, McGhee PA, Surh CD, Goldrath AW. IL-7 and IL-15 differentially regulate CD8+ T cell subsets during contraction of the immune response. Blood. 2008 doi: 10.1182/blood-2008-06-160945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pipkin ME, Sacks JA, Cruz-Guilloty F, Lichtenheld MG, Bevan MJ, Rao A. Interleukin-2 and inflammation induce distinct transcriptional programs that promote the differentiation of effector cytolytic T cells. Immunity. 32:79–90. doi: 10.1016/j.immuni.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalia V, Sarkar S, Subramaniam S, Haining WN, Smith KA, Ahmed R. Prolonged interleukin-2Ralpha expression on virus-specific CD8+ T cells favors terminal-effector differentiation in vivo. Immunity. 32:91–103. doi: 10.1016/j.immuni.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 59.Jabbari A, Harty JT. Secondary memory CD8+ T cells are more protective but slower to acquire a central-memory phenotype. J Exp Med. 2006;203:919–932. doi: 10.1084/jem.20052237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Agarwal P, Raghavan A, Nandiwada SL, Curtsinger JM, Bohjanen PR, Mueller DL, Mescher MF. Gene regulation and chromatin remodeling by IL-12 and type I IFN in programming for CD8 T cell effector function and memory. J Immunol. 2009;183:1695–1704. doi: 10.4049/jimmunol.0900592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kallies A, Xin A, Belz GT, Nutt SL. Blimp-1 transcription factor is required for the differentiation of effector CD8(+) T cells and memory responses. Immunity. 2009;31:283–295. doi: 10.1016/j.immuni.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 62.Rutishauser RL, Martins GA, Kalachikov S, Chandele A, Parish IA, Meffre E, Jacob J, Calame K, Kaech SM. Transcriptional repressor Blimp-1 promotes CD8(+) T cell terminal differentiation and represses the acquisition of central memory T cell properties. Immunity. 2009;31:296–308. doi: 10.1016/j.immuni.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shin H, Blackburn SD, Intlekofer AM, Kao C, Angelosanto JM, Reiner SL, Wherry EJ. A role for the transcriptional repressor Blimp-1 in CD8(+) T cell exhaustion during chronic viral infection. Immunity. 2009;31:309–320. doi: 10.1016/j.immuni.2009.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gong D, Malek TR. Cytokine-dependent Blimp-1 expression in activated T cells inhibits IL-2 production. J Immunol. 2007;178:242–252. doi: 10.4049/jimmunol.178.1.242. [DOI] [PubMed] [Google Scholar]
- 65.Cimmino L, Martins GA, Liao J, Magnusdottir E, Grunig G, Perez RK, Calame KL. Blimp-1 attenuates Th1 differentiation by repression of ifng, tbx21, and bcl6 gene expression. J Immunol. 2008;181:2338–2347. doi: 10.4049/jimmunol.181.4.2338. [DOI] [PubMed] [Google Scholar]
- 66.Martins G, Calame K. Regulation and functions of Blimp-1 in T and B lymphocytes. Annu Rev Immunol. 2008;26:133–169. doi: 10.1146/annurev.immunol.26.021607.090241. [DOI] [PubMed] [Google Scholar]
- 67.Shaffer AL, Yu X, He Y, Boldrick J, Chan EP, Staudt LM. BCL-6 represses genes that function in lymphocyte differentiation, inflammation, and cell cycle control. Immunity. 2000;13:199–212. doi: 10.1016/s1074-7613(00)00020-0. [DOI] [PubMed] [Google Scholar]
- 68.Bachmann MF, Wolint P, Walton S, Schwarz K, Oxenius A. Differential role of IL-2R signaling for CD8+ T cell responses in acute and chronic viral infections. Eur J Immunol. 2007;37:1502–1512. doi: 10.1002/eji.200637023. [DOI] [PubMed] [Google Scholar]
- 69.Kovanen PE, Leonard WJ. Cytokines and immunodeficiency diseases: critical roles of the gamma(c)-dependent cytokines interleukins 2, 4, 7, 9, 15, and 21, and their signaling pathways. Immunol Rev. 2004;202:67–83. doi: 10.1111/j.0105-2896.2004.00203.x. [DOI] [PubMed] [Google Scholar]
- 70.Spolski R, Leonard WJ. Interleukin-21: basic biology and implications for cancer and autoimmunity. Annu Rev Immunol. 2008;26:57–79. doi: 10.1146/annurev.immunol.26.021607.090316. [DOI] [PubMed] [Google Scholar]
- 71.Ozaki K, Spolski R, Ettinger R, Kim HP, Wang G, Qi CF, Hwu P, Shaffer DJ, Akilesh S, Roopenian DC, Morse HC, 3rd, Lipsky PE, Leonard WJ. Regulation of B cell differentiation and plasma cell generation by IL-21, a novel inducer of Blimp-1 and Bcl-6. J Immunol. 2004;173:5361–5371. doi: 10.4049/jimmunol.173.9.5361. [DOI] [PubMed] [Google Scholar]
- 72.Elsaesser H, Sauer K, Brooks DG. IL-21 is required to control chronic viral infection. Science. 2009;324:1569–1572. doi: 10.1126/science.1174182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Frohlich A, Kisielow J, Schmitz I, Freigang S, Shamshiev AT, Weber J, Marsland BJ, Oxenius A, Kopf M. IL-21R on T cells is critical for sustained functionality and control of chronic viral infection. Science. 2009;324:1576–1580. doi: 10.1126/science.1172815. [DOI] [PubMed] [Google Scholar]
- 74.Yi JS, Du M, Zajac AJ. A vital role for interleukin-21 in the control of a chronic viral infection. Science. 2009;324:1572–1576. doi: 10.1126/science.1175194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Margolin K. Cytokine therapy in cancer. Expert Opinion on Biological Therapy. 2008;8:1495–1505. doi: 10.1517/14712598.8.10.1495. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.