Abstract
Enzyme replacement therapy (ERT) with intravenous recombinant human alpha-l-iduronidase (IV rhIDU) is a treatment for patients with mucopolysaccharidosis I (MPS I). Spinal cord compression develops in MPS I patients due in part to dural and leptomeningeal thickening from accumulated glycosaminoglycans (GAG). We tested long-term and every three month intrathecal (IT) and weekly IV rhIDU in MPS I dogs age 12-15 months (Adult) and MPS I pups age 2-23 days (Early) to determine whether spinal cord compression could be reversed, stabilized, or prevented. Five treatment groups of MPS I dogs were evaluated (n=4 per group): IT+IV Adult, IV Adult, IT+IV Early, 0.58 mg/kg IV Early and 1.57 mg/kg IV Early. IT+IV rhIDU (Adult and Early) led to very high iduronidase levels in cervical, thoracic, and lumber spinal meninges (3,600-29,000% of normal), while IV rhIDU alone (Adult and Early) led to levels that were 8.2-176% of normal. GAG storage was significantly reduced from untreated levels in spinal meninges of IT+IV Early (p<0.001), IT+IV Adult (p=0.001), 0.58 mg/kg IV Early (p=0.002) and 1.57 mg/kg IV Early (p<0.001) treatment groups. Treatment of dogs shortly after birth with IT+IV rhIDU (IT+IV Early) led to normal to near-normal GAG levels in the meninges and histologic absence of storage vacuoles. Lysosomal storage was reduced in spinal anterior horn cells in 1.57 mg/kg IV Early and IT+IV Early animals. All dogs in IT+IV Adult and IV Adult groups had compression of their spinal cord at 12-15 months of age determined by magnetic resonance imaging and was due to protrusion of spinal disks into the canal. Cord compression developed in 3 of 4 dogs in the 0.58 mg/kg IV Early group; 2 of 3 dogs in the IT+IV Early group; and 0 of 4 dogs in the 1.57 mg/kg IV Early group by 12-18 months of age. IT+IV rhIDU was more effective than IV rhIDU alone for treatment of meningeal storage, and it prevented meningeal GAG accumulation when begun early. High-dose IV rhIDU from birth (1.57 mg/kg weekly) appeared to prevent cord compression due to protrusion of spinal disks.
Keywords: mucopolysaccharidosis, Hurler, intrathecal, enzyme replacement therapy, lysosomal storage disease, spinal cord compression
1. Introduction
Mucopolysaccharidosis I (MPS I) is an inherited lysosomal storage disease due to deficient activity of alpha-l-iduronidase (iduronidase, EC 3.2.1.76), causing accumulation of glycosaminoglycans (GAG) in many organ systems throughout the body [1]. Hematopoietic stem cell transplantation is clinically used for MPS I and can stabilize or prevent mental retardation when given before significant cognitive delay is present [2]. Intravenous (IV) enzyme replacement therapy (ERT) has been in clinical use since 2003 for MPS I [3], and is used for attenuated (Hurler-Scheie, Scheie) patients, Hurler patients who do not receive hematopoietic stem cell transplantation, and patients awaiting transplantation [4]. Spinal cord compression from MPS I in human patients is caused by one or more of the following factors: spinal canal stenosis due to abnormal vertebral development and articulation with secondary proliferation (bone disease), spinal disk disease, ligamentous thickening, and spinal meningeal thickening [5;6]. Compression of the spinal cord can develop in patients treated with IV ERT using recombinant human alpha-l-iduronidase (rhIDU, [7]). This also occurs, though possibly to a lesser extent, in patients receiving hematopoietic stem cell transplantation [8], which may have a greater impact upon skeletal and neurologic disease due to MPS I [2;9].
To better address spinal cord compression and other central nervous system manifestations of MPS I, rhIDU had been administered intrathecally (IT) to MPS I dogs [10;11]. Nineteen MPS I dogs received three to four injections of 0.46 – 1.38 mg rhIDU every week, month, or three months (quarterly) into the cerebrospinal fluid (CSF) at the level of the cisterna magna. This produced a mean of 23 and 300-fold normal levels of iduronidase activity in total brain and meninges, respectively, and reduced mean total brain GAG to normal levels (measured at 48 hours or three months following the final dose). Treatment also achieved a 57-70% reduction in meningeal GAG levels accompanied by histologic improvement in lysosomal storage. The clinical effects of IT rhIDU were difficult to assess as few dogs had neurologic signs at the time of treatment, and treatment was short-term (three or four injections over six months or less). One dog with gait disturbances due to cord compression improved by neurologic assessments after four monthly IT treatments [11].
Here, we studied the effects of long-term IV rhIDU with and without IT rhIDU in canine MPS I. We studied adult animals, after cord compression had developed, and newborn pups to determine the ability of rhIDU to either reverse or prevent spinal cord compression due to meningeal thickening and disk protrusion. We evaluated clinically-relevant endpoints, including neurologic examinations and magnetic resonance imaging (MRI) of the spine, as well as distribution of rhIDU and reduction of GAG storage in cervical, thoracic, and lumbar spinal meninges.
2. Materials and Methods
2.1 Dogs
Animals were bred at Iowa State University (ISU, Ames, IA) or the University of Pennsylvania (Philadelphia, PA). Animals were housed and the studies conducted at ISU and at the Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center (LA BioMed, Torrance, CA), both AAALAC-accredited facilities. The study was approved by the Institutional Animal Care and Use Review Committees for both institutions. Breeding at the University of Pennsylvania colony also occurred under institutionally approved protocols. MPS I dogs were Plott hounds outbred with beagle and/or terrier stock. Affected animals were identified at birth with buccal enzyme assay and PCR. The colony has a mutation in intron 1 of the canine alpha-l-iduronidase gene that results in abnormal mRNA splicing and introduces a premature termination [12].
2.2 Enzyme administration
MPS I dogs received IV with or without IT rhIDU (formulated as laronidase, lot 4986252, 0.58 mg/ml in 150 mM NaCl, 100 mM sodium phosphate, 0.001% polysorbate 80, pH ~5.8, Biomarin Pharmaceutical, Novato, CA). For weekly IV administration, 0.58 mg/kg rhIDU (~114,000 units/kg, administered to IT+IV Adult, IV Adult, IT+IV Early and 0.58 mg/kg IV Early groups) or 1.57 mg/kg rhIDU (~307,000 units/kg, administered to 1.57 mg/kg IV Early group) was diluted with 1 mg/ml canine albumin and 0.9% saline and infused into a cephalic vein over 3 hours as previously described [13]. For IT administration in adult animals, 1.38 mg (~270,000 units) was diluted in Elliotts B artificial spinal fluid solution (Ben Venue Laboratories, Bedford, Ohio) for a total volume of 6.9 mL. This dose was roughly 0.1 mg/kg body weight, or 0.05 mg/ml CSF. For IT administration in young animals, 0.05 mg/kg body weight (~9,800 units/kg, roughly 0.025 mg/ml CSF) was diluted 2 to 1 by volume with Elliotts B, and was begun between 12 and 30 days of age. One IT+IV Early animal (I-141) received the first IT rhIDU at 112 days of age. The smaller dose of IT rhIDU which was selected for Early animals was roughly equivalent to a lower (0.46 mg) dose previously found to be effective in adult MPS I dogs [11]. We reasoned that this lower dose would be sufficient for prevention of GAG accumulation in Early groups but would not suffice for complete reversal of accumulated GAG in Adult animals. IT rhIDU was administered into the cisterna magna as previously described [11]. The frequency of IT injection was every three months (quarterly) in dogs treated early, and in adult animals was monthly for the first four doses and quarterly for the remaining three doses (Table 1).
Table 1.
Study animals
| Experimental group | Subject | Age at first IV rhIDU | Age at first IT rhIDU | Age at necropsy |
|---|---|---|---|---|
| IT+IV Adult | Ig | 15 m | 15 m | 30 m |
| In* | 15 m | 15 m | --- | |
| JL | 14 m | 14 m | 29 m | |
| Ke | 12 m | 12 m | 27 m | |
| IV Adult | My | 14 m | --- | 29 m |
| Mi | 14 m | --- | 29 m | |
| Mx | 14 m | --- | 29 m | |
| Ms | 14 m | --- | 29 m | |
| IT+IV Early | I-141 | 23 d | 112 d | 18.7 m |
| I-180 | 8 d | 12 d | 15.1 m | |
| I-196 | 8 d | 30 d | 17.3 m | |
| I-200 | 8 d | 30 d | 17.1 m | |
| 1.57 mg/kg IV Early | I-176 | 8 d | --- | 12.9 m |
| I-181 | 7 d | --- | 13.1 m | |
| I-197 | 8 d | --- | 13.0 m | |
| I-202 | 7 d | --- | 13.1 m | |
| 0.58 mg/kg IV Early | I-165 | 3 d | --- | 17.6 m |
| I-186 | 9 d | --- | 17.6 m | |
| I-189 | 9 d | --- | 17.6 m | |
| I-205 | 9 d | --- | 17.5 m | |
| I-139* | 2 d | --- | --- | |
| I-140* | 3 d | --- | --- | |
IT: intrathecal, IV: intravenous, m: month, d: day.
I-139 and I-140 died following the initial IV rhIDU administration. Subject “In” and one untreated MPS I dog died during MRI scan.
2.3 Neurologic and other clinical evaluations
Study animals received neurological examinations by a veterinarian, including general appearance, posture, cranial nerve function, motor, cerebellar, sensory and reflex components [14]. Heart rate, body temperature, and respiratory rate were recorded before each IV and IT rhIDU treatment. Body weight measurements were performed weekly for pups and every 2 weeks for adult study animals. Cell counts with differential evaluation, glucose, protein, and anti-iduronidase antibody titers were performed on blood and CSF samples. CSF specimens contaminated with blood were discarded.
Imaging of the spine (first cervical vertebra to first thoracic vertebra) was performed at the Harbor-UCLA Imaging Center or at ISU using a 1.5 Tesla MRI scanner (GE, Waukesha, WI). A screening spine study (T2-weighted fast-spin echo sagittal study of the spine) was first performed, followed by T1-weighted and T2-weighted fast spin echo non-contrast transverse images of regions of interest. Spinal cord compression was scored from the images without knowledge of treatment group, modified from [15]: absent (grade 0), 360-degree cushion of cerebrospinal fluid around the spinal cord; mild (grade 1), loss of cerebrospinal fluid cushion without indentation of the spinal cord or only slight anterior cord flattening; moderate (grade 2), spinal cord compression; severe (grade 3), severe spinal cord compression. Parenchymal hyperintense signal on T2-weighted imaging, spinal disk protrusion, and disk degeneration were noted and the locations recorded.
2.4 Biochemical evaluations
Forty-eight hours after the last IT rhIDU injection, the animals were euthanized by intracardiac phenobarbital overdose, necropsied (without perfusion), and their spinal cords, meninges, and caudae equinae were removed. Spinal meninges consisted of both dura and arachnoid materes. One cervical, thoracic, and lumbar section of spinal cord and meninges were taken from each animal for triplicate iduronidase and GAG assays. Iduronidase assays were performed on tissue homogenates using a 4-methylumbelliferyl substrate (Glycosynth, Cheshire, UK) as previously described [11]. Protein concentrations were determined by the Bradford method using Bio-Rad reagents (Hercules, CA). GAG was assayed using an Alcian blue binding assay with dermatan sulfate standards [16]. Anti-iduronidase antibodies were assayed in serum and CSF as previously described [13;17]. The dilution at which the reading was performed was selected from serial dilutions in the linear range of the assay.
2.5 Pathology
Histopathologic evaluation was performed on samples from neocortical, cervical, thoracic, and lumbar meninges and cervical, thoracic and lumbar spinal cords. Samples were fixed in neutral buffered 10% formalin and stained with toluidine blue or hematoxylin and eosin for light microscopy.
2.6 Statistics
For each sample assayed biochemically (cervical, thoracic, and lumbar meninges), the mean of triplicate experiments was calculated for each animal. Means of the means and their standard deviation were then calculated for each treatment group. For comparison of MRI scoring, age-matched pre-treatment scans from adult animals were analyzed as untreated. Treatment groups were compared using ANOVA with post-hoc Dunnett's test or Tukey-Kramer where appropriate.
3. Results
The study design is summarized in Table 1. Four adult MPS I dogs received IT+IV rhIDU (IT+IV Adult) and four received IV only at the 0.58 mg/kg weekly dose (IV Adult). Early-treated MPS I dogs received treatment with 0.58 mg/kg weekly IV (0.58 mg/kg IV Early), 1.57 mg/kg weekly IV (1.57 mg/kg IV Early), or 0.58 mg/kg weekly IV plus quarterly IT (IT+IV Early) rhIDU beginning at age 2-23 days and continuing for 56-80 weeks.
3.1 Neurologic findings
Neurologic examinations were performed prior to each IT rhIDU treatment, or at 3-month intervals for IV-only treated dogs. Dogs in both IV Early groups had only end-study neurologic examinations. End-study evaluation of one untreated MPS I dog, two IT+IV Early dogs and one 0.58 mg/kg IV Early dog showed spinal pain and crepitus, accompanied in two cases by diminished neck flexion and in another case by neck fasciculations. Two early-treated animals showed cerebellar signs attributed to canine distemper virus (see section 3.5). Several animals showed decreased vision, assessed by testing the menace reflex (blinking on close visual threat), which was attributed to corneal clouding. The remainder of the dogs in the Early groups showed no evidence of ataxia, paresis, or spinal pain.
All adult dogs had evidence of spinal cord compression by MRI at baseline (age 12-15 months) and minor neurological signs on examination. In the IT+IV Adult group, 2 dogs showed overall improvement in the neurologic examination at end study, and 2 showed no change. Improvements included normalization of thoracic and pelvic limb hopping and thoracic limb proprioceptive positioning from decreased/absent to normal in 1 dog and normalization of pelvic limb withdrawal from decreased hock flexion to normal in 1 dog. In the IV Adult (no IT) group, all 4 dogs had overall worsening of the neurologic examination. Decreased distal limb muscle mass (assessed by visual observation and manual palpation) developed in 3 dogs, decreased pelvic limb hopping in 2 dogs, decreased limb withdrawal reflex in 2 dogs, and decreased tactile and proprioceptive positioning of pelvic limb in 1 dog. Two dogs in the IV Adult group developed pain at the thoracolumbar junction, and 1 dog developed ataxia. Worsening of the extensor carpi radialis reflex occurred in two IT+IV Adult and one IV Adult dog. Decreased cranial tibial reflex occurred in one IT+IV Adult dog. One dog in the IT+IV Adult group with signs of spinal cord compression had previously required steroid and anti-inflammatory treatment, which was discontinued due to improved symptoms after two IT doses.
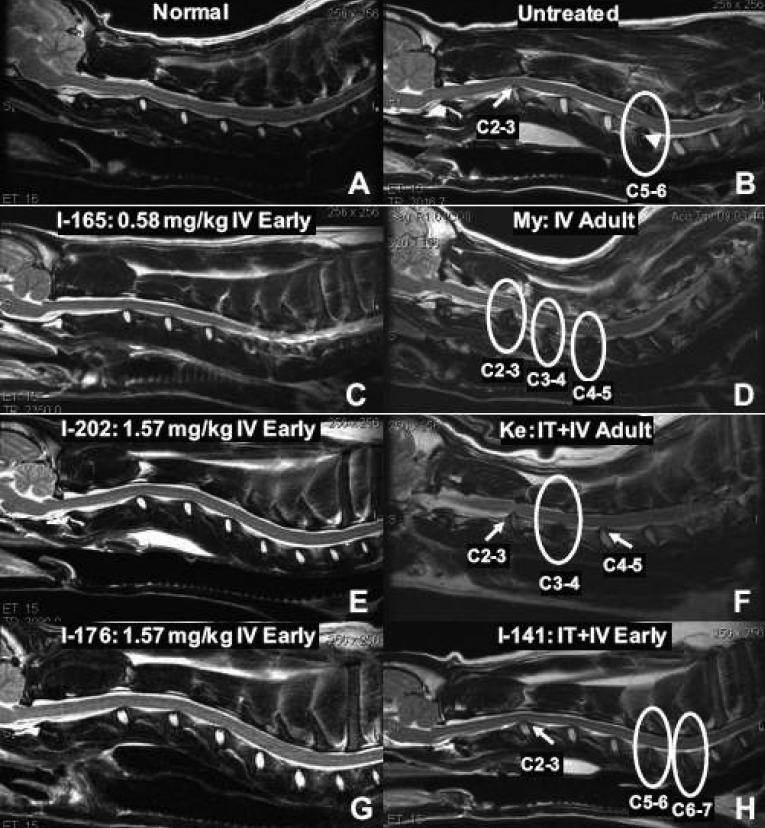
3.2 Magnetic resonance imaging of the spine
Affected MPS I dogs underwent MRI studies of the spinal cord at baseline, and at end study (Table 2). All adult dogs had moderate or severe compression of their spinal cords at baseline (12-15 months of age). Follow-up MRI at end study (27-30 months) showed worsened cord compression (i.e. an increase in the number of compressed levels) in two of four IT+IV Adult dogs, and two of four IV Adult dogs. Cord compression occurred in adult animals secondary to intervertebral disk protrusion (Fig. 1B, D, F) and progressed over time. Parenchymal signal change within the spinal cord occurred in one IV Adult dog and progressed from one to two levels during the study period (not shown). Other findings included spinal disk degeneration and bony proliferation (Table 2). In the early-treatment cohort, two untreated MPS I dogs, four 0.58 mg/kg IV Early, four 1.57 mg/kg IV Early, and three IT+IV Early dogs underwent spinal MRI at 12-19 months. Disk protrusion into the spinal canal was seen in six treated dogs in the Early cohort (three in the IT+IV group and three in the 0.58 mg/kg IV group), and five had mild to moderate spinal cord compression without parenchymal signal change (Fig. 1H). All four dogs in the 1.57 mg/kg IV Early group and one dog in the 0.58 mg/kg IV Early group had no spinal abnormalities detected on MRI (Fig. 1 C, E, G). Post-hoc Tukey-Kramer analysis showed p=0.009 for the number of compressed levels in the group of four 1.57 mg/kg IV Early dogs versus nine 12-19 month-old untreated and pre-treated MPS I dogs.
Table 2.
Spinal abnormalities on MRI in MPS I Dogs
| Cord compression |
Disk disease |
||||||
|---|---|---|---|---|---|---|---|
| Study Group | Subject | Age at study | No. levels | Severity | Signal change (no. levels) | Degeneration (no. levels) | Bony proliferation |
| 1.57 mg/kg IV Early | I-197 | 12 m | 0 | 0 | 0 | 0 | 0 |
| I-202 | 12 m | 0 | 0 | 0 | 0 | 0 | |
| I-176 | 12 m | 0 | 0 | 0 | 0 | 0 | |
| I-181 | 12 m | 0 | 0 | 0 | 0 | 0 | |
| 0.58 mg/kg IV Early | I-165 | 17 m | 0 | 0 | 0 | 0 | 0 |
| I-186 | 17 m | 1 | 1 | 0 | 2 | 0 | |
| I-189 | 17 m | 1 | 2 | 0 | 3 | 2 | |
| I-205 | 17 m | 1 | 1 | 0 | 2 | 0 | |
| IT+IV Early | I-196 | 16 m | 1 | 1 | 0 | 1 | 0 |
| I-180 | 14 m | 0 | 0 | 0 | 3 | 0 | |
| I-141 | 18 m | 1 | 2 | 0 | 3 | 0 | |
| Untreated and Pre-treated (12-19 m) | I-121 | 18 m | 1 | 3 | 1 | 1 | 0 |
| I-134 | 19 m | 1 | 3 | 0 | 2 | 1 | |
| Ig | 15 m | 1 | 2 | 0 | 1 | 0 | |
| In | 15 m | 2 | 2 | 0 | 2 | 1 | |
| JL | 14 m | 1 | 2 | --- | --- | --- | |
| Ke | 12 m | 1 | 2 | 0 | 0 | 0 | |
| My | 14 m | 1 | 2 | 0 | 2 | 2 | |
| Ms | 14 m | 3 | 2 | 0 | 4 | 2 | |
| Mi | 14 m | 3 | 3 | 0 | 4 | 3 | |
| IT+IV Adult | Ig | 30 m | 3 | 2 | 0 | 3 | 2 |
| In | 30 m | 3 | 2 | 0 | 3 | 3 | |
| JL | 29 m | 1 | 1 | 0 | 3 | 2 | |
| Ke | 27 m | 1 | 2 | 0 | 1 | 1 | |
| IV Adult | Mx | 29 m | 3 | 2 | 0 | 5 | 4 |
| My | 29 m | 3 | 2 | 0 | 6 | 2 | |
| Ms | 29 m | 3 | 2 | 0 | 6 | 0 | |
| Mi | 29 m | 3 | 2 | 2 | 6 | 5 | |
| Untreated (28 m) | I-95 | 28 m | 1 | 3 | 1 | 6 | 2 |
| I-87 | 28 m | 1 | 2 | 0 | 3 | 1 | |
IV: intravenous, IT: intrathecal, Un: Untreated (affected), m: months. Motion artifact prevented complete scoring of 14 m scan for Mx and JL. For the spinal cord compression scoring system, see Materials and Methods, section 2.3.
Fig. 1.
Magnetic resonance imaging of the spinal cord. T2-weighted non-contrast sagittal images of the cervical spine. A normal dog (A, age 15 months) showing no abnormalities, and an untreated MPS I dog (B, age 18 months) showing disk protrusion into the canal at C2-3 (arrow) and disk degeneration at C5-6 (circle). Small islands of bony proliferation can be seen within the intervertebral disk at C5-6 (arrowhead). (C, E, G) Spinal MRI of dogs treated with 0.58 mg/kg IV Early (C, age at MRI 17 months) and 1.57 mg/kg IV Early (E, G, age 12 months) showing no abnormalities. (D, F, H) An IV Adult animal at age 29 months (D), an IT+IV Adult dog age 27 months (F) and an IT+IV Early dog age 18 months (H) also show disk degeneration (circles) and disk protrusion (arrows). Circumferential compression is seen in dog Ke (F) at C2-3 (arrow).
3.3 Distribution and iduronidase activity
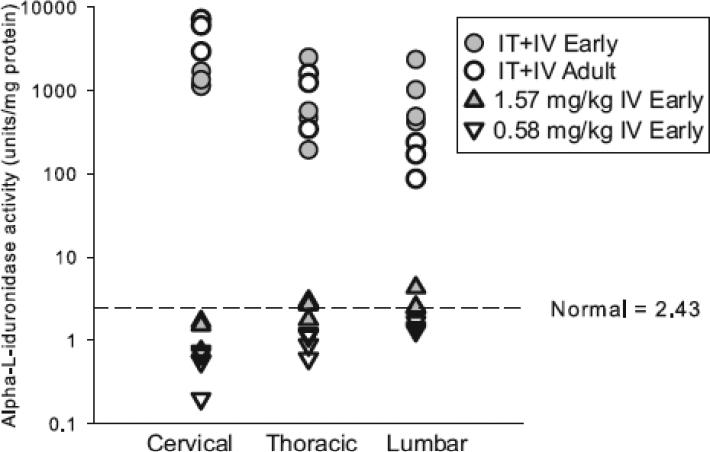
Samples of cervical, thoracic, and lumbar meninges (arachnoid and dura materes) were assayed for iduronidase activity. All intrathecal-treated animals (IT+IV Adult and IT+IV Early groups) had above normal iduronidase activity in the spinal meninges at all three levels, often exceedingly high (range 87.0 to 7,200 units/mg protein, carrier mean 2.43 ± 0.89 units/mg, Fig. 2, Table 3). There was no difference in iduronidase activity levels among animals treated early or as adults. In contrast, animals treated only with IV rhIDU (IV Adult, 0.58 mg/kg IV Early and 1.57 mg/kg IV Early groups) showed lower meningeal iduronidase levels ranging from 0.2 to 4.28 units/mg protein (8.2-176% of normal).
Fig. 2.
Enzymatic activity in spinal meninges following treatment with IV with or without IT rhIDU. Semi-logarithmic scale graph of alpha-l-iduronidase activity in the cervical, thoracic, and lumbar meninges in IT+IV Early (gray circles), IT+IV Adult (open circles), 1.57 mg/kg IV Early (gray triangles), and 0.58 mg/kg IV Early (open inverted triangles) experimental groups. Each animal is represented on the graph.
Table 3.
Activity of alpha-l-iduronidase in spinal meninges
| IT + IV Adult (n=3) | IT + IV Early (n=4) | 0.58 mg/kg IV Early (n=4) | 1.57 mg/kg IV Early (n=3) | |
|---|---|---|---|---|
| Cervical | 5390 ± 2200 | 1330 ± 265 | 0.545 ± 0.242 | 1.32 ± 0.510 |
| Thoracic | 1060 ± 645 | 931 ± 1050 | 0.956 ± 0.268 | 2.49 ± 0.630 |
| Lumbar | 165 ± 75.6 | 1070 ± 892 | 1.43 ± 0.168 | 3.09 ± 1.03 |
| Mean (3-regions) | 2200 ± 785 | 1110 ± 724 | 0.977 ± 0.213 | 2.30 ± 0.585 |
Spinal meningeal iduronidase activity in MPS I unaffected carrier dogs was 2.43 ± 0.894, without substantial regional variation.
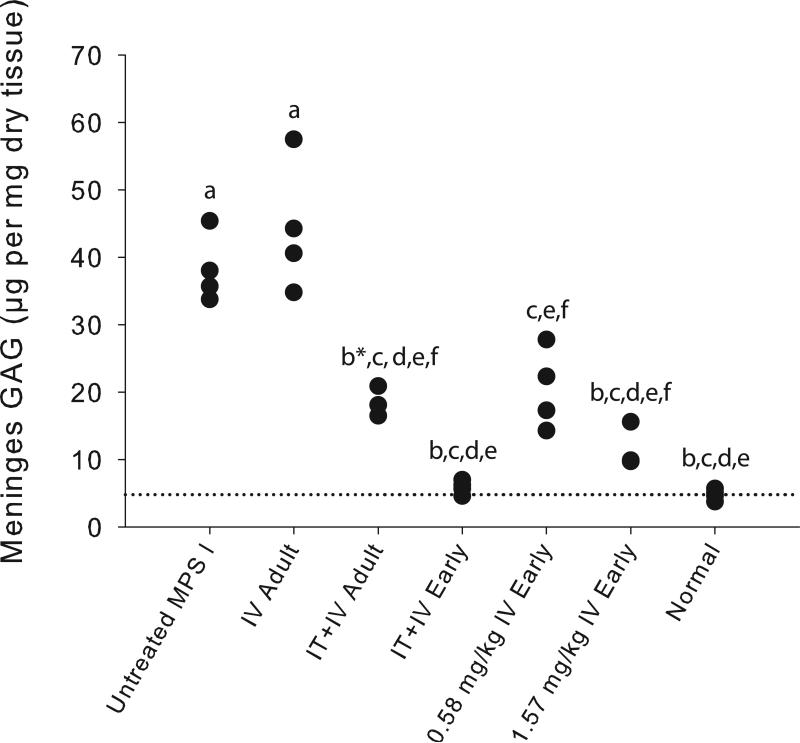
3.4 Reduction of GAG storage
Samples from cervical, thoracic, and lumbar meninges were analyzed separately or averaged to assess reduction of GAG storage following IT and IV rhIDU. Table 4 shows meningeal GAG by spinal region, with statistics performed by post-hoc Dunnett's test (all groups compared to untreated). Untreated animals were age-matched to the early cohort at sacrifice. IT+IV Early, IT+IV Adult, 0.58 mg/kg IV Early and 1.57 mg/kg IV Early rhIDU led to significantly reduced meningeal GAG levels versus untreated animals in all three regions evaluated. The lowest GAG levels were seen in IT+IV Early animals. Figure 3 depicts spinal meningeal GAG averaged over all three regions (cervical, thoracic and lumbar). Tukey-Kramer post-hoc analysis was performed for pooled meningeal GAG (comparison of all treatment and control groups, cervical, thoracic and lumbar combined). This analysis showed statistically significant differences at p<0.01 in multiple treatment groups compared to untreated controls, and between several treatment groups (Fig. 3). IT+IV Early rhIDU led to the lowest meningeal GAG levels (85% reduction vs. untreated MPS I, p<0.001), achieving normal to near-normal meningeal GAG levels in the animals (mean of pooled samples 5.85 ± 1.01, versus normal 4.78 ± 0.82, p=0.34, Fig. 3). There was a 51.6% reduction in meningeal GAG in IT+IV Adult versus untreated MPS I dogs (p=0.001). Treatment from birth with 0.58 mg/kg IV Early or 1.57 mg/kg IV Early rhIDU led to 46.6% (p=0.002) and 69.4% (p<0.001) reduction in GAG levels versus age-matched untreated MPS I animals, respectively. Meningeal GAG was lower in animals treated with early, high-dose IV rhIDU (1.57 mg/kg IV Early, 11.7 ± 3.33) than with the standard dose rhIDU (0.58 mg/kg IV Early, 20.4 ± 5.92). This difference was not statistically significant (p=0.33).
Table 4.
Glycosaminoglycan levels in spinal meninges by region.
| Untreated (n=4) | IT + IV Adult (n=3) | IT + IV Early (n=4) | IV Adult (n=4) | 0.58 mg/kg IV Early (n=4) | 1.57 mg/kg IV Early (n=3) | Normal (n=4) | |
|---|---|---|---|---|---|---|---|
| Cervical | 25.4 ± 6.39 | 13.1 ± 2.89* | 5.80 ± 2.49* | 40.3 ± 9.01 | 18.2 ± 4.40 | 12.6 ± 1.45* | 4.45 ± 0.438 |
| Thoracic | 41.8 ± 8.85 | 18.3 ± 6.13* | 5.47 ± 0.402* | 59.6 ± 21.4 | 19.6 ± 5.75* | 10.4 ± 2.22* | 4.32 ± 1.20 |
| Lumbar | 47.4 ± 7.94 | 24.0 ± 4.89* | 6.27 ± 2.29* | 33.0 ± 3.07* | 23.4 ± 9.03* | 12.2 ± 8.68* | 5.56 ± 2.21 |
p<0.05 versus untreated, by post-hoc Dunnett's test, one-sided
Fig. 3.
Glycosaminoglycan storage in spinal meninges. Quantitative GAG levels in pooled samples from cervical, thoracic, and lumbar meninges in the experimental groups. Each animal is represented on the graph. Untreated MPS I dogs were aged-matched to the early-treatment groups at necropsy. The dotted line indicates the mean of normal animals (4.78 ± 0.818 units/mg). Tukey-Kramer post-hoc analysis yielded results that showed multiple inter group differences. Groups that were similar by statistical analysis are indicated by common letters above each group. Groups with different letter superscripts were significantly different (p<0.01). One comparison (IT+IV Adult versus Normal) was nearly significant at p=0.032.
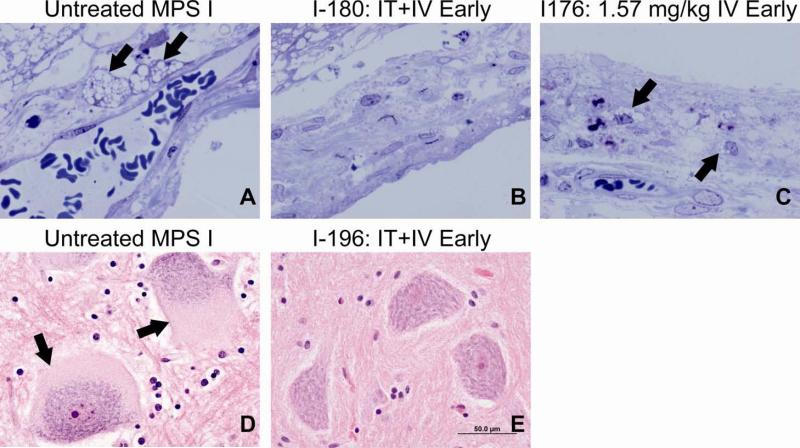
Histologically, lysosomal storage (with the characteristics of GAG) was reduced in meninges of 1.57 mg/kg IV Early MPS I dogs and IT+IV Adult dogs (not shown), and was absent in IT+IV Early dogs (Fig. 4A-C). Spinal anterior horn cells showed large amounts of cytoplasmic pale storage in untreated MPS I animals which was much reduced and in some areas eliminated in 1.57 mg/kg IV Early (not shown) or IT+IV Early animals (Fig. 4D-E). Additional findings included increased cellularity of the dura and mild to marked Wallerian degeneration seen in some untreated, IV-treated, and IT+IV-treated animals alike.
Fig. 4.
Histopathology of meninges and cord. (A-C) Pale lysosomal storage with the characteristics of GAG is indicated by the arrows in toluidine blue-stained neocortical meninges in an untreated MPS I dog (A), an IT+IV Early MPS I dog (B), and a 1.57 mg/kg IV Early MPS I dog (C). (D, E) Hematoxylin and eosin staining of spinal anterior horn cells in an untreated MPS I dog (D) and an IT+IV Early MPS I dog (E). GAG storage is indicated by arrows.
3.5 Safety
No elevation in CSF leukocyte counts occurred in IT-treated dogs. IT+IV Adult and IV Adult dogs developed IgG antibodies to iduronidase in blood and/or CSF. Peak serum ELISA levels in IT+IV Adult and IV Adult animals ranged from 24.8 to 513 OD units/μl (clinical tolerance <20 OD units/μl [13]. CSF anti-iduronidase levels were 10.4 to 13.0 OD units/μl in IT+IV Adult animals. Serum ELISA levels of MPS I dogs in IT+IV Early, 0.58 mg/kg IV Early and 1.57 mg/kg IV Early groups showed that they failed to mount a substantial immune response to the protein antigen. CSF ELISA of IT+IV Early dogs showed undetectable levels of specific IgG antibody in all dogs (clinical tolerance level not known). No inflammatory infiltrate was seen in neocortical or spinal meninges. Two IT+IV Early MPS I dogs showed mild accumulation of cytoplasmic (presumably intralysosomal) lipid in low numbers of macrophages of neocortical meninges on toluidine blue staining of unclear cause. Two early pups died on days 2 and 6, having received IV rhIDU administered within the first 8 hours of life, when colony pup mortality is high (~16% in the first week of life, ISU colony data). One untreated (Kt) and one IT Adult (In) MPS I dog died during anesthesia for magnetic resonance imaging. These animals were included in imaging analyses but not tissue analyses. Two dogs, a 1.57 mg/kg IV Early (I-202, included in the analyses) and an untreated MPS I dog (I-214, not included) developed clinically stable mild to severe cerebellar ataxia, possibly due to an earlier infection with canine distemper virus. Infection could not be confirmed in these dogs due to the chronicity of signs; however, infection was confirmed in other dogs in the colony that displayed CNS signs during this period.
4. Discussion
We studied MPS I dogs treated with IT rhIDU for over one year, to determine whether longer term treatment could stabilize or reverse clinical signs of spinal cord compression. Animals were treated either as adults (after the onset of neurologic disease) or shortly after birth, before neurological deficits associated with cord compression developed, and were compared with age-matched MPS I untreated dogs and MPS I dogs treated with IV rhIDU alone. We found that IT+IV rhIDU was more effective than IV rhIDU alone in addressing lysosomal storage in the spinal meninges, and that treatment from birth with IT injections every 3 months combined with weekly IV rhIDU normalized meningeal GAG in the animals.
Current therapies are inadequate for spinal cord compression in MPS patients. Spinal cord compression can develop in MPS I patients during treatment with enzyme replacement therapy or following bone marrow transplantation [7;8]. Treatment for cord compression requires laminectomy and debridement, frequently at multiple levels, and recurrence or complications may occur [18-20]. Previously, we showed that three or four IT rhIDU injections in adult MPS I dogs could reduce meningeal GAG storage by 57-70% [11]. This was possible because of extremely high enzyme levels in meninges with serial IT injections, several hundred times the levels in carrier animals.
In this study (as in the prior, short-term study [11]), normalization of GAG storage in the meninges of IT+IV Adult animals was not achieved, even after over 1 year of IT+IV rhIDU treatment. However, IT+IV Early enzyme replacement therapy led to normal to near-normal GAG levels in all four treated dogs, showing that prevention of storage is more readily achieved than reversal. IV Adult therapy alone was not successful at reducing meningeal storage in the four adult animals treated. However, 0.58 mg/kg IV Early rhIDU or 1.57 mg/kg IV Early rhIDU did lead to reduced meningeal GAG storage, though levels were still above normal. The lower amounts of enzyme that reach the dura in IV-treated animals may be sufficient to partially prevent but not reverse GAG accumulation there. These findings are consistent with observations that spinal cord compression develops in MPS I patients despite long-term treatment with 0.58 mg/kg weekly IV rhIDU, and suggests that the addition of IT rhIDU may substantially reduce but not normalize meningeal GAG storage once it has accumulated. Clinical trials are ongoing to assess the impact of IT rhIDU on spinal cord compression in MPS I patients with established disease (NCT 00215527 and NCT 00786968).
Long-term IT+IV Adult rhIDU was as effective as short-term treatment (previously published [11]) for reduction of meningeal GAG in adult MPS I dogs. Spinal meningeal GAG levels in four IT+IV Adult dogs treated long-term (15 months) showed a 51% reduction in meningeal GAG, which was comparable to short-term IT+IV treatment in nineteen previously published animals [11], even though the long-term animals were slightly older at sacrifice (28.7 vs. 24.2 months, p=0.03). Adult dogs used in the current study were not tolerant to rhIDU, while Early dogs were tolerant despite the lack of immune suppressive therapy. Immune tolerance to recombinant human N-acetylgalactosamine-4-sulphatase improved clearance of dural storage in IT-treated MPS VI cats [21], and tolerance to rhIDU enhanced the efficacy of IV rhIDU for systemic manifestations in the MPS I dog [17]. Our study was also limited by small numbers of animals per treatment group. Neurologic examinations were not conducted in blinded fashion, as the examiner also administered IT injections.
Previously, we reported clinical improvement of neurologic signs in a single adult MPS I dog treated with short-term IT+IV rhIDU [11]. In the current long-term experiment, the clinical response was more modest and was characterized mostly by stable neurologic signs. MRI of the spine did not show improvement in dogs treated with IT+IV Adult dogs, despite improvement in neurologic examination and meningeal GAG storage. The dura mater cannot be reliably measured on MRI, so change in meningeal thickness could not be assessed. While in human MPS I patients meningeal GAG storage is a major contributor to spinal cord compression, the MPS I dogs showed cord compression due to extradural factors (spinal disk protrusion into the canal) which would not be expected to respond to IT rhIDU. Prevention of spinal cord compression in 1.57 mg/kg IV Early MPS I dogs and attenuation of cord compression in 0.58 mg/kg IV Early and IT+IV Early dogs is likely due to the effects of early IV rhIDU on the spine. Similar results have been seen in MPS I and MPS VII dogs receiving high-dose gene therapy beginning in the neonatal period [22]. Neither intervertebral disk protrusion into the canal nor intravertebral disk degeneration occurred in 1.57 mg/kg IV Early dogs; however as these animals were imaged slightly earlier than untreated or 0.58 mg/kg IV Early, IT+IV Early and IV Early Adult animals (12 months versus 12-18 months), the data do not exclude an age effect. Spinal anterior horn cells showed marked reduction in GAG by histology in IT+IV Early and 1.57 mg/kg IV Early-treated animals. Adult animals treated with short-term IT+IV rhIDU had previously not shown improvement in these neurons [11]. The clinical impact of GAG storage in spinal anterior horn cells is not known.
Newborn screening is currently being developed for MPS I [23]. If screening is widely used, infants with MPS I may begin therapy soon after birth, either with hematopoietic stem cell transplantation (particularly if the genotype predicts Hurler syndrome), or with enzyme replacement therapy, or a combination of enzyme therapy followed by transplantation. Currently, MPS I Hurler patients are identified at a median age of 0.8 years, but individuals with Hurler-Scheie and Scheie forms of MPS I have median ages of diagnosis of 3.9 and 9.8 years, respectively [24]. It is not clear how early intervention must be initiated in MPS I patients to prevent extradural and intradural spinal cord compression. Early intravenous enzyme replacement therapy has been recently shown to be extremely effective in canine MPS I for treatment of systemic disease (Dierenfeld et al., in preparation), and may have prevented intervertebral disk protrusion into the spinal canal. However, while systemic MPS I disease, including spine disease and atrioventricular valve thickness and storage, responded well to early initiation of IV, prevention of storage accumulation in the spinal meninges may require IT enzyme therapy, perhaps on a quarterly (every three month) basis.
Acknowledgment
We gratefully acknowledge the assistance of Sahil Shah, Dr. Larisa Troitskaya, and Jennifer Dancourt with experimental procedures at LA BioMed at Harbor-UCLA, and the many undergraduates who cared for and managed the ISU canine colony. Funding was provided by a grant from the National Institutes of Health (NS054242 to PID), the Ryan Foundation (NME), the Center for Integrated Animal Genomics/ISU (NME), and the State of Iowa Board of Regents Battelle Platform and Infrastructure Grant Programs (NME). Additional affected and breeding animals were provided by Drs. Mark E. Haskins (NIH RR002512, University of Pennsylvania) and Katherine P. Ponder (NIH DK066448, Washington University St. Louis). Recombinant enzyme was donated by Biomarin Pharmaceutical Inc. (Novato, CA).
Abbreviations
- IT
intrathecal
- IV
intravenous
- MPS
mucopolysaccharidosis
- rhIDU
recombinant human alpha-l-iduronidase
- GAG
glycosaminoglycans
- ERT
enzyme replacement therapy
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Neufeld EF, Muenzer J. The mucopolysaccharidoses. In: Scriver CR, Beaudet AL, Valle D, Sly WS, editors. The Metabolic and Molecular Bases of Inherited Disease. eighth ed McGraw-Hill; New York: 2001. pp. 3421–3452. [Google Scholar]
- 2.Bjoraker KJP, Delaney KBA, Peters CMD, Krivit WMD, Shapiro EGP. Long-term outcomes of adaptive functions for children with mucopolysaccharidosis I (Hurler Syndrome) treated with hematopoietic stem cell transplantation. J. Dev. Beh. Pediat. 2006;27:290–296. doi: 10.1097/00004703-200608000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Kakkis ED, Muenzer J, Tiller GE, Waber L, Belmont J, Passage M, Izykowski B, Phillips J, Doroshow R, Walot I, Hoft R, Neufeld E. Enzyme-replacement therapy in mucopolysaccharisosis I. N. Engl. J. Med. 2001;344:182–188. doi: 10.1056/NEJM200101183440304. [DOI] [PubMed] [Google Scholar]
- 4.Tolar J, Grewal SS, Bjoraker KJ, Whitley CB, Shapiro EG, Charnas L, Orchard PJ. Combination of enzyme replacement and hematopoietic stem cell transplantation as therapy for Hurler syndrome. Bone Marrow Transpl. 2007;41:531–535. doi: 10.1038/sj.bmt.1705934. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy P, Swash M, Dean MF. Cervical cord compression in mucopolysaccharidosis. Dev. Med. Child Neurol. 1973;15:194–199. doi: 10.1111/j.1469-8749.1973.tb15160.x. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman HH, Rosenberg HS, Scott CI, Lee YY, Pruessner JL, Butler IJ. Cervical myelopathy due to dural compression in mucopolysaccharidosis. Surg. Neurol. 1982;17:404–410. doi: 10.1016/s0090-3019(82)80004-9. [DOI] [PubMed] [Google Scholar]
- 7.Sifuentes M, Doroshow R, Hoft R, Mason G, Walot I, Diament M, Okazaki S, Huff K, Cox GF, Swiedler SJ, Kakkis ED. A follow-up study of MPS I patients treated with laronidase enzyme replacement therapy for 6 years. Mol. Genet. Metab. 2007;90:171–180. doi: 10.1016/j.ymgme.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Kachur EMD, Del Maestro RMD. Mucopolysaccharidoses and spinal cord compression: Case report and review of the literature with implications of bone marrow transplantation. Neurosurg. 2000;47:223–229. doi: 10.1097/00006123-200007000-00046. [DOI] [PubMed] [Google Scholar]
- 9.Boelens JJ, Wynn RF, O'Meara A, Veys P, Bertrand Y, Souillet G, Wraith JE, Fischer A, Cavazzana-Calvo M, Sykora KW, Sedlacek P, Rovelli A, Uiterwaal CSPM, Wulffraat N. Outcomes of hematopoietic stem cell transplantation for Hurler's syndrome in Europe: A risk factor analysis for graft failure. Bone Marrow Transpl. 2007;40:225–233. doi: 10.1038/sj.bmt.1705718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kakkis E, McEntee M, Vogler C, Le S, Levy B, Belichenko P, Mobley W, Dickson P, Hanson S, Passage M. Intrathecal enzyme replacement therapy reduces lysosomal storage in the brain and meninges of the canine model of MPS I. Mol. Genet. Metab. 2004;83:163–174. doi: 10.1016/j.ymgme.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Dickson P, McEntee M, Vogler C, Le S, Levy B, Peinovich M, Hanson S, Passage M, Kakkis E. Intrathecal enzyme replacement therapy: successful treatment of brain disease via the cerebrospinal fluid. Mol. Genet. Metab. 2007;91:61–68. doi: 10.1016/j.ymgme.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menon KP, Tieu PT, Neufeld EF. Architecture of the canine IDUA gene and mutation underlying canine mucopolysaccharidosis I. Genomics. 1992;14:763–768. doi: 10.1016/s0888-7543(05)80182-x. [DOI] [PubMed] [Google Scholar]
- 13.Kakkis E, Lester T, Yang R, Tanaka C, Anand V, Lemontt J, Peinovich M, Passage M. Successful induction of immune tolerance to enzyme replacement therapy in canine mucopolysaccharidosis I. Proc. Natl. Acad. Sci. USA. 2004;101:829–834. doi: 10.1073/pnas.0305480101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliver JE, Lorenz MD. Handbook of Veterinary Neurology. second ed. WB Saunders; Philadelphia: 1993. [Google Scholar]
- 15.Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: Effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurg. 2003;52:1081–1088. [PubMed] [Google Scholar]
- 16.Kakkis ED, McEntee MF, Schmidtchen A, Neufeld EF, Ward DA, Gompf RE, Kania S, Bedolla C, Chien SL, Shull RM. Long-term and high-dose trials of enzyme replacement therapy in the canine model of mucopolysaccharidosis I. Biochem. Mol. Med. 1996;58:156–167. doi: 10.1006/bmme.1996.0044. [DOI] [PubMed] [Google Scholar]
- 17.Dickson P, Peinovich M, McEntee M, Lester T, Le S, Krieger A, Manuel H, Jabagat C, Passage M, Kakkis E. Immune tolerance improves the efficacy of enzyme replacement therapy in the canine model of mucopolysaccharidosis I. J. Clin. Invest. 2008;118:2868–2876. doi: 10.1172/JCI34676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mut M, Cila A, VarlI K, Akalan N. Multilevel myelopathy in Maroteaux-Lamy syndrome and review of the literature. Clinical Neurology and Neurosurgery. 2005 Apr.107(3):230–235. doi: 10.1016/j.clineuro.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Sostrin RD, Hasso AN, Peterson DI, Thompson JR. Myelographic features of mucopolysaccharidoses: a new sign. Radiol. 1977;125:421–424. doi: 10.1148/125.2.421. [DOI] [PubMed] [Google Scholar]
- 20.Diethelm-Okita B, Whitley C. Cervical cord compression in mucopolysaccharidosis diseases, Abstract #3071. Presented at the 59th Annual Meeting of The American Society of Human Genetics, October 24, 2009, Honolulu, Hawaii. available at http://www.ashg.org/2009meeting/abstracts/fulltext/
- 21.Auclair D, Finnie J, White J, Nielsen T, Fuller M, Kakkis E, Cheng A, O'Neill CA, Hopwood JJ. Repeated intrathecal injections of recombinant human 4-sulphatase remove dural storage in mature mucopolysaccharidosis VI cats primed with a short-course tolerisation regimen. Mol. Genet. Metab. doi: 10.1016/j.ymgme.2009.10.002. In Press. [DOI] [PubMed] [Google Scholar]
- 22.Herati RS, Knox VW, O'Donnell P, D'Angelo M, Haskins ME, Ponder KP. Radiographic evaluation of bones and joints in mucopolysaccharidosis I and VII dogs after neonatal gene therapy. Mol. Genet. Metab. 2008;95:142–151. doi: 10.1016/j.ymgme.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blanchard S, Sadilek M, Scott CR, Turecek F, Gelb MH. Tandem mass spectrometry for the direct assay of lysosomal enzymes in dried blood spots: application to screening newborns for mucopolysaccharidosis I. Clin. Chem. 2008;54:2067–2070. doi: 10.1373/clinchem.2008.115410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pastores GM, Arn P, Beck M, Clarke JTR, Guffon N, Kaplan P, Muenzer J, Norato DYJ, Shapiro E, Thomas J, Viskochil D, Wraith JE. The MPS I registry: Design, methodology, and early findings of a global disease registry for monitoring patients with mucopolysaccharidosis type I. Mol. Genet. Metab. 2007;91:37–47. doi: 10.1016/j.ymgme.2007.01.011. [DOI] [PubMed] [Google Scholar]