Abstract
Objective
To examine views and experiences of conflicts concerning time in healthcare, from the perspective of physicians who have become patients.
Methods
We conducted two in-depth semi-structured two-hour interviews concerning experiences of being health care workers, and becoming a patient, with each of 50 doctors who had serious illnesses.
Results
These doctor-patients often came to realize as they had not before how patients experience time differently, and how “patient-time,” “doctor-time,” and “institution-time” exist and can conflict. Differences arose in both long and short term, regarding historical time (prior eras/decades in medicine), prognosis (months/years), scheduling delays (days/weeks), daily medical events and tasks (hours), and periods in waiting rooms (minutes/hours). Definitions of periods of time (e.g., “fast,” “slow,” “plenty,” and “soon”) also varied widely, and could clash. Professional socialization had heretofore impeded awareness of these differences. Physicians tried to address these conflicts in several ways (e.g., trying to provide test results promptly), though full resolution remained difficult.
Conclusions
Doctors who became patients often now realized how physicians and patients differ in subjective experiences of time. Medical education and research have not adequately considered these issues, which can affect patient satisfaction, doctor-patient relationships and communication, and care.
Practice Implications
Physicians need to be more sensitive to how their definitions, perceptions, and experiences concerning time can differ from those of patients.
Keywords: Doctor-patient relationships, doctor-patient communication, medical education, patient satisfaction, medical ethics, medical socialization, health care delivery
1. Introduction
Subjective views and experiences of time have been examined in many social domains, but have been under-explored in medicine. As managed care has grown, and the health care delivery system has changed, some critics have felt that the amount of time physicians have with each patient has decreased (1-4), though data have challenged this perception, raising critical questions about these phenomena (5-7). Doctors and patients have been found to differ in perceptions of communication (8-10) and risks and benefits (11), and may view time in contrasting ways as well.
In general, time is measured in not only objective, standardized units, but in sociocultural terms (12,13). Cultural factors can shape, e.g., the lengths of future and past time periods that are measured (14). In the workplace, types of tasks and social structures affect how groups experience dimensions of time such as its “flexibility, linearity, pace, punctuality, delay…urgency, scarcity, and future and present time perspectives” (15). In general, the duration of time is also experienced subjectively (16). But questions arise of how two different individuals within a particular social dyadic interaction (e.g., doctors and patients) experience and view these issues concerning time relative to each other.
Within medicine, issues of time have received attention in the past with regard to long-term hospitalizations for psychiatric disorders and TB, before the advent of more effective medications (17-20). Patients and doctors seek norms of timetables to shape expectations (e.g., for discharge from the hospital); and negotiate and bargain about when events such as hospital discharges occur. Timetables structure psychiatric training (17,21) – specifically how professional development transpires over the months and years. Recent attention has also been given to other aspects of time. Though doctor's visits have been perceived as getting shorter (2,3), data have argued otherwise (5-7), and physician visits may in fact be increasing because of increases in the number of elderly patients, many of whom require dietary counseling for hypertension (7). Lengths of hospitalizations have been decreasing, often to due to cost and administrative factors (22-24). Time delays have been documented in receiving treatment – e.g., analgesia for acute abdominal pain (25,26) and treatment for acute MIs that then reduces treatment effectiveness (27). Similarly, patients admitted during off-hours more frequently encounter delays in undergoing catheterization for MIs, leading to higher mortality (28). Long wait times may be associated with decreased overall satisfaction with treatment (29,30), though other research has found that patient perceptions of time are often inaccurate, with over- more than under-estimations of wait times to see physicians (31). Indeed, perceptions rather than actual wait times may predict patient satisfaction (32). Communication about these issues has also been under-explored. The only study identified that mentions such communication reported that most patients who left ERs without being seen said that “more frequent updates on wait times” would have helped them wait longer (33).
Still, many aspects of doctors' and patients' views and approaches concerning time have not been examined – e.g., how do physicians and patients view and respond to perceptions of decreased availability of time together during visits? How do they act as a result?
Doctors who become patients may be able to offer unique perspectives on differences in perceptions of time in medical care, having been forced to experience both sides and points of view in doctor-patient relationships and interactions. Several other aspects of the experiences of physicians who become patients have been discussed, but most prior reports have been anecdotal, single-case accounts (34-37). I have previously reported on how these ill physicians confront and view issues concerning risks and benefits (11), disclosures of their illness (38), and spirituality (39). Role conflicts have been described in other situations (40), and can have numerous manifestations, but these issues have not been explored concerning doctors and patients regarding views and approaches toward time.
2. Methods
Pilot interviews were first conducted about issues concerning physicians who become patients. These interviews led to the development and refinement of an instrument. The full study focused in the initial stage on HIV-infected doctors, and was then expanded to include physicians with other diagnoses, too. Subjects were recruited for the full study through emailed announcements (e.g., stating, “Are you or do you know a physician with a serious illness?”), websites, word of mouth, and ads in newsletters. The PI was then contacted by 48 doctors, 1 dentist, and 1 medical student who had become patients due to serious illnesses (referred to below as “doctors”). Two in-depth, semi-structured interviews of two hours were held with each subject concerning experiences before and after diagnosis. Serious illness was self-defined, and then confirmed by the PI. Of these participants, 27 were HIV positive, and 23 had other medical problems (e.g., cancer, heart disease, and hepatitis). Ages ranged from 25-87, all were Caucasian, except for 1 Latino doctor, 40 were men, and 10 were women. They were interviewed in several cities in participants' homes or offices, or the PI's office – whatever was more convenient for them. Participants were asked about experiences as patients and as providers, and about other aspects of their lives.
Interviews were audiotaped, transcribed, and content-analyzed, informed by grounded theory (41). Initial analyses were conducted during the period in which the interviews were being held. A research team, composed of the PI and a research assistant, examined a subset of interviews to assess factors that shaped subjects' experiences, identifying categories of recurrent themes and issues that were subsequently given codes. A senior consultant with expertise in qualitative research provided input at several stages of this coding process. The team assessed similarities and differences between participants, examining categories that emerged, ranges of variation within categories, and variables that may be involved. A coding manual was developed, and areas of disagreement were examined until consensus was reached. New themes that did not fit into this original coding framework were discussed, and modifications were made in the manual when deemed appropriate. In phase two of the analysis, the research team refined, merged, or subdivided thematic categories into secondary or sub-codes, when suggested by associations or overlap in the data. These codes and sub-codes were then used in analysis of all of the interviews. To ensure coding reliability, all interviews were analyzed by two coders.
The study was approved by the Institutional Review Board at Columbia University and the NY State Psychiatric Institute.
3. Results
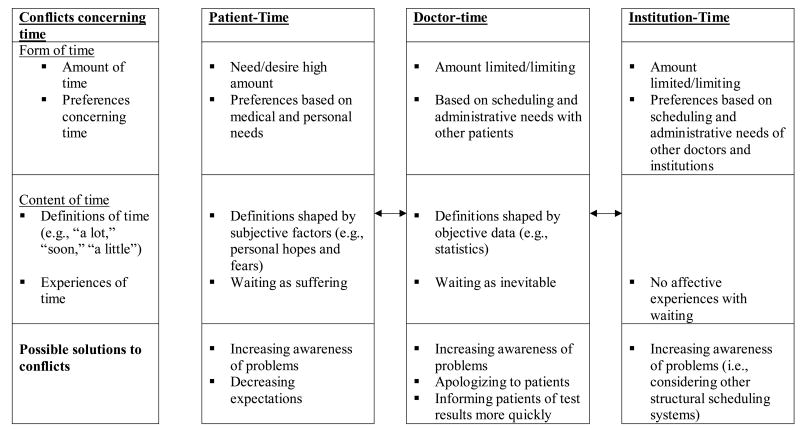
After becoming sick, these physicians often became aware of conflicts between doctors and patients regarding time at several levels. Overall, several themes emerged concerning time as described below and listed in Figure 1. In general, these doctor-patients suggested the existence of three types of time – “patient-time,” “ doctor-time,” and “institutional-time,” with differences in both the form and content of these.
Figure I. Outline of Issues Concerning 3 Types of Time.
Many of these physicians became disappointed with how the “time tables” of physicians, patients, and institutions, and these three types of time flowed differently and could conflict – in both the long-term (e.g., with regard to prognoses), and the short term (e.g., in a waiting room). As outlined in Figure 2, particularly for doctors and patients, conflicts arose over multiple lengths of periods of measurement of time – prognoses (months and years), scheduling delays (days and weeks), and daily schedules of medical events (hours), and periods spent in waiting rooms (minutes to hours) – highlighting the pervasiveness of these tensions. These doctors also noted differences between colleagues related to historical time – prior eras or decades in medicine (e.g., commenting on practice “back in my time…”). This last difference reflected professional seniority and hierarchy (i.e., different relationships with the profession itself between older vs. younger colleagues), rather than tensions between patients and providers per se.
3.1. Available amounts of time
Conflicts often emerged since doctors had limited periods with each patient, while patients in contrast, generally had more time available. Institutional structures (e.g., parameters on how much insurance physicians receive for patient visits) often led to multiple competing demands, and pressures on doctors, reducing the amount of time they had, and created a sense of “institutional–time.” Physicians then had to decide how to integrate these institutional time pressures and constraints into their work each hour and day, and how to handle conflicts that arose.
For example, many physicians pushed to have tests performed rather than examine patients – becoming “very procedure-oriented.” This “procedure-orientation” has several other causes as well – including perceived usefulness of the data, and belief in the objectivity of “the numbers” – and has several critical implications. As a physician with cancer said, “There are very procedure-oriented people: ‘Let's get another chest x-ray.’ They don't listen to my chest, they get a chest x-ray.”
In recent decades, the rise of managed care and of technological interventions approaches have each exacerbated the other in shortening the amount of time doctors have with patients (e.g., “Now, there are many technical fixes, procedures, and tests that totally fill the time and the heads of doctors. So they're a little lost”).
Problems arose not just with physicians, but also with other staff. A few interviewees complained about nurses, too, being pressed for time. (“Human touch is incredibly important. You expect it from nurses, but they don't have any time now, either”). On the other hand, at times, doctors challenged these strictures (i.e., spending more time with a patient than reimbursement covers). Other doctors had switched institutional work settings to one that had a different sense of “institutional-time” (e.g., clinic settings that paid physicians less, but enabled them potentially to spend more time with individual patients, if necessary).
3.2. Preferences concerning timing
For treatment or interventions, doctors, patients, and institutions often clashed over not only how much time was available, but when particular events occurred – e.g., what timelines were ideal, or most convenient. Physicians often forgot patients' timetables and experiences of these. These physician-patients became more aware, e.g., of the disadvantages of doctors, especially surgeons, rounding early in the morning on wards, waking patients up. (“They come at 6:30 a.m. and don't give a damn that another patient lying in the other bed is half-dead. They put the light on, and eight people come scream, shout and drop things”). This difference in timing reflects in part hierarchy, lack of empathy training-instilled norms.
Physicians may also prescribe medications for times of the day such that side effects harm patients more than otherwise. One internist with cancer, e.g., was given medication at night that gave her explosive diarrhea. The drug could have been administered much earlier in the day. She complained to the hospital staff, but in vain. Eventually, she had to “go on strike” to change the hours of dosing.
I was on kayexalate, which gives you massive diarrhea. They gave it to me in the morning, and I got “my business” finished before sleep. But then, only because they didn't think about writing the order until 9:00 p.m., they gave it to me at 10:00 p.m. It was the first day I was allowed out of bed to use the commode. I had all these IV lines, and an oxygen mask, and it was a big production to get 6 feet over to the commode. I also knew how explosive the diarrhea was. So I was up until 2 a.m. waiting for it to happen. I talked about it with the house officer, saying, “I'm going to wait till tomorrow to take it.” But that caused a whole big fuss, so I just took it. The next time they wanted to give me some, I went on strike! Eventually my attending wrote a better order.
These physicians' doctors often failed to grasp the importance and ramifications of timing in patients' lives and quality of life. As she continued,
One doctor tapered me off steroids too quickly before Passover. I said, “Can't we wait a week? I have 16 people coming over for Passover.” He said, “No, I want you to do it now.” He went into this whole thing about his own family's dynamics – he grew up in an orthodox Jewish home, and everybody argued and it was awful. I said, “But that's not the way it is at our house. I really treasure it!” I followed the taper, but it was too fast, and I had to be readmitted. My kids came to the hospital and we had the Seder there. I brought a few things that I had made, and we set the table in the hospital. My doctor had no remorse. It wasn't a medical necessity to taper me then. It's an example of how unresponsive he was to quality of life issues.
Here again, the profession does not follow patient-time, but rather, physician-time and occasionally, institution-time. Bureaucratic inefficiencies and unwieldy management and personnel structures persist. Difficulties start at the outset – during administrative procedures admitting patients to the hospital. (“The method of getting people into the hospital is barbaric – waiting for a bed in the ER for hours.”) These problems are so pervasive and deeply ingrained that being a physician does not wholly eradicate them. Another physician explained,
The surgeon arranged for me to be admitted directly – not through the ER. I came in, but the people in the admitting department couldn't find any documentation. So, with intense pain and vomiting, I waited two hours in the admitting office. My doctor did what he was supposed to do, and it didn't make the mechanism of the hospital function.
When seriously ill, he was admitted, but not evaluated for hours. Finally, he was seen, but only after he called his physician, with whom he was on a first name basis.
I called his office, and said, “Tom, I still haven't been seen by anybody, after two hours.”…Six hours after my admission, the intern and resident came.
Bureaucratically, hospitals seemed organized for the benefit of doctors more than patients. Hence, as both a patient and provider, he felt frightened:
Hospitals and the health system respond to their own needs…hospitals have been shaped around the needs of the doctors, administrators, and business people who run them, rather than around the patients…though these days it doesn't function very well for doctors, either…
Patients were positioned – at times both literally and figuratively – for the benefit of doctors more than patients. Part of the problem arose because of the dual functions of teaching hospitals – to educate trainees and provide care. But no feedback is built-in to change the system. Patients are too sick to provide any, contributing to stasis.
3.3. Definitions of time
Different and often conflicting definitions and understandings of prognoses arose, too. Doctors and patients regularly communicated about the future, but frequently disagreed about the precise meanings of terms – e.g., how long is “long”? How soon is “soon”: hours, days, weeks, months or years? At times, doctors and patients defined “fast” and “slow” very differently. Doctors said, e.g., “We have plenty of time,” but definitions of “plenty” can vary widely, and for a particular patient, both objectively and subjectively, the disease can progress much faster. One internist reported,
My doctor said that Hodgkin's doesn't spread “that quickly;” and the speed probably wasn't going to change what they did, or my outcome. But once you're told that you have cancer, it's very hard to have that overall perspective.
The diagnosis of a life-threatening illness can profoundly heighten the meaning and value of time. Even small periods become more significant, when their total quantity is limited. Moreover, the average natural history of a disease may not apply to all patients, yet despite wide individual variation between patients, it is simpler for physicians to adopt these means.
In making estimations, physicians may rely on objective data (e.g., morbidity and mortality statistical means), but “hedge their bets.” Differences between the approaches of doctors and patients thus became apparent, and can distress the suffering patient. Moreover, physician arrogance can lead doctors to defend their predictions and interpretations of time. As this internist with lymphoma added,
How does he know that my cancer's not going to spread to this or that group of lymph nodes between now and six weeks from now? He says, “Oh, I've seen the course. You're just anxious!”
Doctors thus can dismiss patients' alternative views and concerns about time as anxiety – as psychopathology.
3.4. Differences in experiences of time: waiting as suffering
These physicians often now came to realize the degree to which patients also experience time differently – as longer, since uncertainty and anxiety hang over patients' heads. Previously, these physicians tended to see time as objective – experienced similarly by themselves and their patients – rather than as subjective. Yet waiting, and the ambiguity of not knowing the outcome of tests lengthen the experience of time. (“A person waiting is a person suffering”). This doctor now came to realize as never before the importance of temporal issues, and specifically how painful the uncertainty of anticipating a lab result can be: “The difference between being a doctor and not being a doctor was the timing.”
Even on smaller scales, these ill physicians repeatedly expressed frustration at not having appointments and lab tests immediately. Even when understanding the reasons for delays in waiting rooms, they often became distressed. Several reported being astonished at the anger they felt because of these delays in seeing their doctor. An internist who had an MI said,
I discovered an intense irritation that I had to go and sit in the radiation oncologist's office. I had an appointment at 11:30 a.m. and wasn't seen until after 12:00, and was driven up the wall! I'm not different from anybody else. But why should anyone have to wait around? It is SOP – Standard Operating Procedure. Some doctors are pretty good at figuring out how to have people not wait so long, or get treated better.
Importantly, professional training and socialization had heretofore impeded awareness of this patient frustration. Similarly, institutions and administration may be concerned about time as an objective factor in assessments of productivity, but do not have affective experiences of time in doctor-patient interactions. Yet one of the most difficult aspects of patienthood was sitting with anxious expectation in the waiting room, or anticipating physicians' calls. These doctors, as fellow physicians, appeared to receive more call-backs than did lay patients. But even this special treatment did not fully alleviate the problem. An endocrinologist felt that other physicians would take his calls, which they would not have done if he were “just” a patient. He recognized that he faced fewer delays because he was “halfway between a patient and a doctor.” Still,
Most difficult for me has been the process of waiting – in waiting rooms, and for things that I know don't take this long – calling doctors and not being put through immediately.
This frustration stems in part from the meanings of this delay – the symbolic value that it reflects as an alteration in his status as well.
3.5. Reducing tensions concerning time
Within each period of time measurement, gaps were experienced and negotiated differently. Across all of these categories, conflicts existed and led to frustrations. The multiple periods of time involved suggest the degree of underlying attitudes concerning hierarchies and empathy. Frustrations in each period may build on each other, shaping patient experiences, generating distress and detracting from patient satisfaction.
Yet obstacles existed to mediating these differences. Training and physicianhood blocked awareness of these problems, highlighting how physicians distance and disconnect themselves, seeing and constructing patients as the “other.” Though one doctor admitted, “I know I've kept patients waiting, too,” most had difficulty acknowledging the discrepancy between having kept patients waiting and having to wait themselves.
Many physicians accepted that delayed timetables are “just how things are done.” Awareness of these systemic factors – the fact that diagnoses and treatment and clinical responses take time – can increase, but remain unchanged. An internist with HIV now appreciated these issues more clearly:
I now understand a lot more how long things take to happen when you call the office and ask for something. It could be a lot quicker and easier, but that's just the system, and how people are used to doing things. It's unfortunate, but there's only so much I can change what I do.
Thus, even when recognizing this problem of doctor- vs. patient-time, these physicians generally felt powerless to alter it. An internist who had an MI said:
Rationally, I understood: they want to stack the airplanes up, so that whenever there's an opening, one can land. But it's very irritating.
This acceptance of the system and inability to change it suggest a sense of perceived helplessness – i.e., that institutions that structure the practice of medicine (i.e., related to insurance coverage) generate a timetable that trumps individual physicians' own preferences concerning time.
Shocked and annoyed at their physicians' delays in returning phone calls or answering questions, a few doctor-patients became even more aggressive in their own care (e.g., “I get and interpret my own lab results – otherwise I'd have to wait three months until my next appointment”) In part as a result, some doctors engaged in self-prescribing, too. Yet they realized that lay patients did not have the same options.
Several also now tried not to delay in providing test results to their patients. One radiologist now interrupted what he was doing to tell patients the results of tests.
I always try and run out to them to tell them the results of their scan. [That's]… not new. But now I'll interrupt anything I'm doing to tell them the results. In the past, I would get them the results as quickly as possible, but if I was talking to someone else, I wouldn't get up…Now, I pretty much drop everything, or call the tech: “Go and tell the patient everything is okay.”
Another physician suggested that simply saying to patients, “I'm sorry about keeping you waiting,” could diffuse potential patient frustration. But full resolution of these discrepancies proved elusive.
4. Discussion and Conclusion
4.1. Discussion
When becoming patients, these doctors came to realize, as not before, how their perspectives, definitions, and experiences concerning time differed from those of patients. Aspects of time differed substantially between physicians and patients with regard to both structure and form (i.e., amount of time and schedule preferences) and content (i.e., definitions and experiences). Recognition of differences emerged at all categories of lengths of time, from decades to years to months to hours. These phenomena and related aspects of the roles of doctors and patients can interact. Increased discomfort from anxiety, pain, uncertainty or reduced social status due to illness can decrease the quality and increase the length of the experience of time. Emotional stress due to illness can thus mediate experiences of time (e.g., perceptions of how long is “long”). A perceived or possible decreased supply of time (i.e., a poor prognosis) can increase the value of individual time periods.
Part of these tensions may be inevitable, since the experience of being a patient may invariably involve both waiting and suffering. The words “patient” and “patience” derive from the same Latin root – patientia, to suffer (42). Hence, patience entails waiting and individual suffering. Illness and care of illness often involve unpredictable amounts of time. Emergencies are unplanned. Unforeseeable courses of disease make needs for follow-ups or additional treatment uncertain. Many patients miss appointments or arrive late. Yet the fact that the words “patient” and “patience” are related may reflect, too, historical and institutional issues that remain critical. Traditionally, when medicine offered relatively more palliative and fewer effective treatments, patients suffered and, importantly, waited (i.e., for eventual recovery or death). But institutionally, over time this link may then become further legitimated – i.e., patients are seen as those who suffer and wait – andreflect and foster assumptions, impeding amelioration of these problems.
Indeed, both doctors and institutions often structured medical schedules to meet best their own needs, demands, and priorities, rather than those of patients. These data illustrate the degree to which physician- and institution-, rather than patient-oriented medicine persists. Hierarchies in medicine and managed care's demands on physicians' time for administrative tasks can compound or exacerbate these problems. Surgeons coming early in the morning, waking patients up, may arise in part since delays in individual patient's operations occur later through the course of the day, allowing post-op care to be observed while the surgeon is still available. But this justification may not apply as much for internists. Still, hospital schedules are structured such that generally, patients are in their rooms early in the morning, while often undergoing procedures later in the day. Nonetheless, potentially alternative scheduling systems could be considered and evaluated.
Prior literature on the sociology and anthropology of time has described the social structure of time within particular cultures and settings, e.g., in particular cultural groups or corporate offices (15, 43-45), but less attention has been given to how different individuals in the same social setting or interaction may conflict in their perceptions and definitions of time. Within any one setting, different parties (e.g., doctors and patients) may clearly experience time differently. The present data illustrate these tensions can exist concerning multiple lengths of time (e.g., minutes to months). Importantly, these doctors reveal, too, that they had not heretofore been aware of these differences.
What happens when disagreements occur? One doctor-patient felt compelled to go “on strike” – exercising what she saw as her only option. As a doctor, she felt empowered to oppose vehemently in this way her doctor's orders. Presumably, lay patients would not feel as able to “strike”.
Most importantly, in any case, increased physician, patient, and institutional awareness of these conflicting notions of time, and of their effects on patient experiences, attitudes, satisfaction, and quality of life can be beneficial. Indeed, these issues affect patient satisfaction, and reflect and can exacerbate other tensions in doctor-patient relationships. Physicians often see patients not as equals, but as ‘other’, reflecting differences in power (46). Conflict in definitions of time can cause intense distress and anger, and are seen as further reflecting and representing hierarchy and helplessness.
These data are critical, too, given studies have suggested that the amount of time in office visits is not decreasing, though, anecdotally, perceptions persist that it is. The present data suggest that this discrepancy itself may emerge because of the key roles of subjective notions of time, and the fact that doctors often engage in more technological interventions, raising questions of how available time is being used – how much of it is being spent in verbal communication vs. procedure-related activities. Past studies have not assessed these issues. The present findings that hospital-time conflicts with both patient- and doctor- time appears consistent, too, with data that patients hospitalized during off-hours had worse outcomes (28), suggesting the importance of preferences and ideals in the timing of particular events – not only how much time overall is available, but when events occur. This prior study can now be seen as highlighting one key implication of this clash.
Surprisingly, heretofore, these doctors were not aware that their patients' experiences differed from their own, and importantly, the degree to which that occurred. An individual's experience of time shapes, but can also limit, one's point of view. Within their own practices, these physicians still had difficulty resolving these discrepancies. In part, institutional-time shaped the lives and time structures of both patients and physicians, and these conflicting perspectives seemed difficult to bridge or change. Yet, as above, increased awareness of these problems by doctors, patients, and institutions can help. Patients can reframe their expectations, not personalize delays, and perhaps realize more fully that physicians are themselves responding to larger institutional pressures and constraints.
4.2. Conclusion
Medical education, practice, and research have not optimally addressed these issues, but need to do so. Time is a central concept in estimating course of disease and treatment responses, yet physicians tend to see it as wholly objective. Subjective experiences of time need to be more fully included and examined in research and understandings of patient experiences. Awareness needs to increase that differences in aspects of both the form and content of time – in perceptions, experiences, and interpretations – occur, and can have critical implications.
Further research is needed, too, on how physicians and patients view and manage the time constraints and pressures that each may experience within the current health care system, and how these discrepancies affect other aspects of doctor-patient interactions. It is critical to investigate these phenomena and how exactly they undermine provider-patient communication and relationships, patient satisfaction, adherence to treatment recommendations, patient follow-up, understandings about treatment, and coping with illness. In their interactions, doctors structure time in ways that patients are forced to follow (e.g., in the waiting room), reflecting and reinforcing hierarchies and lack of empathy or understanding by physicians, which future research can further probe.
Similarly, past research has used time as a variable in analyzing other phenomena, noting differences between perceived and actual waiting times (32,33), but has not explored whether and how exactly larger units of time (e.g., decades, years, months, hours) may also be defined or experienced differently, how differences in waiting times are viewed, and what tensions ensue. These notions of conflicting perceptions of time within a setting deserve more attention in other fields as well – specifically, those involving power differentials (e.g., with teachers, parents, and police).
4.3. Practice Implications
As above, clinicians should increase awareness of how differences in perceptions, experiences, and definitions of time exist, and have important ramifications. Failure to recognize these differences may impede doctor-patient communication, relationships, patient satisfaction, adherence, follow-up, and coping. Institutional time generates pressures that doctors cannot always wholly eradicate. But recognition of these gaps can help. Physicians could potentially address tensions that arise due to these differences, demonstrating appreciation of patients' experiences (e.g., by saying “I'm sorry to have kept you waiting”). Such apologies can help quell patient frustration, anger, and tensions, acknowledging that physicians at least recognize and respect patients' experience and suffering. Indeed, lack of recognition of these discrepancies may illustrate disrespect for patients. Physicians should view time not as wholly objective, but as subjective. Doctors can be trained to remedy conflicts that stem from ambiguous definitions (e.g., of “soon,” “quick,” “fast,” “slow,” “long,” “a lot”) by not using such qualitative descriptions, without objective referents. Institutions, too, could recognize more how conflicting definitions and experiences of time can diminish patient satisfaction and outcomes, and address what policies might address these discrepancies (e.g., to reduce delays). In sum, these areas of differing subjective views and definitions of time have important ramifications for future research, practice, and education.
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Table I. Periods of Conflicting Experiences of Time.
| Description | Length(s) of Time |
|---|---|
| Historical Time (i.e., prior “eras” in medicine) |
Decades |
| Prognosis | Months – Years |
| Scheduling Delays | Days – Weeks |
| Daily Schedules | Hours |
| Waiting Rooms | Minutes – Hours |
Acknowledgments
The authors would like to thank Renée C. Fox, Mary DuVernay, Frank Griggs, Shaira Daya, Daniel Fishman, Brian Kristoff, and Jennifer Hersh, for assistance with this project. This project was funded by the Arthur Vining Davis Foundations, the Picker-Commonwealth Scholars Program, the Commonwealth Fund, and in part through the NIMH (Grant K08-MH-1420-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Linzer M, Konrad TR, Douglas J, McMurray JE, Pathman DE, Williams ES, Schwartz MD, Gerrity M, Schekler W, Bigby JA, Rhodes E. Managed care, time pressure, and physician job satisfaction: results from the physician worklife study. J Gen Intern Med. 2000;15:441–450. doi: 10.1046/j.1525-1497.2000.05239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Francis AM, Polissar L, Lorenz AB. Care of patients with colorectal cancer. A comparison of a health maintenance organization and fee-for-service practice. Med Care. 1984;22:418–429. doi: 10.1097/00005650-198405000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Chin S, Harrigill KM. Delay in gynecologic surgical treatment: A comparison of patients in managed care and fee-for-service plans. Obstet and Gynecol. 1999;93:922–927. doi: 10.1016/s0029-7844(99)00005-8. [DOI] [PubMed] [Google Scholar]
- 4.Braddock CH, Snyder L. The doctor will see you shortly: The ethical significance of time for the patient-physician relationship. J Gen Intern Med. 2005;10:1057–1062. doi: 10.1111/j.1525-1497.2005.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mechanic D, McAlpine DD, Rosenthal M. Are patients' office visits with physicians getting shorter? NEJM. 2001;344:198–204. doi: 10.1056/NEJM200101183440307. [DOI] [PubMed] [Google Scholar]
- 6.Weeks WB, Wallace AE. Time and money: A retrospective evaluation of the inputs, outputs, efficiency, and incomes of physicians. Arch Intern Med. 2003;163:944–948. doi: 10.1001/archinte.163.8.944. [DOI] [PubMed] [Google Scholar]
- 7.Stafford R, Saglam D, Causino N, Starfield B, Culpepper L, Marder WD, Blumenthal D. Trends in adult visits to primary care physicians in the United States. Arch Fam Med. 1999;8:26–32. doi: 10.1001/archfami.8.1.26. [DOI] [PubMed] [Google Scholar]
- 8.Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. JAMA. 1997;277:678–682. [PubMed] [Google Scholar]
- 9.Selwyn PA. Prospects for improvement in physicians' communication skills and in prevention of HIV infection. Lancet. 1998;352(9127):506. doi: 10.1016/S0140-6736(05)79247-3. [DOI] [PubMed] [Google Scholar]
- 10.Laine C, Davidoff F. Patient-centered medicine: a professional evolution. JAMA. 1996;275:152–156. [PubMed] [Google Scholar]
- 11.Klitzman R. Views of risks and benefits among doctors who become patients. Patinet Educ Couns. 2006 January 20; doi: 10.1016/j.pec.2005.11.013. available online. [DOI] [PubMed] [Google Scholar]
- 12.Husserl E. Phenomenology of internal time-consciousness. Bloomington, Indiana: Indiana University Press; 1964. [Google Scholar]
- 13.Sorokin PA. Sociocultural causality, space, time: A study of referential principles of sociology and social science. New York: Russell & Russell; 1964. [Google Scholar]
- 14.Klitzman R. The trembling mountain: A personal account of Kuru, cannibals, and Mad Cow Disease. New York: Perseus; 1998. [Google Scholar]
- 15.Ballard DI, Siebold DR. Communication-related organizational structures and work group temporal experiences: The effects of coordination method, technology type, and feedback cycle on members' construals and enactments of time. Commun Monogr. 2004;71:1–27. [Google Scholar]
- 16.James W. The Principles of Psychology. Vol. 1. New York: Dover Publications; 1950. [Google Scholar]
- 17.Light D. The sociological calendar: an analytic tool for fieldwork applied to medical and psychiatric training. Am J Sociol. 1975;80:1145–1164. doi: 10.1086/225948. [DOI] [PubMed] [Google Scholar]
- 18.Dandoy S, Hansen R. Tuberculosis care in general hospitals: Arizona's experience. Am Rev Respir Dis. 1975;112:757–763. doi: 10.1164/arrd.1975.112.6.757. [DOI] [PubMed] [Google Scholar]
- 19.Roth JA. Consistency of rule application to inmates in long-term treatment institutions. Soc Sci Med. 1985;20:247–252. doi: 10.1016/0277-9536(85)90238-2. [DOI] [PubMed] [Google Scholar]
- 20.Zerubavel E. Patterns of time in hospital life: A sociological perspective. Chicago: University of Chicago Press; 1979. pp. 113–116. [Google Scholar]
- 21.Roth JA. Timetables; structuring the passage of time in hospital treatment and other careers. Indianapolis: Bobbs-Merrill; 1963. [Google Scholar]
- 22.Bogaty P, Dumont S, O'Hara GE, Boyer L, Auclair L, Jobin J, Boudreault JR. Randomized trial of a noninvasive strategy to reduce hospital stay for patients with low-risk myocardial infarction. J Am Coll Cardiol. 2001;37:289–1296. doi: 10.1016/s0735-1097(01)01131-7. [DOI] [PubMed] [Google Scholar]
- 23.Every NR, Spertus J, Fihn SD, Hlatky M, Martin JS, Weaver WD. Length of hospital stay after acute myocardial infarction in the Myocardial Infarction Triage and Intervention (MITI) Project registry. J Am Coll Cardiol. 1996;28:287–293. doi: 10.1016/0735-1097(96)00168-4. [DOI] [PubMed] [Google Scholar]
- 24.Neutel CI, Gao RN, Gaudette L, Johansen H. Shorter hospital stays for breast cancer. Health Reports. 2004;16:19–31. [PubMed] [Google Scholar]
- 25.Shabbir J, Ridgway PG, Lynch K, Law ErC, Evoy D, O'Mahony JB, Mealy K. Administration of analgesia for acute abdominal pain sufferers in the accident and emergency setting. Eur J Emerg Med. 2004;11:309–312. doi: 10.1097/00063110-200412000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Tait IS, Ionescu MV, Cuschieri A. Do patients with acute abdominal pain wait unduly long for analgesia? JR Coll Surg Edinb. 1999;44:181–184. [PubMed] [Google Scholar]
- 27.Goldberg RJ, Mooradd M, Gurwitz JH, Rogers WJ, French WJ, Barron HV, Gore JM. Impact of time to treatment with tissue plasminogen activator on morbidity and mortality following acute myocardial infarction (The second National Registry of Myocardial Infarction) Am J Cardiol. 1998;82:259–264. doi: 10.1016/s0002-9149(98)00342-7. [DOI] [PubMed] [Google Scholar]
- 28.Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, Pollack CV, French WJ, Blaney ME, Krumholz HM. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-Segment elevation myocardial infarction. JAMA. 2005;294:803–812. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 29.Feddock CA, Hoellein AR, Griffith CH, Wilson JF, Bowerman JL, Becker NS, Caudill TS. Can physicians improve patient satisfaction with long waiting times? Eval Health Prof. 2005;28:40–52. doi: 10.1177/0163278704273084. [DOI] [PubMed] [Google Scholar]
- 30.Leddy KM, Kaldenberg DO, Becker BW. Timelines in ambulatory care treatment: An examination of patient satisfaction and wait times in medical practices and outpatient test and treatment facilities. J Ambulatory Care Manage. 26:138–149. doi: 10.1097/00004479-200304000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Thompson DA, Yarnold PR, Williams DR, Adams SL. Effects of actual waiting time, perceived waiting time, information delivery, and expressive quality on patient satisfaction in the emergency department. Ann Emerg Med. 1996;28:657–665. doi: 10.1016/s0196-0644(96)70090-2. [DOI] [PubMed] [Google Scholar]
- 32.Thompson DA, Yarnold PR, Adams SL, Spacone AB. How accurate are waiting time perceptions of patients in the emergency department? Ann Emerg Med. 1996;28:652–656. doi: 10.1016/s0196-0644(96)70089-6. [DOI] [PubMed] [Google Scholar]
- 33.Arendt KW, Sadosty AT, Weaver AL, Brent CR, Boie ET. The left-without-being-seen patients: What would keep them from leaving? Ann Emerg Med. 2003;42:317–323. doi: 10.1016/s0196-0644(03)00404-9. [DOI] [PubMed] [Google Scholar]
- 34.Heymann J. Equal partners. Boston: Little Brown; 1995. [Google Scholar]
- 35.Mandell H, Spiro H, editors. When doctors get sick. New York: Plenum; 1987. [Google Scholar]
- 36.Mullan F. Seasons of survival: reflections of a physician with cancer. NEJM. 1985;313:270–273. doi: 10.1056/NEJM198507253130421. [DOI] [PubMed] [Google Scholar]
- 37.Pinner M, Miller B, editors. When doctors are patients. New York: W.W. Norton; 1952. [Google Scholar]
- 38.Klitzman R, Weiss J. Disclosures of illness by physicians to their patients: A qualitative study of doctors with HIV and other serious disorders. Patient Educ Couns. 2006 July 24; doi: 10.1016/j.pec.2006.03.006. available online. [DOI] [PubMed] [Google Scholar]
- 39.Klitzman R. Challenges and changes in spirituality among doctors who become patients. Soc Sci Med. 2005;61:2396–2406. doi: 10.1016/j.socscimed.2005.04.031. [DOI] [PubMed] [Google Scholar]
- 40.Strasburger LH, Gutheil TG, Brodsky AB. On wearing two hats: Role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448–456. doi: 10.1176/ajp.154.4.448. [DOI] [PubMed] [Google Scholar]
- 41.Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. Newbury Park: Sage Publications; 1990. [Google Scholar]
- 42.“Patient.” “Patience.” The Oxford English Dictionary. 2nd. Oxford, England: Oxford University Press; 1989. [Google Scholar]
- 43.Ballard DI, Seibold DR. Organizational members' communication and temporal experience: Scale development and validation. Communic Res. 2004;31(2):135–172. [Google Scholar]
- 44.Postili J. Clock and calendar time: a missing anthropological problem. Time & Society. 2002;11(2/3):251–270. [Google Scholar]
- 45.Whorf BL. The relation of habitual thought and behavior to language. In: Carroll JB, editor. Language, Thought, and Reality: Selected Writings of Benjamin Lee Whorf. Cambridge, MA: MIT Press; 1956. pp. 134–159. [Google Scholar]
- 46.Emanuel EJ, Emanuel LL. Preserving community in health care. J Health Polit Policy Law. 1997;22:147–184. doi: 10.1215/03616878-22-1-147. [DOI] [PubMed] [Google Scholar]