Primary intraocular lymphoma (PIOL) is a rare, aggressive malignancy involving the retina, vitreous or optic nerve head, without (isolated PIOL) or with central nervous system (CNS) involvement. While isolated PIOL may initially manifest unilaterally, the majority (80–90%) of patients eventually develop bilateral disease, and 60–85% progress in the CNS within 2–3 years of initial diagnosis, limiting median survival to only 3 years (Freeman et al, 1987).
The optimal treatment for PIOL is controversial and data on the therapy and outcome of isolated PIOL is limited to retrospective case reports or mostly small series with heterogeneous patient populations and treatment approaches (Akpek et al, 1999, Grimm et al, 2007, Hoffman et al, 2003, Jahnke et al, 2006).
In November 2005, the University of Miami Sylvester Comprehensive Cancer Center lymphoma programme team decided to use a combination of binocular external beam radiation therapy and systemic chemotherapy containing high-dose methotrexate (modified de Angelis regimen) (Abrey et al, 2000) in all patients with newly diagnosed isolated PIOL. Our design aimed to eliminate ocular disease by binocular radiation, and to use concomitant/sequential chemotherapy to eradicate potential microscopic brain disease, which may be responsible for later relapse. Patients were not enrolled in a clinical trial, but were followed and data collected prospectively. This report presents our experience using this approach.
All patients underwent diagnostic pars plana vitrectomy with cytology, immunocytochemistry, flow cytometry and gene rearrangement studies. Staging evaluation, which included computerized tomography scans of chest, abdomen and pelvis, brain magnetic resonance imaging (MRI) scan, lumbar puncture, bone marrow biopsy and aspiration, showed no systemic lymphoma. Radiation therapy of 30–40 (median 36) Gy was given at 1.8–2.0 Gy per fraction to both eyes and orbits including the optic nerve and conus. Chemotherapy consisted of methotrexate 3.5 g/m2 i.v. over 4 h, followed by Leucovorin rescue (15 mg i.v. every 8 h), Vincristine 2 mg i.v. push and Procarbazine 100 mg/m2/day p.o. for 7 days (odd cycles only), given every 2 weeks for 6 cycles. Patients underwent follow-up evaluation every 3–6 months and annual surveillance brain MRI.
Complete response was defined as complete disappearance of lymphomatous infiltrates on post-treatment ophthalmological examination. Overall survival (OS) was calculated from pathological diagnosis until date of death from any cause or last follow-up. Kaplan Meier survival curves were constructed, censoring patients at the time of death or last follow-up. This study was approved by our institutional review board, in accordance with the declaration of Helsinki.
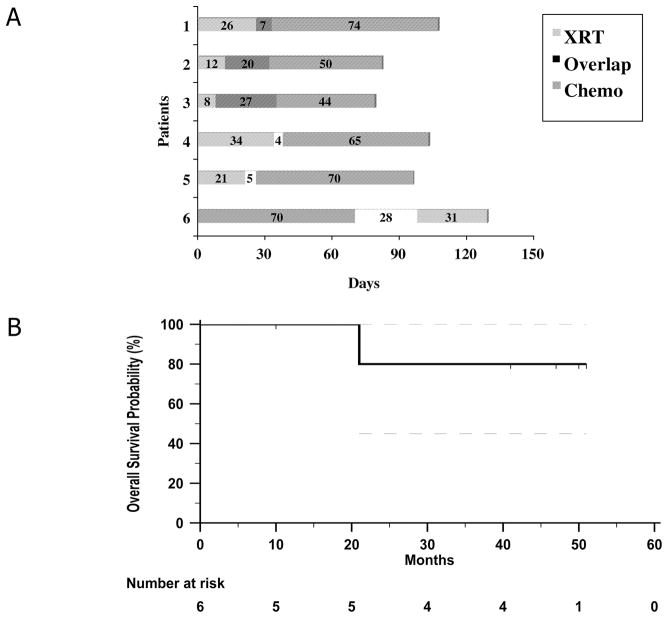
Patient characteristics, clinical and pathological findings, treatment and follow-up data are summarized in Table I. As illustrated in Figure 1a, five patients initially received radiation therapy, followed by chemotherapy, with partial overlap in 3 patients. One patient was first treated with chemotherapy due to personal preference, but thereafter completed a course of ocular radiation therapy. All six patients (4 male, 2 female, median age 61.5 years) completed therapy without major interruptions, delays or side effects and achieved a complete remission (CR). We did not observe any adverse ocular effects during concomitant administration of chemo- and radiotherapy. During median follow-up of 44 (range 10–51) months, one patient developed parenchymal brain relapse and died 21 months after initial diagnosis (Figure 1b), while the remaining 5 patients have maintained CR for a median of 40 months (range 5–47 months). Three patients developed radiation-induced cataract and vascular retinopathy with median latency of 11.5 months (range 5–16 months) after radiation therapy. No other treatment-related long-term side effects have been observed.
Table I.
Clinical features, treatment, and outcome of 6 patients with primary intraocular lymphoma (PIOL)
| Pt | Age | Sex | Symptoms | Laterality | Ophthalmological findings | Treatment* | Ocular complications (latency after RT) | Response | DFS | OS | Vital status | Visual function at last follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 64 | M | Floaters | Bilateral | Vitreous cells, subretinal/choroidal infiltrates | RT (36 Gy), CT × 6, 7 d overlap | None | CR | 16 | 21 | Death due to parenchymal CNS relapse |
Right - 20/30 Left - 20/20 |
| 2 | 59 | M | Blurry vision | Right | Vitreous cells, multifocal subretinal/choroidal infiltrates | RT (36 Gy), CT × 6, 20 d overlap | Vascular retinopathy Cataract (11 months) | CR | 47 | 51 | Alive |
Right - 20/40 Left - 20/20 |
| 3 | 66 | M | Decreased visual acuity, “foggy” | Left | Vitreous cells, subretinal/choroidal and macular infiltrates | RT (36 Gy), CT × 6, 27 d overlap | Cataract Vascular retinopathy 12/16 months) | CR | 46 | 50 | Alive |
Right - 20/20 Left - 20/40 |
| 4 | 71 | F | Decreased visual acuity, “blurry” | Bilateral | Vitreous cells, multifocal subretinal/choroidal infiltrates | RT (40 Gy), CT × 6, sequential (4 d gap) | None | CR | 34 | 41 | Alive |
Right 20/20 Left 20/20 |
| 5 | 59 | M | Floaters | Bilateral | Vitreous cells | RT (36 Gy), CT × 6, sequential (5 d gap) | None | CR | 5 | 10 | Alive |
Right 20/30 Left 20/25 |
| 6 | 55 | F | Decreased visual acuity, ”flakes and floaters” | Bilateral | Vitreous cells, multifocal subretinal/choroidal infiltrates | CT × 6, RT (30 Gy), sequential (28 d gap) | Cataract Vascular retinopathy (5 months) | CR | 40 | 47 | Alive |
Right - 20/30 Left 20/25 |
Abbreviations: M=male, F=female, RT=radiation therapy (given to both eyes in all patients), CT=chemotherapy, d = day, CR=complete remission, DFS=disease-free survival, OS=overall survival, CNS=central nervous system.
exact treatment sequence illustrated in separate graph (Figure 1a)
Figure 1.
Treatment and outcome of PIOL patients. (A) Treatment sequence of radiation therapy (XRT) and chemotherapy in 6 patients with PIOL; (B) Overall Survival of 6 patients with isolated PIOL treated with a combination of binocular external beam radiation therapy and systemic chemotherapy containing high-dose methotrexate (modified de Angelis regimen). Dashed lines represent 95% confidence interval.
Historically, binocular radiation therapy of 30–45 Gy has been the mainstay of treatment for PIOL, yielding response rates of 60–97%, with frequent complete remissions and long-term local control. However, this treatment modality has only minimal impact on OS (Margolis et al, 1980), because CNS relapse occurs in almost all patients after a median of 37 (11 to 84) months, with median survival of 12 to 20 months, thus limiting 5-year OS after radiotherapy to 10 to 29% (Peterson et al, 1993).
Systemic chemotherapy offers the possibility of preventing CNS recurrence and potentially treating the intraocular disease. However, the latter may be difficult, since high-dose intravenous methotrexate, the single most effective agent in the treatment of PCNSL, has been shown to achieve therapeutic, albeit lower concentrations in the vitreous (median 3.4 μM) than in the aqueous humor and cerebrospinal fluid 4 h after administration of 8 g/m2 as a 4-h infusion – a very high dose with significant risk for potentially serious side effects (Batchelor et al, 2003). Moreover, only seven of nine patients with therapeutic drug levels (1 μM or greater) responded to therapy and intraocular relapse occurred in three patients, indicating that chemotherapy with high-dose methotrexate as a single modality may not be sufficient for the treatment of PIOL. We also observed persistence of PIOL in one of our patients (Patient 6) who was first treated with chemotherapy, but subsequently received ocular radiation, resulting in CR.
In a retrospective study from the Memorial Sloan Kettering Cancer Center (Hormigo et al, 2004), eight patients with isolated PIOL were treated with different systemic chemotherapy regimens – most containing either high-dose methotrexate at 3.5 g/m2 and/or high-dose cytarabine at 3 g/m2 or higher - and ocular radiation therapy. Six of eight patients (75%) achieved a CR. Five of eight patients (63%) developed progressive disease in the CNS after a median of 10 months (range 8–25 months), while the other 3 patients remained in CR for a median of 44 months (range 6–47 months). While this approach was similar to ours, it produced inferior results. The total dose, fractionation and sequencing of radiation therapy with chemotherapy that was not uniform, were not specified and may account for the observed difference in outcome compared to our patients. However, considering the small patient numbers, it is possible that these differences are due to chance.
To our knowledge, we present the first report in the literature using a uniform and highly effective treatment approach in a series of patients with isolated PIOL. Further studies of this promising combination regimen in larger cohorts of patients with isolated PIOL are needed.
Acknowledgments
Supported by RO1 CA109335 and RO1 CA122105 from the United States Public Health Service - National Institutes of Health and Dwoskin Family Foundation.
References
- Abrey LE, Yahalom J, DeAngelis LM. Treatment for primary CNS lymphoma: the next step. J Clin Oncol. 2000;18:3144–3150. doi: 10.1200/JCO.2000.18.17.3144. [DOI] [PubMed] [Google Scholar]
- Akpek EK, Ahmed I, Hochberg FH, Soheilian M, Dryja TP, Jakobiec FA, Foster CS. Intraocular-central nervous system lymphoma: clinical features, diagnosis, and outcomes. Ophthalmology. 1999;106:1805–1810. doi: 10.1016/S0161-6420(99)90341-X. [DOI] [PubMed] [Google Scholar]
- Batchelor TT, Kolak G, Ciordia R, Foster CS, Henson JW. High-dose methotrexate for intraocular lymphoma. Clin Cancer Res. 2003;9:711–715. [PubMed] [Google Scholar]
- Freeman LN, Schachat AP, Knox DL, Michels RG, Green WR. Clinical features, laboratory investigations, and survival in ocular reticulum cell sarcoma. Ophthalmology. 1987;94:1631–1639. doi: 10.1016/s0161-6420(87)33256-7. [DOI] [PubMed] [Google Scholar]
- Grimm SA, Pulido JS, Jahnke K, Schiff D, Hall AJ, Shenkier TN, Siegal T, Doolittle ND, Batchelor T, Herrlinger U, Neuwelt EA, Laperriere N, Chamberlain MC, Blay JY, Ferreri AJ, Omuro AM, Thiel E, Abrey LE. Primary intraocular lymphoma: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Ann Oncol. 2007;18:1851–1855. doi: 10.1093/annonc/mdm340. [DOI] [PubMed] [Google Scholar]
- Hoffman PM, McKelvie P, Hall AJ, Stawell RJ, Santamaria JD. Intraocular lymphoma: a series of 14 patients with clinicopathological features and treatment outcomes. Eye (Lond) 2003;17:513–521. doi: 10.1038/sj.eye.6700378. [DOI] [PubMed] [Google Scholar]
- Hormigo A, Abrey L, Heinemann MH, DeAngelis LM. Ocular presentation of primary central nervous system lymphoma: diagnosis and treatment. Br J Haematol. 2004;126:202–208. doi: 10.1111/j.1365-2141.2004.05028.x. [DOI] [PubMed] [Google Scholar]
- Jahnke K, Korfel A, Komm J, Bechrakis NE, Stein H, Thiel E, Coupland SE. Intraocular lymphoma 2000–2005: results of a retrospective multicentre trial. Graefes Arch Clin Exp Ophthalmol. 2006;244:663–669. doi: 10.1007/s00417-005-0138-9. [DOI] [PubMed] [Google Scholar]
- Margolis L, Fraser R, Lichter A, Char DH. The role of radiation therapy in the management of ocular reticulum cell sarcoma. Cancer. 1980;45:688–692. doi: 10.1002/1097-0142(19800215)45:4<688::aid-cncr2820450412>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Peterson K, Gordon KB, Heinemann MH, DeAngelis LM. The clinical spectrum of ocular lymphoma. Cancer. 1993;72:843–849. doi: 10.1002/1097-0142(19930801)72:3<843::aid-cncr2820720333>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]